1. Introduction
The presence of supernumerary teeth in addition to the normal formula is a dental anomaly that affect the maxilla more than the mandible, mostly the premaxilla region, referred to as mesiodens. Conical mesiodens often can erupt into the oral cavity and have a completely formed root. However, their crown can be inverted pointing superiorly, in which case they are less likely to erupt intraoral. Inverted conical mesiodens can be accidental found at the base of the nasal cavity, which is known as an inverted position. The ectopic eruption is one of the common complications of supernumerary teeth [
1,
2].
The etiology of supernumerary teeth has been previously explained through various theories, among them, the phylogenetic reversion or atavism, the hyperactivity of the dental lamina or a combination of genetic factors. The clinical findings in case of supernumerary teeth vary greatly, including: no effect, crowding, malposition, eruption disturbances, the development of follicular cysts, neuralgic manifestations and occasionally eruption into the nasal cavity. According to available data 75% of the mesiodens are impacted [
3,
4].
The impacted supernumeraries may be detected by imaging techniques, such as orthopantomographs (OPG), occlusal, periapical radiographs or cone beam computed tomography (CBCT), which provides more accurate assessments [
5]. Most mesiodens are unerupted during early mixed dentition with the reported range being 79–91%. Their presence is often detected during a routine clinical or radiographic examination without there being an association with any pathology in 7–20% of the cases surveyed [
6,
7].
The nasal floor approach should be considered when extracting an inverted mesiodens, reducing bone removal and preventing anatomical damages. Because a mesiodens mostly develops on the palatal side, many surgeons prefer a palatal approach for surgical extraction [
8]. However, this approach is associated with poor accessibility and a risk of nasopalatine nerve damage. Some surgeons opt for the buccal approach, despite the high risk of injury to nearby permanent teeth [
9]. In 2011, a transoral approach to intranasal teeth, a surgical technique called the modified maxillary vestibular approach with subperiosteal intranasal dissection was suggested to prevent excessive bone removal and complications related to the traditional intraoral buccal or palatal approaches. Compared to the buccal and the palatal approach, the time to find and identify the tooth in the subperiosteal intranasal approach is distinctly shorter [
10].
In general, the higher and deeper position of mesiodens in bone is, the closer they are to the apical root of the adjacent teeth, and the more complications in tooth extraction are involved. The main advantage of the traditional buccal approach is that it provides an excellent surgical view, reducing surgical stress. If the surgeon selects the palatal approach, there are fewer aesthetic problems in the anterior maxillary area, and the postoperative swelling degree is slight. Extensive osteotomy and prolonged operation may decrease the blood supply and pulp vitality of the adjacent teeth [
11]. In addition to intra-oral buccal or palatal trans-alveolar approaches, an endoscopically assisted transnasal technique can be suitable for the removal of mesiodens erupting into the nasal floor [
12]. The location and morphology of inverted mesiodens will affect the choice of the treatment but to date there is no generally accepted surgical procedure to minimize operation injury for high inverted mesiodens.
2. Materials and Methods
