Submitted:
25 September 2024
Posted:
25 September 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Demographics of Sepsis
3. Pathophysiology and Immunological Aspects of Sepsis across Ages
4. Biomarkers and Sepsis
5. Presepsin as a Sepsis Biomarker across Age Groups
5.1. Presepsin as a Sepsis Biomarker in Neonates and Children
5.2. Presepsin as a Sepsis Biomarker in Adults
5.3. Presepsin as a Sepsis Biomarker in Older Adults
6. Published Meta-Analysis on Presepsin as Sepsis Biomarker
7. Discussion
8. Conclusions
Funding
Generative Intelligence Application
Acknowledgments
Conflicts of Interest
References
- Singer M, Deutschman CS, Seymour CW, et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA. 2016;315(8):801-810. [CrossRef]
- Martín S, Pérez A, Aldecoa C. Sepsis and Immunosenescence in the Elderly Patient: A Review. Front Med. 2017;4:20. [CrossRef]
- Rudd KE, Johnson SC, Agesa KM, et al. Global, regional, and national sepsis incidence and mortality, 1990–2017: Analysis for the Global Burden of Disease Study. Lancet. 2020;395(10219):200-211. [CrossRef]
- Vaduganathan M, Mensah GA, Turco JV, Fuster V, Roth GA. The Global Burden of Cardiovascular Diseases and Risk A Compass for Future Health. J Am Coll Cardiol. 2022;80(25):2361-2371. [CrossRef]
- Kerrigan SW, Martin-Loeches I. Public awareness of sepsis is still poor: We need to do more. Intensiv Care Med. 2018;44(10):1771-1773. [CrossRef]
- Fiest KM, Krewulak KD, Brundin-Mather R, et al. Patient, Public, and Healthcare Professionals’ Sepsis Awareness, Knowledge, and Information Seeking Behaviors: A Scoping Review*. Crit Care Med. 2022;50(8):1187-1197. [CrossRef]
- Kim HI, Park S. Sepsis: Early Recognition and Optimized Treatment. Tuberc Respir Dis. 2018;81(1):6-14. [CrossRef]
- Luo J, Jiang W, Weng L, et al. Usefulness of qSOFA and SIRS scores for detection of incipient sepsis in general ward patients: A prospective cohort study. J Crit Care. 2019;51:13-18. [CrossRef]
- Behnes M, Bertsch T, Lepiorz D, et al. Diagnostic and prognostic utility of soluble CD 14 subtype (presepsin) for severe sepsis and septic shock during the first week of intensive care treatment. Critical Care. 2014;18(5). [CrossRef]
- CDC C of DC and P. About Multiple Cause of Death, 1999-2020. About Multiple Cause of Death, 1999-2020. Published September 8, 2023. Accessed July 23, 2023.
- Oikonomakou MZ, Gkentzi D, Gogos C, Akinosoglou K. Biomarkers in pediatric sepsis: A review of recent literature. Biomark Med. 2020;14(10):895-917. [CrossRef]
- Balamuth F, Weiss SL, Neuman MI, et al. Pediatric Severe Sepsis in U.S. Children’s Hospitals* Pediatr Crit Care Med. 2014;15(9):798-805. [CrossRef]
- Gude SS, Peddi NC, Vuppalapati S, Gopal SV, Ramesh HM, Gude SS. Biomarkers of Neonatal Sepsis: From Being Mere Numbers to Becoming Guiding Diagnostics. Cureus. 2022;14(3):e23215. [CrossRef]
- Sharma D, Farahbakhsh N, Shastri S, Sharma P. Biomarkers for diagnosis of neonatal sepsis: A literature review. J Matern-Fetal Neonatal Med. 2018;31(12):1646-1659. [CrossRef]
- Martin GS, Mannino DM, Moss M. The effect of age on the development and outcome of adult sepsis* Crit Care Med. 2006;34(1):15-21. [CrossRef]
- Kramarow EA. Sepsis-related Mortality Among Adults Aged 65 and Over: United States, 2019. NCHS Data Brief. 2021 Nov;(422):1-8. [CrossRef] [PubMed]
- Arora J, Mendelson AA, Fox-Robichaud A. Sepsis: Network pathophysiology and implications for early diagnosis. Am J Physiol-Regul, Integr Comp Physiol. 2023;324(5):R613-R624. [CrossRef]
