Background
About 153,000 people are living with Parkinson's disease in the UK, and one in 37 persons get diagnosed with Parkinson’s in their lifetime. This is expected to increase to 172,000 by 2030 (Parkinson’s UK, 2023). Parkinson’s is a neurodegenerative disorder that affects movement and coordination. Some common symptoms of Parkinson's include tremors, stiffness, and impaired balance. All these adversely affects the quality of life (QoL) of the PwP as well as of their caregivers.
Rahman et al., (2008); and Schrag et al., (2000) found that the QoL of a PwP is adversely affected because of sudden unpredictable on/off states, depression, disability, postural instability, difficulty in walking, difficulty in dressing, falls, urinary incontinence, pain, cognitive impairment and confusion. Rahman et al., (2008) further found that hesitation to begin walking, shuffling gait, freezing, festination, propulsion, and difficulty in turning also had influence on their QoL.
Diagnosis of Parkinson’s not only affects the quality of life of the person diagnosed with Parkinson’s but also that of their carers. In most cases, where the carers are family members (McCrone et al., 2007), the direct and indirect costs of managing the condition are borne by both – the PwP and their carer – more specifically much higher in advanced stages. Gumber et al., (2019) found that there is deterioration in Quality of Life (QoL) of PwP and their carers and family members with the progression of disease. This can be because of family members volunteering their time, altering their employment status, utilising their own resources, developing stress and health problems alongside the deteriorating condition of the PwP.
Informal carers of PwP in advanced stages, especially when the PwP’s cognition is adversely affected, exhibit a significant decreased in QoL (Henry et al., 2020; Rosqvist et al., 2022). They also found that the deterioration in QoL of carers of PwP with a high non-motor symptoms (NMS) burden is higher, especially if the carer was a woman. Of all the informal carers, spousal caregivers are most affected. Modugno et al., (2020) observed that the obligations of carers towards PwP care increased with disease progression and is not just limited to assisting with activities of daily living (ADL). This adversely affects the QoL of informal carers. Santos-García et al., (2022) found that burden, strain, mood, and QoL of the principal carer of a PwP worsened after a 2-year follow-up study. The changes in mood of the PwP and their carers with disease progression add to the carers’ both economic and social burden.
These are the primary contributors to a worsened QoL of PwP and their carers on financial condition. The economic burden associated with the condition, and its progression, exacerbates the deterioration in the QoL of PwP and their carers. Chaudhuri et al., (2024) found that the economic burden of Parkinson’s increased with its progression, and the incremental economic costs for advanced stage condition was higher by an average of £1069 as compared to mild-to-moderate stages. Economic burden of Parkinson’s is estimated for PwP and different stakeholders at different points of time. Weir et al., (2018) found that the mean annual health care cost was higher by £2471 (2013 constant prices) for PwP as compared to those who did not have Parkinson’s per person in the first year post-diagnosis. This increased to £4004 per PwP by 10 years following diagnosis. Costs for PwP with markers of advanced Parkinson’s (i.e., “presence of levodopa-equivalent daily dose > 1100 mg, dyskinesias, falls, dementia, psychosis, hospital admission primarily due to PD, or nursing home placement”) were higher by £1069 per PwP as compared to those without it; all these estimates are at 2013 constant prices.
L. J. Findley et al., (2011) estimated that of all the healthcare costs incurred for an PwP, only 7% contributed to direct medical care. The remaining 93% of costs were comprised of direct non-medical professional care (50%) and indirect informal care (43%). L. J. Findley, (2007) estimated that the annual costs of direct and indirect costs of Parkinson’s ranged between £449 million and £3.3 billion in the UK. They also found that more than direct costs, which comprises largely of inpatient care, nursing home costs, and prescription drugs, the indirect costs, comprising of productivity losses and carer burden are far higher. McCrone et al., (2007) found that the annual service costs (baseline and follow-up combined) were £13,804 per person, of which 80% component was informal care provided by family / friends. They also found that 42% of the follow up costs were because of disability and depression. Moreover, these costs were higher for men as compared to women. L. Findley et al., (2003) had estimated per PwP costs for different stages of Parkinson’s. They further estimated that 38% of direct costs of care is accounted towards NHS costs, 34% towards social services. However, a move from home to residential care for PwP resulted in an approximately 500% increase in the cost of care.
