Submitted:
15 January 2025
Posted:
16 January 2025
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
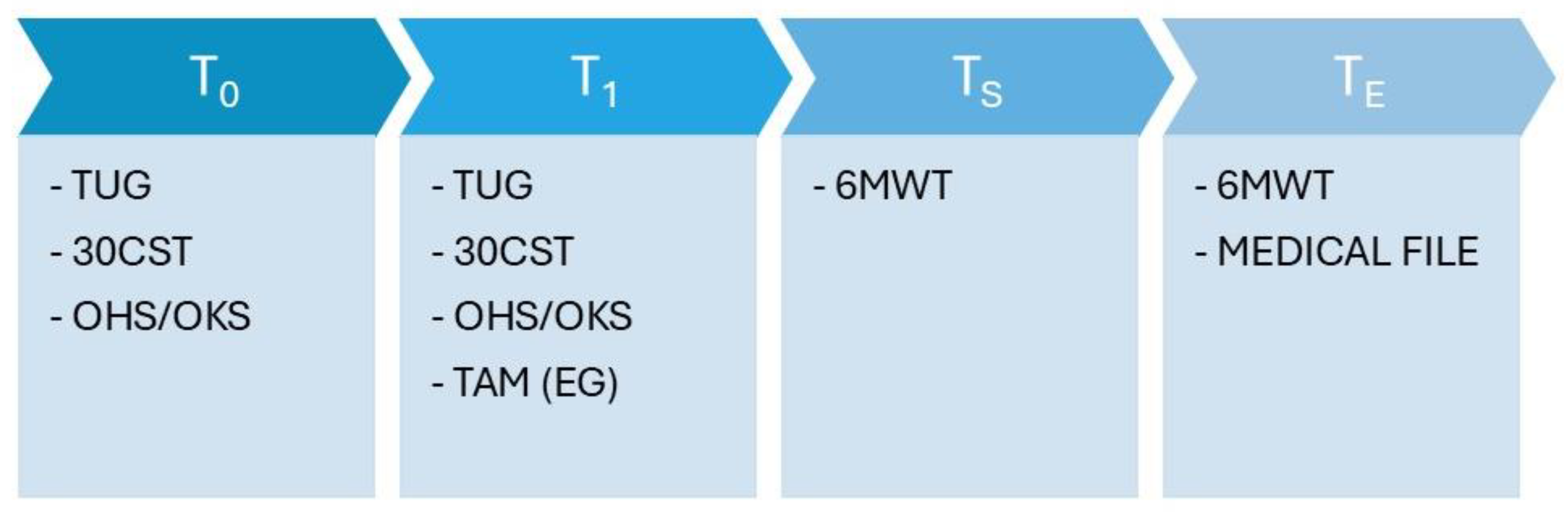
2.2. Study Protocol
2.3. Physical Assessment
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Torre, M.; Ceccarelli, S.; Biondi, A.; Carrani, E.; Masciocchi, M.; Cornacchia, A. Registro Italiano ArtroProtesi. Report Annuale 2020. 2021.
