Submitted:
17 December 2024
Posted:
18 December 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
2.1. Study Design, Setting and Subjects Characteristics
2.2. Image Analysis
2.3. Biochemical Analysis
2.4. Lipoprotein Isolation and Composition
2.5. Lipoprotein Functional Assays
2.5.1. Electronegative LDL
2.5.2. LDL Susceptibility to Aggregation
2.5.3. LDL and HDL Susceptibility to Oxidation
2.5.4. PAF-AH Activity
2.5.5. LDL Size and HDL Subfraction
2.6. Statistical Analysis
3. Results
3.1. Clinical Characteristics and Biochemical Profiles of T2DM Patients and Healthy Controls
3.2. Lipid Profile and Apolipoproteins in Plasma
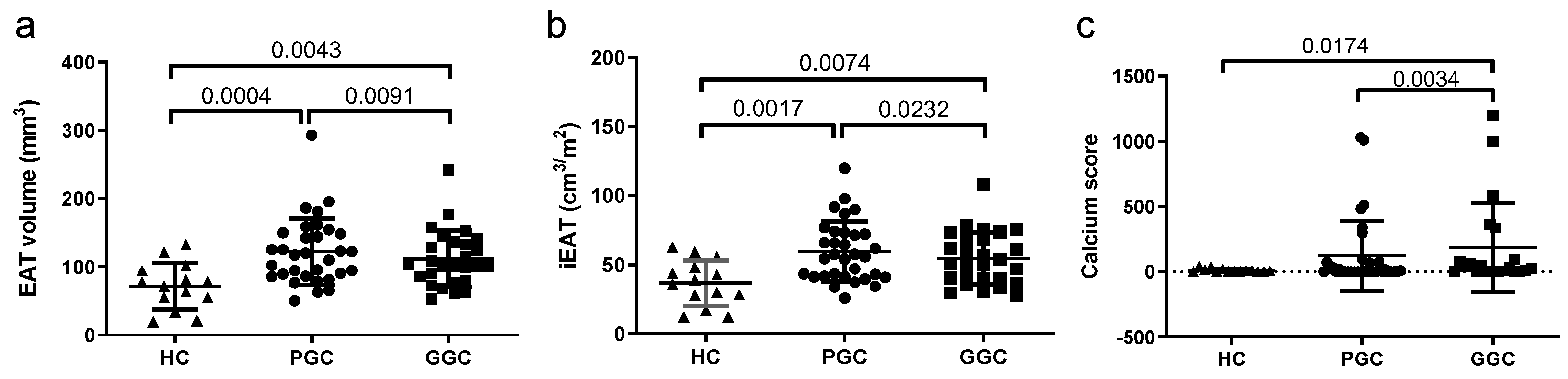
3.3. HF Biomarkers
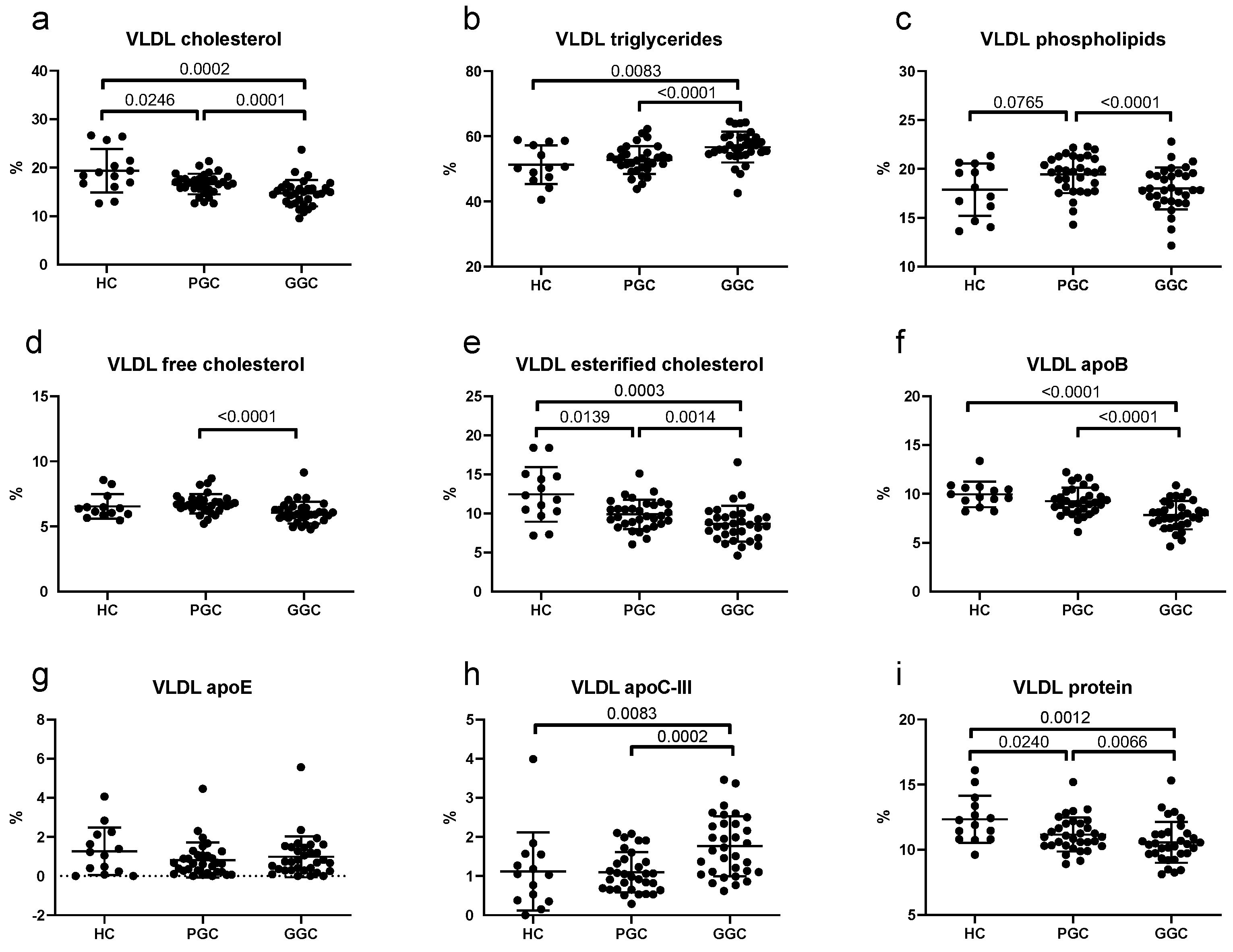
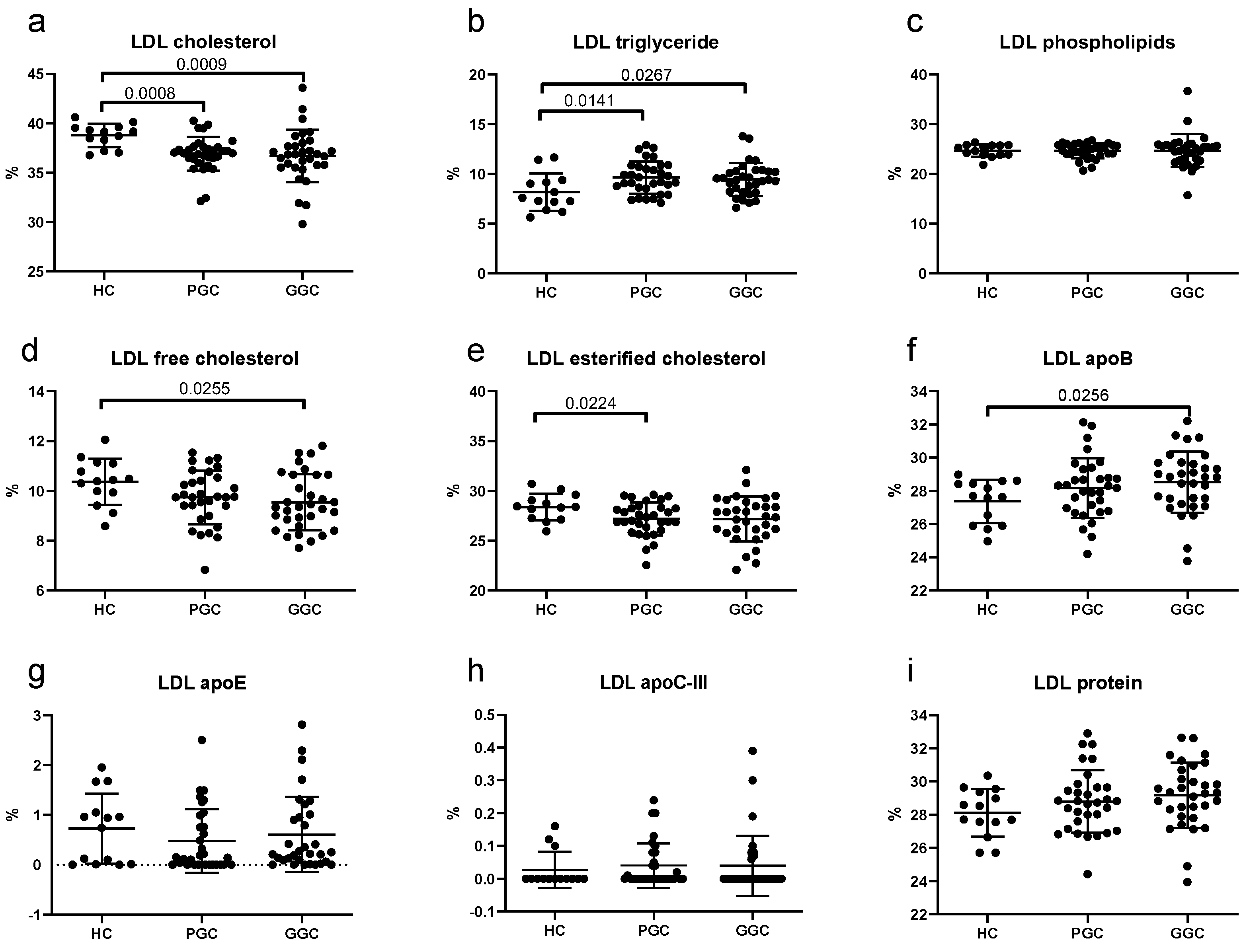
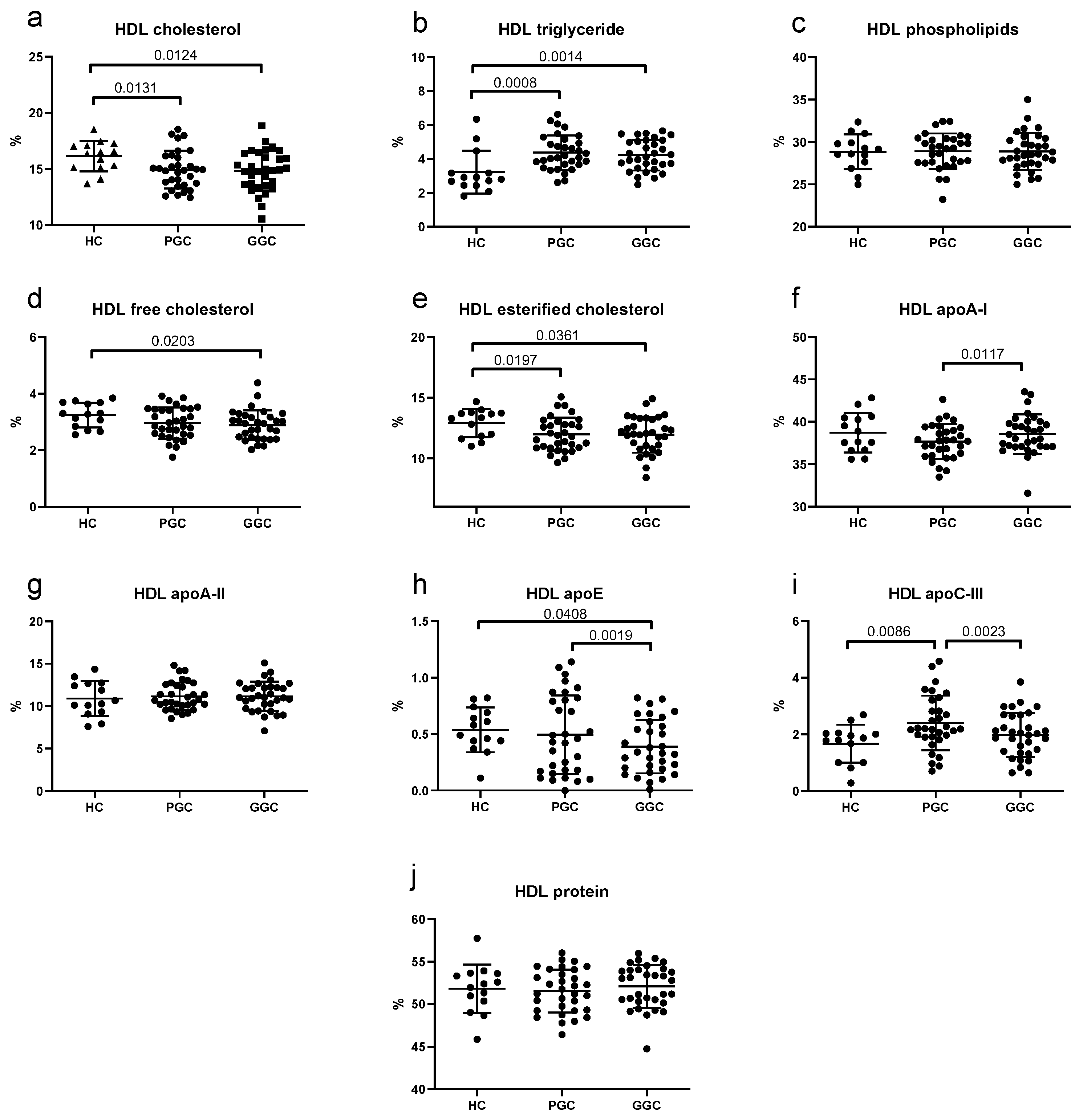
3.5. Lipoprotein Composition
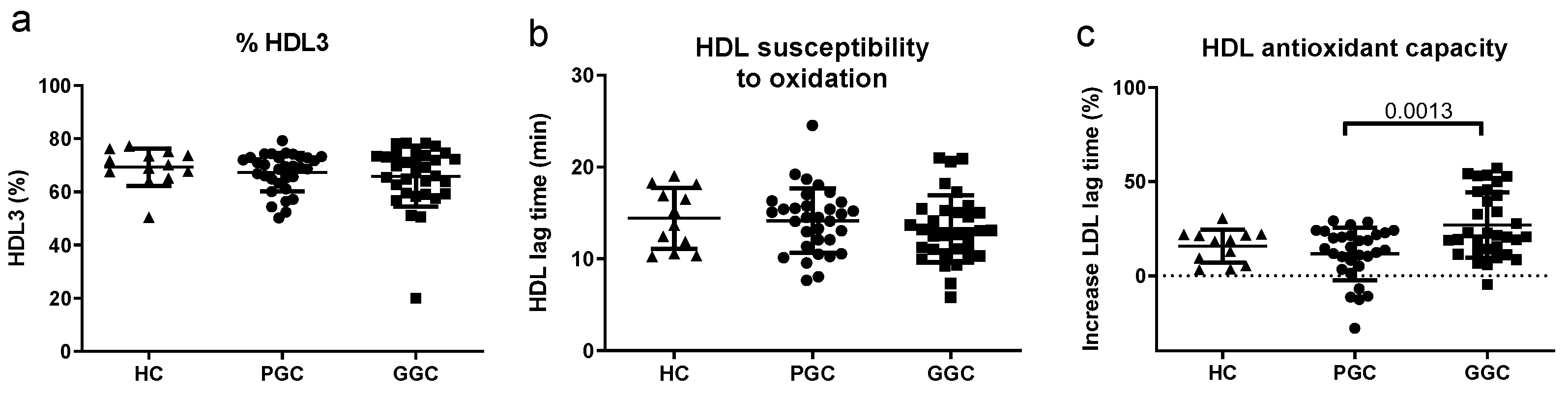
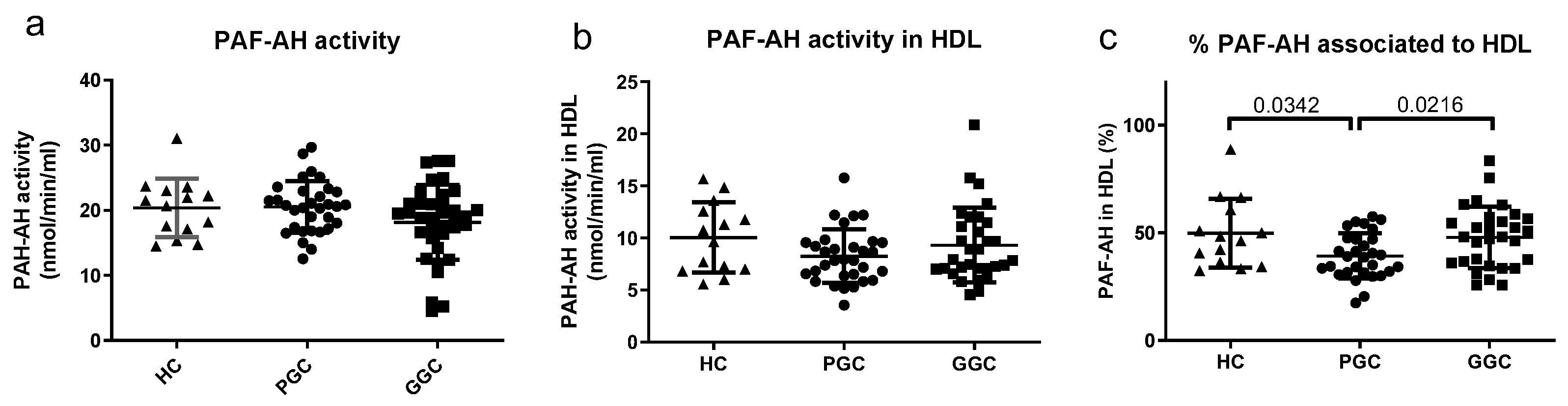
3.6. Lipoprotein Functional Properties
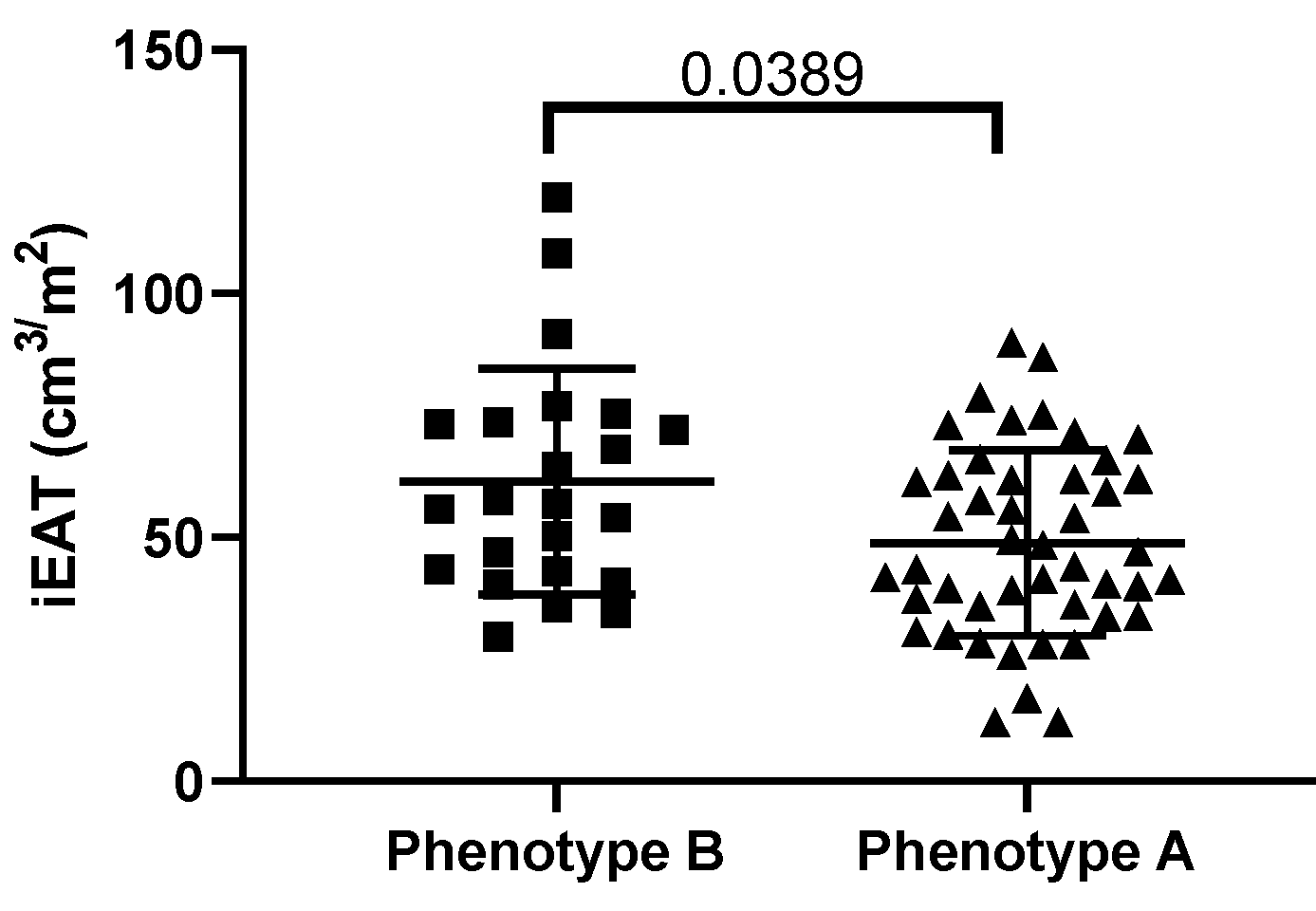
3.7. Correlations with iEAT
3.8. Bivariate and Multivariable Regression Analysis
3.9. Receiver Operating Characteristic Analysis
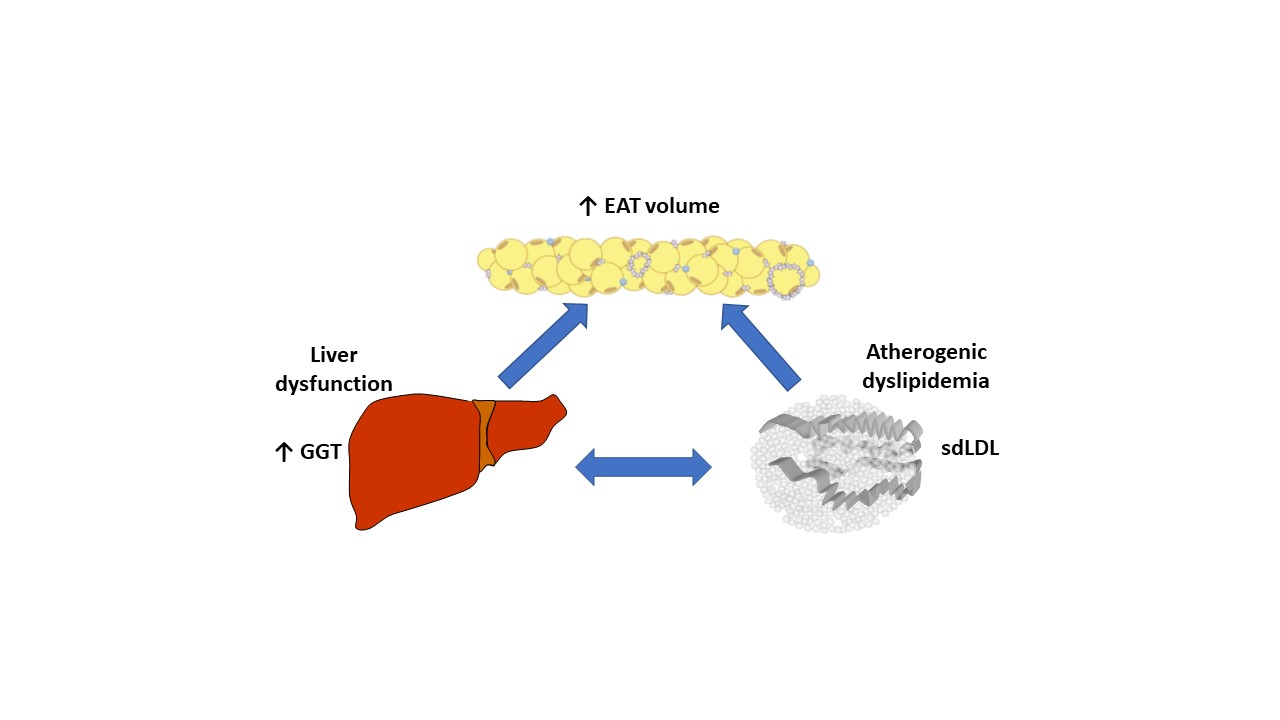
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Scherer, P.E.; Hill, J.A. Obesity, Diabetes, and Cardiovascular Diseases: A Compendium. Circ Res. 2016, 118, 1703–1705. [Google Scholar] [CrossRef] [PubMed]
- Lorenzatti, A.J.; Toth, P.P. New Perspectives on Atherogenic Dyslipidaemia and Cardiovascular Disease. Eur Cardiol. 2020, 15, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Soran, H.; Schofield, J.D.; Adam, S.; Durrington, P.N. Diabetic dyslipidaemia. Curr Opin Lipidol. 2016, 27, 313–322. [Google Scholar] [CrossRef] [PubMed]
- Reis, A.; Rocha, S.; Dias, I.H.; Costa, R.; Soares, R.; Sanchez-Quesada, J.L.; et al. Type 2 Diabetes mellitus alters the cargo of (poly)phenol metabolome and the oxidative status in circulating lipoproteins. Redox Biol. 2023, 59, 102572. [Google Scholar] [CrossRef]
- Sanchez-Quesada, J.L.; Vinagre, I.; De Juan-Franco, E.; Sanchez-Hernandez, J.; Bonet-Marques, R.; Blanco-Vaca, F.; et al. Impact of the LDL subfraction phenotype on Lp-PLA2 distribution, LDL modification and HDL composition in type 2 diabetes. Cardiovasc Diabetol. 2013, 12, 112. [Google Scholar] [CrossRef]
