1. Introduction
Over the past decade, the occurrence of dysglycemia- which encompasses both diabetes and high blood sugar levels approaching those of diabetes (referred to as prediabetes) - has seen a 50% increase in Canada, and this trend is anticipated to persist [
1,
2,
3]. Currently, one out of every three Canadians has some level of dysglycemia. The rate of diabetes has risen more significantly among younger adults (ages 20–49) than among older adults (ages 50 and above) both in Ontario and across Canada [
1,
3,
4]. Young adults diagnosed with diabetes at an early age exhibit a distinct and more severe disease process compared to their older counterparts, requiring more immediate and intensive interventions to manage blood sugar levels [
5,
6].
Researchers report diabetes as colour-coded, meaning it disproportionately affects certain ethnocultural groups such as Blacks and South Asians. This group is vulnerable, even if they do not think they are (i.e. they are vulnerable but unaware). Evidence supports this report, as Black Canadians have faced a doubling of diabetes prevalence in the last decade [
7]. Although there is substantial evidence of the increased risk of diabetes in the Black Canadian population, there is scanty research on the Black population aged 18-39 years. Diabetes Canada recommends universal glycated hemoglobin A1c (HbA1c) cut-offs for diagnosing diabetes; however, studies suggest ethno-cultural adaptability for HbA1c as a diagnostic tool [
8]. Current diabetes diagnoses rely on a cut-off of 6.5% [
9,
10]. The benefits of HbA1c for diabetes diagnosis are numerous, including the fact that there are no set time of day requirements and no special preparations. In addition to HbA1c tests, other tests, such as fasting plasma glucose (FPG) and oral glucose tolerance tests (OGTT), are used for diabetes diagnosis [
3,
10]. FPG requires long fasting hours, which is not always appreciated.
Cultural Relativism and Diabetes
Even though culture and ethnicity are not interchangeable; however, for operational purposes, we used Black Afro-Canadian or Caribbean-Canadian ethnicity as a proxy for the culture of ACB individuals in this study to understand the trend and distribution of dysglycaemia in them [
11] and their behavioural pattern. Among young adults who face more severe disease progression, racial and ethnic minority populations face an even greater burden [
12]. Over the past decade, the cases of diabetes among Black Canadians have seen a twofold increase, with data indicating that Black individuals are twice as likely to develop diabetes compared to other populations [
7,
13,
14,
15]. In Ontario, self-reported diabetes prevalence is 8.5% in Black individuals, which is double the rate of 4.2% observed in White individuals [
7]. Beyond the higher prevalence of diabetes, Black communities face higher rates of complications, including hypertension, retinopathy and kidney disease [
7]. Furthermore, previous scholarly work in this regard has suggested that immigrants of specific ethnic groups, such as South Asians, Chinese, and Blacks, develop diabetes and other metabolic disorders at a higher rate, at an earlier age, and with lower ranges of body mass index (BMI) [
16,
17]. Despite this risk discrepancy between the Black minority and non-minority populations, current glycated hemoglobin A1c (HbA1c) cutoffs remain non-specific in evaluating the glycemic status of ABC communities [
18]. Evidently, the increasing prevalence of diabetes in Black populations is the result of intersections between possible biological differences and access to economic, social and cultural factors [
19]. These intersections highlight that adequate detection, evaluation and mitigation of dysglycemia in the ABC population requires the incorporation of cultural relativity.
Incorporating cultural relativity in diabetes diagnoses allows for early and accurate identification and subsequent mitigation of dysglycemia. This is because cultural characteristics influence illness perceptions and, thus, behaviour [
11]. Early detection of diabetes risk using a culturally relative lens can enhance disease management and lower the chances of developing complications, thereby alleviating some of the disease’s adverse health effects [
11,
20]. Additionally, identifying risk factors and adopting healthier and culturally appropriate lifestyle habits can delay or even prevent the onset of diabetes in those identified with prediabetes [
21], which is a critical public health demand. However, many people with prediabetes or in the initial phases of diabetes do not show symptoms, and this is exacerbated in Black communities, leading to delayed diagnosis and treatment [
3,
22,
23].
The prevalence of dysglycemia is increasing in the ACB community. At the same time, culturally acceptable screening measures are not comprehensive and tailored to address this population’s unique health challenges and lifestyle factors. The Public Health Agency of Canada (PHAC) and the Canadian Task Force of Preventive Health Care developed the Canadian Diabetes Risk Questionnaire (CANRISK) tool to screen diabetes in asymptomatic people. The CANRISK tool is adapted from other diabetes questionnaires that included predictive variables such as the ethnic origin of biological parents and questions related to family history. This tool is cost-effective and helpful in identifying high-risk individuals and prompting further tests [
24]. Although widely accepted, some ethnic subgroups, like young Black Canadians, are under-represented in this tool.
In that context, the study selected these research questions:
What is the percentage of ACB residents (Toronto) aged 18–39 years old who have diabetes and prediabetes?
What risks are identified in this population that influence blood sugar levels?
Is HbA1c a more sensitive and culturally acceptable test than OGTT to diagnose diabetes in ACB communities?
What are the recommendations for framing a culturally acceptable diabetes education protocol for ethnic populations?
2. Methods
This descriptive study collected data between June 2023 and September 2024 to measure the distribution of diabetes and prediabetes among ACB individuals aged 18-39 years in Toronto (Canada) and identify the risks of prediabetes and diabetes among them [
25]. This study used a mixed-method approach (quantitative, qualitative, and blood work) to collect data [
26]. The Public Health Research Ethics Board approved this study protocol for dealing with human participants.
