Submitted:
08 October 2024
Posted:
09 October 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
2.1. Dogs
2.2. Histopathology and Immunohistochemistry
2.3. Image Capture and Analysis
2.4. Statistical Analysis
3. Results
3.1. Relationship between Each Stage and Age or Sex
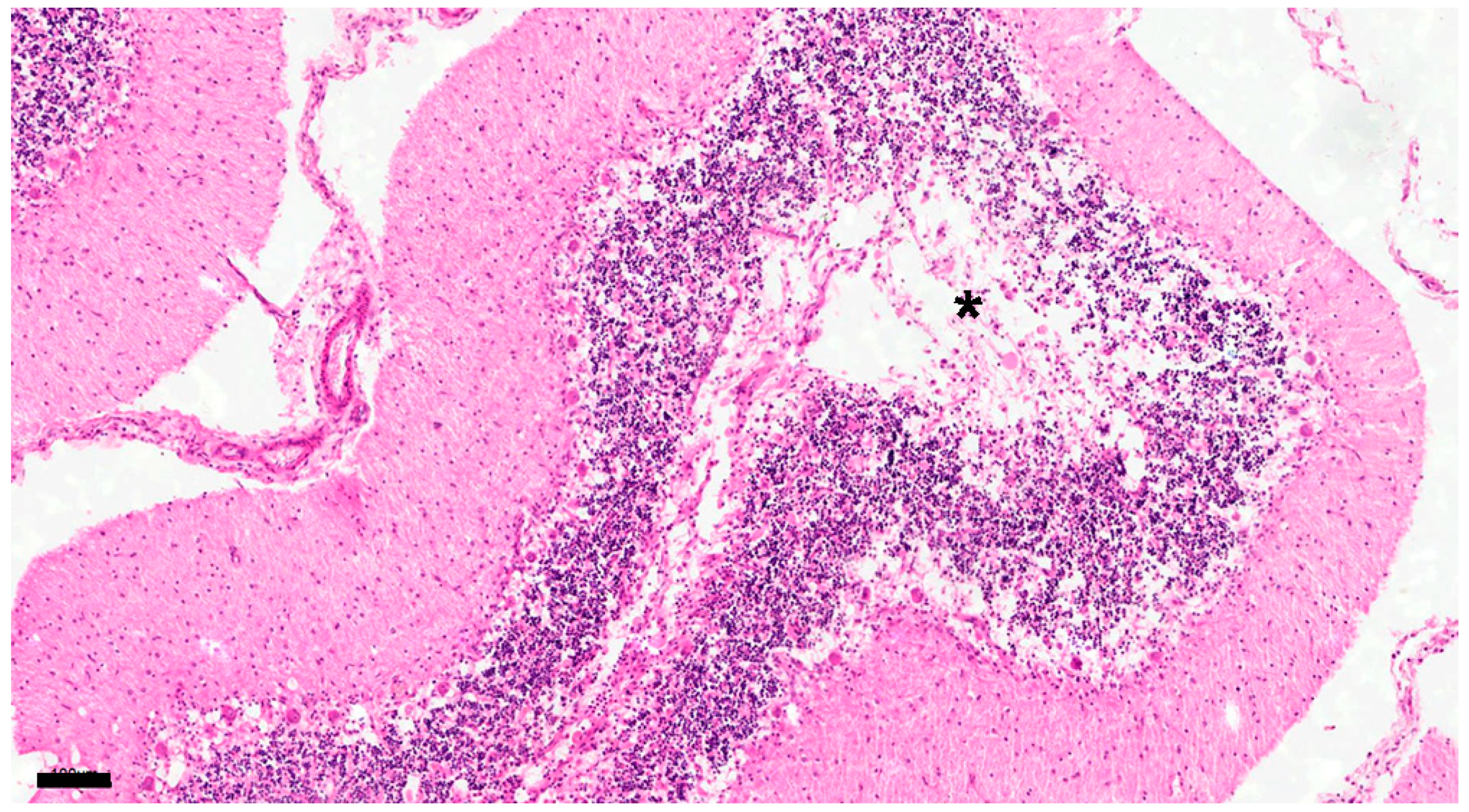
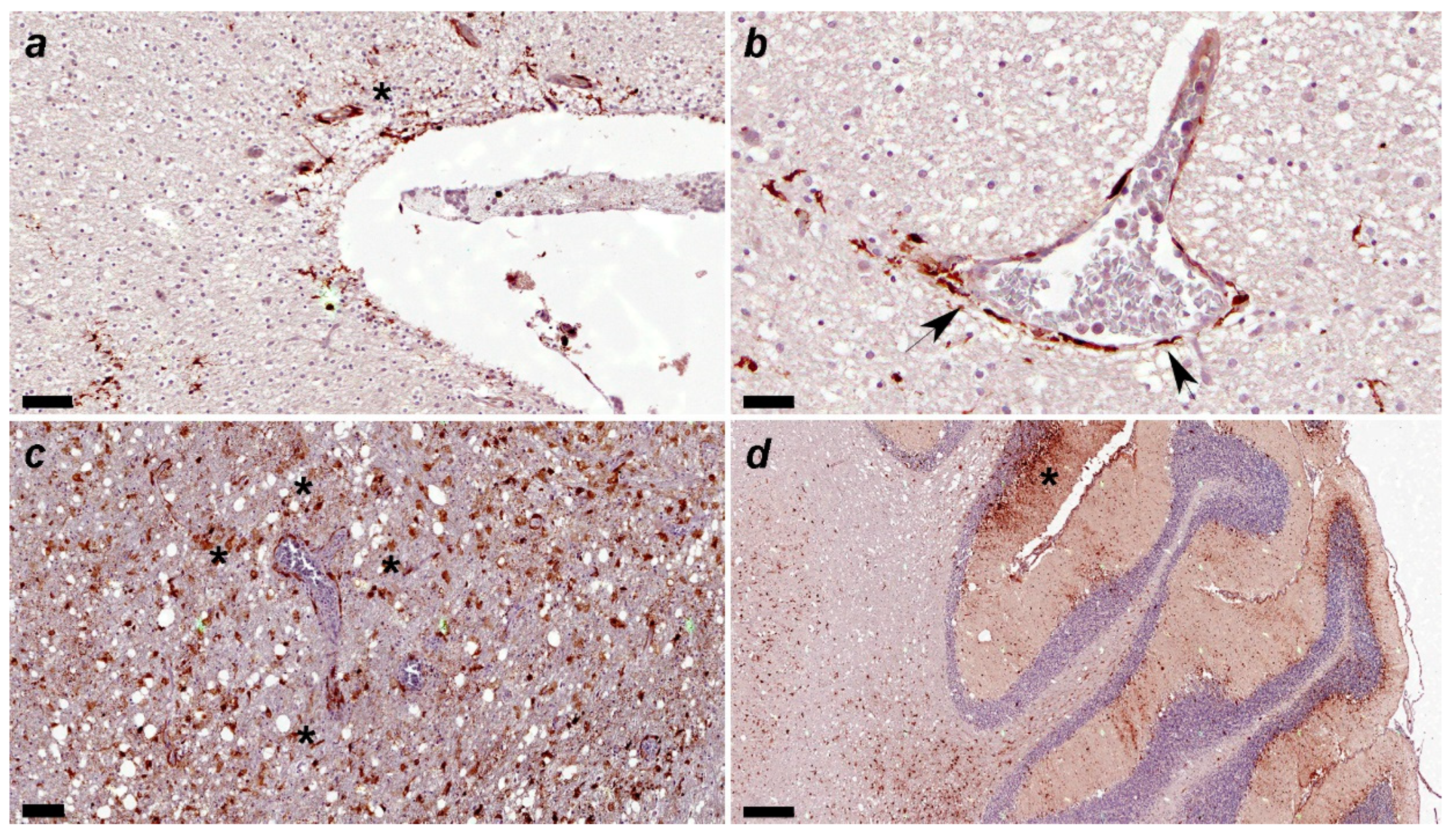
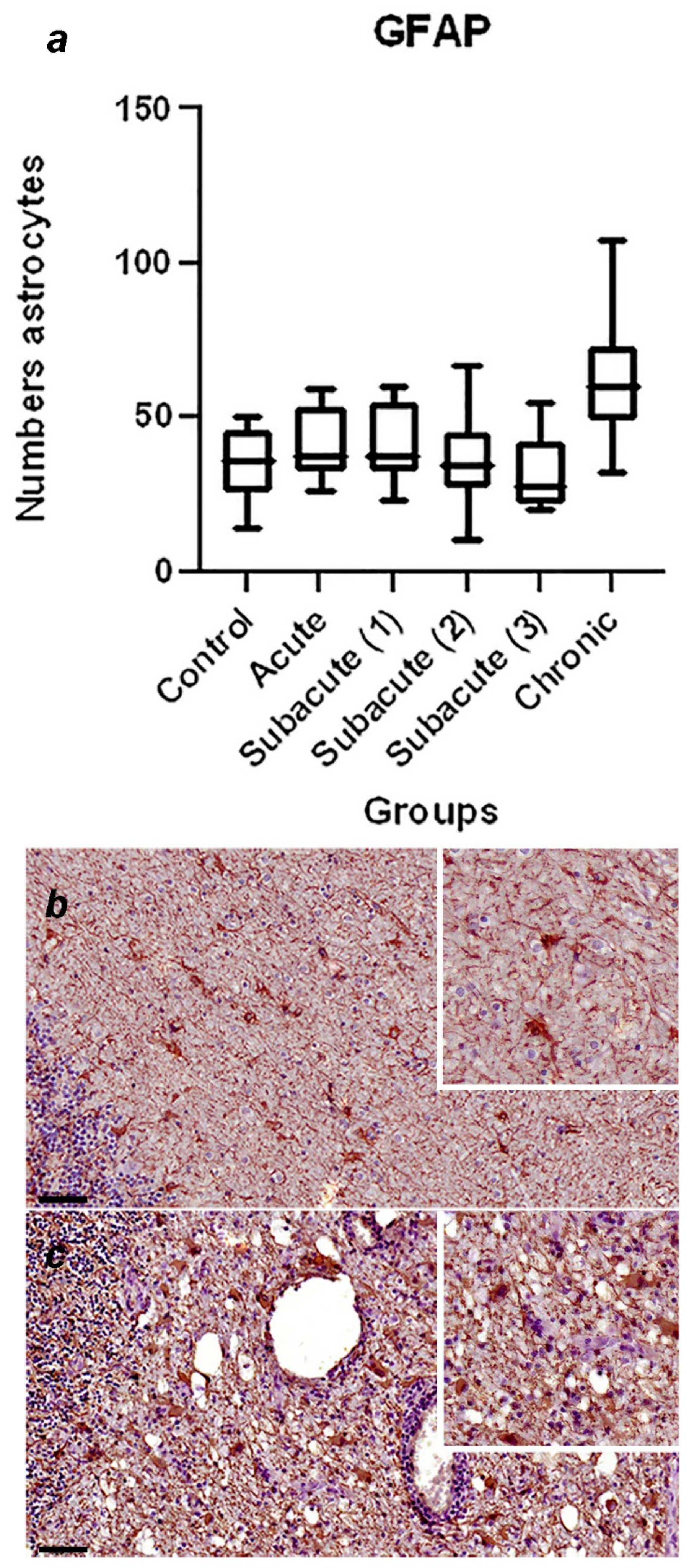
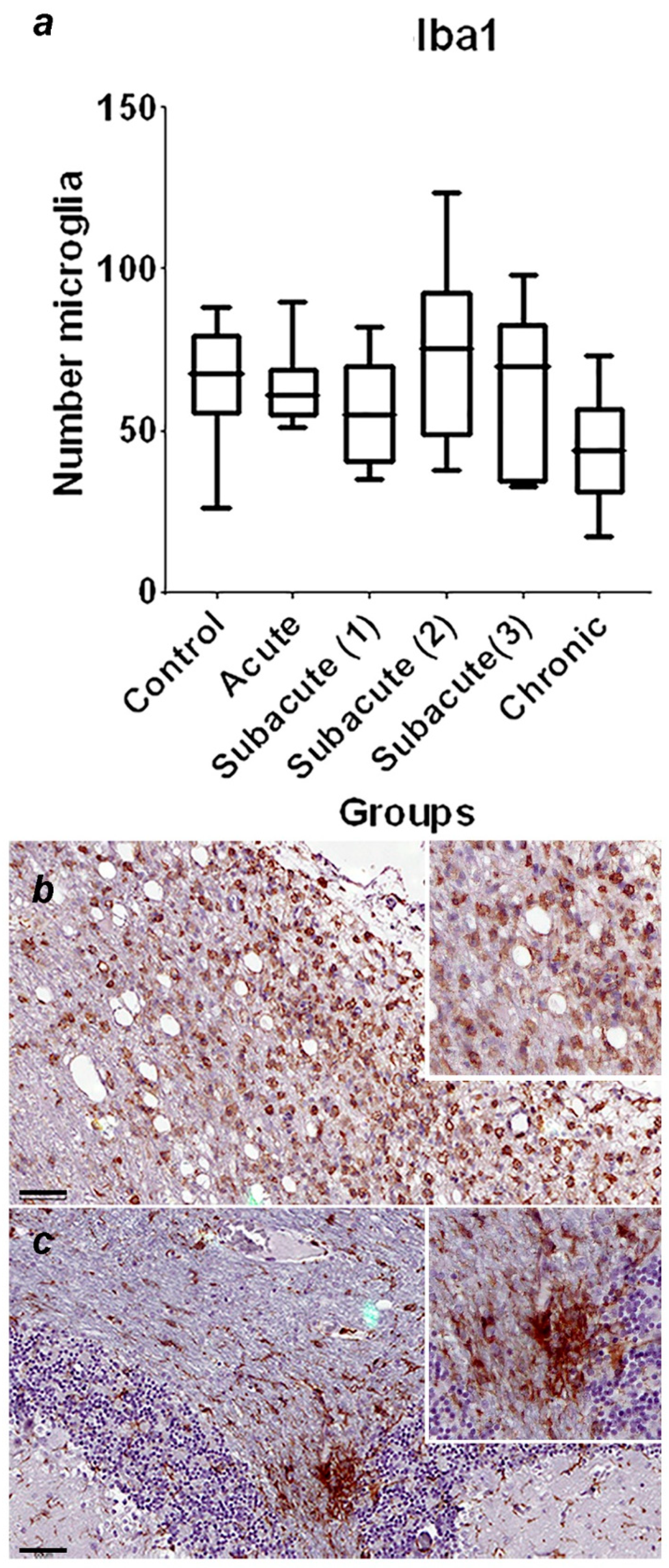
3.2. Histopathological and Immunohistochemical Findings
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Acknowledgments
Conflicts of Interest
References
