1. .Introduction
Limb-lengthening is a surgical procedure used to correct limb length discrepancies, and deformities, or to increase the length of a limb for functional or cosmetic reasons. Short stature is more than a physical condition; it may negatively impact the quality of life for patients [
1]. These individuals often require constant assistance in performing daily activities, such as sitting down or getting up from a chair. The aim of limb lengthening is to enhance these patients’ quality of life.
The evolution of limb-lengthening techniques has significantly advanced with the development of more precise and effective systems. The Ilizarov method was one of the pioneering techniques, utilizing circular external fixation. This method incorporated a complex system of rings, wires, and screws to stabilize the bone during gradual distraction following a deliberate bone break [
2]. However, the advent of hexapod external fixation systems, such as the Taylor Spatial Frame (TSF) - a circular external fixator that employs a computer software program - has revolutionized limb lengthening procedures [
3].
The TSF, introduced by Dr. Charles Taylor in 1994, transformed the understanding and ability to perform indirect reduction and correction of deformities and fractures. It is an external fixator offering three-dimensional control of bone movement. The apparatus employs a combination of rings and bars that, when connected through wires and pins, permit gradual lengthening and correction of deformities. However, employing the TSF necessitates an experienced team of orthopedists capable of accurately handling any corrections [
4].
The aim of this review is to assess, based on the literature, the efficacy of the hexapod ex-ternal fixator compared to other fixators in lengthening patients with short stature and correcting anatomical deformities.
2. Materials and Methods
2.1. Search Strategy