This explains the exponential growth in the economic costs of treatment and care for PwP with the progression of Parkinson’s. Effective treatment and care for Parkinson's aims to manage symptoms and improve quality of life. However, the financial distress caused by treatment and care costs can impact the quality of Parkinson's treatment and subsequently, the QoL of the PwP. Addressing financial distress is essential for ensuring access to effective treatment and care of the person with Parkinson’s as well as safeguarding the wellbeing of the informal carers. PwPs and their families face increased financial burden due to rising out-of-pocket payments to meet healthcare needs including procuring specialized equipment or making modifications in the house / living arrangements to support the PwP with their activities of daily living. Rehabilitation, exercise to loosen joint structures and motion exercises to prevent deformities may add to the expenses for using private physiotherapy and occupational therapy together with procuring specialised equipment to improve body movements. This is over and above prescription / medication expenses.
Costs to cares and lost income due to disability adds to the financial strain. Household expenses augmented with loss of household income in providing care, adds to the distress.
Thus, physical and psychological wellbeing which is already affected by the diagnosis of Parkinson’s itself, and its progression, has a compounding effect because of financial distress caused by out-of-pocket expenses and loss of income. PwP and their carers often are required to reduce working hours or take premature retirement due to ill health and caring responsibilities, respectively.
The main objective of this paper is to examine the impact of financial distress on PwP households with respect to their quality of life, and psychological wellbeing. We have also explored how financial distress affects the quality of life of their informal caregivers
1. Additionally, the study also assesses the influence of socioeconomic background and demographic profile of PwP on their quality of life, and psychological wellbeing using multivariate regression models. This epidemiological study is undertaken in the United Kingdom.
The paper is organised into six sections: Section 2 explain the health economics evaluation framework in the context of economic costs to PwP, their carer and all other stakeholders. Section 3 explains the methodology adopted to estimate financial distress and the patterns in socioeconomic and demographic profile of PwP and their caregivers. Section 4 discusses the patterns in QoL of PwP and their carers by the magnitude of financial distress. Section 5 presents the regression results, which gives insights into the association of financial distress with that of QoL and physical as well as psychological wellbeing of PwP. The key findings of this study are highlighted in section 6; and the policy prescriptions to improve the QoL and wellbeing of PwP and their caregivers are discussed in the same section.
