Submitted:
13 October 2024
Posted:
14 October 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
2.1. Group H
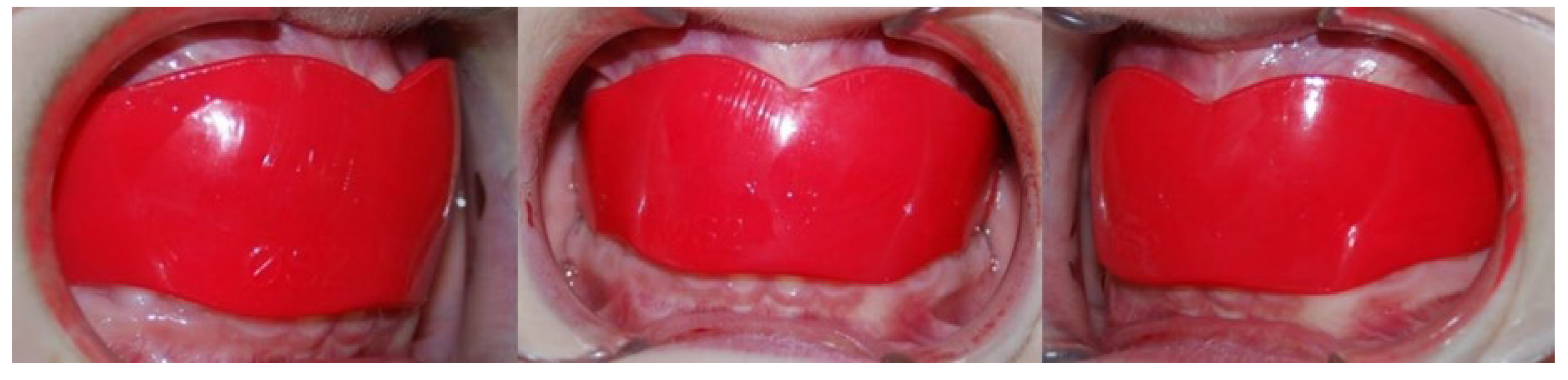
2.2. Group EA
2.3. Group C
2.4. Cephalometric Analysis
2.5. Statistical Analysis
3. Results
3.1. Dental Outcomes
3.2. Aesthetic Outcomes
3.3. Comparison of Outcomes between Groups
- -
- 1+SN: was 3.85° greater in Group C than in Group H, and in Group EA was 4.47° greater than in Group H.
- -
- IMPA: was 5.73° greater in Group H than in Group C and 4.48° greater in Group H than in Group EA.
- -
- 1+TVL: in Group H was 2.19° greater than in Group C.
- -
- UL-TVL: was 2.29° greater in Group C than in Group H, and in Group EA was 1.71° greater than in Group H.
- -
- LL-TVL: in Group H was 2.72° greater than in Group EA.
4. Discussion
Limitations of the Study
5. Conclusions
Contribution
Disclosure of interest
References
- Alhammadi MS, Halboub E, Fayed MS, Labib A, El-Saaidi C: Global distribution of malocclusion traits: A systematic review. Dental Press J Orthod 2018, 23(6):40 e41-40 e10.
- Bock NC, von Bremen J, Ruf S: Stability of Class II fixed functional appliance therapy--a systematic review and meta-analysis. Eur J Orthod 2016, 38(2):129-139.
- ngle EH: Classification of malocclusion. Dent Cosmos 1899, 41:350-357.
- McNamara JA, Jr.: Components of class II malocclusion in children 8-10 years of age. Angle Orthod 1981, 51(3):177-202.
- von Bremen J, Erbe C, Pancherz H, Ruf S: Facial-profile attractiveness changes in adult patients treated with the Herbst appliance. J Orofac Orthop 2014, 75(3):167-174.
- Moss ML: The functional matrix hypothesis revisited. 4. The epigenetic antithesis and the resolving synthesis. Am J Orthod Dentofacial Orthop 1997, 112(4):410-417.
- Baysal A, Uysal T: Soft tissue effects of Twin Block and Herbst appliances in patients with Class II division 1 mandibular retrognathy. Eur J Orthod 2013, 35(1):71-81.
- Di Palma E, Tepedino M, Chimenti C, Tartaglia GM, Sforza C: Effects of the functional orthopaedic therapy on masticatory muscles activity. J Clin Exp Dent 2017, 9(7):e886-e891.