- Michels EHA, Butler JM, Reijnders TDY, et al. Association between age and the host response in critically ill patients with sepsis. Crit Care. 2022;26(1):385. [CrossRef]
- Wynn J, Cornell TT, Wong HR, Shanley TP, Wheeler DS. The Host Response to Sepsis and Developmental Impact. Pediatrics. 2010;125(5):1031-1041. [CrossRef]
- Hincu MA, Zonda GI, Stanciu GD, Nemescu D, Paduraru L. Relevance of Biomarkers Currently in Use or Research for Practical Diagnosis Approach of Neonatal Early-Onset Sepsis. Children. 2020;7(12):309. [CrossRef]
- Camargo JF de, Caldas JP de S, Marba STM. Early neonatal sepsis: Prevalence, complications and outcomes in newborns with 35 weeks of gestational age or more. Rev Paul Pediatr. 2021;40:e2020388. [CrossRef]
- Goldstein B, Giroir B, Randolph A, Sepsis ICC on P. International pediatric sepsis consensus conference: Definitions for sepsis and organ dysfunction in pediatrics* Pediatr Crit Care Med. 2005;6(1):2-8. [CrossRef]
- Schlapbach LJ, Kissoon N. Defining Pediatric Sepsis. JAMA Pediatrics. 2018;172(4):313-314. [CrossRef]
- Sanchez-Pinto LN, Bennett TD, DeWitt PE, et al. Development and Validation of the Phoenix Criteria for Pediatric Sepsis and Septic Shock. JAMA. 2024;331(8). [CrossRef]
- Barsness KA, Bensard DD, Partrick DA, Calkins CM, Hendrickson RJ, McIntyre RC. Endotoxin induces an exaggerated interleukin-10 response in peritoneal macrophages of children compared with adults. J Pediatr Surg. 2004;39(6):912-915. [CrossRef]
- Wynn JL, Scumpia PO, Winfield RD, et al. Defective innate immunity predisposes murine neonates to poor sepsis outcome but is reversed by TLR agonists. Blood. 2008;112(5):1750-1758. [CrossRef]
- Hall M. Immune Modulation in Pediatric Sepsis. J Pediatr Intensiv Care. 2019;08(01):042-050. [CrossRef]
- Wong HR. Pediatric sepsis biomarkers for prognostic and predictive enrichment. Pediatr Res. 2022;91(2):283-288. [CrossRef]
- Lim PPC, Bondarev DJ, Edwards AM, Hoyen CM, Macias CG. The evolving value of older biomarkers in the clinical diagnosis of pediatric sepsis. Pediatr Res. 2023;93(4):789-796. [CrossRef]
- Kathmandu K children H, Jeevan GJ. Clinical, Demographic Profile and Outcome of Children Admitted in PICU with A Diagnosis of Severe Sepsis and Septic Shock. J. Med. Sci. Clin. Res.. 2017, 5(12). [CrossRef]
- Wong HR, Cvijanovich NZ, Anas N, et al. Developing a Clinically Feasible Personalized Medicine Approach to Pediatric Septic Shock. Am J Respir Crit Care Med. 2015;191(3):309-315. [CrossRef]
- Wardi G, Tainter CR, Ramnath VR, et al. Age-related incidence and outcomes of sepsis in California, 2008–2015. J Crit Care. 2021;62:212-217. [CrossRef]
- Poll T van der, Shankar-Hari M, Wiersinga WJ. The immunology of sepsis. Immunity. 2021;54(11):2450-2464. [CrossRef]
- Gentile LF, Nacionales DC, Lopez MC, et al. Protective Immunity and Defects in the Neonatal and Elderly Immune Response to Sepsis. J Immunol. 2014;192(7):3156-3165. 3156. [CrossRef]
- Darden DB, Kelly LS, Fenner BP, Moldawer LL, Mohr AM, Efron PA. Dysregulated Immunity and Immunotherapy after Sepsis. J Clin Med. 2021;10(8):1742. [CrossRef]
- Milbrandt EB, Eldadah B, Nayfield S, Hadley E, Angus DC. Toward an Integrated Research Agenda for Critical Illness in Aging. Am J Respir Crit Care Med. 2012;182(8):995-1003. [CrossRef]
- Jia L, Hao L, Li X, Jia R, Zhang HL. Comparing the predictive values of five scales for 4-year all-cause mortality in critically ill elderly patients with sepsis. Ann Palliat Med. 2021;0(0):6-6. [CrossRef]