- Carvalho, O.V.; Botelho, C.V.; Ferreira, C.G.T.; Scherer, P.O.; Soares-Martins, J.A.P.; Almeida, M.R.; Júnior, A.S. Immunopathogenic and neurological mechanisms of canine distemper virus. Adv Virol 2012, 163860. [Google Scholar] [CrossRef]
- Klemens, J.; Ciurkiewicz, M.; Chludzinski, E.; Iseringhausen, M.; Klotz, D.; Pfankuche, V.M.; Ulrich, R.; Herder, V.; Puff, C.; Baumgärtner, W.; Beineke, A. Neurotoxic potential of reactive astrocytes in canine distemper demyelinating leukoencephalitis. Sci Rep 2019, 9, 11689. [Google Scholar] [CrossRef]
- Lempp, C.; Spitzbarth, I.; Puff, C.; Cana, A.; Kegler, K.; Techangamsuwan, S.; Baumgärtner, W.; Seehusen, F. New Aspects of the Pathogenesis of canine distemper leukoencephalitis. Viruses 2014, 6, 2571–2601. [Google Scholar] [CrossRef]
- Pan, Y.; Liu, X.Y. , Meng, L. P.; Zhu, G.R.; Xia, Y.K.; Chen, J.S; Yoshikawa, T. Pathogenesis of demyelinating encephalopathy in dogs with spontaneous acute canine distemper. J Integr Agric 2013, 12, 334–343. [Google Scholar]
- Vandevelde, M.; Zurbriggen, A. Demyelination in canine distemper virus infection: A review. Acta Neuropathol 2005, 109, 56–68. [Google Scholar] [CrossRef]
- De Nardo, T.F.S.; Bertolo, P.H.L.; Bernardes, P.A.; Munari, D.P.; Machado, G.F.; Jardim, L.S.; Moreira, P.R.R.; Rosolem, M.C.; Vasconcelos, R.O. Contribution of astrocytes and macrophage migration inhibitory factor to immune-mediated canine encephalitis caused by the distemper virus. Vet Immunol Immunopathol 2020, 221, 110010.