This report presents the nasal floor approach as a very reliable option for extracting inverted mesiodens. This method was first described by Sammartino et. al in 2011 [
10], but the main constraints were mainly related to the damage to the nasal mucosa and misplacing the mesiodens into the nasal cavity with the risk of aspiration and causing airway obstruction.
We report our protocol, including the diagnosis process, criteria for choosing this surgical approach and description of the surgical procedure.
2.1. Diagnosis process
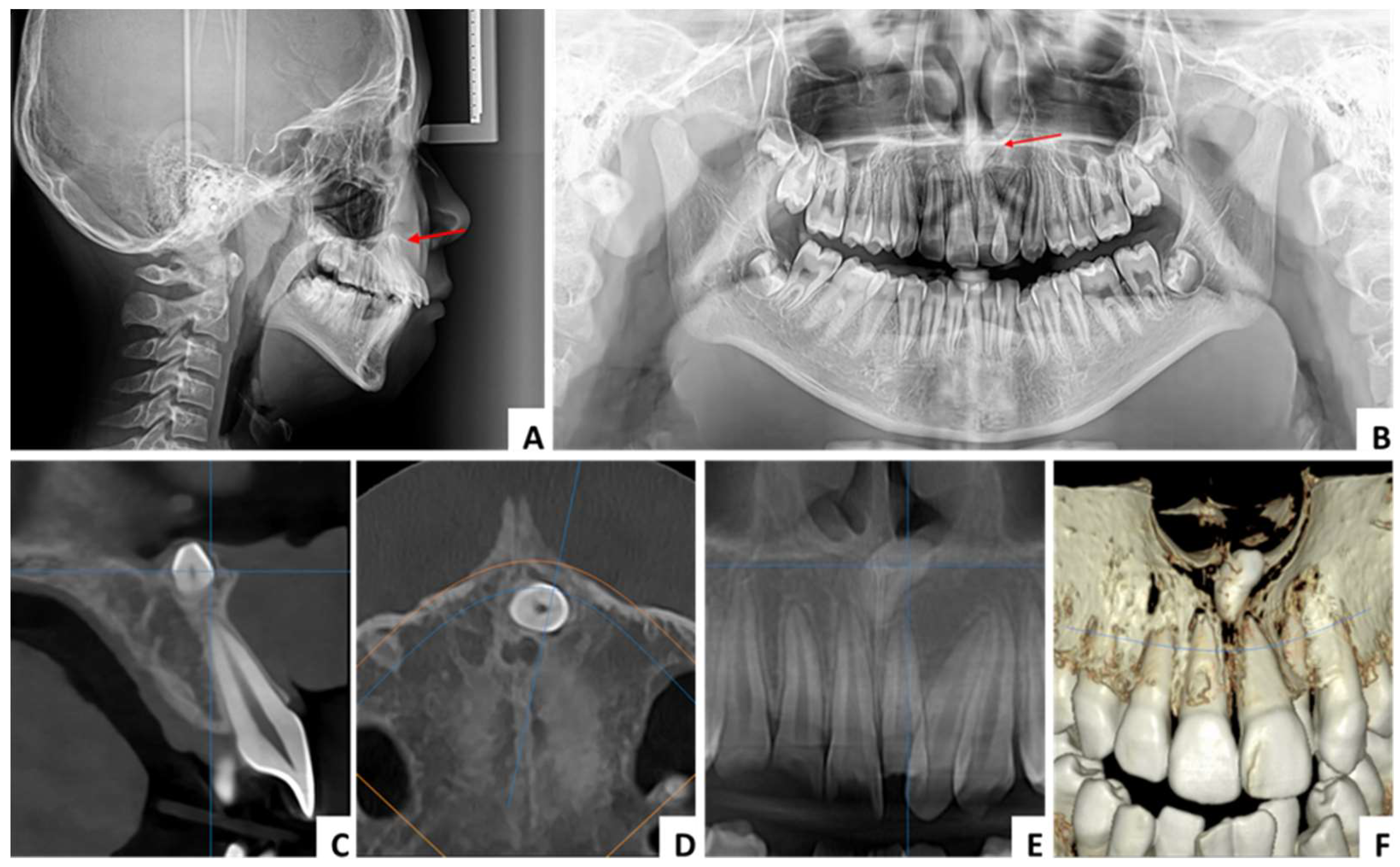
The inverted mesiodens is mainly asymptomatic, in some cases a diastema can be associated. The main diagnostic methods are radiological, especially CBCT. It can be detected also by conventional imaging techniques used in dental practice such as OPG, but in this case there are some serious limitations regarding the lack of clarity in the midline region (
Figure 1). Preoperative CBCT is mandatory in our protocol regarding included mesiodens. It provides an accurate 3D localization, position and shape of the impacted teeth and allow us to choose the appropriate surgical procedure (
Table 1).
2.2. Choice of surgical approach
The main criteria taken into account for determination of the surgical approach are represented by the shortest linear distance to the mesiodens, good surgical field, preventing extensive osteotomy, protection of neighboring teeth, preventing neurovascular injury to the nasopalatine nerve, avoiding prolonged operation time and limited postoperative discomfort for the patient. In case of inverted mesiodens breaching the nasal floor (submucosally or covered with a cortical layer of the nasal floor bone), the nasal floor approach satisfies all these conditions (
Table 2).
2.3. Nasal floor approach procedure
The patients require short term hospitalization and the surgical procedure is performed under general anesthesia (naso or oro tracheal intubation). Local anesthesia (articaine with epinephrine) is also performed for pain control and limited bleeding thus providing a better visualization of the surgical field. A vestibular maxillary incision from the canine to the canine is made, followed by subperiosteal dissection and elevation of the mucoperiosteal flap toward the anterior nasal spine (ANS) and nasal floor. The nasal mucosa is elevated from the base of the piriform aperture and ANS gaining access to the anterior aspect of the nasal floor. Where necessary, the bone partially covering the mesiodens is remove with rotary instruments under saline irrigation. The mesiodens is exposed, gently luxated and removed through the nasal floor using extraction elevators. Bleeding control is achieved and the surgical site is irrigated with saline solution. The mucoperiosteal flap is repositioned and sutured with a single layer 4/0 rapid absorbable sutures. The follow up includes routine clinical and radiological examinations for assessment of possible postoperative complications.
2.4. Case series
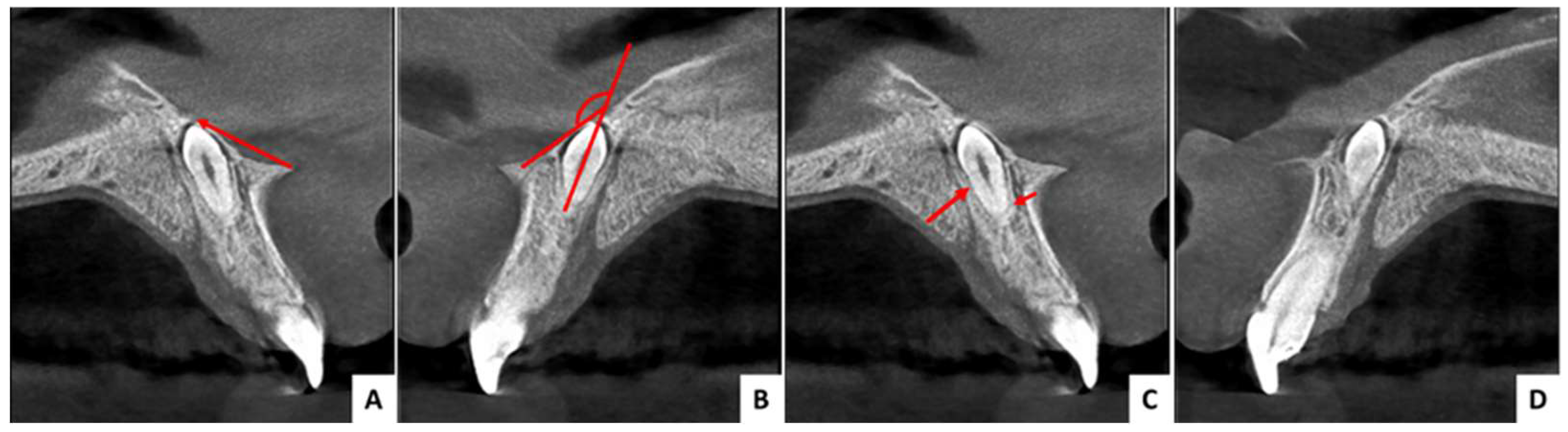
We report a series of cases to support the predictability of this surgical technique. In all cases no clinical symptoms were recorded, the inverted mesiodens were identified following routine radiographic examinations for dental or orthodontic purposes. All patients underwent a CBCT for diagnosis and choice of the surgical approach. The following parameters were determined on the cross-sectional view of the CBCT investigation: angle between the nasal floor line and the axis of the mesiodens, distance from ANS, distance to mesiodens from buccal and palatal aspect, relation with the nasal cavity (submucosally or covered with bone), and the position regarding the nasopalatine canal (
Figure 2).
