Submitted:
05 December 2024
Posted:
06 December 2024
You are already at the latest version
Abstract
Enteral nutrition (EN) formulas are necessary for critically ill patients to meet their metabolic requirements. Polyamines (putrescine, spermidine and spermine) are crucial dietary components, with spermidine being particularly interesting due to its proposed multiple benefits. The requirements for and intake of polyamines have yet to be investigated in adult patients hospitalised in intensive care units (ICUs) exclusively fed via commercial EN formulas. The aim of this study was to determine the polyamine content of EN formulas and the total intake and gastric residual volume (GRV) in adult ICU patients during their first seven days of hospitalisation. Polyamines were analysed in 17 EN formulas using high-performance liquid chromatography (HPLC). The clinical data of 8 patients of both sexes aged 47 to 77 admitted to the ICU were analysed. Differences existed among the analysed EN formulas. The N-acetyl putrescine content was higher than the remaining amines. The daily intake in the ICU was less than 100 μmol (the dietary intake is above 400 μmol). An inverse correlation existed between total daily polyamine intake and daily GRV. Polyamine intake in critically ill patients receiving EN is low and could impact these patients’ feeding tolerance. These findings underscore the need for further research to explore the clinical implications of increasing the polyamine content of EN formulas.
Keywords:
1. Introduction
2. Materials and Methods
2.1. Determination of the Polyamine Content of Commercial EN Formulas via HPLC
2.2. Characteristics of the EN Formulas
2.4. Study Design, Patient Population and Clinical Data
2.5. Statistical Analyses
3. Results
3.1. Polyamine Content of the EN Formulas
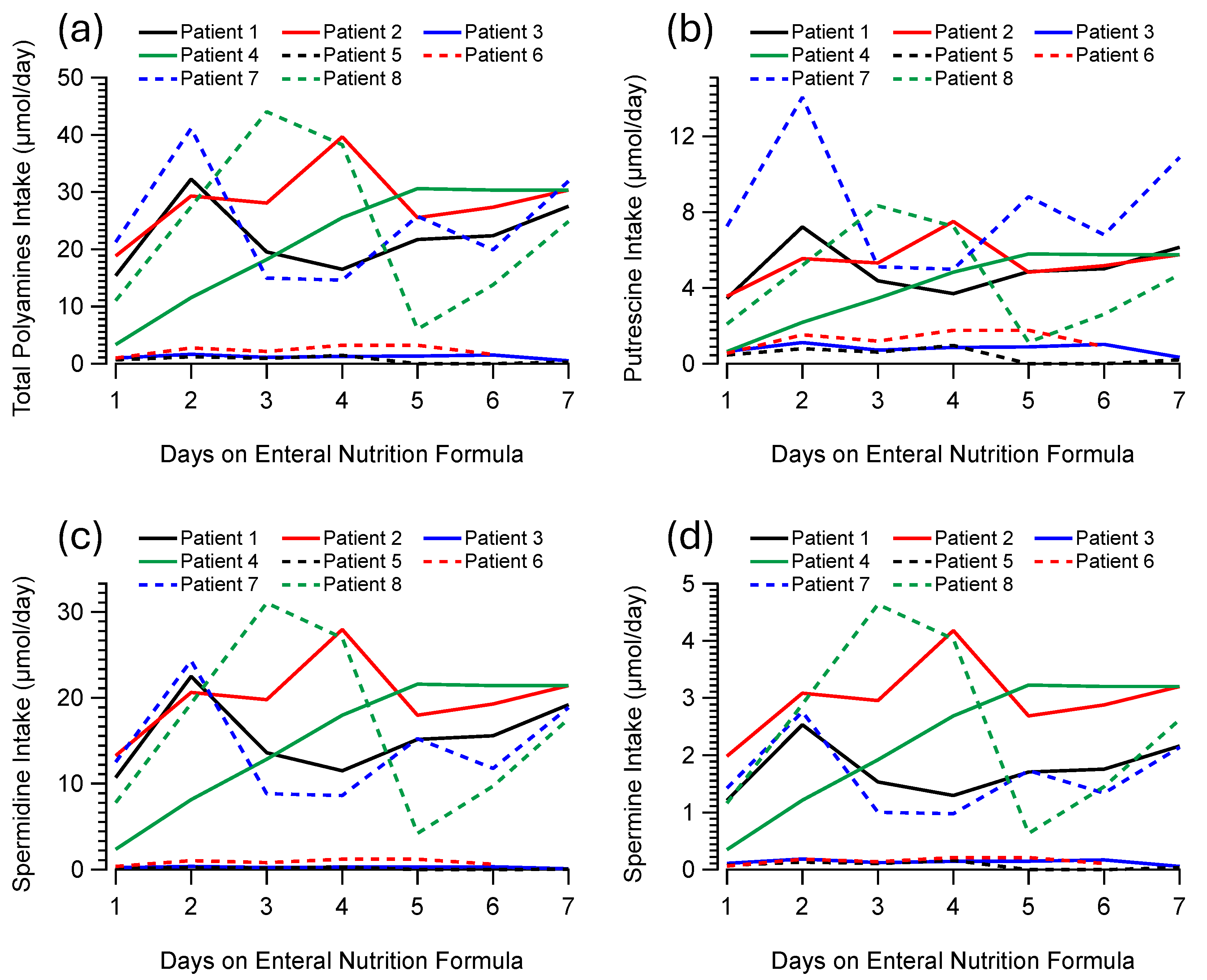
3.2. Patients and Daily Polyamine Intake via EN Formulas
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mozaffarian, D.; Rosenberg, I.; Uauy, R. History of modern nutrition science-implications for current research, dietary guidelines, and food policy. Bmj 2018, 361, k2392. [Google Scholar] [CrossRef] [PubMed]
- Mohamed Elfadil, O.; Velapati, S.R.; Patel, J.; Hurt, R.T.; Mundi, M.S. Enteral Nutrition Therapy: Historical Perspective, Utilization, and Complications. Curr Gastroenterol Rep 2024. [Google Scholar] [CrossRef] [PubMed]
- Wischmeyer, P.E.; Klek, S.; Berger, M.M.; Berlana, D.; Gray, B.; Ybarra, J.; Ayers, P. Parenteral nutrition in clinical practice: International challenges and strategies. Am J Health Syst Pharm 2024, 81, S89–s101. [Google Scholar] [CrossRef] [PubMed]