- Zurbriggen, A.; Schmid, I.; Graber, H.U.; Vandevelde, M. Oligodendroglial pathology in canine distemper. Acta Neuropathol 1998, 95, 71–77. [Google Scholar] [CrossRef]
- Silva, M.C.; Fighera, R.A.; Mazzanti, A. Neuropatologia da cinomose canina: 70 casos (2005-2008). Pesq Vet Bras 2009, 29, 643–652. [Google Scholar] [CrossRef]
- Kabakci, N.; Yarim, M.; Karahan, S.; Guvenc, T.; Yagci, B.B.; Gurcan, I.S. Immunohistochemical investigation of cerebellum in dogs infected with canine distemper virus. Acta Veterinaria Hungarica 2004, 52, 327–337. [Google Scholar] [CrossRef]
- Ulrich, R.; Puff, C.; Wewetzer, K.; Kalkuhl, A.; Deschl, U.; Baumgärtner, W. Transcriptional changes in canine distemper virus-induced demyelinating leukoencephalitis favor a biphasic mode of demyelination. PLOS One 2014, 9, e95917. [Google Scholar] [CrossRef]
- Vandevelde, M.; Fankhauser, R.; Kristensen, F.; Kristensen, B. Immunoglobulins in demyelinating lesions in canine distemper encephalitis. An immunohistological study. Acta Neuropathol 1981, 54, 31–41. [Google Scholar] [CrossRef]
- Bathen-Noethen, A.; Stein, V.M.; Puff, C.; Baumgärtner, W.; Tipold, A. Magnetic resonance imaging findings in acute canine distemper virus infection. J Small Anim Pract 2008, 49, 460–467. [Google Scholar] [CrossRef]
- Beineke, A.; Puff, C.; Seehusen, F.; Baumgärtner, W. Pathogenesis and immunopathology of systemic and nervous canine distemper. Vet Immunol Immunopathol 2009, 127, 1–18. [Google Scholar] [CrossRef]
- Alldinger, S.; Fonfara, S.; Kremmer, E.; Baumgärtner, W. Up-regulation of the hyaluronate receptor CD44 in canine distemper demyelinated plaques. Acta Neuropathol 2000, 99, 138–146. [Google Scholar] [CrossRef]
- Gröters, S.; Alldinger, S.; Baumgärtner, W. Up-regulation of mRNA for matrix metalloproteinases-9 and -14 in advanced lesions of demyelinating canine distemper leukoencephalitis. Acta Neuropathol 2005, 110, 369–382. [Google Scholar] [CrossRef]
- Spitzbarth, I.; Lempp, C.; Kegler, K.; Ulrich, R.; Kalkuhl, A.; Deschl, U.; Baumgärtner, W.; Seehusen, F. Immunohistochemical and transcriptome analyses indicate complex breakdown of axonal transport mechanisms in canine distemper leukoencephalitis. Brain Behav 2016, 3, e00472. [Google Scholar] [CrossRef]
- Rudd, P.A.; Bastien-Hamel, L.E.; von Messling, V. Acute canine distemper encephalitis is associated with rapid neuronal loss and local immune activation. J Gen Virol 2010, 91, 980–989. [Google Scholar] [CrossRef]
- Feijoó, G. ; Yamasaki. K.; Delucchi, L.; Verdes, J.M. Central nervous system lesions caused by canine distemper virus in 4 vaccinated dogs. J Vet Diagn Invest 2021, 33, 640–647. [Google Scholar]
- Summers, B.A.; Greisen, H.A.; Appel, M.J. Early events in canine distemper demyelinating encephalomyelitis. Acta Neuropathol 1979, 46, 1–10. [Google Scholar] [CrossRef]
- Thomas, W.B.; Sorjonen, D.C.; Steiss, J.E. A retrospective evaluation of 38 cases of canine distemper encephalomyelitis. J Am Anim Hosp Associ 1993, 29, 129–133. [Google Scholar]
- Verdes, J.M; Larrañaga, C.; Varela, B.; Iribarnegaray, V.; Yozzi, V.; Feijóo, G.; Yamasaki, K. Histopathological analysis of brains from dogs infected with canine distemper virus. In: Ma D. y Pfaller, CK. Eds. Measles and Related Morbilliviruses: Methods and Protocols. Springer Nature. New York, USA, 2024, Volume 2808, Chapter 14, pp. 177-195.