Taking into account all these parameters and the criteria for choosing the surgical technique, it was decided to use the nasal floor approach procedure for surgical removal of the inverted mesiodens. All surgeries were performed by the same surgical team, consisting of a maxillofacial surgeon and two resident surgeons. All extractions were performed according to a uniform surgical protocol. The postoperative medication consisted in antibiotics (Amoxicillin/clavulanic acid) and nonsteroidal anti-inflammatory drugs (Ibuprofen). The usual postoperative indications were given related to diet, oral hygiene, swelling and in one case to avoid smoking.
The patients were called for follow-ups, the last radiograph (OPG) that was recorded being dated three years after surgery.
3. Results
All mesiodens were successfully removed without exposing the roots of the adjacent central incisors or nasopalatine canal and no damage to the nasal mucosa was recorded. The operation time was approximately 30 minutes in all cases. No other intraoperative or postoperative complications or accidents occurred. None of the patients complained about bleeding, breathing, swelling, difficulties in feeding or maintaining oral hygiene, hypoesthesia or postoperative pain.
One of the patients was female, aged 29, and the other two were male, aged 11 and 16. In one case the angle between the nasal floor line and the axis of the mesiodens was less than 90° (85.93°), in the other two cases it was greater (143.5° and 144.4°). The distance from the ANS was less than 10 mm in two cases (8.98 mm and 8.11 mm) and greater in one (13.22 mm). In all cases the shortest distance to the mesiodens was from the buccal aspect and the mesiodens was positioned in front of the nasopalatine canal. In two cases the mesiodens was covered with bone and in one case it was positioned submucosally (
Table 3).
In all cases, the control radiograph (OPG) taken approximately three years after the surgery did not show any long-term complications or abnormalities in maxillary development (
Figure 5,
Figure 8,
Figure 11).
4. Discussion
The mesiodens is the most common form of a supernumerary tooth [
5,
13,
14]. In the majority of cases they are impacted, usually palatally, but can be found buccally or between the roots of the permanent central incisors. Their position can be normal, inclined or inverted [
5].
The most common complications related to the presence of mesiodens are those related to the alterated eruption of permanent teeth, crowding or spacing of the anterior teeth, root resorption of the adjacent teeth, cystic lesions formation or other bone destructive lesions [
7,
15,
16]. Considering these complications, prophylactically surgical extraction is recomanded [
17,
18,
19].
If the crown of the impacted mesiodens is directed to the nasal cavity, then we refer to as an inverted mesiodens. According to different studies, inverted mesiodens are reported to occur in 9 to 67% of the cases [
7,
20,
21]. This type of mesiodens can interfere with the base of the nasal cavity or the nasal septum and can also erupt into the nose. It is reported that mesiodens are in close contact with the cortical bone of the nasal base in 20.5% of cases [
5].
For the diagnosis and treatment of impacted mesiodens clinical and radiographical assessments are essential. Convetional 2D radiographs such as orthopantomographs (OPG) have some serious limitations regarding the lack of clarity in the midline region. Cone-beam computed tomography (CBCT) is an imaging technique which allows for accurate 3D localization of impacted teeth and has an essential role in choosing the optimal surgical approach [
22].
Endoscopically assisted transnasal approach can be used for removal of inverted mesiodens that are erupted into the nasal cavity or for mesiodens located under the nasal mucosa [23.24].
The most common method used for extraction in case of an included mesiodens mentioned in the literature is the palatal approach, followed by the buccal approach [
25,
26]. The traditional buccal approach provides an excellent surgical view. In case of inverted mesiodens, using this method requires excessive osteotomy and it may lead to an increase in intraoperative accidents and postoperative complications such as damaging the roots of the permanent incisors. Another drawback of this approach is that excessive osteotomy may exacerbate postoperative swelling and pain. To prevent all this, the palatal approach has been widely used, but it carries a high risk of neurovascular injury to the nasopalatine nerve, especially when the mesiodens is positioned in front of the nasopalatine canal [
9].
In 2011 Sammartino et al. described a new technique called “modified maxillary vestibular approach with subperiosteal intranasal dissection” to be used for the extraction of nasal impacted mesiodens [
10]. Using this approach, extensive osteotomy can be avoided in comparison with the palatal or the buccal approach. It is only needed to remove bone around the circumference of the impacted tooth and then the inverted mesiodens can be dislocated in the direction of its long axis towards the nasal floor [
11]. Reduce intraoperative bleeding is also an important advantage of this technique and this is due to the fact that the distribution of blood vessels in the nasal floor is less than that in the buccal side and thus we have less damage of the blood supply during surgery [
27]. The nasal floor approach also provides a good direct view of the surgical site and considering the minimal osteotomy needed and reduce bleeding can provide a short operating time. The approach proves to be effective and minimizes surgical trauma, leading to a significant decrease in postoperative swelling and pain. Studies found in the literature show that this approach offers the highest degree of patient satisfaction compared to the buccal or palatal approach. The low level of pain and swelling allow patients to return to their normal routine very soon after surgery [
11].
The main constraints of the approach are mainly related to the damage to the nasal mucosa and misplacing the mesiodens into the nasal cavity with the risk of aspiration and causing airway obstruction [
11]. For this reason, it seems that this method is contraindicated for dentists without advanced surgical experience. The approach is similar to that used in procedures such as Le Fort I osteotomy or SARPE, which is why this method is rather indicated for maxillofacial surgeons with experience in orthognathic surgery [
12].
For predictability of treatment and limitation of intra- and postoperative complications, a precise protocol related to the diagnostic process and the choice of surgical approach must be applied in the case of an impacted mesiodens.