- Iacobellis, G.; Corradi, D.; Sharma, A.M. Epicardial adipose tissue: anatomic, biomolecular and clinical relationships with the heart. Nat Clin Pract Cardiovasc Med. 2005, 2, 536–543. [Google Scholar] [CrossRef]
- Iacobellis, G. Epicardial fat links obesity to cardiovascular diseases. Prog Cardiovasc Dis. 2023, 78, 27–33. [Google Scholar] [CrossRef]
- Villasante Fricke, A.C.; Iacobellis, G. Epicardial Adipose Tissue: Clinical Biomarker of Cardio-Metabolic Risk. Int J Mol Sci. 2019, 20. [Google Scholar] [CrossRef]
- Puig, N.; Rives, J.; Gil-Millan, P.; Minambres, I.; Ginel, A.; Tauron, M.; et al. Apolipoprotein J protects cardiomyocytes from lipid-mediated inflammation and cytotoxicity induced by the epicardial adipose tissue of diabetic patients. Biomed Pharmacother. 2024, 175, 116779. [Google Scholar] [CrossRef]
- Sardu, C.; D’Onofrio, N.; Torella, M.; Portoghese, M.; Loreni, F.; Mureddu, S.; et al. Pericoronary fat inflammation and Major Adverse Cardiac Events (MACE) in prediabetic patients with acute myocardial infarction: effects of metformin. Cardiovasc Diabetol. 2019, 18, 126. [Google Scholar] [CrossRef]
- Mazurek, T.; Zhang, L.; Zalewski, A.; Mannion, J.D.; Diehl, J.T.; Arafat, H.; et al. Human epicardial adipose tissue is a source of inflammatory mediators. Circulation. 2003, 108, 2460–2466. [Google Scholar] [CrossRef]
- Greulich, S.; Maxhera, B.; Vandenplas, G.; de Wiza, D.H.; Smiris, K.; Mueller, H.; et al. Secretory products from epicardial adipose tissue of patients with type 2 diabetes mellitus induce cardiomyocyte dysfunction. Circulation. 2012, 126, 2324–2334. [Google Scholar] [CrossRef] [PubMed]
- Vianello, E.; Dozio, E.; Arnaboldi, F.; Marazzi, M.G.; Martinelli, C.; Lamont, J.; et al. Epicardial adipocyte hypertrophy: Association with M1-polarization and toll-like receptor pathways in coronary artery disease patients. Nutr Metab Cardiovasc Dis. 2016, 26, 246–253. [Google Scholar] [CrossRef] [PubMed]
- Salgado-Somoza, A.; Teijeira-Fernandez, E.; Fernandez, A.L.; Gonzalez-Juanatey, J.R.; Eiras, S. Changes in lipid transport-involved proteins of epicardial adipose tissue associated with coronary artery disease. Atherosclerosis. 2012, 224, 492–499. [Google Scholar] [CrossRef]
