Submitted:
04 December 2024
Posted:
05 December 2024
You are already at the latest version
Abstract
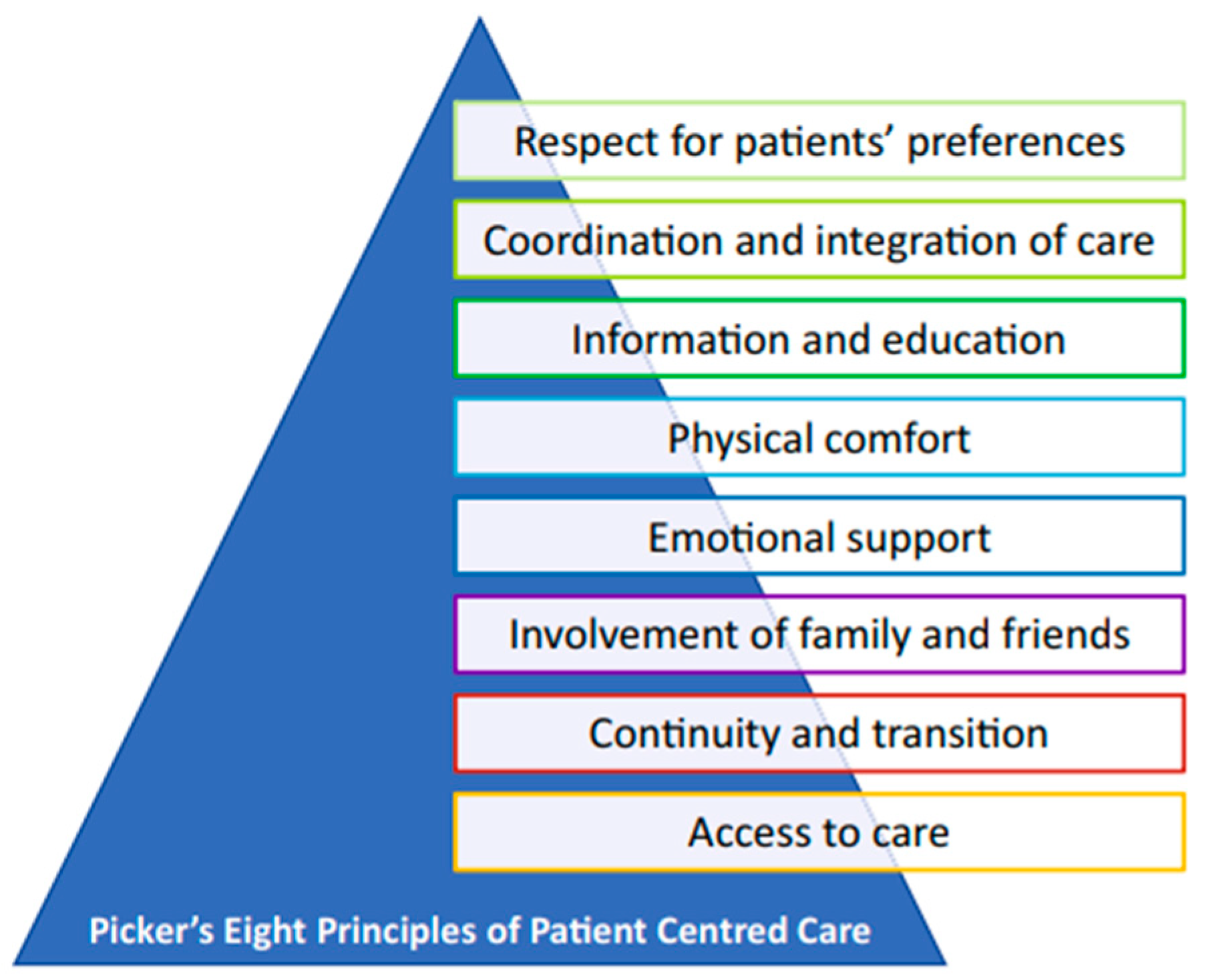
Patient-centered care (PCC) as a philosophy is defined as the provision of care with an emphasis on the person. Patient-centered care is important enough to be one part of the coordination and collaboration efforts of the WHO strategy to eradicate tuberculosis. Patient-centered care is concerned with increasing patient empowerment and understanding of the tuberculosis treatment programme. Tuberculosis treatment adherence can be achieved through several strategies using a multicomponent strategy that includes patient and family education, utilising digital health media, and implementing individualised management.
