Submitted:
25 December 2024
Posted:
26 December 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
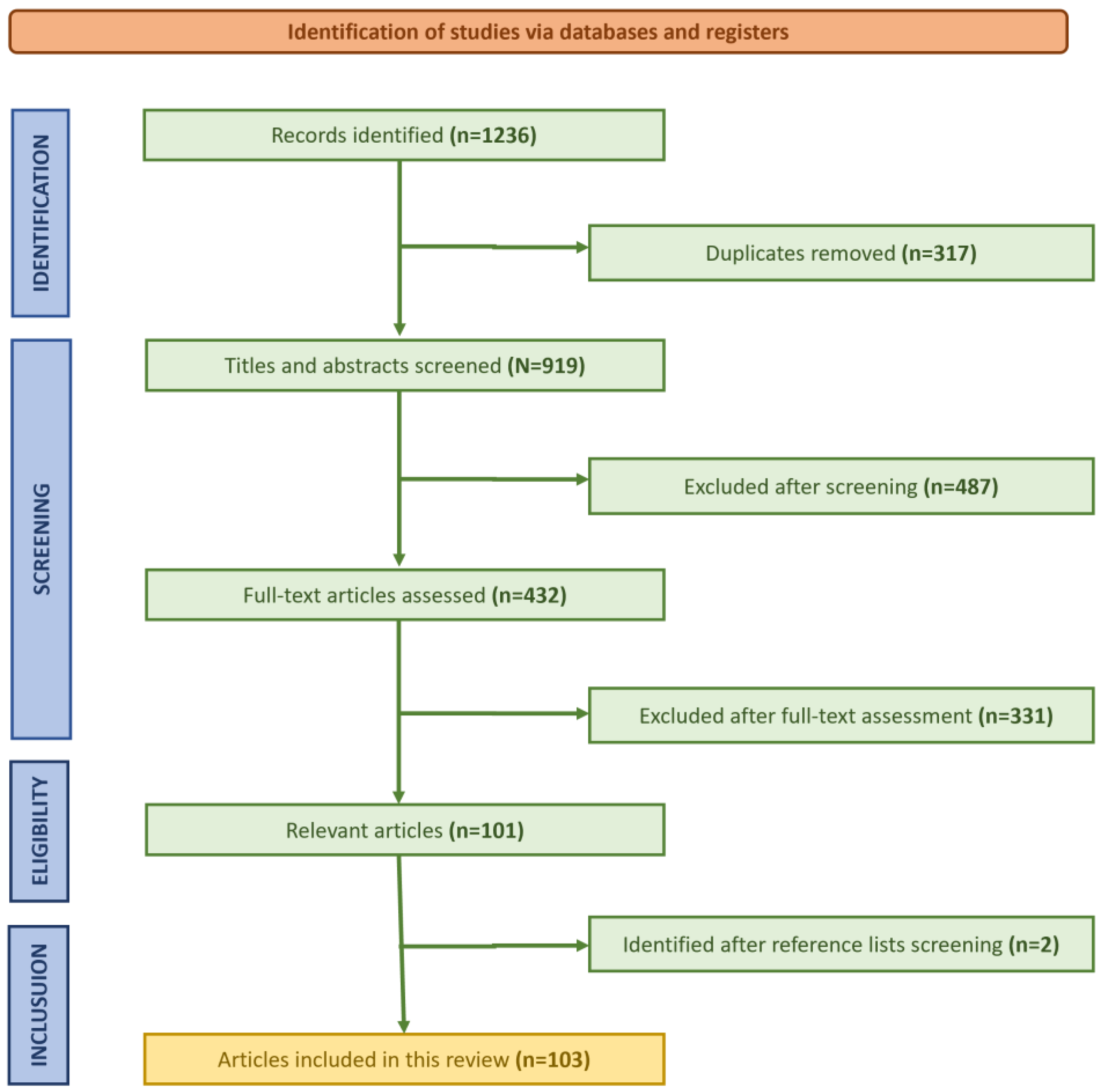
2. Materials and Methods
- Studies examining AI applications in cardiac surgery or related fields.
- Peer-reviewed publications.
- Research focusing on AI technologies such as machine learning, deep learning, computer vision, and robotics.
- Articles discussing preoperative planning, intraoperative assistance, or postoperative management in cardiac surgery.
- Studies addressing ethical, practical, or regulatory considerations in AI use for cardiac surgery.
- Non-peer-reviewed articles, conference abstracts, and editorials.
- Studies focusing solely on non-cardiac surgical specialties.
- Articles without quantitative or qualitative data supporting AI application.
- Duplicate studies across databases.
- Data Extraction and Analysis
- Risk stratification and outcome prediction using machine learning.
- AI-guided imaging and diagnostic technologies.
- Robotic-assisted and computer vision-based surgical systems.
- Ethical and regulatory challenges in AI adoption.
- Future trends and research opportunities in AI for cardiac surgery
2.1. Benefits and Novel Contributions of Artificial Intelligence in Cardiac Surgery
2.1.1. Risk Stratification
2.1.2. Enhanced Surgical Planning
2.1.3. Improved Surgical Accuracy
2.1.4. Real-Time Monitoring and Decision Support
2.1.5. Augmented Cognition and Computer Vision in the Operating Room
2.2. Implementation of Artificial Intelligence in Cardiac Surgery
2.2.1. Preoperative Diagnostic Assistance
2.2.2. Data Collection and Analysis
2.2.3. Machine Learning Algorithms
2.2.4. Robotic-Assisted Surgery
2.2.5. Postoperative Management
2.3. Risks and Challenges of Artificial Intelligence in Cardiac Surgery
2.3.1. Ethical Considerations
2.3.2. Data Privacy and Security
2.3.3. Reliability and Trustworthiness of AI Systems
2.4. Future Directions and Research Opportunities
2.4.1. Advances in AI-Driven Robotics
2.4.2. Predictive and Personalized Care
2.4.3. AI in Healthcare System Optimization
2.4.4. Emerging Technologies and Interdisciplinary Research
2.4.5. Ethical and Regulatory Considerations
3. Limitations
4. Conclusions
References
- Hashimoto DA, Rosman G, Rus D, Meireles OR. Artificial Intelligence in Surgery: Promises and Perils. Ann Surg. 2018 Jul;268(1):70-76. [CrossRef]
- Kilic A. Artificial Intelligence and Machine Learning in Cardiovascular Health Care. Ann Thorac Surg. 2020 May;109(5):1323-1329. [CrossRef]
- Shrestha YR, Krishna V, von Krogh G. Augmenting organizational decision-making with deep learning algorithms: Principles, promises, and challenges. Journal of Business Research. Journal of Business Research 2021;123(2):588-603. [CrossRef]
- Gupta S, Modgil S, Bhattacharyya S, Bose I. Artificial intelligence for decision support systems in the field of operations research: review and future scope of research. Annals of Operations Research. 2022 Jan;308(1):215-74. [CrossRef]
- Jussupow E, Spohrer K, Heinzl A, Gawlitza J. Augmenting medical diagnosis decisions? An investigation into physicians’ decision-making process with artificial intelligence. Information Systems Research. 2021 Sep;32(3):713-35. [CrossRef]
- Kuziemski M, Misuraca G. AI governance in the public sector: Three tales from the frontiers of automated decision-making in democratic settings. Telecomm Policy. 2020 Jul;44(6):101976. [CrossRef]
- Lai V, Chen C, Liao QV, Smith-Renner A, Tan C. Towards a science of human-ai decision making: a survey of empirical studies. arXiv preprint arXiv:2112.11471. 2021 Dec 21.
