Submitted:
22 November 2024
Posted:
25 November 2024
You are already at the latest version
Abstract
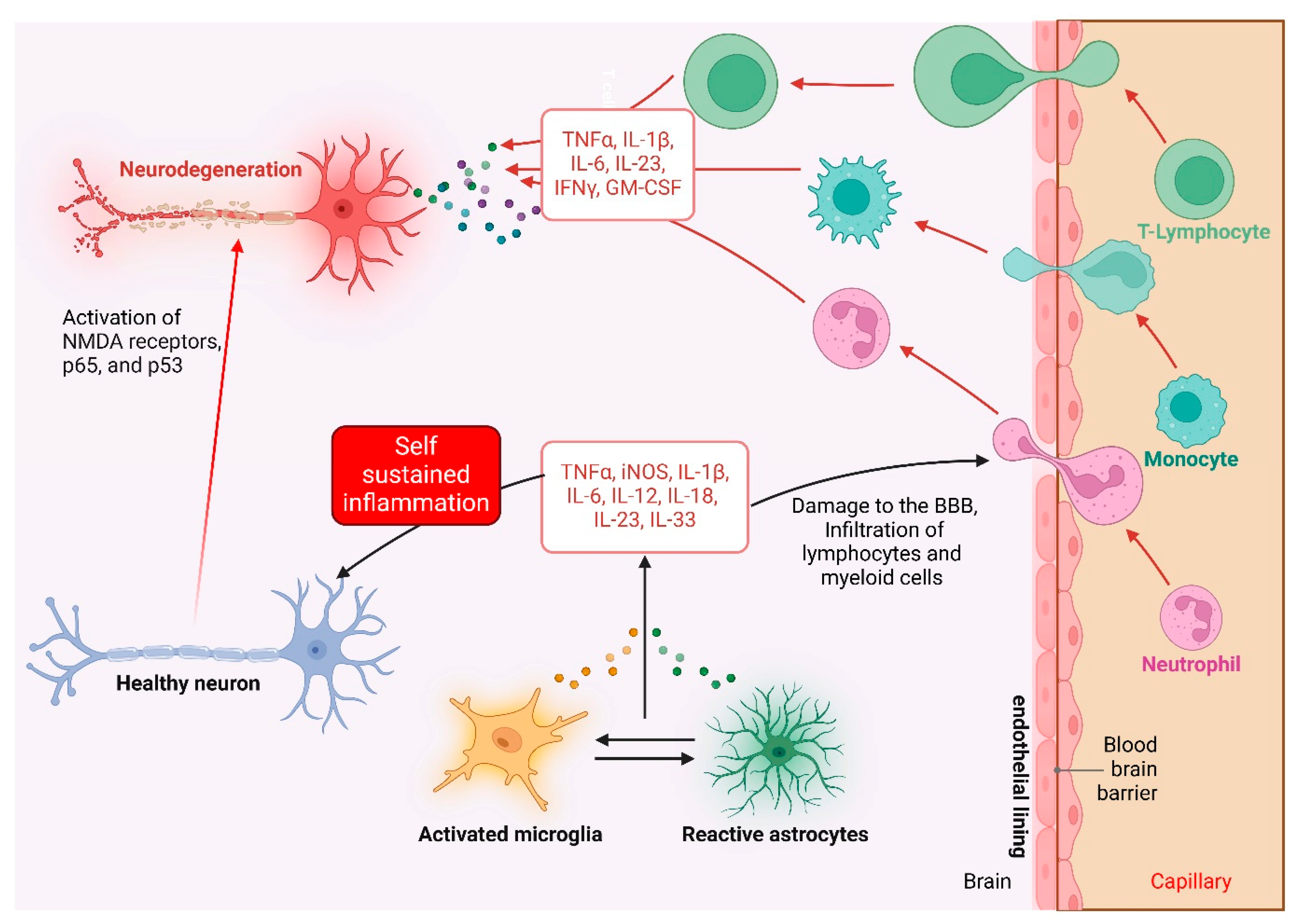
Cytokine-mediated inflammation is becoming recognized as a vital role in the pathophysiology of a wide range of brain illnesses, including neurodegenerative, psychiatric, and neurodevelopmental problems. Pro-inflammatory cytokines such as interleukin-1 (IL-1), tumor necrosis factor-alpha (TNF-α), and interleukin-6 (IL-6) cause neuroinflammation, alter brain function, and accelerate disease development. Despite progress in understanding these pathways, effective medicines to target brain inflammation are still limited. Traditional anti-inflammatory and immunomodulatory drugs are effective in peripheral inflammatory illnesses. Still, they confront substantial hurdles when used on the central nervous system, such as the blood-brain barrier and unwanted systemic effects. The review highlighted the developing treatment techniques for modifying cytokine-driven neuroinflammation, focusing on advances that selectively target critical cytokines involved in brain pathology. Novel approaches, including cytokine-specific inhibitors, antibody-based therapeutics, gene and RNA-based interventions, and sophisticated drug delivery systems like nanoparticles, promise to lower neuroinflammation with greater specificity and safety. Furthermore, developments in biomarker discoveries and neuroimaging techniques improve our ability to monitor inflammatory responses, allowing for more accurate and personalized treatment regimens. Preclinical and clinical trial data demonstrate the therapeutic potential of these tailored techniques. However, significant challenges remain, such as improving delivery across the blood-brain barrier and reducing off-target effects. As research advances, the creation of personalized, cytokine-centered therapeutics has the potential to alter the therapy landscape for brain illnesses, giving patients hope for better results and a higher quality of life.
Keywords:
Introduction
Cytokine-Mediated Inflammation in the Brain
Brain Disorders Associated with Cytokine Dysregulation
1. Neurodegenerative Disorders
2. Psychiatric Disorders
3. Neurodevelopmental Disorders
4. Acute Brain Injuries
5. Multiple Sclerosis (MS) and Autoimmune Disorders
Current Therapeutic Approaches for Inflammation in Brain Disorders
1. Nonsteroidal Anti-Inflammatory Drugs (NSAIDs)
2. Corticosteroids
3. Cytokine-Specific Inhibitors and Monoclonal Antibodies
4. Small Molecule Inhibitors
5. Emerging Therapies: Nanotechnology and Gene-Based Approaches
6. Personalized Medicine and Biomarker-Guided Therapy
Emerging Treatment Strategies for Cytokine-Mediated Inflammation
1. Biologics Targeting Cytokine Pathways
2. Nanotechnology-Based Drug Delivery
3. RNA-Based Therapies
4. Gene Editing and CRISPR Technology
5. Modulation of the Gut-Brain Axis
6. Neuroprotective Peptides and Small Molecules
7. Cellular Therapies
8. Personalized and Biomarker-Guided Therapies
Novel Approaches to Drug Delivery in the Brain
1. Nanotechnology-Based Drug Delivery
2. Ultrasound-Enhanced Delivery
3. Intranasal Drug Delivery
4. Exosome-Based Delivery
5. Polymer-Based Drug Delivery Systems
6. Gene-Delivery Systems
7. Combination Strategies
Potential Biomarkers for Monitoring Inflammatory Response
1. Cytokines and Chemokines in Cerebrospinal Fluid (CSF) and Plasma
2. Microglial and Astrocytic Activation Markers
3. Neurofilament Light Chain (NfL)
4. Immune-Cell-Derived Extracellular Vesicles
5. Metabolites and Lipid Mediators
6. Neuroimaging Biomarkers
7. Genomic and Transcriptomic Markers
8. The Gut-Brain Axis Biomarkers
Preclinical and Clinical Trials
1. Preclinical Studies
- Cytokine Inhibitors: Animal models of AD, PD and MS have shown that cytokine inhibitors effectively reduce neuroinflammation. In transgenic mouse models of AD, monoclonal antibodies targeting TNF-α improved cognitive deterioration (Wong-Guerra et al., 2023). IL-1β inhibitors improved motor function and reduced glial activation in animal models of PD (Godoy, Tarelli, Ferrari, Sarchi, & Pitossi, 2008).