Keywords:
Introduction
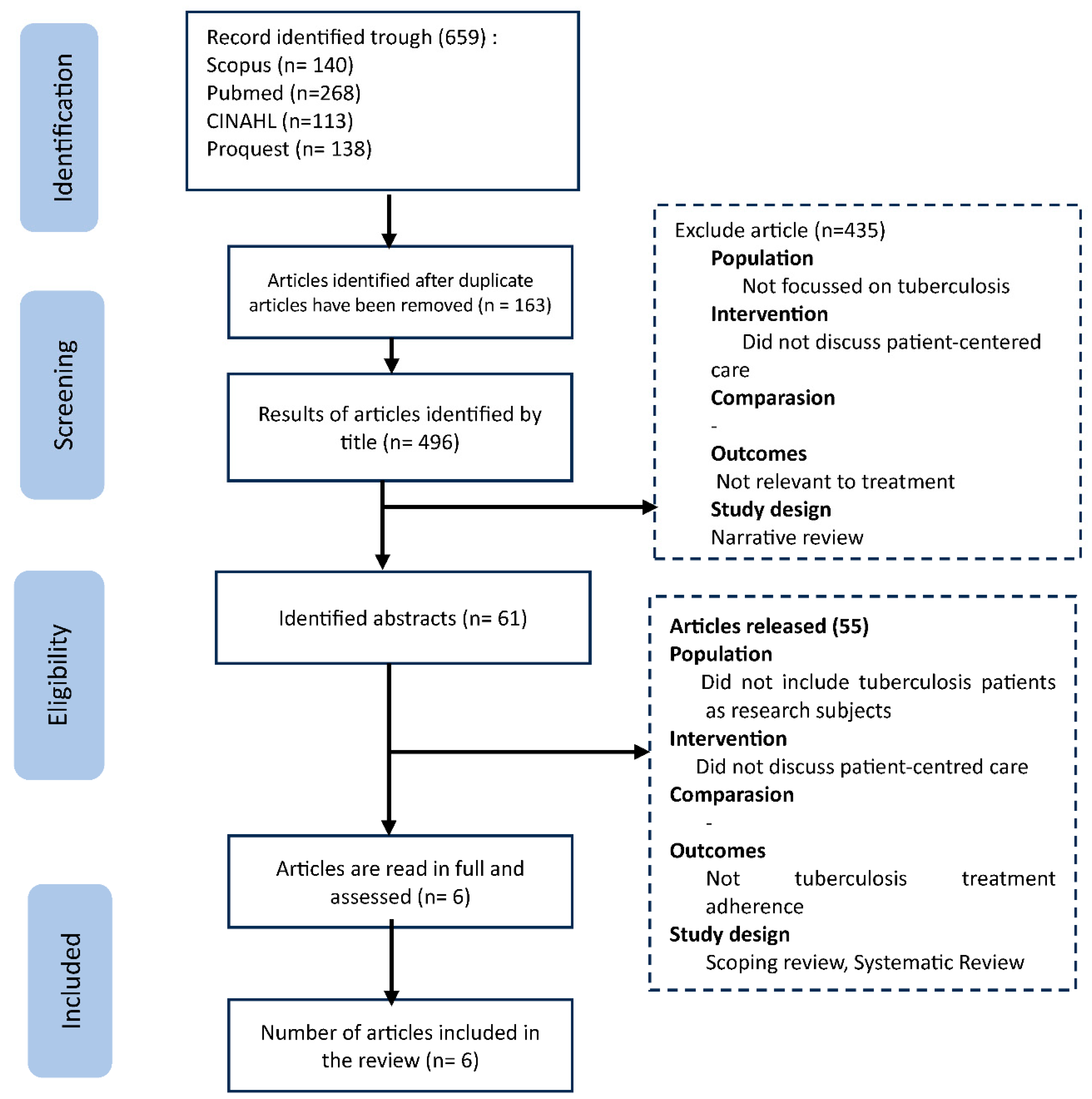
Method
| Participants/population | Population limited to patients with tuberculosis |
| Intervention/Interst | Knowing medication adherence |
| Comparison | Research conducted in developed, developing and poor countries |
| Outcomes | Exploring patient-centred care factors in medication adherence |
| Study design | Randomized controlled trail, pra-eksperimental design and observasional study |
| No | Title and Author | Methods | Hasil Penelitian |
|---|---|---|---|
| 1 |
Effect of a phone reminder system on patient- centered tuberculosis treatment adherence among adults in Northwest Ethiopia: a randomised controlled trial (Gashu, Gelaye, Lester, et al., 2021) |
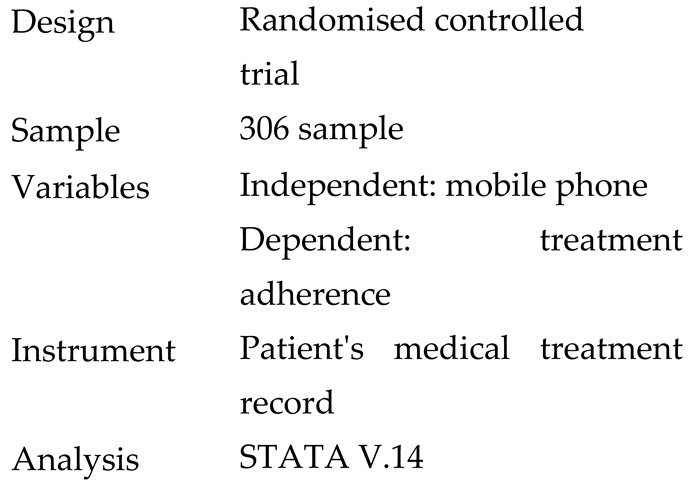 |
The use of a mobile phone with a daily medication reminder system improved adherence to patient-centred TB treatment and provider-patient relationships; however, there was no significant effect on treatment success. |
| 2 |
Patient-centered mobile tuberculosis treatment support tools (TB-TSTs) to improve treatment adherence: A pilot randomized controlled trial exploring feasibility, acceptability and refinement needs (Iribarren et al., 2022) |