- Wang Y, Dong C, Han Y, Gu Z, Sun C. Immunosenescence, aging and successful aging. Front Immunol. 2022;13:942796. [CrossRef]
- Martin-Loeches I, Guia MC, Vallecoccia MS, et al. Risk factors for mortality in elderly and very elderly critically ill patients with sepsis: A prospective, observational, multicenter cohort study. Ann Intensiv Care. 2019;9(1):26. [CrossRef]
- Kaukonen KM, Bailey M, Suzuki S, Pilcher D, Bellomo R. Mortality Related to Severe Sepsis and Septic Shock Among Critically Ill Patients in Australia and New Zealand, 2000-2012. JAMA. 2014;311(13):1308-1316. [CrossRef]
- Woodcock J. The Prospects for “Personalized Medicine” in Drug Development and Drug Therapy. Clin Pharmacol Ther. 2007;81(2):164-169. [CrossRef]
- Woodcock J, Woosley R. The FDA Critical Path Initiative and Its Influence on New Drug Development. Annu Rev Med. 2008;59(1):1-12. [CrossRef]
- im MH, Choi JH. An Update on Sepsis Biomarkers. Infect Chemother. 2020;52(1):1-18. [CrossRef]
- Llitjos, JF., Carrol, E.D., Osuchowski, M.F. et al. Enhancing sepsis biomarker development: Key considerations from public and private perspectives. Crit Care 28, 238 (2024). [CrossRef]
- Liang, P., Wu, Y., Qu, S. et al. Exploring the biomarkers and potential therapeutic drugs for sepsis via integrated bioinformatic analysis. BMC Infect Dis 24, 32 (2024). [CrossRef]
- Deltell JMM, Boter NR. Biomarkers in emergencies: A never-ending race? Emergencias. 2024 Jan;36(1):4-6. Spanish, English. [CrossRef]
- Kadim MM, AL-Dahmoshi HOM, AL-Khikan FHO. Sepsis biomarkers: Current information and future visions. Microbes and Infectious Diseases 2024; 5(4): 201-210.
- Mankowski RT, Anton SD, Ghita GL, et al. Older adults demonstrate biomarker evidence of the persistent inflammation, immunosuppression and catabolism syndrome (PICS) after sepsis. J Gerontol: Ser A. 2021;77(1):glab080-. [CrossRef]
- Feng L, Liu S, Wang J, Gao Y et al. The performance of a combination of heparin-binding protein with other biomarkers for sepsis diagnosis: An observational cohort study BMC Infectious Diseases (2024) 24:755. [CrossRef]
- Clemente C, Fuentes ME, Ortega D, Julián A, Martín-Sánchez FJ, González del Castillo J. Utilidad de la combinación de biomarcadores de respuesta inflamatoria y escalas clínicas para la estratificación del riesgo en pacientes atendidos en urgencias por sospecha de infección. Emergencias. 2024;36:9-16.
- Lippi, Giuseppe. "Sepsis biomarkers: Past, present and future" Clinical Chemistry and Laboratory Medicine (CCLM), vol. 57, no. 9, 2019, pp. 1281-1283. [CrossRef]
- Schuetz P, Beishuizen A, Broyles M, Ferrer R, Gavazzi G, Gluck EH, et al. Procalcitonin (PCT)-guided antibiotic stewardship: An international experts consensus on optimized clinical use. Clin Chem Lab Med 2019;57:1308–18.
- Vincent JL, van der Poll T, Marshall JC. The End of "One Size Fits All" Sepsis Therapies: Toward an Individualized Approach. Biomedicines. 2022 Sep 12;10(9):2260. [CrossRef]
- Bulatova YY, Maltabarova NA, Zhumabayev MB, Li TA, Ivanova MP. Modern Diagnostics of Sepsis and Septic Shock in Children. Electron J Gen Med. 2020;17(5):em216. [CrossRef]
- Lanziotti VS, Póvoa P, Soares M, Silva JRL e, Barbosa AP, Salluh JIF. Use of biomarkers in pediatric sepsis: Literature review. Rev Bras Ter Intensiv. 2016;28(4):472-482. [CrossRef]
- Schuh AM, Leger KJ, Summers C, Uspal NG. Lactic Acidosis in a Critically Ill Patient. Pediatr Emerg Care. 2018;34(9):e165-e167. [CrossRef]
- Kustán P, Horváth-Szalai Z, Mühl D. Nonconventional Markers of Sepsis. EJIFCC. 2017;28(2):122-133.