- Ciavarella D, Lo Russo L, Nichelini J, Mastrovincenzo M, Barbato E, Laurenziello M, Montaruli G, Lo Muzio L: Treatment of hyperdivergent growth pattern and anterior open bite with posterior metallic bite planes. Minerva Stomatol 2017, 66(6):267-274.
- Ciavarella D, Campobasso A, Campa R, Suriano C, Illuzzi G, Cazzolla A, Tepedino M: Cephalometric effects of the elastodontic appliance in managing skeletal Class II division 1 cases. Australasian Orthodontic Journal 2021, 37:251-258.
- Ruf S: Orthodontic treatment of the Class II noncompliant patient. Current principles and techniques (2006). European Journal of Orthodontics 2007, 29(1):110-110.
- Atresh A, Cevidanes LHS, Yatabe M, Muniz L, Nguyen T, Larson B, Manton DJ, Schneider PM: Three-dimensional treatment outcomes in Class II patients with different vertical facial patterns treated with the Herbst appliance. Am J Orthod Dentofacial Orthop 2018, 154(2):238-248 e231.
- Pancherz H, Anehus-Pancherz M: Facial profile changes during and after Herbst appliance treatment. Eur J Orthod 1994, 16(4):275-286.
- Keski-Nisula K, Keski-Nisula L, Salo H, Voipio K, Varrela J: Dentofacial changes after orthodontic intervention with eruption guidance appliance in the early mixed dentition. Angle Orthod 2008, 78(2):324-331.
- Usumez S, Uysal T, Sari Z, Basciftci FA, Karaman AI, Guray E: The effects of early preorthodontic trainer treatment on Class II, division 1 patients. Angle Orthod 2004, 74(5):605-609.
- Keski-Nisula K, Keski-Nisula L, Varrela J: Class II treatment in early mixed dentition with the eruption guidance appliance: effects and long-term stability. Eur J Orthod 2020, 42(2):151-156.
- Moresca AHK, de Moraes ND, Topolski F, Flores-Mir C, Moro A, Moresca RC, Correr GM: Esthetic perception of facial profile changes in Class II patients treated with Herbst or Forsus appliances. Angle Orthod 2020, 90(4):571-577.
- von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP, Initiative S: The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies. Int J Surg 2014, 12(12):1495-1499.
- Cohen J: Statistical Power Analysis. Current Directions in Psychological Science 1992, 1(3):98-101.
- Arnett GW, Jelic JS, Kim J, Cummings DR, Beress A, Worley CM, Jr., Chung B, Bergman R: Soft tissue cephalometric analysis: diagnosis and treatment planning of dentofacial deformity. Am J Orthod Dentofacial Orthop 1999, 116(3):239-253.
- Spyropoulos MN, Halazonetis DJ: Significance of the soft tissue profile on facial esthetics. Am J Orthod Dentofacial Orthop 2001, 119(5):464-471.
- Quintao C, Helena I, Brunharo VP, Menezes RC, Almeida MA: Soft tissue facial profile changes following functional appliance therapy. Eur J Orthod 2006, 28(1):35-41.
- Galluccio G, Guarnieri R, Jamshir D, Impellizzeri A, Ierardo G, Barbato E: Comparative Evaluation of Esthetic and Structural Aspects in Class II Functional Therapy. A Case-Control Retrospective Study. Int J Environ Res Public Health 2021, 18(13).
- . Irezli EC, Baysal A: Changes in the craniofacial structures and esthetic perceptions of soft-tissue profile alterations after distalization and Herbst appliance treatment. Am J Orthod Dentofacial Orthop 2021, 159(3):292-304.