- Kong, S.; Zhang, Y.H.; Zhang, W. Regulation of Intestinal Epithelial Cells Properties and Functions by Amino Acids. Biomed Res Int 2018, 2018, 2819154. [Google Scholar] [CrossRef]
- Demehri, F.R.; Barrett, M.; Ralls, M.W.; Miyasaka, E.A.; Feng, Y.; Teitelbaum, D.H. Intestinal epithelial cell apoptosis and loss of barrier function in the setting of altered microbiota with enteral nutrient deprivation. Front Cell Infect Microbiol 2013, 3, 105. [Google Scholar] [CrossRef]
- Doyle, D.J.; Hendrix, J.M.; Garmon, E.H. American Society of Anesthesiologists Classification [Updated 2023 Aug 17]. 2024.
- Yang, H.; Hou, L.; Sun, H.M.; Ye, S.H. Comparison of micronutrients in adult enteral formulas widely used in clinical practice. Food Sci Nutr 2023, 11, 6096–6105. [Google Scholar] [CrossRef]
- Cantabrana, B.; Peña-Iglesias, P.; Castro-Estrada, P.; Suárez, L.; Bordallo, J.; Barreiro-Alonso, E.; Sánchez, M. Dietary intake of polyamines in a Spanish adult population: Age-dependent correlation with Healthy Eating Index and Dietary Inflammatory Index scores. Nutrition 2024, 130, 112608. [Google Scholar] [CrossRef]
- Liu, B.; Jiang, X.; Cai, L.; Zhao, X.; Dai, Z.; Wu, G.; Li, X. Putrescine mitigates intestinal atrophy through suppressing inflammatory response in weanling piglets. J Anim Sci Biotechnol 2019, 10, 69. [Google Scholar] [CrossRef]
- Minetti, A.; Omrani, O.; Brenner, C.; Allies, G.; Imada, S.; Rösler, J.; Khawaled, S.; Cansiz, F.; Meckelmann, S.W.; Gebert, N.; et al. Polyamines sustain epithelial regeneration in aged intestines by modulating protein homeostasis. bioRxiv 2024. [Google Scholar] [CrossRef]
- Bardócz, S.; Grant, G.; Brown, D.S.; Pusztai, A. Putrescine as a source of instant energy in the small intestine of the rat. Gut 1998, 42, 24–28. [Google Scholar] [CrossRef]
- Tofalo, R.; Cocchi, S.; Suzzi, G. Polyamines and Gut Microbiota. Front Nutr 2019, 6, 16. [Google Scholar] [CrossRef] [PubMed]
- Hesterberg, R.S.; Cleveland, J.L.; Epling-Burnette, P.K. Role of Polyamines in Immune Cell Functions. Med Sci (Basel) 2018, 6. [Google Scholar] [CrossRef] [PubMed]
- Sánchez, M.; Suárez, L.; Andrés, M.T.; Flórez, B.H.; Bordallo, J.; Riestra, S.; Cantabrana, B. Modulatory effect of intestinal polyamines and trace amines on the spontaneous phasic contractions of the isolated ileum and colon rings of mice. Food Nutr Res 2017, 61, 1321948. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.C.; Sim, J.H.; Kim, Y.H.; Kwon, S.C.; Lee, S.J.; Kim, S.R.; Kim, D.W.; Park, S.M.; Youn, S.J.; Lee, S.J.; et al. Effects of polyamines on contractility of guinea-pig gastric smooth muscle. J Korean Med Sci 2007, 22, 48–56. [Google Scholar] [CrossRef]
- ter Steege, J.C.; Buurman, W.A.; Forget, P.P. Spermine induces maturation of the immature intestinal immune system in neonatal mice. J Pediatr Gastroenterol Nutr 1997, 25, 332–340. [Google Scholar] [CrossRef]