2.1. Participant Recruitment
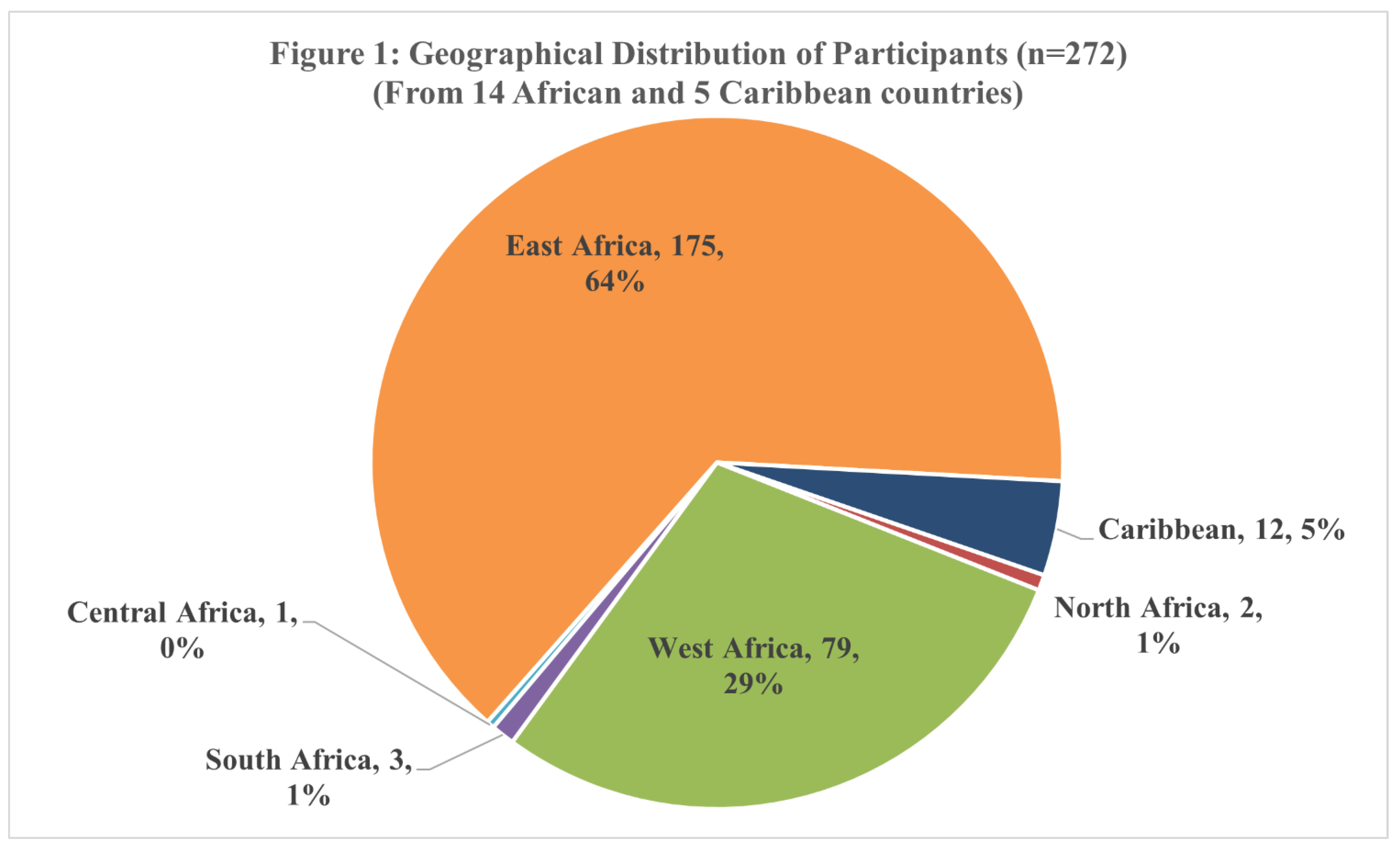
Participants included Black Toronto residents aged between 18 and 39 years who self-identified as of African and Caribbean ancestry. Study participants (n=272) were recruited through community engagement, outreach, flyers and peer-to-peer referrals using a purposive heterogeneous sampling technique to ensure a maximal variation of samples [
27,
28]. This technique allowed for representation of broader ethnic and geographic diversity, inlcuding14 African countries of five regions (East, West, Central, North, and South) and five Caribbean countries (
Figure 1). Participants’ countries of origin were Côte d’Ivoire, Ghana, Nigeria, Chad, Ethiopia, Kenya, Rwanda, Tanzania, Uganda, South Sudan, Cameroon, Angola, South Africa, and Zimbabwe. Caribbean immigrants were from the islands of the Caribbean Sea (Bahamas, Barbados, Guyana, Jamaica, St. Vincent) [
29].
Participants were excluded if they had a previous diagnosis of diabetes with or without medication, if they were not in a physical state to travel to the centre, or if they were not in a mental state to understand or give informed consent, and if they were pregnant.
2.2. Data Collection
After screening for eligibility and receiving informed consent, the trained Peer Researcher (PR) recruited 272 participants. The PR (OM- a Black African physician immigrant) and a volunteer (SN- a Black African medical student) measured height, weight, waist circumference, and blood pressure. The participants were guided to a standard blood testing laboratory in the same building (LifeLabs) for measuring HbA1c and Oral Glucose Tolerance Test (OGTT) following the standard protocol of the Public Health Agency of Canada (PHAC). When the participant had to wait for two hours for the second blood sample for OGTT, the PR collected demographic, behavioural, and lifestyle data from the participants using the self-reported CANRISK tool.
2.3. Diagnoses Thresholds
Based on the Diabetes Canada Guideline, prediabetes was labelled as a Fasting Plasma Glucose (FPG) of 6.1- 6.9 mmol/L, or two hours after a glucose drink (2hPG) of 7.8 - 11.0 mmol/L or glycated hemoglobin (HbA1c) of 6.0% - 6.4% [
9]. The same guideline defined diabetes as an FPG of 7.0 mmol/L or higher, a 2hPG of 11.1 mmol/L or higher, or an HbA1c of 6.5% or higher [
9].