- Bhave, A.; Marker, D.R.; Seyler, T.M.; Ulrich, S.D.; Plate, J.F.; Mont, M.A. Functional Problems and Treatment Solutions After Total Hip Arthroplasty. J. Arthroplasty 2007, 22, 116–124. [Google Scholar] [CrossRef] [PubMed]
- Coudeyre, E.; Jardin, C.; Givron, P.; Ribinik, P.; Revel, M.; Rannou, F. Could Preoperative Rehabilitation Modify Postoperative Outcomes after Total Hip and Knee Arthroplasty? Elaboration of French Clinical Practice Guidelines. Ann. Réadapt. Médecine Phys. 2007, 50, 189–197. [Google Scholar] [CrossRef]
- Rooks, D.S.; Huang, J.; Bierbaum, B.E.; Bolus, S.A.; Rubano, J.; Connolly, C.E.; Alpert, S.; Iversen, M.D.; Katz, J.N. Effect of Preoperative Exercise on Measures of Functional Status in Men and Women Undergoing Total Hip and Knee Arthroplasty. Arthritis Care Res. 2006, 55, 700–708. [Google Scholar] [CrossRef] [PubMed]
- Tew, G.A.; Ayyash, R.; Durrand, J.; Danjoux, G.R. Clinical Guideline and Recommendations on Pre-operative Exercise Training in Patients Awaiting Major Non-cardiac Surgery. Anaesthesia 2018, 73, 750–768. [Google Scholar] [CrossRef] [PubMed]
- Moorthy, K.; Wynter-Blyth, V. Prehabilitation in Perioperative Care. Br. J. Surg. 2017, 104, 802–803. [Google Scholar] [CrossRef]
- Snow, R.; Granata, J.; Ruhil, A.V.S.; Vogel, K.; McShane, M.; Wasielewski, R. Associations Between Preoperative Physical Therapy and Post-Acute Care Utilization Patterns and Cost in Total Joint Replacement. J. Bone Jt. Surg. 2014, 96, e165. [Google Scholar] [CrossRef]
- Fernandes, L.; Roos, E.M.; Overgaard, S.; Villadsen, A.; Søgaard, R. Supervised Neuromuscular Exercise Prior to Hip and Knee Replacement: 12-Month Clinical Effect and Cost-Utility Analysis alongside a Randomised Controlled Trial. BMC Musculoskelet. Disord. 2017, 18, 5. [Google Scholar] [CrossRef] [PubMed]
- Saw, M.M.; Kruger-Jakins, T.; Edries, N.; Parker, R. Significant Improvements in Pain after a Six-Week Physiotherapist-Led Exercise and Education Intervention, in Patients with Osteoarthritis Awaiting Arthroplasty, in South Africa: A Randomised Controlled Trial. BMC Musculoskelet. Disord. 2016, 17, 236. [Google Scholar] [CrossRef] [PubMed]
- Su, W.; Zhou, Y.; Qiu, H.; Wu, H. The Effects of Preoperative Rehabilitation on Pain and Functional Outcome after Total Knee Arthroplasty: A Meta-Analysis of Randomized Controlled Trials. J. Orthop. Surg. 2022, 17, 175. [Google Scholar] [CrossRef] [PubMed]
- Durrand, J.; Singh, S.J.; Danjoux, G. Prehabilitation. Clin. Med. 2019, 19, 458–464. [Google Scholar] [CrossRef] [PubMed]