- van Wettere, W.H.; Willson, N.L.; Pain, S.J.; Forder, R.E. Effect of oral polyamine supplementation pre-weaning on piglet growth and intestinal characteristics. Animal 2016, 10, 1655–1659. [Google Scholar] [CrossRef]
- Schibalski, R.S.; Shulha, A.S.; Tsao, B.P.; Palygin, O.; Ilatovskaya, D.V. The role of polyamine metabolism in cellular function and physiology. American journal of physiology. Cell physiology 2024, 327, C341–c356. [Google Scholar] [CrossRef]
- Xuan, M.; Gu, X.; Li, J.; Huang, D.; Xue, C.; He, Y. Polyamines: their significance for maintaining health and contributing to diseases. Cell Communication and Signaling 2023, 21, 348. [Google Scholar] [CrossRef]
- Soda, K.; Dobashi, Y.; Kano, Y.; Tsujinaka, S.; Konishi, F. Polyamine-rich food decreases age-associated pathology and mortality in aged mice. Exp Gerontol 2009, 44, 727–732. [Google Scholar] [CrossRef]
- Eisenberg, T.; Knauer, H.; Schauer, A.; Büttner, S.; Ruckenstuhl, C.; Carmona-Gutierrez, D.; Ring, J.; Schroeder, S.; Magnes, C.; Antonacci, L.; et al. Induction of autophagy by spermidine promotes longevity. Nat Cell Biol 2009, 11, 1305–1314. [Google Scholar] [CrossRef]
- Kim, J.; Baek, Y.; Lee, S. Dietary polyamine intake lowers the risk of all-cause and cardiovascular disease-related mortality: Follow-up of the Korean National health and nutrition Examination survey 2007–2015. Journal of Functional Foods 2024, 119, 106268. [Google Scholar] [CrossRef]
- Soda, K.; Kano, Y.; Chiba, F. Food polyamine and cardiovascular disease--an epidemiological study. Glob J Health Sci 2012, 4, 170–178. [Google Scholar] [CrossRef] [PubMed]
- Madeo, F.; Hofer, S.J.; Pendl, T.; Bauer, M.A.; Eisenberg, T.; Carmona-Gutierrez, D.; Kroemer, G. Nutritional Aspects of Spermidine. Annu Rev Nutr 2020, 40, 135–159. [Google Scholar] [CrossRef] [PubMed]
- Ralph, A.; Englyst, K.; Bardocz, S. Polyamine content of the human diet. In In Polyamines in Health and Nutrition, Bardócz, S., White, A., Eds.; Kluwer Academic Publishers: London, UK, 1999. [Google Scholar]
- Atiya Ali, M.; Poortvliet, E.; Strömberg, R.; Yngve, A. Polyamines in foods: development of a food database. Food & Nutrition Research 2011, 55, 5572. [Google Scholar] [CrossRef]
- Zoumas-Morse, C.; Rock, C.L.; Quintana, E.L.; Neuhouser, M.L.; Gerner, E.W.; Meyskens, F.L., Jr. Development of a polyamine database for assessing dietary intake. J Am Diet Assoc 2007, 107, 1024–1027. [Google Scholar] [CrossRef]
- Nishibori, N.; Fujihara, S.; Akatuki, T. Amounts of polyamines in foods in Japan and intake by Japanese. Food Chemistry 2007, 100, 491–497. [Google Scholar] [CrossRef]