- Gene Therapy: Preclinical experiments using adeno-associated viral (AAV) vectors to transmit anti-inflammatory cytokines such as IL-10 have shown promise in chronic neuroinflammatory disorders, including ALS and Huntington's disease, by lowering microglial activation and neuronal damage (Parambi et al., 2022).
- Nanoparticle-Based Delivery: In preclinical studies, nanoparticle-based delivery methods improved the CNS bioavailability of cytokine inhibitors. For example, lipid nanoparticles containing siRNA targeting IL-6 dramatically reduced inflammatory indicators and neuronal death in stroke models (Y. Huang et al., 2024).
2. Clinical Trials
- TNF-α Inhibitors: TNF-α inhibitors like infliximab and etanercept, once used for autoimmune illnesses including rheumatoid arthritis, are now utilized to treat CNS disorders. A pilot study of etanercept in post-stroke patients found that it improved motor function and mood by reducing neuroinflammation (Sedger & McDermott, 2014). However, larger randomized controlled trials are necessary to corroborate these findings.
- IL-1β Antagonists: Anakinra, an IL-1 receptor antagonist, was tested in TBI patients and found to reduce systemic inflammatory markers while improving clinical outcomes in early-phase trials (Lindblad et al., 2023). Ongoing trials are evaluating its potential in neurodegenerative illnesses such as AD.
- IL-6 Blockade: Tocilizumab, an IL-6 receptor antagonist, has been studied in depression and schizophrenia. A randomized trial in treatment-resistant depression discovered improvements in depressive symptoms, corresponding with lower peripheral inflammatory markers (Girgis et al., 2018; Knight et al., 2021).
- Combination Therapies: Clinical investigations have indicated that combining anti-inflammatory medicines with neuroprotective techniques can be effective. A phase II trial with minocycline and an IL-1β inhibitor in MS patients found a synergistic benefit, lowering lesion development and neuroinflammatory indicators (Mallah et al., 2020).
3. Immune Modulation in Specific Disorders
- Alzheimer’s Disease: Several trials have investigated immune-modulating drugs in AD. Solanezumab, an anti-amyloid monoclonal antibody that does not directly target cytokines, has shown promise in decreasing neuroinflammatory indicators in CSF (Honig et al., 2018; J. Zhang et al., 2024). Trials that combine amyloid-targeting treatments with anti-inflammatory medications are ongoing.
- Multiple Sclerosis: Phase III trials have proven that therapies that modify cytokine signaling pathways, such as fingolimod and siponimod, significantly reduce relapse rates and lesion volume in MS patients (Piehl, 2021).
- Traumatic Brain Injury: Clinical investigations of stem cell therapy have revealed that mesenchymal stem cells can reduce cytokine-mediated inflammation and increase recovery in TBI patients. These benefits are believed to be mediated by the release of anti-inflammatory cytokines such as IL-10 (R. Zhang et al., 2013).
Future Directions and Perspectives
1. Expanding the Understanding of Cytokine Pathways
2. Precision Medicine Approaches
3. Novel Therapeutic Targets and Agents
4. Innovative Drug Delivery Systems
5. Biomarkers for Real-Time Monitoring
6. Combination Therapies
7. Role of the Gut-Brain Axis
8. Neuroimmune Crosstalk and Aging
9. Regulatory and Ethical Considerations
Conclusion
Abbreviations
References
- Abdelhak, A., Foschi, M., Abu-Rumeileh, S., Yue, J. K., D’Anna, L., Huss, A., … Tumani, H. (2022). Blood GFAP as an emerging biomarker in brain and spinal cord disorders. Nature Reviews Neurology, Vol. 18. [CrossRef]
- Ageeva, T., Rizvanov, A., & Mukhamedshina, Y. (2024). NF-κB and JAK/STAT Signaling Pathways as Crucial Regulators of Neuroinflammation and Astrocyte Modulation in Spinal Cord Injury. Cells, 13(7), 581. [CrossRef]
- Ahmad, M. A., Kareem, O., Khushtar, M., Akbar, M., Haque, M. R., Iqubal, A., … Alhajri, N. (2022). Neuroinflammation: A Potential Risk for Dementia. International Journal of Molecular Sciences, Vol. 23. [CrossRef]
- Aiello, A., Farzaneh, F., Candore, G., Caruso, C., Davinelli, S., Gambino, C. M., … Accardi, G. (2019). Immunosenescence and its hallmarks: How to oppose aging strategically? A review of potential options for therapeutic intervention. Frontiers in Immunology, Vol. 10. [CrossRef]
- Alam, A., Thelin, E. P., Tajsic, T., Khan, D. Z., Khellaf, A., Patani, R., & Helmy, A. (2020). Cellular infiltration in traumatic brain injury. Journal of Neuroinflammation, Vol. 17. [CrossRef]
- Alirezaei, Z., Pourhanifeh, M. H., Borran, S., Nejati, M., Mirzaei, H., & Hamblin, M. R. (2020). Neurofilament Light Chain as a Biomarker, and Correlation with Magnetic Resonance Imaging in Diagnosis of CNS-Related Disorders. Molecular Neurobiology, Vol. 57. [CrossRef]
- Allemailem, K. S., Alsahli, M. A., Almatroudi, A., Alrumaihi, F., Abdulmonem, W. Al, Moawad, A. A., … Khan, A. A. (2023). Innovative Strategies of Reprogramming Immune System Cells by Targeting CRISPR/Cas9-Based Genome-Editing Tools: A New Era of Cancer Management. International Journal of Nanomedicine, Vol. 18. [CrossRef]
- Alsaab, H. O., Alharbi, F. D., Alhibs, A. S., Alanazi, N. B., Alshehri, B. Y., Saleh, M. A., … Alzhrani, R. M. (2022). PLGA-Based Nanomedicine: History of Advancement and Development in Clinical Applications of Multiple Diseases. Pharmaceutics, Vol. 14. [CrossRef]
- Amoriello, R., Memo, C., Ballerini, L., & Ballerini, C. (2024). The brain cytokine orchestra in multiple sclerosis: from neuroinflammation to synaptopathology. Molecular Brain, Vol. 17. [CrossRef]
- Archie, S. R., Al Shoyaib, A., & Cucullo, L. (2021). Blood-brain barrier dysfunction in cns disorders and putative therapeutic targets: An overview. Pharmaceutics, Vol. 13. [CrossRef]
- Ashique, S., Mohanto, S., Ahmed, M. G., Mishra, N., Garg, A., Chellappan, D. K., … Kahwa, I. (2024). Gut-brain axis: A cutting-edge approach to target neurological disorders and potential synbiotic application. Heliyon, 10(13), e34092. [CrossRef]
- Babu, M., & Snyder, M. (2023). Multi-omics profiling for health. Molecular and Cellular Proteomics, 22(6). [CrossRef]
- Badanjak, K., Fixemer, S., Smajić, S., Skupin, A., & Grünewald, A. (2021). The contribution of microglia to neuroinflammation in parkinson’s disease. International Journal of Molecular Sciences, Vol. 22. [CrossRef]