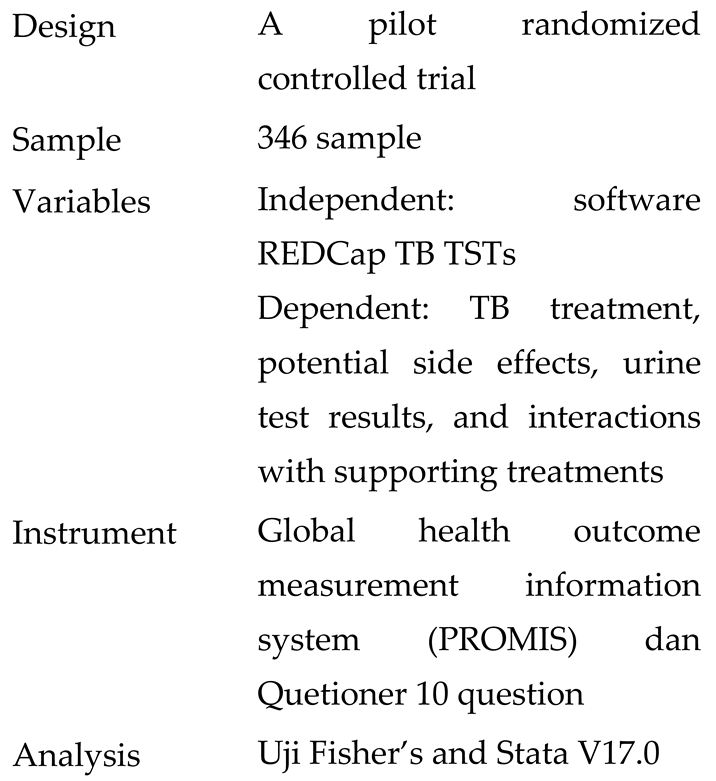 |
The results of this study show that the device is easy to use and can be recommended to support the successful treatment of tuberculosis patients. |
| 3 |
Specific Interventions for Implementing a Patient-Centered Approach to TB Care in Low-Incidence Cities (Pujol-Cruells & Vilaplana, 2019) |
 |
Patient-centred management of tuberculosis is recommended by the WHO, but needs to be implemented regularly with a structured work protocol. |
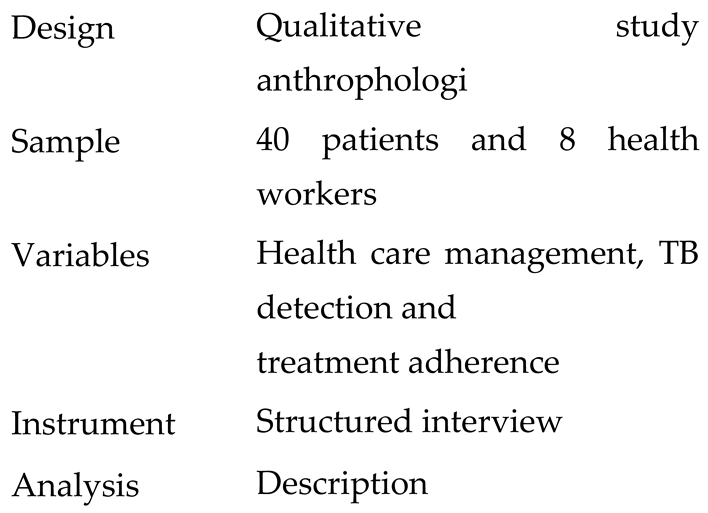
| 4 | Person-centred care in practice: perspectives from a short course regimen for multi-drug resistant tuberculosis in Karakalpakstan, Uzbekistan (Horter et al., 2020) |
 |
Patients with MDR-TB are not used to shared decision-making and feel uncomfortable taking responsibility for their treatment choices. Healthcare professionals are perceived to have greater knowledge and expertise, and patients trust healthcare professionals to act in their best interest, |
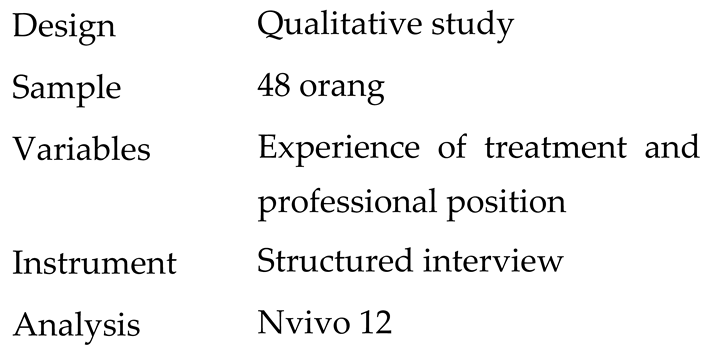
| 5 | “A very humiliating illness”: a qualitative study of patient-centered Care for Rifampicin-Resistant Tuberculosis in South Africa (Furin et al., 2020) |
