1. Introduction
Orthognathic surgery is a surgical procedure that consists of osteotomies and maxillary movements aimed at facial harmony and occlusal repositioning.[
1,
2,
3] Among the techniques ,available for the correction of dentoskeletal deformities, Le Fort I Osteotomy (LFO) is the ,most versatile for the three-dimensional repositioning of the maxilla, which, depending on the magnitude and direction of the proposed movements, can promote changes in the morphology of the maxillary sinus, septum, nasal cavity and attached structures of the osteomeatal complex, according to some authors. [
4,
5,
6,
7,
8] Cone beam computed tomography (CBCT) has become an important tool for the study of the airways and nasal structures. After reformatting and exporting the raw CBCT data, using image processing software that allows the synthesis of several multiplanar images (axial, coronal and sagittal), it is possible to visualize the three-dimensional reconstruction of the mineralized tissues and air spaces of the maxillofacial region with minimal distortion. [
9,
10,
11]
Planning software has allowed the adoption of virtual planning protocols in orthognathic surgery. Dolphin Imaging ® 11.9 software is one of the programs available on the market for surgical simulation, however, there are still few studies involving its accuracy. It is important that these planning software be tested on different anatomical structures to increase the studies available in the literature and provide the possibility of future comparisons with other software. This would increase the reliability of the programs by surgeons and even patients. [
12,
13,
14,
15] Changes in adjacent soft tissues due to the movement of bone structures in patients with dentoskeletal deformities undergoing orthognathic surgery have already been reported in the literature, promoting changes in the respiratory pattern. 16 However, the focus on the posterior upper airways and Obstructive Sleep Apnea Syndrome has reduced investigations in the maxillary sinuses, nasal fossa, ostium region and nasal septum, where the risk of sinusitis is high due to the use of Le. Fort I osteotomy to perform mandibular movements and its intimate involvement with these regions.[ 17,18] Therefore, not only the surgical trauma of osteotomy in the maxillary sinuses in the postoperative period should be evaluated, but also the morphological changes prior or not to surgery, allowing a separation of existing problems from those with iatrogenic causes, in addition to observing whether there may be improvement in these problems. conditions for performing the surgical procedure.[
2,
19,
20]
Therefore, the present research aimed to conduct a retrospective study using CBCT in virtual planning software to evaluate the air volume of the maxillary sinus, detect and diagnose anatomical defects and inserted structures that make up the osteomeatal complex, induced or not by maxillomandibular advancement surgery and/or maxillary impaction at two moments: preoperative (T0) and postoperative of at least 6 months (T1).
2. Materials and Methods
The ethical aspects of this research were evaluated and approved by the Research Ethics Committee of the Faculty of Dentistry of Araçatuba,São Paulo, Brazil University State Paulista “Júlio de Mesquita Filho” - CAAE: 66183722.1.0000.5420, where the Free Informative Consent Form was presented to all patients as a protocol before orthognathic surgery. The methodological procedures involve a selection of Angle class ll and class lll patients, undergoing orthognathic surgery to evaluate, through CBCT, the changes involving the maxillary sinuses after maxillary advancement and/or impaction surgery. These were obtained through the database of a private clinic in Araçatuba-SP, where patients underwent orthognathic jaw surgery and were operated by the same oral and maxillofacial surgeon.
The inclusion criteria for the study consisted of patients with CBCT up to 30 days before the surgical procedure, carried out in the same radiographic laboratory, with a minimum age of 18 years and no maximum age restriction and who underwent CT scans for the post-operative period. -operation from 06 months to 01 year. Exclusion criteria included syndromic patients, smokers, who had presented any flu-like symptoms or allergic rhinitis fifteen days before the radiographic examination or who had undergone previous orthognathic surgery.
The images were obtained by the I-Cat Cone-beam® tomography machine (Imaging Science, Hatfield, PA, USA). The data from the computed tomography scans were converted into Digital Imaging and Communications in Medicine (DICOM) format, and were stored together with the patient's pre-operative documentation as well as their virtual planning, which, using software, were overlaid and virtual planning of the procedure was carried out. surgery.
All surgeries were performed by the same team and with the same surgical, medication and physiotherapeutic planning protocol, where the surgery consisted of a Le Fort l osteotomy in the maxilla and sagittal osteotomy of the mandibular ramus, being fixed with titanium plates and screws from the 1.5 system. mm and 2.0mm respectively.