- Buyukuslu, N.; Hizli, H.; Esin, K.; Garipagaoglu, M. A Cross-Sectional Study: Nutritional Polyamines in Frequently Consumed Foods of the Turkish Population. Foods 2014, 3, 541–557. [Google Scholar] [CrossRef]
- Atiya Ali, M.; Poortvliet, E.; Strömberg, R.; Yngve, A. Polyamines: total daily intake in adolescents compared to the intake estimated from the Swedish Nutrition Recommendations Objectified (SNO). Food Nutr Res 2011, 55. [Google Scholar] [CrossRef]
- Martín-Vicente, P.; López-Martínez, C.; Rioseras, B.; Albaiceta, G.M. Activation of senescence in critically ill patients: mechanisms, consequences and therapeutic opportunities. Annals of intensive care 2024, 14, 2. [Google Scholar] [CrossRef]
- Luo, D.; Lu, X.; Li, Y.; Xu, Y.; Zhou, Y.; Mao, H. Metabolism of Polyamines and Kidney Disease: A Promising Therapeutic Target. Kidney Dis (Basel) 2023, 9, 469–484. [Google Scholar] [CrossRef]
- Eisenberg, T.; Abdellatif, M.; Schroeder, S.; Primessnig, U.; Stekovic, S.; Pendl, T.; Harger, A.; Schipke, J.; Zimmermann, A.; Schmidt, A.; et al. Cardioprotection and lifespan extension by the natural polyamine spermidine. Nat Med 2016, 22, 1428–1438. [Google Scholar] [CrossRef] [PubMed]
- Wang, T.; Li, N.; Zeng, Y. Protective effects of spermidine levels against cardiovascular risk factors: An exploration of causality based on a bi-directional Mendelian randomization analysis. Nutrition 2024, 127, 112549. [Google Scholar] [CrossRef] [PubMed]
- Yarova, P.; Al-Zadjali, R.B.A.; Scott, J.; Josiah, E.; Turnbull, E.; Ebbern, C.E.; Telezhkin, V.S.; Rostron, A.; Riccardi, D.; Simpson, A.J. Polyamines as regulators of pulmonary inflammation. European Respiratory Journal 2024, 64, PA5327. [Google Scholar] [CrossRef]
- Luo, J.; Kim, Y.J.; An, X.; Fan, L.; Erb, C.; Lou, D.; Yao, Y.; Ferguson, A.A.; Pan, Y.; Chen, K. Spermidine dampens inflammation by directly inhibiting Th17 cytokine production through a PRDX1 associated antioxidant pathway. 2021, 2021.2008.2031.458409. [CrossRef]
- Baek, A.R.; Hong, J.; Song, K.S.; Jang, A.S.; Kim, D.J.; Chin, S.S.; Park, S.W. Spermidine attenuates bleomycin-induced lung fibrosis by inducing autophagy and inhibiting endoplasmic reticulum stress (ERS)-induced cell death in mice. Experimental & Molecular Medicine 2020, 52, 2034–2045. [Google Scholar] [CrossRef]
- Chia, T.Y.; Zolp, A.; Miska, J. Polyamine Immunometabolism: Central Regulators of Inflammation, Cancer and Autoimmunity. Cells 2022, 11. [Google Scholar] [CrossRef]
- Arthur, R.; Jamwal, S.; Kumar, P. A review on polyamines as promising next-generation neuroprotective and anti-aging therapy. European Journal of Pharmacology 2024, 978, 176804. [Google Scholar] [CrossRef]
