Submitted:
17 December 2024
Posted:
18 December 2024
You are already at the latest version
Abstract
Keywords:
Introduction
CARDIAC CT: Uses, Implications, Advantages, and Limitations
Materials and Methods
Results
Rare Incidental Findings
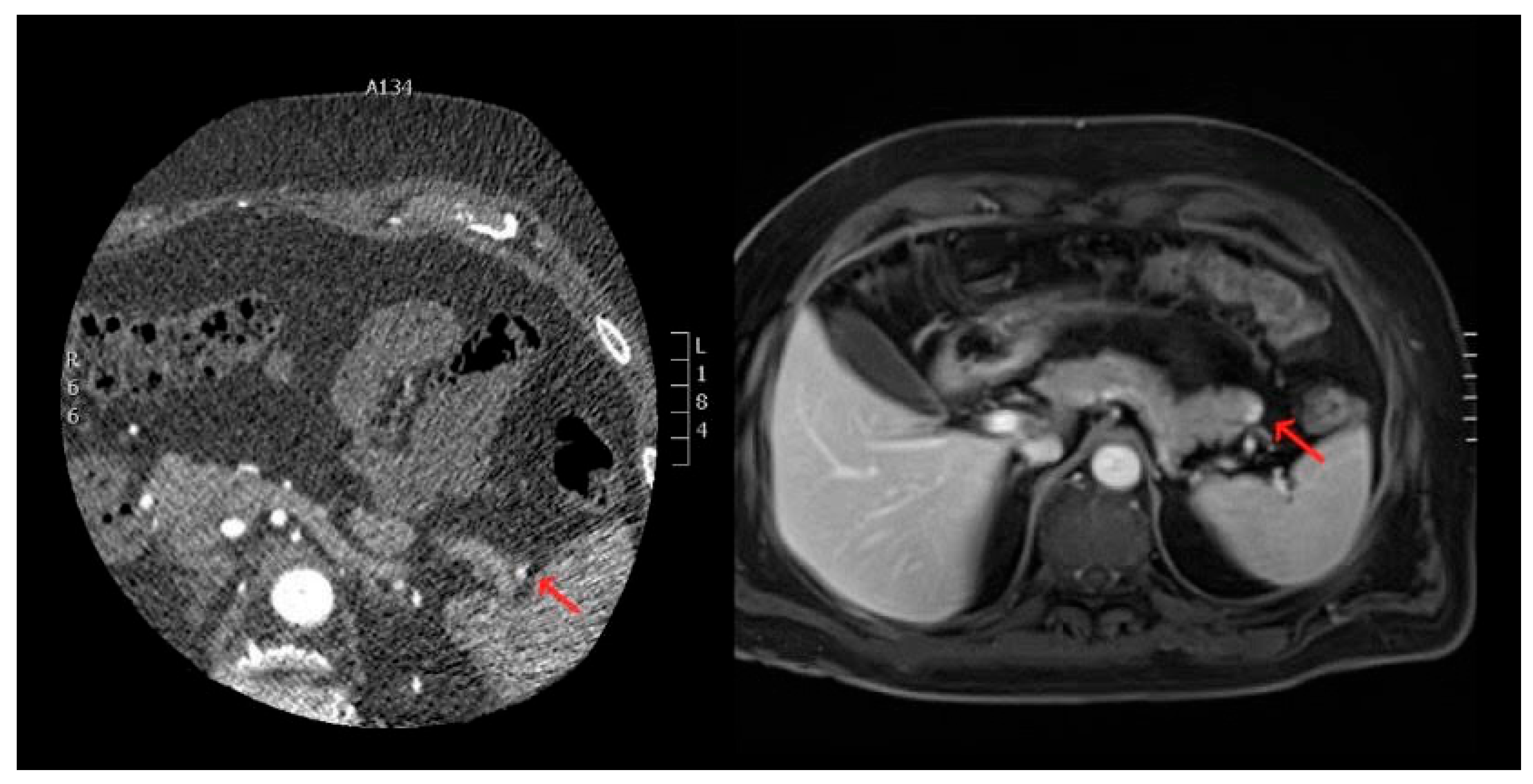
- Neoplastic Lesions in the Thorax and Upper Abdomen: Tumors or neoplastic growths were detected within the thoracic cavity and upper abdominal regions, such as the lung parenchyma and near the upper abdominal organs. These findings included both primary tumors and metastases (Figure 1).
- 2.