We conducted a structured search of four databases from 2004 to 2024: PubMed, Scopus, Web of Science, and Medline. Initially, we used the following words in our literature search: “Lengthening” AND “Short stature” AND “Deformity”, “Hexapod external fixation” OR “Taylor Spatial Frame”. We employed Boolean operators to combine topic words with key-words and search for references in related literature. Our search adhered to the Preferred Re-porting Items for Systematic Review and Meta-analysis (PRISMA) guidelines for a systematic review of rates.
2.2. Inclusion End Exclusion Criteria
The inclusion criteria were as follows: any level of evidence studies; studies written in English; studies with five or more patients; full-text articles; and studies with a Methodological Index for Non-Randomized Studies (MINORS) quality evaluation score of more than 14 points.
The exclusion criteria were as follows: review articles, case reports, and articles with fewer than five patients; articles written in languages other than English; non-human studies; absence of full-text articles; studies with a MINORS quality evaluation score of 13 points or less.
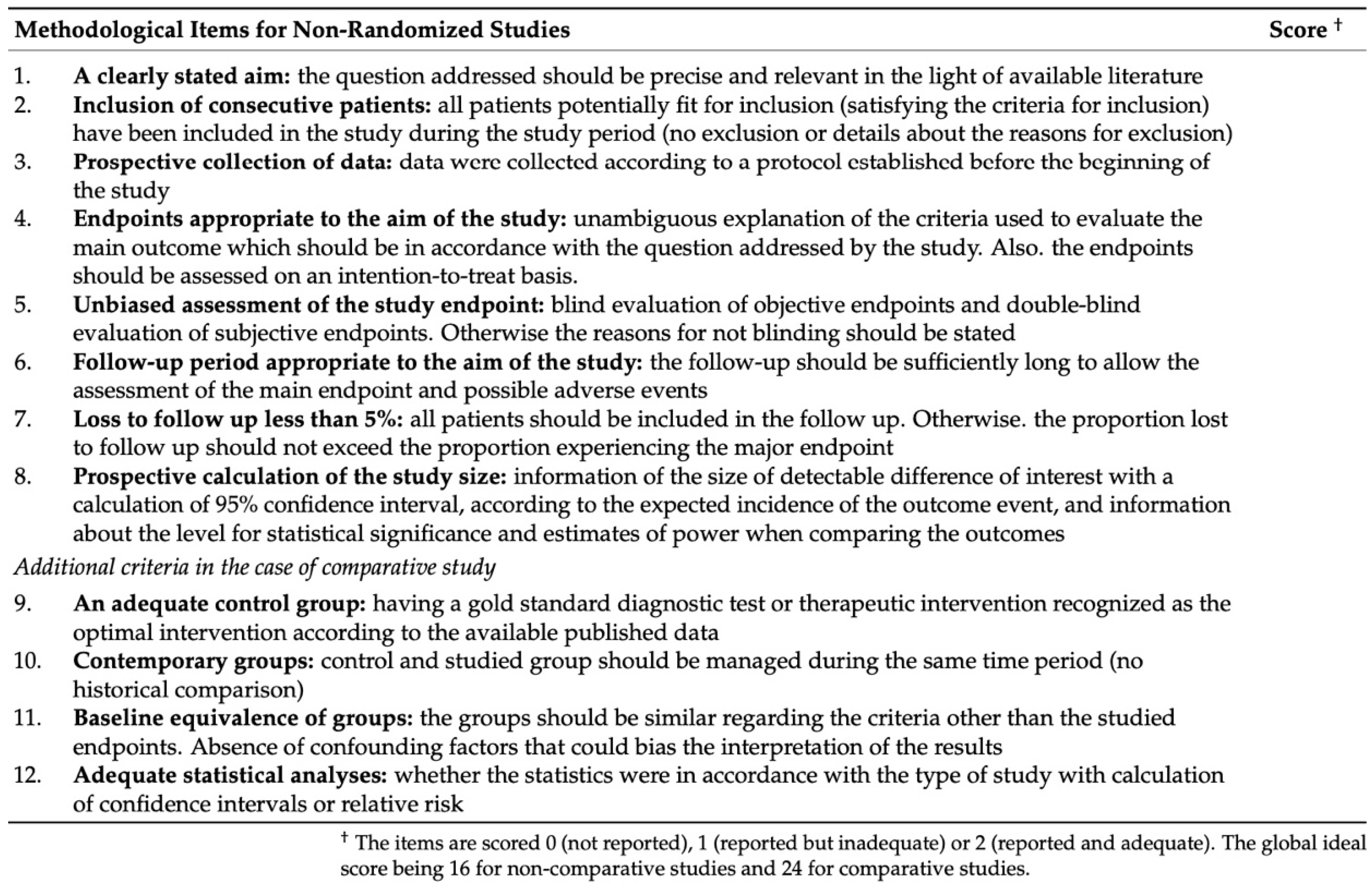
2.3. Quality Evaluation Using the MINORS Checklist
The MINORS Checklist is used to evaluate the adequacy of items based on eight indicators for non-comparative studies. These include: a clearly stated aim; the inclusion of consecutive patients; prospective data collection; endpoints appropriate to the aim of the study; unbiased assessment of the study endpoint; follow-up period suitable for the study’s aim; loss to follow-up less than 5%; and prospective calculation of the study size. Items are scored as follows: 0 (not reported), 1 (reported but inadequate), or 2 (reported and adequate) [
5] (
Figure 1).
2.4. Data Extraction
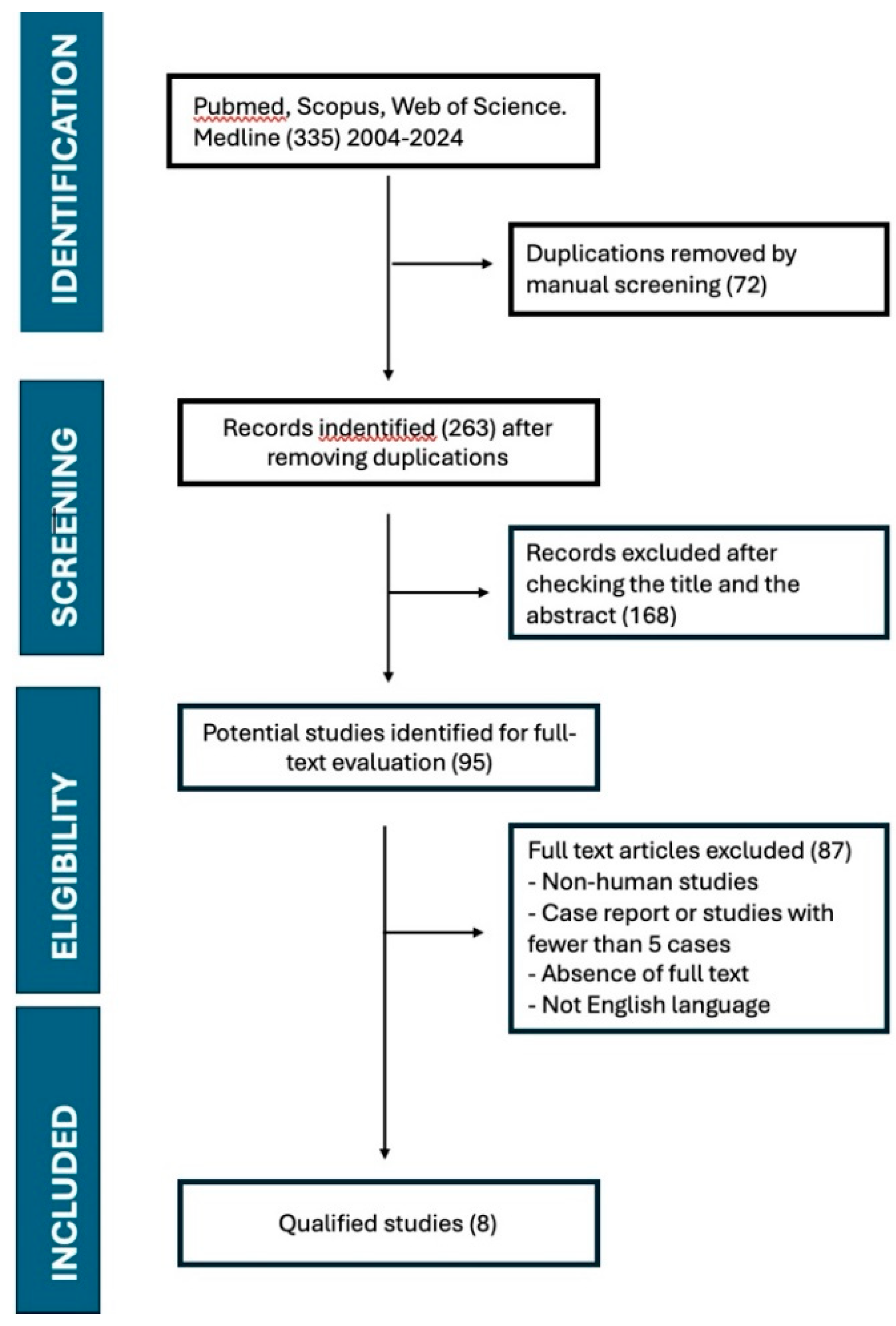
Data were extracted using the PRISMA flowchart. The PRISMA flowchart illustrating the se-lection and screening method is provided in
Figure 2.