The criteria that must be taken into account are: the shortest linear distance to the mesiodens, good surgical field, preventing extensive osteotomy, protection of neighboring teeth, preventing neurovascular injury to the nasopalatine nerve, avoiding prolonged operation time and limited postoperative discomfort for the patient. To satisfy all these criteria, a thorough CBCT analysis must be performed. This analysis includes the following determinations: angle between the nasal floor line and the axis of the mesiodens, distance from ANS, distance to mesiodens from buccal and palatal aspect, relation with the nasal cavity and the position regarding the nasopalatine canal.
Previous studies in the literature have suggested the nasal floor approach in cases where the angle between the nasal floor line and the axis of the mesiodens is less than 90° [
26,
28]. Other studies recommend a distance of up to 10 mm between the ANS and the mesiodens [
9].
However, in our experience it was not difficult to surgically remove inverted mesiodens through the nasal approach even in cases where the angle between the nasal floor line and the axis of the mesiodens was greater than 140° and the distance from ANS greater than 10 mm. Even in these situations, no intra- and postoperative complications or longer operating time were reported.
5. Conclusions
Within the limitations of this paper, the intraoral approach through the nasal floor for surgical removal of inverted mesiodens satisfies all the conditions to be a predictable, safe and time efficient technique. Like any other surgical technique it has its limitations, manly regarding the surgical skills of the operating team, previous experience in orthognathic surgery being necessary. Used correctly, it can be a technique that greatly limits the risk of intra- and post-operative complications and lead to a significant decrease in postoperative swelling and pain. Nowadays, the cone-beam computed tomography (CBCT) has a fundamental role in diagnosis and treatment of included mesiodens. A precise protocol with clear criteria must be used to determine the type of approach in the case of included mesiodens.
Author Contributions
Conceptualization, H.U. and M.P.; methodology, H.U. and F.S.; software H.U. and F.U.; validation, H.U. and M.P.; formal analysis, A.B. and F.U.; investigation, S.D. and A.B.; resources, F.S. and C.C.; data curation A.B. and C.C.; writing-original draft preparation, H.U. and F.S.; writing-review and editing, H.U. and M.P.; visualization, H.U. and S.D.; supervision, H.U.; project administration, H.U. and M.P. All authors have read and agreed to the published version of the manuscript.
Funding
We would like to acknowledge VICTOR BABES UNIVERSITY OF MEDICINE AND PHARMACY TIMIȘOARA for their support in covering the costs of publication for this research paper.
Institutional Review Board Statement
The patient signed a written informed consent form, agreeing to the publication of her medical data and any accompanying images.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data generated in this study may be requested from the corresponding author.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Rajaram Mohan, K.; Pethagounder Thangavelu, R.; Fenn, S.M. Bilateral Inverted Mesiodens: A Rare Case Evaluated by Cone-Beam Computed Tomography. Cureus 2022, 14, e26629. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ahmed, T.; Ahmed, S.; Kaushal, N. Extraction of Supernumerary Nasal Tooth by Endoscopic Approach. Contemp. Clin. Dent. 2021, 12, 321–323. [Google Scholar] [CrossRef] [PubMed]
- Beschiu, L.M.; Craiovan, B.A.; Popa, S.; Micle, D.; Ardelean, L.C.; Rusu, L.C. An Ancient Mesiodens Investigated by Cone Beam CT. Appl. Sci. 2021, 11, 11703. [Google Scholar] [CrossRef]
- Subasioglu, A.; Savas, S.; Kucukyilmaz, E.; Kesim, S.; Yagci, A.; Dundar, M. Genetic background of supernumerary teeth. Eur. J. Dent. 2015, 09, 153–158. [Google Scholar] [CrossRef]
- Mossaz, J.; Kloukos, D.; Pandis, N.; Suter, V.G.A.; Katsaros, C.; Bornstein, M.M. Morphologic characteristics, location, and associated complications of maxillary and mandibular supernumerary teeth as evaluated using cone beam computed tomography. Eur. J. Orthod. 2014, 36, 708–718. [Google Scholar] [CrossRef] [PubMed]
- Sanei-Moghaddam, A.; Hyde, N.; Williamson, P. Endoscopic removal of a supernumerary tooth from the nasal cavity in an adult. Br. J. Oral Maxillofac. Surg. 2009, 47, 484–485. [Google Scholar] [CrossRef] [PubMed]
- Shih, W.-Y.; Hsieh, C.-Y.; Tsai, T.-P. Clinical evaluation of the timing of mesiodens removal. J. Chin. Med Assoc. 2016, 79, 345–350. [Google Scholar] [CrossRef]
- Hauer, L.; Hrusak, D.; Jambura, J.; Gencur, J.; Hosticka, L.; Andrle, P.; Posta, P. Modified maxillary vestibular approach with subperiostal intranasal dissection for surgical extractions of mesiodentes impacted in the floor of the nasal cavity. J. Cranio-Maxillofacial Surg. 2019, 47, 1–5. [Google Scholar] [CrossRef]
- Ku, J.-K.; Jeon, W.-Y.; Baek, J.-A. Case series and technical report of nasal floor approach for mesiodens. J. Korean Assoc. Oral Maxillofac. Surg. 2023, 49, 214–217. [Google Scholar] [CrossRef] [PubMed]
