Submitted:
27 September 2024
Posted:
30 September 2024
You are already at the latest version
Abstract
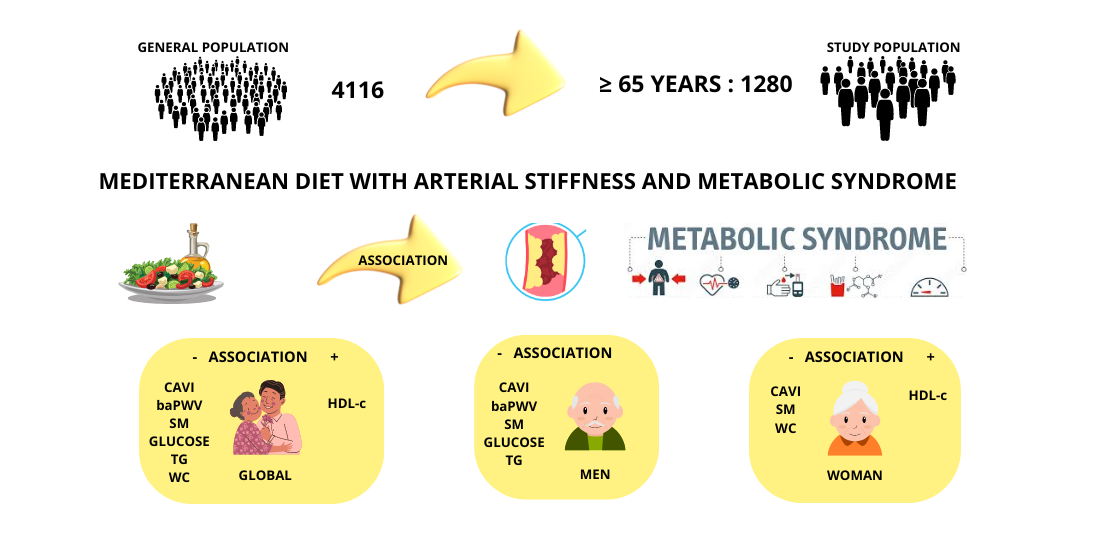
Keywords:
1. Introduction
2. Materials and Methods
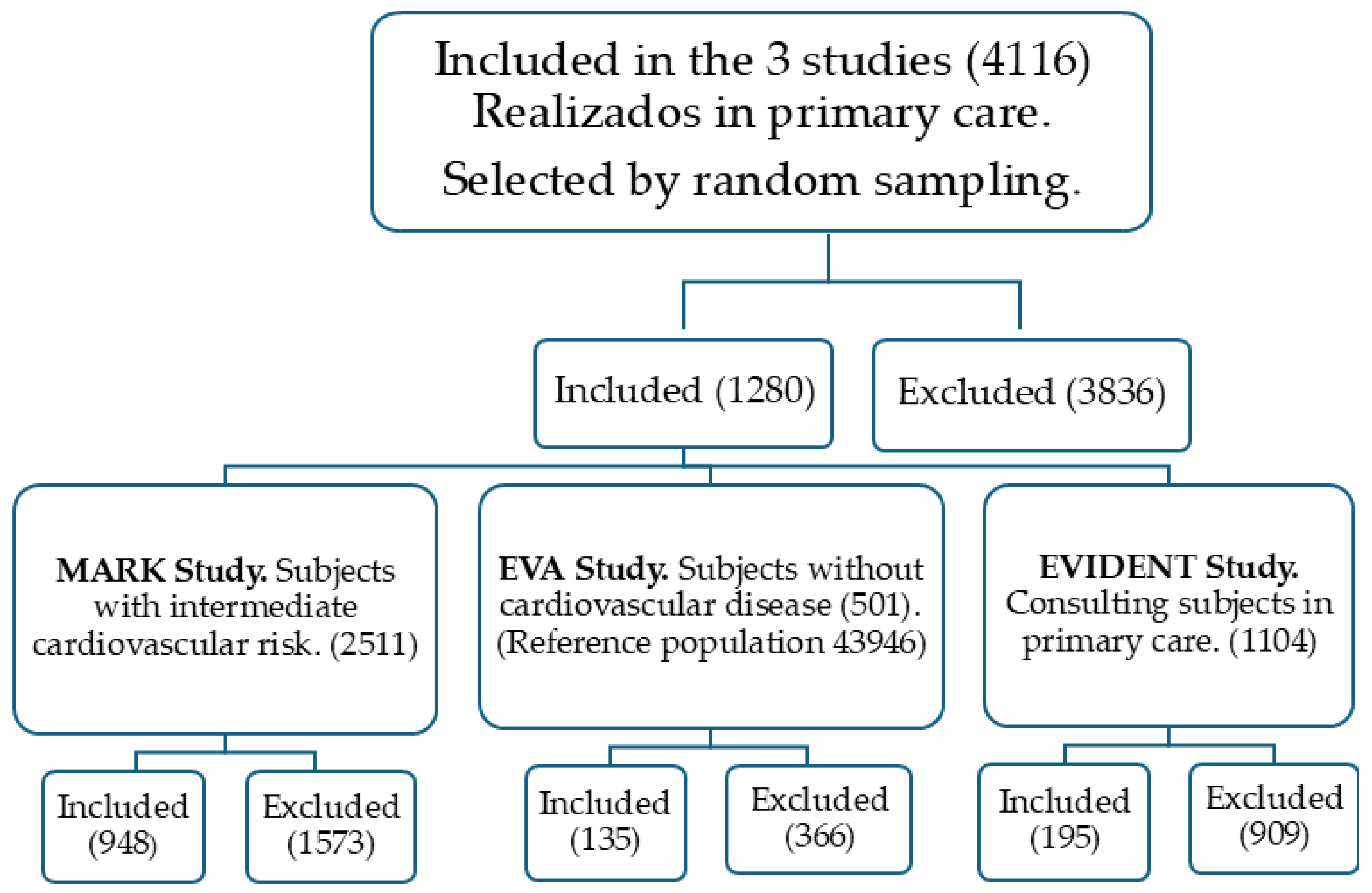
2.1. Type of Study
2.2. Study Population
2.3. Ethics Committee and Participant Consent
2.4. Variables and Measurement Methods
2.4.1. Mediterranean Diet
2.4.2. Metabolic Syndrome
2.4.3. Arterial Stiffness
2.4.4. Cardiovascular Risk Factors
2.5. Statistical Analysis
3. Results
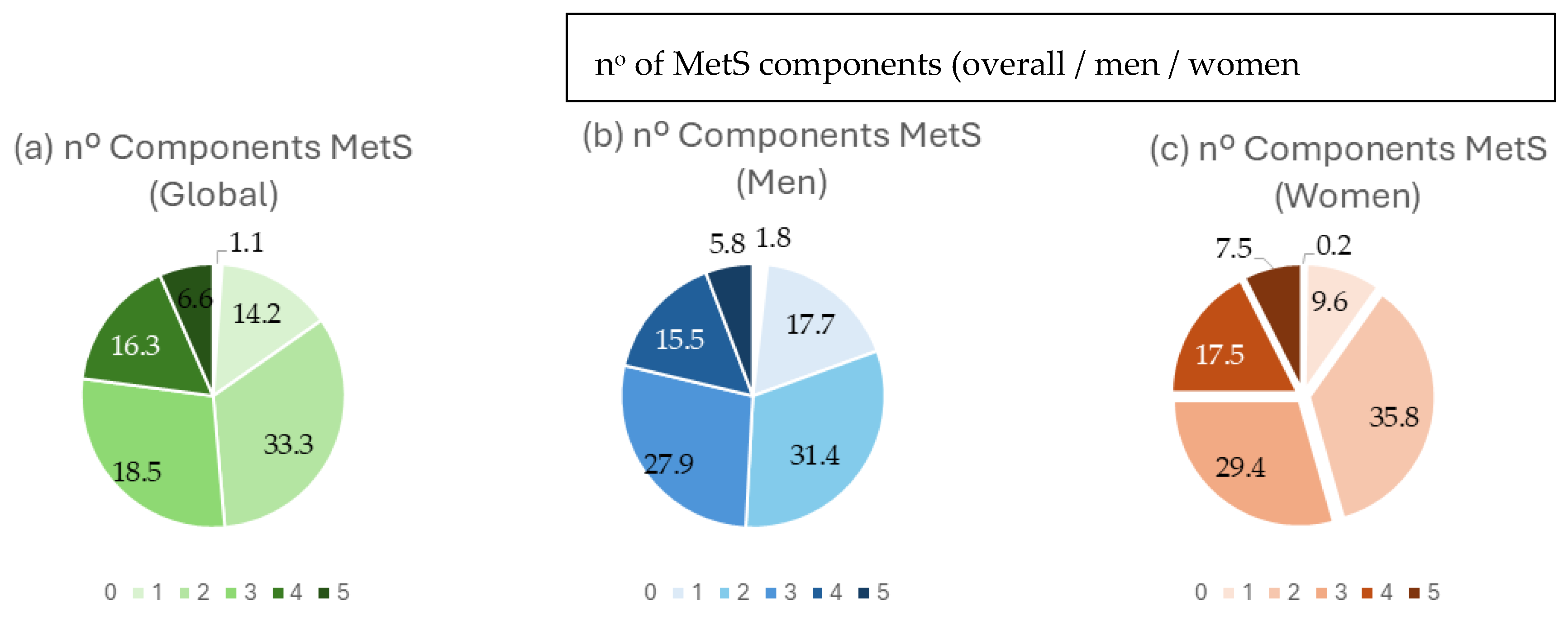
3.1. Participant Characteristics
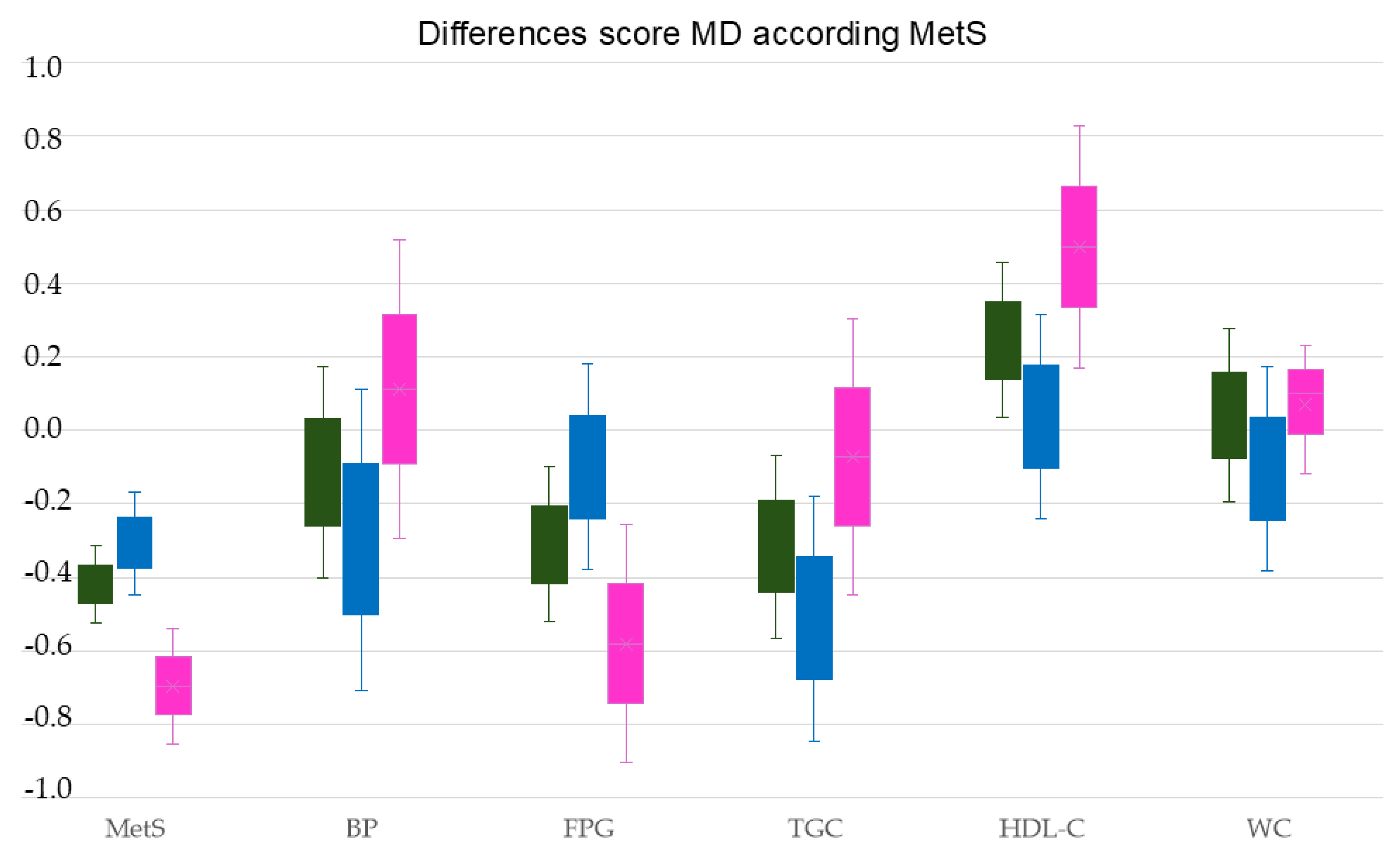
3.2. Association between the Mediterranean Diet and Arterial Stiffness and MetS in People over 65 Years of Age
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Rodríguez-Mañas, L.; Moreno-Villares, J.M.; Álvarez Hernández, J.; Romero Secín, A.A.; López Díaz-Ufano, M.L.; Suárez González, F.; Costa-Grille, A.; López-Miranda, J.; Fernández-Garcia, J.M. Awareness and Self-Reported Knowledge and Training on Nutrition in Older People among Primary Care Practitioners. J Frailty Aging 2024, 13, 157–162. [Google Scholar] [CrossRef] [PubMed]
- Chin, S.; Wong, R.; Hirani, V.; O'Leary, F. Nutrition knowledge assessment tools for older adults and their carers: a scoping review. Nutr Res Rev 2023, 36, 216–231. [Google Scholar] [CrossRef] [PubMed]
- Guo, J.; Schupf, N.; Cruz, E.; Stern, Y.; Mayeux, R.P.; Gu, Y. Association Between Mediterranean Diet and Functional Status in Older Adults: A Longitudinal Study Based on the Washington Heights-Inwood Columbia Aging Project. J Gerontol A Biol Sci Med Sci 2022, 77, 1873–1881. [Google Scholar] [CrossRef] [PubMed]
- Coelho-Júnior, H.J.; Trichopoulou, A.; Panza, F. Cross-sectional and longitudinal associations between adherence to Mediterranean diet with physical performance and cognitive function in older adults: A systematic review and meta-analysis. Ageing Res Rev 2021, 70, 101395. [Google Scholar] [CrossRef]
- Apostolaki, I.; Pepa, A.; Vlassopoulos, A.; Kapsokefalou, M. Social Capital and Self-Perceived Quality of Life-Interrelated Predictors of Mediterranean Diet Adherence in Older Adults. Nutrients 2021, 13. [Google Scholar] [CrossRef]
- Zaragoza-Martí, A.; Ferrer-Cascales, R.; Hurtado-Sánchez, J.A.; Laguna-Pérez, A.; Cabañero-Martínez, M.J. Relationship between Adherence to the Mediterranean Diet and Health-Related Quality of Life and Life Satisfaction among Older Adults. J Nutr Health Aging 2018, 22, 89–96. [Google Scholar] [CrossRef]
- Román, G.C.; Jackson, R.E.; Reis, J.; Román, A.N.; Toledo, J.B.; Toledo, E. Extra-virgin olive oil for potential prevention of Alzheimer disease. Rev Neurol (Paris) 2019, 175, 705–723. [Google Scholar] [CrossRef]
- Kiani, A.K.; Medori, M.C.; Bonetti, G.; Aquilanti, B.; Velluti, V.; Matera, G.; Iaconelli, A.; Stuppia, L.; Connelly, S.T.; Herbst, K.L. , et al. Modern vision of the Mediterranean diet. J Prev Med Hyg 2022, 63, E36–e43. [Google Scholar] [CrossRef]
- Trichopoulou, A.; Martinez-Gonzalez, M.A.; Tong, T.Y.; Forouhi, N.G.; Khandelwal, S.; Prabhakaran, D.; Mozaffarian, D.; de Lorgeril, M. Definitions and potential health benefits of the Mediterranean diet: views from experts around the world. BMC Med 2014, 12, 112. [Google Scholar] [CrossRef]
- Martini, D. Health Benefits of Mediterranean Diet. Nutrients 2019, 11. [Google Scholar] [CrossRef]
- Rees, K.; Takeda, A.; Martin, N.; Ellis, L.; Wijesekara, D.; Vepa, A.; Das, A.; Hartley, L.; Stranges, S. Mediterranean-style diet for the primary and secondary prevention of cardiovascular disease. Cochrane Database Syst Rev 2019, 3, Cd009825. [Google Scholar] [CrossRef]
- Dominguez, L.J.; Di Bella, G.; Veronese, N.; Barbagallo, M. Impact of Mediterranean Diet on Chronic Non-Communicable Diseases and Longevity. Nutrients 2021, 13. [Google Scholar] [CrossRef] [PubMed]