2.4. Single-Subject Research Design
To capture more in-depth information (exploratory sequential approach) about any missing diabetes-related attributable behaviour of the ACB individuals, a single-subject research design was adopted to follow up on 41 (n=41) randomly selected participants (out of the 272) from three subgroups (i) at-risk group (ii) prediabetes group, and (iii) diabetes group [
30]. These qualitative data on influencing behavioural and social factors were analyzed following an Interpretive Phenomenological Analysis protocol [
31]. This longitudinal feature, which was subsequently added to the cross-sectional study design, adds to the mixed-method nature of this research study [
26].
2.5. Data Analysis
Quantitative data was analyzed using the International Machine Business Corporation Statistical Package for the Social Sciences (IBM SPSS) software 29.0.2.0 (20). ANOVA and Regression analyses were done to find any relationships between blood sugar and anthropometric, demographic, or behavioural variables. The qualitative data was analyzed manually using Braun and Clarke’s reflexive thematic approach [
32]. The behavioural and social factors data were analyzed using an interpretive phenomenological analysis (IPA) protocol [
31]. IPA explores details on personal lived experiences and how people explain those experiences as their life events. The next step was triangulating quantitative and qualitative data to interpret the themes and relationships.
3. RESULTS
3.1. Demographic and Geographical Distribution
The mean age of the participants (N=272) was 30.8 ± 4.9 years (ranging between 18 and 39 years), including 38.2% of participants aged between 18 and 29 years and 61.8% between 30 and 39 years (
Table 1). In this study, 65.8% of the participants self-identified as women, 34.2% as men, and none identified as non-binary (
Table 1).
3.2. Glycated Haemoglobin (HbA1c) and Oral Glucose Tolerance Test (OGTT)
The mean HbA1c for these participants was 5.5% ± 0.5 (range 4.2% - 10.0%) (
Table 2). Based on HbA1c levels, 1.5% (n=4) participants were found to have diabetes, 9.2% (n=25) had pre-diabetes, 44.9% (n=122) were at risk for diabetes/pre-diabetes, and 44.5% (n=121) were normal (
Table 3).
The mean FPG value was 4.8 ± 0.6 mmol/L (range 3.5 - 10.1 mmol/L) (
Table 2). This measure identified 1.5% (n=4) participants as having diabetes, 2.6% (n=7) participants as having pre-diabetes, and 96.0% (n=261) participants as being normal or at risk for diabetes/pre-diabetes (
Table 3).
The mean 2hPG after 75 g glucose intake was 5.7 ± 1.6 mmol/L (range 3.3 - 17.1 mmol/L) (
Table 2). Based on 2hPG levels, 1.5% (n=4) participants were found to have diabetes, 7.0% (n=19) participants were found to have prediabetes, and 91.5% (n=249) were found to be normal or at risk for diabetes/pre-diabetes (
Table 3).
The mean height of the participants was 166.2 ± 8.7 cm (range 144.1 - 198.6 cm) (
Table 2). The mean body weight was 78.0 ± 17.3 kg (range 37.5 - 146.2 kg) (
Table 2). The mean BMI was 28.2 ± 5.8 kg/m2 (range 15.8 – 51.5 kg/m2) (
Table 2). The mean waist circumference (WC) was 85.8 ± 13.1 cm (range 56.5 - 132.0 cm) (
Table 2).
Table 3 indicates that HbA1c captured all cases of diabetes as identified by OGTT (FBS and 2hPG), more cases of prediabetes (9.2% by HbA1c VS 2.6% by FBS and 7.0% by 2hPG) and more cases of at-risk individuals (44.9% by HbA1c VS 3.7% by FBS). This means HbA1c has the same level of specificity as OGTT but a higher level of sensitivity to screen populations at risk to prevent end-organ damage (micro and macrovascular consequences) by early diagnosis and prevention.
