1. Introduction
Vacuum therapy – VAC (or negative pressure wound therapy - NPWT) has been successfully used in many branches of medicine for over a dozen years and the list of its applications is constantly growing. The use of this method is observed in the treatment of acute and chronic wounds. It is used, for example, in the treatment of diabetic foot syndrome, necrotizing fasciitis, soft tissue injuries, burns, ulcers and slow-healing postoperative wounds. This method involves creating negative pressure in the wound, i.e. lower than atmospheric pressure, which improves microcirculation in the wound fundus, stimulates the production of new capillaries, cell proliferation and the formation of granulation tissue in the wound [
1].
Dressing wounds was one of the first therapeutic activities performed by humans [
2]. Over the centuries, this art has been one of the most dynamically developing branch of medicine. Over the years of gathering knowledge, experience and the development of medicine, various theories have emerged regarding the proper wound healing and the role of pus in this process. The oldest known written medical record on how to treat wounds comes from Mesopotamia and dates back to 2500–2200 BC [
2]. A clay tablet found from this period contained 15 recipes for external medicines, of which as many as 12 were medicines for treating wounds. The Sumerians used herbs mixed with beer to heal wounds. The Egyptians, who had extensive experience in mummifying corpses, used bandages soaked in honey, resins, olive oil, and green dye consisting of copper filings and vinegar to cover wounds. In this way, attempts were made to obtain astringent and antibacterial properties. The ancient Egyptians distinguished the so-called good wounds - healing without complications and bad wounds - festering. They usually left such festering body lesions open in order to evacuate the pus, which they undoubtedly considered an unfavorable phenomenon [
2,
3]. To mask its unpleasant scent, they used fragrant oils and myrrh. Based on his experience, Hippocrates posited that wounds should be cleansed with wine or vinegar, then applied ointments, bandaged and left "dry" until healing, in accordance with the idea that nature itself would best regenerate damaged tissues [
3].
The Greeks also contributed to the treatment of wounds based on the known properties of verdigris (copper hydroxyacetate - a basic salt of copper and acetic acid) - a strong antiseptic, used in the form of ointments and decoctions [
3]. The Greeks also tried using other specifics, such as secretions and saliva of snakes. It was popular to wrap wounds with bandages made of wool boiled in water, often soaked in wine [
3]. Hippocrates considered suppuration to be a beneficial process for healing. This most famous physician of ancient Greece claimed that it eliminated necrotic fluids from the wound. He did not believe, though, that suppuration was necessary for proper recovery, as his successors claimed [
3]. However, some doctors practicing in the Peloponnese Peninsula drained pus from infected wounds and boils. For this purpose, primitive syringes called pyulcus were used, invented by a barber surgeon named Ctesibios (280 BC). However, this procedure was not popular, in contrast with the removal of excess "congealed" blood while dressing the wound. Injuries were considered diseases, which, at that time, was equivalent to the theory of disturbing balance of the four fluids in the patient's body (blood, bile, black bile and phlegm). Greeks believed that clotted blood was an obstacle to proper wound healing, that is why they used the "opening the veins" procedure, i.e. removing "unnecessary" blood. Hippocrates also mentioned the possibility of putting a tourniquet on a limb to stop massive hemorrhage. However, he warned against the risk of disastrous gangrene caused by too long pressure [
3]. Stopping hemorrhage by using a tourniquet was a rather rare practice and raised doubts among then medics. Romans also gathered their knowledge about wound healing and even compiled it in a kind of manual. In his eight-volume work "De medicina", Cornelius Celsus described the entire spectrum of substances for cleansing wounds and accelerating healing, as well as the surgical tools used [
2,
4]. Moreover, Celsus proposed treatment in the event of various forms of inflammation. He defined four fundamental features of inflammation: rubor et tumor cum calore et dolore, i.e.: redness, swelling, warmth and pain. He wrote a description of the proceeding in case of massive hemorrhage in order to stop the flowing blood and reduce inflammation. He recommended using dry rags (pieces of torn material) directly on the wound first, and then pressing them with a damp sponge wrung out of cold water. In case of further hemorrhage, he advised replacing the used, soaked dressing with a new one, and if this did not work, he recommended using a ligature to tie the vessel from which the blood was flowing [
2]. It had to be done in two places and cut in the middle to facilitate vasoconstriction and occlusion of each end separately. If this was not effective, the wound had to be cauterized. Moreover, he was a supporter of suturing clean wounds and recommended surgical debridement of infected wounds by removing necrotic tissue. This allowed the wound to be reopened so that it could be sutured in the same way as the original injury. Celsus also classified types of wounds - he distinguished acute types, e.g. cut wounds, and chronic types, e.g. pressure sores. Furthermore, he noticed the need to treat injuries using various methods depending on their type [
2]. Reflection on wound treatment appeared in the work of one of the most famous physicians - Claudius Galen (129–200 AD). When treating various wounds, he used ointment made of frankincense resin with aloe, egg white and hairpiece from hare fur. Additionally, to speed up the healing process, he used spiderwebs, ink and the then famous clay from the island of Lemnos, which supposedly had healing properties. Galen recommended four procedures for treating a bleeding wound: direct pressure on the wound with a finger, bringing the edges of the wound together with hooks, tying a vessel close to the wound and applying frankincense ointment [
4]. Galen, unlike Hippocrates, claimed that suppuration of the wound is necessary and desirable for the healing process. In later years, this led to the use of various ointments and other specifics intended to cause infection [
4]. Romans also denied the use of stopping bleeding with tourniquets. This resulted in a slow and gradual shift away from their use to control bleeding. Scribonius, Claudius' court physician, believed that tying a piece of cloth over the wound would squeeze out more blood. However, Galen's views in particular influenced the perspective and practice of treating wounds for many years until the 11th century. In medieval Europe, Galen's views dominated until the 12th century, but wound treatment was based on quack practices that had no basis in previously accumulated empirical knowledge [
3].
In the 12th century, Bologna became an important center of surgery, where Hugh de Lucca, one of the first critics of Galen's teachings, lectured [
2]. While dressing the wounds of soldiers taking part in another crusade, he noticed that wounds washed with wine and not suppurating healed faster than "Galen's" festering ones, which led him to reject the view on the beneficial suppuration of wounds. Unfortunately, Galen's erroneous view on the beneficial importance of wound suppuration survived and was repeated over the next centuries [
3].
In the 14th century, firearms began to be used in warfare, which caused gunshot wounds. Initially, stones were used, and later large-caliber lead bullets. Injuries of this type were characterized by extensive hemorrhages in the injured person's body. Due to the energy acting on the surrounding tissues, they were also accompanied by extensive necrosis. At the beginning, surgeons believed that the causes of infections and deaths of the injured were the poisonous features of black powder, the remains of which were found on the surface of the bullets. An fierce follower of this theory was Giovannida Vigo, a famous Italian surgeon who, as first, attempted to describe the comprehensive treatment of wounds inflicted by an arquebus [
5]. In the book "Practica in arte surgeonica copiosa" dated 1514, he stated that the best remedy for the effects of gunpowder poison would be to pour boiling oil over the wound to cleanse the wounds of gunpowder remnants. Before the views of Leonardo Botallo, who rejected the poisonous features of gunpowder, became popular, the fight against the "poison" after a gunshot took priority over proper treatment [
5]. A chance observation of Ambrose Paré, a field surgeon who ran out of boiling oil to pour on wounds, so he dressed the wounds with egg yolks, oil, and various rags, showed that such treated patients recovered faster [
4]. During the Renaissance and up to the 17th century, wounds were stitched, burned or dressed with rags. Doctors were unable to deal with infections as complications. Only at the beginning of the 20th century, due to the gathered knowledge, the processes significant for proper wound healing were learned. Modern methods of wound treatment combine knowledge of the formation of macrophages from monocytes, angiogenesis processes, and the use of antibiotics and antiseptics. The "Listerian revolution" means not only disinfection of wounds, hands and surgical equipment, but also disinfection and decontamination of operating rooms or places of stay. Dressings play an important role in modern wound treatment. Currently, the search for optimal methods of dressing wounds is still ongoing, taking into account, for example, the specificity of the wound. One way to treat wounds is to use negative pressure.