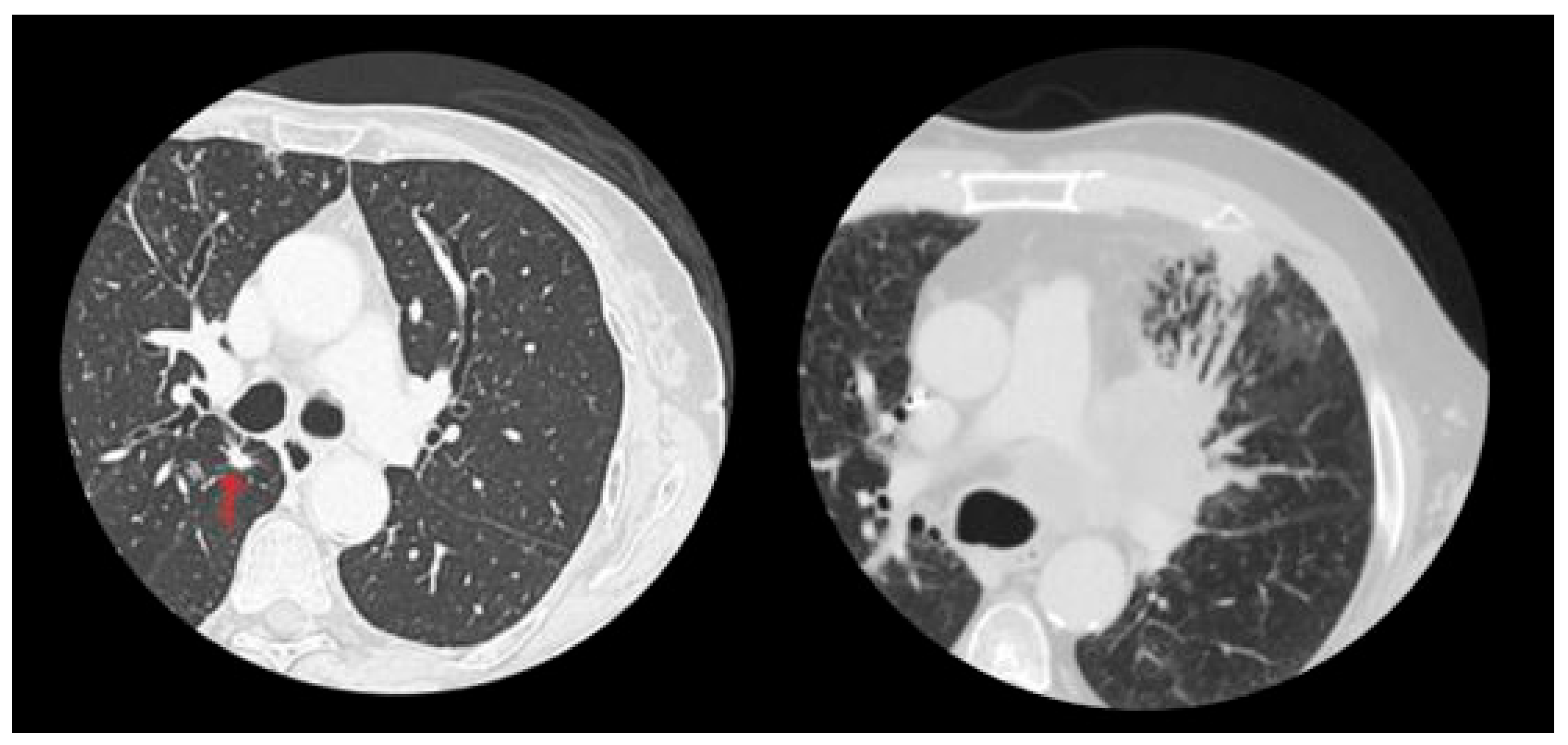
- Pulmonary Micronodules: Small nodular lesions, typically under 10 mm in diameter, were observed within the lung parenchyma. While these findings are often benign, they may require follow-up imaging to rule out early-stage neoplastic processes (Figure 2).
- 3.
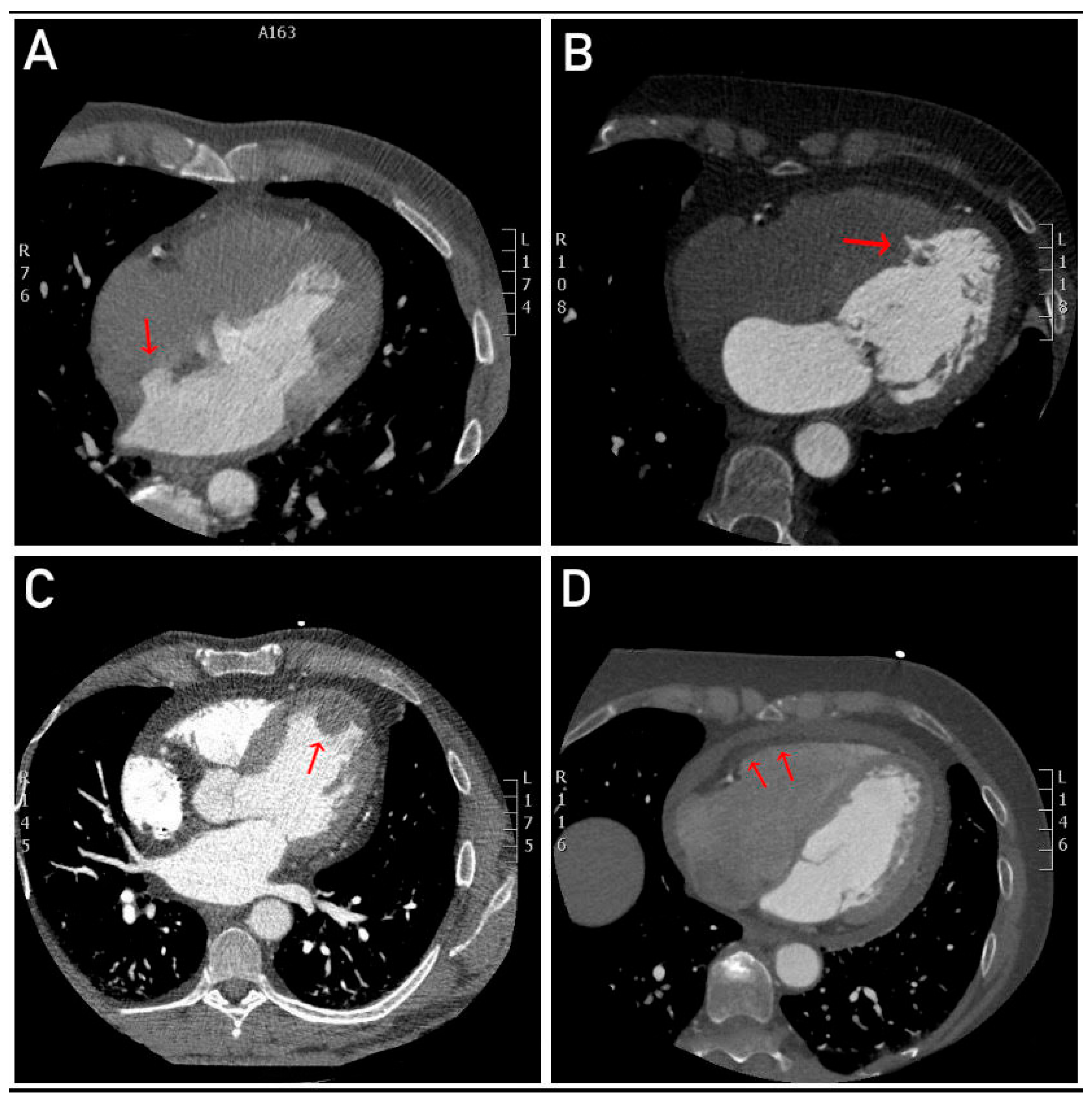
- Nodular Formations in the Myocardium: The presence of nodular structures in the myocardial tissue, which could be indicative of fibrosis, infarction, or other pathologies such as cardiac tumors, was noted.
- 4.
- Revascularization of a False Lumen in a Previously Treated Aortic Dissection: This finding suggests the re-establishment of blood flow to an area of the aorta that was previously affected by dissection, which is a potentially life-threatening condition requiring immediate clinical attention.
- 5.
- Heart Septum Incontinence: This refers to abnormal motion or leakage in the septal region of the heart, which can be associated with congenital or acquired defects in the interatrial or interventricular septum.
- 6.
- Interatrial Septal Aneurysm: An abnormal bulging or pouching of the interatrial septum, which may be associated with an increased risk of embolic events, such as stroke (Figure 3).
- 7.
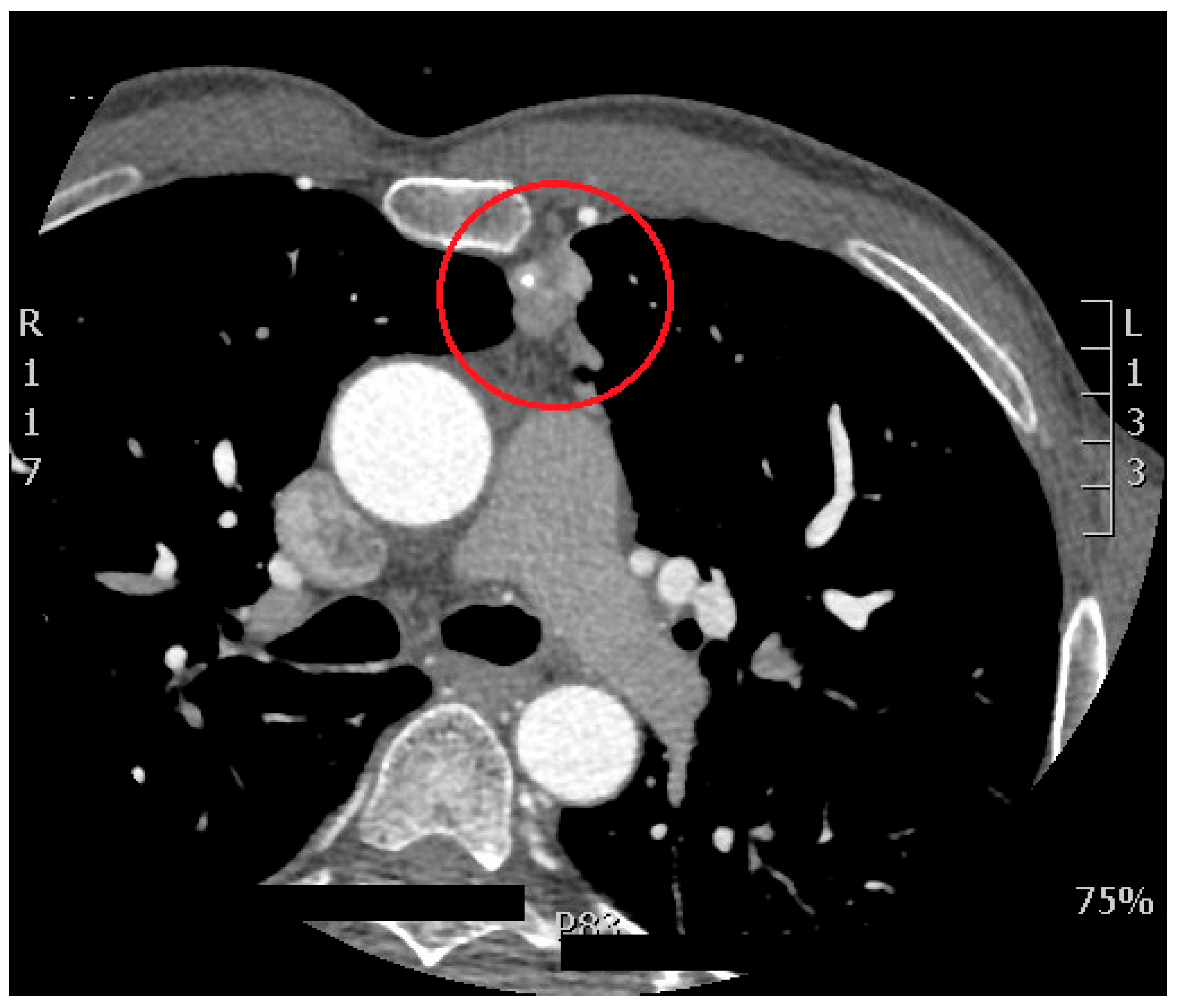
- A retrosternal mass: which was detected as a rare incidental finding during a cardiac CT scan can be clinically significant, as it may indicate a variety of underlying conditions such as malignancies, lymphadenopathy, or benign lesions like thymomas. Although it is an uncommon finding, its detection requires further investigation, as it could be associated with potentially life-threatening conditions, including lung or esophageal tumors. Early identification allows for timely intervention and better clinical management (Figure 4).
Common Incidental Findings
- Hiatal Hernia: A condition where part of the stomach pushes through the diaphragm into the chest cavity. It is often asymptomatic but can be associated with gastroesophageal reflux disease (GERD).
- Hepatic Cystic Lesions: Simple cysts in the liver, which are generally benign but may require monitoring if they increase in size or show atypical features.
- Gallbladder Calculi (Gallstones): The presence of stones in the gallbladder, a common finding that typically has no symptoms unless complications such as cholecystitis arise.
- Signs of Chronic Obstructive Pulmonary Disease (COPD): Radiographic evidence of chronic lung disease, including emphysema and bronchitis, often revealed as parenchymal changes in the lungs and airway abnormalities.
- Pericardial Effusion: The presence of excess fluid in the pericardial sac surrounding the heart, which may be indicative of inflammation, infection, or malignancy