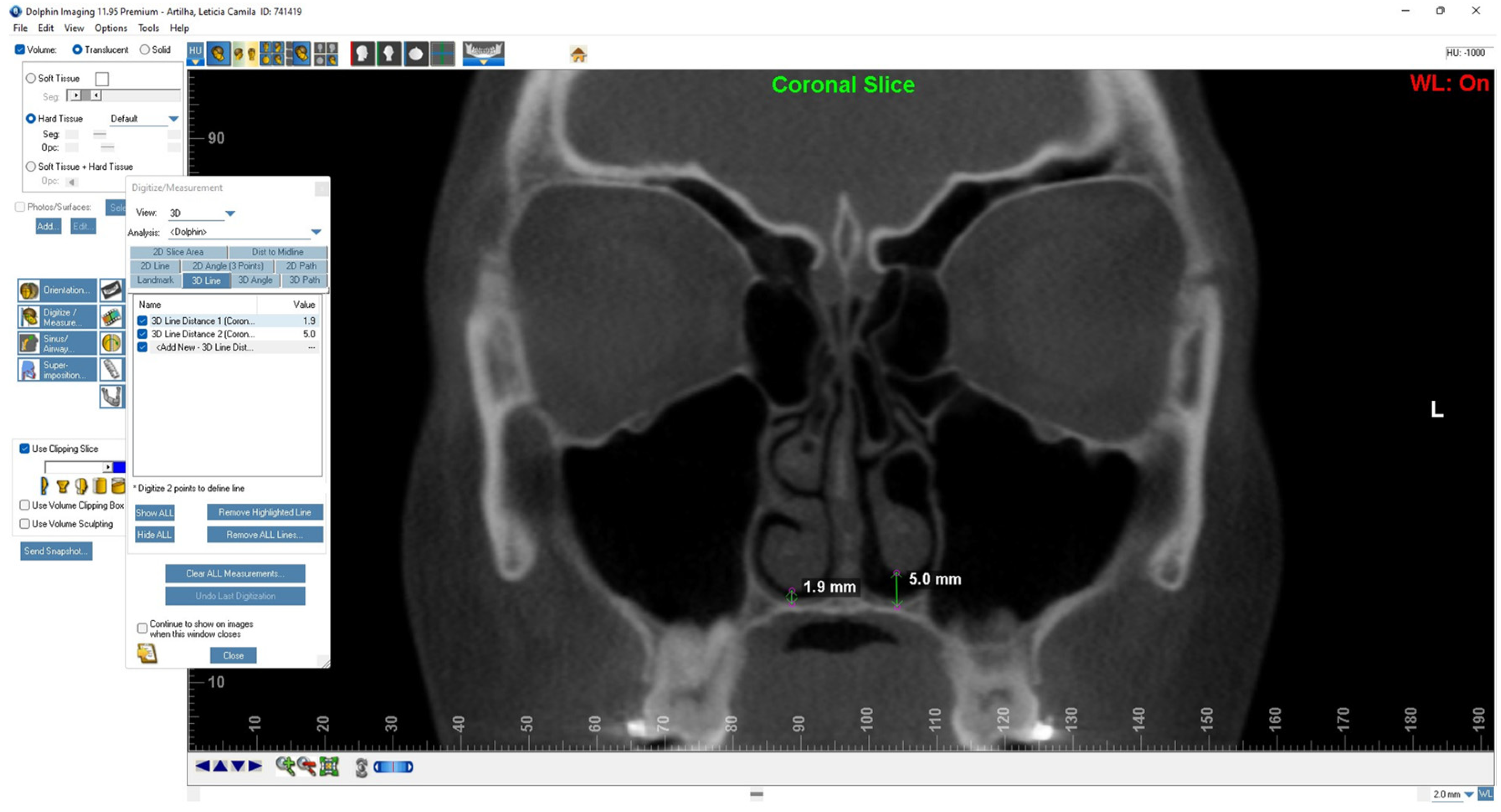
Analyzes of images and clinical information were carried out by the same calibrated researcher, using an imaging program “Dolphin 3D” software, version Dolphin Imaging® 11.9 (Dolphin Imaging and Management Solutions, Patterson Technology, Chatsworth, CA, USA) for analysis. carrying out measurements on tomography scans.
Epidemiological factors such as age, gender, type of deformity were evaluated, in addition to the maxillary sinus and its attached structures such as ostium, deviated septum, influence of turbnectomy and/or septoplasty on the air volume of the maxillary sinus, presence of mucous thickening and presence of retention cysts.
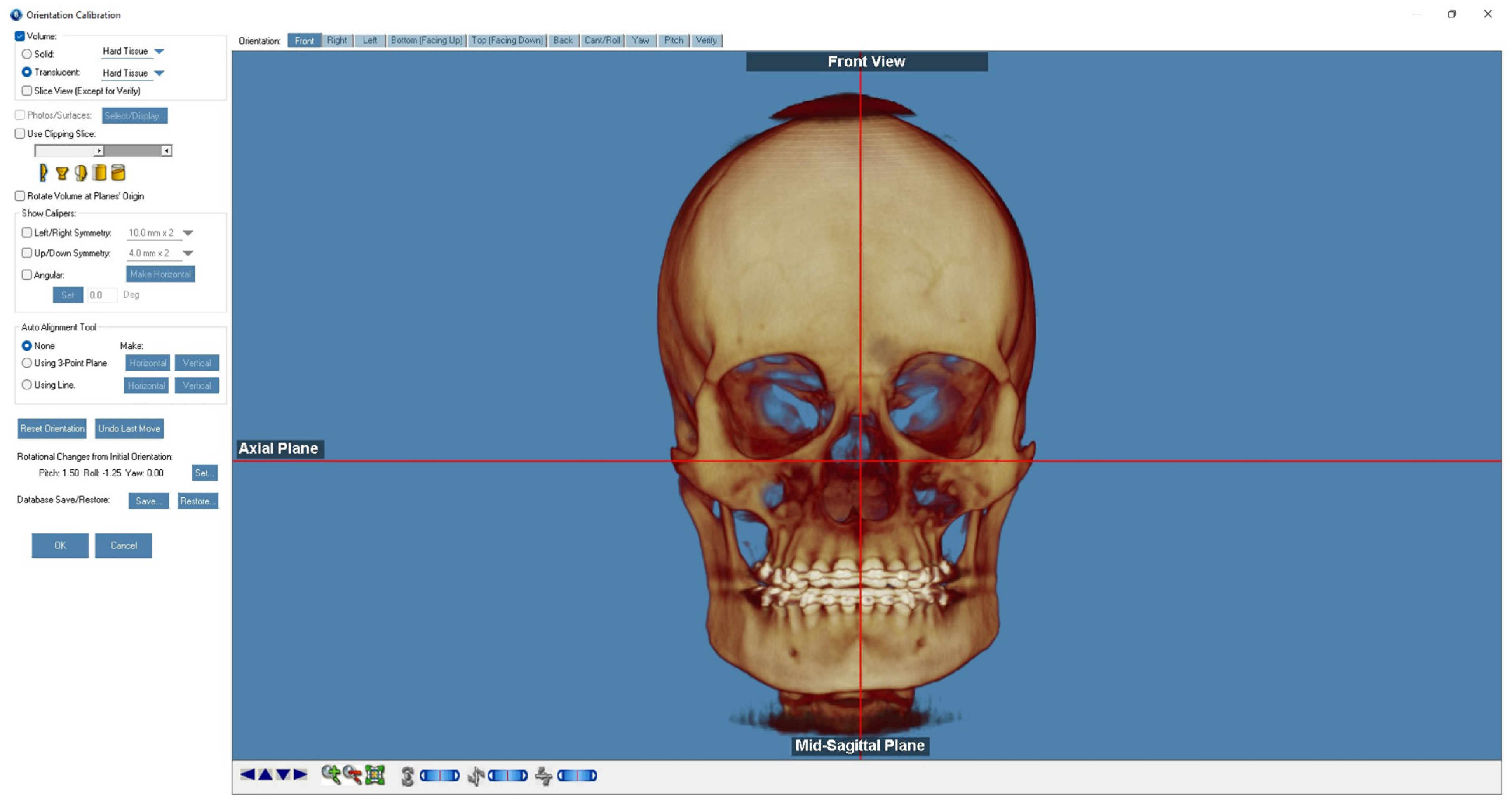
The overlay was done using specific tools in the Dolphin Imaging® 11.9 software. using the static region of the anterior base of the skull as a fixed reference on the sphenoid bone (
Figure 1), according to the protocol described by Haas et al., (2019).