The data extracted for analysis included: the first author and year of publication, the study type, patient count and sex ratio, average age at operation, patients’ clinical characteristics, the type of implant and bone involved, average length increase in cm, healing index (days/cm), follow-up, complications, and limitations of the study.
2.5. Statistical Analysis
The statistical data was analyzed using Microsoft Excel 2021®. The use of descriptive statistics was sufficient, and there was no need to calculate significance levels.
3. Results
3.1. Search Results
Our search strategy yielded 335 articles from 2004 to 2024, incorporating the previously re-ported keywords. After eliminating duplicates through manual screening, we were left with 263 articles. Upon reviewing the titles and abstracts, we discarded an additional 168 articles, leaving us with 95 articles. From these, we excluded non-human studies, case reports, studies involving fewer than five cases, articles where the complete text was unavailable, and articles not written in English. Ultimately, we identified eight articles that met our inclusion and exclusion criteria.
3.2. Basic Characteristics of Included Studies
The basic Characteristics of the included studies are resumed in the
Table 1 [
2,
4,
6,
7,
8,
9,
10,
11].
Eight studies were identified, including three retrospective randomized controlled trials and five cohort studies. These studies divided patients based on etiology, with some comparing the use of hexapod external fixators with other types of external fixators.
Three studies evaluated the application of hexapod external fixation in a specified patient group, specifically focusing on the average length achieved, the average healing rate, and complications.
Five studies compared the results acquired from different groups, separated based on etiology, or the type of external fixator used.
3.3. Patient Demographics
The studies encompassed a total of 479 patients, with an average age of 14.6 years. The reasons for limb lengthening encompass congenital deformities, post-traumatic deformities, and acquired deformities.