Health Economics Evaluation Framework
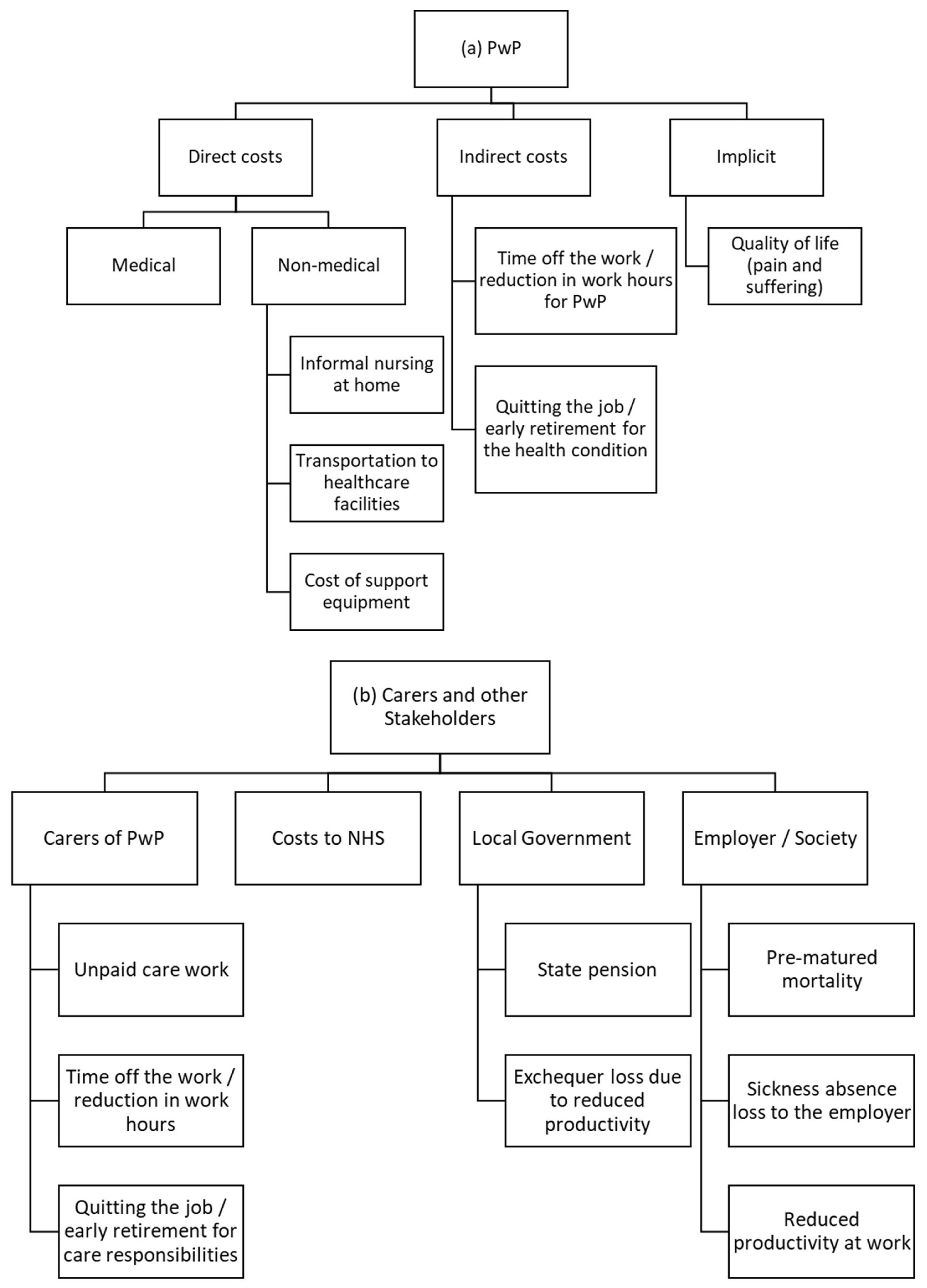
Costs to persons living with Parkinson’s (PwP), NHS, Local Government and employer / society are estimated using the health economics evaluation framework. This study focuses largely on costs to PwPs and their caregivers. Costs are further segregated into direct costs, indirect costs and implicit costs.
Flowcharts 1 (a) and (b) display the economic costs to PwP, their caregivers and other stakeholders.
In this study, we focus only on the costs to PwP and their caregivers for estimating the financial distress. Since the objective of our study is to examine the impact of financial distress on PwP and their informal carers, we have not taken into consideration, the costs to NHS, local government or the society / employer.
Methods and Data
This study employs a cross-sectional design and administers a questionnaire for collecting data on health and living conditions, socioeconomic status, key items on economic and financial costs and quality of life (QoL) of PwP and their caregivers. QoL is measured using the EuroQoL EQ-5D-5L questionnaire and then Quality Adjusted Life Years (QALY) is estimated using England population weighting (N. Devlin et al., 2016; N. J. Devlin & Brooks, 2017; EuroQol Research Foundation, 2019). The sampling method and sample size are discussed in details in Gumber et al., (2017)
2; this paper is an extension of that study. Their study had adopted a mixed-methods approach, of administering a questionnaire as well as in-depth interviews. However, in this paper, we make use of the data collected using questionnaire only.
A questionnaire was administered on 776 PwPs and 546 carers, across all four countries of the United Kingdom during 2015-16. However, this had resulted in an over-representation of respondents of White ethnicity and therefore, a booster sample of 41 PwPs and their 37 carers belonging to Black and Minority Ethnicity (BME) was drawn from Manchester and Sheffield areas.
This questionnaire was administered to collect data on socioeconomic and demographic profile of PwP and their carers. The data on different components of costs to PwP, their carers and other stakeholders were also collected using this questionnaire. Data were collected, for PwP and their carers, through both, online and postal questionnaires, as per the choice of the respondent.