- Escribano, M.I.; Legaz, M.E. High performance liquid chromatography of the dansyl derivatives of putrescine, spermidine, and spermine. Plant Physiol 1988, 87, 519–522. [Google Scholar] [CrossRef]
- Cantabrana, B.; Peña-Iglesias, P.; Castro-Estrada, P.; Suarez, L.; Bordallo, J.; Barreiro-Alonso, E.; Sánchez, M. Dietary intake of polyamines in a Spanish adult population: Age-dependent and correlation with the healthy dietary index and dietary inflammatory index scores. Nutrition (Burbank, Los Angeles County, Calif.) 2024, 112608. [CrossRef]
- Kasahara, N.; Teratani, T.; Yokota, S.; Sakuma, Y.; Sasanuma, H.; Fujimoto, Y.; Ijichi, T.; Urahashi, T.; Yoshitomi, H.; Kitayama, J.; et al. Dietary polyamines promote intestinal adaptation in an experimental model of short bowel syndrome. Scientific Reports 2024, 14, 4605. [Google Scholar] [CrossRef]
- Tan, B.; Xiao, D.; Wang, J.; Tan, B. The Roles of Polyamines in Intestinal Development and Function in Piglets. Animals (Basel) 2024, 14. [Google Scholar] [CrossRef]
- Wang, Z.; Jiang, D.; Wang, X.; Jiang, Y.; Sun, Q.; Ling, W.; An, X.; Ji, C.; Li, S.; Qi, Y.; et al. Spermidine improves the antioxidant capacity and morphology of intestinal tissues and regulates intestinal microorganisms in Sichuan white geese. Front Microbiol 2023, 14, 1292984. [Google Scholar] [CrossRef]
- Rao, J.N.; Xiao, L.; Wang, J.Y. Polyamines in Gut Epithelial Renewal and Barrier Function. Physiology (Bethesda, Md.) 2020, 35, 328–337. [Google Scholar] [CrossRef] [PubMed]
- Chamoto, K.; Zhang, B.; Tajima, M.; Honjo, T.; Fagarasan, S. Spermidine - an old molecule with a new age-defying immune function. Trends Cell Biol 2024, 34, 363–370. [Google Scholar] [CrossRef] [PubMed]
- Yu, L.; Zhang, C.; Zhai, Q. Gut Microbes Participate in Host Polyamine Metabolism. Proc Natl Acad Sci U S A 2024, 121, e2419368121. [Google Scholar] [CrossRef] [PubMed]
- Kovács, T.; Mikó, E.; Vida, A.; Sebő, É.; Toth, J.; Csonka, T.; Boratkó, A.; Ujlaki, G.; Lente, G.; Kovács, P.; et al. Cadaverine, a metabolite of the microbiome, reduces breast cancer aggressiveness through trace amino acid receptors. Scientific Reports 2019, 9, 1300. [Google Scholar] [CrossRef]
- Teng, Y.; Mu, J.; Xu, F.; Zhang, X.; Sriwastva, M.K.; Liu, Q.M.; Li, X.; Lei, C.; Sundaram, K.; Hu, X.; et al. Gut bacterial isoamylamine promotes age-related cognitive dysfunction by promoting microglial cell death. Cell Host Microbe 2022, 30, 944–960.e948. [Google Scholar] [CrossRef]
- Moiseenko, V.I.; Apryatina, V.A.; Gainetdinov, R.R.; Apryatin, S.A. Trace Amine-Associated Receptors’ Role in Immune System Functions. Biomedicines 2024, 12, 893. [Google Scholar] [CrossRef]
- Berry, M.D.; Gainetdinov, R.R.; Hoener, M.C.; Shahid, M. Pharmacology of human trace amine-associated receptors: Therapeutic opportunities and challenges. Pharmacol Ther 2017, 180, 161–180. [Google Scholar] [CrossRef]