The first information regarding the use of negative pressure in medicine comes from the 3rd century AD. Chinese herbalist and alchemist Ge Hong described in his books the influence of locally applied negative pressure on the acupuncture and acupressure effectiveness [
1]. To create negative pressure, he used cupping glasses from which he displaced oxygen with fire and placed them, heated, on the human skin – this caused local suction of the body inside. In the 17th century, work on the effects of vacuum and negative pressure was carried out by the Italian physicist and mathematician Evangelista Torricelli [
6] and the French researcher Blaise Pascal, who discovered that a vacuum has zero pressure. Christian Huygens used negative pressure for the first time in practice by constructing a vacuum pump himself [
3]. However, the most important event was the experiment involving vacuum and negative pressure publicly conducted in 1654 by the German physicist Otto von Guericke [
7]. It consisted of removing air from the inside of the hemispheres using a water piston pump and attempt to separate them. Military surgeon, Dominique Anel, designed a suction syringe with a triangular tip and a wide cannula to remove a foreign body from a wound. This invention was intended to replace the traditional method of wound cleansing [
8]. Another French researcher, Victor Theodore Junod, constructed a vacuum apparatus that replaced the traditional bloodletting method. Later, various modifications of the Junod apparatus were developed, which led to a significant expansion of its use [
3,
9]. In the 19th century, a closed vacuum system was used to drain postoperative wounds. Using drains that tightly connected the wound to the negative-pressure tank, enabled continuous and active outflow of secretions from the operated site. Gotthard Bülau first used this method to decompress postoperative pneumothorax after thoracic procedures. The improved thoracic vacuum drainage system is still in use today [
3,
8]. One of German doctors used cupping glasses and other forms of negative pressure therapy to treat rheumatic diseases, tuberculosis, meningitis, osteitis and lymphadenitis, etc. [
3,
9]. In the 20th century, people were more fascinated with the penicillin discovery than with negative pressure therapy. A breakthrough in negative pressure therapy occurred in Europe during the nine-year Soviet-Afghan war. Surgeon Nail Bagautdinow was the first to apply a negative pressure dressing using a sponge. He described and published the results of research on the infected wounds treatment with a device he constructed. Since then, vacuum therapy dressings have been improved. For example, a moist gauze dressing was used to treat postoperative wound dehiscence, which was intended to reduce swelling and protect the wound against secondary infection. German surgeon, Wim Fleishmann, was the first to use a polyvinyl sponge to fill the wound, which he then sealed with a semi-permeable polyurethane foil [
7,
10,
11]. Louis Argenta and Michael Morykwas replaced polyvinyl sponges with polyurethane ones with larger pores, which enabled more effective drainage, at a vacuum value of 125 mmHg [
12]. This method was initially assumed to be used only for the difficult-to-heal chronic wounds treatment, but later on the assumptions were extended. The NPWT technique is still developing and is becoming an increasingly interesting field of procedure medicine [
8,
11,
13].
VAC therapy involves creating negative pressure in the wound, i.e. lower than atmospheric pressure. It improves microcirculation in the wound fundus, stimulates the production of new capillaries, cell proliferation and the formation of granulation tissue in the wound. Moreover, it supports autolytic cleansing processes and reduces swelling [
4,
10,
14]. The negative pressure treatment kit includes: an electrically powered device generating suction force, a container collecting wound secretions, various types and sizes of sponges filling the wound fundus, connecting drains and a sealing, semi-permeable, self-adhesive foil. Stoma paste is often used for better sealing [
13]. The sponge filling the inside of the wound can be polyurethane or polyvinyl. The standard capacity of the secretion canister is 500–800 ml. Containers are often equipped with a gelling substance that prevents liquid content from flooding the device. The heart of the entire system is a microprocessor responsible for generating the appropriate negative pressure. A clear display ease the use of the system. The device allows choosing continuous or intermittent operation and programming precisely the value of the generated vacuum. The self-adhesive foil tightly covers the surface of the wound and dressing and provides appropriate conditions for the vacuum creation. In the medical application of intra-abdominal negative pressure therapy, non-adhesive foil is used, which aims to separate the organs from the sponge layer [
10,
14].
Negative-pressure wound therapy (NPWT) is a treatment method continuously used in many treatment specialties for several decades. The use of negative pressure is recommended for the treatment of many different types of wounds, both chronic and acute. Before applying NPWT, the wound should be cleansed of necrotic tissue and fibrin and its edges should be refreshed [
13,
14]. The most common reasons for using negative pressure therapy include:
An open bone fracture is always accompanied by perforation of soft tissues, with the risk of wound infection. In open fractures, this may be a risk factor for the post-traumatic osteomyelitis development. Treatment of open fractures begins with surgical debridement, i.e. irrigation of the wound and cleansing it of torn and necrotic tissues, as they may delay the repair processes. The effective use of this technique in 15 patients with open fractures was described in 1993 by Wim Fleischmann et al. [1,15]. According to them, the treatment method used in this group of patients resulted in "effective cleansing and conditioning of the wound, with a clear growth of granulation tissue". The introduction of negative pressure therapy in the early healing period effectively limits the development of inflammation, enables the reduction of the wound size without the need to use many microsurgical procedures [1,15].
Chronic ischemia of the lower limbs is most often caused by impaired vascular patency in the course of atherosclerosis. As the disease process progresses, changes such as ulceration, infection, phlegmon, and necrosis appear. In the course of chronic ischemia of the lower limbs, negative pressure therapy is used both to treat ulcers and places after tissue reconstructions using flaps or skin grafts after successful revascularizations [1,16]. Preparing the wound for skin transplantation by stimulating granulation is also an indication for the use of NPWT [1,16].
Burn wounds are prone to infection, and the occurrence of infection significantly impairs and slows down the healing process. The use of negative pressure therapy in the treatment of burns reduces the possibility of wound contamination by microorganisms. Electrical or mechanical-thermal burns may cause massive breakdown of striated muscles. The use of NPWT significantly reduces the concentration of myoglobin in the blood, preventing the occurrence of acute kidney failure. The use of negative pressure therapy also has a positive effect on the healing of the skin graft because it prevents its displacement [1,17]. The standard negative pressure used on burn wounds is between 80 mm Hg and 120 mm Hg, but in case of extensive wounds with exposed blood vessels or nerves, it should be as low as possible. Skillful use of NPWT enables good wound preparation for closure by eliminating infectious agents, stimulating granulation, reducing swelling and ensuring optimal healing conditions [17].
Necrotising fasciitis is a severe bacterial infection that causes necrosis of the skin, connective tissue and fascial compartments. As the disease progresses, blisters filled with dark fluid appear, swelling and necrosis develops reaching to the fascia [17]. Early and aggressive surgical intervention is the most important in treatment. Necrotic tissues are removed with a large margin, which significantly reduces the spread of infection. Material should also be collected for microbiological examination in order to isolate the pathogen and quickly introduce targeted antibiotic therapy. Vacuum therapy should be performed continuously, and the value of the dosed negative pressure should be approximately 125 mm Hg and should be maintained until the infection is controlled, then therapy can be continued intermittently. This scheme gives a good chance of curing the patient and avoids the need to amputate the limb. The NPWT method is also used to secure the graft [18].