- Salgado-Somoza, A.; Teijeira-Fernandez, E.; Rubio, J.; Couso, E.; Gonzalez-Juanatey, J.R.; Eiras, S. Coronary artery disease is associated with higher epicardial retinol-binding protein 4 (RBP4) and lower glucose transporter (GLUT) 4 levels in epicardial and subcutaneous adipose tissue. Clin Endocrinol (Oxf). 2012, 76, 51–58. [Google Scholar] [CrossRef]
- Mancio, J.; Azevedo, D.; Saraiva, F.; Azevedo, A.I.; Pires-Morais, G.; Leite-Moreira, A.; et al. Epicardial adipose tissue volume assessed by computed tomography and coronary artery disease: a systematic review and meta-analysis. Eur Heart J Cardiovasc Imaging. 2018, 19, 490–497. [Google Scholar] [CrossRef]
- Shmilovich, H.; Dey, D.; Cheng, V.Y.; Rajani, R.; Nakazato, R.; Otaki, Y.; et al. Threshold for the upper normal limit of indexed epicardial fat volume: derivation in a healthy population and validation in an outcome-based study. Am J Cardiol. 2011, 108, 1680–1685. [Google Scholar] [CrossRef]
- Kotha, S.; Plein, S.; Greenwood, J.P.; Levelt, E. Role of epicardial adipose tissue in diabetic cardiomyopathy through the lens of cardiovascular magnetic resonance imaging - a narrative review. Ther Adv Endocrinol Metab. 2024, 15, 20420188241229540. [Google Scholar] [CrossRef]
- Yuvaraj, J.; Isa, M.; Che, Z.C.; Lim, E.; Nerlekar, N.; Nicholls, S.J.; et al. Atherogenic index of plasma is associated with epicardial adipose tissue volume assessed on coronary computed tomography angiography. Sci Rep. 2022, 12, 9626. [Google Scholar] [CrossRef]
- American Diabetes, A. 2. Classification and Diagnosis of Diabetes. Diabetes Care. 2016, 39 (Suppl 1), S13–S22. [Google Scholar] [CrossRef]
- Mancia, G.; Fagard, R.; Narkiewicz, K.; Redon, J.; Zanchetti, A.; Bohm, M.; et al. 2013 ESH/ESC guidelines for the management of arterial hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J. 2013, 34, 2159–2219. [Google Scholar] [CrossRef] [PubMed]
- Oudkerk, M.; Stillman, A.E.; Halliburton, S.S.; Kalender, W.A.; Mohlenkamp, S.; McCollough, C.H.; et al. Coronary artery calcium screening: current status and recommendations from the European Society of Cardiac Radiology and North American Society for Cardiovascular Imaging. Int J Cardiovasc Imaging. 2008, 24, 645–671. [Google Scholar] [CrossRef] [PubMed]