Discussion
Implications for Future Practice
Conclusions
Funding
Ethical Approval
Informed Consent Statement
Conflict of Interest
References
- Hell, M.M.; Emrich, T.; Lurz, P.; von Bardeleben, R.S.; Schmermund, A. Cardiac CT Beyond Coronaries: Focus on Structural Heart Disease. Curr Heart Fail Rep. 2023, 20, 484–492. [Google Scholar] [CrossRef] [PubMed]
- Singh, V.; Dorbala, S. Normal Variants and Pitfalls in Cardiac PET/CT. Semin Nucl Med. 2021, 51, 441–457. [Google Scholar] [CrossRef] [PubMed]
- Daghem, M.; Newby, D.E. Detecting unstable plaques in humans using cardiac CT: Can it guide treatments? Br J Pharmacol. 2021, 178, 2204–2217. [Google Scholar] [CrossRef]
- Azarine, A.; Scalbert, F.; Garçon, P. Cardiac functional imaging. Presse Med. 2022, 51, 104119. [Google Scholar] [CrossRef]
- Bugnon, S. Quid du coro-CT dans le diagnostic de la maladie coronarienne obstructive ? Rev Med Suisse. 2022, 18, 1527. [Google Scholar] [CrossRef] [PubMed]
- Kumar, A.; Stillman, A.E.; Chatzizisis, Y.S. Coronary plaque phenotyping with cardiac CTA: Separating the signal from the noise. Atherosclerosis. 2023, 373, 66–68. [Google Scholar] [CrossRef]
- Bradley, C.; Berry, C. Definition and epidemiology of coronary microvascular disease. J Nucl Cardiol. 2022, 29, 1763–1775. [Google Scholar] [CrossRef]
- Guo, F.; Yan, J.; Xue, X. The relationship between CTA performances and cardiac function indicators in myocardial bridge and mural coronary artery. Am J Transl Res. 2023, 15, 4779–4787. [Google Scholar] [PubMed]
- Apfaltrer, G.; Lavra, F.; De Cecco, C.N.; Varga-Szemes, A.; van Assen, M.; Mastrodicasa, D.; Scarabello, M.; Eid, M.H.; Griffith, L.P.; Nance, J.W.; Litwin, S.E.; Saba, L.; Schoepf, U.J. Predictive Value of Cardiac CTA, Cardiac MRI, and Transthoracic Echocardiography for Cardioembolic Stroke Recurrence. AJR Am J Roentgenol. 2021, 217, 336–346. [Google Scholar] [CrossRef]
- Serruys, P.W.; Hara, H.; Garg, S.; Kawashima, H.; Nørgaard, B.L.; Dweck, M.R.; Bax, J.J.; Knuuti, J.; Nieman, K.; Leipsic, J.A.; Mushtaq, S.; Andreini, D.; Onuma, Y. Coronary Computed Tomographic Angiography for Complete Assessment of Coronary Artery Disease: JACC State-of-the-Art Review. J Am Coll Cardiol. 2021, 78, 713–736. [Google Scholar] [CrossRef] [PubMed]
- Gitsioudis, G.; Marwan, M.; Schneider, S.; Schmermund, A.; Korosoglou, G.; Hausleiter, J.; Schroeder, S.; Rixe, J.; Leber, A.; Bruder, O.; Katus, H.A.; Senges, J.; Achenbach, S. A systematic report on non-coronary cardiac CTA in 1097 patients from the German cardiac CT registry. Eur J Radiol. 2020, 130, 109136. [Google Scholar] [CrossRef] [PubMed]
- Zhao, K.; Zhang, L.; Wang, L.; Zeng, J.; Zhang, Y.; Xie, X. Benign incidental cardiac findings in chest and cardiac CT imaging. Br J Radiol. 2023, 96, 20211302. [Google Scholar] [CrossRef]