- Punnoose, A.; Claydon-Mueller, L.S.; Weiss, O.; Zhang, J.; Rushton, A.; Khanduja, V. Prehabilitation for Patients Undergoing Orthopedic Surgery: A Systematic Review and Meta-Analysis. JAMA Netw. Open 2023, 6, e238050. [Google Scholar] [CrossRef] [PubMed]
- Kisner, C.; Colby, L.A.; Borstad, J. Therapeutic Exercise Foundations and Techniques; F.A. Davis Company: Philadelphia, Pennsylvania, 2017. [Google Scholar]
- Svinøy, O.-E.; Bergland, A.; Risberg, M.A.; Pripp, A.H.; Hilde, G. Better before–Better after: Efficacy of Prehabilitation for Older Patients with Osteoarthritis Awaiting Total Hip Replacement—a Study Protocol for a Randomised Controlled Trial in South-Eastern Norway. BMJ Open 2019, 9, e031626. [Google Scholar] [CrossRef] [PubMed]
- Reininga, I.H.F.; Stevens, M.; Wagenmakers, R.; Bulstra, S.K.; Van Den Akker-Scheek, I. Minimally Invasive Total Hip and Knee Arthroplasty—Implications for the Elderly Patient. Clin. Geriatr. Med. 2012, 28, 447–458. [Google Scholar] [CrossRef] [PubMed]
- Karimijashni, M.; Yoo, S.; Barnes, K.; Poitras, S. Pre- and Post-Operative Rehabilitation Interventions in Patients at Risk of Poor Outcomes Following Knee or Hip Arthroplasty: Protocol for Two Systematic Reviews. Adv. Rehabil. Sci. Pract. 2023, 12, 27536351231170956. [Google Scholar] [CrossRef]
- Walls, R.J.; McHugh, G.; O’Gorman, D.J.; Moyna, N.M.; O’Byrne, J.M. Effects of Preoperative Neuromuscular Electrical Stimulation on Quadriceps Strength and Functional Recovery in Total Knee Arthroplasty. A Pilot Study. BMC Musculoskelet. Disord. 2010, 11, 119. [Google Scholar] [CrossRef] [PubMed]
- Stevens, J.E.; Mizner, R.L.; Snyder-Mackler, L. Neuromuscular Electrical Stimulation for Quadriceps Muscle Strengthening After Bilateral Total Knee Arthroplasty: A Case Series. J. Orthop. Sports Phys. Ther. 2004, 34, 21–29. [Google Scholar] [CrossRef]
- Talbot, L.A.; Gaines, J.M.; Ling, S.M.; Metter, E.J. A Home-Based Protocol of Electrical Muscle Stimulation for Quadriceps Muscle Strength in Older Adults with Osteoarthritis of the Knee. J. Rheumatol. 2003, 30, 1571–1578. [Google Scholar] [PubMed]
- Lyons, C.L.; Robb, J.B.; Irrgang, J.J.; Fitzgerald, G.K. Differences in Quadriceps Femoris Muscle Torque When Using a Clinical Electrical Stimulator Versus a Portable Electrical Stimulator. Phys. Ther. 2005, 85, 44–51. [Google Scholar] [CrossRef]
- Lyons, C.L.; Robb, J.B.; Irrgang, J.J.; Fitzgerald, G.K. Differences in Quadriceps Femoris Muscle Torque When Using a Clinical Electrical Stimulator versus a Portable Electrical Stimulator. Phys. Ther. 2005, 85, 44–51. [Google Scholar] [CrossRef]