3.4. Lengthening Achieved
The lengthening achieved ranged from 3 to 5.9 cm. The healing index is the ratio between the total treatment time (TTT, defined as the number of days from EF implant to removal) and the total lengthening outcome achieved, expressed in days/cm2. It ranged from 37 to 68.6 days/cm2.
3.5. Duration of Follow-Up
The duration of follow-up refers to the time that patients were monitored after the removal of the EF. It is dependent on the patient’s age at the time of the operation, with younger patients requiring a more extended follow-up than older ones. The average follow-up period ranged from 6.8 months to 6 years post EF removal.
3.6. Complications
Most of these studies utilize Paley’s classification to distinguish between problems, obstacles, and true complications. Problems are defined as postoperative difficulties that are completely resolved with nonoperative intervention. Obstacles, on the other hand, are difficulties that necessitate operative intervention but resolve after surgery. True complications are problems that occur intraoperatively and remain unresolved following treatment completion [
7]. The most frequent complications include pin site infections, compartment syndrome, and delayed union. Less common complications encompass deep infections and neurovascular injury.
4. Discussion
This systematic review evaluated the use of hexapod external fixation (HEF) for limb-lengthening in patients with short stature and deformities. The primary focus was on out-comes related to lengthening achieved, healing index, complications, and follow-up duration. After a thorough screening of 335 articles, only eight studies met the inclusion criteria, collectively involving a total of 479 patients. The studies provided invaluable insights into the effectiveness and safety of HEF for treating short stature and deformities of various etiologies.
The lengths achieved in the studies spanned from 3 to 5.9 cm, aligning with prior records that advocate moderate lengthening outcomes with external fixators for deformity correction in pediatric and adolescent age. The healing index, fluctuating between 37 and 68.6 days/cm, portrays the efficiency of the bone healing procedure during lengthening. Even though the healing index seen in this review is relatively high in contrast to certain other reports on convention-al external fixation methods (20–30 days/cm), it fits the span noted for hexapod external fixators, renowned for their precision and multi-plane deformity rectification aptitude. A heightened healing index may serve as a sign of the cases’ complexity, as clients often come with congenital or post-injury deformities that demand not only lengthening but conspicuous correction of an-gular deformities [
10].
The mean follow-up duration showed significant variability, ranging from 6.8 months to 6 years, reflecting the variability in patient age and the nature of their deformities. Generally, younger patients require a longer follow-up to confirm complete bone healing and monitor for potential long-term complications [
2]. Although most of the studies included in this review reported a follow-up duration exceeding one year, several studies featured a shorter follow-up time. This fact limits the assessment of late complications such as joint stiffness or growth disturbances. This fluctuation in follow-up duration might contribute to some inconsistencies in reported complication rates across the various studies.
The complications associated with HEF, as reported in the reviewed studies, were consistent with those observed in earlier studies concerning limb-lengthening with external fixators [
7]. Pin site infections, compartment syndrome, and delayed union were the most common issues, which were categorized according to Paley’s classification [
2]. These complications are well-known in external fixation techniques, largely relating to the mechanical stresses and soft tissue involvement during the distraction process. Though less common complications such as deep infections and neurovascular injuries were also reported, their incidence remains relatively low.
Pin site infections, though common, were typically managed conservatively, and complications such as compartment syndrome and delayed union were addressed with surgical intervention. The hexapod fixator’s capacity to deliver multidimensional correction may contribute to a slightly higher occurrence of these complications. However, it also permits more precise correction of deformities, potentially reducing the requirement for more invasive surgeries in the future. The comparatively low occurrence of severe complications such as neurovascular injury, a concern with other forms of external fixation, demonstrates the safety of the hexapod system com-pared to other techniques [
12].
The magnetic intramedullary nail (MIN) represents a more recent innovation in the limb-lengthening field. This device operates via an external magnetic field that stimulates the mechanical expansion of an internal nail, typically inserted into the intramedullary canal of a bone. This system facilitates non-invasive lengthening and deformity correction, with the external device merely controlling the magnetic field that propels the internal expansion [
13].
A key advantage of the MIN is its minimal invasiveness compared to the hexapod external fixator [
14,
15]. The procedure involves a singular surgical incision for nail insertion, eliminating external components protruding from the limb. This reduction in external features diminishes the risk of infection, enhances patient comfort, and delivers a more aesthetic outcome [
16]. Additionally, as the nail is internal, external adjustments and cumbersome devices are unnecessary, significantly improving the patient’s quality of life during treatment.