- Andreo-López, M.C.; Contreras-Bolívar, V.; Muñoz-Torres, M.; García-Fontana, B.; García-Fontana, C. Influence of the Mediterranean Diet on Healthy Aging. Int J Mol Sci 2023, 24. [Google Scholar] [CrossRef] [PubMed]
- Mazza, E.; Ferro, Y.; Pujia, R.; Mare, R.; Maurotti, S.; Montalcini, T.; Pujia, A. Mediterranean Diet In Healthy Aging. J Nutr Health Aging 2021, 25, 1076–1083. [Google Scholar] [CrossRef] [PubMed]
- Papadopoulou, S.K.; Detopoulou, P.; Voulgaridou, G.; Tsoumana, D.; Spanoudaki, M.; Sadikou, F.; Papadopoulou, V.G.; Zidrou, C.; Chatziprodromidou, I.P.; Giaginis, C. , et al. Mediterranean Diet and Sarcopenia Features in Apparently Healthy Adults over 65 Years: A Systematic Review. Nutrients 2023, 15. [Google Scholar] [CrossRef]
- Rudzińska, A.; Perera, I.; Gryglewska, B.; Gąsowski, J.; Piotrowicz, K. Can the Mediterranean diet decrease the risk of depression in older persons - a systematic review. Psychiatr Pol 2023, 57, 339–354. [Google Scholar] [CrossRef]
- Wermers, J. Mediterranean-style diet for the primary and secondary prevention of cardiovascular disease: Summary of a Cochrane review. Explore (NY) 2020, 16, 201–202. [Google Scholar] [CrossRef]
- Estruch, R.; Ros, E.; Salas-Salvadó, J.; Covas, M.I.; Corella, D.; Arós, F.; Gómez-Gracia, E.; Ruiz-Gutiérrez, V.; Fiol, M.; Lapetra, J. , et al. Primary Prevention of Cardiovascular Disease with a Mediterranean Diet Supplemented with Extra-Virgin Olive Oil or Nuts. N Engl J Med 2018, 378, e34. [Google Scholar] [CrossRef]
- Rees, K.; Takeda, A.; Martin, N.; Ellis, L.; Wijesekara, D.; Vepa, A.; Das, A.; Hartley, L.; Stranges, S. Mediterranean-Style Diet for the Primary and Secondary Prevention of Cardiovascular Disease: A Cochrane Review. Glob Heart 2020, 15, 56. [Google Scholar] [CrossRef]
- Cabré, J.J.; Barrio, F.; Vizcaíno, J.; Martínez, A.; Mur, T.; Sagarra, R.; Dalmau, S. Results of the implementation of the DP-TRANSFERS project in Catalonia: A translational method to improve diabetes screening and prevention in primary care. Rev Clin Esp (Barc) 2024. [Google Scholar] [CrossRef]
- Jennings, A.; Berendsen, A.M.; de Groot, L.; Feskens, E.J.M.; Brzozowska, A.; Sicinska, E.; Pietruszka, B.; Meunier, N.; Caumon, E.; Malpuech-Brugère, C. , et al. Mediterranean-Style Diet Improves Systolic Blood Pressure and Arterial Stiffness in Older Adults. Hypertension 2019, 73, 578–586. [Google Scholar] [CrossRef] [PubMed]
- Dominguez, L.J.; Veronese, N.; Di Bella, G.; Cusumano, C.; Parisi, A.; Tagliaferri, F.; Ciriminna, S.; Barbagallo, M. Mediterranean diet in the management and prevention of obesity. Exp Gerontol 2023, 174, 112121. [Google Scholar] [CrossRef] [PubMed]
- Tuttolomondo, A.; Simonetta, I.; Daidone, M.; Mogavero, A.; Ortello, A.; Pinto, A. Metabolic and Vascular Effect of the Mediterranean Diet. Int J Mol Sci 2019, 20. [Google Scholar] [CrossRef] [PubMed]
- van den Brink, A.C.; Brouwer-Brolsma, E.M.; Berendsen, A.A.M.; van de Rest, O. The Mediterranean, Dietary Approaches to Stop Hypertension (DASH), and Mediterranean-DASH Intervention for Neurodegenerative Delay (MIND) Diets Are Associated with Less Cognitive Decline and a Lower Risk of Alzheimer's Disease-A Review. Adv Nutr 2019, 10, 1040–1065. [Google Scholar] [CrossRef] [PubMed]
- Mentella, M.C.; Scaldaferri, F.; Ricci, C.; Gasbarrini, A.; Miggiano, G.A.D. Cancer and Mediterranean Diet: A Review. Nutrients 2019, 11. [Google Scholar] [CrossRef]
- Georgoulis, M.; Damigou, E.; Chrysohoou, C.; Barkas, F.; Anastasiou, G.; Kravvariti, E.; Tsioufis, C.; Liberopoulos, E.; Sfikakis, P.P.; Pitsavos, C. , et al. Mediterranean diet trajectories and 20-year incidence of cardiovascular disease: The ATTICA cohort study (2002-2022). Nutr Metab Cardiovasc Dis 2024, 34, 153–166. [Google Scholar] [CrossRef]
- Tanaka, T.; Talegawkar, S.A.; Jin, Y.; Bandinelli, S.; Ferrucci, L. Association of Adherence to the Mediterranean-Style Diet with Lower Frailty Index in Older Adults. Nutrients 2021, 13. [Google Scholar] [CrossRef]