- Benninger, F., Glat, M. J., Offen, D., & Steiner, I. (2016). Glial fibrillary acidic protein as a marker of astrocytic activation in the cerebrospinal fluid of patients with amyotrophic lateral sclerosis. Journal of Clinical Neuroscience, 26. [CrossRef]
- Bhol, N. K., Bhanjadeo, M. M., Singh, A. K., Dash, U. C., Ojha, R. R., Majhi, S., … Jena, A. B. (2024). The interplay between cytokines, inflammation, and antioxidants: mechanistic insights and therapeutic potentials of various antioxidants and anti-cytokine compounds. Biomedicine & Pharmacotherapy, 178, 117177. [CrossRef]
- Bouras, M., Asehnoune, K., & Roquilly, A. (2022). Immune modulation after traumatic brain injury. Frontiers in Medicine, Vol. 9. [CrossRef]
- Bourgognon, J.-M., & Cavanagh, J. (2020). The role of cytokines in modulating learning and memory and brain plasticity. Brain and Neuroscience Advances, 4. [CrossRef]
- Branchi, I., Viglione, A., Vai, B., Cirulli, F., Benedetti, F., & Poggini, S. (2024). Breaking free from the inflammatory trap of depression: Regulating the interplay between immune activation and plasticity to foster mental health. Neuroscience Applied, 3. [CrossRef]
- Brett, B. L., Gardner, R. C., Godbout, J., Dams-O’Connor, K., & Keene, C. D. (2022). Traumatic Brain Injury and Risk of Neurodegenerative Disorder. Biological Psychiatry, Vol. 91. [CrossRef]
- Brokowski, C., & Adli, M. (2019). CRISPR Ethics: Moral Considerations for Applications of a Powerful Tool. Journal of Molecular Biology, Vol. 431. [CrossRef]
- Buga, A. M., Padureanu, V., Riza, A. L., Oancea, C. N., Albu, C. V., & Nica, A. D. (2023). The Gut–Brain Axis as a Therapeutic Target in Multiple Sclerosis. Cells, Vol. 12. [CrossRef]
- Burgess, A., Shah, K., Hough, O., & Hynynen, K. (2015). Focused ultrasound-mediated drug delivery through the blood-brain barrier. Expert Review of Neurotherapeutics, Vol. 15. [CrossRef]
- Bustin, S. A., & Jellinger, K. A. (2023). Advances in Molecular Medicine: Unravelling Disease Complexity and Pioneering Precision Healthcare. International Journal of Molecular Sciences, Vol. 24. [CrossRef]
- Cabrera-Pastor, A. (2024). Extracellular Vesicles as Mediators of Neuroinflammation in Intercellular and Inter-Organ Crosstalk. International Journal of Molecular Sciences, 25(13), 7041. [CrossRef]
- Chang, J. W. (2020). The potential role of gene therapy for the treatment of neuropathic pain. Molecular Pain, 16.
- Chen, Yijun, & Yu, Y. (2023). Tau and neuroinflammation in Alzheimer’s disease: interplay mechanisms and clinical translation. Journal of Neuroinflammation, Vol. 20. [CrossRef]
- Chen, Yvonne, Mateski, J., Gerace, L., Wheeler, J., Burl, J., Prakash, B., … Adams, B. D. (2024). Non-coding RNAs and neuroinflammation: implications for neurological disorders. Experimental Biology and Medicine, Vol. 249. [CrossRef]
- Chery, J. (2016). RNA therapeutics: RNAi and antisense mechanisms and clinical applications. Postdoc Journal, 4(7). [CrossRef]
- Chi, S., & Lee, M. S. (2021). Personalized medicine using neuroimmunological biomarkers in depressive disorders. Journal of Personalized Medicine, Vol. 11. [CrossRef]
- Corrigan, M., O’Rourke, A. M., Moran, B., Fletcher, J. M., & Harkin, A. (2023). Inflammation in the pathogenesis of depression: a disorder of neuroimmune origin. Neuronal Signaling, Vol. 7. [CrossRef]
- Coutinho, A. E., & Chapman, K. E. (2011). The anti-inflammatory and immunosuppressive effects of glucocorticoids, recent developments and mechanistic insights. Molecular and Cellular Endocrinology, Vol. 335. [CrossRef]
- Danikowski, K. M., Jayaraman, S., & Prabhakar, B. S. (2017). Regulatory T cells in multiple sclerosis and myasthenia gravis. Journal of Neuroinflammation, Vol. 14. [CrossRef]
- Dawidowski, B., Górniak, A., Podwalski, P., Lebiecka, Z., Misiak, B., & Samochowiec, J. (2021). The role of cytokines in the pathogenesis of schizophrenia. Journal of Clinical Medicine, 10(17). [CrossRef]
- Desine, S., Hollister, B. M., Abdallah, K. E., Persaud, A., Hull, S. C., & Bonham, V. L. (2020). The Meaning of Informed Consent: Genome Editing Clinical Trials for Sickle Cell Disease. AJOB Empirical Bioethics, 11(4). [CrossRef]
- Dupont, A. C., Largeau, B., Ribeiro, M. J. S., Guilloteau, D., Tronel, C., & Arlicot, N. (2017). Translocator protein-18 kDa (TSPO) positron emission tomography (PET) imaging and its clinical impact in neurodegenerative diseases. International Journal of Molecular Sciences, Vol. 18. [CrossRef]
- Egli, M., & Manoharan, M. (2023). Chemistry, structure and function of approved oligonucleotide therapeutics. Nucleic Acids Research, 51(6). [CrossRef]
- Ekhator, C., Qureshi, M. Q., Zuberi, A. W., Hussain, M., Sangroula, N., Yerra, S., … Pendyala, P. R. (2023). Advances and Opportunities in Nanoparticle Drug Delivery for Central Nervous System Disorders: A Review of Current Advances. Cureus. [CrossRef]
- Evangelatos, G., Bamias, G., Kitas, G. D., Kollias, G., & Sfikakis, P. P. (2022). The second decade of anti-TNF-a therapy in clinical practice: new lessons and future directions in the COVID-19 era. Rheumatology International, Vol. 42. [CrossRef]
- Freire, M. A. M., Rocha, G. S., Bittencourt, L. O., Falcao, D., Lima, R. R., & Cavalcanti, J. R. L. P. (2023). Cellular and Molecular Pathophysiology of Traumatic Brain Injury: What Have We Learned So Far? Biology, Vol. 12. [CrossRef]
- Fu, S., Wang, Y., Xia, X., & Zheng, J. C. (2020). Exosome engineering: Current progress in cargo loading and targeted delivery. NanoImpact, Vol. 20. [CrossRef]
- Gao, C., Jiang, J., Tan, Y., & Chen, S. (2023). Microglia in neurodegenerative diseases: mechanism and potential therapeutic targets. Signal Transduction and Targeted Therapy, Vol. 8. [CrossRef]
- Girgis, R. R., Ciarleglio, A., Choo, T., Haynes, G., Bathon, J. M., Cremers, S., … Brown, A. S. (2018). A Randomized, Double-Blind, Placebo-Controlled Clinical Trial of Tocilizumab, An Interleukin-6 Receptor Antibody, for Residual Symptoms in Schizophrenia. Neuropsychopharmacology, 43(6). [CrossRef]
- Godoy, M. C. P., Tarelli, R., Ferrari, C. C., Sarchi, M. I., & Pitossi, F. J. (2008). Central and systemic IL-1 exacerbates neurodegeneration and motor symptoms in a model of Parkinson’s disease. Brain, 131(7). [CrossRef]
- Goines, P. E., & Ashwood, P. (2013). Cytokine dysregulation in autism spectrum disorders (ASD): Possible role of the environment. Neurotoxicology and Teratology, 36. [CrossRef]
- Goodin, D. S. (2014). Glucocorticoid treatment of multiple sclerosis. In Handbook of Clinical Neurology (Vol. 122). [CrossRef]