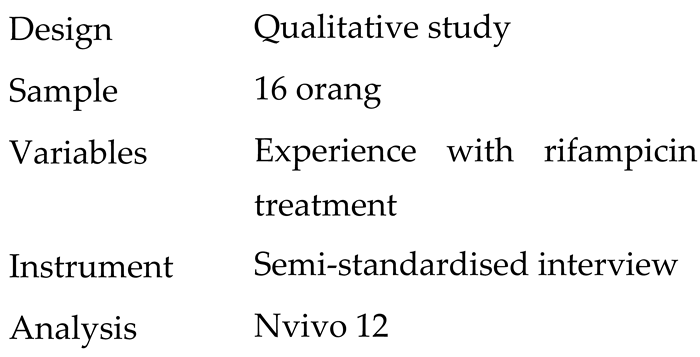 |
Rifampicin-resistant TB robs people of their physical, social, economic, psychological, and emotional well-being far beyond the period when treatment is administered. Efforts to address this issue are as important as new drugs and diagnostics in the fight against TB. |
| 6 | Adherence to TB treatment remains low during continuation phase among adult patients in Northwest Ethiopia (Gashu, Gelaye, & Tilahun, 2021) |
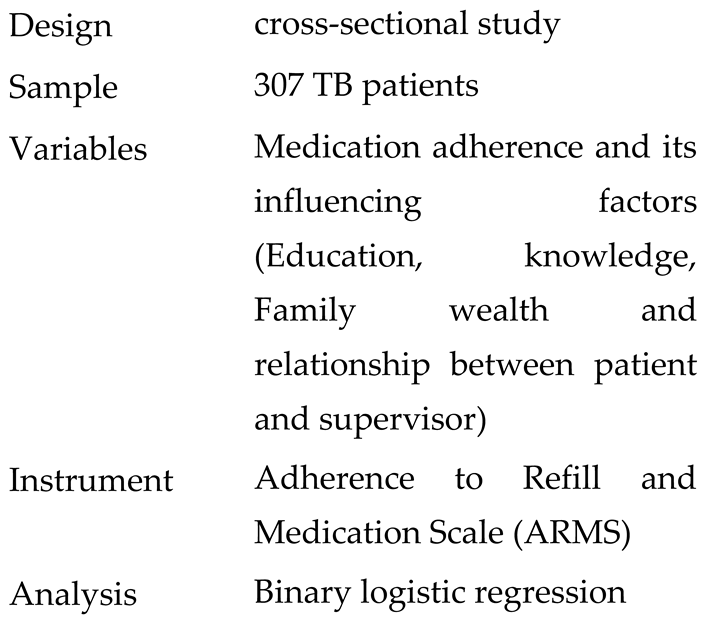 |
Patient adherence to TB treatment remains low during the continuation phase. There was a positive association between education level, knowledge, family wealth, and provider-patient relationship with patient adherence. with patient adherence. Forgetfulness, travelling far, and feeling sick were the main reasons for non-adherence. adherence to TB treatment. |
Results and Discussion
Ontology of Patient Centered Care on Treatment Adherence Tuberculosis Patients
Epistemiology of Patient Centered Care on Treatment Adherence Tuberculosis Patients
Aksiologi of Patient Centered Care on Treatment Adherence Tuberculosis Patients
Conclusion
References