- Chen, Y.; Hu, Z.; Li, M.; Jia, Y.; He, T.; Liu, Z.; et al. Comparison of nongated chest CT and dedicated calcium scoring CT for coronary calcium quantification using a 256-dector row CT scanner. Acad Radiol. 2019, 26, e267–74. [Google Scholar] [CrossRef] [PubMed]
- Jacobs, P.C.; Prokop, M.; van der Graaf, Y.; Gondrie, M.J.; Janssen, K.J.; de Koning, H.J.; et al. Comparing coronary artery calcium and thoracic aorta calcium for prediction of all-cause mortality and cardiovascular events on low-dose non-gated computed tomography in a high-risk population of heavy smokers. Atherosclerosis. 2019, 209, 455–62. [Google Scholar] [CrossRef]
- Haller, C.; Vandehei, A.; Fisher, R.; Boster, J.; Shipley, B.; Kaatz, C.; et al. Incidence and implication of coronary artery calcium on non-gated chest computed tomography scans: A large observational cohort. Cureus. 2019. [Google Scholar] [CrossRef] [PubMed]
- Shim, S.S.; Oh, Y.W.; Kong, K.A.; Ryu, Y.J.; Kim, Y.; Jang, D.H. Pulmonary nodule size evaluation with chest tomosynthesis and CT: A phantom study. BJR. 2019, 88, 20140040. [Google Scholar] [CrossRef] [PubMed]
- Liang, C.H.; Liu, Y.C.; Wu, M.T.; Garcia-Castro, F.; Alberich-Bayarri, A.; Wu, F.Z. Identifying pulmonary nodules or masses on chest radiography using deep learning: external validation and strategies to improve clinical practice. Clin Radiol. 2019, 75, 38–45. [Google Scholar] [CrossRef] [PubMed]
- Amariei, D.E.; Dodia, N.; Deepak, J.; Hines, S.E.; Galvin, J.R.; Atamas, S.P.; et al. Combined pulmonary fibrosis and emphysema: pulmonary function testing and a pathophysiology perspective. Medicina (Kaunas). 2019, 55, E580. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.-H.; Duan, J.; Han, X.; Liu, X.; Zhou, J.; Wang, X.; et al. High incidence and mortality of pneumothorax in critically ill patients with COVID-19. Heart Lung. 2021, 50, 37–43. [Google Scholar] [CrossRef]
- Mazzone, P.J.; Gould, M.K.; Arenberg, D.A.; Chen, A.C.; Choi, H.K.; Detterbeck, F.C.; et al. Management of lung nodules and lung cancer screening during the COVID-19 pandemic: Chest expert panel report. Radiol Imaging Cancer. 2040, 2, e204013. [Google Scholar] [CrossRef]
- Kassem, M.N.E.; Masallat, D.T. Clinical application of chest computed tomography (CT) in detection and characterization of coronavirus (COVID-19) pneumonia in adults. J Digit Imaging. 2021, 34, 273–83. [Google Scholar] [CrossRef] [PubMed]
- Javidan-Nejad, C. MDCT of trachea and main bronchi. Thorac Surg Clin. 2010, 20, 65–84. [Google Scholar] [CrossRef]
- D’Errico, L.; Salituri, F.; Ciardetti, M.; Favilla, R.; Mazzarisi, A.; Coppini, G.; et al. Quantitative analysis of epicardial fat volume: effects of scanning protocol and reproducibility of measurements in non-contrast cardiac CT vs. coronary CT angiography. Quant Imaging Med Surg. 2017, 7, 326–35. [Google Scholar] [CrossRef] [PubMed]