- De Klerk, T.C.; Dounavi, D.M.; Hamilton, D.F.; Clement, N.D.; Kaliarntas, K.T. Effects of Home-Based Prehabilitation on Pre- and Postoperative Outcomes Following Total Hip and Knee Arthroplasty: A Systematic Review and Meta-Analysis. Bone Jt. Open 2023, 4, 315–328. [Google Scholar] [CrossRef]
- World Medical Association Declaration of Helsinki: Ethical Principles for Medical Research Involving Human Subjects. JAMA 2013, 310, 2191. [CrossRef] [PubMed]
- Kear, B.M.; Guck, T.P.; McGaha, A.L. Timed Up and Go (TUG) Test: Normative Reference Values for Ages 20 to 59 Years and Relationships With Physical and Mental Health Risk Factors. J. Prim. Care Community Health 2017, 8, 9–13. [Google Scholar] [CrossRef] [PubMed]
- Alcazar, J.; Kamper, R.S.; Aagaard, P.; Haddock, B.; Prescott, E.; Ara, I.; Suetta, C. Relation between Leg Extension Power and 30-s Sit-to-Stand Muscle Power in Older Adults: Validation and Translation to Functional Performance. Sci. Rep. 2020, 10, 16337. [Google Scholar] [CrossRef]
- Hamilton, D.F.; Loth, F.L.; MacDonald, D.J.; Giesinger, K.; Patton, J.T.; Simpson, A.H.; Howie, C.R.; Giesinger, J.M. Treatment Success Following Joint Arthroplasty: Defining Thresholds for the Oxford Hip and Knee Scores. J. Arthroplasty 2018, 33, 2392–2397. [Google Scholar] [CrossRef]
- Murray, D.W.; Fitzpatrick, R.; Rogers, K.; Pandit, H.; Beard, D.J.; Carr, A.J.; Dawson, J. The Use of the Oxford Hip and Knee Scores. J. Bone Joint Surg. Br. 2007, 89, 1010–1014. [Google Scholar] [CrossRef]
- Ma, Q.; Liu, L. The Technology Acceptance Model: A Meta-Analysis of Empirical Findings. J. Organ. End User Comput. 2004, 16, 59–72. [Google Scholar] [CrossRef]
- ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories ATS Statement: Guidelines for the Six-Minute Walk Test. Am. J. Respir. Crit. Care Med. 2002, 166, 111–117. [CrossRef]
- Unver, B.; Kahraman, T.; Kalkan, S.; Yuksel, E.; Karatosun, V. Reliability of the Six-Minute Walk Test after Total Hip Arthroplasty. HIP Int. 2013, 23, 541–545. [Google Scholar] [CrossRef] [PubMed]
- Bohannon, R.W.; Crouch, R. Minimal Clinically Important Difference for Change in 6-minute Walk Test Distance of Adults with Pathology: A Systematic Review. J. Eval. Clin. Pract. 2017, 23, 377–381. [Google Scholar] [CrossRef] [PubMed]
- Şavkin, R.; Büker, N.; Güngör, H.R. The Effects of Preoperative Neuromuscular Electrical Stimulation on the Postoperative Quadriceps Muscle Strength and Functional Status in Patients with Fast-Track Total Knee Arthroplasty. Acta Orthop. Belg. 2021, 87, 735–744. [Google Scholar] [CrossRef] [PubMed]
