1. Introduction
The mandible accounts for the majority of fractures due to trauma. This fact may be related to the anterior position that the mandible occupies in relation to the other bones of the face [
1] . The causes of mandible fractures are varied and include motor vehicle accidents (MVAs), assault, domestic violence, falls, sports and work-related accidents, ballistic injuries, and pathologic fractures[
2]. Angle fractures are the most common among the mandibular fractures[
3]. Computed tomography (CT) has become the gold standard for diagnosis of mandible fractures, offering advantages for both surgical planning and assessing dental involvement[
4]. The internal fixation is used as definitive treatment. There are many methods availed for internal fixations and the Champy's method is one of more acceptable method for internal fixation of mandibular angle fracture[
5]. The Dimensional plate is an alternative fixation system that saves time compared to the standard miniplate and is simultaneously stabilized by a tensile and compressionzone.Itcanbestabilizedsimultaneouslybytensileandcompressionzones.Thisfixationmethodalsomakesthe3-Dplatemalleable, low profile, and easy to apply. [
6]. The stability of the 3-D plate does not derive from the thickness of the plate but from the combination of the screws fixed monocortically to the outer cortex forming cuboid[
7]. 3-D plate holds fracture segments rigidly by resisting the shearing, bending, torsional forces acting around the fracture and minimizes the buccolingual splaying and gap formation in lower border[
8] .
2. Patients and Methods:
The current study was conducted on 16 patients, age ranged from 18-50 years. Ethical approval was obtained from Faculty of Dental Medicine, Assiut branch, Al-Azhar University ethical committee approval (N:AUAREC20220007-7).
2.1. Inclusion Criteria:
Patients older than 18 years and patients who sustained unfavorable mandibular angle fracture requiring internal fixation.
2.2. Exclusion Criteria:
Immune compromised patients, Edentulous patients, Patients with osteoporosis and osteopetrosis, Patients with loss of soft tissue over fracture line.
2.3. Sample Size Calculation:
According to clinical data, sample size calculation was undertake via G power version 3.1 statistical software based on the following pre-established parameters: an alpha-type error of 0.05, a power test of 0.80 and according to the following formula: n= 2(Za+Zb)2 x(S)2/ (d)2.where S = 0.55 and d = 0.60, A total sample of at least 16 subject appeared to be sufficient.
2.4. Grouping :
Divided into 2 groups:
Group I: eight patients treated with 3D curved angle plate.
Group II : eight patients treated with two standard miniplates.
2.5. Evaluation:
Pre and post-operative evaluations were done by clinical and radiographic means. It includes: Orthopantomogram and CT scan. All patients were followed-up for a minimum of 6 months postoperatively. Clinical assessment was done on the 1, 3 and 12 weeks, 3 and 6 months postoperatively.
2.6. Surgical Procedure:
The patient was placed in a supine position and general anesthesia was administered via nasotracheal intubation. Surgical sites were then prepared and draped. Local anesthetic solution (lidocaine) with vasoconstrictor (Epinephrine 1:200,000) was infiltrated along operative area for hemostasis. Cefotax 1000 mg vial and dexamethasone 4 mg ampule was given at beginning of operation in 500ml Saline solution by IV infusion after skin test to exclude allergic complications.
2.7. Surgical Approaches:
Intraoral incision: extending from anterior border of ramus downward and forward along external oblique ridge traversing mucosa, submucosa, buccinator muscle, and periosteum. Reaching buccally on attached gingiva opposite lower second molar region, then reflection of mucoperiosteum was carried out using mucoperiosteal elevator so that fracture line was clearly exposed.
Trans-buccal incision: a triangle shaped zone created. Line 1 (trago-basal line). Line 2 (cantho-gonial line). Line 3 (mandibular line)[
9]. A small extraoral incision (approximately1 cm)corresponding to the fracture site was made. An appropriate titanium miniplate was applied and the fracture site was held intraorally by an assistant. A blunt dissection was made through the extraoral stab incision to facilitate entry of the drill and screw holder cum diver to the fracture site. A hole was drilled ,a screw was placed, and tightened until proper depth and control was achieved.