Then, select the “Superimpose now” option, which automatically superimposes the two tomography scans in a more refined way. Skull orientation - through the “Analysis/ Verify Results” function, use the “Export Orientation to 2nd Volume” tool so that T1 has the same spatial orientation and coordinates on the y (vertical), x ( transverse) and z (sagittal) than T0, saving them afterwards (
Figure 2).
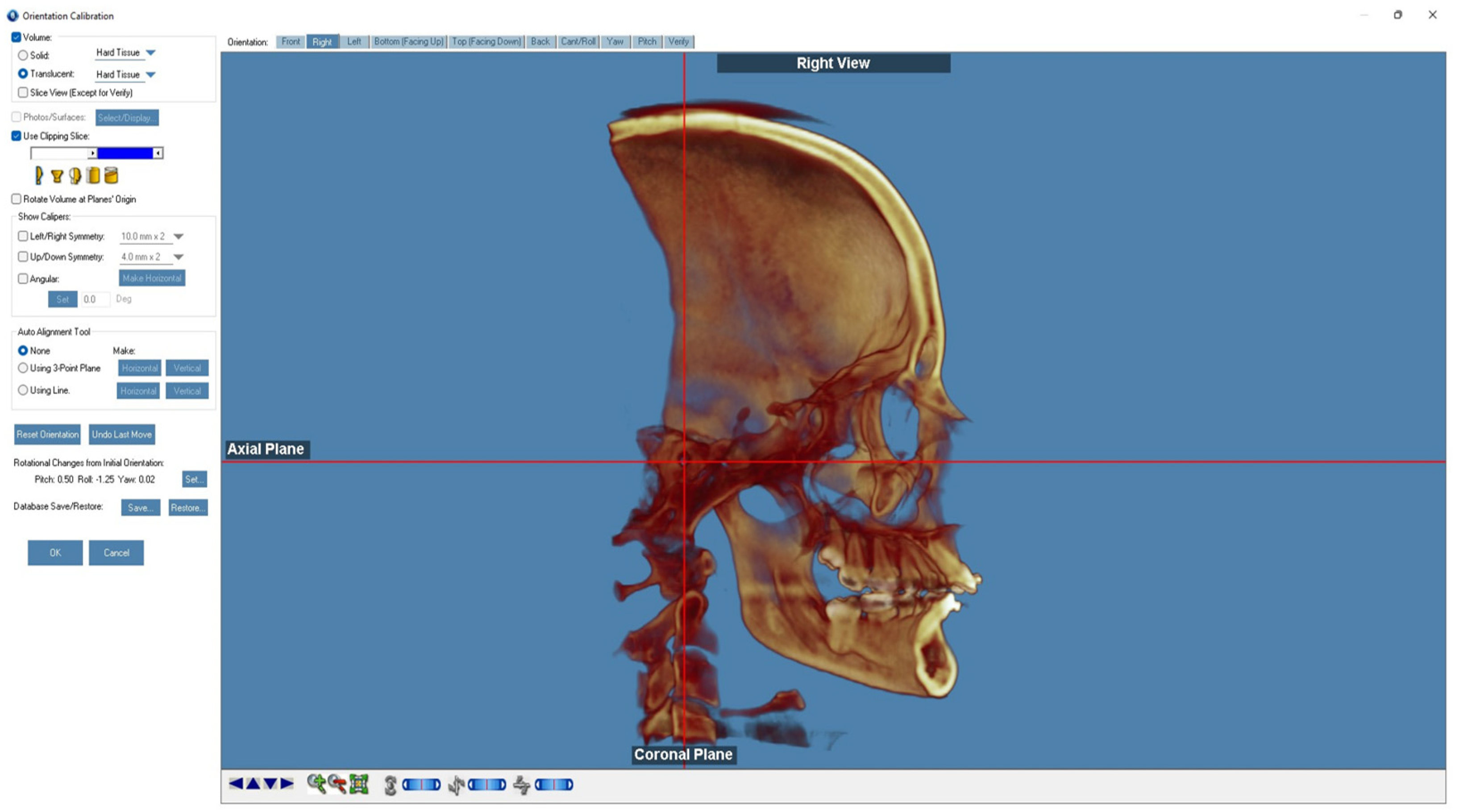
Using the “Sinus/Airway” tool in the Dolphing Imaging software, the first step was to segment the regions of interest (ROI) for the nasal cavity, nasopharynx and maxillary sinuses in sagittal, axial and coronal views. Delimiting the described ROI, “Seed points” were added, filling the regions of interest, and using the “Updating Airway” command, the 3D volumetric model of the nasal cavity and separate nasopharynx were obtained. The comparative three-dimensional assessment of the volume (mm3) of T0 and T1 was quantified. The right and left maxillary sinuses were manually delimited taking into account the anatomical limits of their walls seen on CT scans in the coronal, sagittal and coronal sections, separately to obtain the average volumes (mm3) (
Figure 3).
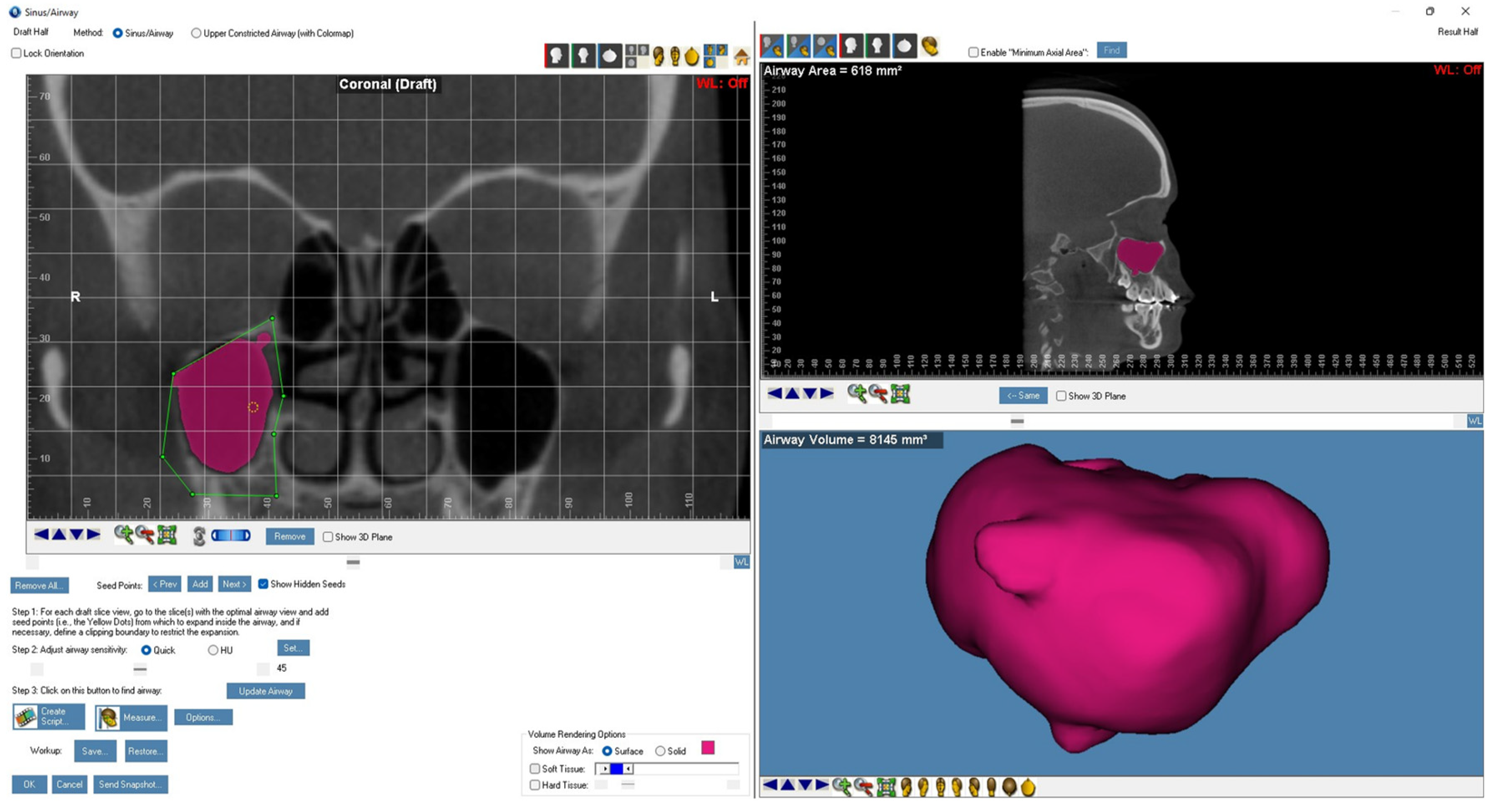
The deviation of the nasal septum was analyzed using the coronal section of the tomographic examination. The angle of septal deviation (ADS) was measured using a line that connects the crista galli with the anterior nasal spine (vertical reference plane - y axis) and a second line that connects the crista galli to the most deviated point of the nasal septum. , after marking the reference points, the angular measurement tool of the Dolphin 3D software was used. For “S”-shaped septa, the largest angle was taken into consideration. There was also a final manual check to verify the adequate measurement of septal deviation (
Figure 4).