3.3. Identified Risk Factors
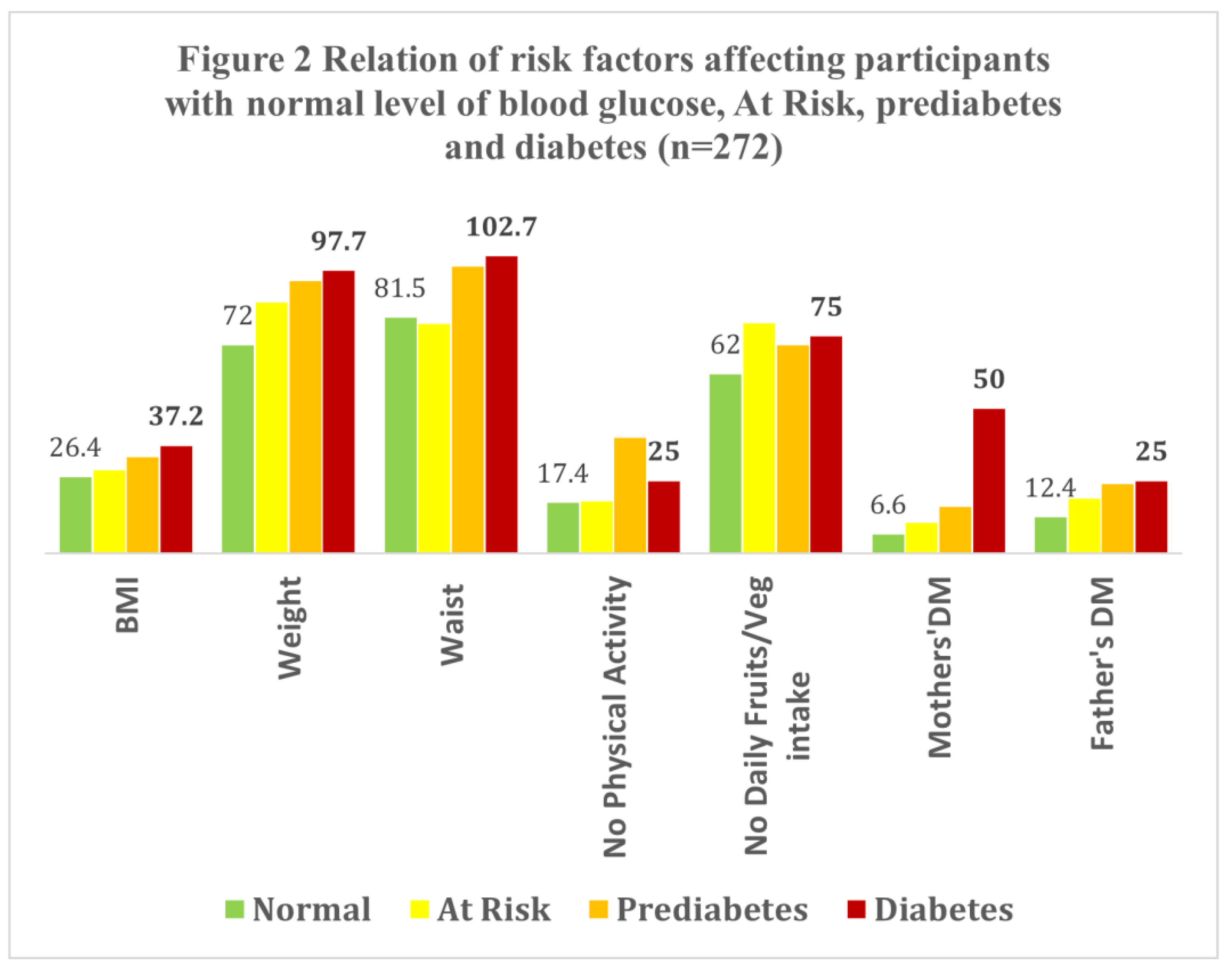
Figure 2 indicates a linear trend of the severity of glucose intolerance with increasing Body Mass Index (BMI), weight, and waist circumference. For participants with diabetes, 50% of mothers and 25% of fathers had a history of having diabetes. In comparison, 16% of mothers of participants with pre-diabetes and 24% of fathers had a history of having diabetes.
Participants with diabetes (n=4) had a mean BMI of 37.2 ± 1.4 kg/m
2, a WC of 102.7 ± 7.6 cm, and a weight of 97.7 ± 4.9 kg (
Figure 2). One-fourth of them (25%) do not do intentional physical activity, while 75% do not eat fruits or vegetables daily. Participants with prediabetes (n=25) had a mean BMI of 33.2 ± 5.9 kg/m
2, a WC of 99.1 ± 10.6 cm, and a weight of 94.2 ± 16.2 kg (
Figure 2). About 40% do not do intentional physical activity, while 72% do not eat fruits or vegetables daily.
Participants in the ‘At Risk’ category (n=122, by HbA1c levels) had a mean BMI of 28.7 ± 5.5 kg/m
2, a WC of 86.9 ± 12.6 cm, and a weight of 79.3 ± 17.4 kg (
Figure 2). About 18% of them do not do any physical activity, and 79.5% do not eat any fruits or vegetables daily. About 10.7% of participant’s mothers and 18.9% of fathers had a history of having diabetes.
Further, interpretive analysis shows a linear relationship between increasing blood sugar and anthropometric measures of weight, BMI, and WC (F=10.4, df1=3, df2=266 p<0.001). Age is also proportionately related to having diabetes in this subset of the population (F=3.5, df1=2, df2=269, p<0.05). Participants’ mothers’ having diabetes is found to be more of a predictor (p=0.1) of higher blood sugar levels than the fathers having diabetes (p=0.4).
To understand the predictors of diabetes, a Factor Analysis was done for participants who were in the ‘At Risk’ group(n=122). The statistical acceptability of the analysis was tested by the Kaiser-Meyer-Olkin (KMO) Measure of Sampling Adequacy, which was 0.735 (greater than 0.60), and Bartlett’s test of sphericity, which was significant (p < 0.01). This allowed the team to proceed with Exploratory Factor Analysis, where WC, BMI, and weight were found to be the most important factors for increased blood sugar in these populations (the Eigenvalues were 0.953,0.941, and 0.934, respectively).
3.4. Lifestyle, Diet, and Mental Health Challenges
Participants in at-risk, prediabetes, and diabetes groups (n=41) were randomly selected for a qualitative interview to learn more about their behavioural, cultural, and familial attributes. The collected qualitative data was analyzed following the IPA approach and matched with the quantitative data collected by the CANRISK tool (Smith & Osborn, 2015). This data included participants’ lifestyle, diet, family history of diabetes, mental health, and changes in physical and lifestyle factors resulting from migration to Canada to identify a trend within each group.
In the ‘At Risk’ group, 60% of respondents agreed to consume high-calorie food weekly. They also agreed that they eat when hungry or when food is available and generally eat after 8 PM. About 20% of respondents reported a family history of diabetes in either one or both biological parents. Regarding lifestyle, all participants confirmed that they did not smoke or drink and agreed to only participate in slight physical activities such as brisk walking. Likewise, 80% of participants expressed feelings of anxiety or depression that step from either adjustment to the harsh weather in Canada and the Canadian workplace, difficulty in finding a job, or a combination of these.