- Balasubramanian N, Ye Y, Xu M. Substituting human decision-making with machine learning: Implications for organizational learning. Academy of Management Review. 2022 Jul;47(3):448-65. [CrossRef]
- Allyn J, Allou N, Augustin P, Philip I, Martinet O, Belghiti M, Provenchere S, Montravers P, Ferdynus C. A Comparison of a Machine Learning Model with EuroSCORE II in Predicting Mortality after Elective Cardiac Surgery: A Decision Curve Analysis. PLoS One. 2017 Jan 6;12(1):e0169772. [CrossRef]
- Nashef SAM, Ali J. Artificial intelligence and cardiac surgery risk assessment. Eur J Cardiothorac Surg. 2023 Jun 1;63(6):ezad226. [CrossRef]
- Poullis M. The transformation of risk modelling in cardiac and thoracic surgery through artificial intelligence. Eur J Cardiothorac Surg. 2024 Jan 2;65(1):ezae013. [CrossRef]
- Lee HC, Yoon HK, Nam K, Cho YJ, Kim TK, Kim WH, Bahk JH. Derivation and Validation of Machine Learning Approaches to Predict Acute Kidney Injury after Cardiac Surgery. J Clin Med. 2018 Oct 3;7(10):322. [CrossRef]
- Allyn J, Allou N, Augustin P, Philip I, Martinet O, Belghiti M, Provenchere S, Montravers P, Ferdynus C. A Comparison of a Machine Learning Model with EuroSCORE II in Predicting Mortality after Elective Cardiac Surgery: A Decision Curve Analysis. PLoS One. 2017 Jan 6;12(1):e0169772. [CrossRef]
- Palmieri V, Montisci A, Vietri MT, Colombo PC, Sala S, Maiello C, Coscioni E, Donatelli F, Napoli C. Artificial intelligence, big data and heart transplantation: Actualities. Int J Med Inform. 2023 Aug;176:105110. [CrossRef]
- Agasthi P, Buras MR, Smith SD, Golafshar MA, Mookadam F, Anand S, Rosenthal JL, Hardaway BW, DeValeria P, Arsanjani R. Machine learning helps predict long-term mortality and graft failure in patients undergoing heart transplant. Gen Thorac Cardiovasc Surg. 2020 Dec;68(12):1369-1376. [CrossRef]
- Mestres CA, Quintana E, Pereda D. Will artificial intelligence help us in predicting outcomes in cardiac surgery? J Card Surg. 2022 Nov;37(11):3846-3847.
- Penny-Dimri JC, Bergmeir C, Perry L, Hayes L, Bellomo R, Smith JA. Machine learning to predict adverse outcomes after cardiac surgery: a systematic review and meta-analysis. J Thorac Cardiovasc Surg. 2022;163(6):2075-2087.e9. [CrossRef]
- Bodenhofer U, Haslinger-Eisterer B, Minichmayer A, Hermanutz G, Meier J. Machine learning-based risk profile classification of patients undergoing elective heart valve surgery. Eur J Cardiothorac Surg. 2021 Dec 1;60(6):1378-1385.
- Shuhaiber JH, Conte JV. Machine learning in heart valve surgery. Eur J Cardiothorac Surg. 2021 Dec 1;60(6):1386-1387. [CrossRef]
- Gomes B, Pilz M, Reich C, Leuschner F, Konstandin M, Katus HA, Meder B. Machine learning-based risk prediction of intrahospital clinical outcomes in patients undergoing TAVI. Clin Res Cardiol. 2021 Mar;110(3):343-356. [CrossRef]
- Kalisnik JM, Bauer A, Vogt FA, Stickl FJ, Zibert J, Fittkau M, Bertsch T, Kounev S, Fischlein T. Artificial intelligence-based early detection of acute kidney injury after cardiac surgery. Eur J Cardiothorac Surg. 2022 Oct 4;62(5):ezac289. doi: 10.1093/ejcts/ezac289.
- Fliegenschmidt J, Hulde N, Preising MG, Ruggeri S, Szymanowski R, Meesseman L, Sun H, von Dossow V. Artificial intelligence predicts delirium following cardiac surgery: A case study. J Clin Anesth. 2021 Dec;75:110473. [CrossRef]
- Goswami R. The current state of artificial intelligence in cardiac transplantation. Curr Opin Organ Transplant. 2021 Jun 1;26(3):296-301.
- Naruka V, Arjomandi Rad A, Subbiah Ponniah H, Francis J, Vardanyan R, Tasoudis P, Magouliotis DE, Lazopoulos GL, Salmasi MY, Athanasiou T. Machine learning and artificial intelligence in cardiac transplantation: A systematic review. Artif Organs. 2022 Sep;46(9):1741-1753. [CrossRef]
- Lisboa PJG, Jayabalan M, Ortega-Martorell S, Olier I, Medved D, Nilsson J. Enhanced survival prediction using explainable artificial intelligence in heart transplantation. Sci Rep. 2022 Nov 14;12(1):19525. [CrossRef]
- Lin Y, Hu J, Xu R, Wu S, Ma F, Liu H, Xie Y, Li X. Application of Logistic Regression and Artificial Intelligence in the Risk Prediction of Acute Aortic Dissection Rupture. J Clin Med. 2022 Dec 26;12(1):179.
- Mastrodicasa D, Codari M, Bäumler K, Sandfort V, Shen J, Mistelbauer G, Hahn LD, Turner VL, Desjardins B, Willemink MJ, Fleischmann D. Artificial Intelligence Applications in Aortic Dissection Imaging. Semin Roentgenol. 2022 Oct;57(4):357-363.
- Ostberg NP, Zafar MA, Mukherjee SK, Ziganshin BA, Elefteriades JA. A machine learning approach for predicting complications in descending and thoracoabdominal aortic aneurysms. J Thorac Cardiovasc Surg. 2023 Oct;166(4):1011-1020.e3.
- Guo T, Fang Z, Yang G, Zhou Y, Ding N, Peng W, Gong X, He H, Pan X, Chai X. Machine Learning Models for Predicting In-Hospital Mortality in Acute Aortic Dissection Patients. Front Cardiovasc Med. 2021 Sep 17;8:727773. [CrossRef]
- Farooqi HA, Nabi R. Harnessing artificial intelligence, machine learning and novel approaches to tackle mortality in acute type A aortic dissection. Eur J Cardiothorac Surg. 2024 Mar 29;65(4):ezae131.
- Fleischmann D, Afifi RO, Casanegra AI, Elefteriades JA, Gleason TG, Hanneman K, Roselli EE, Willemink MJ, Fischbein MP; American Heart Association Council on Cardiovascular Radiology and Intervention; Council on Arteriosclerosis, Thrombosis and Vascular Biology; Council on Clinical Cardiology; and Council on Cardiovascular Surgery and Anesthesia. Imaging and Surveillance of Chronic Aortic Dissection: A Scientific Statement From the American Heart Association. Circ Cardiovasc Imaging. 2022 Mar;15(3):e000075.
