Submitted:
10 January 2025
Posted:
10 January 2025
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Methods
2.1. Literature Search Strategy
2.2. Inclusion and Exclusion Criteria
2.3. Data Extraction
2.4. Quality Assessment
2.5. Statistical Analysis
3. Result
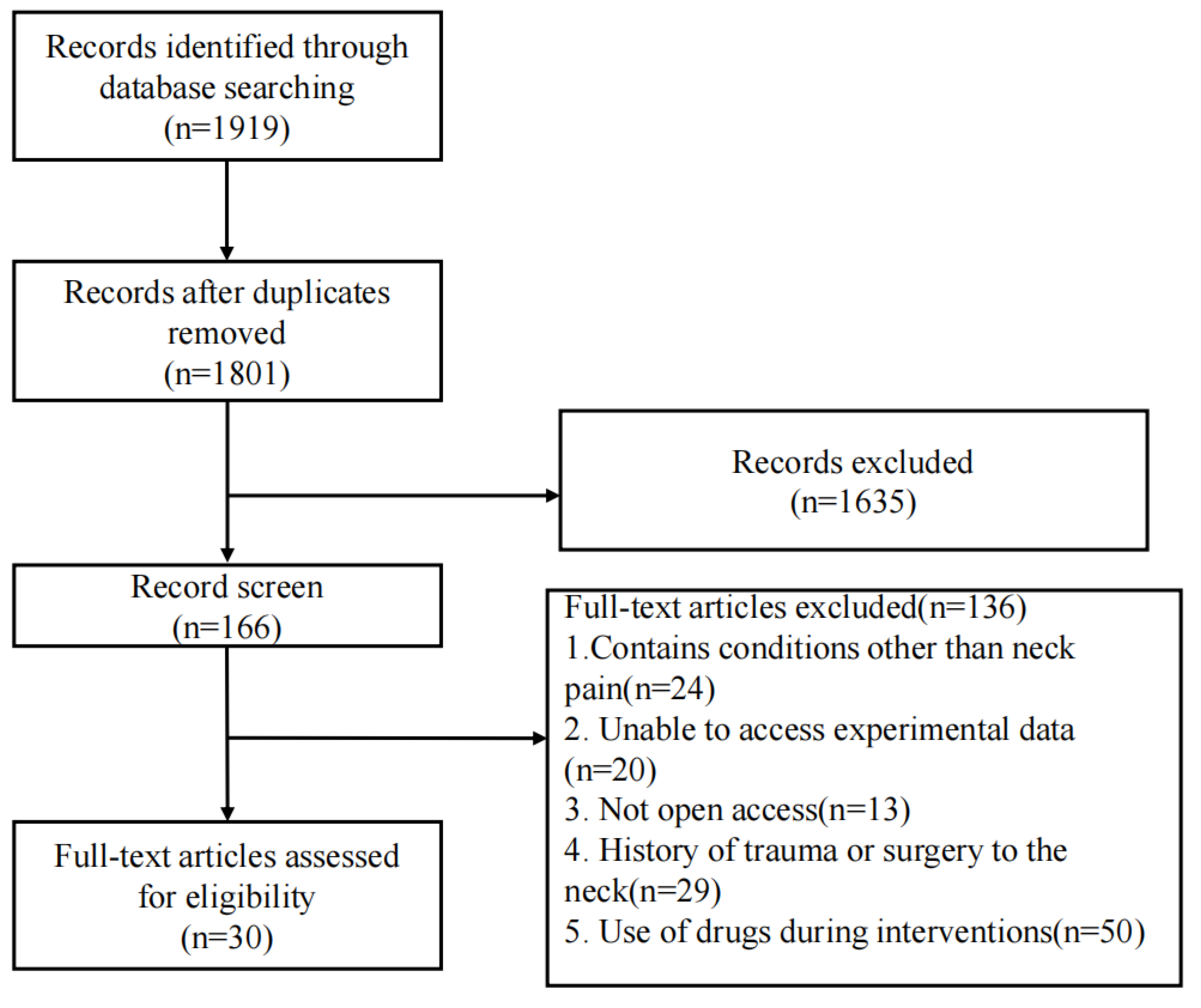
3.1. Literature Selection
3.2. Characteristics of the Included Studies
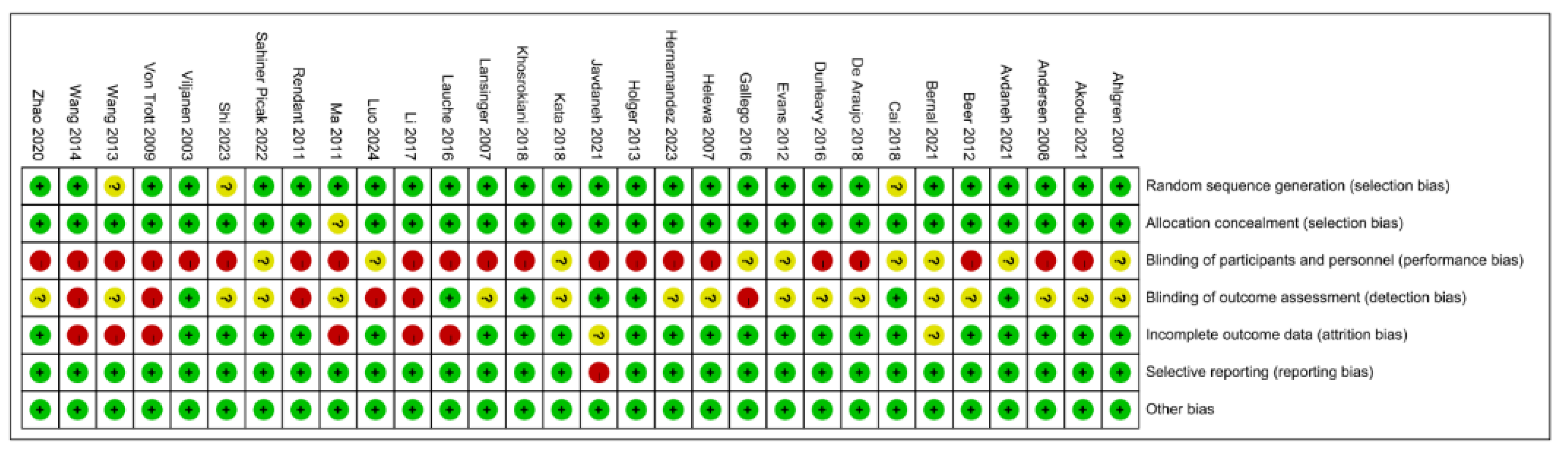
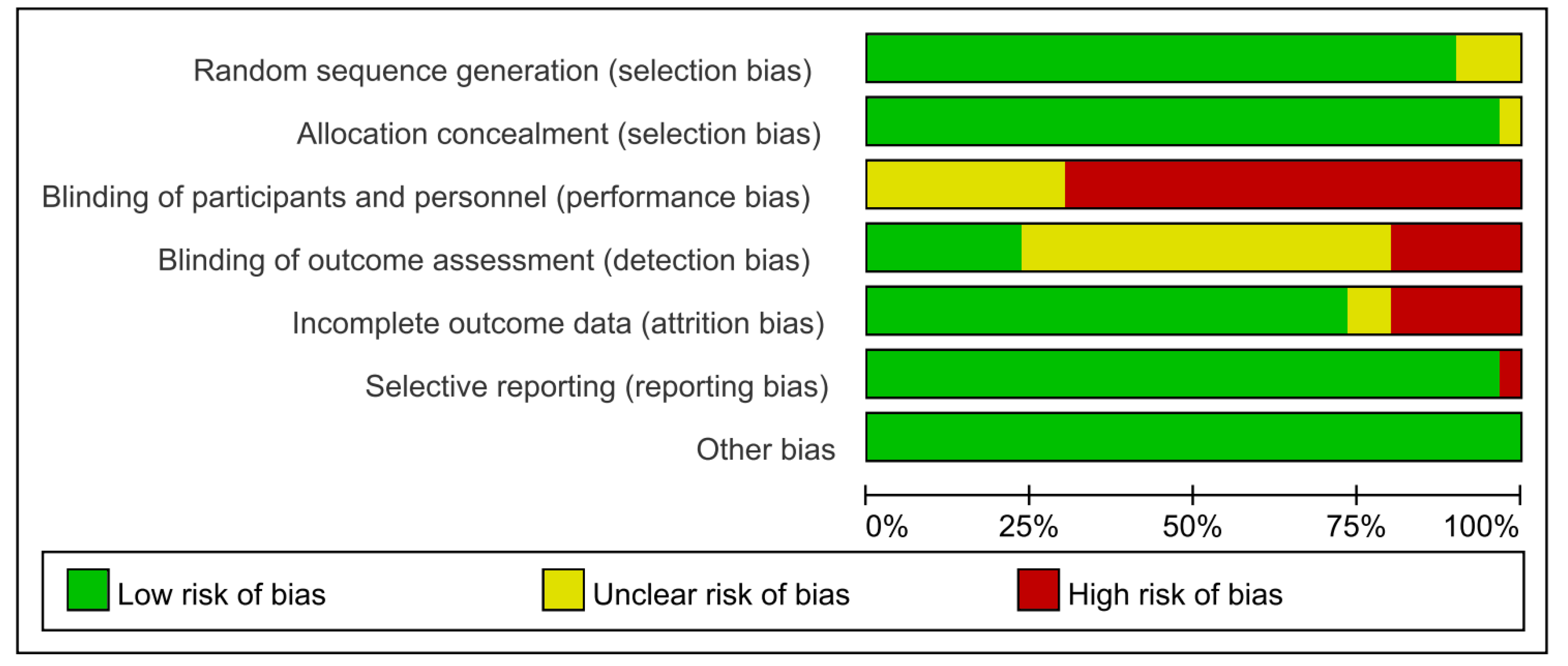
3.3. Result of Assessment
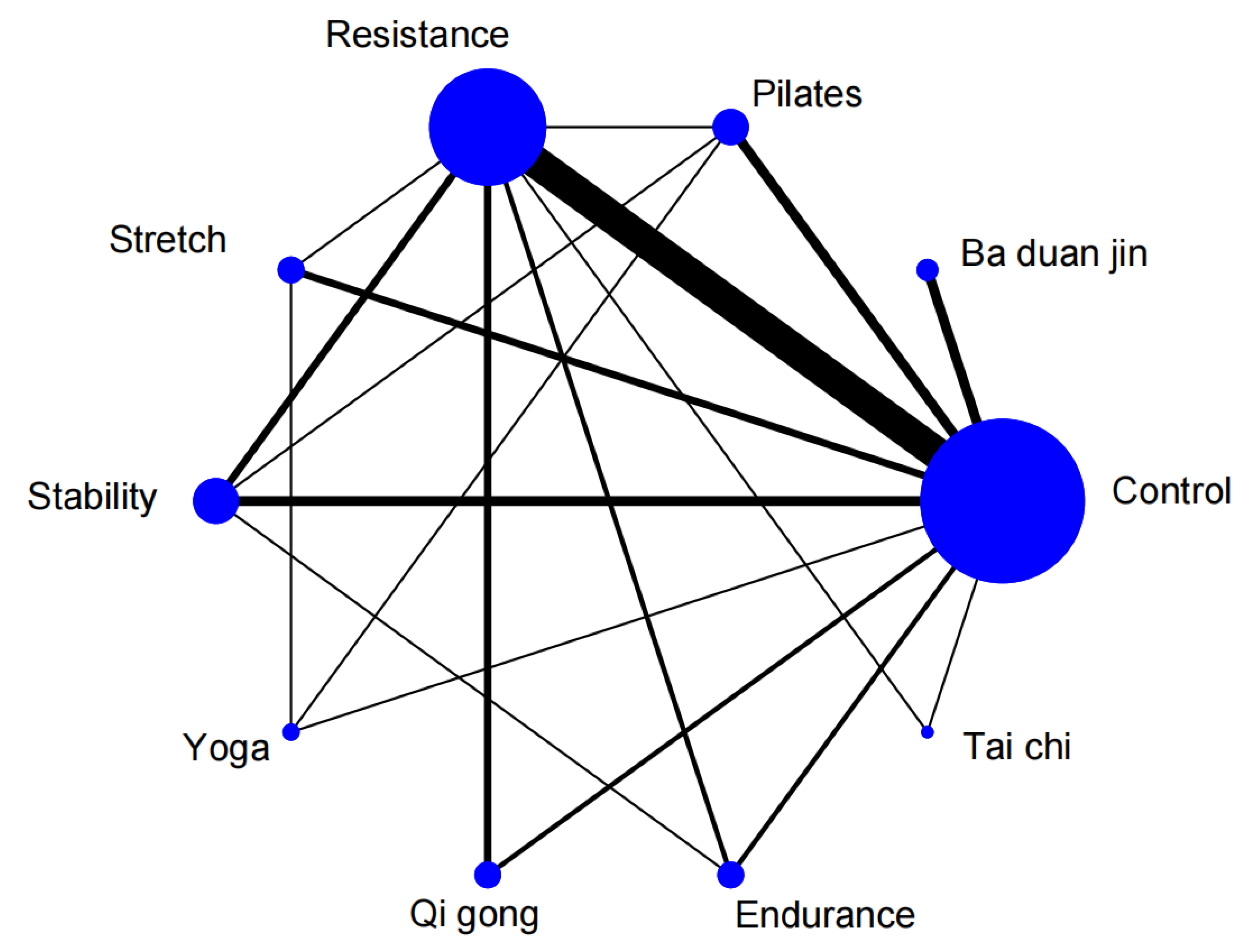
3.4. Network Meta-Analysis
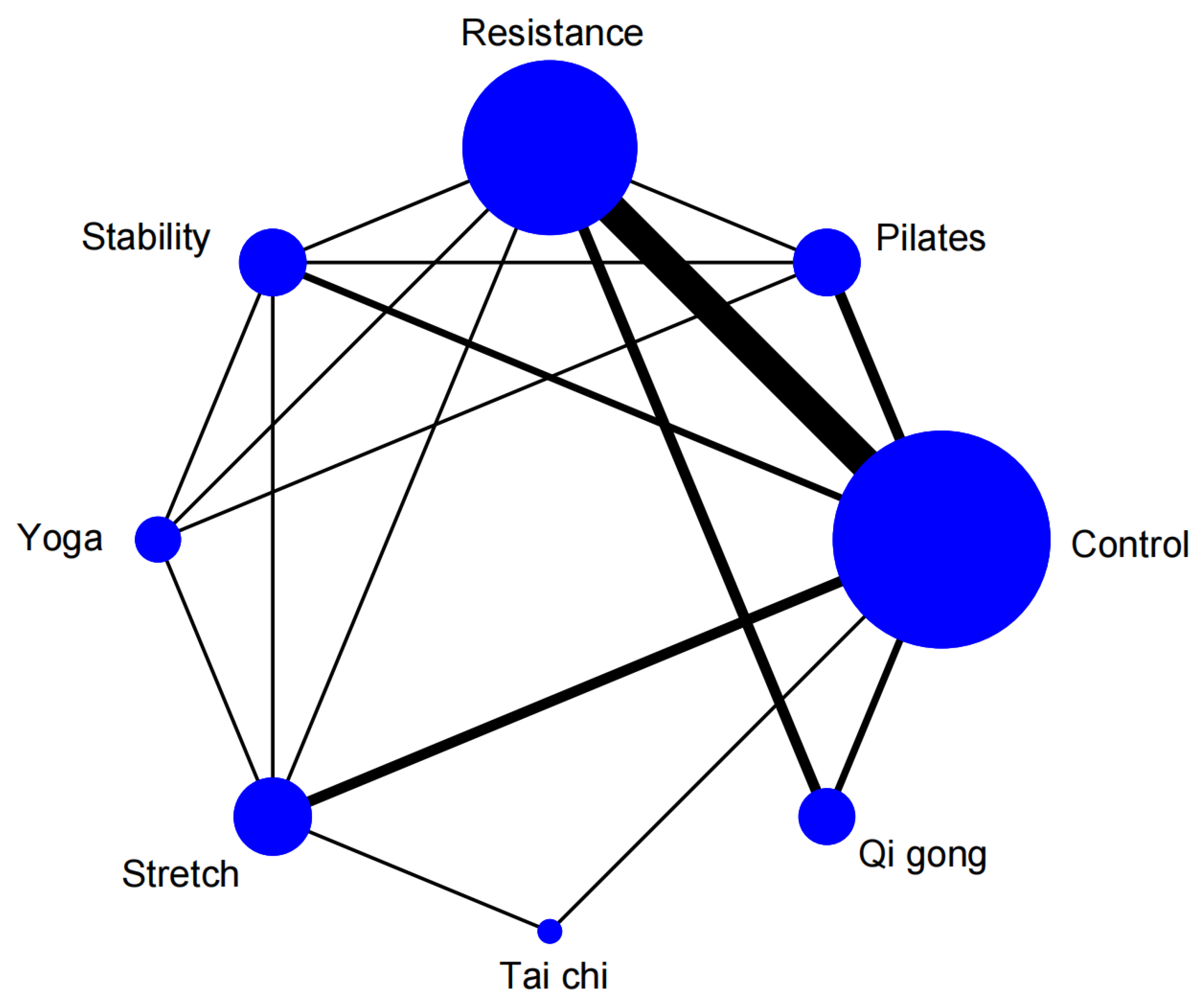
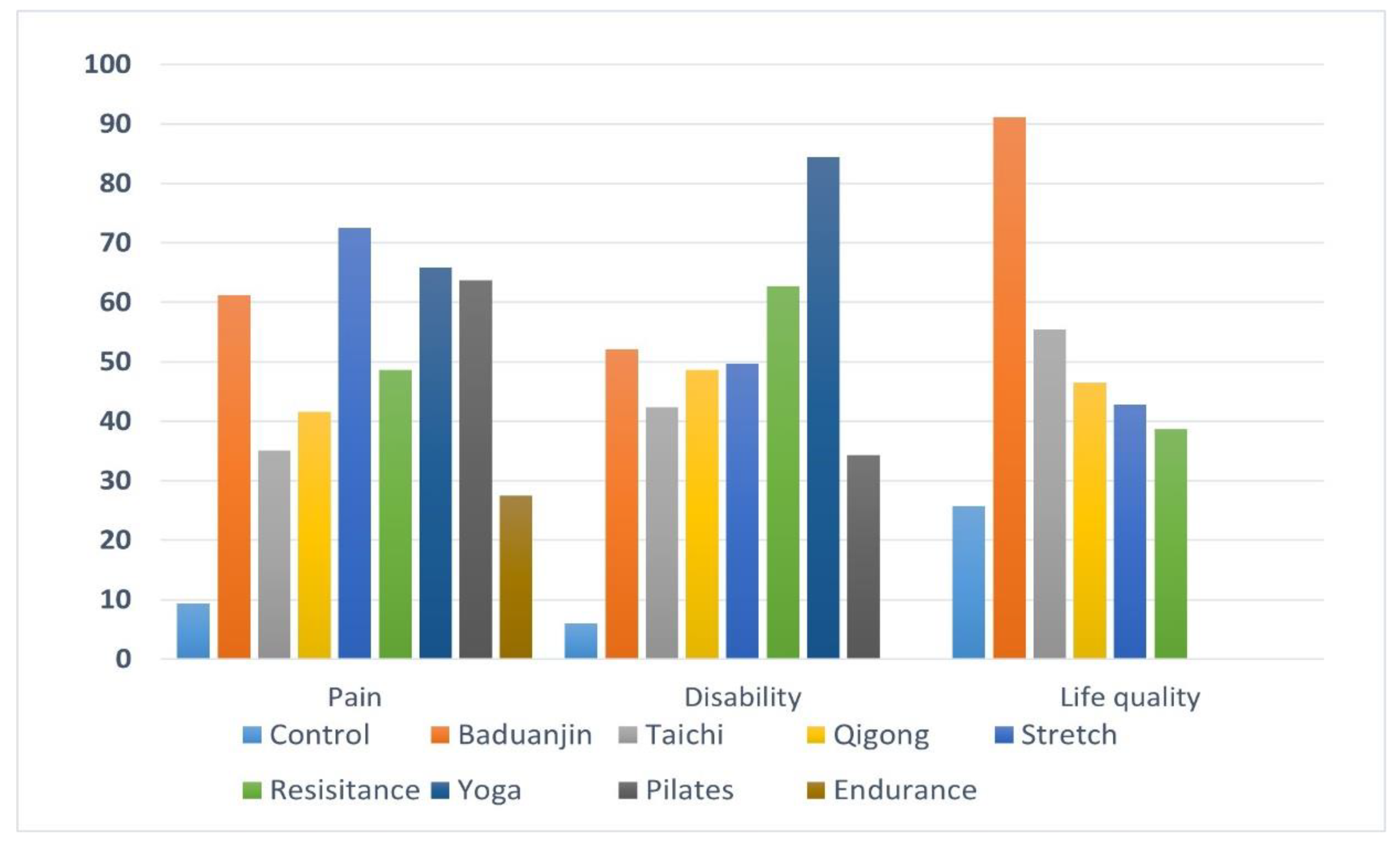
3.4.1. Pain Level
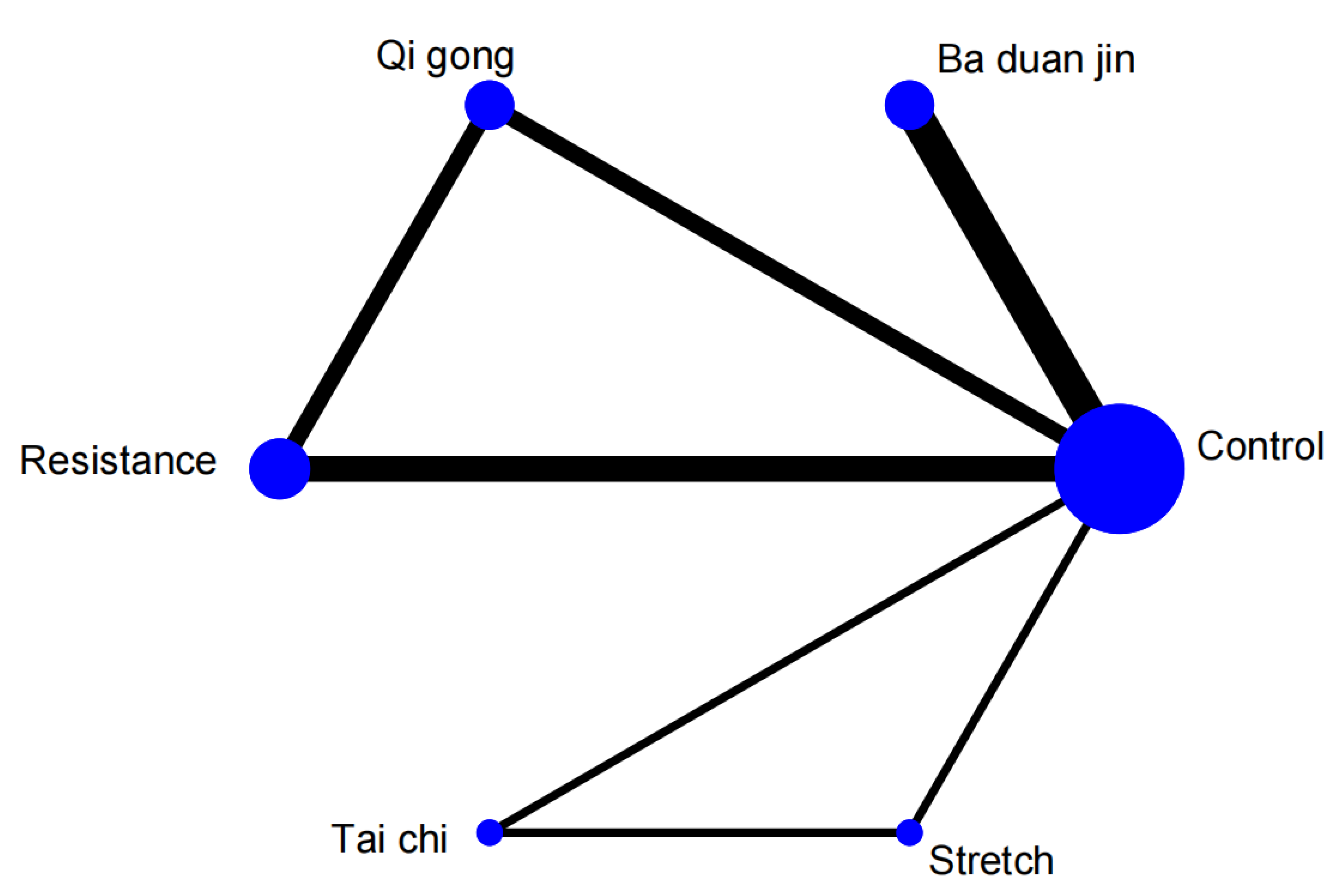
3.4.2. Neck Dysfunction
3.4.3. Life Quality
4. Discussion
4.1. Pain Improvement
4.2. Neck Dysfunction
4.3. Life Quality
5. Conclusion
References
- Nyirö, L.; Peterson, C.K.; Humphreys, B.K. Exploring the definition of "acute" neck pain: a prospective cohort observational study comparing the outcomes of chiropractic patients with 0-2 weeks, 2-4 weeks and 4-12 weeks of symptoms. Chiropractic & Manual Therapies 2017, 25. [Google Scholar] [CrossRef]