- Gunaydin, C., & Bilge, S. S. (2018). Effects of nonsteroidal anti-inflammatory drugs at the molecular level. Eurasian Journal of Medicine, Vol. 50. [CrossRef]
- Guo, Q., Jin, Y., Chen, X., Ye, X., Shen, X., Lin, M., … Zhang, J. (2024). NF-κB in biology and targeted therapy: new insights and translational implications. Signal Transduction and Targeted Therapy, Vol. 9. [CrossRef]
- Guthridge, J. M., Wagner, C. A., & James, J. A. (2022). The promise of precision medicine in rheumatology. Nature Medicine, Vol. 28. [CrossRef]
- Hampel, H., Caraci, F., Cuello, A. C., Caruso, G., Nisticò, R., Corbo, M., … Lista, S. (2020). A Path Toward Precision Medicine for Neuroinflammatory Mechanisms in Alzheimer’s Disease. Frontiers in Immunology, Vol. 11. [CrossRef]
- Han, Y., Yang, J., Fang, J., Zhou, Y., Candi, E., Wang, J., … Shi, Y. (2022). The secretion profile of mesenchymal stem cells and potential applications in treating human diseases. Signal Transduction and Targeted Therapy, Vol. 7. [CrossRef]
- Haney, M. J., Klyachko, N. L., Zhao, Y., Gupta, R., Plotnikova, E. G., He, Z., … Batrakova, E. V. (2015). Exosomes as drug delivery vehicles for Parkinson’s disease therapy. Journal of Controlled Release, 207. [CrossRef]
- He, Q., Liu, J., Liang, J., Liu, X., Li, W., Liu, Z., … Tuo, D. (2018). Towards improvements for penetrating the blood-brain barrier—recent progress from a material and pharmaceutical perspective. Cells, Vol. 7. [CrossRef]
- Heneka, M. T., Carson, M. J., Khoury, J. El, Landreth, G. E., Brosseron, F., Feinstein, D. L., … Kummer, M. P. (2015). Neuroinflammation in Alzheimer’s disease. The Lancet Neurology, Vol. 14. [CrossRef]
- Honig, L. S., Vellas, B., Woodward, M., Boada, M., Bullock, R., Borrie, M., … Siemers, E. (2018). Trial of Solanezumab for Mild Dementia Due to Alzheimer’s Disease. New England Journal of Medicine, 378(4). [CrossRef]
- Hu, X., li, J., Fu, M., Zhao, X., & Wang, W. (2021). The JAK/STAT signaling pathway: from bench to clinic. Signal Transduction and Targeted Therapy, Vol. 6. [CrossRef]
- Huang, X., Hussain, B., & Chang, J. (2021). Peripheral inflammation and blood–brain barrier disruption: effects and mechanisms. CNS Neuroscience and Therapeutics, 27(1). [CrossRef]
- Huang, Y., Guo, X., Wu, Y., Chen, X., Feng, L., Xie, N., & Shen, G. (2024). Nanotechnology’s frontier in combatting infectious and inflammatory diseases: prevention and treatment. Signal Transduction and Targeted Therapy, Vol. 9. [CrossRef]
- Isik, S., Yeman Kiyak, B., Akbayir, R., Seyhali, R., & Arpaci, T. (2023). Microglia Mediated Neuroinflammation in Parkinson’s Disease. Cells, Vol. 12. [CrossRef]
- Iyer, S. S., & Cheng, G. (2012). Role of interleukin 10 transcriptional regulation in inflammation and autoimmune disease. Critical Reviews in Immunology, 32(1). [CrossRef]
- Jellinger, K. A. (2010). Basic mechanisms of neurodegeneration: A critical update. Journal of Cellular and Molecular Medicine, 14(3). [CrossRef]
- Jones, K. L., Croen, L. A., Yoshida, C. K., Heuer, L., Hansen, R., Zerbo, O., … Van De Water, J. (2017). Autism with intellectual disability is associated with increased levels of maternal cytokines and chemokines during gestation. Molecular Psychiatry, 22(2). [CrossRef]
- Jung, S. M., & Kim, W. U. (2022). Targeted Immunotherapy for Autoimmune Disease. Immune Network, Vol. 22. [CrossRef]
- Kadry, H., Noorani, B., & Cucullo, L. (2020). A blood–brain barrier overview on structure, function, impairment, and biomarkers of integrity. Fluids and Barriers of the CNS, Vol. 17. [CrossRef]
- Kaduševičius, E. (2021). Novel applications of nsaids: Insight and future perspectives in cardiovascular, neurodegenerative, diabetes and cancer disease therapy. International Journal of Molecular Sciences, Vol. 22. [CrossRef]
- Khoshandam, M., Soltaninejad, H., Mousazadeh, M., Hamidieh, A. A., & Hosseinkhani, S. (2024). Clinical applications of the CRISPR/Cas9 genome-editing system: Delivery options and challenges in precision medicine. Genes and Diseases, Vol. 11. [CrossRef]
- Kim, K., Kim, H., Bae, S. H., Lee, S. Y., Kim, Y. H., Na, J., … Youn, H. (2020). [18F]CB251 PET/MR imaging probe targeting translocator protein (TSPO) independent of its Polymorphism in a Neuroinflammation Model. Theranostics, 10(20). [CrossRef]
- Kip, E., & Parr-Brownlie, L. C. (2023). Healthy lifestyles and wellbeing reduce neuroinflammation and prevent neurodegenerative and psychiatric disorders. Frontiers in Neuroscience, Vol. 17. [CrossRef]
- Knight, J. M., Costanzo, E. S., Singh, S., Yin, Z., Szabo, A., Pawar, D. S., … Drobyski, W. R. (2021). The IL-6 antagonist tocilizumab is associated with worse depression and related symptoms in the medically ill. Translational Psychiatry, 11(1). [CrossRef]
- Kouba, B. R., de Araujo Borba, L., Borges de Souza, P., Gil-Mohapel, J., & Rodrigues, A. L. S. (2024). Role of Inflammatory Mechanisms in Major Depressive Disorder: From Etiology to Potential Pharmacological Targets. Cells, Vol. 13. [CrossRef]
- Krishnarajah, S., & Becher, B. (2022). TH Cells and Cytokines in Encephalitogenic Disorders. Frontiers in Immunology, Vol. 13. [CrossRef]
- Kumar, M. A., Baba, S. K., Sadida, H. Q., Marzooqi, S. Al, Jerobin, J., Altemani, F. H., … Bhat, A. A. (2024). Extracellular vesicles as tools and targets in therapy for diseases. Signal Transduction and Targeted Therapy, Vol. 9. [CrossRef]
- Kumari, A., Kaur, A., & Aggarwal, G. (2023). The emerging potential of siRNA nanotherapeutics in treatment of arthritis. Asian Journal of Pharmaceutical Sciences, Vol. 18. [CrossRef]
- Kumari, S., Dhapola, R., Sharma, P., Singh, S. K., & Reddy, D. H. K. (2023). Implicative role of cytokines in neuroinflammation mediated AD and associated signaling pathways: Current progress in molecular signaling and therapeutics. Ageing Research Reviews, Vol. 92. [CrossRef]
- Kuwabara, T., Ishikawa, F., Kondo, M., & Kakiuchi, T. (2017). The Role of IL-17 and Related Cytokines in Inflammatory Autoimmune Diseases. Mediators of Inflammation, 2017. [CrossRef]
- Kwon, H. S., & Koh, S. H. (2020). Neuroinflammation in neurodegenerative disorders: the roles of microglia and astrocytes. Translational Neurodegeneration, Vol. 9. [CrossRef]
- Leal, M., Casabona, J., Puntel, M., & PITOSSI, F. (2013). Interleukin-1β and tumor necrosis factor-α: reliable targets for protective therapies in Parkinson’s Disease? . Frontiers in Cellular Neuroscience , 7.