Table 1 gives an overview of the socioeconomic and demographic profile of these respondents:
Table 1 shows that two-thirds of PwP were men and one-third were women. The level of education for a majority is beyond GCSE (65.5%) and they are currently married (78.6%). Out of a total 546 carers, two-thirds of them were women, mainly spouses of the PwP. A large number of PwP (74%) were not working, of which 23.7% took early retirement due to ill health. Also, 56% of their carers had retired from the workforce, with 11.4% due to caring responsibilities or ill health.
A close to 76% PwP lived either with their spouse or with their children or in an extended family; 14% lived on their own. More than 75% PwP and a close to 75% of their carers had household income less than £30000. Almost 32% persons were living with Parkinson’s had been diagnosed with somewhere between 5-10 years, and a close to 20% between 2-5 years. Apart from the characteristics mentioned in
Table 1, the mean age of caregivers was 62.6 years (as compared to 67.1 years for PwP).
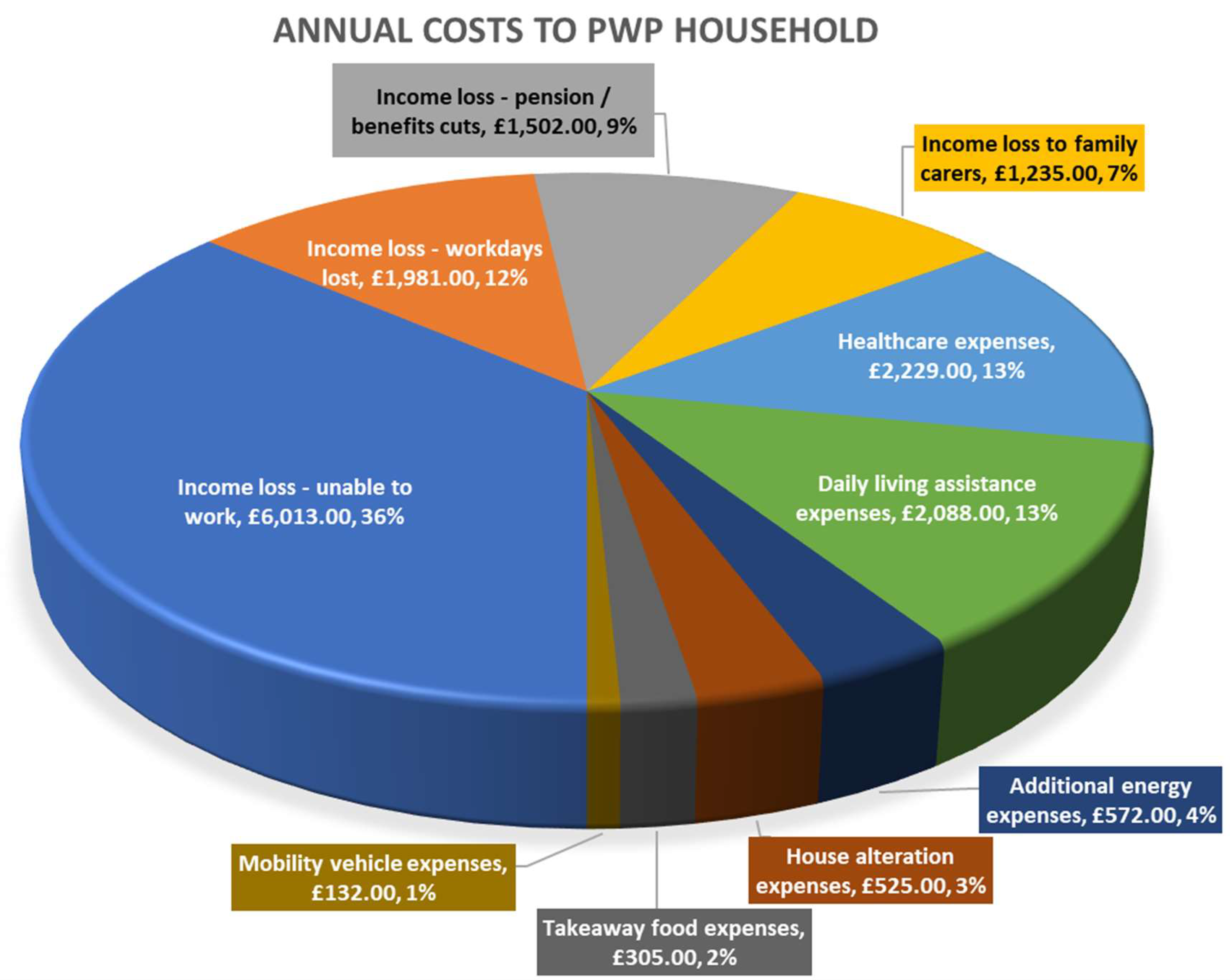
Financial distress to PwP and their carers comprised of 10 components, out of which 6 were different types of expenses, and four of them were because of income loss. PwP and their carers had to either reduce the number of work hours or take a premature retirement because of health and caring responsibilities, respectively.