- Asua, J.; Orruño, E.; Reviriego, E.; Gagnon, M.P. Healthcare Professional Acceptance of Telemonitoring for Chronic Care Patients in Primary Care. BMC Med. Inform. Decis. Mak. 2012, 12, 139. [Google Scholar] [CrossRef] [PubMed]
- AlQudah, A.A.; Al-Emran, M.; Shaalan, K. Technology Acceptance in Healthcare: A Systematic Review. Appl. Sci. 2021, 11, 10537. [Google Scholar] [CrossRef]
- Sumin, A.N.; Oleinik, P.A.; Bezdenezhnykh, A.V.; Bezdenezhnykh, N.A. Prehabilitation in Cardiovascular Surgery: The Effect of Neuromuscular Electrical Stimulation (Randomized Clinical Trial). Int. J. Environ. Res. Public. Health 2023, 20, 2678. [Google Scholar] [CrossRef] [PubMed]
- Marin, L.; Albanese, I.; Gentile, F.L.; Patanè, P.; Manzoni, F.; Pedrotti, L.; Ottobrini, S. Scoliosis: Online Exercises versus Telerehabilitation. A Feasibility Trial. Minerva Orthop. 2021, 72. [Google Scholar] [CrossRef]
- Maffiuletti, N.A.; Roig, M.; Karatzanos, E.; Nanas, S. Neuromuscular Electrical Stimulation for Preventing Skeletal-Muscle Weakness and Wasting in Critically Ill Patients: A Systematic Review. BMC Med. 2013, 11, 137. [Google Scholar] [CrossRef]


| Parameter | Time |
| Total time of treatment | 30 min |
| Pulse width | 300 µs |
| Contraction | 6 s |
| Rest | 10 s |
| Ramp | 2 s |
| EG (n = 20, 12F) | HG (n = 20, 8F) | |||
| Pre | Post | Pre | Post | |
| Age | 67.65 (65.07, 70.23) | - | 68.15 (65.54, 70.76) | - |
| Number of sessions (n) | - | 11 (11, 12) | - | 12 (12, 12) |
| Hospitalization days (n) | 14.20 (12.42, 15.98) | - | 14.20 (13.01, 15.39) | - |
| 30CST (n) | 11.95 (10.78, 13.13) | 14.35 (13.07, 15.63)* | 11.35 (9.80, 12.90) | 13.65 (12.19, 15.11) |
| TUG (s) | 11.40 (10.30, 12.51) | 9.30 (8.38, 10.22)* | 10.67 (9.18, 12.15) | 8.87 (7.93, 9.82)* |
| Oxford scale | 23.75 (21.13, 26.38) | 29.75 (27.33, 32.17)* | 26.80 (23.525, 30.08) | 28.60 (25.78, 31.42)* |
| 6MWT (m) | 194.25 (170.44, 218.06) | 336.50 (292.89, 380.11)* | 180.75 (153.46, 208.04) | 271.75 (236.39, 307.12)* |
| TAM | - | 26.26 (25.69, 26.84) | - | - |
| Difference Between Groups(EG – HG) | |||
| Mean difference (95% CI) | p-value | Cohen’s d | |
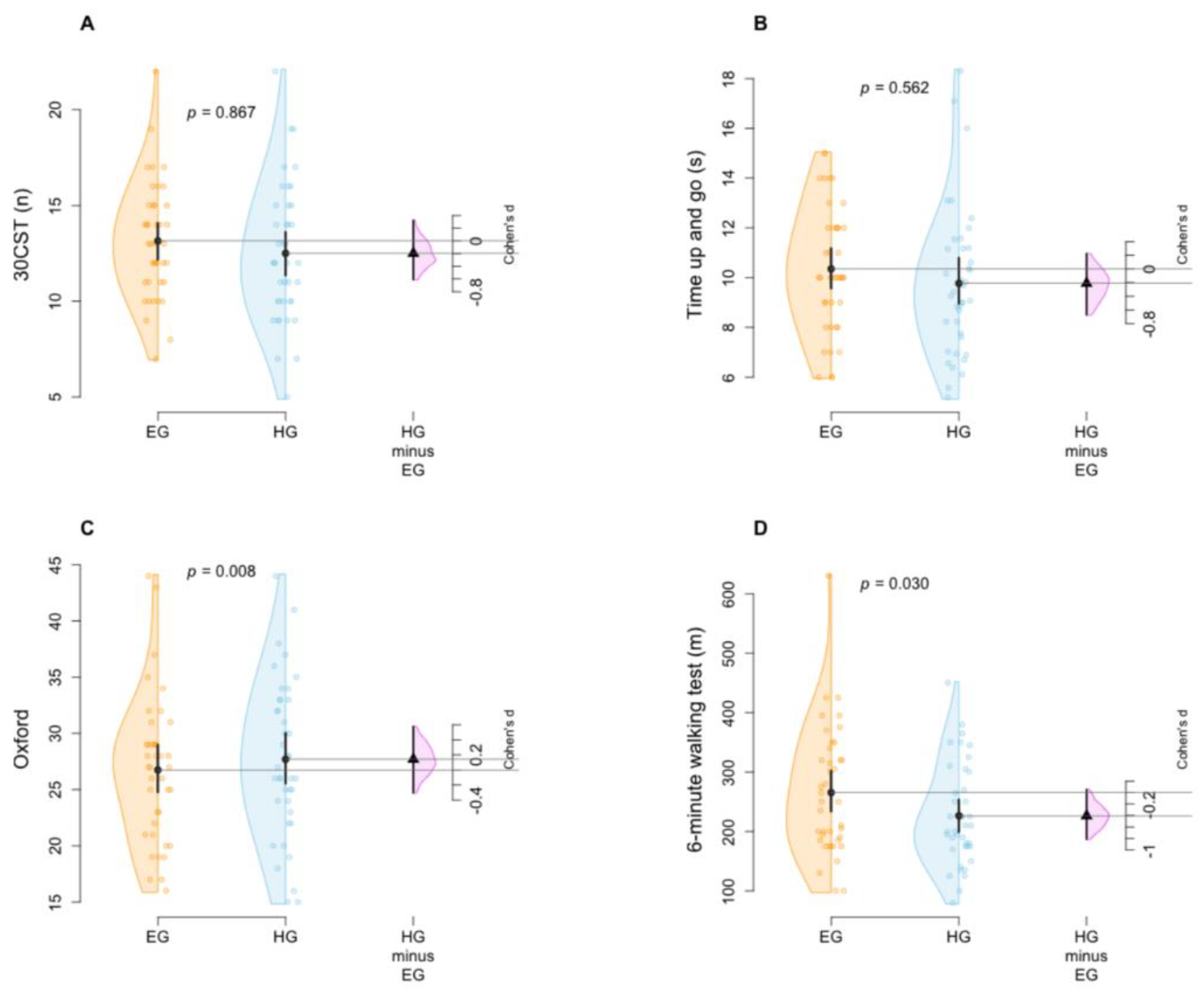
| 30CST (n) | 0.10 (-1.10, 1.30) | 0.867 | 0.196 |
| TUG (s) | -0.31 (-1.37, 0.76) | 0.562 | 0.211 |
| Oxford scale | 4.20 (1.17, 7.23) | 0.008* | 0.142 |
| 6MWT (m) | 41.90 (3.95, 79.84) | 0.030* | 0.405 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).