- Lecca, D., Jung, Y. J., Scerba, M. T., Hwang, I., Kim, Y. K., Kim, S., … Greig, N. H. (2022). Role of chronic neuroinflammation in neuroplasticity and cognitive function: A hypothesis. Alzheimer’s and Dementia, 18(11). [CrossRef]
- Lee, J. H., Kam, E. H., Kim, J. M., Kim, S. Y., Kim, E. J., Cheon, S. Y., & Koo, B. N. (2017). Intranasal administration of interleukin-1 receptor antagonist in a transient focal cerebral ischemia rat model. Biomolecules and Therapeutics, 25(2). [CrossRef]
- Li, X., Li, C., Zhang, W., Wang, Y., Qian, P., & Huang, H. (2023). Inflammation and aging: signaling pathways and intervention therapies. Signal Transduction and Targeted Therapy, 8(1), 239. [CrossRef]
- Lin, C., Kong, Y., Chen, Q., Zeng, J., Pan, X., & Miao, J. (2024). Decoding sTREM2: its impact on Alzheimer’s disease – a comprehensive review of mechanisms and implications. Frontiers in Aging Neuroscience, 16. [CrossRef]
- Lindblad, C., Rostami, E., & Helmy, A. (2023). Interleukin-1 Receptor Antagonist as Therapy for Traumatic Brain Injury. Neurotherapeutics, Vol. 20. [CrossRef]
- Litman, T. (2019). Personalized medicine—concepts, technologies, and applications in inflammatory skin diseases. APMIS, Vol. 127. [CrossRef]
- Liu, J. Y., Chen, H. Y., Lin, J. J., Lu, M. K., Tan, H. P., Jang, F. L., & Lin, S. H. (2020). Alterations of plasma cytokine biomarkers for identifying age at onset of schizophrenia with neurological soft signs. International Journal of Medical Sciences, 17(2). [CrossRef]
- Liu, T. W., Chen, C. M., & Chang, K. H. (2022). Biomarker of Neuroinflammation in Parkinson’s Disease. International Journal of Molecular Sciences, Vol. 23. [CrossRef]
- Małkowska, P., & Sawczuk, M. (2023). Cytokines as Biomarkers for Evaluating Physical Exercise in Trained and Non-Trained Individuals: A Narrative Review. International Journal of Molecular Sciences, Vol. 24. [CrossRef]
- Mallah, K., Couch, C., Borucki, D. M., Toutonji, A., Alshareef, M., & Tomlinson, S. (2020). Anti-inflammatory and Neuroprotective Agents in Clinical Trials for CNS Disease and Injury: Where Do We Go From Here? Frontiers in Immunology, Vol. 11. [CrossRef]
- Mallick, R., Basak, S., Das, R. K., Banerjee, A., Paul, S., Pathak, S., & Duttaroy, A. K. (2024). Roles of the gut microbiota in human neurodevelopment and adult brain disorders. Frontiers in Neuroscience, 18.
- Mattar, C. N. Z., Chew, W. L., & Lai, P. S. (2024). Embryo and fetal gene editing: Technical challenges and progress toward clinical applications. Molecular Therapy Methods and Clinical Development, Vol. 32. [CrossRef]
- Meeker, K. L., Butt, O. H., Gordon, B. A., Fagan, A. M., Schindler, S. E., Morris, J. C., … Ances, B. M. (2022). Cerebrospinal fluid neurofilament light chain is a marker of aging and white matter damage. Neurobiology of Disease, 166. [CrossRef]
- Mitchell, M. J., Billingsley, M. M., Haley, R. M., Wechsler, M. E., Peppas, N. A., & Langer, R. (2021). Engineering precision nanoparticles for drug delivery. Nature Reviews Drug Discovery, Vol. 20. [CrossRef]
- Mithaiwala, M. N., Santana-Coelho, D., Porter, G. A., & O’connor, J. C. (2021). Neuroinflammation and the Kynurenine pathway in CNS disease: Molecular mechanisms and therapeutic implications. Cells, Vol. 10. [CrossRef]
- Mittal, K. R., Pharasi, N., Sarna, B., Singh, M., Rachana, Haider, S., … Jha, N. K. (2022). Nanotechnology-based drug delivery for the treatment of CNS disorders. Translational Neuroscience, Vol. 13. [CrossRef]
- Nady, D. S., Bakowsky, U., & Fahmy, S. A. (2023). Recent advances in brain delivery of synthetic and natural nano therapeutics: Reviving hope for Alzheimer’s disease patients. Journal of Drug Delivery Science and Technology, Vol. 89. [CrossRef]
- Naqvi, S., Panghal, A., & Flora, S. J. S. (2020). Nanotechnology: A Promising Approach for Delivery of Neuroprotective Drugs. Frontiers in Neuroscience, Vol. 14. [CrossRef]
- Noori, A. S., Rajabi, P., Sargolzaei, J., & Alaghmand, A. (2024). Correlation of biochemical markers and inflammatory cytokines in autism spectrum disorder (ASD). BMC Pediatrics, 24(1), 696. [CrossRef]
- Parambi, D. G. T., Alharbi, K. S., Kumar, R., Harilal, S., Batiha, G. E. S., Cruz-Martins, N., … Mathew, B. (2022). Gene Therapy Approach with an Emphasis on Growth Factors: Theoretical and Clinical Outcomes in Neurodegenerative Diseases. Molecular Neurobiology, Vol. 59. [CrossRef]
- Pardridge, W. M. (2020). Blood-Brain Barrier and Delivery of Protein and Gene Therapeutics to Brain. Frontiers in Aging Neuroscience, Vol. 11. [CrossRef]
- Pathak, D., & Sriram, K. (2023). Molecular Mechanisms Underlying Neuroinflammation Elicited by Occupational Injuries and Toxicants. International Journal of Molecular Sciences, Vol. 24. [CrossRef]
- Pathak, S., Nadar, R., Kim, S., Liu, K., Govindarajulu, M., Cook, P., … Moore, T. (2024). The Influence of Kynurenine Metabolites on Neurodegenerative Pathologies. International Journal of Molecular Sciences, Vol. 25. [CrossRef]