- Hung SK, Lan HM, Han ST, Wu CC, Chen KF. Current Evidence and Limitation of Biomarkers for Detecting Sepsis and Systemic Infection. Biomedicines. 2020;8(11):494. [CrossRef]
- Teggert A, Datta H, Ali Z. Biomarkers for Point-of-Care Diagnosis of Sepsis. Micromachines. 2020;11(3):286. [CrossRef]
- Wagner KH, Cameron-Smith D, Wessner B, Franzke B. Biomarkers of Aging: From Function to Molecular Biology. Nutrients. 2016;8(6):338. [CrossRef]
- Franceschi C, Bonafè M, Valensin S, et al. Inflamm-aging: An Evolutionary Perspective on Immunosenescence. Ann N York Acad Sci. 2000;908(1):244-254. [CrossRef]
- Ginde AA, Blatchford PJ, Trzeciak S, et al. Age-Related Differences in Biomarkers of Acute Inflammation During Hospitalization for Sepsis. Shock. 2014;42(2):99-107. [CrossRef]
- Yende S, D’Angelo G, Kellum JA, et al. Inflammatory Markers at Hospital Discharge Predict Subsequent Mortality after Pneumonia and Sepsis. Am J Respir Crit Care Med. 2008;177(11):1242-1247.
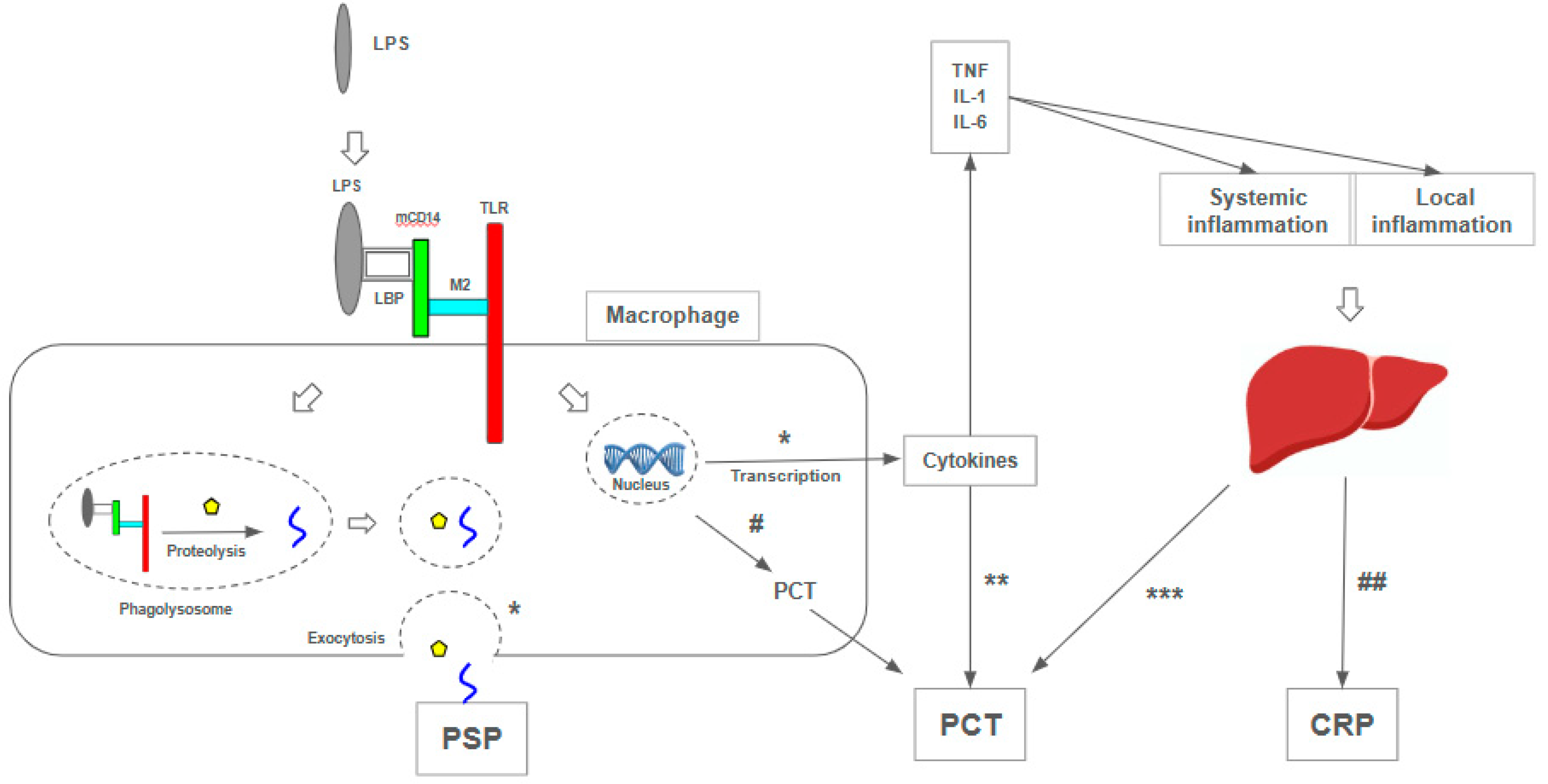
- Velissaris D, Zareifopoulos N, Karamouzos V, et al. Presepsin as a Diagnostic and Prognostic Biomarker in Sepsis. Cureus. Published online 2021. 2021. [CrossRef]
- Yaegashi Y, Shirakawa K, Sato N, et al. Evaluation of a newly identified soluble CD14 subtype as a marker for sepsis. Journal of Infection and Chemotherapy. 2005;11(5):234-238. [CrossRef]
- Arai Y, Mizugishi K, Nonomura K, Naitoh K, Takaori-Kondo A, Yamashita K. Phagocytosis by human monocytes is required for the secretion of presepsin. J Infect Chemother. 2015;21(8):564-569. [CrossRef]
- MDsave. Blood culture. Published July 24, 2023. Available online: https://www.mdsave.com/procedures/blood-culture/d787ffc9.
- Truehealthlabs. 2023;(Culture). Available online: https://truehealthlabs.com/product/blood-culture/.
- Henriquez-Camacho C, Losa J. Biomarkers for sepsis. BioMed Research International. 2014;2014. [CrossRef]
- Park J, Yoon JH, Ki HK, Ko JH, Moon HW. Performance of presepsin and procalcitonin predicting culture-proven bacterial infection and 28-day mortality: A cross sectional study. Frontiers in Medicine. 2022;9. [CrossRef]
- Pierrakos C, Velissaris D, Bisdorff M, Marshall JC, Vincent JL. Biomarkers of sepsis: Time for a reappraisal. Critical Care. 2020;24(1). [CrossRef]
- Memar MY, Baghi HB. Presepsin: A promising biomarker for the detection of bacterial infections. Biomed Pharmacother. 2019;111:649-656. [CrossRef]