- Zhou M, Luo X, Wang X, Xie T, Wang Y, Shi Z, Wang M, Fu W. Deep Learning Prediction for Distal Aortic Remodeling After Thoracic Endovascular Aortic Repair in Stanford Type B Aortic Dissection. J Endovasc Ther. 2024 Oct;31(5):910-918. [CrossRef]
- Antonacci AC, Dechario SP, Antonacci C, Husk G, Patel V, Nicastro J, Coppa G, Jarrett M. Cognitive Bias Impact on Management of Postoperative Complications, Medical Error, and Standard of Care. J Surg Res. 2021 Feb;258:47-53.
- Armstrong BA, Dutescu IA, Tung A, Carter DN, Trbovich PL, Wong S, Saposnik G, Grantcharov T. Cognitive biases in surgery: systematic review. Br J Surg. 2023 May 16;110(6):645-654.
- Varpaei HA, Robbins LB, Ling J, Lehto RH, Bender CM. Anaesthesia-related cognitive dysfunction following cardiothoracic surgery in late middle-age and younger adults: A scoping review. Nurs Crit Care. 2024 May;29(3):457-465. [CrossRef]
- Prowle JR, Forni LG, Bell M, Chew MS, Edwards M, Grams ME, Grocott MPW, Liu KD, McIlroy D, Murray PT, Ostermann M, Zarbock A, Bagshaw SM, Bartz R, Bell S, Bihorac A, Gan TJ, Hobson CE, Joannidis M, Koyner JL, Levett DZH, Mehta RL, Miller TE, Mythen MG, Nadim MK, Pearse RM, Rimmele T, Ronco C, Shaw AD, Kellum JA. Postoperative acute kidney injury in adult non-cardiac surgery: joint consensus report of the Acute Disease Quality Initiative and PeriOperative Quality Initiative. Nat Rev Nephrol. 2021 Sep;17(9):605-618.
- Li G, Wang H, Zhang M, Tupin S, Qiao A, Liu Y, Ohta M, Anzai H. Prediction of 3D Cardiovascular hemodynamics before and after coronary artery bypass surgery via deep learning. Commun Biol. 2021 Jan 22;4(1):99. [CrossRef]
- Stam WT, Goedknegt LK, Ingwersen EW, Schoonmade LJ, Bruns ERJ, Daams F. The prediction of surgical complications using artificial intelligence in patients undergoing major abdominal surgery: A systematic review. Surgery. 2022 Apr;171(4):1014-1021.
- Lam K, Chen J, Wang Z, Iqbal FM, Darzi A, Lo B, Purkayastha S, Kinross JM. Machine learning for technical skill assessment in surgery: a systematic review. NPJ Digit Med. 2022 Mar 3;5(1):24.
- Farhadi F, Barnes MR, Sugito HR, Sin JM, Henderson ER, Levy JJ. Applications of artificial intelligence in orthopaedic surgery. Front Med Technol. 2022 Dec 15;4:995526.
- Aggarwal R, Sounderajah V, Martin G, Ting DSW, Karthikesalingam A, King D, Ashrafian H, Darzi A. Diagnostic accuracy of deep learning in medical imaging: a systematic review and meta-analysis. NPJ Digit Med. 2021 Apr 7;4(1):65.
- Cepolina F, Razzoli RP. An introductory review of robotically assisted surgical systems. Int J Med Robot. 2022 Aug;18(4):e2409.
- Özgüner O, Shkurti T, Huang S, Hao R, Jackson RC, Newman WS, Çavuşoğlu MC. Camera-Robot Calibration for the da Vinci® Robotic Surgery System. IEEE Trans Autom Sci Eng. 2020 Oct;17(4):2154-2161. [CrossRef]
- Australian Genomics Health Alliance Acute Care Flagship; Lunke S, Eggers S, Wilson M, Patel C, Barnett CP, Pinner J, Sandaradura SA, Buckley MF, Krzesinski EI, de Silva MG, Brett GR, Boggs K, Mowat D, Kirk EP, Adès LC, Akesson LS, Amor DJ, Ayres S, Baxendale A, Borrie S, Bray A, Brown NJ, Chan CY, Chong B, Cliffe C, Delatycki MB, Edwards M, Elakis G, Fahey MC, Fennell A, Fowles L, Gallacher L, Higgins M, Howell KB, Hunt L, Hunter MF, Jones KJ, King S, Kumble S, Lang S, Le Moing M, Ma A, Phelan D, Quinn MCJ, Richards A, Richmond CM, Riseley J, Rodgers J, Sachdev R, Sadedin S, Schlapbach LJ, Smith J, Springer A, Tan NB, Tan TY, Temple SL, Theda C, Vasudevan A, White SM, Yeung A, Zhu Y, Martyn M, Best S, Roscioli T, Christodoulou J, Stark Z. Feasibility of Ultra-Rapid Exome Sequencing in Critically Ill Infants and Children With Suspected Monogenic Conditions in the Australian Public Health Care System. JAMA. 2020 Jun 23;323(24):2503-2511.
- Paterson C, Bacon R, Dwyer R, Morrison KS, Toohey K, O’Dea A, Slade J, Mortazavi R, Roberts C, Pranavan G, Cooney C, Nahon I, Hayes SC. The Role of Telehealth During the COVID-19 Pandemic Across the Interdisciplinary Cancer Team: Implications for Practice. Semin Oncol Nurs. 2020 Dec;36(6):151090. [CrossRef]
- Picozzi P, Nocco U, Labate C, Gambini I, Puleo G, Silvi F, Pezzillo A, Mantione R, Cimolin V. Advances in Robotic Surgery: A Review of New Surgical Platforms. Electronics. 2024; 13(23):4675.
- Innocenti B, Bori E. Robotics in orthopaedic surgery: why, what and how? Arch Orthop Trauma Surg. 2021 Dec;141(12):2035-2042.
- Sameera V, Bindra A, Rath GP. Human errors and their prevention in healthcare. J Anaesthesiol Clin Pharmacol. 2021 Jul-Sep;37(3):328-335.
- Politi RE, Mills PD, Zubkoff L, Neily J. Delays in Diagnosis, Treatment, and Surgery: Root Causes, Actions Taken, and Recommendations for Healthcare Improvement. J Patient Saf. 2022 Oct 1;18(7):e1061-e1066.
- Ferrari E, Gallo M, Wang C, Zhang L, Taramasso M, Maisano F, Pirelli L, Berdajs D, von Segesser LK. Three-dimensional printing in adult cardiovascular medicine for surgical and transcatheter procedural planning, teaching and technological innovation. Interact Cardiovasc Thorac Surg. 2020 Feb 1;30(2):203-214. [CrossRef]
- Duhaylongsod F. Artificial artificial intelligence: surgeon intuition and computers to predict graft patency. J Thorac Cardiovasc Surg. 2006 Sep;132(3):466-7.
- Dias RD, Shah JA, Zenati MA. Artificial intelligence in cardiothoracic surgery. Minerva Cardioangiol. 2020 Oct;68(5):532-538.
- AZ. Jones B, Reed B, Hayanga JA. Autonomously Driven: Artificial Intelligence in Cardiothoracic Surgery. Ann Thorac Surg. 2020 Aug;110(2):373.