- McDonagh, T.A.; Metra, M.; Adamo, M.; Gardner, R.S.; Baumbach, A.; Bohm, M.; et al. 2023 Focused Update of the 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2023, 44, 3627–3639. [Google Scholar] [CrossRef] [PubMed]
- Havel, R.J.; Eder, H.A.; Bragdon, J.H. The distribution and chemical composition of ultracentrifugally separated lipoproteins in human serum. J Clin Invest. 1955, 34, 1345–1353. [Google Scholar] [CrossRef]
- Benitez, S.; Villegas, V.; Bancells, C.; Jorba, O.; Gonzalez-Sastre, F.; Ordonez-Llanos, J.; et al. Impaired binding affinity of electronegative low-density lipoprotein (LDL) to the LDL receptor is related to nonesterified fatty acids and lysophosphatidylcholine content. Biochemistry. 2004, 43, 15863–15872. [Google Scholar] [CrossRef]
- Bancells, C.; Benitez, S.; Jauhiainen, M.; Ordonez-Llanos, J.; Kovanen, P.T.; Villegas, S.; et al. High binding affinity of electronegative LDL to human aortic proteoglycans depends on its aggregation level. J Lipid Res. 2009, 50, 446–455. [Google Scholar] [CrossRef]
- Bancells, C.; Villegas, S.; Blanco, F.J.; Benitez, S.; Gallego, I.; Beloki, L.; et al. Aggregated electronegative low density lipoprotein in human plasma shows a high tendency toward phospholipolysis and particle fusion. J Biol Chem. 2010, 285, 32425–32435. [Google Scholar] [CrossRef]
- Rivas-Urbina, A.; Rotllan, N.; Santos, D.; Julve, J.; Escola-Gil, J.C.; Sanchez-Quesada, J.L. Assessment of Ex Vivo Antioxidative Potential of Murine HDL in Atherosclerosis. Methods Mol Biol. 2022, 2419, 283–292. [Google Scholar] [CrossRef]
- Sanchez-Quesada, J.L.; Benitez, S.; Otal, C.; Franco, M.; Blanco-Vaca, F.; Ordonez-Llanos, J. Density distribution of electronegative LDL in normolipemic and hyperlipemic subjects. J Lipid Res. 2002, 43, 699–705. [Google Scholar] [CrossRef]
- Krauss, R.M. Lipids and lipoproteins in patients with type 2 diabetes. Diabetes Care. 2004, 27, 1496–1504. [Google Scholar] [CrossRef]
- Iacobellis, G. Epicardial adipose tissue in endocrine and metabolic diseases. Endocrine. 2014, 46, 8–15. [Google Scholar] [CrossRef] [PubMed]
- Christensen, R.H.; von Scholten, B.J.; Hansen, C.S.; Jensen, M.T.; Vilsboll, T.; Rossing, P.; et al. Epicardial adipose tissue predicts incident cardiovascular disease and mortality in patients with type 2 diabetes. Cardiovasc Diabetol. 2019, 18, 114. [Google Scholar] [CrossRef] [PubMed]