A very serious postoperative complication occurring after cardiac surgery is wound infection and sternum instability [1,19]. Treatment of sternum wounds resulting from sternotomy requires simultaneous introduction of antibiotic therapy and negative pressure. In this case, the negative pressure dressing is applied in the operating room. The negative pressure value should initially be 50–70 mm Hg and should gradually increase up to 125 mm Hg. Therapy should always be performed continuously, which enables stabilization of the sternum and shoulder girdle and helps to avoid mechanical damage to the right ventricle of the heart. The negative pressure dressing should be replaced not less frequently than every 3 days [19].
Complicated wounds treated with the open abdominal technique constitute a major problem in surgery. An increase in intra-abdominal pressure leads to a significant deterioration of tissue perfusion and changes within the peritoneal cavity. NPWT facilitates the control of intra-abdominal pressure and ensures continuous outflow of secretions, which significantly improves the results of open abdominal treatment. Wound dehiscence or infection, entero-atmospheric fistulas and stomas complicated by necrosis are among the indications for the use of negative pressure therapy in the abdominal cavity [5].
Anastomotic leak is the most common postoperative complication after anterior rectal resection. Endoscopic negative pressure therapy is a relatively new method of treating documented anastomotic leak with the presence of a leakage cavity outside the intestinal lumen. In the first stage, an endoscope should be introduced into the abscess cavity and it should be cleansed by rinsing. Before insertion, the sponge should be cut appropriately so that it tightly fills the abscess cavity but does not protrude into the rectum. The use of a special cover in which the sponge is placed minimizes tissue traumatization. The vacuum value should be between 50–125 mm Hg. The dressing should be replaced every 2–3 days The use of E-VAC enables to eliminate the unpleasant odor that usually occurs in case of abscesses or fistulas in this location [20].
Diabetic foot syndrome is a serious clinical problem among diabetic patients. The pain and unpleasant odor accompanying the wound are factors that isolate the patient from society. Additionally, the wound location makes it difficult to move normally, which is why the patient often loses the ability to perform their previous social roles. Regardless of the cause of diabetic foot syndrome, it is worth implementing negative pressure treatment because it improves tissue blood supply, reduces the size of the wound, limits infection and minimizes the need to amputate the limb. [21].
The location of the lesions in the perianal area makes it very difficult to cover them with classic dressings. This is due to the direct proximity of the mouths of the digestive and urinary tracts, and additionally, in case of women, to the reproductive system. Changes occurring around the perianal location include:
o perianal fistulas,
o pilonidal cyst,
o Fournier's gangrene,
o rectum and crotch injuries,
o skin diseases in the buttock area,
o wounds and bedsores in the sacrum area,
o perineal wounds with complicated healing,
o failure of colon low anastomoses [1,22].
Applying a negative pressure dressing in the perianal area requires great precision. When applying a dressing using sponges, their number should be precisely determined and documented to avoid leaving material in the wound. If the patient experiences very severe pain during therapy, the negative pressure parameters should be reduced. For NPWT to have a therapeutic effect, the negative pressure value should not be less than 70 mm Hg. The use of negative pressure therapy accelerates the process of granulation tissue formation and reduces the wound size. A tight dressing protects the wound against infection with secretions, positively affecting wound healing.
In case of wounds, the most common problem is severe bleeding, which outside controlled conditions (hospital, outpatient clinic) can lead to death and must be absolutely held back until professional help arrives or until transport to a medical facility. The most popular modern methods of stopping bleeding include:
They have been known for decades in virtually unchanged form and are still used today. Limb hemorrhage constitutes 60% of preventable combat deaths. It has been shown that using a tourniquet before the symptoms of hemorrhagic shock occur increases the chance of survival by 96%, therefore the ease of use of the tourniquet and the ability of the injured person to do it (using one hand) are important. Indications for the use of a tourniquet are:
o hemorrhages from limbs that cannot be controlled by other methods,
o hemorrhage occurring in conjunction with airway obstruction or cardiac arrest; quickly stopping the bleeding with a tourniquet allows intervention in another area,
o hemorrhages from trapped limbs in places difficult to access for rescuers,
o mass events in which the amount of forces and resources does not allow to control hemorrhages by other methods.
They are a modern method of stopping bleeding in combat conditions. Their aim is to close the lumen and thus the blood flow through large blood vessels in the pelvis. Due to their size, the buckles are not part of the soldier's personal dressing, and third parties are required to use them.
As can be seen from the above, dressings that stop bleeding can be divided into two categories: pressure dressings (where pressure is exerted from the outside) and dressings soaked in substances that increase blood clotting. Due to human anatomy (the main blood vessels run inside the body, and their compression can lead to death and often makes it difficult to determine the place of bleeding), pressure dressings are difficult (and sometimes even impossible) to use on wounds located on the patient's torso, which makes them useful mainly in case of limbs.
Dressings soaked in chemical substances, due to the necessity to introduce gauze (a hemostatic substance) around the bleeding site, require a large enough wound diameter as well as knowledge regarding the location of the bleeding site. In case of gunshot and stab wounds to the torso, this may be difficult to achieve.
Considering the above, it seems that vacuum dressings may be effective in stopping bleeding from wounds that penetrate deep into the body. An additional advantage is the possibility of treating pneumothorax in penetrating chest wounds, as well as the low risk of complications.
Vacuum-Assisted Closure (VAC) dressings are advanced systems used in the treatment of difficult-to-heal wounds. These dressings use controlled negative pressure to aid the healing process. There are several types of negative pressure dressings, each designed for different types of wounds and clinical situations:
-
Foam dressing:
o V.A.C. GranuFoam™: Highly elastic foam dressings used for deep, complex wounds,
o V.A.C. GranuFoam Silver™: Contains silver, which has antibacterial properties, which helps in the treatment of wounds at infection risk;
-
Gauze dressing:
-
Specialty dressing:
VAC dressings can have different sizes and, therefore, different scope of application. The appropriate set choice depends on the size of the wound, its location, amount of exudate and the specific therapeutic needs of the patient. The decision to choose a specific set is usually made by the medical team, taking into consideration patient’s individual needs and the characteristics of the wound.