4. Discussion
The definition of ‘Black African’ is agreed upon. However, defining ‘Black Caribbean’ required a literature search and peer consultation. Geographically, the Caribbean includes the countries surrounding the Caribbean Sea, including Venezuela, Colombia, Panama, Costa Rica, Nicaragua, Honduras, Guatemala, Belize, the Yucatan Peninsula of Mexico, Cuba, Hispaniola, Jamaica, Puerto Rico, the Virgin Islands and Trinidad [
33]. However, many people, including participants in this study, may describe themselves as Caribbean persons despite not being from a geographic Caribbean region. This discrepancy is in part due to colonial connotations, which have led to the term Caribbean being used to describe many geographic regions that have little to do with physical geography but instead arise from the cultural, economic, ethnic, and political similarities between countries of the Caribbean and those nearby [
34]. Given these discrepancies, in the current study, the term Black Caribbean was used to characterize African-descendant residents of the islands in the Caribbean Sea, some South and Central American countries (Guyana, Suriname, and Belize), and islands in the Atlantic (Turks and Caicos Islands) [
29]. The participants represented 14 African countries in five regions and 5 Caribbean countries.
Culture and ethnicity are complex topics and not always interchangeable; however, the study team decided to use ethnicity data as a proxy indicator for culture data in this study. Other studies also adopted a similar consideration [
11]. This study collected representative data from immigrants from all over African and Caribbean countries (of different ethnicities) to share information on various cultures across the continents.
The mean HbA1c of the participants (n=272) was found to be 5.5 mmol/L (higher than the standard Canadian value), which falls in the category of ‘At Risk’ of diabetes as per Canadian guidelines. Taloyan et al. (2021) reported that the HbA1c of African immigrants is higher than Swedish-born participants [
35]. Herman and Cohen (2012) also reported that Black people have a higher HbA1c than non-Blacks [
8].
The study screened 1.4% of participants with diabetes, one of whom (HbA1c of 10 and a BMI of 28.26 kg/m2) required urgent primary care consultation. As a Community-Based Action Research study through an equity lens, participants and their communities who require urgent care receive immediate benefits from the research activity. This is CBR’s social and research commitment [
36]. Following the current diagnostic criteria of Diabetes Canada guidelines, HbA1c screened 47.4% of cases of prediabetes (Chi-square value 113.2, df 9, p<0.001) and 75% of cases of diabetes (Chi-square value 199.5, df 6, p<0.001) diagnosed by OGTT [
9]. This study found HbA1c 24% more sensitive than OGTT for screening prediabetes. Other studies with Black and other ethnic minorities also observed that HbA1c’s diagnostic sensitivity is higher [
37,
38]. This observation recommends that HbA1c can be used as a sensitive screening tool for ethnic minorities.
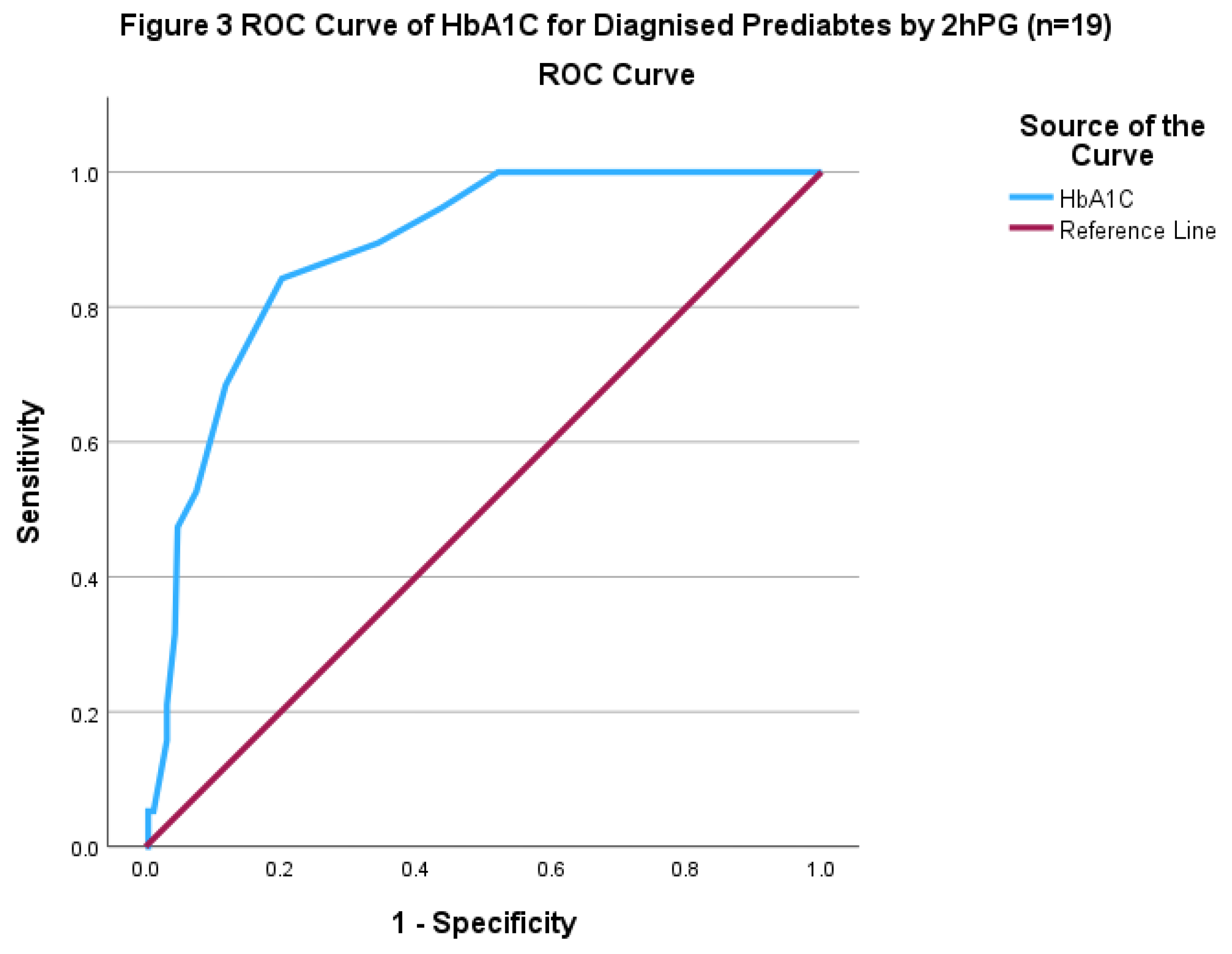
To test the sensitivity and specificity of HbA1c for participants diagnosed by OGTT with prediabetes and diabetes, the Receiver Operator Characteristic (ROC) Curve was attempted. The area value of the analysis with prediabetes data was 0.881, p< 0.001, and CI 0.817-0.944, meaning a good fit for analysis. The HbA1c cut-off value of HbA1c for prediabetes was 5.7% (
Figure 3).