31
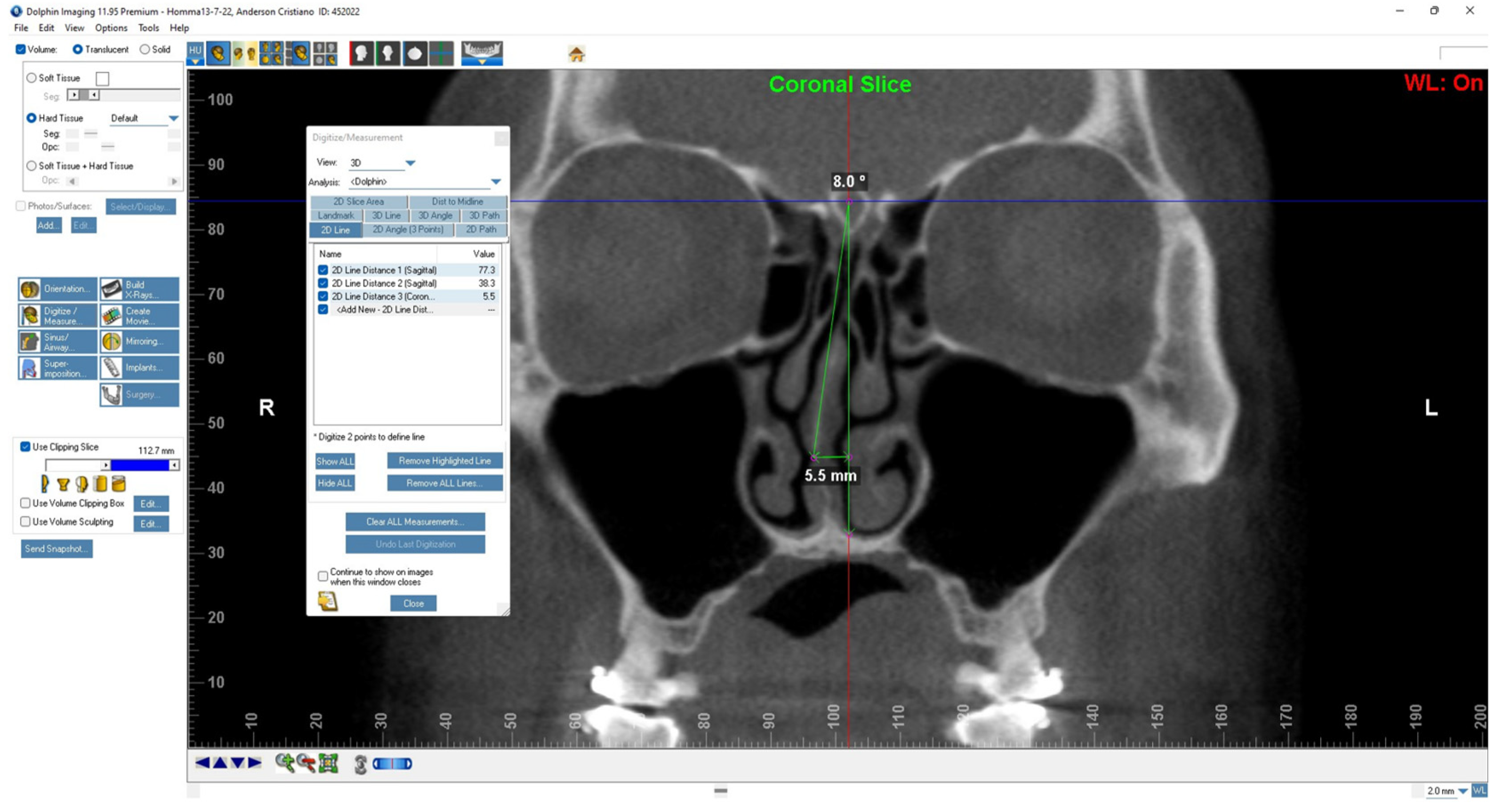
The presence or absence of the maxillary ostium on the tomography was analyzed in the coronal, axial and sagittal sections (
Figure 5). Proper function of the maxillary sinus depends on the patency of the maxillary ostium. When present, the patency of the maxillary ostium was assessed as obstructed or patent, based on the coronal section.
The software R (version 4.1.0, 2023), Microsoft Excel 365 (2023) and Jamovi (Version 2.3, 2022) were used.