- Sammartino, G.; Trosino, O.; Perillo, L.; Cioffi, A.; Marenzi, G.; Mortellaro, C. Alternative Transoral Approach for Intranasal Tooth Extraction. J. Craniofacial Surg. 2011, 22, 1944–1946. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Cheng, Y.; Lu, J.; Zhang, P.; Ning, Y.; Xue, L.; Zhang, Y.; Wang, J.; Hao, Y.; Wang, X. Extraction of high inverted mesiodentes via the labial, palatal and subperiostal intranasal approach: A clinical prospective study. Journal of Cranio-Maxillofacial Surgery 2023, 51, 433–440. [Google Scholar] [CrossRef] [PubMed]
- Elseyoufi, M.; Alrabiaa, A.H.; Tsakiris, P. Removal of nasally impacted mesiodens by maxillary vestibular transnasal approach. Adv. Oral Maxillofac. Surg. 2023, 10. [Google Scholar] [CrossRef]
- Fernández Montenegro, P.; Valmaseda Castellón, E.; Berini Aytés, L.; Gay Escoda, C. Retrospective study of 145 supernumerary teeth. Med Oral Patol Oral Cir Bucal. 2006, 11, E339–E344. [Google Scholar] [PubMed]
- Ferrés-Padró, E.; Prats-Armengol, J.; Ferrés-Amat, E. A descriptive study of 113 unerupted supernumerary teeth in 79 pediatric patients in Barcelona. Med Oral Patol Oral Cir Bucal. 2009, 14, E146–52. [Google Scholar] [PubMed]
- Finkelstein, T.; Shapira, Y.; Pavlidi, A.M.; Schonberger, S.; Blumer, S.; Sarne, O.; Shpack, N. Prevalence and Characteristics of Supernumerary Teeth in Israeli Orthodontic Patients. J. Clin. Pediatr. Dent. 2019, 43, 244–251. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.; Jeong, T.; Kim, J.; Shin, J.; Kim, S. Effects of mesiodens on adjacent permanent teeth: a retrospective study in Korean children based on cone-beam computed tomography. Int. J. Paediatr. Dent. 2017, 28, 161–169. [Google Scholar] [CrossRef]
- Russell, K.A.; Folwarczna, M.A. Mesiodens--diagnosis and management of a common supernumerary tooth. J Can Dent Assoc. 2003, 69, 362–6. [Google Scholar]
- Ayers, E.; Kennedy, D.; Wiebe, C. Clinical recommendations for management of mesiodens and unerupted permanent maxillary central incisors. Eur. Arch. Paediatr. Dent. 2014, 15, 421–428. [Google Scholar] [CrossRef]
- Pescia, R.; Kiliaridis, S.; Antonarakis, G.S. Spontaneous eruption of impacted maxillary incisors after surgical extraction of supernumerary teeth: a systematic review and meta-analysis. Clin. Oral Investig. 2020, 24, 3749–3759. [Google Scholar] [CrossRef]
- Canoglu, E.; Er, N.; Cehreli, Z.C. Double Inverted Mesiodentes: Report of an Unusual Case. Eur. J. Dent. 2009, 03, 219–223. [Google Scholar] [CrossRef]
- Syriac, G.; Joseph, E.; Rupesh, S.; Philip, J.; Cherian, S.A.; Mathew, J. Prevalence, characteristics, and complications of supernumerary teeth in nonsyndromic pediatric population of South India: A clinical and radiographic study. J. Pharm. Bioallied Sci. 2017, 9, 231–S236. [Google Scholar] [CrossRef]
- Aoun, G.; Nasseh, I. Mesiodens within the Nasopalatine Canal: An Exceptional Entity. Clin. Pr. 2016, 6, 903. [Google Scholar] [CrossRef] [PubMed]
- Sanei-Moghaddam, A.; Hyde, N.; Williamson, P. Endoscopic removal of a supernumerary tooth from the nasal cavity in an adult. Br. J. Oral Maxillofac. Surg. 2009, 47, 484–485. [Google Scholar] [CrossRef] [PubMed]
- Clementini, M.; Morlupi, A.; Agrestini, C.; Di Girolamo, M.; Di Girolamo, S.; Ottria, L. Endoscopic removal of supernumerary tooth from the nasal cavity of a child: a case report. Oral Implantol (Rome) 2012, 5, 21–5. [Google Scholar]
- Kong, J.; Peng, Z.; Zhong, T.; Shu, H.; Wang, J.; Kuang, Y.; Ding, G. Clinical Analysis of Approach Selection of Extraction of Maxillary Embedded Mesiodens in Children. Dis. Markers 2022, 2022, 1–9. [Google Scholar] [CrossRef]
- Kimura, M.; Yasui, T.; Asoda, S.; Nagamine, H.; Soma, T.; Karube, T.; Kodaka, R.; Muraoka, W.; Nakagawa, T.; Onizawa, K. Evaluation of the surgical approach based on impacted position and direction of mesiodens. J. Oral Maxillofac. Surg. Med. Pathol. 2022, 35, 23–29. [Google Scholar] [CrossRef]
- Garcia-Denche, J.T.; Abbushi, A.; Hernández, G.; Fernández-Tresguerres, I.; Lopez-Cabarcos, E.; Tamimi, F. Nasal Floor Elevation for Implant Treatment in the Atrophic Premaxilla: A Within-Patient Comparative Study. Clin. Implant. Dent. Relat. Res. 2014, 17, e520–e530. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, A.; Hanazawa, Y. An effective mesiodens extraction method involving an intraoral approach through the nasal floor bone. Oral Sci. Int. 2019, 16, 193–195. [Google Scholar] [CrossRef]
Figure 1.
Radiological diagnostic methods - conventional 2D radiographs vs CBCT in a case of included mesiodens (A) - lateral cephalometric, (B) – OPG, (C) – CBCT cross-sectional view, (D) – CBCT axial view, (E) – CBCT panorama view, (D) – CBCT 3D reconstruction.
Figure 1.
Radiological diagnostic methods - conventional 2D radiographs vs CBCT in a case of included mesiodens (A) - lateral cephalometric, (B) – OPG, (C) – CBCT cross-sectional view, (D) – CBCT axial view, (E) – CBCT panorama view, (D) – CBCT 3D reconstruction.
Figure 2.
CBCT analysis: (A) - distance from ANS, (B) - angle between the nasal floor line and the axis of the mesiodens, (C) - distance to mesiodens from buccal and palatal aspect, (D) - position regarding the nasopalatine canal.
Figure 2.
CBCT analysis: (A) - distance from ANS, (B) - angle between the nasal floor line and the axis of the mesiodens, (C) - distance to mesiodens from buccal and palatal aspect, (D) - position regarding the nasopalatine canal.