In comparison, the cut-off value for diabetes was found to be 6.4% (Area value 0.969, p<0.001, CI 0.969-1.007) (the poor sample size made the interpretation invalid for the diabetes group). The standard HbA1c value for prediabetes is 6.0%-6.4%, and for diabetes is 6.5% or more [
9]. This analysis recommends setting a lower HbA1c cut-off for diagnosing prediabetes and diabetes in ACB individuals. Alternatively, the Canadian Guidelines should be revised, raising the cut-offs. This finding can be tested with other ethnic groups, such as South Asians or Indigenous Communities, to determine a culturally relative, not a universal, cut-off for diabetes.
As a test procedure, the precision and compliance with the OGTT are lower than HbA1c. This was identified in qualitative discussions with participants whose fasting blood sugar was more than the blood sugar level measured 2 hours after a 75 g glucose drink. Their food behaviour of having supper late in the evening and their cultural preferences for a more carbohydrate-rich diet cause a higher fasting sugar level. They do not drink the whole 75 g glucose because “too sweet to drink in the morning”. They do not trust what is free to drink and pour it in the bathroom. Some save it for their children at home and drink water from their bottles. Some drink it slowly over an hour, mixed with water. After this information, we drew attention to the LifeLabs quality assurance team. They trained their staff to check and control the process so that everyone finished the glucose in front of them in five minutes. We controlled the study participants, but these are the feelings of these ACB individuals, as they mentioned. Therefore, we recommend doing HbA1c and random blood sugar for diagnostic purposes for ACBs and also for other ethnic minorities if they have similar cultural traits. This will also reduce costs and increase patient compliance without compromising diagnostic precision.
Qualitative data also explored how food insecurity affects their food behaviour and a cultural trait of preferring carbohydrate-rich food and eating late in the evening. The participants consider the at-risk nature of these findings primarily due to their diet, lifestyle and immigration status rather than family history. Their mental health has been an issue that needs to be addressed. They have settlement anxiety and workplace culture anxiety. Some of them have drinking alcohol as a habit, while most of them are not.
Considering the previous study findings that diabetes affects some ethnicity or racial groups more than others, ethnic-based or culture-based intervention is asked for [
39,
40,
41,
42]. This study emphasizes that immigrants of early age groups must be screened with the updated CANRISK tool [
43].
Strengths and Limitations
Participants were recruited from multiple Access Alliance locations across Toronto. Despite a meticulous design to collect representative samples of the target population and rigorous data analysis techniques, the sample size is not large and needs mindful interpretation for generalization. Collecting qualitative data to interpret quantitative findings was a supplement to ensure data accuracy and validity. However, culturally competent further longitudinal research on this issue with a larger sample size is required to generalize the findings.
5. Conclusions
This screening identified that ACB individuals aged 18-39 years are vulnerable to diabetes and prediabetes, with over 44% of them being at risk. Their ethnicity is a factor; however, their food habit, lifestyle, and settlement challenges in Canada are other contributory factors for dysglycaemia. They have unique food cultures and preferences; therefore, they need culturally appropriate diet education from their peers (proximity principle) and flexibility in dietary options. As such, proximity and flexibility can be very instrumental tools for successful diabetes education programs. The intersectional analysis found HbA1c to be a more sensitive and culturally acceptable measure than OGTT to screen ACB individuals at risk/prediabetes. HbA1c level is found higher in ACB populations which requires larger longitudinal research to set a culture-relative equity-focused cut-off for ethnic minorities (instead of the current universal cut-off) to diagnose prediabetes and diabetes. Considering mental health as a significant issue in ethnic minorities with dysglycaemia, diabetes education also requires incorporating mental health consultations for them.
Author Contributions
Methodology, Akm Alamgir; Formal analysis, Akm Alamgir; Investigation, Osezua Momoh; Data curation, Akm Alamgir and Rhea Raghunauth; Writing – original draft, Rhea Raghunauth and Osezua Momoh; Writing – review & editing, Akm Alamgir and Cliff Ledwos; Supervision, Akm Alamgir; Project administration, Akm Alamgir; Funding acquisition, Cliff Ledwos.
Funding
We are grateful to the Public Health Agency of Canada (PHAC) and the Public Health Ontario (PHO) for funding this study [PHAC Memo# 4500447703].
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Health Canada and the Public Health Agency of Canada Research Ethics Board [REB 2021-029P].
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The original contributions presented in this study are included in the article/supplementary material. Further inquiries can be directed to the corresponding author(s).
Acknowledgements
The study thanks the reviewers for their thoughtful feedback, making the article more readable and accessible. We are also grateful to the participants who agreed to be included in the study. We acknowledge the support of the primary care team, research team, and the senior management of Access Alliance for supporting this study. LifeLabs professionally completed blood work with the highest levels of diligence.
Conflicts of Interest
There is no conflict of interest to mention.
References
- Diabetes 360o: A framework for a diabetes strategy for Canada. (2018). Diabetes Canada. https://www.diabetes.ca/DiabetesCanadaWebsite/media/Advocacy-and-Policy/Diabetes-360-Recommendations.