- Ren, J.; Yao, G.; Ren, L.; Wang, Y.; Gao, J.; Zhang, Y. Exploring the Associations Between Non-Traditional Lipid Parameters and Epicardial Adipose Tissue Volume. Angiology. 2023, 33197231207264. [Google Scholar] [CrossRef] [PubMed]
- Urata, T.; Kishino, T.; Watanabe, K.; Shibasaki, S.; Yotsukura, M.; Mori, H.; et al. Sonographically Measured Adipose Tissue Thickness Correlates with Laboratory Test Abnormalities Reflecting Metabolic State in Elderly Women. Metab Syndr Relat Disord. 2022, 20, 148–155. [Google Scholar] [CrossRef]
- Donmez, Y.; Bulut, A. Epicardial fat thickness is significantly increased and related to LDL cholesterol level in patients with familial hypercholesterolemia. J Ultrasound. 2019, 22, 309–314. [Google Scholar] [CrossRef]
- Rubio-Guerra, A.F.; Benitez-Maldonado, D.R.; Lozano-Nuevo, J.J.; Arana-Pazos, K.C.; Huerta-Ramirez, S.; Narvaez-Rivera, J.L. Correlation between epicardial fat thickness and biochemical markers of metabolic risk. Med Clin (Barc). 2018, 151, 236–238. [Google Scholar] [CrossRef]
- Colom, C.; Vilades, D.; Perez-Cuellar, M.; Leta, R.; Rivas-Urbina, A.; Carreras, G.; et al. Associations between epicardial adipose tissue, subclinical atherosclerosis and high-density lipoprotein composition in type 1 diabetes. Cardiovasc Diabetol. 2018, 17, 156. [Google Scholar] [CrossRef]
- Tchernof, A.; Lamarche, B.; Prud’Homme, D.; Nadeau, A.; Moorjani, S.; Labrie, F.; et al. The dense LDL phenotype. Association with plasma lipoprotein levels, visceral obesity, and hyperinsulinemia in men. Diabetes Care. 1996, 19, 629–637. [Google Scholar] [CrossRef]
- Goff, D.C.; Jr D’Agostino, R.B.; Jr Haffner, S.M.; Otvos, J.D. Insulin resistance and adiposity influence lipoprotein size and subclass concentrations. Results from the Insulin Resistance Atherosclerosis Study. Metabolism. 2005, 54, 264–270. [Google Scholar] [CrossRef]
- Barchuk, M.; Schreier, L.; Lopez, G.; Cevey, A.; Baldi, J.; Fernandez Tome, M.D.C.; et al. Glycosylphosphatidylinositol-anchored high density lipoprotein-binding protein 1 and angiopoietin-like protein 4 are associated with the increase of lipoprotein lipase activity in epicardial adipose tissue from diabetic patients. Atherosclerosis. 2019, 288, 51–59. [Google Scholar] [CrossRef]