- Di Daniele, N.; Noce, A.; Vidiri, M.F.; Moriconi, E.; Marrone, G.; Annicchiarico-Petruzzelli, M.; D'Urso, G.; Tesauro, M.; Rovella, V.; De Lorenzo, A. Impact of Mediterranean diet on metabolic syndrome, cancer and longevity. Oncotarget 2017, 8, 8947–8979. [Google Scholar] [CrossRef]
- Laurent, S.; Boutouyrie, P.; Cunha, P.G.; Lacolley, P.; Nilsson, P.M. Concept of Extremes in Vascular Aging. Hypertension 2019, 74, 218–228. [Google Scholar] [CrossRef]
- Williams, B.; Mancia, G.; Spiering, W.; Agabiti Rosei, E.; Azizi, M.; Burnier, M.; Clement, D.L.; Coca, A.; de Simone, G.; Dominiczak, A. , et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J Hypertens 2018, 36, 1953–2041. [Google Scholar] [CrossRef]
- Visseren, F.L.J.; Mach, F.; Smulders, Y.M.; Carballo, D.; Koskinas, K.C.; Bäck, M.; Benetos, A.; Biffi, A.; Boavida, J.M.; Capodanno, D. , et al. 2021 ESC Guidelines on cardiovascular disease prevention in clinical practice. Eur Heart J 2021, 42, 3227–3337. [Google Scholar] [CrossRef] [PubMed]
- Ohkuma, T.; Ninomiya, T.; Tomiyama, H.; Kario, K.; Hoshide, S.; Kita, Y.; Inoguchi, T.; Maeda, Y.; Kohara, K.; Tabara, Y. , et al. Brachial-Ankle Pulse Wave Velocity and the Risk Prediction of Cardiovascular Disease: An Individual Participant Data Meta-Analysis. Hypertension 2017, 69, 1045–1052. [Google Scholar] [CrossRef] [PubMed]
- Yasuharu, T.; Setoh, K.; Kawaguchi, T.; Nakayama, T.; Matsuda, F. Brachial-ankle pulse wave velocity and cardio-ankle vascular index are associated with future cardiovascular events in a general population: The Nagahama Study. J Clin Hypertens (Greenwich) 2021, 23, 1390–1398. [Google Scholar] [CrossRef] [PubMed]
- Matsushita, K.; Ding, N.; Kim, E.D.; Budoff, M.; Chirinos, J.A.; Fernhall, B.; Hamburg, N.M.; Kario, K.; Miyoshi, T.; Tanaka, H. , et al. Cardio-ankle vascular index and cardiovascular disease: Systematic review and meta-analysis of prospective and cross-sectional studies. J Clin Hypertens (Greenwich) 2019, 21, 16–24. [Google Scholar] [CrossRef]
- Miyoshi, T.; Ito, H.; Shirai, K.; Horinaka, S.; Higaki, J.; Yamamura, S.; Saiki, A.; Takahashi, M.; Masaki, M.; Okura, T. , et al. Predictive Value of the Cardio-Ankle Vascular Index for Cardiovascular Events in Patients at Cardiovascular Risk. J Am Heart Assoc 2021, 10, e020103. [Google Scholar] [CrossRef]
- Liese, A.D.; Couch, S.C.; The, N.S.; Crandell, J.L.; Lawrence, J.M.; Crume, T.L.; Mayer-Davis, E.J.; Zhong, V.W.; Urbina, E.M. Association between diet quality indices and arterial stiffness in youth with type 1 diabetes: SEARCH for Diabetes in Youth Nutrition Ancillary Study. J Diabetes Complications 2020, 34, 107709. [Google Scholar] [CrossRef]
- Alberti, K.G.; Eckel, R.H.; Grundy, S.M.; Zimmet, P.Z.; Cleeman, J.I.; Donato, K.A.; Fruchart, J.C.; James, W.P.; Loria, C.M.; Smith, S.C., Jr. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 2009, 120, 1640–1645. [Google Scholar] [CrossRef]
- Mottillo, S.; Filion, K.B.; Genest, J.; Joseph, L.; Pilote, L.; Poirier, P.; Rinfret, S.; Schiffrin, E.L.; Eisenberg, M.J. The metabolic syndrome and cardiovascular risk a systematic review and meta-analysis. J Am Coll Cardiol 2010, 56, 1113–1132. [Google Scholar] [CrossRef]
- Kotani, K.; Satoh-Asahara, N.; Nakakuki, T.; Yamakage, H.; Shimatsu, A.; Tsukahara, T. Association between metabolic syndrome and multiple lesions of intracranial atherothrombotic stroke: a hospital-based study. Cardiovasc Diabetol 2015, 14, 108. [Google Scholar] [CrossRef] [PubMed]
- Jiang, B.; Li, B.; Wang, Y.; Han, B.; Wang, N.; Li, Q.; Yang, W.; Huang, G.; Wang, J.; Chen, Y. , et al. The nine-year changes of the incidence and characteristics of metabolic syndrome in China: longitudinal comparisons of the two cross-sectional surveys in a newly formed urban community. Cardiovasc Diabetol 2016, 15, 84. [Google Scholar] [CrossRef]
- Saklayen, M.G. The Global Epidemic of the Metabolic Syndrome. Curr Hypertens Rep 2018, 20, 12. [Google Scholar] [CrossRef] [PubMed]