- Lohman, E.B.; Pacheco, G.R.; Gharibvandi, L.; Daher, N.; Devore, K.; Bains, G.; AlAmeri, M.; Berk, L.S. The immediate effects of cervical spine manipulation on pain and biochemical markers in females with acute non-specific mechanical neck pain: a randomized clinical trial. Journal of Manual & Manipulative Therapy 2019, 27, 186–196. [Google Scholar] [CrossRef]
- Cerezo-Téllez, E.; Torres-Lacomba, M.; Mayoral-del-Moral, O.; Pacheco-da-Costa, S.; Prieto-Merino, D.; Sánchez-Sánchez, B. Health related quality of life improvement in chronic non-specific neck pain: secondary analysis from a single blinded, randomized clinical trial. Health and quality of life outcomes 2018, 16. [Google Scholar] [CrossRef] [PubMed]
- Tsang, S.M.H.; Szeto, G.P.Y.; Xie, Y.F.; Lee, R.Y.W. Association of electromyographic activation patterns with pain and functional disability in people with chronic neck pain. European Journal of Applied Physiology 2018, 118, 1481–1492. [Google Scholar] [CrossRef]
- Haldeman, S.; Carroll, L.; Cassidy, J.D. Findings From The Bone and Joint Decade 2000 to 2010 Task Force on Neck Pain and Its Associated Disorders. Journal of occupational and environmental medicine 2010, 52, 424–427. [Google Scholar] [CrossRef]