- Rivas-Urbina, A.; Benitez, S.; Perez, A.; Sanchez-Quesada, J.L. Modified low-density lipoproteins as biomarkers in diabetes and metabolic syndrome. Front Biosci (Landmark Ed). 2018, 23, 1220–1240. [Google Scholar] [CrossRef] [PubMed]
- Jayaraman, S.; Chavez, O.R.; Perez, A.; Minambres, I.; Sanchez-Quesada, J.L.; Gursky, O. Binding to heparin triggers deleterious structural and biochemical changes in human low-density lipoprotein, which are amplified in hyperglycemia. Biochim Biophys Acta Mol Cell Biol Lipids. 2020, 1865, 158712. [Google Scholar] [CrossRef] [PubMed]
- Kotani, K.; Tsuzaki, K.; Sakane, N. The relationship between gamma-glutamyltransferase (GGT), bilirubin (Bil) and small dense low-density lipoprotein (sdLDL) in asymptomatic subjects attending a clinic for screening dyslipidaemias. Ann Acad Med Singap. 2014, 43, 216–219. [Google Scholar] [CrossRef] [PubMed]
- Young Kim, S.; Mun, S.; Yu, J.H.; Jin, Y.J.; Ju Suh, Y.; Cho, S.H.; et al. Association between small dense LDL levels and hepatic fibrosis in patients with nonalcoholic fatty liver disease. Medicine (Baltimore). 2022, 101, e30527. [Google Scholar] [CrossRef]
- Imajo, K.; Hyogo, H.; Yoneda, M.; Honda, Y.; Kessoku, T.; Tomeno, W.; et al. LDL-migration index (LDL-MI), an indicator of small dense low-density lipoprotein (sdLDL), is higher in non-alcoholic steatohepatitis than in non-alcoholic fatty liver: a multicenter cross-sectional study. PLoS One. 2014, 9, e115403. [Google Scholar] [CrossRef]
- Ege, M.R.; Guray, U.; Guray, Y.; Demirkan, B.; Kisacik, H. Serum gamma-glutamyltransferase levels correlate with epicardial adipose tissue thickness in patients with coronary artery disease. Angiology. 2013, 64, 21–25. [Google Scholar] [CrossRef]
- Ding, L.; Peng, K.; Lin, L.; Li, M.; Wang, T.; Dai, M.; et al. The impact of fat distribution on subclinical coronary atherosclerosis in middle-aged Chinese adults. Int J Cardiol. 2017, 235, 118–123. [Google Scholar] [CrossRef]
- Vandermeersch, A.; Ameye, S.; Puype, D.; Petitjean, D.; De Buyzere, M.; Langlois, M.R. Estimation of the low-density lipoprotein (LDL) subclass phenotype using a direct, automated assay of small dense LDL-cholesterol without sample pretreatment. Clin Chim Acta. 2010, 411, 1361–1366. [Google Scholar] [CrossRef]