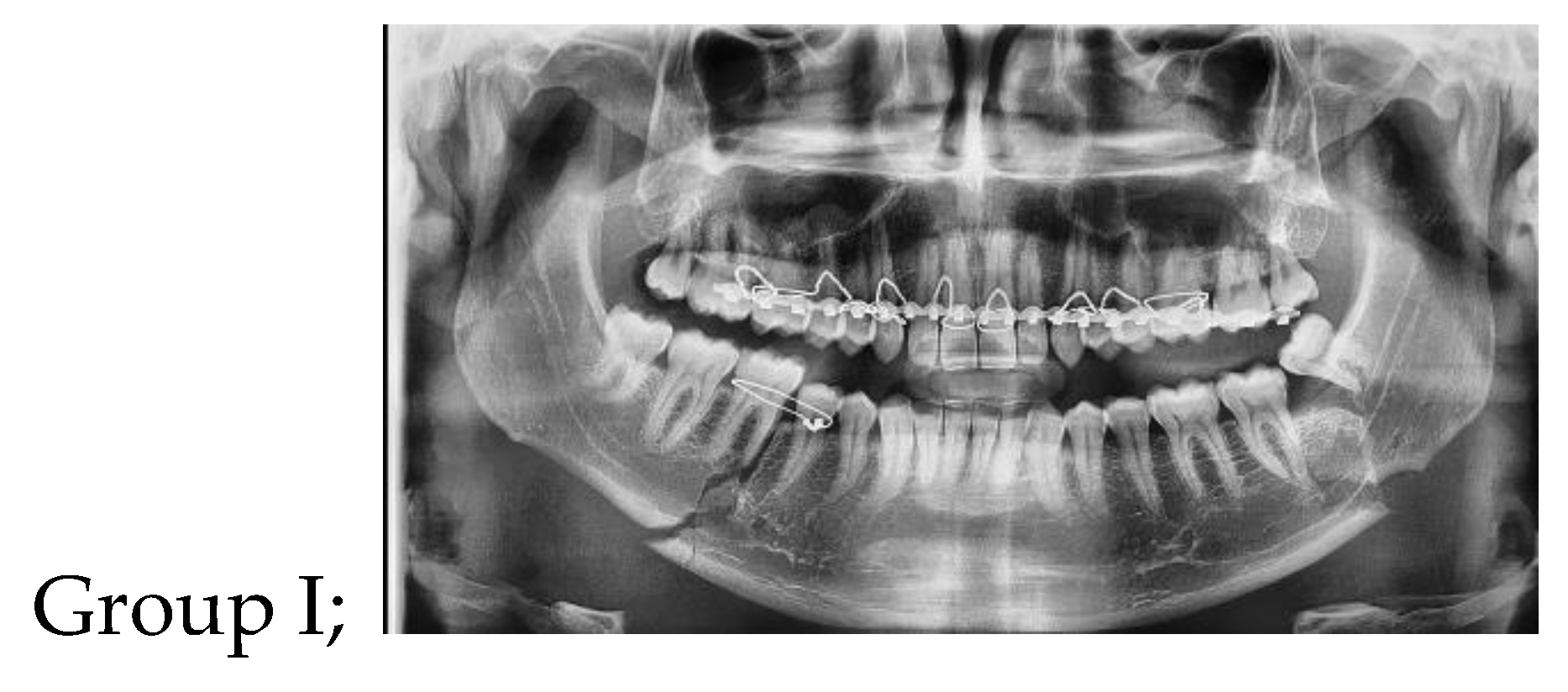
Figure 1.
Photoradiograph of panoramic view showing displaced left mandibular angle and right body fracture
1.
Figure 1.
Photoradiograph of panoramic view showing displaced left mandibular angle and right body fracture
1.