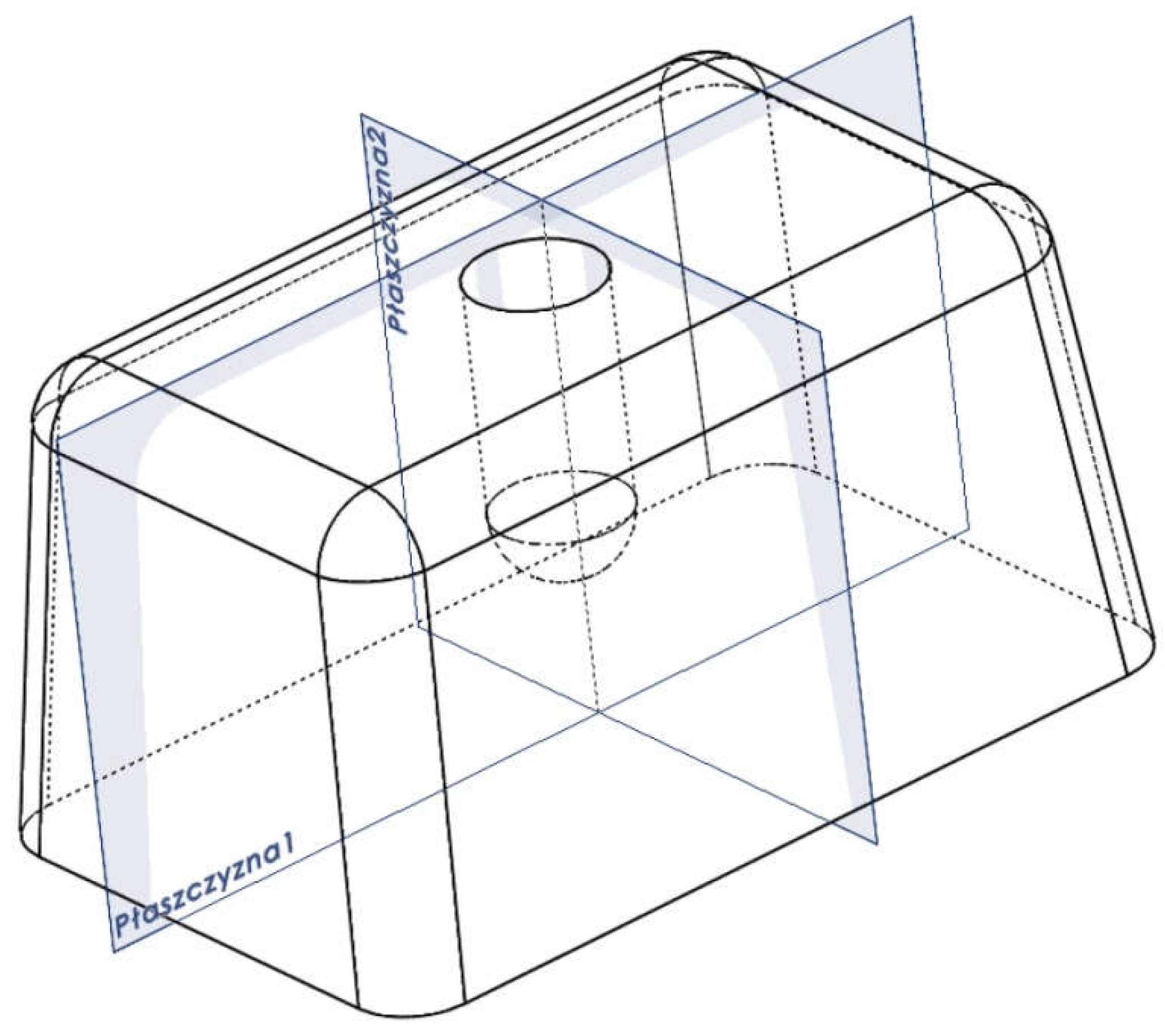
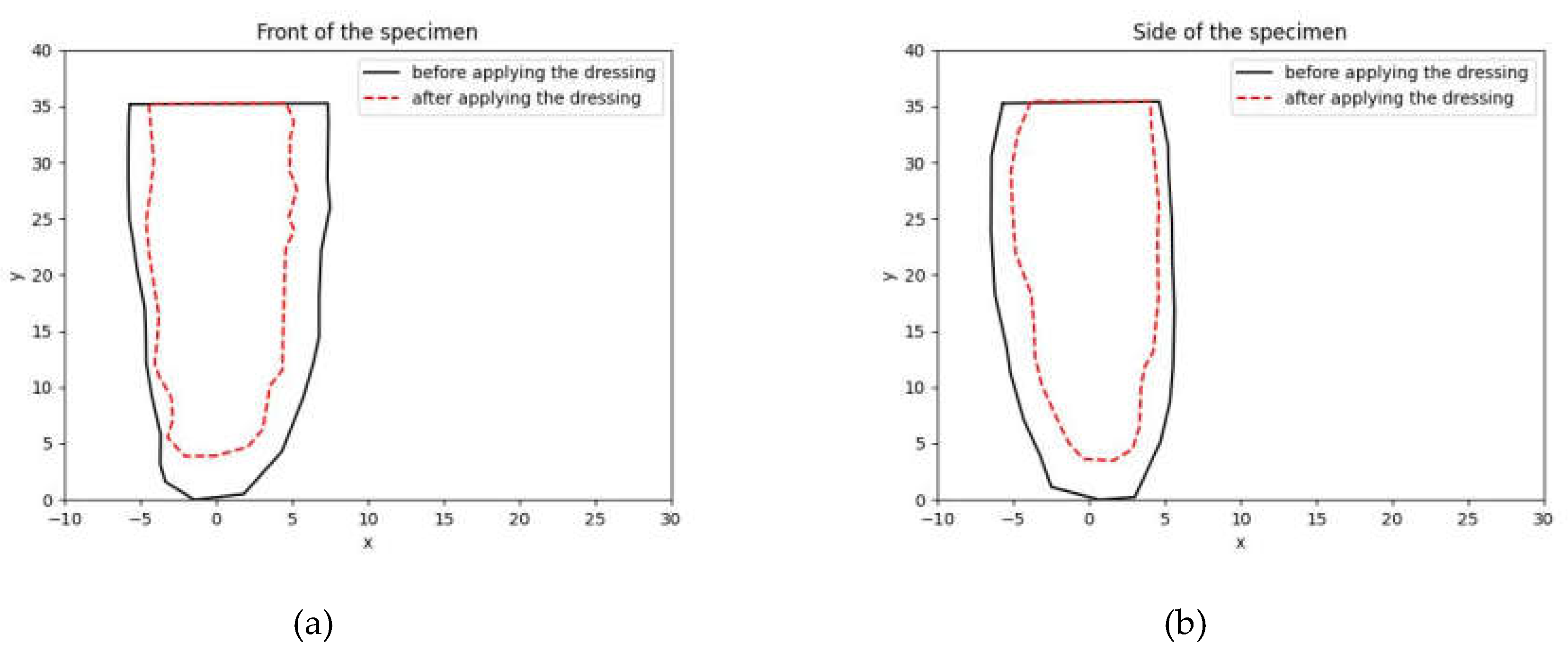
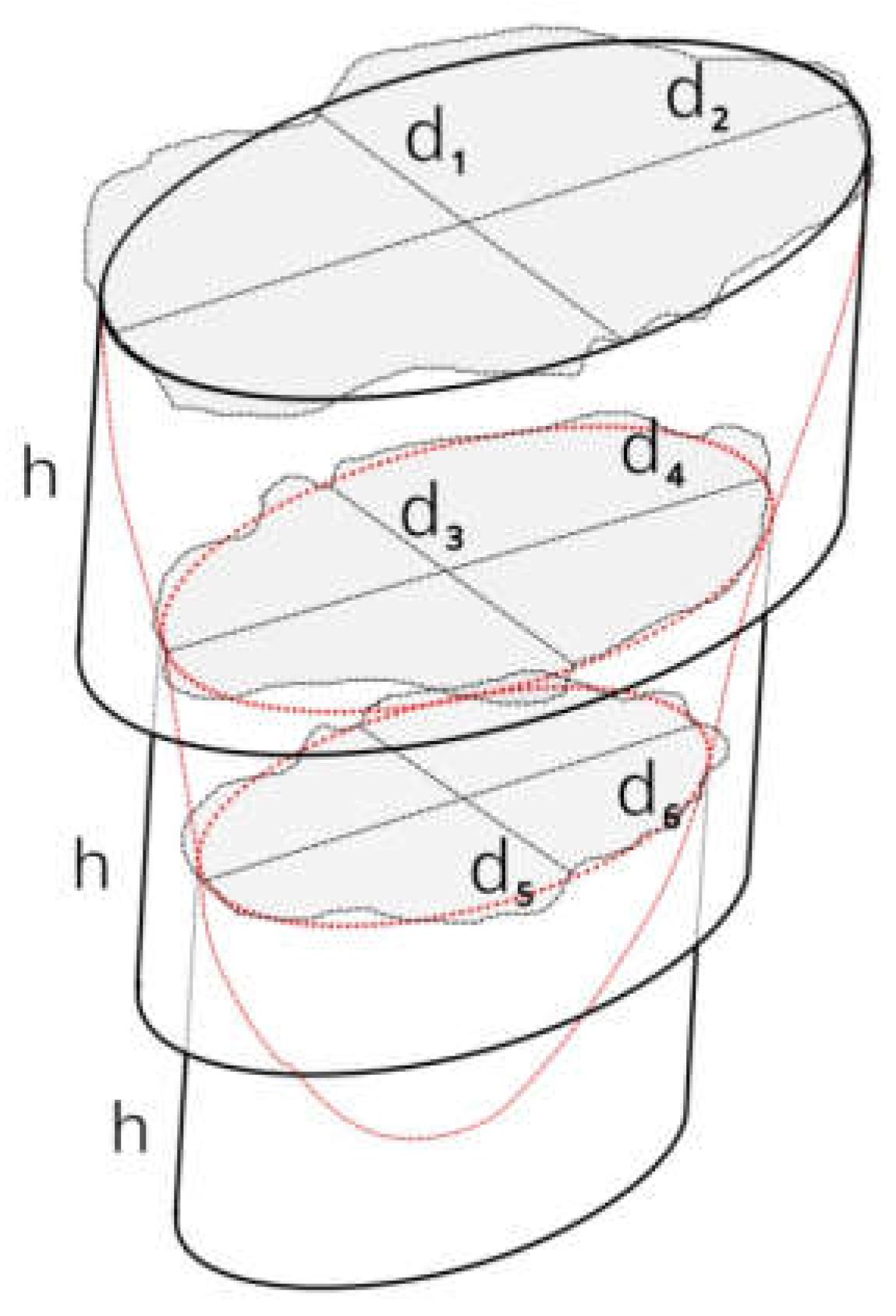