- Xuesong, F.; Enshi, W.; Jianxun, H.; Lei, Z.; Xiaoli, Z.; Hui, Y. Comparison of seven different reagents of peroxidase method for small and dense low density lipoprotein cholesterol (sdLDL-C) measurement. J Clin Lab Anal. 2021, 35, e23660. [Google Scholar] [CrossRef]
- Amor, A.J.; Pinyol, M.; Sola, E.; Catalan, M.; Cofan, M.; Herreras, Z.; et al. Relationship between noninvasive scores of nonalcoholic fatty liver disease and nuclear magnetic resonance lipoprotein abnormalities: A focus on atherogenic dyslipidemia. J Clin Lipidol. 2017, 11, 551–561. [Google Scholar] [CrossRef]
- Cromwell, W.C.; Otvos, J.D. Low-density lipoprotein particle number and risk for cardiovascular disease. Curr Atheroscler Rep. 2004, 6, 381–387. [Google Scholar] [CrossRef]



| HC (n = 14) | PGC (n = 36) | GGC (n = 36) | |
| Age (years) | 53.8 ± 5.23 | 55.8 ± 9,41 | |
| Sex (m/f) | 10/4 (71.4) | 25/11 | |
| BMI (kg/m2) | 28.28 ± 4.98 | 33.53 ± 7.27 # | 31.87 ± 5.59 *# |
| Weight (kg) | 81.72 ± 15.55 | 95.07 ± 19.38 # | 90.05 ± 14.18 *# |
| WC (cm) | 97.14 ± 8.84 | 109.41 ± 14.68 # | 107.59 ± 11.61 *# |
| Smoking habit | 4 (28,6) | 10 (27.8) | 10 (27.8) |
| Dyslipidemia | 0 (0) | 12 (33.3) # | 10 (27.8) |
| Hypertension | 2 (14.3) | 12 (33.3) # | 12 (33.3) |
| Hypoglycemic treatment | |||
| Metformin | - | - | 30 |
| Empaglifozin | - | - | 33 |
| GLP1-rA | - | - | 2 |
| DPP4i | - | - | 4 |
| HC(n = 14) | PGC(n = 36) | GGC(n = 36) | |
| HbA1c (%) | 5.4 ± 0.2 | 11.7 ± 2.1 # | 6.1 (0.77) *# |
| Glucose (mg/dL) | 88.9 ± 10.2 | 157.5 ± 66.6 # | 117.2 ± 20.3 *# |
| C-peptide (pmol/L) | nd | 841 (642.1) | 1034 (301.5) |
| Bilirubin (µmol/L) | 12.5 ± 4.8 | 10.8 ± 4.3 | 10.5 ± 3.6 |
| AST (U/L) | 22.62 ± 4.3 | 34.4 ± 17.7 # | 22.9 ± 13.2 *# |
| ALT (U/L) | 22.64 ± 9.1 | 42.9 ± 22.8 # | 27.9 ± 19.0 *# |
| ALP (U/L) | 70.4 ± 12.8 | 97.5 ± 25.5 # | 84.9 ± 19.1 *# |
| GGT (U/L) | 24.9 ± 11.4 | 52.6 ± 62.2 # | 35.2 ± 41.6 *# |
| CRP (mg/L) | 1.3 (1.72) | 7.7 (7.4) # | 2.35 (5.05) *# |
| Lipid profile | |||
| Cholesterol (mg/dL) | 194.6 ± 39.84 | 189.84 ± 37.61 | 180.91 ± 47.92 |
| Triglyceride (mg/dL) | 69.48 (61.06) | 141.6 (101.82) # | 132.8 (67.26) # |