3. Results
During the period of acquisition of pre- and post-operative tomography scans, the research involved the involvement of 34 participants, however 2 were excluded due to flu episodes appearing in the medical record a week prior to the tomographic examination and 1 patient was removed because he had already undergone surgery. previous orthognathic. Thus, the final sample consisted of 31 patients, with a prevalent age range of 21 to 31 years. In terms of gender, the division was 15 women (48%) and 16 men (52%). Regarding the classification of dentoskeletal deformities, 17 patients (55%) were Class II and 14 (45%) were Class III. Regarding maxillary advancement, 17 patients (55%) had this maxillary advancement procedure alone and 14 patients (45%) had it associated with maxillary impaction.
The morphological changes present in the pre- and post-operative periods were compared with sex, deformity classification and maxillary impaction, with a view to identifying any association as a risk factor or predisposition, with no statistical difference between the groups with class ll and class lll deformity. And the presence of deviated septum was also not different between the groups with presence and absence of maxillary impaction. Descriptively, attention is drawn to the proportion of maxillary impaction between the class ll and lll groups with 32% and 13% (p=0.0092) respectively, a 60% reduction in class lll when compared to class ll .This demonstrates that the maxillary advancement with impaction procedure was less used in class III patients.
The volumes of the right and left maxillary sinuses pre- and post-operatively were compared, the mean (standard deviation) of the right maxillary sinuses pre- and post-operatively was 12.66 (1.59) and 12.27 (1.69) respectively with medians of 12.74 and 12.36. When comparing the volumes of the left maxillary sinuses pre- and post-operatively, the mean (standard deviation) was 12.23 (2.03) and 12.43 (2.1), respectively, with medians of 12.64 and 12.41. There was no significant difference between the distribution of values on the right and left sides pre- and post-operatively .
The presence of morphological changes at T0 and T1 was analyzed based on the presence or absence of retention cyst, mucosal thickening, deviated septum, turbonectomy and/or septoplasty performed or not. Regarding retention cyst and mucosal thickening, there was no presence pre-surgery, and post-surgery the incidence was 2 cases (6.45%) for retention cyst and 10 cases (32.25%) for minimal mucosal thickening. mucosa.
For “deviated septum” and “turbnectomy and/or septoplasty” the Mc Nemar test was applied, where deviated septum in T0 was present in 19 cases (58.1%) and in T1 12 cases (38. 7%) maintained the septal deviation, with a reduction of six previously described cases, these differences in proportions were significant. For turbonectomy and/or septoplasty in T0 there was the presence of 2 cases (6.4%), that is, who had already undergone this surgical procedure and in T1 the presence of 22 cases (70.9%) submitted to this procedure for the first time, an 11-fold increase. A total of 9 patients did not undergo turbonectomy and/or septoplasty. These differences in proportions were significant.
The analysis of the maxillary ostium pre and post surgery for the categories absent, present, obstructed and present patent, using the Stuart-Maxwuell test. For obstruction of the right maxillary ostium at T0 there were 4 cases absent (12.9%), 5 present obstructed (16.1%), and 22 present patent (71.0%), at T1 there were 2 absent (6.45% ), 2 present obstructed (6.45%) and 27 present patent (87.1%). For left maxillary ostium obstruction at T0 there was 1 case absent (3.2%), 5 present obstructed (16.1%), and 25 present patent (80.7%), at T10 they were absent, 4 present obstructed (12, 9%) and 27 present patent (87.1%). Descriptively, a decrease in cases of present obstruction and an increase in cases of present obstruction can be seen post-operatively, however, the differences between the proportions in the pre- and post-operative period for left and right maxillary ostium obstruction did not show significant differences.
4. Discussion
The maxillary sinus was first described by Leonardo Da Vinci in 1489
21. Later, in 1651, the English anatomist Nathaniel Highmore described the maxillary sinus as the largest and the first to be developed of the paranasal sinuses.[
22,
23]Currently, there is the presence of studies demonstrating the positive impact of orthognathic surgery on the upper airways, however, there is a lack of studies involving the maxillary sinus, which can be affected by Le Fort I osteotomy, since this is included in the osteotomy line
. [
2,
3,
19] The results obtained in the present study included a predominant age group of 21 to 31 years old with 48.4%, showing that the surgical procedure was carried out mainly in young patients and the prevalence of males (52%). Regarding the type of prevalent deformity, there were patients with Angle class II with no maxillary impaction.
Some studies have demonstrated a reduction in the air volume of the maxillary sinus after orthognathic surgery, as mentioned by Nocini et al.[
24] However, the present study did not demonstrate a significant statistical difference between the distribution of values on the right and left sides pre- and post-operatively. This fact can be justified due to the period of CBCT analyzed being at least 6 months post-operatively, since from this period onwards it is possible to consider that the mucosa of the maxillary sinuses has recovered from the surgical trauma.
The literature cites septal deviation as one of the main anatomical complications found in the postoperative period of maxillary surgery using OLFI with impaction, as well as occasional septal perforation and sinusitis, as demonstrated by Haarmann et al. [
8,
13,
25]At T0 there was presence of 19 cases (58.1%) and at T1 12 cases (38.7%) maintained septal deviation, with a reduction of six previously described cases. In the current analysis, with turbnectomy and/or septoplasty performed on 22 patients (70.9%) of the sample, it was possible to verify that more than 50% of patients underwent this plasty, which may justify the reduction in cases of septal deviation for better relocation of the turbinates.