- Alele, F., & Aduli, B. M. (2023). An introduction to research methods for undergraduate health profesional students. James Cook University.
- Bachnick, S., Ausserhofer, D., Baernholdt, M., & Simon, M. (2018). Patient-centered care, nurse work environment and implicit rationing of nursing care in Swiss acute care hospitals: A cross-sectional multi-center study. International Journal of Nursing Studies, 81(November 2017), 98–106. [CrossRef]
- Barrett, M., Boyne, J., Brandts, J., Brunner-La Rocca, H. P., De Maesschalck, L., De Wit, K., Dixon, L., Eurlings, C., Fitzsimons, D., Golubnitschaja, O., Hageman, A., Heemskerk, F., Hintzen, A., Helms, T. M., Hill, L., Hoedemakers, T., Marx, N., McDonald, K., Mertens, M., … Zippel-Schultz, B. (2019). Artificial intelligence supported patient self-care in chronic heart failure: a paradigm shift from reactive to predictive, preventive and personalised care. EPMA Journal, 10(4), 445–464. [CrossRef]
- Boyarchuk, O. R., & Antoniuk, I. M. (2023). A patient-centered care for the management of children with rare diseases: collaboration between physicians, nurses, and patients. Child’s Health, 18(6), 458–464. [CrossRef]
- Bruzual, A. D. (2018). Person-centered medicine. Gaceta Medica de Caracas, 126(1), 40–51.