- Jappar, I.A.; Chua, T.; Htoo, M.M.A.; Cheah, F.K.; Allen, J.C.; Tan, S.Y. Diagnosis of anomalous origin and course of coronary arteries using non-contrast cardiac CT scan and detection features. J Cardiovasc Comput Tomogr. 2012, 6, 335–45. [Google Scholar] [CrossRef]
- Busse, A.; Cantré, D.; Beller, E.; Streckenbach, F.; Öner, A.; Ince, H.; et al. Cardiac CT: why, when, and how: update 2019. Radiologe. 2019, 59, 1–9. [Google Scholar] [CrossRef] [PubMed]
- O’Sullivan, J.W.; Muntinga, T.; Grigg, S.; Ioannidis, J.P.; Ebrahim, S. Diagnosis and prognosis of coronary artery disease by cardiac imaging: systematic review and meta-analysis. J Am Coll Cardiol. 2017, 70, 2323–33. [Google Scholar] [CrossRef]
- Xie, Y.; Wang, Y.; Zhang, Y.; Zhang, J. Cardiac CT in coronary artery disease: Assessment of coronary plaque and its functional impact. J Cardiovasc Comput Tomogr. 2023, 17, 392–400. [Google Scholar] [CrossRef]
- De Cecco, C.N.; Marin, D.; Valsangiacomo-Buechel, E.R.; Knisely, A.; Kozerke, S.; Schoepf, U.J. New advances in CT imaging of cardiovascular disease. Curr Cardiovasc Imaging Rep. 2023, 16, 115–125. [Google Scholar] [CrossRef]
- Kato, M.; Shimada, K.; Ghosh, D.; Lamba, R.; Kline-Rogers, E.; Masoudi, F.A. Insights into coronary artery calcification quantification by CT imaging. Am Heart J. 2023, 246, 119–128. [Google Scholar] [CrossRef]
- Berman, D.S.; Budoff, M.J.; Koo, B.K.; Kwon, H.J.; Pundziute, G.; Abbott, B.; et al. Multi-center study of coronary CTA for the assessment of coronary artery disease: A comparative analysis with invasive coronary angiography and outcomes. JACC Cardiovasc Imaging. 2023, 16, 2020–2031. [Google Scholar] [CrossRef]
- Li, H.; He, B.; Zhang, L.; Xu, S.; Zhang, Q.; Li, J.; et al. The role of coronary CT angiography in determining cardiovascular risk in patients with a history of chest pain. Cardiology. 2023, 138, 105–112. [Google Scholar] [CrossRef]
- Min, J.K.; Halaweish, A.F.; Taylor, C.A.; Leipsic, J.; Fuster, V. Imaging coronary atherosclerosis with computed tomography: Implications for clinical practice. Circulation. 2023, 147, 1880–1893. [Google Scholar] [CrossRef]
- Schuijf, J.D.; Mangiacapra, F.; Berman, D.S.; Dey, D. Coronary CT angiography for risk stratification in patients with stable angina. J Nucl Cardiol. 2022, 29, 1732–1744. [Google Scholar] [CrossRef]
- Wang, Z.; Liu, J.; Yang, J.; Li, S.; Zhang, Y.; Li, Z. Use of cardiac CT in guiding the management of non-ST-elevation acute coronary syndrome. J Cardiovasc Comput Tomogr. 2022, 16, 335–341. [Google Scholar] [CrossRef]