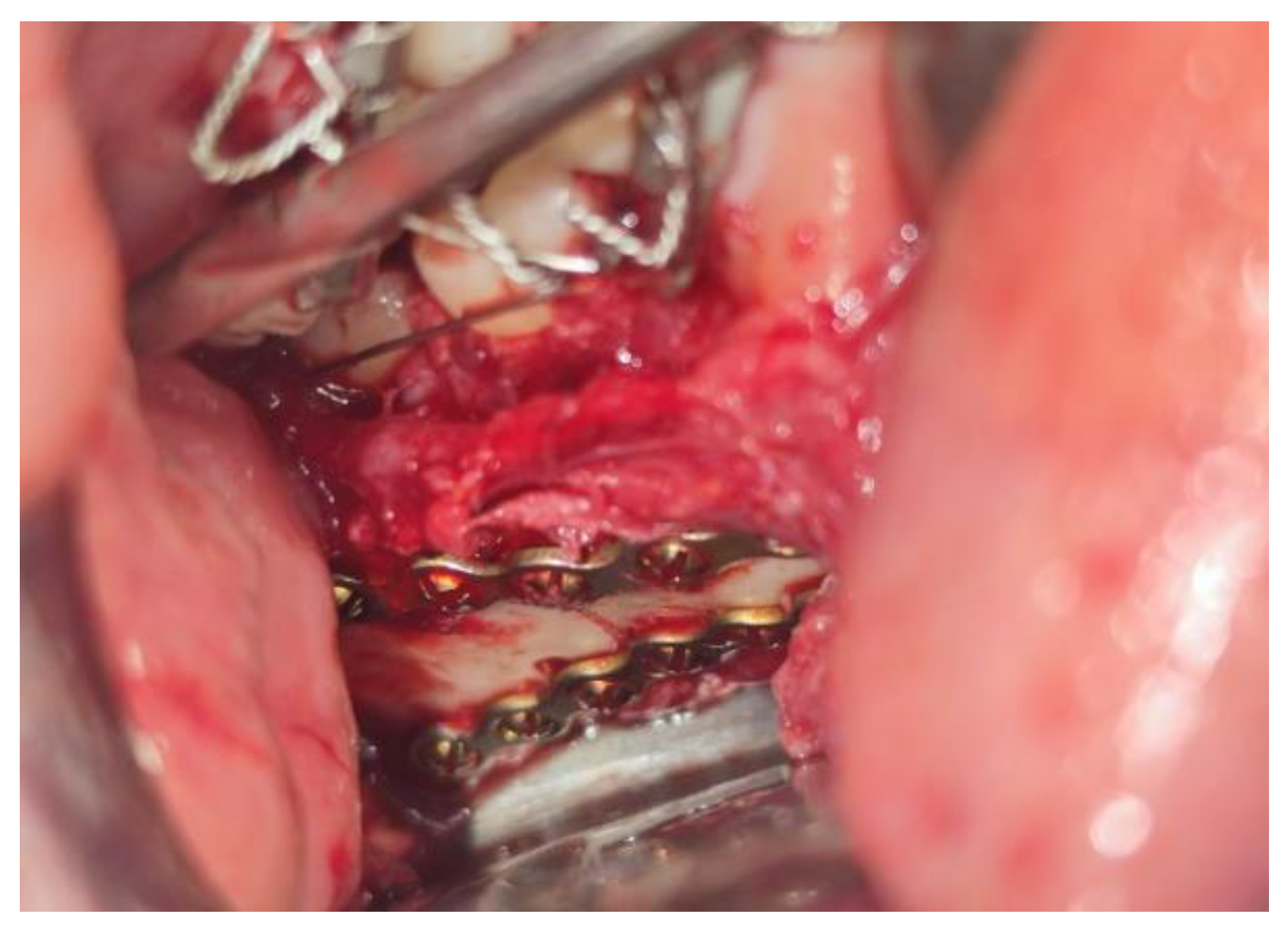
Figure 2.
Clinical photograph showing fixation of displaced mandibular angle fracture by 3D plate 1.
Figure 2.
Clinical photograph showing fixation of displaced mandibular angle fracture by 3D plate 1.
Figure 3.
Photoradiograph of panoramic view showing after 6 months1 .
Figure 3.
Photoradiograph of panoramic view showing after 6 months1 .