- Fairley, R.A.; Knesl, O.; Pesavento, P.A.; Elias, B.C. Post-vaccinal distemper encephalitis in two Border Collie cross littermates. N Z Vet J 2015, 63, 117–20. [Google Scholar] [CrossRef]
- Verdes, J.M.; de Sant’Ana, F.J.F.; Sabalsagaray, M.J.; Okada, K.; Calliari, A.; Moraña, J.A.; de Barros, C.S.L. Calbindin D28k distribution in neurons and reactive gliosis in cerebellar cortex of natural rabies virus-infected cattle. J Vet Diagn Invest 2016, 28, 361–8. [Google Scholar] [CrossRef]
- Seehusen, F.; Orlando, E.A.; Wewetzer, K.; Baumgärtner, W. Vimentin-positive astrocytes in canine distemper: a target for canine distemper virus especially in chronic demyelinating lesions? Acta Neuropathol 2007, 114, 597–608. [Google Scholar] [CrossRef]
- Mutinelli, F.; Vandevelde, M.; Griot, C.; Richard, A. Astrocytic infection in canine distemper virus-induced demyelination. Acta Neuropathol 1989, 77, 333–335. [Google Scholar] [CrossRef]
- Summers, B.A.; Appel, M.J. Demyelination in canine distemper encephalomyelitis: an ultrastructural analysis. J Neurocytol 1987, 16, 871–881. [Google Scholar] [CrossRef]
- Correale, J.; Farez, M.F. The Role of Astrocytes in multiple sclerosis progression. Front Neurol 2015, 6, 180. [Google Scholar] [CrossRef]
- Baumgärtner, W.; Orvell, C.; Reinacher, M. Naturally occurring canine distemper virus encephalitis: distribution and expression of viral polypeptides in nervous tissues. Acta Neuropathol 1989, 78, 504–512. [Google Scholar] [CrossRef]