- Cornier, M.A.; Dabelea, D.; Hernandez, T.L.; Lindstrom, R.C.; Steig, A.J.; Stob, N.R.; Van Pelt, R.E.; Wang, H.; Eckel, R.H. The metabolic syndrome. Endocr Rev 2008, 29, 777–822. [Google Scholar] [CrossRef]
- Merchant, R.A.; Chan, Y.H.; Lim, J.Y.; Morley, J.E. Prevalence of Metabolic Syndrome and Association with Grip Strength in Older Adults: Findings from the HOPE Study. Diabetes Metab Syndr Obes 2020, 13, 2677–2686. [Google Scholar] [CrossRef] [PubMed]
- Sotos-Prieto, M.; Ortolá, R.; Ruiz-Canela, M.; Garcia-Esquinas, E.; Martínez-Gómez, D.; Lopez-Garcia, E.; Martínez-González, M.; Rodriguez-Artalejo, F. Association between the Mediterranean lifestyle, metabolic syndrome and mortality: a whole-country cohort in Spain. Cardiovasc Diabetol 2021, 20, 5. [Google Scholar] [CrossRef] [PubMed]
- Gallardo-Alfaro, L.; Bibiloni, M.D.M.; Mascaró, C.M.; Montemayor, S.; Ruiz-Canela, M.; Salas-Salvadó, J.; Corella, D.; Fitó, M.; Romaguera, D.; Vioque, J. , et al. Leisure-Time Physical Activity, Sedentary Behaviour and Diet Quality are Associated with Metabolic Syndrome Severity: The PREDIMED-Plus Study. Nutrients 2020, 12. [Google Scholar] [CrossRef] [PubMed]
- Gomez-Marcos, M.A.; Martinez-Salgado, C.; Gonzalez-Sarmiento, R.; Hernandez-Rivas, J.M.; Sanchez-Fernandez, P.L.; Recio-Rodriguez, J.I.; Rodriguez-Sanchez, E.; García-Ortiz, L. Association between different risk factors and vascular accelerated ageing (EVA study): study protocol for a cross-sectional, descriptive observational study. BMJ Open 2016, 6, e011031. [Google Scholar] [CrossRef]
- Martí, R.; Parramon, D.; García-Ortiz, L.; Rigo, F.; Gómez-Marcos, M.A.; Sempere, I.; García-Regalado, N.; Recio-Rodriguez, J.I.; Agudo-Conde, C.; Feuerbach, N. , et al. Improving interMediAte risk management. MARK study. BMC Cardiovasc Disord 2011, 11, 61. [Google Scholar] [CrossRef]
- Recio-Rodríguez, J.I.; Martín-Cantera, C.; González-Viejo, N.; Gómez-Arranz, A.; Arietaleanizbeascoa, M.S.; Schmolling-Guinovart, Y.; Maderuelo-Fernandez, J.A.; Pérez-Arechaederra, D.; Rodriguez-Sanchez, E.; Gómez-Marcos, M.A. , et al. Effectiveness of a smartphone application for improving healthy lifestyles, a randomized clinical trial (EVIDENT II): study protocol. BMC Public Health 2014, 14, 254. [Google Scholar] [CrossRef]
- World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. Jama 2013, 310, 2191–2194. [CrossRef]
- Schröder, H.; Fitó, M.; Estruch, R.; Martínez-González, M.A.; Corella, D.; Salas-Salvadó, J.; Lamuela-Raventós, R.; Ros, E.; Salaverría, I.; Fiol, M. , et al. A short screener is valid for assessing Mediterranean diet adherence among older Spanish men and women. J Nutr 2011, 141, 1140–1145. [Google Scholar] [CrossRef]
- Shirai, K.; Hiruta, N.; Song, M.; Kurosu, T.; Suzuki, J.; Tomaru, T.; Miyashita, Y.; Saiki, A.; Takahashi, M.; Suzuki, K. , et al. Cardio-ankle vascular index (CAVI) as a novel indicator of arterial stiffness: theory, evidence and perspectives. J Atheroscler Thromb 2011, 18, 924–938. [Google Scholar] [CrossRef] [PubMed]
- Salas-Salvadó, J.; Rubio, M.A.; Barbany, M.; Moreno, B. [SEEDO 2007 Consensus for the evaluation of overweight and obesity and the establishment of therapeutic intervention criteria]. Med Clin (Barc) 2007, 128, 184–196. [Google Scholar] [CrossRef]
- O'Brien, E.; Asmar, R.; Beilin, L.; Imai, Y.; Mancia, G.; Mengden, T.; Myers, M.; Padfield, P.; Palatini, P.; Parati, G. , et al. Practice guidelines of the European Society of Hypertension for clinic, ambulatory and self blood pressure measurement. J Hypertens 2005, 23, 697–701. [Google Scholar] [CrossRef]
- 2013 Practice guidelines for the management of arterial hypertension of the European Society of Hypertension (ESH) and the European Society of Cardiology (ESC): ESH/ESC Task Force for the Management of Arterial Hypertension. J Hypertens 2013, 31, 1925–1938. [CrossRef] [PubMed]