| Formula Type | Name | Manufacturer |
|---|---|---|
| Complete, polymeric | ||
| Hyperproteic and hypercaloric | Fresubin Thickened | Fresnius kabi |
| Isosource Protein Fibre | Nestlé | |
| Novasource GI Protein | Nestlé | |
| Osmolite Plus | Abbott | |
| Normoproteic and hypercaloric | Nutrison Energy | Nutricia |
| Nutrison Energy Multi Fibre | Nutricia | |
| Normoproteic and normocaloric | Fresubin Original Fibre | Fresnius kabi |
| Nutrison | Nutricia | |
| Osmolite | Abbott | |
| Hyperproteic and normocaloric | Impact Enteral | Nestlé |
| Complete, special | ||
| Hyperproteic and hypercaloric | Impact | Nestlé |
| Nepro HP | Abbott | |
| Nutrison Advanced Diason | Nutricia | |
| Energy HP | ||
| Normoproteic and hypercaloric | Nutricomp Hepa | B. Braun |
| Oxepa | Abbott | |
| Hypoproteic and hypercaloric | Nepro LP | Abbott |
| Proteic | Protein NM | Cantabria Labs |
| EN Formulas (n) | Putrescine | Spermidine | Spermine | N-Acetyl Putrescine | N-Acetyl Spermidine | N-Acetyl Spermine | Total Polyamines |
|---|---|---|---|---|---|---|---|
| Fresubin Original Fibre (8) (Fresenius Kabi) |
1.87(0.2) | 11.46(0.66) | 2.55(0.17) | 42.39(3.72) | 0.58(0.05) | 0.28(0.04) | 15.88(0.95) |
| Fresubin Thickened (1) (Fresenius Kabi) |
2.73 | 1.37 | 0.52 | 176.69 | 3.76 | 0.67 | 4.62 |
| Impact (4) (Nestle Health Science) |
5.81(0.4) | 12.48(1.27) | 10.82(0.99) | 20.81(0.58) | 1.45(0.3) | 1.47(0.33) | 29.1(2.48)ǂ |
| Impact Enteral (1) (Nestle Health Science) |
10.67 | 18.24 | 12.78 | 29.74 | 3.75 | 2.62 | 41.69 |
| Isosource Protein Fibre (6) (Nestle Health Science) |
5.88(1.04) | 10.04(1.72) | 1.52(0.27) | 22.71(9.99) | 0.66(0.07) | 0.2(0.02) | 17.43(2.58) |
| Nepro HP (2) (Abbott) | 4.91(1.26) | 2.24(0.63) | 0.55(0.26) | 53.45(7.08) | 1.27(0.73) | 0.14(0.11) | 7.7(2.15) |
| Nepro LP (6) (Abbott) | 1.33(0.44) | 0.89(0.23) | 0.35(0.1) | 28.5(1.44) | 1.66(0.78) | 0.07(0.01) | 2.57(0.65) |
| Novasource GI Protein (3) (Nestle Health Science) |
1.18(0.28) | 0.81(0.22) | 0.14(0.09) | 21.2(5.73) | 0.48(0.32) | 0.02 | 2.13(0.56) |
| Nutricomp HEPA (9) (B Braun Sharing Expertise) |
3.28(1.21) | 1.09(0.27) | 0.55(0.24) | 307.99(177.85) | 6.93(1.22) | 0.32(0.17) | 4.92(1.46) |
| Nutrison (5) (Nutricia) | 5.13(0.87) | 15.99(3.89) | 1.8(0.41) | 177.59(64.52) | 1.63(0.91) | 0.26(0.12) | 22.92(5.02)ǂ |
| Nutrison Advanced Diason Energy HP (10) (Nutricia) |
5.75(0.74) | 21.42(1.36) | 3.2(0.21) | 35.15(3.43) | 1.49(0.13) | 0.54(0.07) | 30.37(1.98)ǂ |
| Nutrison Energy (1) (Nutricia) | 11.13 | 13.91 | 1.16 | 287.73 | 1.25 | 0.18 | 26.19 |
| Nutrison Energy Multifibre (3) (Nutricia) |