- Maddaloni C, Rose DUD, Santisi A, et al. The Emerging Role of Presepsin (P-SEP) in the Diagnosis of Sepsis in the Critically Ill Infant: A Literature Review. Int J Mol Sci. 2021;22(22):12154. [CrossRef]
- Piccioni A, Santoro MC, Cunzo T de, et al. Presepsin as Early Marker of Sepsis in Emergency Department: A Narrative Review. Medicina. 2021;57(8):770. [CrossRef]
- Ferreira T, Candido MA, Soriano FG. Sepsis biomarkers: A review of the diagnostic value of presepsin. Revista de Medicina. 2023;102(1). [CrossRef]
- Kyriazopoulou E, Leventogiannis K, Tavoulareas G, et al. Presepsin as a diagnostic and prognostic biomarker of severe bacterial infections and COVID-19. Scientific Reports. 2023;13(1). [CrossRef]
- Puspaningtyas NW, Karyanti MR, Paramita TN, et al. Presepsin as a promising biomarker for early detection of post-operative infection in children. Front Pediatr. 2023;11:1036993. [CrossRef]
- Tzialla C, Manzoni P, Achille C, Bollani L, Stronati M, Borghesi A. New Diagnostic Possibilities for Neonatal Sepsis. Am J Perinatol. 2018;35(06):575-577. [CrossRef]
- Pugni L, Pietrasanta C, Milani S, et al. Presepsin (Soluble CD14 Subtype): Reference Ranges of a New Sepsis Marker in Term and Preterm Neonates. PLoS ONE. 2015;10(12):e0146020. [CrossRef]
- Montaldo P, Rosso R, Santantonio A, Chello G, Giliberti P. Presepsin for the detection of early-onset sepsis in preterm newborns. Pediatr Res. 2017;81(2):329-334. [CrossRef]
- Ruan L, Chen GY, Liu Z, et al. The combination of procalcitonin and C-reactive protein or presepsin alone improves the accuracy of diagnosis of neonatal sepsis: A meta-analysis and systematic review. Crit Care. 2018;22(1):316. [CrossRef]
- Bellos I, Fitrou G, Pergialiotis V, Thomakos N, Perrea DN, Daskalakis G. The diagnostic accuracy of presepsin in neonatal sepsis: A meta-analysis. Eur J Pediatr. 2018;177(5):625-632. [CrossRef]
- Yoon SH, Kim EH, Kim HY, Ahn JG. Presepsin as a diagnostic marker of sepsis in children and adolescents: A systemic review and meta-analysis. BMC Infectious Diseases. 2019;19(1). [CrossRef]
- Korpelainen S, Intke C, Hämäläinen S, Jantunen E, Juutilainen A, Pulkki K. Soluble CD14 as a Diagnostic and Prognostic Biomarker in Hematological Patients with Febrile Neutropenia. Dis Markers. 2017;2017:9805609. [CrossRef]
- Olad E, Sedighi I, Mehrvar A, et al. Presepsin (scd14) as a marker of serious bacterial infections in chemotherapy induced severe neutropenia. Iran J Pediatr. 2014;24(6):715-722.