- GómezSánchez, M.; Gómez Sánchez, L.; Patino-Alonso, M.C.; Alonso-Domínguez, R.; Sánchez-Aguadero, N.; Lugones-Sánchez, C.; Rodríguez Sánchez, E.; García Ortiz, L.; Gómez-Marcos, M.A. Adherence to the Mediterranean Diet in Spanish Population and Its Relationship with Early Vascular Aging according to Sex and Age: EVA Study. Nutrients 2020, 12. [Google Scholar] [CrossRef] [PubMed]
- Caparello, G.; Galluccio, A.; Giordano, C.; Lofaro, D.; Barone, I.; Morelli, C.; Sisci, D.; Catalano, S.; Andò, S.; Bonofiglio, D. Adherence to the Mediterranean diet pattern among university staff: a cross-sectional web-based epidemiological study in Southern Italy. Int J Food Sci Nutr 2020, 71, 581–592. [Google Scholar] [CrossRef]
- Guallar-Castillón, P.; Pérez, R.F.; López García, E.; León-Muñoz, L.M.; Aguilera, M.T.; Graciani, A.; Gutiérrez-Fisac, J.L.; Banegas, J.R.; Rodríguez-Artalejo, F. Magnitude and management of metabolic syndrome in Spain in 2008-2010: the ENRICA study. Rev Esp Cardiol (Engl Ed) 2014, 67, 367–373. [Google Scholar] [CrossRef]
- Fernández-Bergés, D.; Cabrera de León, A.; Sanz, H.; Elosua, R.; Guembe, M.J.; Alzamora, M.; Vega-Alonso, T.; Félix-Redondo, F.J.; Ortiz-Marrón, H.; Rigo, F. , et al. Metabolic syndrome in Spain: prevalence and coronary risk associated with harmonized definition and WHO proposal. DARIOS study. Rev Esp Cardiol (Engl Ed) 2012, 65, 241–248. [Google Scholar] [CrossRef]
- Hirode, G.; Wong, R.J. Trends in the Prevalence of Metabolic Syndrome in the United States, 2011-2016. Jama 2020, 323, 2526–2528. [Google Scholar] [CrossRef]
- Ma, K.; Liu, H.; Guo, L.; Li, J.; Lei, Y.; Li, X.; Sun, L.; Yang, L.; Yuan, T.; Wang, C. , et al. Comparison of metabolic syndrome prevalence and characteristics using five different definitions in China: a population-based retrospective study. Front Public Health 2024, 12, 1333910. [Google Scholar] [CrossRef]
- Jahangiry, L.; Khosravi-Far, L.; Sarbakhsh, P.; Kousha, A.; EntezarMahdi, R.; Ponnet, K. Prevalence of metabolic syndrome and its determinants among Iranian adults: evidence of IraPEN survey on a bi-ethnic population. Sci Rep 2019, 9, 7937. [Google Scholar] [CrossRef] [PubMed]
- Alipour, P.; Azizi, Z.; Raparelli, V.; Norris, C.M.; Kautzky-Willer, A.; Kublickiene, K.; Herrero, M.T.; Emam, K.E.; Vollenweider, P.; Preisig, M. , et al. Role of sex and gender-related variables in development of metabolic syndrome: A prospective cohort study. Eur J Intern Med 2024, 121, 63–75. [Google Scholar] [CrossRef] [PubMed]
- Cubas-Basterrechea, G.; Elío, I.; Alonso, G.; Otero, L.; Gutiérrez-Bardeci, L.; Puente, J.; Muñoz-Cacho, P. Adherence to the Mediterranean Diet Is Inversely Associated with the Prevalence of Metabolic Syndrome in Older People from the North of Spain. Nutrients 2022, 14. [Google Scholar] [CrossRef]
- Al Kudsee, K.; Vahid, F.; Bohn, T. High adherence to the Mediterranean diet and Alternative Healthy Eating Index are associated with reduced odds of metabolic syndrome and its components in participants of the ORISCAV-LUX2 study. Front Nutr 2022, 9, 1087985. [Google Scholar] [CrossRef]
- Hassani Zadeh, S.; Salehi-Abargouei, A.; Mirzaei, M.; Nadjarzadeh, A.; Hosseinzadeh, M. The association between dietary approaches to stop hypertension diet and mediterranean diet with metabolic syndrome in a large sample of Iranian adults: YaHS and TAMYZ Studies. Food Sci Nutr 2021, 9, 3932–3941. [Google Scholar] [CrossRef]
- Filippou, C.D.; Thomopoulos, C.G.; Konstantinidis, D.G.; Dimitriadis, K.S.; Chrysochoou, C.A.; Tatakis, F.A.; Siafi, E.P.; Tousoulis, D.M.; Nihoyannopoulos, P.I.; Panagiotakos, D.B. , et al. Effect of DASH vs. mediterranean diet accompanied by a salt restriction on metabolic syndrome and cardiometabolic risk factors in adults with high normal blood pressure or grade 1 hypertension: secondary analyses of a randomized controlled trial. Hellenic J Cardiol 2024. [Google Scholar] [CrossRef] [PubMed]