Regarding retention cysts, there was an incidence of 2 cases (6.45%) post-surgery and 10 cases (32.25%) for minimal mucosal thickening. When comparing the measurement periods, it differs from some studies such as that by Valstar et al., which demonstrates worsening of clinical and tomographic characteristics obtained in the immediate postoperative period of patients undergoing Le Fort I type osteotomy.[
26] Therefore, Such complications can be considered as a temporary situation since in the postoperative period of at least six months present in this study the situation changes to minimal incidence, highlighting another advantage of this surgical technique in the long term for the patients lives.[
1]
The ostium (ostium) is an opening that drains the airways directly into the nasal cavity (sphenoidal ostium), or indirectly through more complex anatomical structures (frontal recess).[
27] Thus, an obstruction of the ostium may be related to a reduction in ciliary activity, qualitatively compromising the maxillary sinus, as it leads to a reduction in the blood supply of the sinus mucosa, favoring maxillary sinusitis. This is related to edema of the mucous membrane that narrows at the ostium and impairs the transport capacity of the mucociliary system(89).[
27,
29,
30] In the present study, a decrease in the postoperative period of cases of present obstructed ostium and an increase in cases of present patent ostium was noted. Therefore, orthognathic surgery when performed in conjunction with turbnectomy, which is a vertical plasty of the nasal turbinates, causes a release of septal compression and relocation of the turbinates, favoring the reduction of edema of the mucous membrane that pre-surgically pressed the region of nasal ostium.
Therefore, the present study includes as a positive and differential point a retrospective postoperative evaluation with a minimum of 6 months, in order to allow the recovery of the maxillary sinus, avoiding the effects resulting from the immediate postoperative period, such as edema. The sample selection included strict inclusion criteria, such as pre-operative tomographic scans from 15 to 30 days, where patients did not show signs of flu based on the information contained in the medical records, increasing the accuracy of the study.
This is a homogeneous sample, especially in the choice of the type of surgery and the direction of skeletal movements, showing how maxillary advancement with or without impaction influences the patient's postoperative period. In addition, a prevalent feature of the patient's age and gender, as these factors can alter the volume of the maxillary sinus. Also, another variable analyzed was the skeletal class, where in both Angle classes taken into consideration in the study there was no statistical difference in the volumetric analysis of the maxillary sinuses.
5. Conclusions
This section is not mandatory but can be added to the manuscript if the discussion is unusually long or complex.
Author Contributions
All authors attest that they meet the current ICMJE criteria for authorship. L.F.O. collected, analyzed, and interpreted the clinical data and wrote the manuscript M.D.P., V.N.L. and O.M.F. made substantial contributions to the acquisition of the clinical data. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted and approved by the Institutional 66183722.1.0000.5420, for studies involving humans.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The datasets generated and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Yamada T, Sugiyama G, Mori Y. Masticatory muscle function affects the pathological conditions of dentofacial deformities. Jpn Dent Sci Ver. 2020;56(1):56–61.
- Foltán R, Hoffmannová J, Pavlíková G, Hanzelka T, Klíma K, Horká E, et al. The influence of orthognathic surgery on ventilation during sleep. Int J Oral Maxillofac Surg. 2011;40(2):146–9.
- Faur CI, Roman RA, Bran S, Dinu C, Coclici A, Rotaru H, Hedesiu M. The Changes in Upper Airway Volume after Orthognathic Surgery Evaluated by Individual Segmentation on CBCT Images. Maedica (Bucur). 2019 Sep;14(3):213-219. [CrossRef] [PubMed] [PubMed Central]
- Almuzian M, Almukhtar A, Ju X, Al-Hiyali A, Benington P, Ayoub A. Effects of Le Fort I Osteotomy on the Nasopharyngeal Airway-6-Month Follow-Up. J Oral Maxillofac Surg. 2016 Feb;74(2):380-91. [CrossRef] [PubMed]
- Iturralde-Garrote A, Sanz JL, Forner L, Melo M, Puig-Herreros C. Volumetric Changes of the Paranasal Sinuses with Age: A Systematic Review. J Clin Med. 2023 ;12(10):3355. 9 May. [CrossRef] [PubMed] [PubMed Central]
- Nocini PF, D'Agostino A, Trevisiol L, Favero V, Pessina M, Procacci P. Is Le Fort I Osteotomy Associated With Maxillary Sinusitis? J Oral Maxillofac Surg. 2016 Feb;74(2):400.e1-400.e12. Epub 2015 Oct 19. [CrossRef] [PubMed]
- Cohen O, Warman M, Fried M, Shoffel-Havakuk H, Adi M, Halperin D, Lahav Y. Volumetric analysis of the maxillary, sphenoid and frontal sinuses: A comparative computerized tomography based study. Auris Nasus Larynx. 2018 Feb;45(1):96-102. Epub 2017 Mar 22. [CrossRef] [PubMed]