Health economics evaluation framework, described in the previous section, was used to estimate the annual costs to PwP households (PwP + their caregivers, who are largely, their spouses). The components and the cost of each component can be seen in
Figure 1. Summing up, the annual costs (financial distress) to PwP households work out to £16582.
Psychological wellbeing of PwP and their carers was measured on the following metrics:
EuroQoL EQ-5D-5L,
Visual analogue scale (VAS) for overall health state (ranging between 0 ‘worst’ and 100 ‘best’ health imaginable), and
Wellbeing scores (life satisfaction, worthwhileness, happiness and anxiousness), all measured on 0 to 10 scale, which were adapted from the Office for National Statistics, (2012).
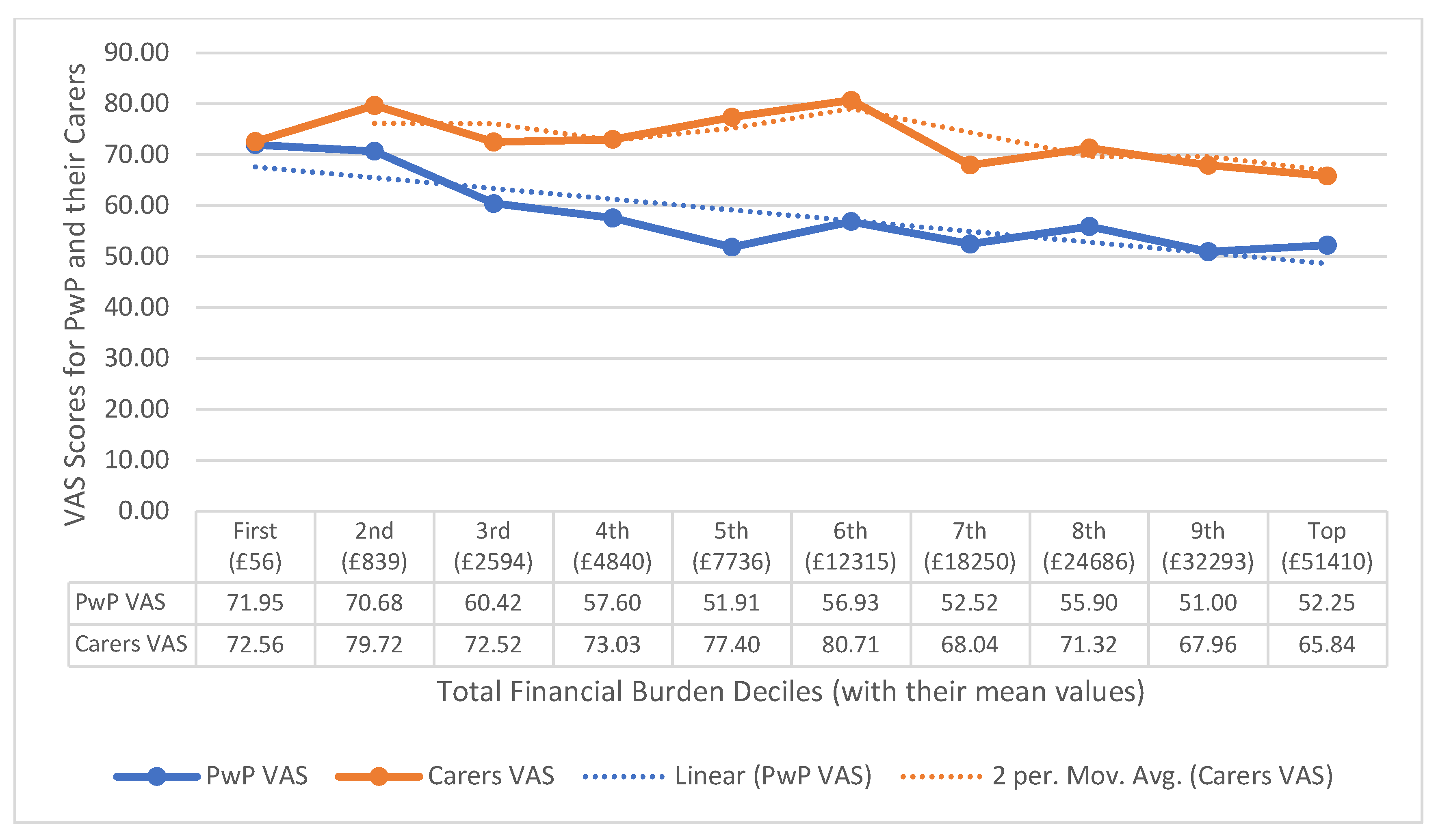
Individual-level QALY were estimated by combining the responses for the five dimensions of Euro-QoL using the weight suggested by N. Devlin et al., (2016). The average QALY score for PwP was 0.576 and that of their carers was 0.674; QALY score of 1 means one year of life in perfect health. The mean Visual Analogue Scale (VAS) score was 57.9 for PwP and that of their carers was 70.1. The QALY and VAS scores are based on the responses from 650 PwP and 301 carers.
Wellbeing scores are based on the responses from 638 PwP and 294 carers. The mean wellbeing score for PwP was 5.3 for satisfaction with life, 5.5 for how happy they felt yesterday. The corresponding wellbeing scores for their carers were 5.7 for satisfaction with life and 5.8 for happiness.
QoL and wellbeing scores for PwP and their carers are discussed in detail, in the following section.
Impact (Determinants) of Financial Distress on QoL and Wellbeing of PwPs
