Introduction
Fall-related injuries (FRIs) are a prevalent cause of hospitalization among adults over 65 years of age.[
1] In the older adults population, falls are intertwined with psychological distress, health complications, a decline in quality of life and even death. [
2,
3,
4,
5] To date, FRIs are the second-largest contributor to the economic burden in hospitalization, and once they occur, will have implications on directly or indirectly affected parties (e.g., families, caregivers, healthcare system, ...).[
6,
7]
Potential solutions include nutrition strategies,[
8] hip fracture protectors (HPs),[
9,
10] fall risk detection systems,11 and adapted routines or living spaces.[
12] Recent statistics collected in both Canada and the United-States are suggesting an increase in FRIs and a projected growth.[
13,
14] Based on these results, we hypothesize that the existing solutions may not adequately meet the criteria for addressing the contemporary implications of FRIs in North America.
Among FRIs, hip fractures lead to greater risk of death and disability and substantial healthcare costs.
15, 16 Inflatable HPs is a special class of HPs. It relies on an airbag deployment system which can yield higher impact absorption.[
17] Although they may be effective in theory, adoption of potentially effective inflatable HPs in the older population will be instrumental in successfully studying its applicability in society and preventing FRIs.[
18,
19]
We hypothesize that the successful adoption of our prototype
Air-Sequr, an intelligent inflatable HP (IIHP), into the lifestyles of older adults is contingent upon its acceptance.[
20] We incorporated a
human-centered design approach in our program,[
21] and now sought to evaluate its acceptance amongst older adults. In this context, we developed a 20-minutes questionnaire to assess acceptance, based on literature precedence.[
22] We used an interviewer-administered approach on a random sample of older adults in a retirement home.
Material & Methods
Distastes, discomfort, side effects, and relative complexity (of use) are listed as barriers to the acceptance of HPs.[
23] We hypothesized that similar parameters will affect the acceptance of inflatable HP garments such as our
Air-Sequr prototype. Consequently, we built a questionnaire to probe the above-mentioned barriers categorized into ease of use and comfort, utilizing a Likert scale as a psychometric tool.[
24] We excluded esthetics as an evaluation category due to previous investigations not presented in this study, which suggested an overall positive feedback. The questions relating to perception and utility were formulated as 'yes' or 'no'.
Participants
All participants were new to our technological garment. They were recruited immediately on-site if they expressed a willingness to participate and were not compensated prior to participation. All interviewed participants were assumed French speaking and 65 years of age or above, except for one participant being 55 years of age. All interviewed participants were deemed physically, and cognitively capable of being part of our study by our healthcare professional and were familiar with FRIs and associated health consequences.
Data Collection
After explaining the objective of the study and obtaining the oral consent of the participant, an online survey was used to collect anonymized responses to our questionnaire. Prior to data collection, we designated a full section of questions to participants’ perceptions towards falls by inquiring about direct or indirect fall experiences. This was done to ensure uniformity among the sample, as perceptions of falls are linked to acceptance of protective devices.[
20] Participants were asked to agree or disagree using a 5-point Likert scale, where 5 indicated strongly agree, 4 indicated agree, 3 indicated neutral, 2 indicated disagree, and 1 indicated strongly disagree. The study did not collect sensitive information and hence was not part of any committee review process.
We clustered three questions on perceived ease of use: putting on, removing it, and weight. These metrics were chosen because they directly assess the practicality of using our Air-Sequr IIHP prototype in everyday situations. Weight was viewed as mainly influencing ease of use due to movement impairment, albeit with potential effects on comfort. We then selected four questions on perceived comfort: garment fabric, sitting, standing up, and walking. These aspects were included to evaluate how comfortable the IIHP is during various activities. Finally, to understand perceived utility was evaluated by probing perceived effectiveness and purchase intentions.
Data Analysis
In total, we collected data from 18 participants, but 2 were excluded due to refusal to wear the IIHP. The 16 completed questionnaires were used in the acceptance evaluation. Most of the 16 participants were females (87.5%) with an average age of 82.4 years (median = 85.5, mode = 89, STD = 9.5). All user characteristic data were not verified.
Upon completion and compilation of the data, we processed the data in means, medians, standard deviations and confidence intervals (P=95%) for each Likert Scale metrics.
Study Setting
The study was conducted in a private senior care home situated in the remote areas of Montreal (Quebec, Canada). The selection of this location was based on relevance of its occupants to our study, effective communication with the management, and the independence of its occupants.