- Martemucci, G.; Khalil, M.; Di Luca, A.; Abdallah, H.; D'Alessandro, A.G. Comprehensive Strategies for Metabolic Syndrome: How Nutrition, Dietary Polyphenols, Physical Activity, and Lifestyle Modifications Address Diabesity, Cardiovascular Diseases, and Neurodegenerative Conditions. Metabolites 2024, 14. [Google Scholar] [CrossRef]
- Romero-Cabrera, J.L.; García-Ríos, A.; Sotos-Prieto, M.; Quintana-Navarro, G.; Alcalá-Díaz, J.F.; Martín-Piedra, L.; Torres-Peña, J.D.; Luque, R.M.; Yubero-Serrano, E.M.; Delgado-Lista, J. , et al. Adherence to a Mediterranean lifestyle improves metabolic status in coronary heart disease patients: A prospective analysis from the CORDIOPREV study. J Intern Med 2023, 293, 574–588. [Google Scholar] [CrossRef]
- George, E.S.; Gavrili, S.; Itsiopoulos, C.; Manios, Y.; Moschonis, G. Poor adherence to the Mediterranean diet is associated with increased likelihood of metabolic syndrome components in children: the Healthy Growth Study. Public Health Nutr 2021, 24, 2823–2833. [Google Scholar] [CrossRef]
- Bakaloudi, D.R.; Chrysoula, L.; Kotzakioulafi, E.; Theodoridis, X.; Chourdakis, M. Impact of the Level of Adherence to Mediterranean Diet on the Parameters of Metabolic Syndrome: A Systematic Review and Meta-Analysis of Observational Studies. Nutrients 2021, 13. [Google Scholar] [CrossRef]
- Fan, H.; Wang, Y.; Ren, Z.; Liu, X.; Zhao, J.; Yuan, Y.; Fei, X.; Song, X.; Wang, F.; Liang, B. Mediterranean diet lowers all-cause and cardiovascular mortality for patients with metabolic syndrome. Diabetol Metab Syndr 2023, 15, 107. [Google Scholar] [CrossRef] [PubMed]
- Gonçalves, C.; Moreira, H.; Santos, R. Systematic review of mediterranean diet interventions in menopausal women. AIMS Public Health 2024, 11, 110–129. [Google Scholar] [CrossRef] [PubMed]
- Gómez-Sánchez, L.; Rodríguez-Sánchez, E.; Ramos, R.; Marti-Lluch, R.; Gómez-Sánchez, M.; Lugones-Sánchez, C.; Tamayo-Morales, O.; Llamas-Ramos, I.; Rigo, F.; García-Ortiz, L. , et al. The Association of Dietary Intake with Arterial Stiffness and Vascular Ageing in a Population with Intermediate Cardiovascular Risk-A MARK Study. Nutrients 2022, 14. [Google Scholar] [CrossRef] [PubMed]
- Cobos-Palacios, L.; Ruiz-Moreno, M.I.; Muñoz-Ubeda, M.; López-Sampalo, A.; Vilches-Perez, A.; Vargas-Candela, A.; Benitez-Porres, J.; Navarro-Sanz, A.; Pérez-Belmonte, L.M.; Lopez-Carmona, M.D. , et al. A healthy lifestyle is associated with lower arterial stiffness in a metabolically healthy elderly population with overweight or obesity. J Hypertens 2022, 40, 1808–1814. [Google Scholar] [CrossRef]
- Lasalvia, P.; Gianfagna, F.; Veronesi, G.; Franchin, M.; Tozzi, M.; Castelli, P.; Grandi, A.M.; Zambon, A.; Iacoviello, L.; Ferrario, M.M. Identification of dietary patterns in a general population of North Italian adults and their association with arterial stiffness. The RoCAV study. Nutr Metab Cardiovasc Dis 2021, 31, 44–51. [Google Scholar] [CrossRef]
- Navarro Cáceres, A.; Navarro-Matías, E.; Gómez-Sánchez, M.; Tamayo-Morales, O.; Lugones-Sánchez, C.; González-Sánchez, S.; Rodríguez-Sánchez, E.; García-Ortiz, L.; Gómez-Sánchez, L.; Gómez-Marcos, M.A. , et al. Increase in Vascular Function Parameters According to Lifestyles in a Spanish Population without Previous Cardiovascular Disease-EVA Follow-Up Study. Nutrients 2023, 15. [Google Scholar] [CrossRef]
- Palombo, C.; Kozakova, M. Arterial stiffness, atherosclerosis and cardiovascular risk: Pathophysiologic mechanisms and emerging clinical indications. Vascul Pharmacol 2016, 77, 1–7. [Google Scholar] [CrossRef]
- Rossi, P.; Francès, Y.; Kingwell, B.A.; Ahimastos, A.A. Gender differences in artery wall biomechanical properties throughout life. J Hypertens 2011, 29, 1023–1033. [Google Scholar] [CrossRef]
- Chester, R.; Sander, G.; Fernandez, C.; Chen, W.; Berenson, G.; Giles, T. Women have significantly greater difference between central and peripheral arterial pressure compared with men: the Bogalusa Heart Study. J Am Soc Hypertens 2013, 7, 379–385. [Google Scholar] [CrossRef]
| Blood pressure | BP figures ≥130/85 mmHg or treatment with antihypertensives |