- Baraka A, Zakaria M. Presepsin as a diagnostic marker of bacterial infections in febrile neutropenic pediatric patients with hematological malignancies. Int J Hematol. 2018;108(2):184-191. [CrossRef]
- Giavarina D, Carta M. Determination of reference interval for presepsin, an early marker for sepsis. Biochem Med. 2015;25(1):64-68. [CrossRef]
- Zvyagin AA, Demidova VS, Smirnov GV. Dinamika biomarkerov sepsisa kak pokazatel’ éffektivnosti intensivnoĭ terapii. Khirurgiia. 2019;(2):53-57. [CrossRef]
- Ikeda T, Kamohara H, Suda S, et al. Comparative evaluation of endotoxin activity level and various biomarkers for infection and outcome of ICU-admitted patients. Biomedicines. 2019;7(3). [CrossRef]
- Fischer P, Grigoras C, Bugariu A, et al. Are presepsin and resistin better markers for bacterial infection in patients with decompensated liver cirrhosis? Digestive and Liver Disease. 2019;51(12):1685-1691. [CrossRef]
- Fujii E, Fujino K, Eguchi Y. An evaluation of clinical inflammatory and coagulation markers in patients with sepsis: A pilot study. Acute Medicine & Surgery. 2019;6(2):158-164. [CrossRef]
- Chen J, Huang ZB, Li H, et al. Early Diagnostic Biomarkers of Sepsis for Patients with Acute-on-Chronic Liver Failure: A Multicenter Study. Infectious Diseases and Therapy. 2021;10(1):281-290. [CrossRef]
- Tsujimoto K, Hata A, Fujita M, Hatachi S, Yagita M. Presepsin and procalcitonin as biomarkers of systemic bacterial infection in patients with rheumatoid arthritis. Int J Rheum Dis. 2018 Jul;21(7):1406-141. [CrossRef]
- Koizumi Y, Shimizu K, Shigeta M, et al. Plasma presepsin level is an early diagnostic marker of severe febrile neutropenia in hematologic malignancy patients. BMC Infectious Diseases. 2017;17(1). [CrossRef]
- Kang T, Yoo J, Choi H, Lee S, Jekarl DW, Kim Y. Performance evaluation of presepsin using a Sysmex HISCL-5000 analyzer and determination of reference interval. Journal of Clinical Laboratory Analysis. 2022;36(9). [CrossRef]
- Dragoş D, Ghenu MI, Timofte D, Balcangiu-Stroescu AE, Ionescu D, Manea MM. The cutoff value of presepsin for diagnosing sepsis increases with kidney dysfunction, a cross-sectional observational study. Medicine (United States). 2023;102(1):E32620-E32620. 3262. [CrossRef]
- Imai Y, Taniguchi K, Iida R, Nitta M, Uchiyma K, Takasu A. Diagnostic accuracy of presepsin in predicting bacteraemia in elderly patients admitted to the emergency department: Prospective study in Japan. BMJ Open. 2019;9(12):e030421. [CrossRef]
- Ruangsomboon O, Panjaikaew P, Monsomboon A, Chakorn T, Permpikul C, Limsuwat C. Diagnostic and prognostic utility of presepsin for sepsis in very elderly patients in the emergency department. Clin Chim Acta. 2020;510:723-732. [CrossRef]
- Claessens YE, Trabattoni E, Grabar S, et al. Plasmatic presepsin (sCD14-ST) concentrations in acute pyelonephritis in adult patients. Clinica Chimica Acta. 2017;464:182-188. [CrossRef]
- Musso CG, Oreopoulos DG. Aging and Physiological Changes of the Kidneys Including Changes in Glomerular Filtration Rate. Nephron Physiol. 2011;119(Suppl 1):p1-p5. [CrossRef]
- Chenevier-Gobeaux C, Trabattoni E, Roelens M, Borderie D, Claessens YE. Presepsin (sCD14-ST) in emergency department: The need for adapted threshold values? Clin Chim Acta. 2014;427:34-36. [CrossRef]
- Nagata T, Yasuda Y, Ando M, et al. Clinical impact of kidney function on presepsin levels. PLoS ONE. 2015;10(6). [CrossRef]
- Kim H, Song1 J, *, et al. Presepsin levels for discriminating sepsis and predicting mortality among organ failure patients stratified by hypercreatinemia. Signa Vitae. Published online 2023. [CrossRef]