- Dіachuk, D. D., Moroz, G. Z., Hidzynska, I. M., & Kravchenko, A. M. (2023). Implementation of Patient-Centered Care and Medical Care Improvement: Current State (Review). Clinical and Preventive Medicine, 1(23), 67–77. [CrossRef]
- Epstein, R. M., & Street, R. L. (2011). The Values and Value of Patient-Centered. 9(2), 100–103. [CrossRef]
- Eryong, L., Qinglin, M., Qian, W., Jing, W., & Lin, Z. (2022). Interpretation of WHO Guidelines on tuberculosis care and support. Chinese Journal of Antituberculosis, 44(12), 1449–1259.
- Frezza, E. (2019). Patient-Centered Healthcare: Transforming the Relationship Between Physicians and Patients (1st ed.) (1st Editio). Productivity Press. [CrossRef]
- Furin, J., Loveday, M., Hlangu, S., Dickson-hall, L., Roux, S., Nicol, M., & Cox, H. (2020). “ A very humiliating illness ” : a qualitative study of patient-centered Care for Rifampicin-Resistant Tuberculosis in South Africa. 1–11.
- Gashu, K. D., Gelaye, K. A., Lester, R., & Tilahun, B. (2021). Effect of a phone reminder system on patient-centered tuberculosis treatment adherence among adults in northwest ethiopia: A randomised controlled trial. BMJ Health and Care Informatics, 28(1), 1–10. [CrossRef]
- Gashu, K. D., Gelaye, K. A., & Tilahun, B. (2021). Adherence to TB treatment remains low during continuation phase among adult patients in Northwest Ethiopia. BMC Infectious Diseases, 21(1), 1–11. [CrossRef]
- Gluyas, H. (2015). Patient-centred care: improving healthcare outcomes. Continuing Professional Development, 151, 10–17.
- Goldfarb, M. J., Saylor, M. A., Bozkurt, B., Code, J., Di Palo, K. E., Durante, A., Flanary, K., Masterson Creber, R., Ogunniyi, M. O., Rodriguez, F., & Gulati, M. (2024). Patient-Centered Adult Cardiovascular Care: A Scientific Statement From the American Heart Association. Circulation, 149(20), E1176–E1188. [CrossRef]
- Guarnier, T. S., Das G. Da Silva Teixeira, M., Dos R. Costa, D., Dos Santos, A. S., Bubach, S., Sales, C. M. ., & Das D. Rissino, S. (2021). Tuberculosis diagnosis - An ontology-driven conceptual model. CEUR Workshop Proceedings.
- Hanlie Myburgh, I., Baloyi, D., Id, M. L., Id, S. M., Osman, M., Wademan, D., Hesseling, A., & Hoddinott, G. (2023). PLOS GLOBAL PUBLIC HEALTH A scoping review of patient-centred tuberculosis care interventions : Gaps and opportunities. 1–16. [CrossRef]
- Horter, S., Daftary, A., Keam, T., Bernays, S., Bhanushali, K., Chavan, D., Denholm, J., Furin, J., Jaramillo, E., Khan, A., Lin, Y. D., Lobo, R., Loveday, M., Majumdar, S. S., Mistry, N., Patel, H., Rane, S., Swaminathan, A., Triasih, R., … du Cros, P. (2021). Person-centred care in TB. International Journal of Tuberculosis and Lung Disease, 25(10), 784–787. [CrossRef]
- Horter, S., Stringer, B., Gray, N., Parpieva, N., Safaev, K., Tigay, Z., Singh, J., & Achar, J. (2020). Person-centred care in practice : perspectives from a short course regimen for multi-drug resistant tuberculosis in. 1–11.
- Iribarren, S. J., Milligan, H., Chirico, C., Goodwin, K., Schnall, R., Telles, H., Iannizzotto, A., Sanjurjo, M., Lutz, B. R., Pike, K., Rubinstein, F., Rhodehamel, M., Leon, D., Keyes, J., & Demiris, G. (2022). Patient-centered mobile tuberculosis treatment support tools (TB-TSTs) to improve treatment adherence: A pilot randomized controlled trial exploring feasibility, acceptability and refinement needs. The Lancet Regional Health - Americas, 13, 100291. [CrossRef]
- Isaac KS, N. (2024). Physicians, know thy patient. Journal of the Royal College of Physicians of Edinburgh, 54(1), 84–88.