Additionally, the automatic lengthening process, managed by a remote magnetic system, provides greater precision and predictability. The rate and rhythm of lengthening can be adjusted with minimal patient intervention, thereby reducing the frequency of clinical visits and manual adjustments, a common requirement with external fixators.
Nonetheless, despite the distinct advantages posed by the magnetic nail in terms of comfort and convenience, it comes with its own limitations. The most significant challenge is its technical complexity, which requires precise surgical planning. The intramedullary nail may not be suitable for all deformities, particularly those necessitating significant correction in multiple planes. In such situations, external fixators prove to be more versatile. Additionally, the cost of the MIN is relatively high and its availability may be limited within various healthcare systems, posing a hindrance to its accessibility.
Lengthening over an intramedullary device in conjunction with an external fixator has been examined in the context of lower limbs. Paley et al. demonstrated that the outcomes of lengthening over an intramedullary nail, when combined with an external fixator, were superior in a population of young adults compared to using an external fixator alone [
12].
Several studies have compared the use of the hexapod external fixator with other types of external fixators, such as Ilizarov frames. The results indicated that the hexapod system provided more precise correction in three-dimensional space and was associated with slightly im-proved functional outcomes. However, the increased complexity of using the hexapod frame may contribute to extended treatment time and higher healing index observed in some studies. Therefore, the decision to use the hexapod external fixator should depend on the patient’s specific needs, including the severity and complexity of the deformity, as well as the patient’s age and potential for future growth.
Despite the value provided by this systematic review, several constraints need acknowledgment. The relatively small quantity of studies included (n=8) alongside the variation in study design, patient demographics, and follow-up durations hinder firm conclusions regarding the long-term effectiveness and safety of the hexapod external fixator for limb lengthening across all patient groups. Also, the restriction to English-language studies might introduce a language bias, thus restricting the generalizability of the conclusions. Moreover, the studies considered in this analysis varied in quality scores per the MINORS checklist, which might impact the reliability of particular findings. Future research with more substantial sample sizes extended follow-up durations, and standardized methodologies is necessary for a more precise understanding of the long-term effects correlated with HEF.
5. Conclusions
In conclusion, the hexapod external fixator seems to be an effective and relatively safe method for limb-lengthening in patients with short stature and deformities. Good outcomes were observed in terms of achieved lengthening and typical complications for external fixation techniques. While the healing index is slightly elevated in comparison to traditional external fixators, the precision, and capability to correct multi-planar deformities make the hexapod a beneficial option for specific patient groups. Further high-quality studies involving larger sample sizes and longer follow-up periods are required to confirm these outcomes and refine treatment protocols using this technique.
Author Contributions
Conceptualization, G.T.; methodology, M.M.; software, M.I.; validation, G.T.; formal analysis, S.M.; investigation, G.C.; resources, M.M.; data curation, M.I.; writing—original draft preparation, M.M.; writing—review and editing, G.T.; visualization, M.S.; supervision, V.P.; project administration, G.T.; funding acquisition, V.P. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data is available in the manuscript.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Guerreschi, F.; Tsibidakis, H. Cosmetic Lengthening: What Are the Limits? Journal of Children’s Orthopaedics 2016, 10, 597–604. [Google Scholar] [CrossRef] [PubMed]