- Koutinas, A.F.; et al. Relation of clinical sings to pathological changes in 19 cases of canine distemper encephalomyelitis. J Comp Pathol 2002, 126, 47–56. [Google Scholar] [CrossRef]
- Muller, C.F.; Fatzer, R.S.; Beck, K.; Vandevelde, M.; Zurbriggen, A. Studies on canine distemper virus persistence in the central nervous system. Acta Neuropathol 1995, 89, 438–445. [Google Scholar] [CrossRef]
- Axthelm, M.K.; Krakowka, S. Canine distemper virus: the early blood-brain barrier lesion. Acta Neuropathol 1987, 75, 27–33. [Google Scholar] [CrossRef]
- Frisk, A.L.; König, M.; Moritz, A.; Baumgärtner, W. Detection of canine distemper virus nucleoprotein RNA by reverse transcription-PCR using serum, whole blood, and cerebrospinal fluid from dogs with distemper. J Clin Microbiol 1999, 37, 3634–3643. [Google Scholar] [CrossRef]
- Higgins, R.J.; Krakowka, S.G.; Metzler, A.E.; Koestner, A. Primary demyelination in experimental canine distemper virus induced encephalomyelitis in gnotobiotic dogs. Sequential immunologic and morphologic findings. Acta Neuropathol 1982, 58, 1–8. [Google Scholar] [CrossRef]
- Rudd, P.A.; Cattaneo, R.; von Messling, V. Canine distemper virus uses both the anterograde and the hematogenous pathway for neuroinvasion. J Virol 2006, 80, 9361–9370. [Google Scholar] [CrossRef]
- Summers, B.A.; Greisen, H.A.; Appel, M.J. Canine distemper encephalomyelitis: variation with virus strain. J Comp Pathol 1984, 94, 65–75. [Google Scholar] [CrossRef]