- Siontis KC, Noseworthy PA, Attia ZI, Friedman PA. Artificial intelligence-enhanced electrocardiography in cardiovascular disease management. Nat Rev Cardiol. 2021 Jul;18(7):465-478. [CrossRef]
- Maier-Hein L, Eisenmann M, Sarikaya D, März K, Collins T, Malpani A, Fallert J, Feussner H, Giannarou S, Mascagni P, Nakawala H, Park A, Pugh C, Stoyanov D, Vedula SS, Cleary K, Fichtinger G, Forestier G, Gibaud B, Grantcharov T, Hashizume M, Heckmann-Nötzel D, Kenngott HG, Kikinis R, Mündermann L, Navab N, Onogur S, Roß T, Sznitman R, Taylor RH, Tizabi MD, Wagner M, Hager GD, Neumuth T, Padoy N, Collins J, Gockel I, Goedeke J, Hashimoto DA, Joyeux L, Lam K, Leff DR, Madani A, Marcus HJ, Meireles O, Seitel A, Teber D, Ückert F, Müller-Stich BP, Jannin P, Speidel S. Surgical data science - from concepts toward clinical translation. Med Image Anal. 2022 Feb;76:102306.
- Dubey R, Bryde DJ, Dwivedi YK, Graham G, Foropon C, Papadopoulos T. Dynamic digital capabilities and supply chain resilience: The role of government effectiveness. International Journal of Production Economics. 2023 Apr 1;258:108790.
- Sutton RT, Pincock D, Baumgart DC, Sadowski DC, Fedorak RN, Kroeker KI. An overview of clinical decision support systems: benefits, risks, and strategies for success. NPJ Digit Med. 2020 Feb 6;3:17.
- Patil S, Shankar H. Transforming healthcare: harnessing the power of AI in the modern era. International Journal of Multidisciplinary Sciences and Arts. 2023 Jul 10;2(1):60-70.
- Kumar K, Kumar P, Deb D, Unguresan ML, Muresan V. Artificial Intelligence and Machine Learning Based Intervention in Medical Infrastructure: A Review and Future Trends. Healthcare (Basel). 2023 Jan 10;11(2):207.
- Zhou S, Ma X, Jiang S, Huang X, You Y, Shang H, Lu Y. A retrospective study on the effectiveness of Artificial Intelligence-based Clinical Decision Support System (AI-CDSS) to improve the incidence of hospital-related venous thromboembolism (VTE). Ann Transl Med. 2021 Mar;9(6):491.
- Maheshwari K, Cywinski JB, Papay F, Khanna AK, Mathur P. Artificial Intelligence for Perioperative Medicine: Perioperative Intelligence. Anesth Analg. 2023 Apr 1;136(4):637-645. [CrossRef]
- James MT, Har BJ, Tyrrell BD, Faris PD, Tan Z, Spertus JA, Wilton SB, Ghali WA, Knudtson ML, Sajobi TT, Pannu NI, Klarenbach SW, Graham MM. Effect of Clinical Decision Support With Audit and Feedback on Prevention of Acute Kidney Injury in Patients Undergoing Coronary Angiography: A Randomized Clinical Trial. JAMA. 2022 Sep 6;328(9):839-849.
- Zenati MA, Kennedy-Metz L, Dias RD. Cognitive Engineering to Improve Patient Safety and Outcomes in Cardiothoracic Surgery. Semin Thorac Cardiovasc Surg. 2020 Spring;32(1):1-7. [CrossRef]
- Mumtaz H, Saqib M, Ansar F, Zargar D, Hameed M, Hasan M, Muskan P. The future of Cardiothoracic surgery in Artificial intelligence. Ann Med Surg (Lond). 2022 Jul 31;80:104251.
- Kennedy-Metz LR, Mascagni P, Torralba A, Dias RD, Perona P, Shah JA, Padoy N, Zenati MA. Computer Vision in the Operating Room: Opportunities and Caveats. IEEE Trans Med Robot Bionics. 2021 Feb;3(1):2-10. doi: 10.1109/tmrb.2020.3040002.
- Padoy N. Machine and deep learning for workflow recognition during surgery. Minim Invasive Ther Allied Technol. 2019 Apr;28(2):82-90.
- Park SY, Lee JH, Stein H, Heo SY, Kim HK. Initial experience with and surgical outcomes of da Vinci single-port system in general thoracic surgery. J Thorac Dis. 2022 Jun;14(6):1933-1940.
- Ojima T, Nakamura M, Hayata K, Kitadani J, Takeuchi A, Yamaue H. Comparison of short-term surgical outcomes using da Vinci S, Si and Xi Surgical System for robotic gastric cancer surgery. Sci Rep. 2021 May 26;11(1):11063.
- Taye MM. Understanding of Machine Learning with Deep Learning: Architectures, Workflow, Applications and Future Directions. Computers. 2023; 12(5):91.
- Huang JD, Wang J, Ramsey E, Leavey G, Chico TJA, Condell J. Applying Artificial Intelligence to Wearable Sensor Data to Diagnose and Predict Cardiovascular Disease: A Review. Sensors (Basel). 2022 Oct 20;22(20):8002. [CrossRef]
- Zhong Z, Yuan X, Liu S, Yang Y, Liu F. Machine learning prediction models for prognosis of critically ill patients after open-heart surgery. Sci Rep. 2021 Feb 9;11(1):3384.
- Zea-Vera R, Ryan CT, Navarro SM, Havelka J, Wall MJ Jr, Coselli JS, Rosengart TK, Chatterjee S, Ghanta RK. Development of a Machine Learning Model to Predict Outcomes and Cost After Cardiac Surgery. Ann Thorac Surg. 2023 Jun;115(6):1533-1542.
- Garza-Herrera R. Humans use tools: From handcrafted tools to artificial intelligence. J Vasc Surg Venous Lymphat Disord. 2024 Mar;12(2):101705.
- Zhang J, Gajjala S, Agrawal P, Tison GH, Hallock LA, Beussink-Nelson L, Lassen MH, Fan E, Aras MA, Jordan C, Fleischmann KE, Melisko M, Qasim A, Shah SJ, Bajcsy R, Deo RC. Fully Automated Echocardiogram Interpretation in Clinical Practice. Circulation. 2018 Oct 16;138(16):1623-1635.
- Thompson WR, Reinisch AJ, Unterberger MJ, Schriefl AJ. Artificial Intelligence-Assisted Auscultation of Heart Murmurs: Validation by Virtual Clinical Trial. Pediatr Cardiol. 2019 Mar;40(3):623-629. [CrossRef]
- AA. Sun S, Jiang Z, Wang H, Fang Y. Automatic moment segmentation and peak detection analysis of heart sound pattern via short-time modified Hilbert transform. Comput Methods Programs Biomed. 2014 May;114(3):219-30.
- Lin YT, Lin CS, Tsai CS, Tsai DJ, Lou YS, Fang WH, Lee YT, Lin C. Comprehensive clinical application analysis of artificial intelligence-enabled electrocardiograms for screening multiple valvular heart diseases. Aging (Albany NY). 2024 May 16;16(10):8717-8731.