- Ueki K, Yoshizawa K, Moroi A, Hotta A, Tsutsui T, Fukaya K, Hiraide R, Takayama A, Tsunoda T, Saito Y, Iguchi R, Kosaka A, Ikawa H. Evaluation of maxillary sinus after Le Fort I osteotomy using various fixation materials. J Craniomaxillofac Surg. 2017 Apr;45(4):552-557. Epub 2017 Jan 31. [CrossRef] [PubMed]
- Abate A, Cavagnetto D, Lanteri V, Maspero C. Three-dimensional evaluation of the maxillary sinus in patients with different skeletal classes and cranio-maxillary relationships assessed with cone beam computed tomography. Sci Rep. 2023 Feb 6;13(1):2098. [CrossRef] [PubMed] [PubMed Central]
- Yang SM, Park SI, Kye SB, Shin SY. Computed tomographic assessment of maxillary sinus wall thickness in edentulous patients. J Oral Rehabil. 2012 Jun;39(6):421-8. Epub 2012 Apr 3. [CrossRef] [PubMed]
- Ueki K, Takayama A, Moroi A, Yoshizawa K. Computed Tomography Assessment of Maxillary Sinus and Inferior Nasal Airway After Le Fort I Osteotomy. J Craniofac Surg. 2022 Sep 1;33(6):1835-1839. Epub 2022 Jun 28. [CrossRef] [PubMed]
- Atakan A, Ozcirpici AA, Pamukcu H, Bayram B. Does Le Fort I osteotomy have an influence on nasal cavity and septum deviation? Niger J Clin Pract. 2020 Feb;23(2):240-245. [CrossRef] [PubMed]
- Iturralde-Garrote A, Sanz JL, Forner L, Melo M, Puig-Herreros C. Volumetric Changes of the Paranasal Sinuses with Age: A Systematic Review. J Clin Med. 2023 ;12(10):3355. 9 May. [CrossRef] [PubMed] [PubMed Central]
- On SW, Baek SH, Choi JY. Quantitative Evaluation of the Postoperative Changes in Nasal Septal Deviation by Diverse Movement of the Maxilla After Le Fort I Osteotomy. J Craniofac Surg. 2020 Jul-Aug;31(5):1251-1255. [CrossRef] [PubMed]
- Mommaerts MY, Lippens F, Abeloos JV, Neyt LF. A discussion about the discussion. Nasal profile changes after maxillary impaction and advancement surgery. J Oral Maxillofac Surg. 2000 Oct;58(10):1198. [CrossRef] [PubMed]
- Honrado CP, Lee S, Bloomquist DS, Larrabee WF Jr. Quantitative assessment of nasal changes after maxillomandibular surgery using a 3-dimensional digital imaging system. Arch Facial Plast Surg. 2006 Jan-Feb;8(1):26-35. [CrossRef] [PubMed]
- Ariji Y, Kuroki T, Moriguchi S, Ariji E, Kanda S. Age changes in the volume of the human maxillary sinus: a study using computed tomography. Dentomaxillofac Radiol. 1994 Aug;23(3):163-8. [CrossRef] [PubMed]
- Panou E, Motro M, Ateş M, Acar A, Erverdi N. Dimensional changes of maxillary sinuses and pharyngeal airway in Class III patients undergoing bimaxillary orthognathic surgery. Angle Orthod. 2013 Sep;83(5):824-31. Epub 2013 Feb 25. [CrossRef] [PubMed] [PubMed Central]
- Burkhard JP, Dietrich AD, Jacobsen C, et al. Cephalometric and three-dimensional assessment of the posteriorairway space and imaging software reliability analysis before and after orthognathic surgery. Journal of Cranio-Maxillo-Facial Surgery. 2014;7:1428–1436.
- Ariji Y, Fukuda M, Kise Y, Nozawa M, Yanashita Y, Fujita H, Katsumata A, Ariji E. Contrast-enhanced computed tomography image assessment of cervical lymph node metastasis in patients with oral cancer by using a deep learning system of artificial intelligence. Oral Surg Oral Med Oral Pathol Oral Radiol. 2019 May;127(5):458-463. Epub 2018 Oct 15. [CrossRef] [PubMed]
- Jakobsone G, Stenvik K, Espeland L. The effect of maxillary advancement and impaction on the upper airway after bimaxillary surgery to correct Class III malocclusion. Int J Oral Maxillofac Surg. 2011;139:369–376.
- Whyte A, Boeddinghaus R. The maxillary sinus: physiology, development and imaging anatomy. Dentomaxillofac Radiol. 2019;48(8):20190205.
- Gulec M, Tassoker M, Magat G, Lale B, Ozcan S, Orhan K. Three-dimensional volumetric analysis of the maxillary sinus: a cone-beam computed tomography study. Folia Morphol (Warsz). 2019.
- Nocini PF, D’Agostino A, Trevisiol L, Favero V, Pessina M, Procacci P. Is le Fort i Osteotomy Associated with Maxillary Sinusitis? J Oral Maxillofac Surg.
- HAARMANN S, Budihardja AS, Wolff KD, Wangerin K. Changes in acoustic airway profiles and nasal airway resistance after Le Fort I osteotomy and functional rhinosurgery: a prospective study. Int J Oral Maxillofac Surg. 2009 Apr;38(4):321-5.
- Valstar MH, Baas EM, Te Rijdt JP, De Bondt BJ, Laurens E, De Lange J. Maxillary sinus recovery and nasal ventilation after Le Fort I osteotomy: a prospective clinical, endoscopic, functional and radiographic evaluation. Int J Oral Maxillofac Surg. 2013;42(11):1431–6.
- Som, PM. CT of the paranasal sinuses. Neuroradiology. 1985;27(3), 189-201. [Google Scholar]
- Brook, I. Microbiology and antimicrobial management of sinusitis. J Laryngol Otol. 2005;119(4):251-8.
- Lanza DC, Kennedy DW. Adult rhinosinusitis defined. Otolaryngol Head Neck Surg. 1997;117(3 Pt 2):S1-7.
- . Lindberg S, And AC, Runer T. Nitric oxide (NO) production in the upper airways is decreased in chronic sinusitis. Acta Otolaryngol. 1997;117(1):113-7.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).