- Hoy, D.G.; Protani, M.; De, R.; Buchbinder, R. The epidemiology of neck pain. Best Practice & Research in Clinical Rheumatology 2010, 24, 783–792. [Google Scholar] [CrossRef]
- Blanpied, P.R.; Gross, A.R.; Elliott, J.M.; Devaney, L.L.; Clewley, D.; Walton, D.M.; Sparks, C.; Robertson, E.K. Neck Pain: Revision 2017. Journal of Orthopaedic & Sports Physical Therapy 2017, 47, A1–A83. [Google Scholar] [CrossRef]
- Kjaer, P.; Kongsted, A.; Hartvigsen, J.; Isenberg-Jørgensen, A.; Schiøttz-Christensen, B.; Søborg, B.; Krog, C.; Møller, C.M.; Halling, C.M.B.; Lauridsen, H.H. National clinical guidelines for non-surgical treatment of patients with recent onset neck pain or cervical radiculopathy. European Spine Journal 2017, 26, 2242–2257. [Google Scholar] [CrossRef]
- Bier, J.D.; Scholten-Peeters, W.G.M.; Staal, J.B.; Pool, J.; van Tulder, M.W.; Beekman, E.; Knoop, J.; Meerhoff, G.; Verhagen, A.P. Clinical Practice Guideline for Physical Therapy Assessment and Treatment in Patients With Nonspecific Neck Pain. Physical therapy 2017, 98, 162–171. [Google Scholar] [CrossRef]