- Dammerer, D.; Kirschbichler, K.; Donnan, L.; Kaufmann, G.; Krismer, M.; Biedermann, R. Clinical Value of the Taylor Spatial Frame: A Comparison with the Ilizarov and Orthofix Fixators. Journal of Children’s Orthopaedics 2011, 5, 343–349. [Google Scholar] [CrossRef] [PubMed]
- Iobst, C. Advances in Pediatric Limb Lengthening: Part 1. JBJS Rev 2015, 3. [Google Scholar] [CrossRef]
- Chalopin, A.; Geffroy, L.; Pesenti, S.; Hamel, A.; Launay, F. Correction of Axial Deformity during Lengthening in Fibular Hypoplasia: Hexapodal versus Monorail External Fixation. Orthopaedics & Traumatology: Surgery & Research 2017, 103, 755–759. [Google Scholar] [CrossRef]
- Slim, K.; Nini, E.; Forestier, D.; Kwiatkowski, F.; Panis, Y.; Chipponi, J. METHODOLOGICAL INDEX FOR NON-RANDOMIZED STUDIES (MINORS): DEVELOPMENT AND VALIDATION OF A NEW INSTRUMENT. ANZ Journal of Surgery 2003, 73, 712–716. [Google Scholar] [CrossRef] [PubMed]
- Roy, A.; Pesenti, S.; Chalopin, A.; Peltier, E.; Jouve, J.-L.; Launay, F. Can the TrueLok Hexapod SystemTM Be Used to Accurately Correct Lower Limb Deformity in Children? Orthopaedics & Traumatology: Surgery & Research 2020, 106, 1361–1366. [Google Scholar] [CrossRef]
- Riganti, S.; Nasto, L.A.; Mannino, S.; Marrè Brunenghi, G.; Boero, S. Correction of Complex Lower Limb Angular Deformities with or without Length Discrepancy in Children Using the TL-HEX Hexapod System: Comparison of Clinical and Radiographical Results. Journal of Pediatric Orthopaedics B 2019, 28, 214–220. [Google Scholar] [CrossRef] [PubMed]
- Blondel, B.; Launay, F.; Glard, Y.; Jacopin, S.; Jouve, J.-L.; Bollini, G. Limb Lengthening and Deformity Correction in Children Using Hexapodal External Fixation: Preliminary Results for 36 Cases. Orthopaedics & Traumatology: Surgery & Research 2009, 95, 425–430. [Google Scholar] [CrossRef]
- Horn, J.; Steen, H.; Huhnstock, S.; Hvid, I.; Gunderson, R.B. Limb Lengthening and Deformity Correction of Congenital and Acquired Deformities in Children Using the Taylor Spatial Frame. Acta Orthopaedica 2017, 88, 334–340. [Google Scholar] [CrossRef] [PubMed]
- Fadel, M.; Hosny, G. The Taylor Spatial Frame for Deformity Correction in the Lower Limbs. International Orthopaedics (SICOT) 2005, 29, 125–129. [Google Scholar] [CrossRef] [PubMed]
- Docquier, P.-L.; Rodriguez, D.; Mousny, M. Three-Dimensional Correction of Complex Leg Deformities Using a Software Assisted External Fixator. 2008, 74.
- Sun, X.-T.; Easwar, T.R.; Manesh, S.; Ryu, J.-H.; Song, S.-H.; Kim, S.-J.; Song, H.-R. Complications and Outcome of Tibial Lengthening Using the Ilizarov Method with or without a Supplementary Intramedullary Nail: A CASE-MATCHED COMPARATIVE STUDY. The Journal of Bone and Joint Surgery. British volume, 2011; 93-B, 782–787. [Google Scholar] [CrossRef]
- Fragomen, A.T.; Rozbruch, S.R. Lengthening of the Femur with a Remote-Controlled Magnetic Intramedullary Nail: Retrograde Technique. JBJS Essential Surgical Techniques 2016, 6, e20. [Google Scholar] [CrossRef] [PubMed]
- Emara, K.M.; Mahran, M.A.; Ghaly, N.A.M.; EL-Husseini, T.F.; Al Kersh, M.A. Comparison between Lengthening over Nail and Conventional Ilizarov Lengthening: A Prospective Randomized Clinical Study. Strategies in Trauma and Limb Reconstruction 2013, 8, 97–101. [Google Scholar] [CrossRef] [PubMed]
- Jager, T.; Popkov, D.; Lascombes, P.; Popkov, A.; Journeau, P. Elastic Intramedullary Nailing as a Complement to Ilizarov’s Method for Forearm Lengthening: A Comparative Pediatric Prospective Study. Orthopaedics & Traumatology: Surgery & Research 2012, 98, 376–382. [Google Scholar] [CrossRef]
- Pietrzak, S.; Grzelecki, D.; Parol, T.; Czubak, J. Comparison of Intramedullary Magnetic Nail, Monolateral External Distractor, and Spatial External Fixator in Femur Lengthening in Adolescents with Congenital Diseases. JCM 2021, 10, 5957. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).