- Shozushima T, Takahashi G, Matsumoto N, Kojika M, Okamura Y, Endo S. Usefulness of presepsin (sCD14-ST) measurements as a marker for the diagnosis and severity of sepsis that satisfied diagnostic criteria of systemic inflammatory response syndrome. Journal of Infection and Chemotherapy. 2011;17(6):764-769. [CrossRef]
- Endo S, Suzuki Y, Takahashi G, et al. Usefulness of presepsin in the diagnosis of sepsis in a multicenter prospective study. Journal of Infection and Chemotherapy. 2012;18(6):891-897. [CrossRef]
- Maldeghem I van, Nusman CM, Visser DH. Soluble CD14 subtype (sCD14-ST) as biomarker in neonatal early-onset sepsis and late-onset sepsis: A systematic review and meta-analysis. BMC Immunol. 2019;20(1):17. [CrossRef]
- Poggi C, Bianconi T, Gozzini E, Generoso M, Dani C. Presepsin for the detection of late-onset sepsis in preterm newborns. Pediatrics. 2015;135(1):68-75. [CrossRef]
- Wu CC, Lan HM, Han ST, et al. Comparison of diagnostic accuracy in sepsis between presepsin, procalcitonin, and C-reactive protein: A systematic review and meta-analysis. Annals of Intensive Care. 2017;7(1). [CrossRef]
- Zheng Z, Jiang L, Ye L, Gao Y, Tang L, Zhang M. The accuracy of presepsin for the diagnosis of sepsis from SIRS: A systematic review and meta-analysis. Annals of Intensive Care. 2015;5(1):1-13. [CrossRef]
- Liu Y, Hou J huan, Li Q, Chen K jun, Wang SN, Wang J min. Biomarkers for diagnosis of sepsis in patients with systemic inflammatory response syndrome: A systematic review and meta-analysis. SpringerPlus. 2016;5(1). [CrossRef]
- Kondo Y, Umemura Y, Hayashida K, Hara Y, Aihara M, Yamakawa K. Diagnostic value of procalcitonin and presepsin for sepsis in critically ill adult patients: A systematic review and meta-analysis. J Intensiv Care. 2019;7(1):22. [CrossRef]
- Yang HS, Hur M, Yi A, Kim H, Lee S, Kim SN. Prognostic value of presepsin in adult patients with sepsis: Systematic review and meta-analysis. PLoS ONE. 2018;13(1):e0191486. [CrossRef]
- Zhu Y, Li X, Guo P, Chen Y, Li J, Tao T. The accuracy assessment of presepsin (sCD14-ST) for mortality prediction in adult patients with sepsis and a head-to-head comparison to PCT: A meta-analysis. Therapeutics and Clinical Risk Management. 2019;15:741-753. [CrossRef]
- Ali FT, Ali MAM, Elnakeeb MM, Bendary HNM. Presepsin is an early monitoring biomarker for predicting clinical outcome in patients with sepsis. Clinica Chimica Acta. 2016;460:93-101. [CrossRef]
- Yu H, Qi Z, Hang C, Fang Y, Shao R, Li C. Evaluating the value of dynamic procalcitonin and presepsin measurements for patients with severe sepsis. Am J Emerg Med. 2017;35(6):835-841. [CrossRef]
- Boyd CM, Landefeld CS, Counsell SR, et al. Recovery of Activities of Daily Living in Older Adults After Hospitalization for Acute Medical Illness. J Am Geriatr Soc. 2008;56(12):2171-2179. 2171. [CrossRef]
- Wynn JL, Wong HR. Fetal and Neonatal Physiology (Fifth Edition). Sect XXVI: Pathophysiol Neonatal Dis. 2017;(J Immunol19272014):1536-1552.e10. [CrossRef]
- Sampson D, Yager TD, Fox B, et al. Blood transcriptomic discrimination of bacterial and viral infections in the emergency department: A multi-cohort observational validation study. BMC Med. 2020;18(1):185. [CrossRef]
- Kwizera A, Baelani I, Mer M, et al. The long sepsis journey in low- and middle-income countries begins with a first step...but on which road? Crit Care. 2018;22(1):64. [CrossRef]
- Maruna P, Nedelníková K, Gurlich R. Physiology and genetics of procalcitonin. Physiol Res. 2000;49(1):S57-61.