- Bobos, P.; MacDermid, J.C. Appraisal of Clinical Practice Guideline: Management of neck pain. J Physiother 2018, 64, 127. [Google Scholar] [CrossRef]
- Alzahrani, H.; Mackey, M.; Stamatakis, E.; Zadro, J.R.; Shirley, D. The association between physical activity and low back pain: a systematic review and meta-analysis of observational studies (vol 9, pg 8244, 2019). Scientific reports 2020, 10. [Google Scholar] [CrossRef]
- Lin, I.H.; Chang, K.H.; Liou, T.H.; Tsou, C.M.; Huang, Y.C. Progressive shoulder-neck exercise on cervical muscle functions in middle-aged and senior patients with chronic neck pain. European Journal of Physical and Rehabilitation Medicine 2018, 54, 13–21. [Google Scholar] [CrossRef] [PubMed]
- Caputo, G.M.; Di Bari, M.; Naranjo Orellana, J. Group-based exercise at workplace: short-term effects of neck and shoulder resistance training in video display unit workers with work-related chronic neck pain-a pilot randomized trial. Clinical rheumatology 2017, 36, 2325–2333. [Google Scholar] [CrossRef] [PubMed]
- Dunleavy, K.; Kava, K.; Goldberg, A.; Malek, M.H.; Talley, S.A.; Tutag-Lehr, V.; Hildreth, J. Comparative effectiveness of Pilates and yoga group exercise interventions for chronic mechanical neck pain: quasi-randomised parallel controlled study. Physiotherapy 2016, 102, 236–242. [Google Scholar] [CrossRef]
- Ghaderi, F.; Jafarabadi, M.A.; Javanshir, K. The clinical and EMG assessment of the effects of stabilization exercise on nonspecific chronic neck pain: A randomized controlled trial. Journal of Back and Musculoskeletal Rehabilitation 2017, 30, 211–219. [Google Scholar] [CrossRef]
- Hutton, B.; Salanti, G.; Caldwell, D.M.; Chaimani, A.; Schmid, C.H.; Cameron, C.; Ioannidis, J.P.; Straus, S.; Thorlund, K.; Jansen, J.P.; et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Annals of internal medicine 2015, 162, 777–784. [Google Scholar] [CrossRef]
- Bennett, M.M.; Crowe, B.J.; Price, K.L.; Stamey, J.D.; Seaman, J.W., Jr. Comparison of Bayesian and frequentist meta-analytical approaches for analyzing time to event data. J Biopharm Stat 2013, 23, 129–145. [Google Scholar] [CrossRef]
- Wan, X.; Wang, W.; Liu, J.; Tong, T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol 2014, 14, 135. [Google Scholar] [CrossRef]