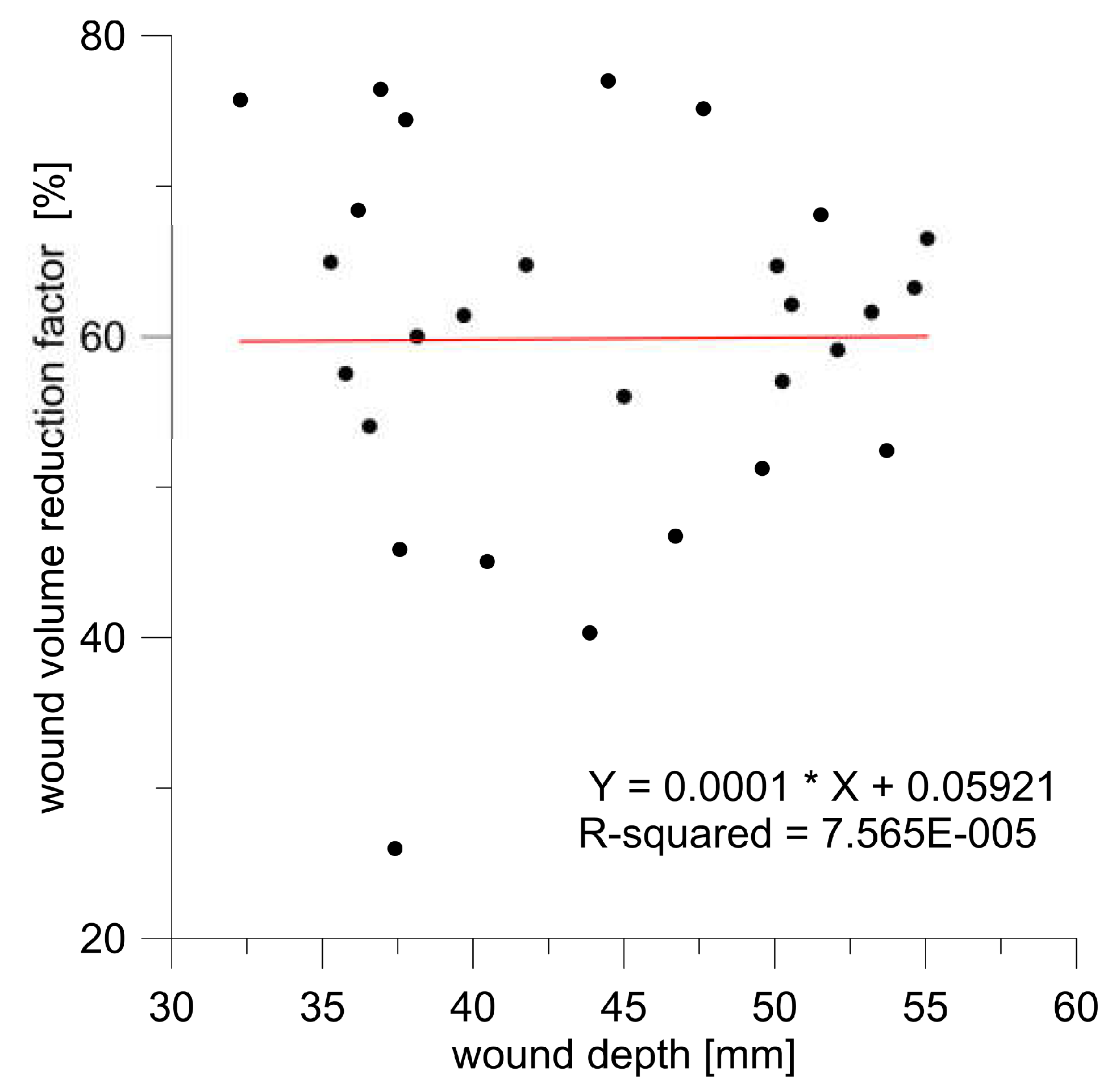
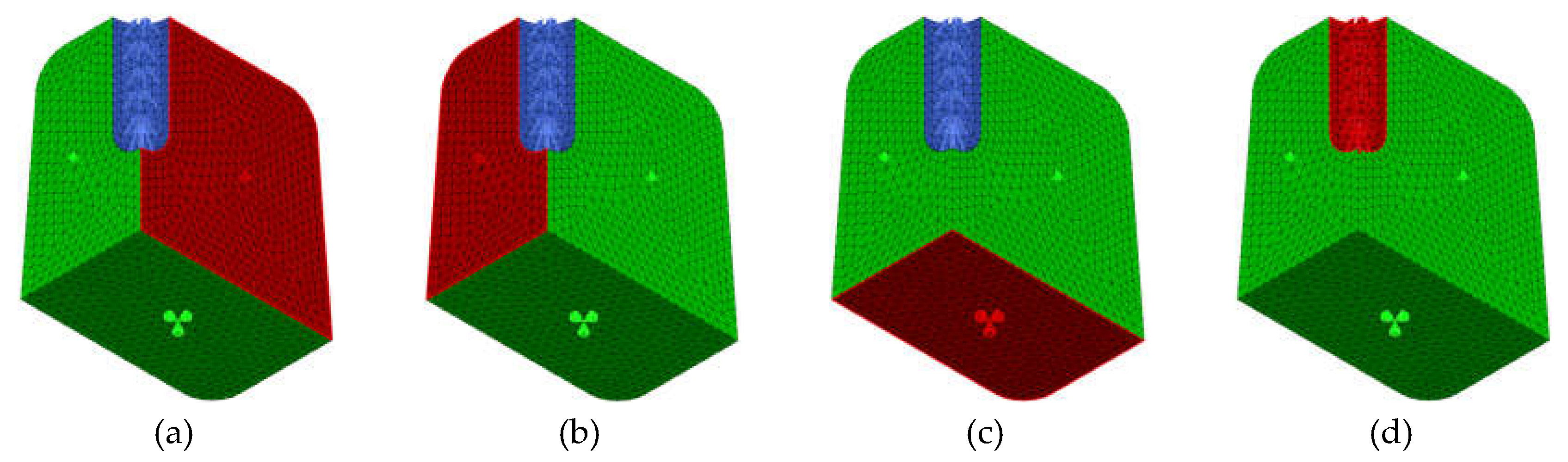
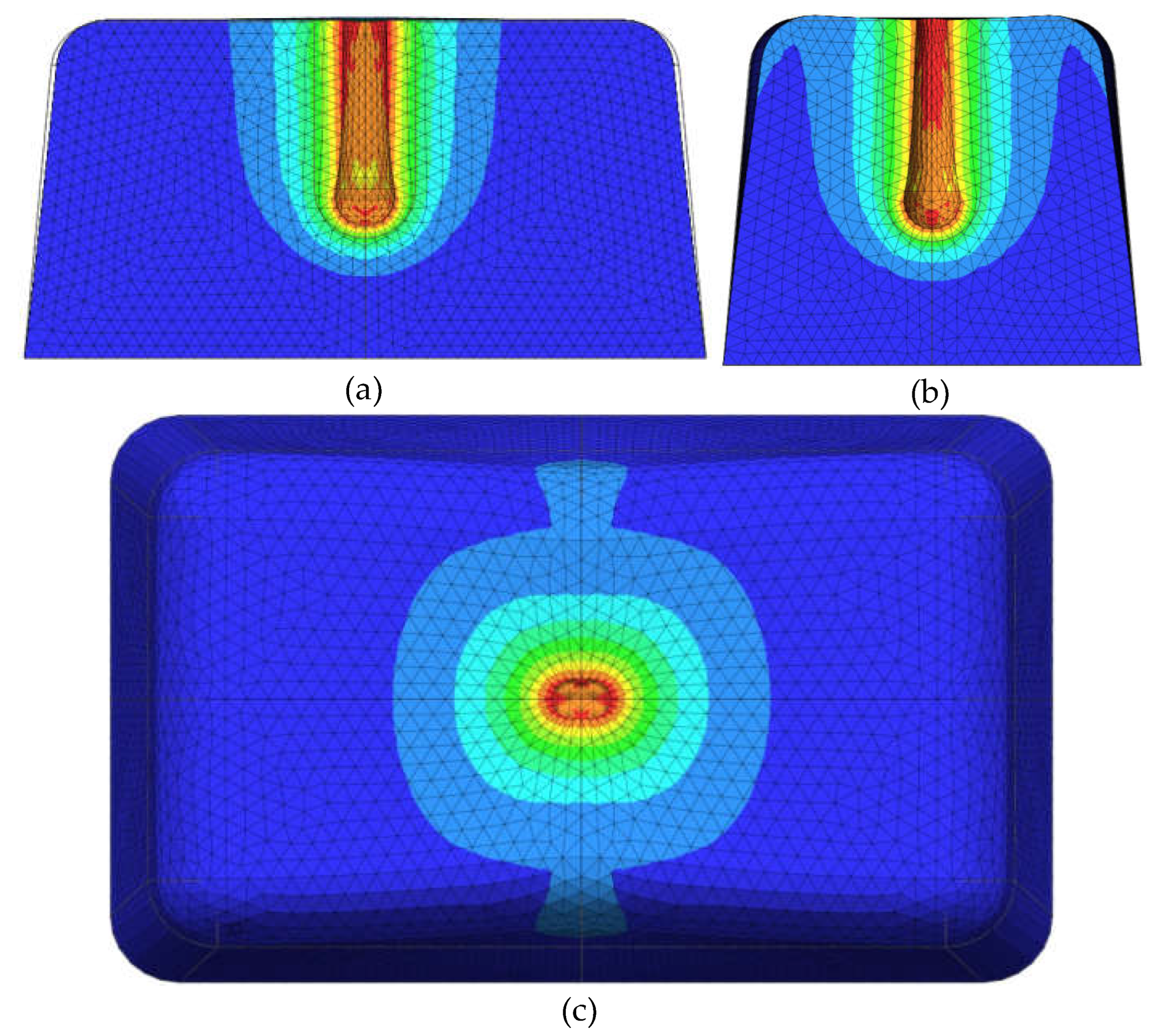