- Piehl, F. (2021). Current and emerging disease-modulatory therapies and treatment targets for multiple sclerosis. Journal of Internal Medicine, Vol. 289. [CrossRef]
- Pignataro, G., Cataldi, M., & Taglialatela, M. (2022). Neurological risks and benefits of cytokine-based treatments in coronavirus disease 2019: from preclinical to clinical evidence. British Journal of Pharmacology, Vol. 179. [CrossRef]
- Poletti, S., Mazza, M. G., & Benedetti, F. (2024). Inflammatory mediators in major depression and bipolar disorder. Translational Psychiatry, 14(1), 247. [CrossRef]
- Postolache, T. T., Wadhawan, A., Can, A., Lowry, C. A., Woodbury, M., Makkar, H., … Stiller, J. W. (2020). Inflammation in traumatic brain injury. Journal of Alzheimer’s Disease, Vol. 74. [CrossRef]
- Qin, J., Ma, Z., Chen, X., & Shu, S. (2023). Microglia activation in central nervous system disorders: A review of recent mechanistic investigations and development efforts. Frontiers in Neurology, Vol. 14. [CrossRef]
- Ramesh, G., Maclean, A. G., & Philipp, M. T. (2013). Cytokines and chemokines at the crossroads of neuroinflammation, neurodegeneration, and neuropathic pain. Mediators of Inflammation, 2013. [CrossRef]
- Reichardt, S. D., Amouret, A., Muzzi, C., Vettorazzi, S., Tuckermann, J. P., Lühder, F., & Reichardt, H. M. (2021). The role of glucocorticoids in inflammatory diseases. Cells, Vol. 10. [CrossRef]
- Rhie, S. J., Jung, E. Y., & Shim, I. (2020). The role of neuroinflammation on pathogenesis of affective disorders. Journal of Exercise Rehabilitation, Vol. 16. [CrossRef]
- Rider, P., Carmi, Y., & Cohen, I. (2016). Biologics for Targeting Inflammatory Cytokines, Clinical Uses, and Limitations. International Journal of Cell Biology, Vol. 2016. [CrossRef]
- Ridker, P. M., & Rane, M. (2021). Interleukin-6 Signaling and Anti-Interleukin-6 Therapeutics in Cardiovascular Disease. Circulation Research, Vol. 128. [CrossRef]
- Rodríguez-Gómez, J. A., Kavanagh, E., Engskog-Vlachos, P., Engskog, M. K. R., Herrera, A. J., Espinosa-Oliva, A. M., … Burguillos, M. A. (2020). Microglia: Agents of the CNS Pro-Inflammatory Response. Cells, Vol. 9. [CrossRef]
- Rosenzweig, J. M., Lei, J., & Burd, I. (2014). Interleukin-1 receptor blockade in perinatal brain injury. Frontiers in Pediatrics, Vol. 2. [CrossRef]
- Schimmel, S., Acosta, S., & Lozano, D. (2017). Neuroinflammation in traumatic brain injury: A chronic response to an acute injury. Brain Circulation, 3(3). [CrossRef]
- Schwartz, D. M., Kanno, Y., Villarino, A., Ward, M., Gadina, M., & O’Shea, J. J. (2017). JAK inhibition as a therapeutic strategy for immune and inflammatory diseases. Nature Reviews Drug Discovery, Vol. 16. [CrossRef]
- Sedger, L. M., & McDermott, M. F. (2014). TNF and TNF-receptors: From mediators of cell death and inflammation to therapeutic giants - past, present and future. Cytokine and Growth Factor Reviews, Vol. 25. [CrossRef]
- Sen, S., Xavier, J., Kumar, N., Ahmad, M. Z., & Ranjan, O. P. (2023). Exosomes as natural nanocarrier-based drug delivery system: recent insights and future perspectives. 3 Biotech, Vol. 13. [CrossRef]
- Shawky, A. M., Almalki, F. A., Abdalla, A. N., Abdelazeem, A. H., & Gouda, A. M. (2022). A Comprehensive Overview of Globally Approved JAK Inhibitors. Pharmaceutics, Vol. 14. [CrossRef]
- Shi, Y., Riese, D. J., & Shen, J. (2020). The Role of the CXCL12/CXCR4/CXCR7 Chemokine Axis in Cancer. Frontiers in Pharmacology, Vol. 11. [CrossRef]
- Simon, D. W., McGeachy, M. J., Baylr, H., Clark, R. S. B., Loane, D. J., & Kochanek, P. M. (2017). The far-reaching scope of neuroinflammation after traumatic brain injury. Nature Reviews Neurology, Vol. 13. [CrossRef]
- Smith, J. A., Das, A., Ray, S. K., & Banik, N. L. (2012). Role of pro-inflammatory cytokines released from microglia in neurodegenerative diseases. Brain Research Bulletin, Vol. 87. [CrossRef]
- Sochocka, M., Diniz, B. S., & Leszek, J. (2017). Inflammatory Response in the CNS: Friend or Foe? Molecular Neurobiology, Vol. 54. [CrossRef]
- Solanki, R., Karande, A., & Ranganathan, P. (2023). Emerging role of gut microbiota dysbiosis in neuroinflammation and neurodegeneration. Frontiers in Neurology, Vol. 14. [CrossRef]
- Su, Y., Sun, B., Gao, X., Dong, X., Fu, L., Zhang, Y., … Han, B. (2020). Intranasal Delivery of Targeted Nanoparticles Loaded With miR-132 to Brain for the Treatment of Neurodegenerative Diseases. Frontiers in Pharmacology, 11. [CrossRef]
- Suganya, K., & Koo, B. S. (2020). Gut–brain axis: Role of gut microbiota on neurological disorders and how probiotics/prebiotics beneficially modulate microbial and immune pathways to improve brain functions. International Journal of Molecular Sciences, Vol. 21. [CrossRef]
- Tamura, T., Cheng, C., Chen, W., Merriam, L. T., Athar, H., Kim, Y. H., … Kim, E. Y. (2023). Single-cell transcriptomics reveal a hyperacute cytokine and immune checkpoint axis after cardiac arrest in patients with poor neurological outcome. Med, 4(7). [CrossRef]