Interviews were executed using a protocol to ensure uniform question formulation, consistent user experience, and favor ease of data collection. We set up five stations and an adapted setting inspired by a previously published acceptance study.[
22] Participants were asked questions over a 20-minutes questionnaire period by one of the trained interviewers. The station setup and the atmosphere during the interview process were engineered to be professional, yet comfortable, to provide an overall pleasant experience.
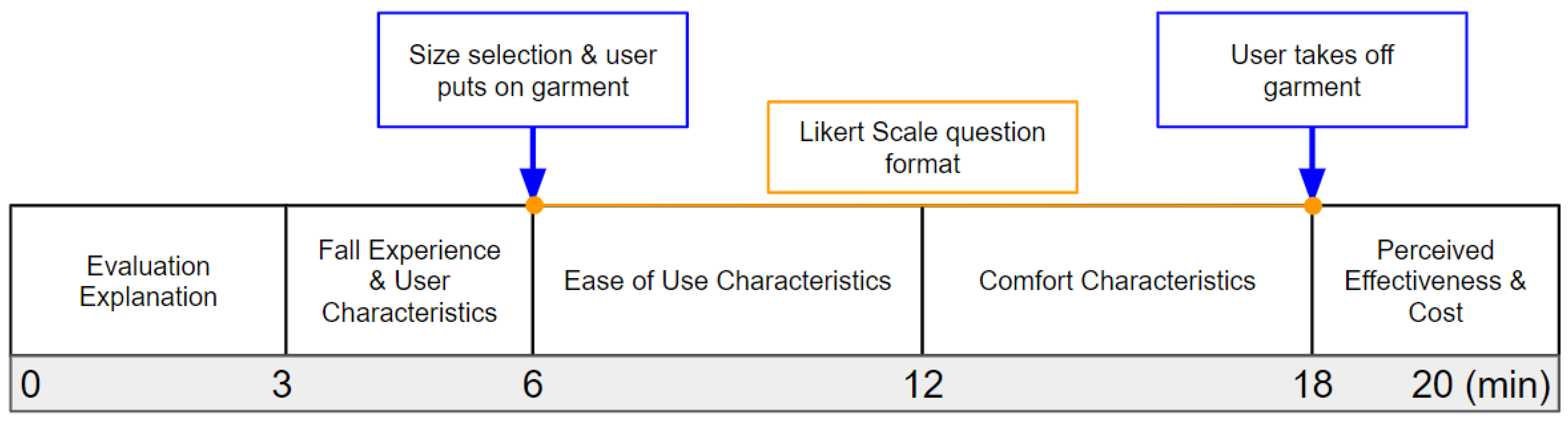
A typical interview process is summarized in
Figure 1. First, a volunteer welcomes the participant and directs them to the interviewer. The interviewer then explains the study and obtains consent for the collection of data, including questionnaire answers, age, and sex. The participant is subsequently asked to provide information about their fall experiences and share relevant characteristics. Following this, the participant puts on the garment over their clothing and answers the questionnaire using a 5-point Likert scale format.[
24] Finally, the user is asked to remove the garment, watch a 20-seconds video demonstrating how
Air-Sequr IIHP prototype works, and evaluate the ease of removal, intention of purchase and perceived effectiveness. Once the interview process was completed, the participant was asked to provide feedback outside the scope of this study to one of our volunteers and given a low-value participation gift regardless of their feedback quality or the information shared during the interview.
Device
The system used in this study is Air-Sequr IIHP prototype. It consists of an outer polyester cover, serving as the garment and an integrated airbag system. This polyester cover integrates an airbag system which incorporates gas cartridges and electronics that predict falls using our machine-learning algorithms.
Results
We compiled the 9-questions Likert scale feedback from participants into mean, median, and range as shown in
Table 1. The perceived ease of use was evaluated using the Likert score on ease of removal, putting on, and the weight of our
Air-Sequr IIHP prototype. The perceived comfort was evaluated by garment fabric, comfort while sitting, standing up, and walking. Finally, we sought to validate these acceptance metrics by evaluating perceptions of the utility of our IIHP on fracture protection efficiency and purchase intention compiled as shown in
Table 2.
Discussion
Ease of Use
Participants rated the ease of putting on and removing the Air-Sequr IIHP prototype with mean scores of 4.31 and 4.44, respectively, and median scores of 4.50 and 5.00. These positive ratings indicate that most users found the IIHP convenient to manipulate. The relatively low standard deviations of 0.70 and 0.81 for putting on and removing respectively reflect a consistent user experience across the sample, suggesting that the design of our Air-Sequr IIHP prototype accommodates a wide range of abilities and minimizes the risk of user error or difficulty. While the additional mass from the inflatable modules negatively impacts the weight, as indicated by the above-neutral score (mean: 3.22, median: 3.50), it may serve as a necessary trade-off for enhanced protection and is not negatively perceived by the users.