- Chiu, M.; Maclagan, L. C.; Tu, J. V.; Shah, B. R. Temporal trends in cardiovascular disease risk factors among white, South Asian, Chinese and black groups in Ontario, Canada, 2001 to 2012: A population-based study. BMJ Open, 0072. [Google Scholar] [CrossRef]
- Public Health Agency of Canada (PHAC). Diabetes: Symptoms and treatment. Government of Canada; 2023. https://www.canada.ca/en/public-health/services/chronic-diseases/diabetes/symptoms-treatment.html#a2.
- Lipscombe, L. L.; Hux, J. E. Trends in diabetes prevalence, incidence, and mortality in Ontario, Canada 1995-2005: A population-based study. Lancet, 2007, 369, 750–756. [Google Scholar] [CrossRef] [PubMed]
- Gungor, N.; Bacha, F.; Saad, R.; Janosky, J.; Arslanian, S. Youth type 2 diabetes: Insulin resistance, beta-cell failure, or both? Diabetes Care, 2005, 28, 638–644. [Google Scholar] [CrossRef] [PubMed]
- Viner, R.; White, B.; Christie, D. (2017). Type 2 diabetes in adolescents: A severe phenotype posing major clinical challenges and public health burden. Lancet, 2017, 389, 2252–2260. [Google Scholar] [CrossRef] [PubMed]
- Swaleh, R. M.; Yu, C. “A touch of sugar”: A qualitative study of the impact of health beliefs on type 1 and type 2 diabetes self-management among black Canadian adults. Can J Diabetes, 2021, 45, 607–613.e2. [Google Scholar] [CrossRef] [PubMed]
- Herman, W. H.; Cohen, R.M. Racial and ethnic differences in the relationship between HbA1c and blood glucose: implications for the diagnosis of diabetes. The Journal of clinical endocrinology and metabolism, 2012, 97, 1067–1072. [Google Scholar] [CrossRef]
- Punthakee, Z.; Goldenberg, R.; Katz, P. for Diabetes Canada Clinical Practice Guidelines Expert Committee. Definition, Classification and Diagnosis of Diabetes, Prediabetes and Metabolic Syndrome. Can J Diabetes, 1. [CrossRef]
- WHO. Use of Glycated Haemoglobin (HbA1c) in the Diagnosis of Diabetes Mellitus: Abbreviated Report of a WHO Consultation. Geneva: World Health Organization, 2011. Available from: https://www-ncbi-nlm-nih-gov.myaccess.library.utoronto. 3042.
- Scollan-Koliopoulos, M.; Rapp, K.J.; Bleich, D. Afrocentric Cultural Values and Beliefs: Movement Beyond the Race and Ethnicity Proxy to Understand Views of Diabetes. The Diabetes Educator, 2012, 38, 488–498. [Google Scholar] [CrossRef]
- Haw, J. S.; Shah, M.; Turbow, S.; Egeolu, M.; Umpierrez, G. Diabetes Complications in Racial and Ethnic Minority Populations in the USA. Current Diabetes Reports, 2021, 21, 2. [Google Scholar] [CrossRef]
- Peek, M. E.; Odoms-Young, A.; Quinn, M. T.; Gorawara-Bhat, R.; Wilson, S. C.; Chin, M. H. Race and shared decision-making: Perspectives of African-Americans with diabetes. Social Sci Med, 2010, 71, 1–9. [Google Scholar] [CrossRef]
- Hyman, I.; Gucciardi, E.; Patychuk, D.; Rummens, J. A.; Shakya, Y.; Kljujic, D.; Bhamani, M.; Boqaileh, F. Self-management, health service use and information seeking for diabetes care among Black Caribbean immigrants in Toronto. Canadian J Diabetes, 2014, 38, 32–37. [Google Scholar] [CrossRef]
- Goddu, A. P.; Raffel, K. E.; Peek, M. E. A story of change: The influence of narrative on African-Americans with diabetes. Patient Education and Counseling, 2015, 98, 1017–1024. [Google Scholar] [CrossRef]
- Newbold, K. B.; Danforth, J. Health status and Canada’s immigrant population. Social Sci Med. 2003, 57, 1981–1995. [Google Scholar] [CrossRef] [PubMed]
- Gee, E. M.; Kobayashi, K. M.; Prus, S. G. Examining the healthy immigrant effect in mid- to later life: Findings from the Canadian Community Health Survey. Can J Aging, /: 23 Suppl 1: S61-69. https, 1566. [Google Scholar]
- Khosla, L.; Bhat, S.; Fullington, L.A.; Horlyck-Romanovsky, M.F. HbA1c Performance in African Descent Populations in the United States with Normal Glucose Tolerance, Prediabetes, or Diabetes: A Scoping Review. Prev Chronic Dis, 2021, 18, 200365. [Google Scholar] [CrossRef] [PubMed]
- Jones, V.; Crowe, M. How people from ethnic minorities describe their experiences of managing type-2 diabetes mellitus: A qualitative meta-synthesis. Int J Nursing Studies, 2017, 76, 78–91. [Google Scholar] [CrossRef] [PubMed]
- Chatterjee, S.; Khunti, K.; Davies, M. J. Type 2 diabetes. Lancet, 2017, 389, 2239–2251. [Google Scholar] [CrossRef]
- Knowler, W. C.; Barrett-Connor, E.; Fowler, S. E.; Hamman, R. F.; Lachin, J. M.; Walker, E. A.; Nathan, D. M. Diabetes Prevention Program Research Group. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002, 346, 393–403. [Google Scholar] [CrossRef]
- Rosella, L. C.; Lebenbaum, M.; Fitzpatrick, T.; Zuk, A.; Booth, G. L. Prevalence of prediabetes and undiagnosed diabetes in Canada (2007-2011) according to fasting plasma glucose and HbA1c screening criteria. Diabetes Care, 2015, 38, 1299–1305. [Google Scholar] [CrossRef]
- Young, T. K.; Mustard, C. A. Undiagnosed diabetes: Does it matter? CMAJ, 2001, 164, 24–28. [Google Scholar]
- Lemieux, C.L.; de Groh, M.; Gibbons, L.; Morrison, H.; Jiang, Y. A Tool to Assess Risk of Type 2 Diabetes in Canadian Adults. Can J Diabetes, 2020, 44, 445–447. [Google Scholar] [CrossRef]
- Daly, J.; Willis, K.; Small, R.; Green, J.; Welch, N.; Kealy, M.; Hughes, E. A hierarchy of evidence for assessing qualitative health research. J Clin Epid, 2007, 60, 43–49. [Google Scholar] [CrossRef]
- Creswell, J. W. (2014). Research design: Qualitative, quantitative, and mixed methods approaches (4th ed). SAGE Publications.