|---|---|
| Glycemia | FBG ≥ 100 mg/dl or treatment with hypoglycemic medication |
| Triglycerides | TGC ≥ 150 mg/dl or lipid-lowering medication |
| HDL-cholesterol | HDL-C < 40 mg/dl in men or < 50mg/dl in women |
| Waist circumference | WC ≥ 88 cm in women or WC ≥ 102 cm in men |
| Overall (n=1,280) | Men (n=736) | Women (n=544) |
p value | ||||||
| Mediterranean diet | Mean or nº | SD or (%) | Mean or nº | SD or (%) | Mean or nº | SD or (%) | |||
| MD (total score) | 6.00 | 1.90 | 5.92 | 1.92 | 6.11 | 1.88 | 0.036 | ||
| MD adherence, n (%) | 504 | (39) | 288 | (40) | 216 | (40) | 0.440 | ||
| Conventional risk factors | |||||||||
| Age, (years) | 69.52 | 3.58 | 69.47 | 3.51 | 69.58 | 3.67 | 0.286 | ||
| SBP, (mmHg) | 136.81 | 17.95 | 138.86 | 17.42 | 134.03 | 18.31 | <0.001 | ||
| DBP, (mmHg) | 80.15 | 10.06 | 80.96 | 9.67 | 79.04 | 10.48 | <0.001 | ||
| Hypertension, n (%) | 947 | (74) | 548 | (74%) | 399 | (73%) | 0.350 | ||
| Antihypertensive drugs, n (%) | 739 | (58) | 410 | (56) | 329 | (61) | 0.049 | ||
| HDL cholesterol, (mg/dl) | 54.10 | 14.79 | 50.96 | 12.79 | 58.33 | 16.20 | <0.001 | ||
| Triglycerides, (mg/dl) | 121.43 | 57.56 | 120.87 | 60.49 | 122.18 | 53.38 | 0.344 | ||
| Dyslipidemia, n (%) | 1042 | (81) | 564 | (77) | 478 | (88) | <0.001 | ||
| Lipid–lowering drugs, n (%) | 463 | (36) | 240 | (33) | 223 | (41) | 0.001 | ||
| FPG, (mg/dl) | 103.04 | 28.91 | 104.37 | 28.61 | 101.23 | 29.23 | 0.028 | ||
| Diabetes mellitus, n (%) | 298 | (23) | 180 | (25) | 118 | (22) | 0.142 | ||
| Hypoglycemic drugs, n (%) | 261 | (20) | 155 | (21) | 106 | (19) | 0.268 | ||
| WC, cm | 99.61 | 10.94 | 102.59 | 9.42 | 95.57 | 11.55 | <0.001 | ||
| Obesity, n (%) | 391 | (30) | 206 | (28) | 185 | (34) | 0.012 | ||
| Arterial stiffness | |||||||||
| CAVI | 9.30 | 1.11 | 9.49 | 1.05 | 9.03 | 1.13 | <0.001 | ||
| baPWV, m/sec | 15.82 | 2.56 | 15.75 | 2.46 | 15.92 | 2.68 | <0.001 | ||
| MetS and its components | |||||||||
| Number of MetS components | 2.64 | 1.14 | 2.55 | 1.17 | 2.77 | 1.09 | 0.129 | ||
| Mets, n (%) | 658 | (51) | 362 | (49) | 296 | (54) | 0.036 | ||
| BP ≥ 130/85 mmHg, n (%) | 1082 | (84) | 639 | (87) | 443 | (81) | 0.005 | ||
| FPG ≥ 100 mg/dL, n (%) | 541 | (42) | 334 | (45) | 207 | (38) | 0.005 | ||
| TGC ≥150 mg/dL, n (%) | 289 | (23) | 162 | (22) | 127 | (23) | 0.303 | ||
| HDL-C mg/dL < 40 men, < 50 women, n (%) | 308 | (24) | 119 | (16) | 189 | (35) | <0.001 | ||
| WC ≥88 cm women, ≥102 cm men, n (%) | 798 | (62) | 385 | (52) | 413 | (76) | <0.001 | ||
| With MetS (n=658) | Without MetS (n=622) | p value | |||
| Mediterranean Diet | Mean or N | SD or (%) | Mean or N | SD or (%) | |
| MD (total score) | 5.85 | 1.81 | 6.16 | 1.98 | 0.003 |
| MD adherence, n (%) | 232 | (35.3) | 272 | (54.0) | 0.002 |
| Conventional risk factors | |||||
| Men, n (%) | 362 | (51) | 374 | (49) | 0.236 |
| Women, n (%) | 296 | (54) | 248 | (46) | 0.036 |
| Age, (years) | 69.46 | 3.31 | 69.58 | 3.84 | 0.534 |
| SBP, (mmHg) | 139.08 | 16.38 | 134.41 | 19.21 | <0.001 |
| DBP, (mmHg) | 81.16 | 9.85 | 79.07 | 10.18 | <0.001 |
| Hypertension, n (%) | 562 | (85) | 385 | (62) | <0.001 |
| Antihypertensive drugs, n (%) | 447 | (68) | 292 | (47) | <0.001 |
| HDL cholesterol, (mg/dl) | 47.78 | 11.23 | 60.79 | 15.17 | <0.001 |
| Triglycerides, (mg/dl) | 146.26 | 64.78 | 95.12 | 32.17 | <0.001 |
| Dyslipidemia, n (%) | 534 | (82) | 508 | (81) | 0.411 |
| Lipid–lowering drugs, n (%) | 268 | (41) | 195 | (31) | <0.001 |
| FPG, (mg/dl) | 114.28 | 32.28 | 91.16 | 18.55 | <0.001 |
| Diabetes mellitus, n (%) | 248 | (38) | 50 | (8) | <0.001 |
| Hypoglycemic drugs, n (%) | 222 | (34) | 39 | (6) | <0.001 |
| WC, cm | 103.37 | 10.83 | 95.64 | 9.56 | <0.001 |
| Obesity, n (%) | 291 | (44) | 100 | (26) | <0.001 |
| Arterial stiffness | |||||
| CAVI | 9.33 | 1.12 | 9.25 | 1.10 | 0.200 |
| baPWV, m sec | 16.15 | 2.58 | 15.47 | 2.49 | <0.001 |
| MetS and its components | |||||
| Number of MetS components | 3.57 | 0.71 | 1.66 | 0.52 | <0.001 |