| Dental measurements | |
|---|---|
| 1+SN | Basal incisor angle between the line joining S-N and the straight line passing between the incisal edge and API+ (Apical Point upper Incisor) |
| IMPA | Incisor angle between the line passing through the lower incisor margin and API- (Apical Point lower Incisor) and the Go-Me line |
| 1+TVL | Linear distance between the most vestibular point of 1+ and the TVL |
| Aesthetic measurements | |
| SupportLab-TVL | Linear value of the distance between the lip support point and the True Vertical Line |
| UL-TVL | Linear value of the distance between the most protruding point of the upper lip and the True Vertical Line |
| LL-TVL | Linear value of the distance between the most protruding point of the lower lip and the True Vertical Line |
| B’-TVL | Linear value of the distance between the most recessed point of the chin and the True Vertical Line |
| POG’-TVL | Linear value of the distance between the most protruding point of the chin and the True Vertical Line |
| Group C | GROUP EA | GROUP H | ||||
|---|---|---|---|---|---|---|
|
1+SN Median Mean Std.Deviation Std.Error of mean Normality test P value |
T0 | T1 | T0 | T1 | T0 | T1 |
|
103,72 105,90 4,82 1,07 N.S. |
106,12 107 5,80 1,29 N.S. |
97,96 96,85 10,84 2,42 <0.05 |
101,10 100,90 7,77 1,73 <0.05 |
109,50 110,00 7,74 1,73 N.S. |
108,20 107,50 6,42 1,43 <0.05 |
|
| N.S. | p< 0.01 | p< 0.01 | ||||
|
IMPA Median Mean Std.Deviatiom Std.Error of mean Normality test P value |
92,13 90,85 6,48 1,45 <0.05 |
93,25 91,18 7,24 1,62 <0.05 |
95,49 95,98 3,09 0,69 <0.05 |
96,58 97,20 6,34 1,41 <0.05 |
95,47 94,79 3,99 0,89 N.S. |
100,70 100,90 3,45 0,77 N.S. |
| N.S. | N.S. | p< 0.01 | ||||
|
1+TVL Median Mean Std.Deviation Std.Error of mean Normality test P value |
-10,65 -11,98 2,82 0,63 <0.05 |
-11,89 -10,57 2,54 0,57 <0.05 |
-9,89 -9,66 2,46 0,55 N.S. |
-9,41 -8,83 2,24 0,50 N.S. |
-8,08 -8,33 2,02 0,45 N.S. |
-9,39 -9,11 1,50 0,33 N.S. |
| N.S. | N.S. | N.S. | ||||
|
SupportLab-TVL Median Mean Std. Deviation Std. Error of Mean Normality test P value |
-0,21 -0,24 0,68 0,15 <0.05 |
0,02 0,04 2,0 0,44 <0.05 |
-0,03 0,36 1,74 0,39 N.S. |
-0,08 0,04 0,93 0,20 N.S. |
-0,66 -0,44 0,86 0,19 N.S. |
-0,28 -0,08 1,01 0,22 <0.05 |
| N.S. | N.S. | N.S. | ||||
|
UL TVL Median Mean Std. Deviation Std. Error of Mean Normality test P value |
1,29 1,49 1,92 0,42 N.S. |
0,68 0,71 3,26 0,72 N.S. |
2,33 2,09 2,13 0,47 <0.05 |
1,76 2,04 2,26 0,50 N.S. |
0,80 1,05 1,13 0,25 N.S. |
0,88 1,37 1,31 0,29 N.S |
| N.S. | N.S. | N.S. | ||||
|
LL TVL Median Mean Std. Deviation Std. Error of Mean Normality test P value |
-5,17 -5,44 4,00 0,89 <0.05 |
-3,43 -3,77 3,48 0,77 <0.05 |
-2,86 -2,33 2,96 0,66 <0.05 |
-1,19 -1,42 3,35 0,75 N.S. |
-2,71 -2,82 1,89 0,42 N.S. |
0,18 -0,51 2,21 0,49 N.S. |
| p<0.01 | N.S. | p< 0.01 | ||||
|
B’ TVL Median Mean Std. Deviation Std. Error of Mean Normality test P value |
-15,26 -15,81 5,12 1,14 <0.05 |
-13,31 -13,86 3,74 0,83 <0.05 |
-11,65 -12,19 2,96 0,66 N.S. |
-9,58 -10,40 3,95 0,88 N.S. |
-12,27 -12,33 2,55 0,57 N.S. |