| HDLc (mg/dL) | 54.46 ± 12.31 | 40.08 ± 9.37 # | 45.03 ± 8.47 *# |
| LDLc (mg/dL) | 123.01 ± 33.04 | 119.80 ± 31.65 | 105.56 ± 37.82 |
| VLDLc (mg/dL) | 14.0 (12.3) | 31.01 ± 12.11 # | 26.77 (13.02) # |
| Lp(a) (mg/L) | 241.7 ± 215.1 | 234.5 ± 277.3 | 266.9 ± 297.7 |
| Apolipoprotein | |||
| ApoB (g/L) | 0.93 ± 0.25 | 1.07 ± 0.26 # | 0.94 ± 0.31 |
| ApoA-I (g/L) | 1.65 ± 0.26 | 1.31 ± 0.23 # | 1.43 ± 0.24 *# |
| ApoA-II (mg/L) | 43.83 ± 4.93 | 34.19 ± 6.53 # | 37.42 ± 6.31 *# |
| ApoC-III (mg/L) | 8.22 (6.58) | 7.61 (6.64) | 8.57 (8.8) |
| ApoE (mg/L) | 5.76 ± 1.60 | 5.85 ± 1.81 | 5.33 ± 1.75 |
| HDL Composition | p | r |
| % cholesterol | 0.597 | -0.063 |
| % triglycerides | 0.268 | 0.133 |
| % phospholipids | 0.252 | 0.138 |
| % free cholesterol | 0.072 | -0.214 |
| % esterified cholesterol | 0.847 | 0.023 |
| % apo A-I | 0.023 | -0.268 |
| % apo A-II | 0.707 | 0.045 |
| % apo E | 0.391 | -0.103 |
| % apo C-III | 0.035 | 0.251 |
| HDL Function | ||
| Total PAF-AH | 0.356 | 0.111 |
| PAF-AH in HDL (nmol/min/mL) | 0.176 | 0.162 |
| PAF-AH in HDL (%) | 0.25 | 0.137 |
| HDL2 | 0.901 | 0.015 |
| HDL3 | 0.901 | -0.015 |
| Antioxidant capacity of HDL | 0.584 | -0.067 |
| HDL susceptibility to oxidation | 0.738 | -0.041 |
| LDL Composition | p | r | ||
| % cholesterol | 0.848 | -0.023 | ||
| % triglycerides | 0.822 | -0.027 | ||
| % phospholipids | 0.495 | 0.082 | ||
| % free cholesterol | 0.068 | -0.217 | ||
| % esterified cholesterol | 0.360 | 0.110 | ||
| % apo A-I | 0.789 | -0.032 | ||
| % apo E | 0.501 | -0.081 | ||
| % apo C-III | 0.755 | -0.037 | ||
| LDL Function | ||||
| LDL susceptibility to aggregation | 0.258 | -0.135 | ||
| LDL(-) | 0.807 | -0.029 | ||
| LDL size | 0.007 | -0.320 | ||
| LDL susceptibility to oxidation | 0.252 | -0.143 | ||
| Bivariate analysis | β | p |
| Age | 0.413 | <0.001 |
| BMI | 0.300 | 0.009 |
| GGT | 0.467 | <0.001 |
| LDLsize | -0.372 | 0.002 |
| HbA1c | 0.237 | 0.049 |
| Tg | 0.189 | 0.111 |
| %ApoAI in HDL | -0.22 | 0.065 |
| %ApoCIII in HDL | 0.198 | 0.098 |
| β | p | R2 | |
| Age | 0.484 | <0.001 | 0.505 |
| Sex | 0.164 | 0.085 | |
| BMI | 0.164 | 0.089 | |
| LDL size | -0.268 | 0.01 | |
| GGT | 0.343 | 0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