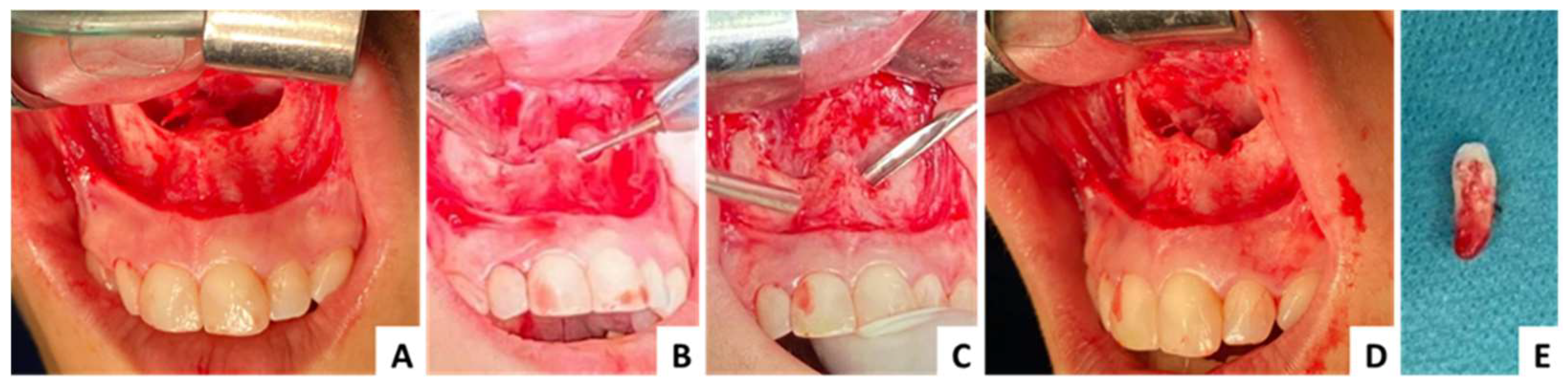
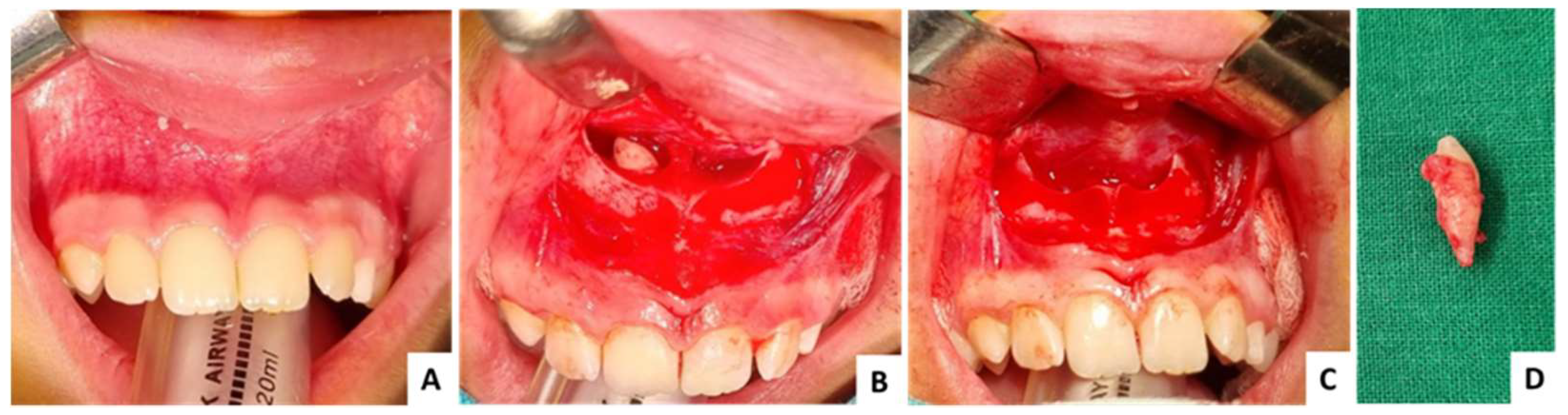
Figure 3.
Case 1 - clinical aspects: (A) - elevation of the mucoperiosteal flap and nasal mucosa, (B) - osteotomy with rotary instruments, (C) - luxation and extraction of the mesiodens using extraction elevators, (D) – intraoperative aspect after extraction, (E) – extracted mesiodens.
Figure 3.
Case 1 - clinical aspects: (A) - elevation of the mucoperiosteal flap and nasal mucosa, (B) - osteotomy with rotary instruments, (C) - luxation and extraction of the mesiodens using extraction elevators, (D) – intraoperative aspect after extraction, (E) – extracted mesiodens.