- Long Q, Ye X, Zhao Q. Artificial intelligence and automation in valvular heart diseases. Cardiol J. 2020;27(4):404-420.
- Kusunose K, Abe T, Haga A, Fukuda D, Yamada H, Harada M, Sata M. A Deep Learning Approach for Assessment of Regional Wall Motion Abnormality From Echocardiographic Images. JACC Cardiovasc Imaging. 2020 Feb;13(2 Pt 1):374-381.
- G S, Gopalakrishnan U, Parthinarupothi RK, Madathil T. Deep learning supported echocardiogram analysis: A comprehensive review. Artif Intell Med. 2024 May;151:102866.
- Jeganathan J, Knio Z, Amador Y, Hai T, Khamooshian A, Matyal R, Khabbaz KR, Mahmood F. Artificial intelligence in mitral valve analysis. Ann Card Anaesth. 2017 Apr-Jun;20(2):129-134.
- Ionasec RI, Georgescu B, Gassner E, Vogt S, Kutter O, Scheuering M, Navab N, Comaniciu D. Dynamic model-driven quantitative and visual evaluation of the aortic valve from 4D CT. Med Image Comput Comput Assist Interv. 2008;11(Pt 1):686-94.
- Lalys F, Esneault S, Castro M, Royer L, Haigron P, Auffret V, Tomasi J. Automatic aortic root segmentation and anatomical landmarks detection for TAVI procedure planning. Minim Invasive Ther Allied Technol. 2019 Jun;28(3):157-164.
- Baeßler B, Mauri V, Bunck AC, Pinto Dos Santos D, Friedrichs K, Maintz D, Rudolph T. Software-automated multidetector computed tomography-based prosthesis-sizing in transcatheter aortic valve replacement: Inter-vendor comparison and relation to patient outcome. Int J Cardiol. 2018 Dec 1;272:267-272.
- Bernard O, Lalande A, Zotti C, Cervenansky F, Yang X, Heng PA, Cetin I, Lekadir K, Camara O, Gonzalez Ballester MA, Sanroma G, Napel S, Petersen S, Tziritas G, Grinias E, Khened M, Kollerathu VA, Krishnamurthi G, Rohe MM, Pennec X, Sermesant M, Isensee F, Jager P, Maier-Hein KH, Full PM, Wolf I, Engelhardt S, Baumgartner CF, Koch LM, Wolterink JM, Isgum I, Jang Y, Hong Y, Patravali J, Jain S, Humbert O, Jodoin PM. Deep Learning Techniques for Automatic MRI Cardiac Multi-Structures Segmentation and Diagnosis: Is the Problem Solved? IEEE Trans Med Imaging. 2018 Nov;37(11):2514-2525.
- Backhaus SJ, Staab W, Steinmetz M, Ritter CO, Lotz J, Hasenfuß G, Schuster A, Kowallick JT. Fully automated quantification of biventricular volumes and function in cardiovascular magnetic resonance: applicability to clinical routine settings. J Cardiovasc Magn Reson. 2019 Apr 25;21(1):24. [CrossRef]
- Fries JA, Varma P, Chen VS, Xiao K, Tejeda H, Saha P, Dunnmon J, Chubb H, Maskatia S, Fiterau M, Delp S, Ashley E, Ré C, Priest JR. Weakly supervised classification of aortic valve malformations using unlabeled cardiac MRI sequences. Nat Commun. 2019 Jul 15;10(1):3111.
- Bowdish ME, D’Agostino RS, Thourani VH, Schwann TA, Krohn C, Desai N, Shahian DM, Fernandez FG, Badhwar V. STS Adult Cardiac Surgery Database: 2021 Update on Outcomes, Quality, and Research. Ann Thorac Surg. 2021 Jun;111(6):1770-1780. [CrossRef]
- Han M, Chen L, Aras K, Liang C, Chen X, Zhao H, Li K, Faye NR, Sun B, Kim JH, Bai W, Yang Q, Ma Y, Lu W, Song E, Baek JM, Lee Y, Liu C, Model JB, Yang G, Ghaffari R, Huang Y, Efimov IR, Rogers JA. Catheter-integrated soft multilayer electronic arrays for multiplexed sensing and actuation during cardiac surgery. Nat Biomed Eng. 2020 Oct;4(10):997-1009.
- Ljungqvist O, de Boer HD, Balfour A, Fawcett WJ, Lobo DN, Nelson G, Scott MJ, Wainwright TW, Demartines N. Opportunities and Challenges for the Next Phase of Enhanced Recovery After Surgery: A Review. JAMA Surg. 2021 Aug 1;156(8):775-784. doi: 10.1001/jamasurg.2021.0586. Erratum in: JAMA Surg. 2021 Aug 1;156(8):800. [CrossRef]
- Manickam P, Mariappan SA, Murugesan SM, Hansda S, Kaushik A, Shinde R, Thipperudraswamy SP. Artificial Intelligence (AI) and Internet of Medical Things (IoMT) Assisted Biomedical Systems for Intelligent Healthcare. Biosensors (Basel). 2022 Jul 25;12(8):562.
- Maier-Hein L, Vedula SS, Speidel S, Navab N, Kikinis R, Park A, Eisenmann M, Feussner H, Forestier G, Giannarou S, Hashizume M, Katic D, Kenngott H, Kranzfelder M, Malpani A, März K, Neumuth T, Padoy N, Pugh C, Schoch N, Stoyanov D, Taylor R, Wagner M, Hager GD, Jannin P. Surgical data science for next-generation interventions. Nat Biomed Eng. 2017 Sep;1(9):691-696.
- Loftus TJ, Upchurch GR Jr, Bihorac A. Use of Artificial Intelligence to Represent Emergent Systems and Augment Surgical Decision-making. JAMA Surg. 2019 Sep 1;154(9):791-792. [CrossRef]
- BC. Montisci A, Palmieri V, Vietri MT, Sala S, Maiello C, Donatelli F, Napoli C. Big Data in cardiac surgery: real world and perspectives. J Cardiothorac Surg. 2022 Oct 29;17(1):277.
- Vasey B, Nagendran M, Campbell B, Clifton DA, Collins GS, Denaxas S, Denniston AK, Faes L, Geerts B, Ibrahim M, Liu X, Mateen BA, Mathur P, McCradden MD, Morgan L, Ordish J, Rogers C, Saria S, Ting DSW, Watkinson P, Weber W, Wheatstone P, McCulloch P; DECIDE-AI expert group. Reporting guideline for the early stage clinical evaluation of decision support systems driven by artificial intelligence: DECIDE-AI. BMJ. 2022 May 18;377:e070904. [CrossRef]
- Zavaleta-Monestel E, Quesada-Villaseñor R, Arguedas-Chacón S, García-Montero J, Barrantes-López M, Salas-Segura J, Anchía-Alfaro A, Nieto-Bernal D, Diaz-Juan DE. Revolutionizing Healthcare: Qure. AI’s Innovations in Medical Diagnosis and Treatment. Cureus. 2024 Jun 3;16(6):e61585.
- Harrer S, Shah P, Antony B, Hu J. Artificial Intelligence for Clinical Trial Design. Trends Pharmacol Sci. 2019 Aug;40(8):577-591.