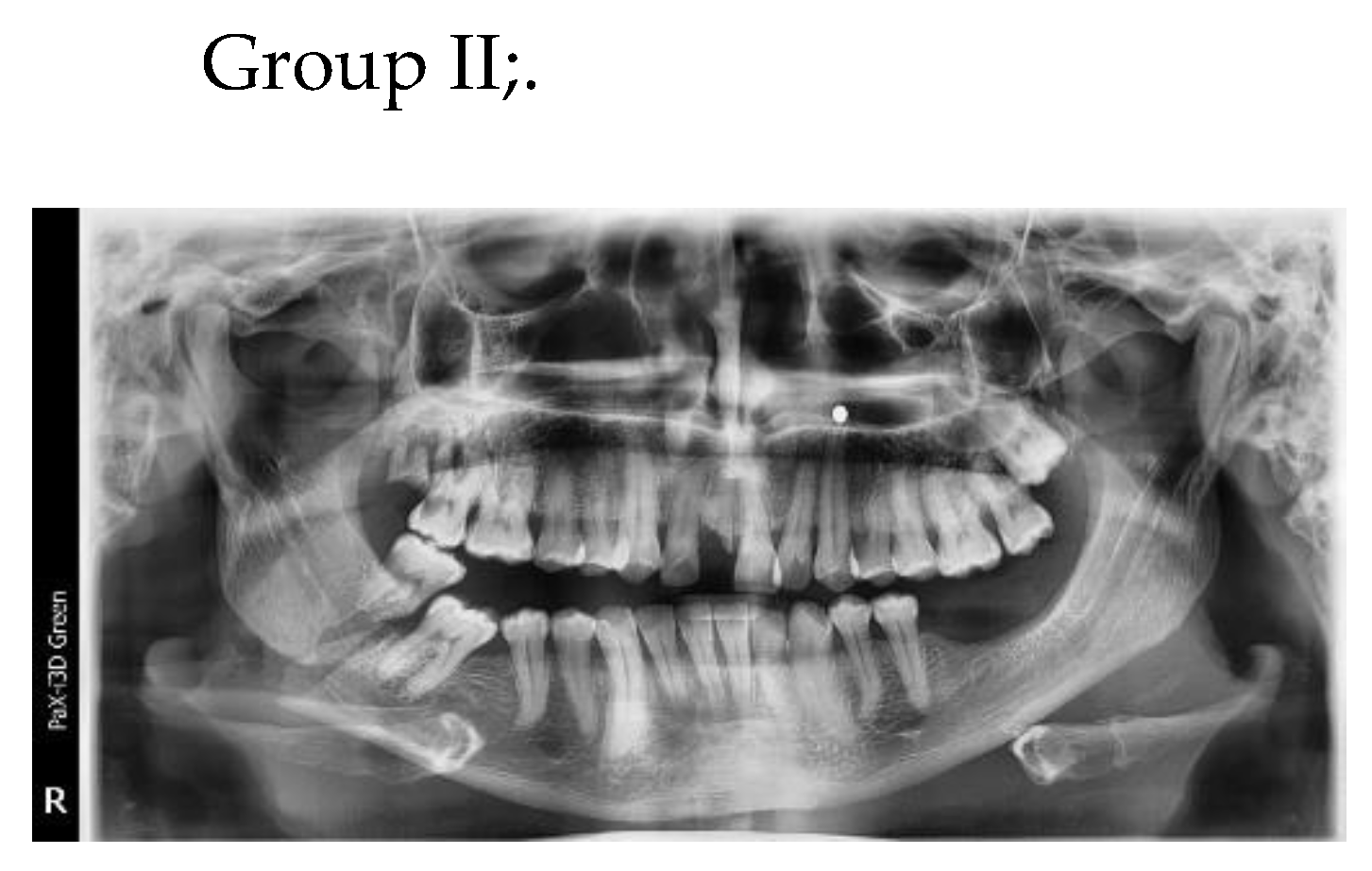
Figure 4.
Photoradiograph of panoramic view showing displaced right mandibular angle fracture1.
Figure 4.
Photoradiograph of panoramic view showing displaced right mandibular angle fracture1.
Figure 5.
Clinical photograph showing fixation of displaced mandibular angle fracture by two 1.
Figure 5.
Clinical photograph showing fixation of displaced mandibular angle fracture by two 1.
Figure 6.
Photoradiograph of panoramic view showing fixation two miniplate after 6 months1 .
Figure 6.
Photoradiograph of panoramic view showing fixation two miniplate after 6 months1 .
3. Results
There was no statistically significant difference in the gender distribution of the two groups. In comparisons between the two groups regarding preoperative, degree of displacement, soft tissue damage, fracture site, occlusal status, edema, and sensory abnormalities, the results were non statistically significant. ( p value >0.05). Comparison of time elapsed since initial trauma and definitive fixation (days) between two groups, the results was non-statistically significant (p value >0.05) was 7.25 days among cases of group I compared to 6.75 days among cases of group II. Regarding the comparison of time elapsed between plate adaptation and definitive fixation (min) between two groups, the results was statistically significant (p value 0.05) as 6 cases out of 8 cases in each study group had no associated fracture, also all cases in both group I and II had no hardware complication and had normal occlusion after 3 month postoperatively. Regarding postoperative elastic, difference was non-statistically significant and all cases in both groups reached to the normal occlusion state after 3 month postoperatively. Regarding the comparison between occlusion state preoperative and 3 month postoperative in each study group separately, the results was highly statistically significant (p value <0.001) as all cases with deranged occlusion preoperatively became normal after 3 month postoperatively either in group I or group II. By comparing between two groups interincisal opening (mm), the result was statistically significant (p value <0.05) as higher among cases of group I (mean=38 ± 2.5) than among cases of group II (mean=35±2.7). By comparing between two groups pre and postoperative intergonial width, the result were non-statistically significant (p value >0.05). By comparing between group I (3D curved angle strut plate) and group II (standard miniplate) regarding Post-operative complication, the results was non-statistically significant (p value >0.05) as only 1 case in group I had Wound dehiscence compared to no case in group II. Regarding the comparison between immediate post-operative bone density and after 6 months in each studied group separately, Results were statistically significant (p value <0.05).