- Hecht, H.S.; Cronin, P.; Shapiro, M.D.; Puchner, S.B.; Takx, R.A.; Maron, D.J.; et al. Effect of coronary CTA on the prediction of future cardiovascular events in the general population: The CONFIRM study. J Am Coll Cardiol. 2023, 78, 839–850. [Google Scholar] [CrossRef]
- Steigner, M.; Chang, H.; Gaffar, R.; Aslam, S.; Jafari, Z.; Karim, A.; et al. Accuracy of coronary CT angiography for predicting the presence and severity of coronary artery disease. J Comput Assist Tomogr. 2022, 46, 749–755. [Google Scholar] [CrossRef]
- Pelisek J, Jirak P, Stepper M, Klooster D, Ruzicka M, Bozkurt M, et al. Multi-detector CT coronary angiography in the diagnosis of coronary artery disease: Comparison with traditional coronary angiography. Eur J Radiol. 2021, 137, 109661. [CrossRef]
- Kuipers, L.; de Groot, G.; Brink, M.; Smit, A.; Rossen, R.; MacNeil, B.; et al. Non-invasive imaging for the evaluation of coronary artery disease: A systematic review of the role of CT, MRI, and PET. Eur Heart J. 2022, 43, 3927–3938. [Google Scholar] [CrossRef]
- Li, X.; Yin, Z.; Li, Y.; Liu, T.; Zhang, T.; Gao, P. Evaluation of myocardial ischemia using cardiac CT: Comparison with conventional stress tests. Cardiovasc Diagn Ther. 2023, 13, 70–78. [Google Scholar] [CrossRef]
- Deegan, P.; Abdulla, S.; Douglas, P.S.; Leipsic, J. New insights into coronary CTA: The future of non-invasive coronary artery disease evaluation. JACC Cardiovasc Imaging. 2023, 16, 119–132. [Google Scholar] [CrossRef]
- Koo, B.K.; Hwang, D.; Lee, J.M.; Ahn, J.M.; Park, J.S.; Cho, Y.K.; et al. Prognostic value of coronary CT angiography in patients with suspected coronary artery disease: A meta-analysis. J Am Coll Cardiol. 2022, 80, 1511–1523. [Google Scholar] [CrossRef]
- Bittencourt, M.S.; Massaro, J.M.; O’Donnell, C.J.; Hoffmann, U.; Blankstein, R.; Hulten, E.; et al. Coronary artery calcium score and risk prediction for coronary heart disease events in low-risk individuals. JAMA Cardiol. 2023, 8, 126–134. [Google Scholar] [CrossRef]
- McGlinchey, D.; Collett, L.; Foster, D.; Zeglinski, C.; Sandoval, J.; Goellner, J.; et al. The role of coronary CT angiography in clinical practice: Impact on clinical decision-making and patient outcomes. Cardiovasc Imaging. 2023, 19, 227–235. [Google Scholar] [CrossRef]
- Luo, X.; Jin, L.; Zhang, X.; Li, H.; Zhang, W.; Wu, Z. The diagnostic accuracy of coronary CT angiography for detection of coronary artery disease in patients with diabetes: A meta-analysis. Diabetes Technol Ther. 2023, 25, 613–620. [Google Scholar] [CrossRef]
- Marom, E.M.; Costa, M.A.; Leclerc, G.; Chia, A.; Wolfson, T. The emerging role of coronary CT angiography in post-operative cardiovascular management. J Cardiovasc Comput Tomogr. 2023, 17, 149–158. [Google Scholar] [CrossRef]
- Zhang, Y.; Li, B.; Huang, X.; Zeng, Z.; Zhang, Z.; Wang, W. Cardiac CT for the evaluation of heart disease: From coronary artery disease to myocardial disease. J Cardiovasc Comput Tomogr. 2022, 16, 488–496. [Google Scholar] [CrossRef]