| BP ≥ 130/85 mmHg, n (%) | 621 | (94) | 461 | (74) | <0.001 |
| FPG ≥ 100 mg/dL, n (%) | 445 | (68) | 95 | (15) | <0.001 |
| TGC ≥ 150 mg/dL, n (%) | 270 | (41) | 19 | (7) | <0.001 |
| HDL-C mg/dL < 40 men, < 50 women, n (%) | 268 | (40) | 40 | (13) | <0.001 |
| WC ≥88 cm women, ≥102 cm men, n (%) | 517 | (78) | 281 | (35) | <0.001 |
| Global | β | (95% | CI) | R2 | p |
|---|---|---|---|---|---|
| Number of MetS components | -0.168 | (-0.269 | to -0.068) | 3.30 | 0.001 |
| SBP, (mmHg) | 0.001 | (-0.005 | to 0.007) | 2.90 | 0.669 |
| DBP, (mmHg) | -0.005 | (-0.015 | to 0.006) | 3.00 | 0.402 |
| FPG, (mg/dl) | -0.007 | (-0.012 | to -0.003) | 3.70 | 0.001 |
| Triglycerides, (mg/dl) | -0.003 | (-0.005 | to -0.002) | 3.90 | <0.001 |
| HDL cholesterol, (mg/dl) | 0.013 | (0.006 | to 0.020) | 3.90 | <0.001 |
| WC, cm | -0.018 | -(0.028 | to -0.008) | 3.90 | <0.001 |
| CAVI | -0.196 | (-0.294 | to -0.099) | 4.00 | <0.001 |
| baPWV, m/sec | -0.065 | (-0.107 | to -0.060) | 3.30 | 0.002 |
| Women | |||||
| Number of MetS components | -0.115 | (-0.282 | to 0.051) | 5.20 | 0.174 |
| SBP, (mmHg) | 0.004 | (-0.004 | to 0.013) | 5.00 | 0.329 |
| DBP, (mmHg) | -0.012 | (-0.027 | to 0.002) | 4.90 | 0.099 |
| FPG, (mg/dl) | -0.001 | (-0.009 | to 0.006) | 4.00 | 0.681 |
| Triglycerides, (mg/dl) | -0.002 | (-0.005 | to 0.001) | 5.00 | 0.302 |
| HDL cholesterol, (mg/dl) | 0.017 | (0.008 | to 0.027) | 7.10 | 0.001 |
| WC, cm | -0.026 | (-0.040 | to -0.012) | 6.40 | <0.001 |
| CAVI | -0.150 | (-0.293 | to -0.008) | 5.50 | 0.038 |
| baPWV, m/sec | -0.021 | (-0.082 | to 0.040) | 4.00 | 0.499 |
| Men | |||||
| Number of MetS components | -0.181 | -0.307 | to -0.056 | 4.50 | 0.005 |
| SBP, (mmHg) | -0.002 | -0.009 | to 0.006 | 3.50 | 0.702 |
| DBP, (mmHg) | 0.003 | -0.012 | to 0.018 | 3.80 | 0.663 |
| FPG, (mg/dl) | -0.011 | -0.016 | to -0.005 | 4.50 | <0.001 |
| Triglycerides, (mg/dl) | -0.004 | -0.006 | to -0.002 | 5.10 | <0.001 |
| HDL cholesterol, (mg/dl) | 0.006 | -0.005 | to 0.017 | 3.70 | 0.281 |
| WC, cm | -0.009 | -0.024 | to 0.006 | 3.00 | 0.230 |
| CAVI | -0.230 | -0.363 | to -0.097 | 4.80 | 0.001 |
| baPWV, m/sec | -0.099 | -0.155 | to -0.043 | 4.30 | 0.001 |
| Global. | OR | (95% | CI) | R2 | p |
|---|---|---|---|---|---|
| MetS | 0.675 | (0.528 | to 0.864) | 2.50 | 0.002 |
| BP ≥ 130/85 mmHg | 0.932 | (0.651 | to 1.335) | 1.50 | 0.701 |
| FPG ≥ 100 mg/dl | 0.640 | (0.477 | to 0.859) | 2.40 | 0.003 |
| Triglycerides ≥ 150 mg/dl | 0.747 | (0.566 | to 0.986) | 1.90 | 0.040 |
| HDL-C mg/dl < 40 men, <50 mg/dl women | 1.749 | (1.315 | to 2.326) | 3.10 | <0.001 |
| WC ≥ 88 cm women, ≥102 cm men | 0.815 | (0.645 | to 1.553) | 1.50 | 0.088 |
| CAVI | 0.835 | (0.749 | to 0.931) | 2.50 | 0.001 |
| baPWV, m/sec | 0.939 | (0.896 | to 0.984) | 2.10 | 0.008 |
| Women | |||||
| MetS | 0.605 | (0.410 | to 0.895) | 6.00 | 0.012 |
| BP ≥ 130/85 mmHg | 1.347 | (0.770 | to 2.356) | 4.70 | 0.296 |
| FPG ≥ 100 mg/dl | 0.604 | (0.376 | to 0.971) | 5.50 | 0.033 |
| Triglycerides ≥ 150 mg/dl | 1.035 | (0.681 | to 1.573) | 4.50 | 0.873 |
| HDL-C mg/dl < 40 men, < 50 women | 1.792 | (1.221 | to 2.632) | 6.70 | 0.003 |
| WC ≥ 88 cm women, ≥ 102 cm men | 0.751 | (0.495 | to 1.140) | 4.50 | 0.178 |
| CAVI | 0.841 | (0.713 | to 0.991) | 5.30 | 0.038 |
| baPWV, m/sec | 0.952 | (0.887 | to 1.022) | 4.70 | 0.171 |
| Men | |||||
| MetS | 0.760 | (0.552 | to 1.046) | 3.20 | 0.093 |
| BP ≥ 130/85 mmHg | 0.685 | (0.423 | to 1.109) | 3.10 | 0.124 |
| FPG ≥ 100 mg/dl | 0.696 | (0.477 | to 1.015) | 3.30 | 0.060 |
| Triglycerides ≥ 150 mg/dl | 0.609 | (0.417 | to 0.891) | 3.90 | 0.011 |
| HDL-C mg/dl < 40 men, < 50 women | 1.665 | (1.082 | to 2.563) | 3.70 | 0.020 |
| WC ≥ 88 cm women, ≥102 cm men | 0.840 | (0.622 | to 1.134) | 2.90 | 0.255 |
| CAVI | 0.825 | (0.711 | to 0.957) | 3.70 | 0.011 |
| baPWV, m/sec | 0.924 | (0.867 | to 0.985) | 3.60 | 0.015 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