- Jaramillo, J., Yadav, R., & Herrera, R. (2019). Why every word counts : towards patient- and people-centered tuberculosis care. 23(1100), 547–551.
- Khachadourian, V., Truzyan, N., Harutyunyan, A., Thompson, M. E., Harutyunyan, T., & Petrosyan, V. (2015). People-centered tuberculosis care versus standard directly observed therapy: Study protocol for a cluster randomized controlled trial. Trials, 16(1), 1–7. [CrossRef]
- Martín, D., Barbosa, P., Ramos, J. P., Vieira, M., & Duarte, R. (2024). People first: a participatory community approach on patient-reported outcomes in tuberculosis. Breathe, 20(1). [CrossRef]
- Migliori, G. B. (2021). Essential Tuberculosis (M. C. Raviglione (ed.)). Springer Nature Switzerland AG.
- Mkopi, A., Range, N., Amuri, M., Geubbels, E., Lwilla, F., Egwaga, S., Schulze, A., & Van Leth, F. (2013). Health workers’ performance in the implementation of Patient Centred Tuberculosis Treatment (PCT) strategy under programmatic conditions in Tanzania: A cross sectional study. BMC Health Services Research, 13(1), 1–7. [CrossRef]
- Mkopi, A., Range, N., Lwilla, F., Egwaga, S., Schulze, A., Geubbels, E., & van Leth, F. (2012). Adherence to Tuberculosis Therapy among Patients Receiving Home-Based Directly Observed Treatment: Evidence from the United Republic of Tanzania. PLoS ONE, 7(12), 1–7. [CrossRef]
- Olukunle A, O., Deshendran, M., Anban W, P., & Christopher, S. (2015). An Ontology for Tuberculosis Treatment Adherence Behaviour. ACM International Conference Proceeding Series.
- Pujol-Cruells, A., & Vilaplana, C. (2019). Specific Interventions for Implementing a Patient-Centered Approach to TB Care in Low-Incidence Cities. Frontiers in Medicine, 6(November), 1–8. [CrossRef]
- Ren, J., Han, D., Zhang, J., Wang, Y., Huang, Q., Tian, T., & Li, X. (2021). Development and psychometric testing of the supportive care needs scale for patients with tuberculosis (Scn-tb). Patient Preference and Adherence, 15, 2267–2278. [CrossRef]
- Snyman, L., E., V., Duran, L. T., E., M., V.D., A., X, H., & P., I. (2018). “I didn’t know so many people cared about me”: Support for patients who interrupt drug-resistant TB treatment. International Journal of Tuberculosis and Lung Disease, 22(9), 1023–1030. [CrossRef]
- Staden, V., & Werdie, C. (2023). Holistic framework in person centered medicine. Person Centered Medicin, 83–103.
- Walsh, A., Bodaghkhani, E., Etchegary, H., Alcock, L., Patey, C., Senior, D., & Asghari, S. (2022). Patient-centered care in the emergency department: a systematic review and meta-ethnographic synthesis. International Journal of Emergency Medicine, 15(1), 1–12. [CrossRef]
- Wedemire, C., Brody, R., & Ganzer, H. (2022). Integration of patient-centered care in nutrition support decision-making: A case report. Nutrition in Clinical Practice, 37(1), 209–214. [CrossRef]
- Global Tuberculosis Report.
- WHO. (2024). Global tuberculosis report 2024.
- Wildana, W. (2018). BAB 1 faktor yang berhubungan dengan status gizi pada penderita tuberkulosis paru di. Energies, 6(1), 1–8. http://journals.sagepub.com/doi/10.1177/1120700020921110%0Ahttps://doi.org/10.1016/j.reuma.2018.06.001%0Ahttps://doi.org/10.1016/j.arth.2018.03.044%0Ahttps://reader.elsevier.com/reader/sd/pii/S1063458420300078?token=C039B8B13922A2079230DC9AF11A333E295FCD8.
- Worth Health Organization. (2021). Global Tuberculosis Report. World Health Organization.
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