- Arcaya, M. C.; Schnake-Mahl, A.; Binet, A.; Simpson, S.; Church, M. S.; Gavin, V.; Coleman, B.; Levine, S.; Nielsen, A.; Carroll, L.; Ursprung, S.; Wood, B.; Reeves, H.; Keppard, B.; Sportiche, N.; Partridge, J.; Figueroa, J.; Frakt, A.; Alfonzo, M.; … Youmans, T. Community change and resident needs: Designing a participatory action research study in metropolitan Boston. Health & Place, 2018, 52, 221–230. [Google Scholar] [CrossRef]
- Benoot, C.; Hannes, K.; Bilsen, J. The use of purposeful sampling in a qualitative evidence synthesis: A worked example on sexual adjustment to a cancer trajectory. BMC Med Res Method, 2016, 16, 21. [Google Scholar] [CrossRef] [PubMed]
- Bennett, N.R.; Francis, D.K.; Ferguson, T.S.; Hennis, A.J.; Wilks, R.J.; Harris, E.N.; MacLeish, M.M.; Sullivan, L.W. : U.S. Caribbean Alliance for Health Disparities Research Group (USCAHDR). Disparities in diabetes mellitus among Caribbean populations: a scoping review. Int J Equity Health, 2015, 14, 23. [Google Scholar] [CrossRef]
- Janosky, J. E. Use of the single subject design for practice based primary care research. Postgraduate medical journal, 2005, 81, 549–551. [Google Scholar] [CrossRef] [PubMed]
- Smith, J. A.; Osborn, M. Interpretative phenomenological analysis as a useful methodology for research on the lived experience of pain. British J Pain, 2015, 9, 41–42. [Google Scholar] [CrossRef] [PubMed]
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qualitative Res Psychology, 2006, 3, 77–101. [Google Scholar] [CrossRef]
- Caribbean Sea | definition, location, map, islands, & facts | Britannica. (, 2024). https://www.britannica. 24 May.
- Williams, E. H.; Bunkley-Williams, L. What and where is the Caribbean? A modern definition. The Florida Geographer, 2021, 52, 3–28. [Google Scholar]
- Taloyan, M.; Salminen, H.; Melin, F.; Steiner, K.; Östenson, C. (2021). Comparing the diagnostic accuracy of HbA1c for pre-diabetes and diabetes between foreign-born and Swedish-born primary healthcare patients. Res Square (Preprint),2021). [CrossRef]
- Alamgir, Akm. ; Roy, P.; Taverna, F. Levels of Engagement of South Asian Participants in Health Research: Effectiveness of Community-Based Research (CBR) Framework. J Sci Res and Reports, 2024, 30, 880–897. [Google Scholar] [CrossRef]
- Booth, R.A.; Jiang, Y.; Morrison, H.; Orpana, H.; Van Katwyk, S.R.; Lemieux, C. Ethnic dependent differences in diagnostic accuracy of glycated hemoglobin (HbA1c) in Canadian adults. Diabetes Res Clin Practice, 2018, 136, 143–149. [Google Scholar] [CrossRef]
- Mostafa, S. A.; Davies, M. J.; Webb, D.; Gray, L. J.; Srinivasan, B. T.; Jarvis, J.; Khunti, K. The potential impact of using glycated haemoglobin as the preferred diagnostic tool for detecting Type 2 diabetes mellitus. Diabetic Medicine, 2010, 27, 762–769. [Google Scholar] [CrossRef]
- Pham, T. M.; Carpenter, J. R.; Morris, T. P.; Sharma, M.; Petersen, I. Ethnic differences in the prevalence of type 2 diabetes diagnoses in the UK: Cross-sectional analysis of the health improvement network primary care database. Clin Epid, 2019, 11, 1081–1088. [Google Scholar] [CrossRef]
- Fazli, G. S.; Moineddin, R.; Bierman, A. S.; Booth, G. L. Ethnic differences in prediabetes incidence among immigrants to Canada: A population-based cohort study. BMC Medicine, 2019, 17, 100. [Google Scholar] [CrossRef] [PubMed]
- Bird, Y.; Lemstra, M.; Rogers, M.; Moraros, J. The relationship between socioeconomic status/income and prevalence of diabetes and associated conditions: A cross-sectional population-based study in Saskatchewan, Canada. Int J Equity in Health, 2015, 14, 93. [Google Scholar] [CrossRef] [PubMed]
- Gagné, T.; Veenstra, G. Inequalities in Hypertension and Diabetes in Canada: Intersections between Racial Identity, Gender, and Income. Ethn Dis. 2017, 27, 27, 371–378. [Google Scholar] [CrossRef]
- Hux, J. E.; Ivis, F.; Flintoft, V.; Bica, A. Diabetes in Ontario: Determination of prevalence and incidence using a validated administrative data algorithm. Diabetes Care, 2002, 25, 512–516. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).