- Tansey, M. G., & Goldberg, M. S. (2010). Neuroinflammation in Parkinson’s disease: Its role in neuronal death and implications for therapeutic intervention. Neurobiology of Disease, Vol. 37. [CrossRef]
- Taylor, M. A., & Kokiko-Cochran, O. N. (2024). Context is key: glucocorticoid receptor and corticosteroid therapeutics in outcomes after traumatic brain injury. Frontiers in Cellular Neuroscience, Vol. 18. [CrossRef]
- Turner, M. D., Nedjai, B., Hurst, T., & Pennington, D. J. (2014). Cytokines and chemokines: At the crossroads of cell signalling and inflammatory disease. Biochimica et Biophysica Acta - Molecular Cell Research, Vol. 1843. [CrossRef]
- Ullah, H., Arbab, S., Tian, Y., Liu, C. Q., Chen, Y., Qijie, L., … Li, K. (2023). The gut microbiota–brain axis in neurological disorder. Frontiers in Neuroscience, Vol. 17. [CrossRef]
- Uzuegbunam, B. C., Rummel, C., Librizzi, D., Culmsee, C., & Hooshyar Yousefi, B. (2023). Radiotracers for Imaging of Inflammatory Biomarkers TSPO and COX-2 in the Brain and in the Periphery. International Journal of Molecular Sciences, Vol. 24. [CrossRef]
- Valera, E., & Masliah, E. (2016). Combination therapies: The next logical Step for the treatment of synucleinopathies? Movement Disorders, Vol. 31. [CrossRef]
- Vieira, C. P., Lelis, C. A., Ochioni, A. C., Rosário, D. K. A., Rosario, I. L. S., Vieira, I. R. S., … Junior, C. A. C. (2024). Estimating the therapeutic potential of NSAIDs and linoleic acid-isomers supplementation against neuroinflammation. Biomedicine & Pharmacotherapy, 177, 116884. [CrossRef]
- Vilotić, A., Nacka-Aleksić, M., Pirković, A., Bojić-Trbojević, Ž., Dekanski, D., & Jovanović Krivokuća, M. (2022). IL-6 and IL-8: An Overview of Their Roles in Healthy and Pathological Pregnancies. International Journal of Molecular Sciences, Vol. 23. [CrossRef]
- Wang, D., Tai, P. W. L., & Gao, G. (2019). Adeno-associated virus vector as a platform for gene therapy delivery. Nature Reviews Drug Discovery, Vol. 18. [CrossRef]
- Wang, J.-H., Gessler, D. J., Zhan, W., Gallagher, T. L., & Gao, G. (2024). Adeno-associated virus as a delivery vector for gene therapy of human diseases. Signal Transduction and Targeted Therapy, 9(1), 78. [CrossRef]
- Wang, K., Zhu, Y., Liu, K., Zhu, H., & Ouyang, M. (2024). Adverse events of biologic or small molecule therapies in clinical trials for inflammatory bowel disease: A systematic review and meta-analysis. Heliyon, 10(4). [CrossRef]
- Wang, W. Y., Tan, M. S., Yu, J. T., & Tan, L. (2015). Role of pro-inflammatory cytokines released from microglia in Alzheimer’s disease. Annals of Translational Medicine, Vol. 3. [CrossRef]
- Winkle, M., El-Daly, S. M., Fabbri, M., & Calin, G. A. (2021). Noncoding RNA therapeutics — challenges and potential solutions. Nature Reviews Drug Discovery, Vol. 20. [CrossRef]
- Wong, B., Birtch, R., Rezaei, R., Jamieson, T., Crupi, M. J. F., Diallo, J. S., & Ilkow, C. S. (2023). Optimal delivery of RNA interference by viral vectors for cancer therapy. Molecular Therapy, Vol. 31. [CrossRef]
- Wong-Guerra, M., Calfio, C., Maccioni, R. B., & Rojo, L. E. (2023). Revisiting the neuroinflammation hypothesis in Alzheimer’s disease: a focus on the druggability of current targets. Frontiers in Pharmacology, Vol. 14. [CrossRef]
- Wongrakpanich, S., Wongrakpanich, A., Melhado, K., & Rangaswami, J. (2018). A comprehensive review of non-steroidal anti-inflammatory drug use in the elderly. Aging and Disease, Vol. 9. [CrossRef]
- Wu, J. R., Hernandez, Y., Miyasaki, K. F., & Kwon, E. J. (2023). Engineered nanomaterials that exploit blood-brain barrier dysfunction for delivery to the brain. Advanced Drug Delivery Reviews, Vol. 197. [CrossRef]
- Yan, M., Sun, Z., Zhang, S., Yang, G., Jiang, X., Wang, G., … Tian, X. (2024). SOCS modulates JAK-STAT pathway as a novel target to mediate the occurrence of neuroinflammation: Molecular details and treatment options. Brain Research Bulletin, 213, 110988. [CrossRef]
- Yi, M., Li, T., Niu, M., Zhang, H., Wu, Y., Wu, K., & Dai, Z. (2024). Targeting cytokine and chemokine signaling pathways for cancer therapy. Signal Transduction and Targeted Therapy, 9(1), 176. [CrossRef]
- Yonezawa, S., Koide, H., & Asai, T. (2020). Recent advances in siRNA delivery mediated by lipid-based nanoparticles. Advanced Drug Delivery Reviews, Vol. 154–155. [CrossRef]
- Yuan, T., Tang, H., Xu, X., Shao, J., Wu, G., Cho, Y. C., … Liang, G. (2023). Inflammation conditional genome editing mediated by the CRISPR-Cas9 system. IScience, 26(6). [CrossRef]
- Yuan, Y. H., Liu, J., You, Y. G., Chen, X. H., Yuan, L. C., Wen, Y., … Zhang, Y. (2021). Transcriptomic Analysis of Mycobacterium leprae-Stimulated Response in Peripheral Blood Mononuclear Cells Reveal Potential Biomarkers for Early Diagnosis of Leprosy. Frontiers in Cellular and Infection Microbiology, 11. [CrossRef]