The principal objective of this study is to examine how financial distress and socioeconomic background and demographic profile influences the wellbeing scores of PwPs. Therefore, four separate regressions were undertaken to examine the effect of financial distress and socioeconomic background and demographic profile on (1) QALY, (2) VAS Scores, (3) life satisfaction scores and (4) happiness (wellbeing) scores of PwP only (and not their carers).
The predictors for all the four models are the same to ensure comparability of the predictors on various psychological wellbeing indicators. The outcome variables are: (1) quality of life as estimated using the EQ-5d-5L questionnaire, (2) VAS Scores, (3) Life satisfaction score, and (4) Happiness score.
There are 12 predictors to each of these four regression equations. Out of these 12 predictors, demographic characteristics of the PwP are explained by age and gender (male and female). Social characteristics of PwP are represented by marital status, education and ethnicity (Whites or Non-Whites). Economic status of a PwP is represented by house ownership (owned or otherwise), working or not / retired) and their household income categories. Disease specific predictors are number of years since the diagnosis of Parkinson’s, number of medications for Parkinson’s treatment and number of visits to healthcare professionals / services. Financial distress predictors are out-of-pocket payments, and income loss. However, the actual calculations of out-of-pocket expenditures and income losses are added to arrive at the total estimate of financial distress and then categorised into deciles.
The regression equation is given in equation 1:
where,
= QoL scores for the first regression,
VAS scores the second regression,
Life satisfaction scores for the third, and
Happiness scores for the fourth regression equations.