- Mbuagbaw, L.; Rochwerg, B.; Jaeschke, R.; Heels-Andsell, D.; Alhazzani, W.; Thabane, L.; Guyatt, G.H. Approaches to interpreting and choosing the best treatments in network meta-analyses. Syst Rev 2017, 6, 79. [Google Scholar] [CrossRef]
- Shim, S.; Yoon, B.H.; Shin, I.S.; Bae, J.M. Network meta-analysis: application and practice using Stata. Epidemiol Health 2017, 39, e2017047. [Google Scholar] [CrossRef]
- Shi, Z. Study on Fitness Qigong Baduanjin Improving the Quality of Life of Patients with Chronic Neck Pain. Contemporary Sports Technology 2023, 13, 37–40. [Google Scholar] [CrossRef]
- Zhao, M. Research on the Effects of Pilates-based Exercises for Chronic Nonspecific Neck Pain. Bulletin of Sport Science & Technology 2020, 28, 167–168. [Google Scholar] [CrossRef]
- Cai, Y.; Liu, A.; Yao, Z.; Li, J.; Wang, Y. The impact of Baduanjin on the quality of life of middle-aged and elderly people with chronic neck pain. Chinese Journal of Gerontology 2018, 38, 2934–2936. [Google Scholar]
- Wang, J. The effects of regular Qigong-Ba Duan Jin practice on promoting the health in patients with chronic neck pain. 硕士, Beijing University of Chinese Medicine, 2013.