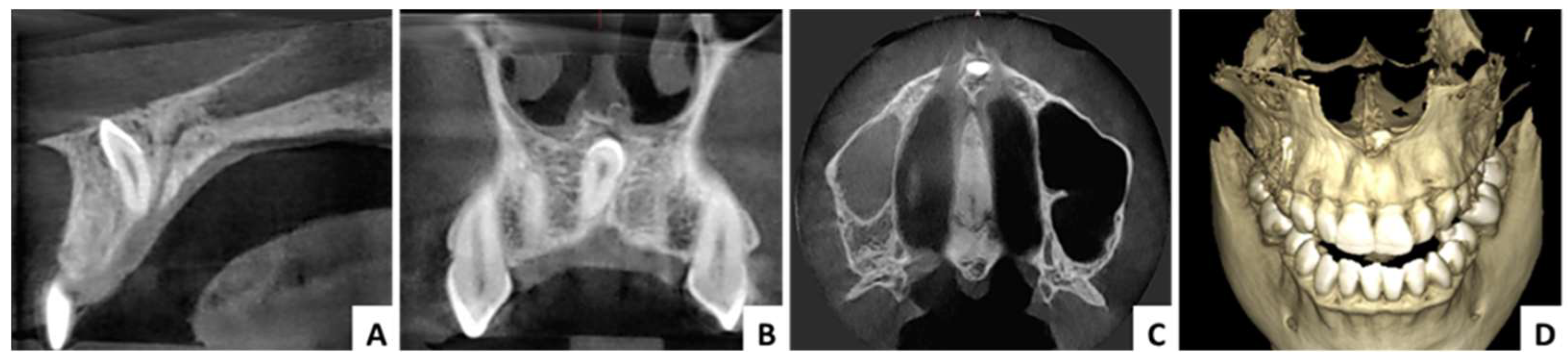
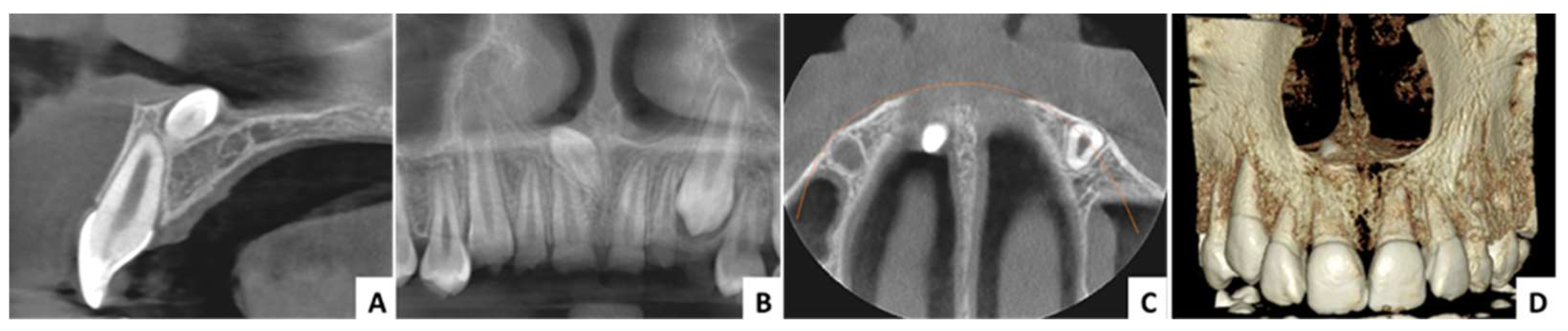
Figure 4.
Case 1 – radiological aspects: (A) - CBCT cross-sectional view, (B) – CBCT panorama view, (C) – CBCT axial view, (D) – CBCT 3D reconstruction.
Figure 4.
Case 1 – radiological aspects: (A) - CBCT cross-sectional view, (B) – CBCT panorama view, (C) – CBCT axial view, (D) – CBCT 3D reconstruction.
Figure 5.
Case 1 - Follow-up OPG, three years after surgery.
Figure 5.
Case 1 - Follow-up OPG, three years after surgery.
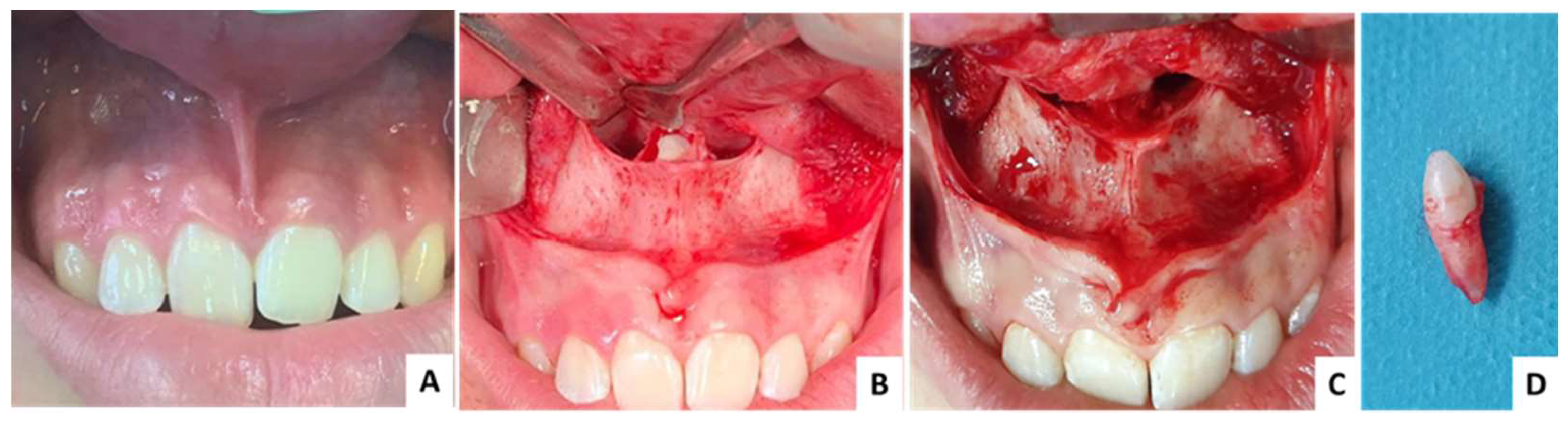
Figure 6.
Case 2 - clinical aspects: (A) – initial clinical aspect, no symptoms recorded, (B) – exposed mesiodens, (C)- intraoperative aspect after extraction, (D) – extracted mesiodens.
Figure 6.
Case 2 - clinical aspects: (A) – initial clinical aspect, no symptoms recorded, (B) – exposed mesiodens, (C)- intraoperative aspect after extraction, (D) – extracted mesiodens.