- Moingeon P, Chenel M, Rousseau C, Voisin E, Guedj M. Virtual patients, digital twins and causal disease models: Paving the ground for in silico clinical trials. Drug Discov Today. 2023 Jul;28(7):103605.
- Shaikh F, Dehmeshki J, Bisdas S, Roettger-Dupont D, Kubassova O, Aziz M, Awan O. Artificial Intelligence-Based Clinical Decision Support Systems Using Advanced Medical Imaging and Radiomics. Curr Probl Diagn Radiol. 2021 Mar-Apr;50(2):262-267.
- Schwartz JM, George M, Rossetti SC, Dykes PC, Minshall SR, Lucas E, Cato KD. Factors Influencing Clinician Trust in Predictive Clinical Decision Support Systems for In-Hospital Deterioration: Qualitative Descriptive Study. JMIR Hum Factors. 2022 May 12;9(2):e33960. [CrossRef]
- Kierner S, Kucharski J, Kierner Z. Taxonomy of hybrid architectures involving rule-based reasoning and machine learning in clinical decision systems: A scoping review. J Biomed Inform. 2023 Aug;144:104428. [CrossRef]
- Yasmin F, Shah SMI, Naeem A, Shujauddin SM, Jabeen A, Kazmi S, Siddiqui SA, Kumar P, Salman S, Hassan SA, Dasari C, Choudhry AS, Mustafa A, Chawla S, Lak HM. Artificial intelligence in the diagnosis and detection of heart failure: the past, present, and future. Rev Cardiovasc Med. 2021 Dec 22;22(4):1095-1113. [CrossRef]
- Dearani JA. Robotic heart surgery: Hype or hope? J Thorac Cardiovasc Surg. 2018 Mar;155(3):943-944.
- Kassahun Y, Yu B, Tibebu AT, Stoyanov D, Giannarou S, Metzen JH, Vander Poorten E. Surgical robotics beyond enhanced dexterity instrumentation: a survey of machine learning techniques and their role in intelligent and autonomous surgical actions. Int J Comput Assist Radiol Surg. 2016 Apr;11(4):553-68. doi: 10.1007/s11548-015-1305-z. Epub 2015 Oct 8. Erratum in: Int J Comput Assist Radiol Surg. 2016 May;11(5):847. [CrossRef]
- Liu Z, Zhang C, Ge S. Efficacy and safety of robotic-assisted versus median sternotomy for cardiac surgery: results from a university affiliated hospital. J Thorac Dis. 2023 Apr 28;15(4):1861-1871.
- Dokollari A, Sicouri S, Prendergrast G, Ramlawi B, Mahmud F, Kjelstrom S, Wertan M, Sutter F. Robotic-Assisted Versus Traditional Full-Sternotomy Coronary Artery Bypass Grafting Procedures: A Propensity-Matched Analysis of Hospital Costs. Am J Cardiol. 2024 Feb 15;213:12-19.
- Jung JJ, Jüni P, Lebovic G, Grantcharov T. First-year Analysis of the Operating Room Black Box Study. Ann Surg. 2020 Jan;271(1):122-127.
- Chang YJ, Hung KC, Wang LK, Yu CH, Chen CK, Tay HT, Wang JJ, Liu CF. A Real-Time Artificial Intelligence-Assisted System to Predict Weaning from Ventilator Immediately after Lung Resection Surgery. Int J Environ Res Public Health. 2021 Mar 8;18(5):2713.
- Tseng PY, Chen YT, Wang CH, Chiu KM, Peng YS, Hsu SP, Chen KL, Yang CY, Lee OK. Prediction of the development of acute kidney injury following cardiac surgery by machine learning. Crit Care. 2020 Jul 31;24(1):478.
- Fernandes MPB, Armengol de la Hoz M, Rangasamy V, Subramaniam B. Machine Learning Models with Preoperative Risk Factors and Intraoperative Hypotension Parameters Predict Mortality After Cardiac Surgery. J Cardiothorac Vasc Anesth. 2021 Mar;35(3):857-865.
- Mufti HN, Hirsch GM, Abidi SR, Abidi SSR. Exploiting Machine Learning Algorithms and Methods for the Prediction of Agitated Delirium After Cardiac Surgery: Models Development and Validation Study. JMIR Med Inform. 2019 Oct 23;7(4):e14993.
- AY. Hayıroğlu Mİ, Altay S. The Role of Artificial Intelligence in Coronary Artery Disease and Atrial Fibrillation. Balkan Med J. 2023 May 8;40(3):151-152.
- Clark SC. Can ChatGPT transform cardiac surgery and heart transplantation? J Cardiothorac Surg. 2024 Feb 26;19(1):108.
- Nedadur R, Bhatt N, Liu T, Chu MWA, McCarthy PM, Kline A. The Emerging and Important Role of Artificial Intelligence in Cardiac Surgery. Can J Cardiol. 2024 Oct;40(10):1865-1879.
- Gumbs AA, Frigerio I, Spolverato G, Croner R, Illanes A, Chouillard E, Elyan E. Artificial Intelligence Surgery: How Do We Get to Autonomous Actions in Surgery? Sensors (Basel). 2021 Aug 17;21(16):5526.
- Guni A, Varma P, Zhang J, Fehervari M, Ashrafian H. Artificial Intelligence in Surgery: The Future is Now. Eur Surg Res. 2024 Jan 22. [CrossRef]
- Elendu C, Amaechi DC, Elendu TC, Jingwa KA, Okoye OK, John Okah M, Ladele JA, Farah AH, Alimi HA. Ethical implications of AI and robotics in healthcare: A review. Medicine (Baltimore). 2023 Dec 15;102(50):e36671.
- Riva G, Wiederhold BK, Succi S. Zero Sales Resistance: The Dark Side of Big Data and Artificial Intelligence. Cyberpsychol Behav Soc Netw. 2022 Mar;25(3):169-173. [CrossRef]
- Zhang J, Zhang ZM. Ethics and governance of trustworthy medical artificial intelligence. BMC Med Inform Decis Mak. 2023 Jan 13;23(1):7. [CrossRef]
- Bleher H, Braun M. Diffused responsibility: attributions of responsibility in the use of AI-driven clinical decision support systems. AI Ethics. 2022;2(4):747-761.
- Lopez-Jimenez F, Attia Z, Arruda-Olson AM, Carter R, Chareonthaitawee P, Jouni H, Kapa S, Lerman A, Luong C, Medina-Inojosa JR, Noseworthy PA, Pellikka PA, Redfield MM, Roger VL, Sandhu GS, Senecal C, Friedman PA. Artificial Intelligence in Cardiology: Present and Future. Mayo Clin Proc. 2020 May;95(5):1015-1039.
- Haendel MA, Chute CG, Bennett TD, Eichmann DA, Guinney J, Kibbe WA, Payne PRO, Pfaff ER, Robinson PN, Saltz JH, Spratt H, Suver C, Wilbanks J, Wilcox AB, Williams AE, Wu C, Blacketer C, Bradford RL, Cimino JJ, Clark M, Colmenares EW, Francis PA, Gabriel D, Graves A, Hemadri R, Hong SS, Hripscak G, Jiao D, Klann JG, Kostka K, Lee AM, Lehmann HP, Lingrey L, Miller RT, Morris M, Murphy SN, Natarajan K, Palchuk MB, Sheikh U, Solbrig H, Visweswaran S, Walden A, Walters KM, Weber GM, Zhang XT, Zhu RL, Amor B, Girvin AT, Manna A, Qureshi N, Kurilla MG, Michael SG, Portilla LM, Rutter JL, Austin CP, Gersing KR; N3C Consortium. The National COVID Cohort Collaborative (N3C): Rationale, design, infrastructure, and deployment. J Am Med Inform Assoc. 2021 Mar 1;28(3):427-443.