- Hernandez-Lucas, P.; Leirós-Rodríguez, R.; Lopez-Barreiro, J.; García-Soidán, J.L. Effects of back school-based intervention on non-specific neck pain in adults: a randomized controlled trial. BMC Sports Sci Med Rehabil 2023, 15, 60. [Google Scholar] [CrossRef]
- Sahiner Picak, G.; Yesilyaprak, S.S. Effects of clinical pilates exercises in patients with chronic nonspecific neck pain: a randomized clinical trial. Irish journal of medical science 2022. [Google Scholar] [CrossRef]
- Javdaneh, N.; Saeterbakken, A.H.; Shams, A.; Barati, A.H.T.a.d.n.c.o.i. Pain Neuroscience Education Combined with Therapeutic Exercises Provides Added Benefit in the Treatment of Chronic Neck Pain. International journal of environmental research and public health 2021, 18. [Google Scholar] [CrossRef]
- Bernal-Utrera, C.; Anarte-Lazo, E.; Gonzalez-Gerez, J.J.; Saavedra-Hernandez, M.; De-La-Barrera-Aranda, E.; Serrera-Figallo, M.A.; Gonzalez-Martin, M.; Rodriguez-Blanco, C. Effect of Combined Manual Therapy and Therapeutic Exercise Protocols on the Postural Stability of Patients with Non-Specific Chronic Neck Pain. A Secondary Analysis of Randomized Controlled Trial. J Clin Med 2021, 11. [Google Scholar] [CrossRef]
- avdaneh, N.; Molayei, F.; Kamranifraz, N. Effect of adding motor imagery training to neck stabilization exercises on pain, disability and kinesiophobia in patients with chronic neck pain. Complementary therapies in clinical practice 2021, 42, 101263. [Google Scholar] [CrossRef]
- de Araujo Cazotti, L.; Jones, A.; Roger-Silva, D.; Ribeiro, L.H.C.; Natour, J. Effectiveness of the Pilates Method in the Treatment of Chronic Mechanical Neck Pain: A Randomized Controlled Trial. Arch Phys Med Rehabil 2018, 99, 1740–1746. [Google Scholar] [CrossRef]
- Dunleavy, K.; Kava, K.; Goldberg, A.; Malek, M.H.; Talley, S.A.; Tutag-Lehr, V.; Hildreth, J. Comparative effectiveness of Pilates and yoga group exercise interventions for chronic mechanical neck pain: quasi-randomised parallel controlled study. Physiotherapy 2016, 102, 236–242. [Google Scholar] [CrossRef]
- von Trott, P.; Wiedemann, A.M.; Lüdtke, R.; Reishauer, A.; Willich, S.N.; Witt, C.M. Qigong and exercise therapy for elderly patients with chronic neck pain (QIBANE): a randomized controlled study. J Pain 2009, 10, 501–508. [Google Scholar] [CrossRef]
- Helewa, A.; Goldsmith, C.H.; Smythe, H.A.; Lee, P.; Obright, K.; Stitt, L. Effect of therapeutic exercise and sleeping neck support on patients with chronic neck pain: A randomized clinical trial. Journal of Rheumatology 2007, 34, 151–158. [Google Scholar] [PubMed]
- Khosrokiani, Z.; Letafatkar, A.; Sokhanguei, Y. Long-term effect of direction-movement control training on female patients with chronic neck pain. Journal of bodywork and movement therapies 2018, 22, 217–224. [Google Scholar] [CrossRef]
- Li, X.; Lin, C.; Liu, C.; Ke, S.; Wan, Q.; Luo, H.; Huang, Z.; Xin, W.; Ma, C.; Wu, S. Comparison of the effectiveness of resistance training in women with chronic computer-related neck pain: a randomized controlled study. Int Arch Occup Environ Health 2017, 90, 673–683. [Google Scholar] [CrossRef] [PubMed]
- Rendant, D.; Pach, D.; Lüdtke, R.; Reisshauer, A.; Mietzner, A.; Willich, S.N.; Witt, C.M. Qigong versus exercise versus no therapy for patients with chronic neck pain: a randomized controlled trial. Spine 2011, 36, 419–427. [Google Scholar] [CrossRef] [PubMed]
- Viljanen, M.; Malmivaara, A.; Uitti, J.; Rinne, M.; Palmroos, P.; Laippala, P. Effectiveness of dynamic muscle training, relaxation training, or ordinary activity for chronic neck pain: randomised controlled trial. BMJ (Clinical research ed.) 2003, 327, 475. [Google Scholar] [CrossRef] [PubMed]
- Beer, A.; Treleaven, J.; Jull, G. Can a functional postural exercise improve performance in the cranio-cervical flexion test?--a preliminary study. Man Ther 2012, 17, 219–224. [Google Scholar] [CrossRef]
- Ma, C.; Szeto, G.P.; Yan, T.; Wu, S.; Lin, C.; Li, L. Comparing biofeedback with active exercise and passive treatment for the management of work-related neck and shoulder pain: a randomized controlled trial. Arch Phys Med Rehabil 2011, 92, 849–858. [Google Scholar] [CrossRef]
- Andersen, L.L.; Kjaer, M.; Søgaard, K.; Hansen, L.; Kryger, A.I.; Sjøgaard, G. Effect of two contrasting types of physical exercise on chronic neck muscle pain. Arthritis and rheumatism 2008, 59, 84–91. [Google Scholar] [CrossRef]
- Ahlgren, C.; Waling, K.; Kadi, F.; Djupsjöbacka, M.; Thornell, L.E.; Sundelin, G. Effects on physical performance and pain from three dynamic training programs for women with work-related trapezius myalgia. J Rehabil Med 2001, 33, 162–169. [Google Scholar] [CrossRef]
- Wang, J.-Y.; Guo, H.; Tang, L.; Meng, J.; Hu, L.-y. Case-control study on regular Ba Duan Jin practice for patients with chronic neck pain. International Journal of Nursing Sciences 2014, 1, 360–366. [Google Scholar] [CrossRef]