- Dong R, Wan B, Lin S, et al. Procalcitonin and Liver Disease: A Literature Review. J Clin Transl Hepatol. 2019;7(1):51-55. [CrossRef]
- Oberhoffer M, Stonans I, Russwurm S, et al. Procalcitonin expression in human peripheral blood mononuclear cells and its modulation by lipopolysaccharides and sepsis-related cytokines in vitro. J Lab Clin Med. 1999;134(1):49-55. [CrossRef]
- Pepys MB, Hirschfield GM. C-reactive protein: A critical update. J Clin Investig. 2003;111(12):1805-1812. 1805. [CrossRef]
| Age Group | Author | Admission Medium PSP Levels (ng/mL) | Cutoff Values (ng/mL) | |||
|---|---|---|---|---|---|---|
| Sepsis | Non Sepsis | Survivor | Non Survivor | |||
| Neonates & children | Poggi et al. 2015 [107] | 1295 | 562 | - | - | 885 |
| Pugni et al. 2015 [79] | - | 649 | - | - | - | |
| Montaldo et al. 2016 [80] | 598 | 328 | - | - | 788 * | |
| Korpelainen et al. 2017 [84] | 1432 | - | - | - | - | |
| Bellos et al. 2018 [82] | - | - | - | - | 650–850 ** | |
| Baraka et al. 2018 [86] | 1014 | 178 | - | - | Multiple | |
| Yoon et al. 2019 [83] | - | - | - | - | 650 ** | |
| Puspaningtyas et al. 2023 [77] | 806.5 | 717 | - | - | 761 * | |
| Adults | Shozushima et al. 2011 [104] | 817.9 | 190 | - | - | 399 |
| Endo et al. 2012 [105] | 1579 | 312 | - | - | Multiple | |
| Giavarina et al. 2015 [87] | 55-184 | - | - | - | - | |
| Ali et al. 2016 [114] | 1183 | 472 | 615,5 | 1301 | Multiple | |
| Yu et al. 2017 [115] | - | - | 1230,5 | 1269 | - | |
| Claessens et al. 2017 [99] | 476 | 200 | - | - | - | |
| Ikeda et al. 2019 [89] | - | - | 3251 | 1108 | - | |
| Zvyagyn et al. 2019 [88] | - | - | 1718 | 3266 | - | |
| Dragoş et al. 2023 [96] | 1039 | 372 | - | - | - | |
| Old adults | Imai et al. 2019 [97] | 639.93 | 866.56 | - | - | 285 |
| Ruangsomboon et al. 2020 [98] | 746 | 316 | 470 | 795 | Multiple | |
| Aspects | Pediatric | Adult | Elderly |
|---|---|---|---|
| Positive | Early elevation, affordable cost, better diagnostic performance (PCT and CRP) and prognostic validity (30-day mortality), monitoring of antibiotic therapy, levels not influenced by gestational age, predictor of clinical evolution in febrile neutropenics | Better prognostic validity (PCT, CRP, ESR), correlation with hospital mortality in sepsis and septic shock, prognostic validity (28-day mortality), correlation with clinical outcomes, stable in different clinical scenarios (cirrhosis, rheumatoid arthritis, febrile neutropenia) | A better predictor of bacteremia in the Emergency Department (PCT, CRP), similar diagnostic accuracy to PCT, similar prognostic accuracy (qSOFA, SIRS) |
| Negative | Poor predictor of bacterial infection (PCT), non-standardized cutoff points, inaccessible in most scenarios | Poor predictor of bacterial infection (PCT), requires adjustments when kidney function is altered | Diagnostic and prognostic accuracy lower than combination (PCT + CRP + PSP), major renal dysfunction in older adults, specific cutoff point (immunosenescence) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).