- Wünschmann A, Lopez-Astacio, R. ; Armién, A.G.; Reed, L.; Parrish, C.R. Parvovirus-induced encephalitis in a juvenile raccoon. J Vet Diagn Invest 2021, 33, 140–143.
- Potgieter, L.N.; Patton, CS. Multifocal cerebellar cortical necrosis caused by canine distemper virus infection in a raccoon. J Am Vet Med Assoc 1984, 185, 1397–1399. [Google Scholar]
- Dudd, P.A.; Bastien-Hamel, L.E.; von Messling, V. Acute canine distemper encephalitis is associated with rapid neuronal loss and local immune activation. J Gen Virol 2010, 91, 980–989. [Google Scholar]
- Vandevelde, M.; Zurbriggen, A. The neurobiology of canine distemper virus infection. Vet Microbiol 1995, 44, 271–280. [Google Scholar] [CrossRef]
| Primary Antibody | Source | Dilution | Species / type | Detection system |
|---|---|---|---|---|
| MCA 1893 Canine Distemper Virus |
Biorad | 1:250 | Mouse / monoclonal | Mouse on canine HRP-Polymer |
| Glial Fibrillary Protein (GFAP) | Biocare Medical | RTU* | Mouse / monoclonal | MACH 4 Universal HRP-Polymer |
| Anti-Iba1 (ab5076) | Abcam | 1:1000 | Goat / polyclonal | Rabbit Anti-Goat IgG H&L (HRP) ab6741 |
| Calbindin (orb5912) | Biorbyt | 1:200 | Rabbit / polyclonal | MACH 4 Universal HRP-Polymer |
| Groups | Number of animals | Average month age (range) |
Histopathological findings |
|---|---|---|---|
| Control | 5 | (45 days old – 6 years old) | No changes |
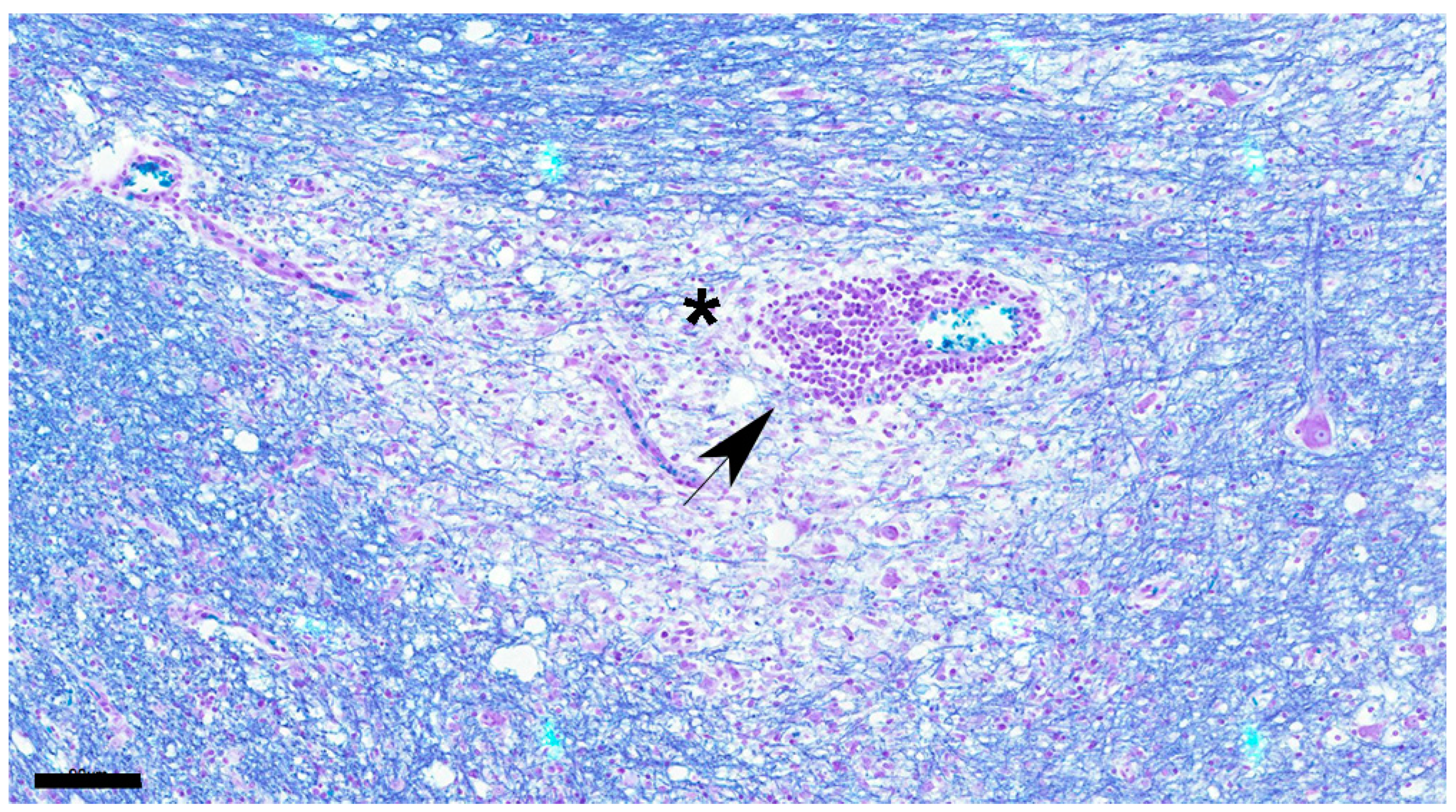
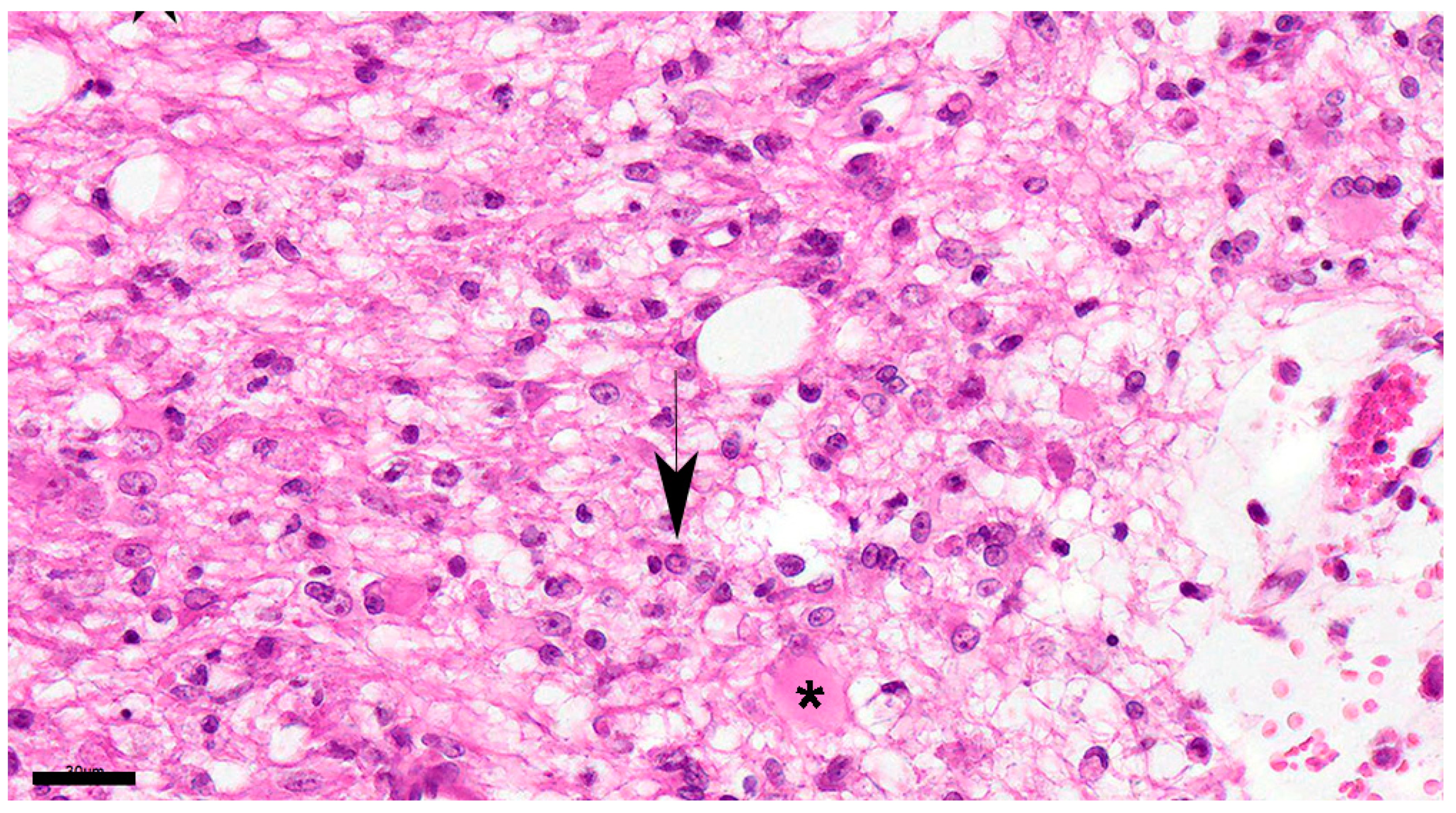
| Acute | 4 | (25 days old – 3 years old) | glial cell reaction, inclusion bodies, CDV immunoreactive particles, meningitis |