4. Discussion:
ORIF of mandibular fracture includes intraoral and extraoral approach of the fracture site and direct osteosynthesis with transosseous wires, lag screws or miniplates[
10].
Titanium is the metal of choice as a fixation plate primarily; mainly because of its high biocompatibility and ease of manipulation. Titanium 3D plate system, a modification of the miniplate, was developed by Farmand to meet the requirement for semi-rigid fixation with fewer complications [
11]. The 3D plate is so named because of its action of holding the fracture fragment in a rigid way to resist three-dimensional forces, namely shearing, bending, and twisting forces. thus named. [
12].
The average size of the mandibular canal ranges from 2.1 to 4.9 mm. It should be noted that the value of 4.9 mm may be too high because it was determined on panoramic radiographs without taking into account the magnification factor [
13]. Chen et al. reported that no significant difference in mandibular canal diameter at the level of the mental foramen was observed when comparing males and females in American subjects (2.2 mm) and Taiwanese subjects (2.1 mm) using CBCT images [
14]. A study of 100 patients in the first molar region using CBCT cross-sectional images showed that only 8% of the sample had a mandibular canal size <2 mm [
15]. In the present study, making the distance between holes in superior and inferior linear plates 5mm which is more than the average by 0.1 to 2.9 mm, this design gives it an advantage over other designs, with sensory impairment of the inferior alveolar nerve after injury ranging from 5.7 to 58% and persistent sensory impairment ranging from 0.9 to 66.7% [
16]. The plate design consists of two parallel plates joined together to increase load-bearing capacity, with height of 11 mm, length of 34 mm, a distance 7 mm between the outer and inner holes, and a distance of 9 mm between the holes in the middle.
The transbuccal approach was used because it provides good visualization and accessibility and leaves a less noticeable scar. The time required to reduce and fix the MAF using this approach was 19.25 ± 5.1 minutes (Gr. I) and 32 ± 5.7 minutes (Gr. II). The difference in operative time between the two groups was statistically significant (P = 0.003).
An important morphological parameter of the mandible is the gonial angle, Dhara et al. also examined variables of age; gender, and third molar, status and found that these variables were not associated with mandibular angle fractures [
17]. A study by Larrazabal-Moron and Sanchis-Gimeno also found a significant negative correlation between age and gonial angle values(r = −0.365, P < 0.001)[
18]. Panneerselvam et al., however, detected almost twice as many cases of angled fractures as non-angled fractures [
19]. The intergonial width refers to the distance between the two angles of the mandible, and is usually between 82 and 94 mm, with a mean of 88 mm [
20] , In the present study, neither result was statistically significant.
This was the case in the study by Goyal M et al[
21] who found that the 3D plating system was easy to adjust, had a shorter insertion time, and minimal dissection during the surgical phase.
5. Conclusion
The 2.0mm titanium 3D curved angle strut plate is used to fix mandibular angle fractures and has relatively few or no postoperative complications compared with other techniques. It provides greater stability and resists torsional forces in mandibular angle fractures. Due to this exceptional stability, none of the patients in our series required postoperative MMF.
| 1 |
Developed by the authors |
References
- Sangalette BS, Levatti TT, Vieira LV, Filho JLT, Pastori CM, Toledo GL. Treatment of Fracture Sequel in the Mandibular Angle Region. Case Rep Surg. 2019 Jul 4;2019:4627301. [CrossRef]
- Panesar K, Susarla SM. Mandibular Fractures: Diagnosis and Management. Semin Plast Surg. 2021 Oct 11;35(4):238-249. [CrossRef]
- Perez R, Oeltjen JC, Thaller SR. A review of mandibular angle fractures. Craniomaxillofac Trauma Reconstr. 2011 Jun;4(2):69-72. [CrossRef]
- Stanford-Moore G, Murr AH. Mandibular Angle Fractures. Facial Plast Surg Clin North Am. 2022 Feb;30(1):109-116.