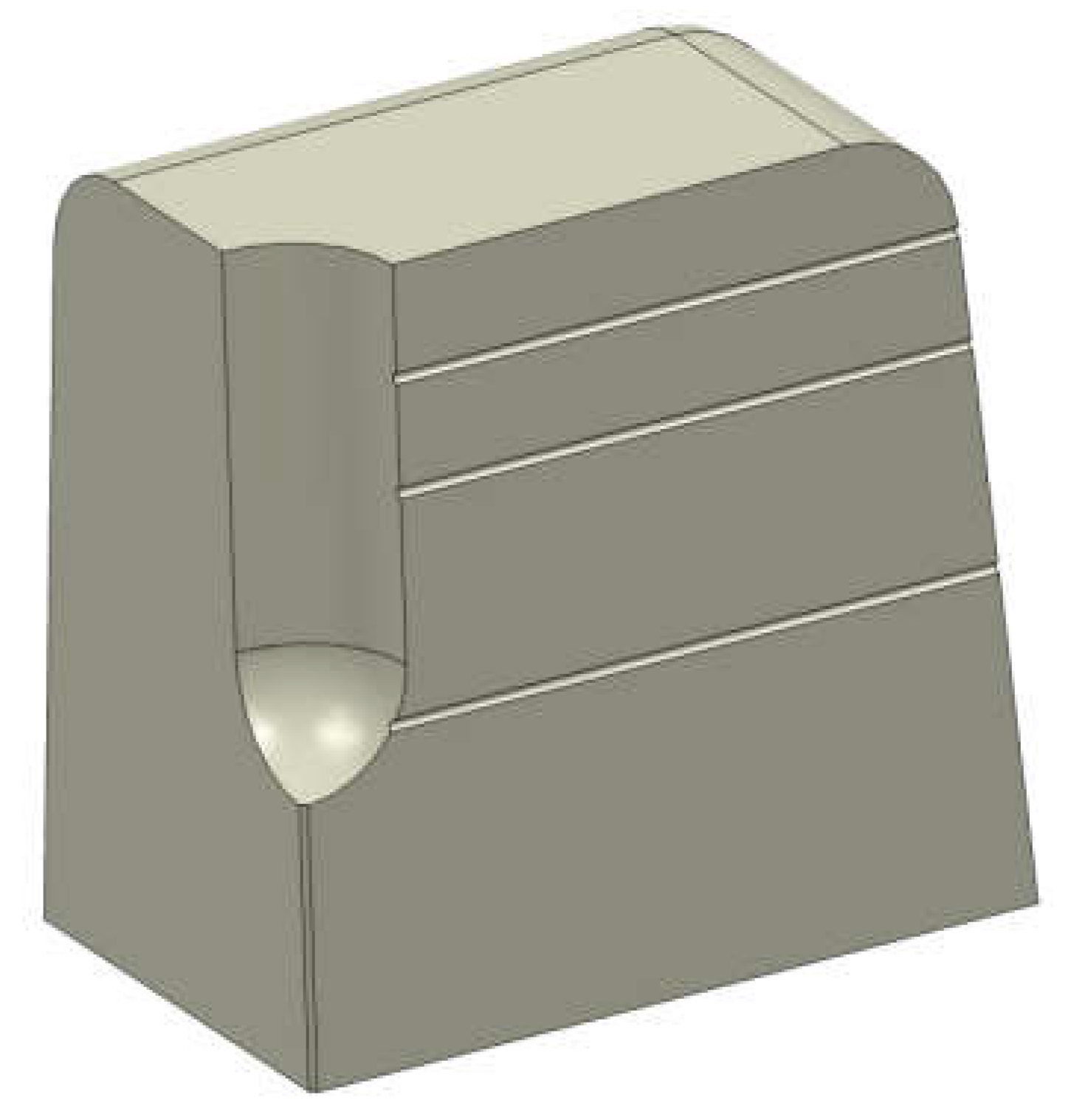
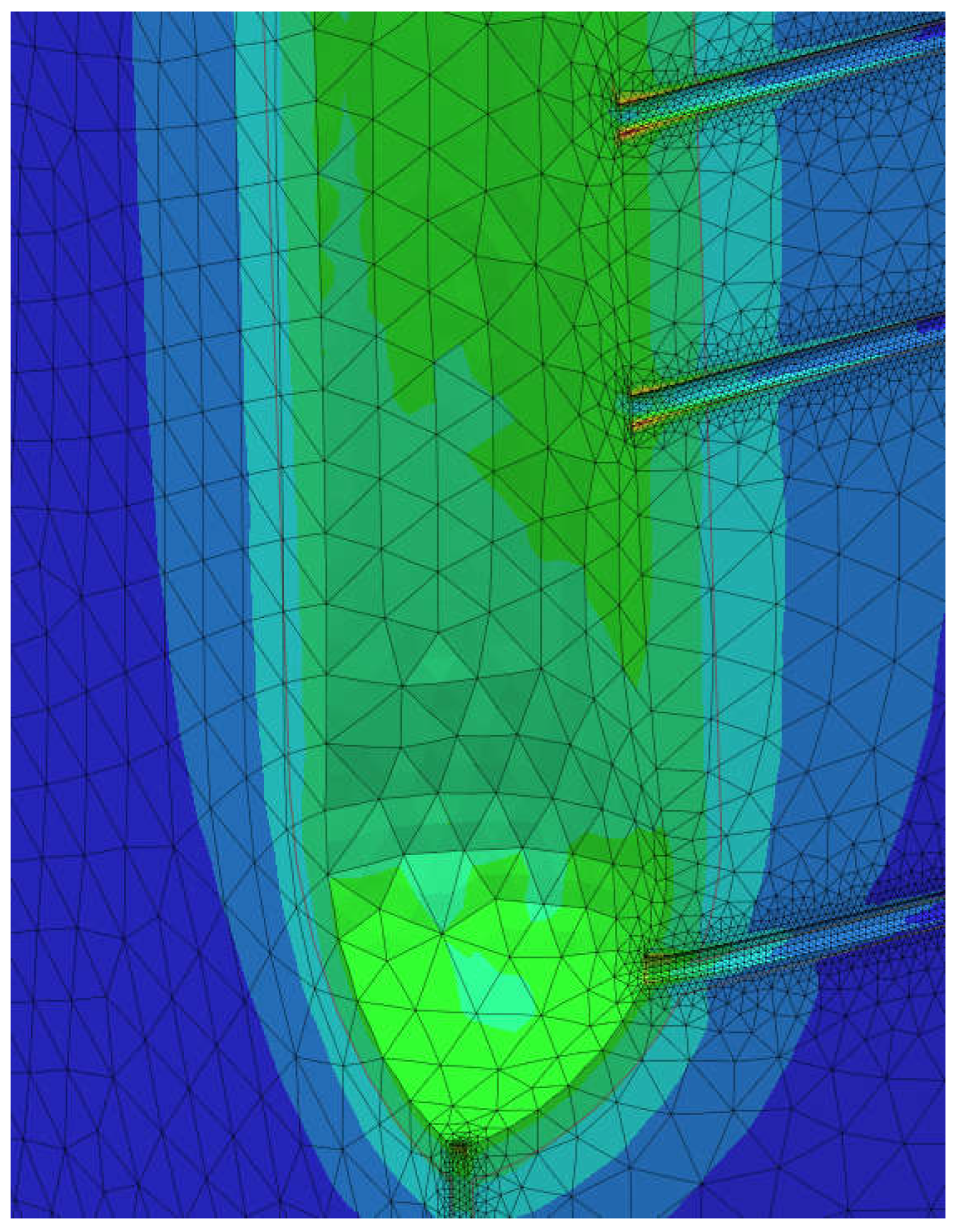