- Zakari, S., Niels, N. K., Olagunju, G. V., Nnaji, P. C., Ogunniyi, O., Tebamifor, M., … Ogunlana, O. O. (2024). Emerging biomarkers for non-invasive diagnosis and treatment of cancer: a systematic review. Frontiers in Oncology, 14. [CrossRef]
- Zhang, J., Zhang, Y., Wang, J., Xia, Y., Zhang, J., & Chen, L. (2024). Recent advances in Alzheimer’s disease: mechanisms, clinical trials and new drug development strategies. Signal Transduction and Targeted Therapy, 9(1), 211. [CrossRef]
- Zhang, R., Liu, Y., Yan, K., Chen, L., Chen, X. R., Li, P., … Jiang, X. D. (2013). Anti-inflammatory and immunomodulatory mechanisms of mesenchymal stem cell transplantation in experimental traumatic brain injury. Journal of Neuroinflammation, 10. [CrossRef]
- Zhang, W., Xiao, D., Mao, Q., & Xia, H. (2023). Role of neuroinflammation in neurodegeneration development. Signal Transduction and Targeted Therapy, Vol. 8. [CrossRef]
- Zhang, Y., Wang, J., Ye, Y., Zou, Y., Chen, W., Wang, Z., & Zou, Z. (2023). Peripheral cytokine levels across psychiatric disorders: A systematic review and network meta-analysis. Progress in Neuro-Psychopharmacology and Biological Psychiatry, Vol. 125. [CrossRef]
- Zhao, Y., Gan, L., Ren, L., Lin, Y., Ma, C., & Lin, X. (2022). Factors influencing the blood-brain barrier permeability. Brain Research, 1788. [CrossRef]
- Zhou, R., Ji, B., Kong, Y., Qin, L., Ren, W., Guan, Y., & Ni, R. (2021). PET Imaging of Neuroinflammation in Alzheimer’s Disease. Frontiers in Immunology, Vol. 12. [CrossRef]
- Zhou, Z., Zhang, R., Zhou, A., Lv, J., Chen, S., Zou, H., … Liu, Z. (2024). Proteomics appending a complementary dimension to precision oncotherapy. Computational and Structural Biotechnology Journal, 23, 1725–1739. [CrossRef]
- Zhuang, W. Z., Lin, Y. H., Su, L. J., Wu, M. S., Jeng, H. Y., Chang, H. C., … Ling, T. Y. (2021). Mesenchymal stem/stromal cell-based therapy: mechanism, systemic safety and biodistribution for precision clinical applications. Journal of Biomedical Science, Vol. 28. [CrossRef]
- Zipp, F., Bittner, S., & Schafer, D. P. (2023). Cytokines as emerging regulators of central nervous system synapses. Immunity, Vol. 56. [CrossRef]
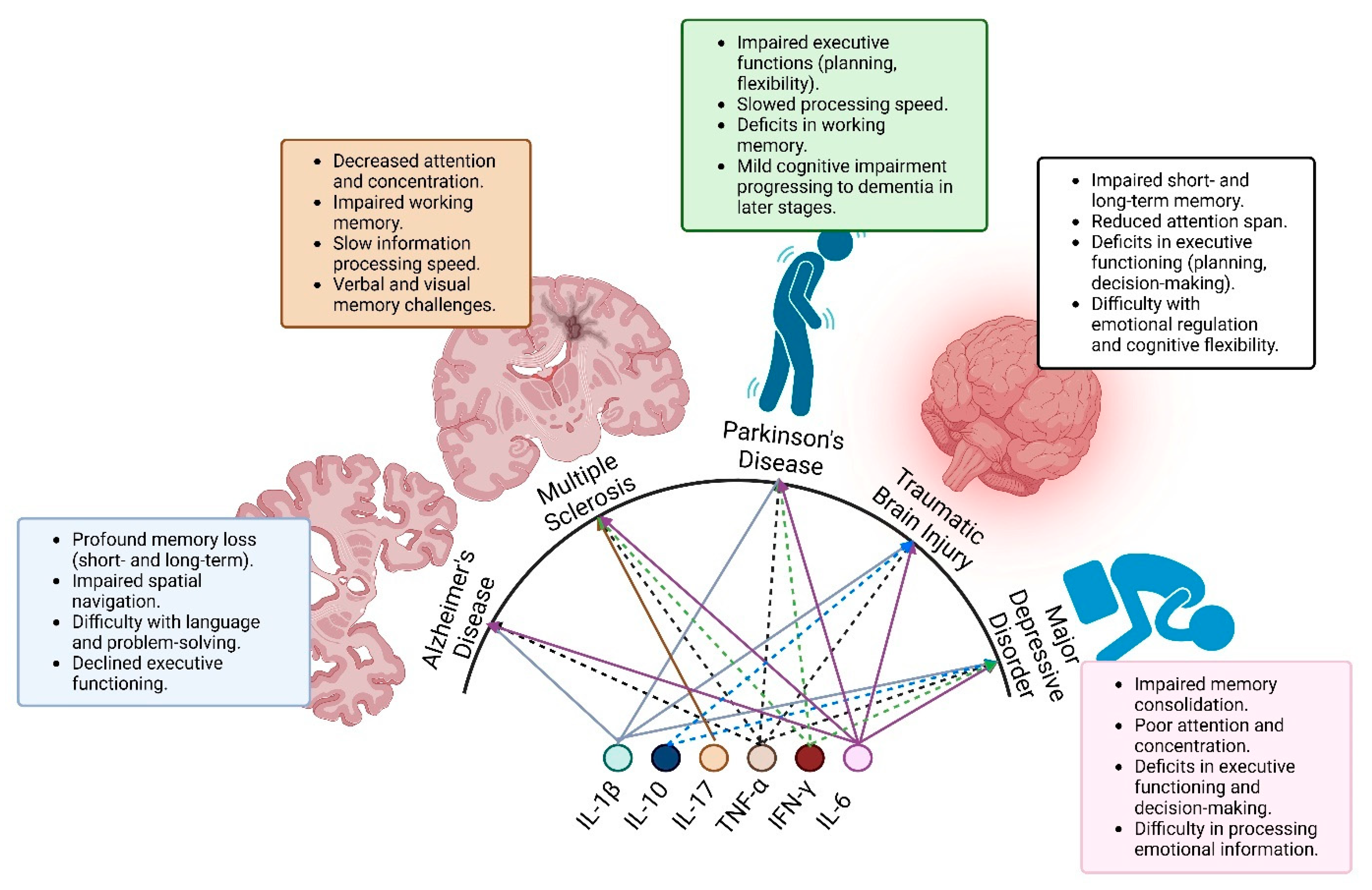
| Disorder | Key Cytokines | Pathophysiological Role | Potential Therapeutic Target |
|---|---|---|---|
| AD | IL-1β, TNF-α, IL-6 | Promotes amyloid aggregation, neurotoxicity | Anti-TNF therapies (e.g., infliximab) |
| MS | IFN-γ, IL-17, TNF-α, IL-6 | Activates immune cells, demyelination | Anti-IL-17 monoclonal antibodies |
| MDD | IL-6, TNF-α, IFN-γ, IL-17, IL-10, IL-1β | Induces HPA axis dysregulation, neuronal apoptosis | Anti-IL-6 agents (e.g., tocilizumab) |
| PD | IL-1β, TNF-α, IL-6, IFN-γ | Microglial activation, dopaminergic neuron loss | Microglia inhibitors |
| TBI | IL-1β, IL-10, TNF-α, IL-6 | Acute inflammation, secondary injury cascade | Cytokine modulators |
| Therapy | Condition | Phase | Key Findings |
|---|---|---|---|
| Tocilizumab | Depression | Phase II | Reduced inflammatory markers, improved mood |
| Infliximab | AD | Phase II | Attenuated neuroinflammation, early efficacy |
| JAK Inhibitors (Tofacitinib) | MS | Phase I | Reduced immune cell infiltration |
| IL-17 Monoclonal Antibody | MS | Phase III | Decreased relapse rates |
| Microbiome Therapies | PD | Phase I | Modulation of systemic inflammation |
| Therapy Type | Example Agents | Targeted Cytokines | Status (Preclinical/Clinical) |
|---|---|---|---|
| Biologics | Infliximab, Tocilizumab | TNF-α, IL-6 | Clinical Phase II–III |
| Small Molecules | JAK inhibitors (ruxolitinib) | JAK/STAT pathway | Clinical Phase I–II |
| Antisense Oligonucleotides | N/A | IL-1β | Preclinical |
| Gene Therapy | CRISPR/Cas9 | TNF-α and IL-6 | Preclinical |
| Microbiome Therapies | Probiotics, Prebiotics | Gut-derived cytokines | Clinical Phase I |
| Technology | Mechanism | Advantages | Challenges |
| Nanoparticles | Targeted drug release | High specificity, BBB penetration | Variability in BBB uptake |
| Focused Ultrasound | Temporary BBB disruption | Non-invasive, real-time control | Risk of tissue damage |
| Liposomes | Encapsulation of drugs | Reduced systemic toxicity | Limited CNS targeting |
| Receptor-Mediated Transport | Ligand-receptor interaction | Enhanced BBB transport | Requires specific ligand design |
| Hydrogels | Localized release | Sustained delivery at target site | Limited mobility for CNS-wide effects |
| Biomarker Type | Source (CSF/Blood) | Diagnostic Use | Current Status |
| Cytokines (IL-6, IL-1β) | Blood | Monitor systemic inflammation | Validated for clinical use |
| Extracellular Vesicles | CSF/Blood | Indicator of CNS injury | Experimental |
| Neurofilament Light (NFL) | CSF/Blood | Axonal damage detection | Approved for Alzheimer’s monitoring |
| Proteomic Signatures | Blood/CSF | Disease-specific inflammatory profile | Under investigation |
| Imaging Biomarkers | PET scans, MRI | Visualization of neuroinflammation | Validated for research |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