- Bohluli B, Mohammadi E, Oskui IZ, Moharamnejad N. Treatment of mandibular angle fracture: Revision of the basic principles. Chin J Traumatol. 2019 Apr;22(2):117-119. [CrossRef]
- Wusiman P, Yarbag A, Wurouzi G, Mijiti A, Moming A. Three dimensional versus standard miniplate fixation in management of mandibular fractures: A systematic review and meta-analysis. J Craniomaxillofac Surg. 2016 Oct;44(10):1646-1654. [CrossRef]
- Kanubaddy, S.R., Devireddy, S.K., Rayadurgam, K.K. et al. Management of Mandibular Angle Fractures: Single Stainless Steel Linear Miniplate Versus Rectangular Grid Plate—A Prospective Randomised Study. J. Maxillofac. Oral Surg. 15, 535–541 (2016). [CrossRef]
- Kanubaddy SR, Devireddy SK, Rayadurgam KK, Gali R, Dasari MR, Pampana S. Management of Mandibular Angle Fractures: Single Stainless Steel Linear Miniplate Versus Rectangular Grid Plate-A Prospective Randomised Study. J Maxillofac Oral Surg. 2016 Dec;15(4):535-541.
- Gulses A, Kilic C, Sencimen M. Determination of a safety zone for transbuccal trocar placement: an anatomical study. Int J Oral Maxillofac Surg. 2012 Aug;41(8):930-3. [CrossRef]
- Barde DH, Mudhol A, Ali FM, Madan RS, Kar S, Ustaad F. Efficacy of 3-dimensional plates over Champys miniplates in mandibular anterior fractures. J Int Oral Health 2014;6:20-6.
- Alkan A et al. Biomechanical comparison of different plating techniques in repair of mandibular angle fractures. Oral Surg Oral Med Oral Pathol Oral Radiol Endod.2007. 104:752–756. [CrossRef]
- Al-Moraissi EA, Mounair RM, El-Sharkawy TM, El-Ghareeb TI. Comparison between three-dimensional and standard miniplates in the management of mandibular angle fractures: a prospective, randomized, double-blind, controlled clinical study. Int J Oral Maxillofac Surg. 2015 Mar;44(3):316-21. [CrossRef]
- Thomas von Arx, Scott Lozanoff. Clinical Oral Anatomy, 2017. ISBN : 978-3-319-41991-6.
- Aung NM, Myint KK. Bifid Mandibular Canal: A Proportional Meta-Analysis of Computed Tomography Studies. Int J Dent. 2023 Mar 6;2023:9939076. [CrossRef]
- Oliveira-Santos C, Capelozza AL, Dezzoti MS, Fischer CM, Poleti ML, Rubira-Bullen IR. Visibility of the mandibular canal on CBCT cross-sectional images. J Appl Oral Sci. 2011 May-Jun;19(3):240-3.
- Thurmuller P, Dodson TB, Kaban LB. Nerve injuries associated with facial trauma: Natural history, management, and outcome of treatment. OMFS Clin of N Amer 2001;13:283–293.
- Chole RH, Patil RN, Balsaraf Chole S, Gondivkar S, Gadbail AR, Yuwanati MB. Association of mandible anatomy with age, gender, and dental status: a radiographic study. ISRN Radiol. 2013 Dec 18;2013:453763. [CrossRef]
- Larrazabal-Moron C, Sanchis-Gimeno JA. Gonial angle growth patterns according to age and gender. Ann Anat. 2018 Jan;215:93-96. [CrossRef]
- Tiwari P, Bera RN, Chauhan N. Magnitude of gonial angle influence on the commonness of mandibular angle fractures. Ann Maxillofac Surg 2020;10:190-4. [CrossRef]
- Ladeira DB, Cruz AD, Almeida SM, Bóscolo FN. Influence of the intergonial distance on image distortion in panoramic radiographs. Dentomaxillofac Radiol. 2012 Jul;41(5):417-21. [CrossRef]
- Goyal M, Marya K, Chawla S, Pandey R. Mandibular osteosynthesis: a comparative evaluation of two different fixation systems using 2.0 mm titanium miniplates and 3-D locking plates. J Oral Maxillofac. Surg 2011:10:32-7.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).