Our study's findings on the ease of use of the Air-Sequr prototype are encouraging and suggest that this device could be an easy-to-use option for older adults seeking additional protection against falls. The high ease-of-use scores likely result from several design features, particularly the garment's ability to be worn like regular clothing.
Perceived Comfort
The IIHP was evaluated on several dimensions of comfort, including garment fabric, sitting, standing up, and walking.
Participants rated the comfort of the garment fabric with a mean score of 4.59 and a median score of 5.00, reflecting a positive perception. The standard deviation of 0.51 indicates that this comfort rating was consistent among the participants. The high score for garment fabric suggests that the material used in the intelligent inflatable Air-Sequr prototype is soft, non-irritating and positively perceived, which are essential qualities for a device intended for prolonged use.
The comfort ratings for various activities, including sitting (mean = 4.36, median = 4.00), standing up (mean = 4.60, median = 5.00), and walking (mean = 4.57, median = 5.00), were all positively perceived. These scores suggest that the Air-Sequr IIHP prototype does not significantly impede movement or cause discomfort during these specific activities. The consistency in comfort ratings across different postures and movements, as indicated by standard deviations of 0.63, 0.51, and 0.51 for sitting, standing up, and walking, respectively, suggests a similar user experience among participants in these activities. The positive and consistent comfort metrics obtained may indicate that our IIHP is suitable for everyday use, allowing users to engage in routine activities with minimal discomfort.
Perceived Protection & Purchase Intention
We addressed participants' perceived protection and purchase intention for the
Air-Sequr IIHP prototype. All participants (100%) believed they would be protected in the event of a fall when wearing our
Air-Sequr prototype. This unanimous response underscores the device’s perceived effectiveness in providing impact protection after viewing our demonstration video. The high confidence in the IIHP’s protective capability is crucial, as it directly influences the willingness to wear the device regularly and enhances overall acceptance.[
20] Furthermore, a majority (75%) of participants expressed a willingness to buy the
Air-Sequr IIHP prototype HFP. The positive purchase intentions may be linked to the favorable acceptance metrics observed in our study.
Conclusions
By focusing on a user-centered design approach, we developed an accepted device among older adults in the study. Our Air-Sequr IIHP prototype demonstrates promising potential for reducing fall-related injuries if effective and adopted. Future evaluation should continue in pre-clinical application and assessment of its acceptance and effectiveness should be conducted in a larger and more diverse older adult population.
Data Availability Statement
The protocol and data underlying this study are available upon request.
Acknowledgment
We are thankful to Les Habitations Bordeleaux for their support. We thank our staff for their contributions: J. Haddad, A. Dalbec-Constant, K., Sellamou, A. and Hamrouni, K.
Notes
| 1 |
NS declares no conflict of interests. NMM, MB and PL have financial interests Air-Sequr IIHP prototype. All authors have approved the final version of this manuscript. |
References
- Rau, C.-S.; Lin, T.-S.; Wu, S.-C.; Yang, J.C.-S.; Hsu, S.-Y.; Cho, T.-Y.; Hsieh, C.-H. Geriatric hospitalizations in fall-related injuries. Scand. J. Trauma, Resusc. Emerg. Med. 2014, 22, 63–63, . [CrossRef]
- Ribeiro, O.; Santos, .R. Psychological Correlates of Fear of Falling in the Elderly. Educ. Gerontol. 2014, 41, 69–78, . [CrossRef]
- Durgun, H.; Turan, N.; Kaya, H. Relationship between fall behavior and quality of life of elderly individuals. Psychol. Heal. Med. 2021, 27, 1366–1372, . [CrossRef]
- Goswami, N., Falls and fall-prevention in older persons: geriatrics meets spaceflight! Frontiers in physiology 2017, 8, 603.