- Inoue, M.; Kim, J.H.; Jeong, Y.J.; Song, J.H.; Lee, J.H.; Park, S.M. Comparison of coronary CT angiography and invasive coronary angiography for risk stratification in asymptomatic individuals. J Cardiovasc Comput Tomogr. 2022, 16, 379–386. [Google Scholar] [CrossRef]
- Kim, Y.J.; Yoon, C.H.; Cho, J.Y.; Lee, H.J.; Lee, S.; Park, Y.; et al. Predictive value of coronary CT angiography for major adverse cardiovascular events in patients with chest pain: A cohort study. J Am Heart Assoc. 2023, 12, e022023. [Google Scholar] [CrossRef]
- De Ferrari, G.M.; Arnesano, M.; Casella, S.; Cicala, S.; Moroni, P.; Bartoli, D.; et al. Coronary CT angiography for assessment of myocardial perfusion in coronary artery disease: A comparison with invasive coronary physiology. J Cardiovasc Comput Tomogr. 2023, 17, 11–18. [Google Scholar] [CrossRef]
- Shah, N.R.; Aschwanden, M.; Allam, A.H.; Zeng, X.; Shams, A.; Sharma, M.; et al. Coronary CT angiography and its impact on the management of patients with suspected coronary artery disease: A randomized trial. JAMA Intern Med. 2023, 183, 199–206. [Google Scholar] [CrossRef]

| Month and year | Total of exam | Type of incidental finding at CT scan | Number of positive Cardiac-CT |
| APRIL, 2022 | 5 | - | |
| 1 patient with dyspnea on exertion | STRATUM OF PERICARDIAL EFFUSION | ||
| MAY, 2022 | 13 | 2 | |
| 1 patient with a control of stent apposition | NODULAR FORMATION AT THE MYOCARDIUM | ||
| 1 patient with epigastric pain | PULMONARY MICRONODULE AND JATAL HERNIA | ||
| 1 patient with breathlessness | PULMONARY NODULES | ||
| JUNE, 2022 | 10 | - | |
| - | - | ||
| JULY, 2022 | 13 | - | |
| 1 patient with epigastric pain | STRATUM OF PERICARDIAL EFFUSION | ||
| 1 patient with hypertension, and a previous surgical procedure on the aorta | REVASCULARIZATION OF THE FALSE LUMEN OF A PREVIOUSLY SURGICALLY TREATED AORTIC DISSECTION | ||
| AUGUST, 2022 | 6 | - | |
| 1 patient with dyspnea on exertion | RIGHT BREAST THICKENING. ON THROUGH-ABDOMEN SCANS: LITHIASIS OF THE GALLBLADDER |
||
| 1 patient with breathlessness | ON THROUGH-ABDOMEN SCANS: HYPODENSE FORMATION AT THE IVS OF THE LIVER AND RETROPERITONEAL LYMPHADENOPATHY | ||
| SEPTEMBER, 2022 | 12 | 1 | |
| 1 patient with dyspnea on exertion | STRATUM OF PERICARDIAL EFFUSION | ||
| 1 patient with epigastric pain | STRATUM OF PERICARDIAL EFFUSION AND JATAL HERNIA | ||
| OCTOBER, 2022 | 12 | 2 | |
| 1 patient with angor | RETROSTERNAL SOLID TISSUE | ||
| 1 patient with epigastric pain | CONSISTENT JATAL HERNIA | ||
| NOVEMBER, 2022 | 27 | 3 | |
| - | - | ||
| DECEMBER, 2022 | 11 | ||
| - | - | ||
| JANUARY, 2023 | 19 | 1 | |