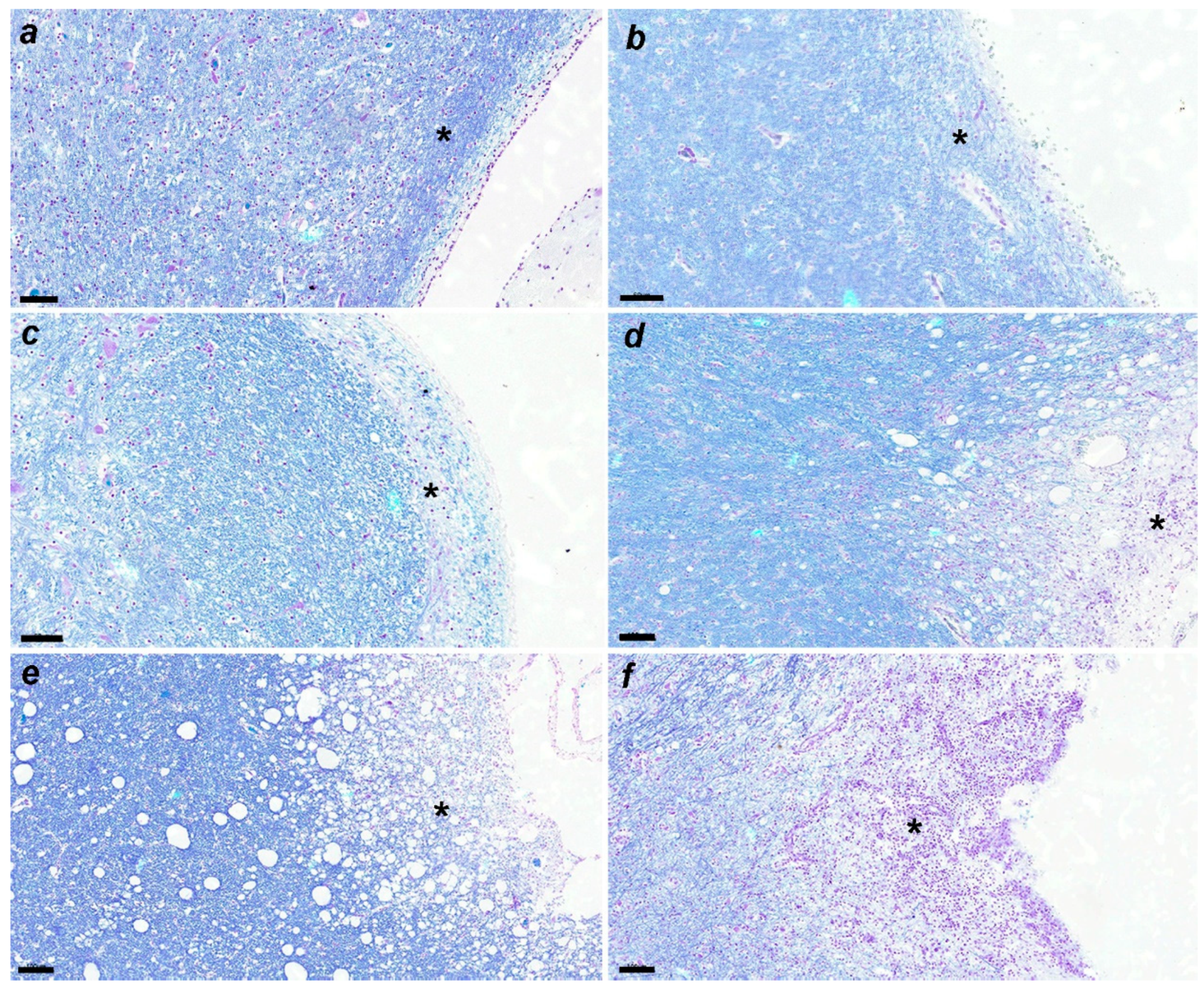
| Subacute 1 | 4 | (30 days old – 3 years old) | demyelination, glial cell reaction, inclusion bodies, CDV immunoreactive particles, meningitis |
| Subacute 2 | 9 | (2 months old – 10 years old) | demyelination, glial cell reaction, inclusion bodies, CDV immunoreactive particles, meningitis, mild decreased granular layer cells and Purkinje cells |
| Subacute 3 | 5 | (3 months old – 3 years old) | demyelination, glial cell reaction, inclusion bodies, CDV immunoreactive particles, meningitis, moderate decreased granular layer cells and Purkinje cells |
| Chronic | 6 | (3 months old – 3 years old) | demyelination, gliosis, glial cell reaction, inclusion bodies, CDV immunoreactive particles, meningitis, severe decreased granular layer cells and Purkinje cells |
| Groups | Number of animals | Average month age (range) |
Numbers | ||
|---|---|---|---|---|---|
| astrocytes | microglias | Purkinje cells | |||
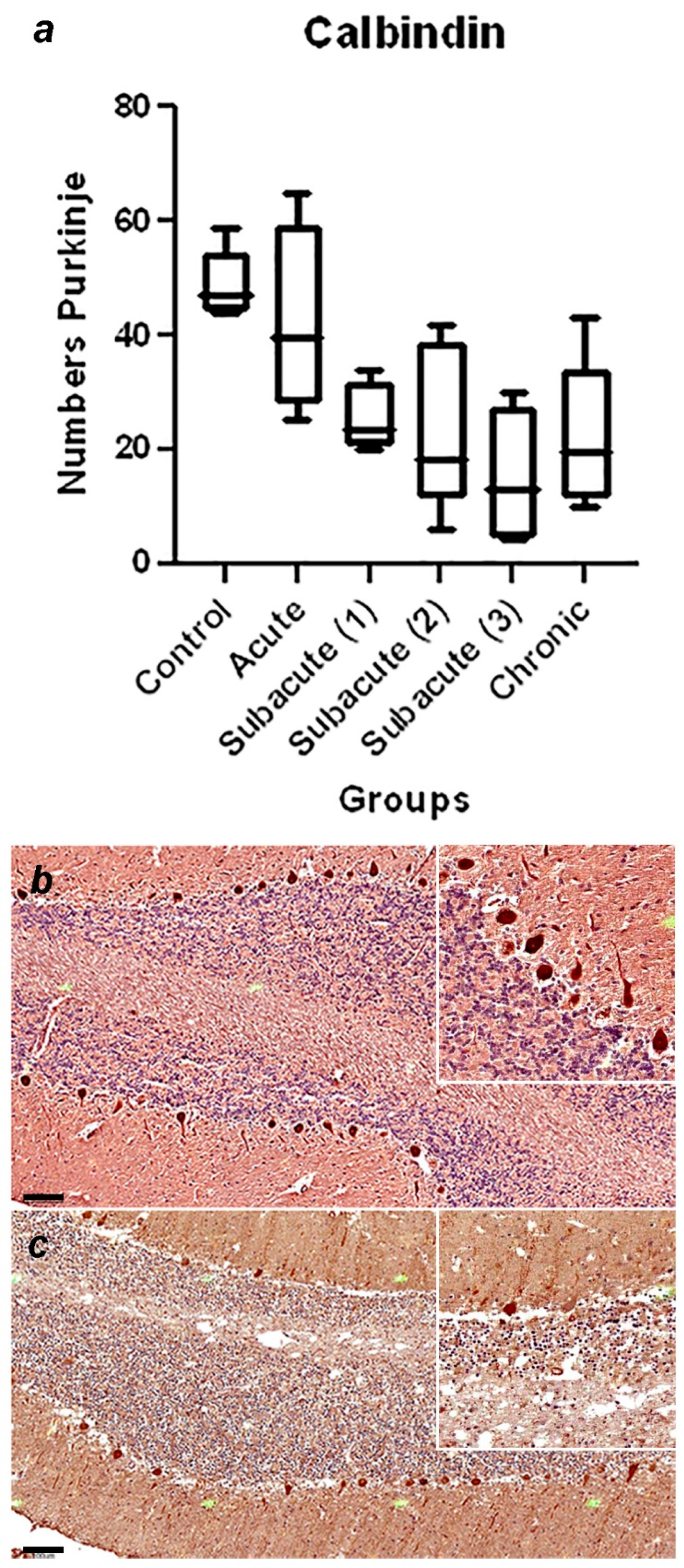
| Control | 5 | (45 days old – 6 years old) | 35 ± 11a | 64 ± 19 | 49 ± 6a |
| Acute | 4 | (25 days old – 3 years old) | 41 ± 12 | 64 ± 13 | 42 ± 17 |
| Subacute 1 | 4 | (30 days old – 3 years old) | 42 ± 13 | 56 ± 16 | 25 ± 6 |
| Subacute 2 | 9 | (2 months old – 10 years old) | 36 ± 13 | 75 ± 26 | 24 ± 14b |
| Subacute 3 | 5 | (3 months old – 3 years old) | 32 ± 12 | 63 ± 26 | 15 ± 12c |
| Chronic | 6 | (3 months old – 3 years old) | 63 ± 22b | 44 ± 17 | 23 ± 13d |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