- Zulfiqar, A.-A.; Habchi, P.; Dembele, I.A.; Andres, E. Association of Frailty Status with Risk of Fall among Hospitalized Elderly Patients: A Cross-Sectional Study in an Acute Geriatric Unit. Medicines 2022, 9, 48, . [CrossRef]
- Faes, M.C.; Reelick, M.F.; Banningh, L.W.J.-W.; de Gier, M.; Esselink, R.A.; Rikkert, M.G.O. Qualitative study on the impact of falling in frail older persons and family caregivers: Foundations for an intervention to prevent falls. Aging Ment. Heal. 2010, 14, 834–842, . [CrossRef]
- Gelbard, R.; Inaba, K.; Okoye, O.T.; Morrell, M.; Saadi, Z.; Lam, L.; Talving, P.; Demetriades, D. Falls in the elderly: a modern look at an old problem. Am. J. Surg. 2014, 208, 249–253, . [CrossRef]
- A Bischoff, H.; Stähelin, H.B.; Dick, W.; Akos, R.; Knecht, M.; Salis, C.; Nebiker, M.; Theiler, R.; Pfeifer, M.; Begerow, B.; et al. Effects of Vitamin D and Calcium Supplementation on Falls: A Randomized Controlled Trial. J. Bone Miner. Res. 2003, 18, 343–351, . [CrossRef]
- Kannus, P.; Parkkari, J.; Niemi, S.; Pasanen, M.; Palvanen, M.; Järvinen, M.; Vuori, I. Prevention of Hip Fracture in Elderly People with Use of a Hip Protector. New Engl. J. Med. 2000, 343, 1506–1513, . [CrossRef]
- Wang, J.; Sun, Y.; Chen, Z.; Jin, Y.; Xu, Y. [Design and Research of Wearable Fall Protection Device for the Elderly]. Zhongguo Yi Liao Qi Xie Za Zhi 2023, 47, 278–283.
- Singh, A.; Rehman, S.U.; Yongchareon, S.; Chong, P.H.J. Sensor Technologies for Fall Detection Systems: A Review. IEEE Sensors J. 2020, 20, 6889–6919, . [CrossRef]
- Vieira, E.R.; Palmer, R.C.; Chaves, P.H. Prevention of falls in older people living in the community. BMJ 2016, 353, i1419, . [CrossRef]
- nbsp;CDC. Keep on Your Feet—Preventing Older Adult Falls. Available online: https://www.cdc.gov/injury/features/older-adult-falls/index.html (accessed on 4 April 2021).
- Surveillance report on falls among older adults in Canada. https://www.canada.ca/en/public-health/services/publications/healthy-living/surveillance-report-falls-older-adults-canada.html.
- Nilsson, M.; Eriksson, J.; Larsson, B.; Odén, A.; Johansson, H.; Lorentzon, M., Fall risk assessment predicts fall-related injury, hip fracture, and head injury in older adults. Journal of the American Geriatrics Society 2016, 64 (11), 2242-2250.
- Chou, S.-E.; Rau, C.-S.; Tsai, Y.-C.; Hsu, S.-Y.; Hsieh, H.-Y.; Hsieh, C.-H. Risk factors and complications contributing to mortality in elderly patients with fall-induced femoral fracture: A cross-sectional analysis based on trauma registry data of 2,407 patients. Int. J. Surg. 2019, 66, 48–52, . [CrossRef]
- Duma, S.; Caine, J.; Coleman, D.; Langmead, M.; Leung, K.; Ng, T.; Weatherholtz, J.; Whitehair, M.; Wilson, K. In Development of an inflatable hip protection system: design for hip fracture prevention and increased compliance, Annual Meeting of the American Society of Biomechanics, Blacksburg, VA, 2006.
- Renaud, K.; Van Biljon, J. In Predicting technology acceptance and adoption by the elderly: a qualitative study, Proceedings of the 2008 annual research conference of the South African Institute of Computer Scientists and Information Technologists on IT research in developing countries: riding the wave of technology, 2008; pp 210-219.
- Howland, J.; Peterson, E.; Kivell, E. Hip protectors efficacy and barriers to adoption to prevent fall-related injuries in older adults: Findings and recommendations from an international workgroup. J. Saf. Res. 2006, 37, 421–424, . [CrossRef]
- Taherdoost, H. A review of technology acceptance and adoption models and theories. Procedia Manuf. 2018, 22, 960–967, . [CrossRef]
- Andrews, S.R. Human-centred design research during the pandemic: using an online survey to inform personas of women at risk of hip fracture. Des. Heal. 2023, 1–13, . [CrossRef]
- Park, J.H.; Lee, J.R. Wearing Evaluation of the Fall Impact Protective Pants for the Elderly Women. J. Korean Soc. Cloth. Text. 2017, 41, 615–632, . [CrossRef]
- Korall, A.M.; Feldman, F.; Scott, V.J.; Wasdell, M.; Gillan, R.; Ross, D.; Thompson-Franson, T.; Leung, P.-M.; Lin, L. Facilitators of and Barriers to Hip Protector Acceptance and Adherence in Long-term Care Facilities: A Systematic Review. J. Am. Med Dir. Assoc. 2015, 16, 185–193, . [CrossRef]
- Joshi, A.; Kale, S.; Chandel, S.; Pal, D. K., Likert scale: Explored and explained. British journal of applied science & technology 2015, 7 (4), 396-403.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).