10.8(0.86) | 18.69(2.26) | 2.12(0.4) | 311.19(6.73) | 1.12(0.16) | 0.29(0.04) | 31.61(2.2)ǂ |
| Osmolite (1) (Abbott) | 1.7 | 1.2 | 0.16 | 19.82 | 0.39 | 0.22 | 3.06 |
| Osmolite Plus (3) (Abbott) | 1.96(0.03) | 1.25(0.08) | 0.17(0.01) | 19.43(0.96) | 0.38(0.02) | 0.09(0.01) | 3.38(0.11) |
| Oxepa (2) (Abbott) | 1.5(0.05) | 3.06(0.41) | 0.3(0.04) | 24.41(0.78) | 0.75(0.05) | 0.26(0.07) | 4.86(0.4) |
| Proteina NM (2) (Cantabria Labs) | 0.53(0.1) | 0 | 0.52(0.01) | 7.45(0.2) | 0.48(0.05) | 2.21 | 1.05(0.09) |
| EN Formulas (n) | Cadaverine | Tyramine |
β-phenyl- #ethylamine |
Isoamylamine |
|---|---|---|---|---|
| Fresubin Original Fibre (8) (Fresenius Kabi) |
1.21(0.1)*** | 0.97(0.08) | 0.26(0.03)*** | 7.78(2.94) |
| Fresubin Thickened (1) (Fresenius Kabi) |
1.66 | 4.01 | 0 | 8.43 |
| Impact (4) (Nestle Health Science) | 1.32(0.1)* | 1.59(0.08) | 0.55(0.02)*** | 1.71(0.25) |
| Impact Enteral (1) (Nestle Health Science) |
2.88 | 3.03 | 0.54 | 7.26 |
| Isosource Protein Fibre (6) (Nestle Health Science) |
1.4(0.32)* | 2.25(0.5) | 0.34(0.03)*** | 5.22(1.43) |
| Nepro HP (2) (Abbott) | 1.72(0.67) | 4(0.41) | 1.42(0.48) | 14.27(7.14) |
| Nepro LP (6) (Abbott) | 0.58(0.19)*** ɸɸ | 2.17(1.48) | 1.32(0.68)*** | 5.11(1.92) |
| Novasource GI Protein (3) (Nestle Health Science) |
0.6(0.14)*** ɸ | 0.78(0.26) | 0.05 | 4.32(0.31) |
| Nutricomp HEPA (9) (B Braun Sharing Expertise) |
1.62(0.35)* | 2.44(0.51) | 6.87(1.01)*** | 63.33(29.49) |
| Nutrison (5) (Nutricia) | 0.81(0.18)*** ɸ | 1.82(0.39) | 0.6(0.33)*** | 7.08(1.36) |
| Nutrison Advanced Diason Energy HP (10) (Nutricia) |
2.67(0.22) | 1.5(0.15) | 0.65(0.09)*** | 5.23(1.12) |
| Nutrison Energy (1) (Nutricia) | 1.04 | 3.47 | 0.34 | 8 |
| Nutrison Energy Multifibre (3) (Nutricia) |
2.47(0.13) | 1.32(0.21) | 0.56(0.08)*** | 4.13(1.98) |
| Osmolite (1) (Abbott) | 0.62 | 0.71 | 0.46 | 2.32 |
| Osmolite Plus (3) (Abbott) | 0.68(0.02) | 0.79(0.07) | 0.39(0.01)*** | 2.07(0.62) |
| Oxepa (2) (Abbott) | 0.53(0.05) | 0.71 | 0.6(0.07) | 1.42(0.08) |
| Proteina NM (2) (Cantabria Labs) | 3.74 | 0 | 0.56(0.02) | 4.44(0.87) |
| Biogenic Amines | Daily Intake via EN (Standard Error) (µmol) | Range of Daily Intake via EN (µmol) |
|---|---|---|
| Putrescine | 4.04 (1.01) | 0.21–14.06 |
| Spermidine | 11.53 (3.42) | 0.07–32.39 |
| Spermine | 1.62 (0.49) | 0.03–4.84 |
| Total Polyamines | 17.18 (4.79) | 0.31–45.92 |
| N-Acetyl putrescine | 81.59 (27.35) | 3.87–405.17 |
| N -Acetyl spermidine | 1.26 (0.14) | 0.16–2.36 |
| N -Acetyl spermine | 0.27 (0.08) | 0.01–0.82 |
| Cadaverine | 1.47 (0.38) | 0.1–4.04 |
| Tyramine | 1.11 (0.16) | 0.15–2.56 |
| β-Phenyletylamine | 0.73 (0.18) | 0.02–2.34 |
| Isoamylamine | 7.05 (1.49) | 0.58–21.53 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