-8,83 -10,07 3,50 0,78 N.S. |
| N.S. | p< 0.01 | p<0.05 | ||||
|
POG’ TVL Median Mean Std. Deviation Std. Error of Mean Normality test P value |
-18,93 -17,73 5,42 1,21 N.S. |
-15,32 -14,43 5,49 1,22 N.S. |
-13,63 -12,85 3,42 0,76 <0.05 |
-10,19 -10,01 3,51 0,78 <0.05 |
-11,95 -12,86 4,30 0,96 N.S. |
-7,57 -10,28 5,98 1,33 N.S. |
| p<0.05 | p<0.01 | p <0.05 | ||||
| Sum of squares | df | Mean square | F | Sig. | ||
|---|---|---|---|---|---|---|
| 1+SN | Between groups | 234.82 | 4 | 117.41 | 7.294 | 0.002* |
| Within groups | 917.55 | 114 | 16.09 | |||
| Total | 1152.37 | 118 | ||||
| 1-GOME(IMPA) | Between groups | 381.28 | 4 | 190.61 | 8.49 | 0.001* |
| Within groups | 1279.46 | 114 | 22.447 | |||
| Total | 1660.70 | 118 | ||||
| 1+TVL | Between groups | 51.52 | 4 | 25.76 | 4.32 | 0.018* |
| Within groups | 339.88 | 114 | 5.96 | |||
| Total | 391.40 | 118 | ||||
| SUPPORTLAB-TVL | Between groups | 5.45 | 4 | 2.72 | 1.06 | 0.353 |
| Within groups | 146.39 | 114 | 2.56 | |||
| Total | 151.85 | 118 | ||||
| UL TVL | Between groups | 56.81 | 4 | 28.40 | 14.57 | 0.000* |
| Within groups | 111.06 | 114 | 1.94 | |||
| Total | 167.87 | 118 | ||||
| LL TVL | Between groups | 74.26 | 4 | 37.13 | 5.60 | 0.006* |
| Within groups | 377.47 | 114 | 6.62 | |||
| Total | 451.73 | 118 | ||||
| B’ TVL | Between groups | 5.38 | 4 | 2.69 | 0.21 | 0.805 |
| Within groups | 705.64 | 114 | 12.38 | |||
| Total | 711.02 | 118 | ||||
| POG’ TVL | Between groups | 10.90 | 4 | 5.45 | 0.29 | 0.750 |
| Within groups | 1073.05 | 114 | 18.82 | |||
| Total | 1083.96 | 118 | ||||
| Dependent variable | (I) Group | (J) Group | Mean difference (I − J) |
Std error | Sig. | 95% Confidence interval | |
|---|---|---|---|---|---|---|---|
| Lower bound | Upper bound | ||||||
| 1+SN | C EA EA |
H | 3.85* | 1.26 | 0.01 | 0.79 | 6.90 |
| C | 0.62 | 1.26 | 0.87 | −2.42 | 3.67 | ||
| H | 4.47* | 1.26 | 0.00 | 1.42 | 7.25 | ||
| 1-GOME (IMPA) | C EA EA |
H | -5.73* | 1.49 | 0.00 | -9.34 | -2.13 |
| C | 0.89 | 1.49 | 0.82 | −2.70 | 4.50 | ||
| H | -4.84* | 1.49 | 0.00 | -8.44 | -1.23 | ||
| 1+TVL | C EA EA |
H | -2.19* | 0.77 | 0.01 | 0.33 | 4.05 |
| C | -0.59 | 0.77 | 0.72 | -2.45 | 1.26 | ||
| H | 1.60 | 0.77 | 0.10 | -0.25 | 3.45 | ||
| SUPPORTLAB-TVL | C EA EA |
H | -0.10 | 0.50 | 0.97 | -1.32 | 1.11 |
| C | -0.57 | 0.50 | 0.49 | -1.79 | 0.64 | ||
| H | -0.68 | 0.50 | 0.37 | -1.90 | 0.53 | ||
| UL TVL | C EA EA |
H | 2.29* | 0.44 | 0.00 | 1.22 | 3.35 |
| C | -0.57 | 0.44 | 0.39 | -1.63 | 0.48 | ||
| H | 1.71* | 0.44 | 0.00 | 0.65 | 2.77 | ||
| LL TVL | C EA EA |
H | -1.33 | 0.81 | 0.23 | -3.29 | 0.62 |
| C | -1.38 | 0.81 | 0.21 | -3.34 | 0.56 | ||
| H | -2.72* | 0.81 | 0.00 | -4.68 | -0.76 | ||
| B’ TVL | C EA EA |
H | -0.30 | 1.11 | 0.96 | -2.97 | 2.37 |
| C | -0.42 | 1.11 | 0.92 | -3.10 | 2.24 | ||
| H | -0.73 | 1.11 | 0.79 | -3.40 | 1.94 | ||
| POG’ TVL | C EA EA |
H | 1.04 | 1.37 | 0.72 | -2.25 | 4.34 |
| C | -0.49 | 1.37 | 0.93 | -3.79 | 2.80 | ||
| H | 0.54 | 1.37 | 0.91 | -2.75 | 3.85 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