- Kim M, Sohn H, Choi S, Kim S. Requirements for Trustworthy Artificial Intelligence and its Application in Healthcare. Healthc Inform Res. 2023 Oct;29(4):315-322.
- Jeyaraman M, Balaji S, Jeyaraman N, Yadav S. Unraveling the Ethical Enigma: Artificial Intelligence in Healthcare. Cureus. 2023 Aug 10;15(8):e43262.
- Rasheed K, Qayyum A, Ghaly M, Al-Fuqaha A, Razi A, Qadir J. Explainable, trustworthy, and ethical machine learning for healthcare: A survey. Comput Biol Med. 2022 Oct;149:106043. [CrossRef]
- Ahmad Z, Rahim S, Zubair M, Abdul-Ghafar J. Artificial intelligence (AI) in medicine, current applications and future role with special emphasis on its potential and promise in pathology: present and future impact, obstacles including costs and acceptance among pathologists, practical and philosophical considerations. A comprehensive review. Diagn Pathol. 2021 Mar 17;16(1):24. [CrossRef]
- Oehring R, Ramasetti N, Ng S, Roller R, Thomas P, Winter A, Maurer M, Moosburner S, Raschzok N, Kamali C, Pratschke J, Benzing C, Krenzien F. Use and accuracy of decision support systems using artificial intelligence for tumor diseases: a systematic review and meta-analysis. Front Oncol. 2023 Oct 4;13:1224347.
- M S, Murugappan A, T M. Cognitive computing technological trends and future research directions in healthcare - A systematic literature review. Artif Intell Med. 2023 Apr;138:102513.
- Trayanova NA, Lyon A, Shade J, Heijman J. Computational modeling of cardiac electrophysiology and arrhythmogenesis: toward clinical translation. Physiol Rev. 2024 Jul 1;104(3):1265-1333. [CrossRef]
- Morley J, Machado CCV, Burr C, Cowls J, Joshi I, Taddeo M, Floridi L. The ethics of AI in health care: A mapping review. Soc Sci Med. 2020 Sep;260:113172.
- Reddi HV, Wand H, Funke B, Zimmermann MT, Lebo MS, Qian E, Shirts BH, Zou YS, Zhang BM, Rose NC, Abu-El-Haija A; ACMG Laboratory Quality Assurance Committee. Electronic address: documents@acmg.net. Laboratory perspectives in the development of polygenic risk scores for disease: A points to consider statement of the American College of Medical Genetics and Genomics (ACMG). Genet Med. 2023 May;25(5):100804. [CrossRef]
- Ahsani-Estahbanati E, Sergeevich Gordeev V, Doshmangir L. Interventions to reduce the incidence of medical error and its financial burden in health care systems: A systematic review of systematic reviews. Front Med (Lausanne). 2022 Jul 27;9:875426.
- Nedadur R, Wang B, Tsang W. Artificial intelligence for the echocardiographic assessment of valvular heart disease. Heart. 2022 Sep 26;108(20):1592-1599. doi: 10.1136/heartjnl-2021-319725.
- Boal M, Di Girasole CG, Tesfai F, Morrison TEM, Higgs S, Ahmad J, Arezzo A, Francis N. Evaluation status of current and emerging minimally invasive robotic surgical platforms. Surg Endosc. 2024 Feb;38(2):554-585.
- Knudsen JE, Ghaffar U, Ma R, Hung AJ. Clinical applications of artificial intelligence in robotic surgery. J Robot Surg. 2024 Mar 1;18(1):102.
- Wang DD, Qian Z, Vukicevic M, Engelhardt S, Kheradvar A, Zhang C, Little SH, Verjans J, Comaniciu D, O’Neill WW, Vannan MA. 3D Printing, Computational Modeling, and Artificial Intelligence for Structural Heart Disease. JACC Cardiovasc Imaging. 2021 Jan;14(1):41-60.
- Krittanawong C, Johnson KW, Rosenson RS, Wang Z, Aydar M, Baber U, Min JK, Tang WHW, Halperin JL, Narayan SM. Deep learning for cardiovascular medicine: a practical primer. Eur Heart J. 2019 Jul 1;40(25):2058-2073.
- Topol EJ. High-performance medicine: the convergence of human and artificial intelligence. Nat Med. 2019 Jan;25(1):44-56. [CrossRef]
- Krajcer Z. Artificial Intelligence in Cardiovascular Medicine: Historical Overview, Current Status, and Future Directions. Tex Heart Inst J. 2022 Mar 1;49(2):e207527.
- Shah P, Kendall F, Khozin S, Goosen R, Hu J, Laramie J, Ringel M, Schork N. Artificial intelligence and machine learning in clinical development: a translational perspective. NPJ Digit Med. 2019 Jul 26;2:69.
- Zong Q, He C, Long B, Huang Q, Chen Y, Li Y, Dang Y, Cai C. Targeted Delivery of Nanoparticles to Blood Vessels for the Treatment of Atherosclerosis. Biomedicines. 2024 Jul 6;12(7):1504. [CrossRef]
- Gray RA, Pathmanathan P. Patient-Specific Cardiovascular Computational Modeling: Diversity of Personalization and Challenges. J Cardiovasc Transl Res. 2018 Apr;11(2):80-88. [CrossRef]
- Rad AA, Vardanyan R, Lopuszko A, Alt C, Stoffels I, Schmack B, Ruhparwar A, Zhigalov K, Zubarevich A, Weymann A. Virtual and Augmented Reality in Cardiac Surgery. Braz J Cardiovasc Surg. 2022 Mar 10;37(1):123-127.
- Sulague RM, Beloy FJ, Medina JR, Mortalla ED, Cartojano TD, Macapagal S, Kpodonu J. Artificial intelligence in cardiac surgery: A systematic review. World J Surg. 2024 Sep;48(9):2073-2089.