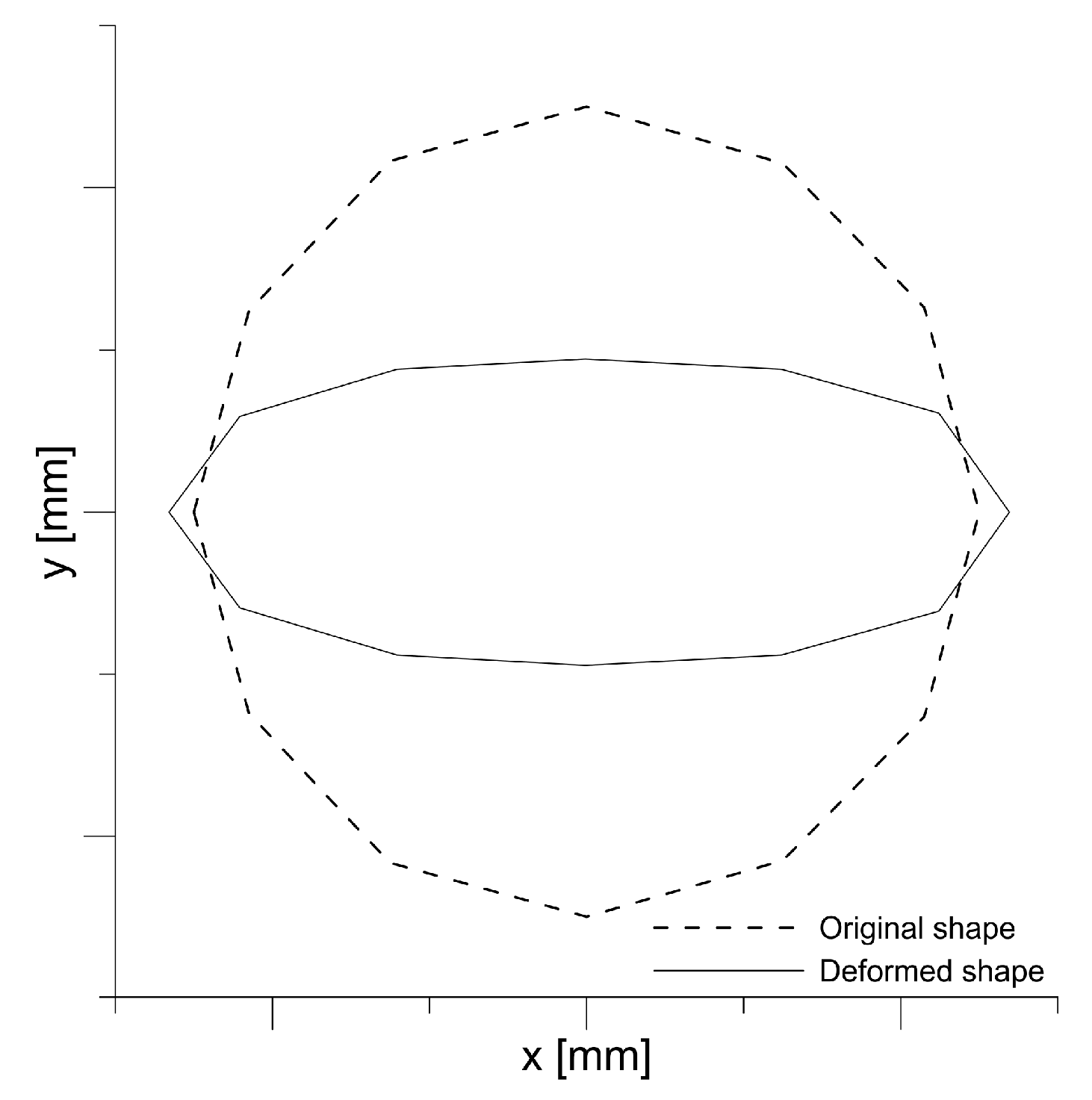
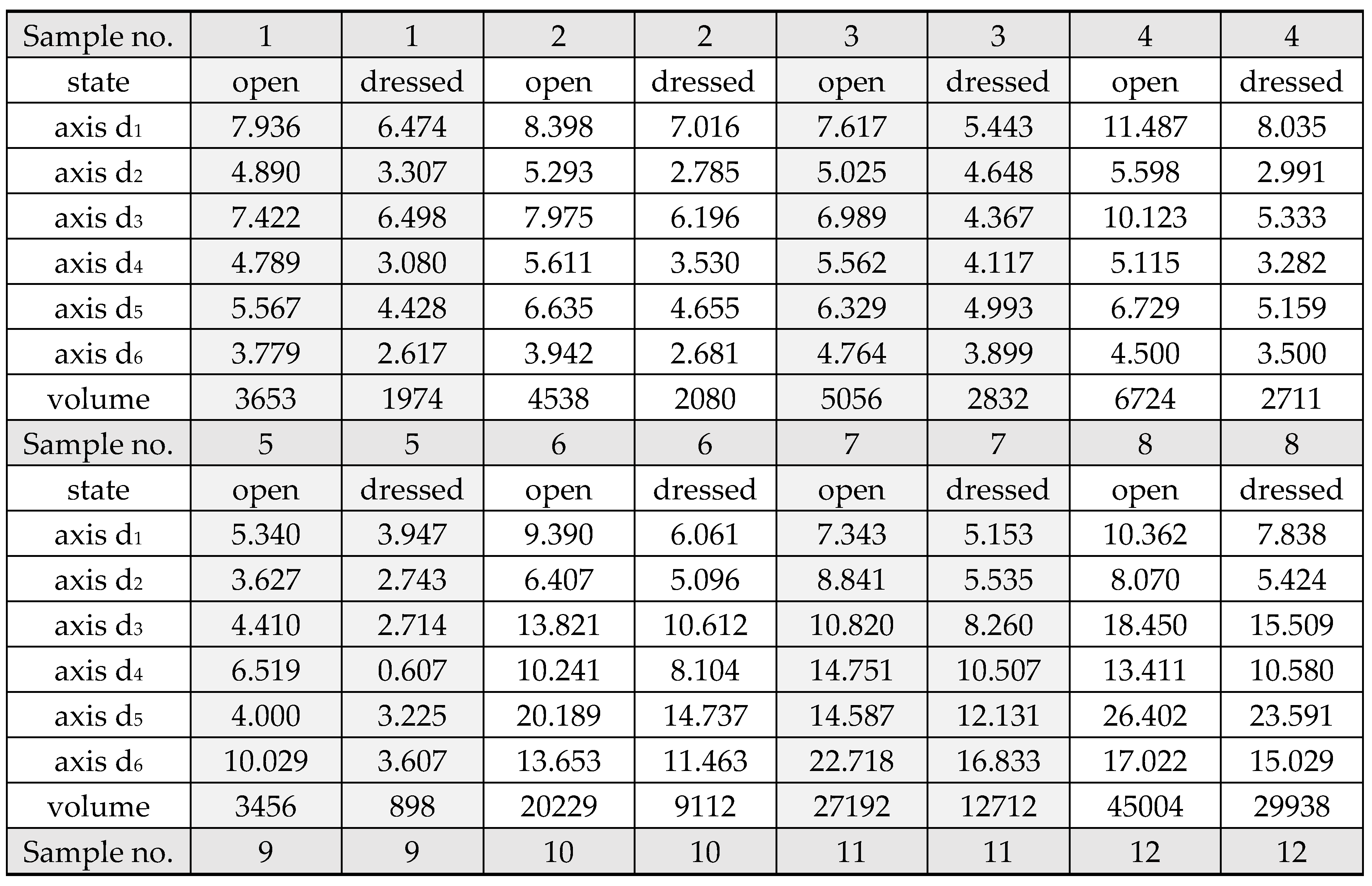
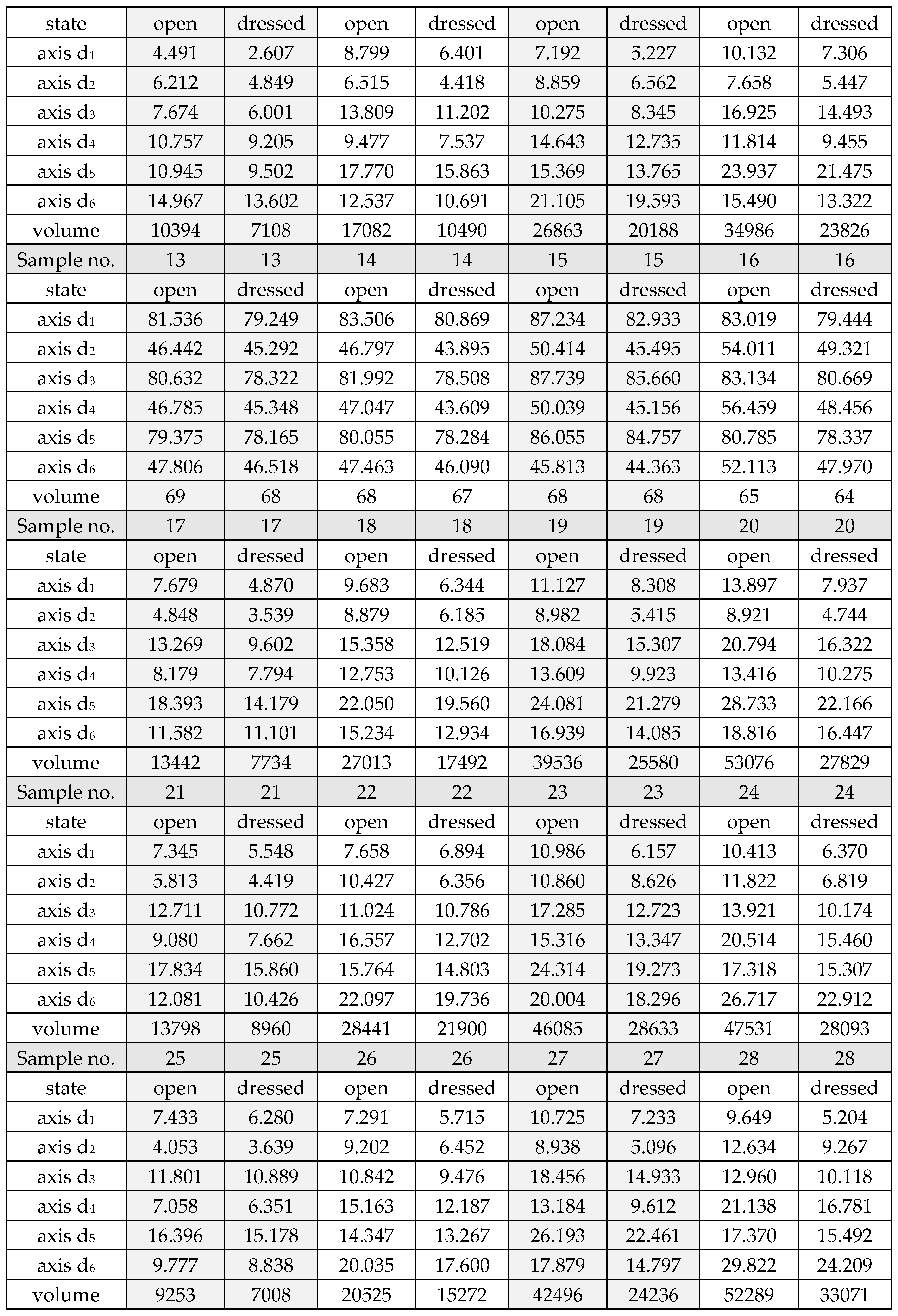
The article presents the results of research on the behavior of a wound covered with a negative pressure dressing.