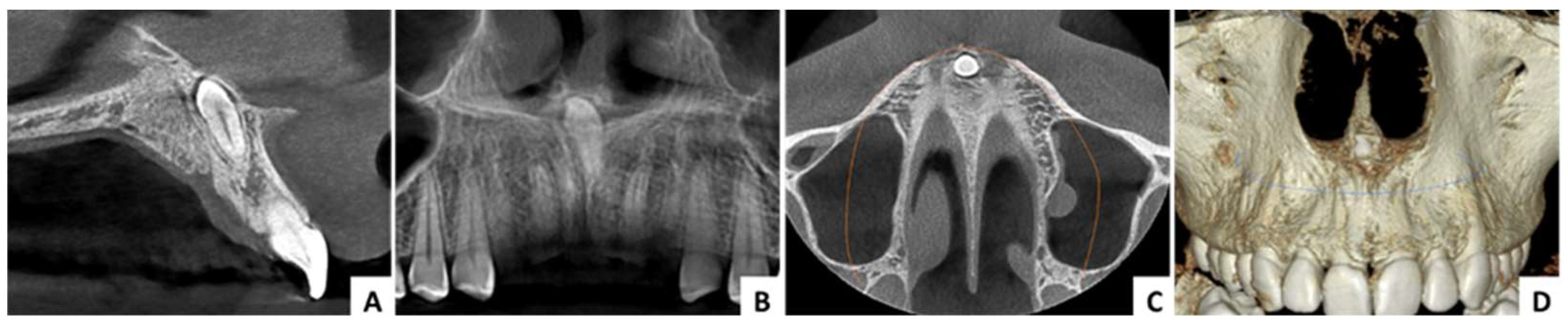
Figure 7.
Case 2 – radiological aspects: (A) - CBCT cross-sectional view, (B) – CBCT panorama view, (C) – CBCT axial view, (D) – CBCT 3D reconstruction.
Figure 7.
Case 2 – radiological aspects: (A) - CBCT cross-sectional view, (B) – CBCT panorama view, (C) – CBCT axial view, (D) – CBCT 3D reconstruction.
Figure 8.
Case 2 - Follow-up OPG, three years after surgery.
Figure 8.
Case 2 - Follow-up OPG, three years after surgery.
Figure 9.
Case 3 - clinical aspects: (A) – initial clinical aspect, no symptoms recorded, (B) – exposed mesiodens, (C)- intraoperative aspect after extraction, (D) – extracted mesiodens.
Figure 9.
Case 3 - clinical aspects: (A) – initial clinical aspect, no symptoms recorded, (B) – exposed mesiodens, (C)- intraoperative aspect after extraction, (D) – extracted mesiodens.
Figure 10.
Case 3 – radiological aspects: (A) - CBCT cross-sectional view, (B) – CBCT panorama view, (C) – CBCT axial view, (D) – CBCT 3D reconstruction.
Figure 10.
Case 3 – radiological aspects: (A) - CBCT cross-sectional view, (B) – CBCT panorama view, (C) – CBCT axial view, (D) – CBCT 3D reconstruction.
Figure 11.
Case 3 - Follow-up OPG, three years after surgery.
Figure 11.
Case 3 - Follow-up OPG, three years after surgery.
Table 1.
The basic steps in the diagnosis process for impacted mesiodens.
Table 1.
The basic steps in the diagnosis process for impacted mesiodens.
| Diagnosis process |
Observations |
| Clinical examination |
The inverted mesiodens is mainly asymptomatic but in some cases can cause midline displacement, diastema, rotation, delayed eruption of permanent teeth, crowding or spacing of the anterior teeth. |
| Convetional radiography (OPG, occlusal, periapical, lateral cephalometric radiographs) |
In case of convetional 2D radiographs, mainly OPG, the structures outside the focal area may be totally obscured by other structures and do not appear. Also, the precise localization relative to neighboring structures and teeth of some mesiodens would require the use of an additional occlusal radiography. |
| Cone-beam computed tomography (CBCT) |
CBCT is a 3D imaging technique and an excellent method of evaluation and diagnosis. It has a fundamental role in the precise localization of the mesiodens, the connection with the neighboring anatomical structures and teeth. Thus, has an important role in choosing the appropriate surgical procedure. |
Table 2.
Determination of the surgical approach.
Table 2.
Determination of the surgical approach.
| Criteria |
Observations |
| Distance to the mesiodens |
It is preferable to use the approach that offers the shortest distance to the included mesiodens |
| Surgical field |
The traditional buccal approach provides an excellent surgical view compared with the palatal approach. It has its limitations due to the fact that the included mesiodens is found predominantly on the palatal side. The nasal floor approach can also provide a good direct view of the surgical site. |
| Osteotomy |
Extensive osteotomy should be avoided because it may lead to an increase in intraoperative accidents and postoperative complications. Osteotomy in the anterior maxillary is likely to exacerbate postoperative swelling and pain. The nasal floor approach can prevent excessive removal of palatal or buccal bone to access the inverted mesiodens. |
| Neighboring teeth |
Included mesiodens mostly develops on the palatal side. The traditional buccal approach carries a high risk of damaging the roots of the permanent incisors. For this reason, a palatal approach for surgical extraction is preferred. |
| Neurovascular injury |
The palatal approach carries a high risk of neurovascular injury to the nasopalatine nerve, especially when the mesiodens is positioned in front of the nasopalatine canal. |
| Operation time |
Prolonged operation time can decrease the blood supply and pulp vitality of the adjacent teeth. Also, in these cases, postoperative swelling and pain will be significantly exacerbated. |
| Patient postoperative discomfort |
There is no generally accepted surgical procedure to minimize surgery injury for inverted mesiodens, but limited osteotomy and short operation time can lead to a significant decrease in postoperative swelling and pain. |
Table 3.
Results.
| Case no. |
1 |
2 |
3 |
| Age (years)/Sex |
29/F |
11/M |
16/M |
| Angle between the nasal floor line and the axis of the mesiodens |
85.93° |
143.5° |
144.4° |
| Distance from ANS (mm) |
8.98 |
8.11 |
13.22 |
|
Distance to mesiodens from buccal aspect(mm)
|
4.71 |
3.70 |
3.84 |
| Distance to mesiodens from palatal aspect (mm) |
6.43 |
5.47 |
6.82 |
| Relation with nasal cavity |
Covered with bone |
Submucosally |
Covered with bone |
| Position regarding nasopalatine canal |
In front |
In front |
In front |
| Operation time (minutes) |
30 |
28 |
31 |
| Complications |
No |
No |
No |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).