- Bhushan R, Grover V. The Advent of Artificial Intelligence into Cardiac Surgery: A Systematic Review of Our Understanding. Braz J Cardiovasc Surg. 2024 Jul 22;39(5):e20230308. [CrossRef]
- Mestres CA, Quintana E, Pereda D. Will artificial intelligence help us in predicting outcomes in cardiac surgery? J Card Surg. 2022 Nov;37(11):3846-3847.
| Reference Number | Authors | Year | Key Outcomes and Contributions | Relevance to Review |
|---|---|---|---|---|
| [9] | Allyn J, et al. | 2017 | Compared ML models with EuroSCORE II for mortality prediction after elective cardiac surgery. ML showed superior predictive capabilities. | Directly evaluates AI’s clinical utility in cardiac surgery outcomes. |
| [10] | Nashef SAM & Ali J | 2023 | Explores AI-based risk assessment models for cardiac surgery, emphasizing accuracy and clinical applicability. | Relevant to risk modeling and decision-making in cardiac surgery. |
| [11] | Poullis M | 2024 | Discusses AI’s transformation of risk modeling in cardiac and thoracic surgery, highlighting predictive advances. | Key for understanding AI’s role in predictive risk assessment in this field. |
| [12] | Lee HC, et al. | 2018 | Developed and validated ML models for predicting acute kidney injury after cardiac surgery with high accuracy. | Provides critical insights into AI’s impact on postoperative management. |
| [14] | Palmieri V, Montisci A, Vietri MT, et al. | 2023 | AI applications in heart transplantation, with emphasis on predictive modeling for patient outcomes and diagnostic tools. | Provides insights into the integration of AI in specialized cardiac surgery contexts. |
| [15] | Agasthi P, Buras MR, Smith SD, et al. | 2020 | Explored ML tools for long-term graft survival prediction in heart transplantation. | Relevant to extending AI applications to long-term postoperative outcomes in cardiac surgery. |
| [17] | Penny-Dimri JC, et al. | 2022 | Systematic review of ML methods for predicting adverse outcomes in cardiac surgery, showing promise but limited by data and study design. | Offers a meta-perspective on AI applications in predicting surgical complications. |
| [18] | Bodenhofer U, et al. | 2021 | Demonstrated that ML-based tools outperform EuroSCORE for risk classification in heart valve surgery. | Directly relevant to improving preoperative risk stratification with AI. |
| [19] | Shuhaiber JH, Conte JV | 2021 | Examined ML applications in heart valve surgery, focusing on predictive analytics for outcomes and complications. | Directly applicable to improving precision in valve-related surgical interventions. |
| [20] | Gomes B, et al. | 2021 | Developed ML-based risk prediction for intrahospital outcomes in TAVI, showing superior accuracy over traditional scores. | Highlights AI’s role in precision risk assessment for TAVI. |
| [21] | Kalisnik JM, et al. | 2022 | Developed an AI model for early detection of acute kidney injury post-cardiac surgery, achieving high accuracy. | Critical for postoperative monitoring and complication prevention with AI. |
| [22] | Fliegenschmidt J, et al. | 2021 | Demonstrated AI’s potential for predicting postoperative delirium in cardiac surgery patients. | Expands AI’s applications to cognitive outcome monitoring post-surgery. |
| [24] | Naruka V, et al. | 2022 | Systematic review of ML and AI in cardiac transplantation, emphasizing predictive modeling for graft survival. | Highlights AI’s potential in complex and specialized cardiac interventions. |
| [25] | Lisboa PJG, et al. | 2022 | Developed explainable AI models for predicting survival in heart transplantation. | Relevant for advancing transparency and accuracy in AI predictions in cardiac surgery. |
| [26] | Lin Y, et al. | 2022 | Used AI-based logistic regression for predicting rupture risk in acute aortic dissection patients. | Highlights AI’s role in high-stakes preoperative decision-making. |
| [28] | Ostberg NP, et al. | 2023 | Applied ML to predict complications in thoracoabdominal aortic aneurysms. | Expands AI applications to complex vascular conditions managed in cardiac surgery. |
| [29] | Guo T, et al. | 2021 | Developed ML models for predicting in-hospital mortality in acute aortic dissection. | Highlights AI’s potential in improving acute care decision-making in cardiac surgery. |
| [30] | Farooqi HA & Nabi R | 2024 | Discusses novel AI and ML approaches to reducing mortality in acute type A aortic dissection. | Highlights innovative approaches in critical cardiac conditions. |
| [35] | Varpaei HA, Robbins LB, Ling J, et al. | 2024 | Scoping review on AI-related cognitive dysfunction after cardiothoracic surgery. | Examines postoperative cognitive outcomes, a less explored AI application in cardiac surgery. |
| [37] | Li G, Wang H, Zhang M, et al. | 2021 | Predicts 3D cardiovascular hemodynamics before and after coronary artery bypass using deep learning techniques. | Demonstrates AI’s role in personalized surgical planning and postoperative assessments. |
| [50] | Ferrari E, Gallo M, Wang C, et al. | 2020 | Explores AI and 3D printing for procedural planning, teaching, and innovation in cardiovascular surgeries. | Highlights AI’s role in advanced visualization and surgical preparation. |
| [52] | Dias RD, Shah JA, Zenati MA | 2020 | Discussed AI’s role in cardiothoracic surgery, focusing on real-time decision support and workflow optimization. | Broadly relevant to all facets of AI integration in cardiac surgery. |
| [53] | Jones B, et al. | 2020 | Reviews autonomously driven AI applications in cardiothoracic surgery, focusing on real-time guidance and precision. | Expands understanding of AI’s autonomy in surgical practices. |
| [63] | Zenati MA, et al. | 2020 | Examined cognitive engineering and AI to enhance patient safety and outcomes in cardiothoracic surgery. | Explores interdisciplinary approaches combining AI and cognitive science in surgery. |
| [64] | Mumtaz H, et al. | 2022 | Discusses future directions of AI in cardiothoracic surgery, with focus on surgical innovation and patient outcomes. | Provides forward-looking perspectives on AI applications. |
| [83] | Lalys F, et al. | 2019 | Developed automatic aortic root segmentation and anatomical landmark detection for TAVI procedural planning using AI. | Demonstrates AI’s utility in precision planning for complex cardiac interventions. |
| [109] | Tseng PY, et al. | 2020 | Developed ML models using intraoperative and preoperative data to predict cardiac surgery-associated acute kidney injury. | Highlights AI’s role in enhancing postoperative complication management. |
| [110] | Fernandes MPB, et al. | 2021 | Integrated preoperative and intraoperative data into ML models to predict mortality after cardiac surgery. | Showcases the impact of AI in improving surgical mortality predictions. |
| [111] | Mufti HN, et al. | 2019 | Exploited ML algorithms to predict postoperative delirium following cardiac surgery. | Relevant to improving postoperative cognitive outcome predictions. |
| [113] | Clark SC | 2024 | Explores the transformative role of AI tools like ChatGPT in cardiac surgery and heart transplantation. | Highlights the potential integration of conversational AI in surgery and training. |
| [114] | Nedadur R, et al. | 2024 | Examines emerging AI tools in cardiac surgery, with a focus on clinical applications and future potential. | Discusses cutting-edge advancements in AI for cardiac surgery. |
| [143] | Rad AA, et al. | 2022 | Reviews applications of virtual and augmented reality in cardiac surgery. | Expands on future technologies integrating with AI in cardiac surgery. |
| [144] | Sulague RM, et al. | 2024 | Systematic review of AI applications in cardiac surgery, focusing on risk prediction, surgical accuracy, and clinical outcomes. | Comprehensive summary of AI’s utility across various phases of cardiac surgery. |
| [145] | Bhushan R & Grover V | 2024 | Reviews current understanding of AI’s impact on cardiac surgery, with an emphasis on predictive and robotic technologies. | Provides a systematic overview of AI advancements relevant to cardiac surgery. |
| [146] | Mestres CA, et al. | 2022 | Highlights AI’s potential for predicting surgical outcomes, emphasizing the need for validation and clinical integration. | Discusses challenges and opportunities for AI adoption in outcome prediction. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