| 1 patient with dyspnea on exertion | ON THROUGH-ABDOMEN SCANS: HYPODENSE FORMATION AT THE VS AND VIIIS OF THE LIVER | ||
| FEBRUARY, 2023 | 21 | 3 | |
| 1 patient with epigastric pain | ON THROUGH-ABDOMEN SCANS: HYPODENSE FORMATION AT THE IVS AND VIIS OF THE LIVER | ||
| MARCH, 2023 | 33 | 4 | |
| 1 patient with epigastric pain | CONSISTENT JATAL HERNIA | ||
| APRIL, 2023 | 11 | - | |
| 1 patient with dyspnea on exertion | PATENCY OF THE INTERVENTRICULAR SEPTUM | ||
| 1 patient with dyspnea | PULMONARY PARENCHYMAL THICKENING WITH SUBPLEURAL AND INTERLOBULAR THICKENING | ||
| 1 patient with epigastric pain | CONSISTENT JATAL HERNIA | ||
| 1 patient with breathlessness | COPD (CHRONIC OBSTRUCTIVE PULMONARY DISEASE) SIGN | ||
| 1 patient with occasional chest pain | INTRAMURAL ANEURYSM OF THE INTERATRIAL SEPTUM WITHOUT OBVIOUS SHUNT | ||
| MAY, 2023 | 28 | 3 | |
| 1 patient with dyspnea on exertion | COPD SIGN | ||
| 1 patient with arrhythmia and cardiovascular risk factors | CONSOLIDATIVE PULMONARY FOCUS FROM PROBABLE INFLAMMATORY OUTCOME | ||
| 1 patient with dyspnea on exertion | RIGHT VENTRICULAR LATERAL MARGIN THICKENING WITH CONSENSUAL LUNG CONSOLIDATION | ||
| JUNE, 2023 | 27 | 7 | |
| 1 patient with dyspnea on exertion | SUSPICIOUS AREA WITH CONTRAST ENHANCEMENT AT THE TAIL OF THE PANCREAS | ||
| JULY, 2023 | 12 | 2 | |
| 1 patient with dyspnea on exertion and breathlessness | COPD SIGN | ||
| 1 patient with epigastric pain | CONSISTENT JATAL HERNIA | ||
| AUGUST, 2023 | 7 | - | |
| 1 patient with epigastric pain | CONSISTENT JATAL HERNIA | ||
| SEPTEMBER, 2023 | 8 | 2 | |
| 1 patient with occasional heart palpitation | NEGATIVE T WAVE ON ECG MONITORING | ||
| OCTOBER, 2023 | 16 | 2 | |
| 1 patient with dyspnea on exertion | CYLINDRICAL AND CYSTIC BRONCHIECTASIS, 8 MM PULMONARY NODULE, AND ADDITIONAL MICRONODULES WITH LYMPHADENOPATHY (11 MM THE LARGEST SUBCARINAL) | ||
| 1 patient with occasional chest pain | ABUNDANT SHARE OF PERICARDIAL FAT | ||
| 1 patient with cardiovascular risk factors | MICRONODULE (6MM) AT THE LINGULA AND PLEURAL PLAQUES | ||
| NOVEMBER, 2023 | 10 | 1 | |
| 1 patient with dyspnea on exertion | LUNG NODULES OF ABOUT 12 AND 9 MM | ||
| 1 patient with cardiovascular risk factors, and increased phlogosis indices | PERICARDIAC PULMONARY PARENCHYMAL CONSOLIDATION | ||
| DECEMBER, 2023 | 10 | 2 | |
| 1 patient with breathlessness |
COPD (CHRONIC OBSTRUCTIVE PULMONARY DISEASE) SIGN | ||
| JANUARY, 2024 | 6 | 1 | |
| 1 patient with dyspnea on exertion |
OSTEOLYTIC LESION AT THE SOMA OF T4 | ||
| FEBRUARY, 2024 | 9 | 1 | |
| MARCH, 2024 | 14 | 3 | |
| 1 patient with epigastric pain | CONSISTENT JATAL HERNIA | ||
| APRIL, 2024 | 12 | ||
| 1 patient with dyspnea on exertion | CALCIFIC LYMPH NODE IN MEDIASTINUM |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