- Lauche, R.; Stumpe, C.; Fehr, J.; Cramer, H.; Cheng, Y.W.; Wayne, P.M.; Rampp, T.; Langhorst, J.; Dobos, G. The Effects of Tai Chi and Neck Exercises in the Treatment of Chronic Nonspecific Neck Pain: A Randomized Controlled Trial. The journal of pain 2016, 17, 1013–1027. [Google Scholar] [CrossRef] [PubMed]
- Evans, R.; Bronfort, G.; Schulz, C.; Maiers, M.; Bracha, Y.; Svendsen, K.; Grimm, R.; Garvey, T.; Transfeldt, E. Supervised Exercise With and Without Spinal Manipulation Performs Similarly and Better Than Home Exercise for Chronic Neck Pain. Spine 2012, 37, 903–914. [Google Scholar] [CrossRef] [PubMed]
- Izquierdo, T.G.; Pecos-Martin, D.; Girbés, E.L.; Plaza-Manzano, G.; Caldentey, R.R.; Melús, R.M.; Mariscal, D.B.; Falla, D. Comparison of Cranio-Cervical Flexion Training Versus Cervical Proprioception Training in Patients with Chronic Neck Pain: A Randomized Controlled Clinical Trial. Journal of Rehabilitation Medicine 2016, 48, 48–55. [Google Scholar] [CrossRef]
- Lansinger, B.; Larsson, E.; Liselott, C.P.; Carlsson, J.Y. Qigong and exercise therapy in patients with long-term neck pain. Spine 2007, 32, 2415–2422. [Google Scholar] [CrossRef]
- Luo, Y.; Fan, Y.; Ma, T.; Wang, L.; Wu, H. The intervention of neck resistance training in different postures for chronic nonspecific neck pain. Chinese Journal of Rehabilitation Medicine 2024, 39, 693–698. [Google Scholar]
- Akodu, A.K.; Nwanne, C.A.; Fapojuwo, O.A. Efficacy of neck stabilization and Pilates exercises on pain, sleep disturbance and kinesiophobia in patients with non-specific chronic neck pain: A randomized controlled trial. Journal of bodywork and movement therapies 2021, 26, 411–419. [Google Scholar] [CrossRef]
- Kaka, B.; Ogwumike, O.O.; Adeniyi, A.F.; Maharaj, S.S.; Ogunlade, S.O.; Bello, B. Effectiveness of neck stabilisation and dynamic exercises on pain intensity, depression and anxiety among patients with non-specific neck pain: a randomised controlled trial. Scandinavian journal of pain 2018, 18, 321–331. [Google Scholar] [CrossRef]
- Cramer, H.; Lauche, R.; Hohmann, C.; Lüdtke, R.; Haller, H.; Michalsen, A.; Langhorst, J.; Dobos, G. Randomized-controlled Trial Comparing Yoga and Home-based Exercise for Chronic Neck Pain. Clinical Journal of Pain 2013, 29, 216–223. [Google Scholar] [CrossRef]
- Falla, D.; Jull, G.; Hodges, P.W. Feedforward activity of the cervical flexor muscles during voluntary arm movements is delayed in chronic neck pain. Exp Brain Res 2004, 157, 43–48. [Google Scholar] [CrossRef]
- Ylinen, J.; Salo, P.; Nykänen, M.; Kautiainen, H.; Häkkinen, A. Decreased isometric neck strength in women with chronic neck pain and the repeatability of neck strength measurements. Arch Phys Med Rehabil 2004, 85, 1303–1308. [Google Scholar] [CrossRef] [PubMed]
- Clark, D.R.; Lambert, M.I.; Hunter, A.M. Contemporary perspectives of core stability training for dynamic athletic performance: a survey of athletes, coaches, sports science and sports medicine practitioners. Sports medicine-open 2018, 4, 32. [Google Scholar] [CrossRef] [PubMed]
- Wu, B.; Yuan, H.; Geng, D.; Zhang, L.; Zhang, C. The impact of a stabilization exercise on neck pain: a systematic review and meta-analysis. Journal of Neurological Surgery Part A: Central European Neurosurgery 2020, 81, 342–347. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Wang, y.; Zhang, Z.; Zhu, Y.; Chen, P. Exercise therapy for neck pain:Consensus from Chinese Experts. Journal of Shanghai University of Sport 2020, 44, 59–69. [Google Scholar] [CrossRef]
- Denham-Jones, L.; Gaskell, L.; Spence, N.; Pigott, T. A systematic review of the effectiveness of Pilates on pain, disability, physical function, and quality of life in older adults with chronic musculoskeletal conditions. Musculoskeletal care 2022, 20, 10–30. [Google Scholar] [CrossRef]
- Cramer, H.; Klose, P.; Brinkhaus, B.; Michalsen, A.; Dobos, G. Effects of yoga on chronic neck pain: a systematic review and meta-analysis. Clin Rehabil 2017, 31, 1457–1465. [Google Scholar] [CrossRef]
- Tul, Y.; Unruh, A.; Dick, B.D. Yoga for chronic pain management: a qualitative exploration. Scandinavian journal of caring sciences 2011, 25, 435–443. [Google Scholar] [CrossRef]
- Bai, Z.; Guan, Z.; Fan, Y.; Liu, C.; Yang, K.; Ma, B.; Wu, B. The effects of qigong for adults with chronic pain: systematic review and meta-analysis. The American journal of Chinese medicine 2015, 43, 1525–1539. [Google Scholar] [CrossRef]
- Li, J.; Yu, F.; Huang, N.; Lu, J.; Xu, W.; Liu, N. Effect of Baduanjin exercise on patients with chronic heart failure: protocol for a systematic review and meta-analysis. BMJ open 2019, 9, e028771. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).