Predictors:
= actual age of the PwP
= dichotomous categorical: male and female (reference category: female),
= dichotomous categorical: married and not married / single (reference category: not married / single),
= dichotomous categorical: higher education or otherwise (reference category: other than higher education),
= dichotomous categorical: whites and BMEs (reference category: whites),
= dichotomous categorical: owned and not owned (reference category: house not owned by the PwP),
= dichotomous categorical: working and not-working (including retired) (reference category: not working),
= six categories of income ranging from less than £10,000 to £50,000 and more, and a seventh category of PwP who did not disclose their income (reference category: income not reported),
= number of years since diagnosis of Parkinson’s, categorised into six groups ranging from less than 2 years to more than 20 twenty years (reference category: less than 2 years),
= number of visits to healthcare professional / services in a year,
= number of medications for Parkinson’s and other long-term conditions,
= deciles of the total of out-of-pocket expenses + income loss, with lowest mean expenses in the first decile, which increase with the deciles and the highest mean expenses in the 10th decile (reference category: 1st decile)
Beta coefficients
= intercept coefficient
to are the slope coefficients of the respective predictors.
It may be noted that the quadratic term for age in the equation is used because it is observed that the QoL, VAS and wellbeing would decrease sharply after stage 3 (Parkinson’s Community Help, 2021). Moreira et al., (2017) also observed that the quality of life and wellbeing decrease sharply after moderate Parkinson’s (that is eight years or more since the diagnosis), whereas mild Parkinson’s did not have any effect on the QoL or wellbeing. They further observed that the QoL was affected by stigma, decline in cognition, increased impairment in mobility and ADL. Using a quadratic term implies that we hypothesise improved quality of life in early years of diagnosis and that is because physiotherapy intervention and rehabilitation exercises in early stages would improve the mobility and delays the impairment in ADL (Cholewa et al., 2014; Tomlinson et al., 2012).
The regression results are in
Table 2:
Regression results from
Table 2 show that:
Demographic indicators: None of the QoL score, VAS and wellbeing scores
3 are found significant across gender or marital status. Gender is classified as male and female, and marital status as married / cohabiting and singles (including divorced, widowed, separated). QoL scores, VAS and life satisfaction increases to an extent with age, and then falls. The non-linear relationship with age was highly significant for three out of four models. The magnitude of life satisfaction score declines continuously with increase in the duration of Parkinson’s since the diagnosis. This means that Parkinson’s diagnosis influences life satisfaction the most as compared to other QoL and wellbeing scores.
Social indictors: QoL score, VAS and life satisfaction scores are significant for education. PwP with higher education have these scores higher by 0.1 (0.09 to 0.11) standard deviations (sd) as compared to those below this level of education. This include no formal education, attended school but did not complete, completed school with or without qualification, educational qualification beyond school and other levels of education. Only VAS scores are significant across ethnicity (whites versus BME). Compared to whites, VAS score of BME is lower by 0.084 sd. BME (Black & Minority Ethnic) group include Asian / Asian British, Black/African/Caribbean/Black British, Mixed / Multiple ethnic groups and other non-whites.
Economic indicators: All four scores – QoL, VAS and wellbeing – are higher for PwP with own house by 0.11 to 0.14 sd as compared to those without, and for working PwP by 0.07 to 0.11 sd as compared to non-working. Own house includes own with and without mortgage and also shared owned. All other are housing association tenants (sheltered or non-sheltered), local authority tenants (sheltered or non-sheltered), private renters, living with parents / partners / children / friends, residing in a residential / nursing home, no fixed abode and other non-owners of the house. Working PwP include all those who are employed full-time, part-time or self-employed. Non-working PwP include all those who are unemployed, not working or retired early because of illness / incapacity or for caring responsibilities or retired because of age, pensioners, and homemakers. Only QoL and VAS scores are significant for income-group: compared to those who have not disclosed their annual income, the QoL score of those with an income of £50,000 or more, is higher by 0.093 sd, and VAS score is higher by 0.076 sd for the income-group £30,000 - £39,999. However, wellbeing scores are not influenced by income.
Parkinson’s specific: All the four scores worsen for persons diagnosed with Parkinson’s for 10 years or more, as compared to those diagnosed for less than 2 years. There is no difference in any of the QoL, VAS or wellbeing scores for persons diagnosed with Parkinson’s for less than 10 years as compared to those diagnosed with it for less than 2 years. QoL scores worsen by 0.22 sd for people diagnosed with Parkinson’s between for 10-15 years, and then relatively improve for those diagnosed with Parkinson’s for 15 to 20 years and more. VAS and happiness scores worsen for 10-15 years, relatively improve for 15-20 years and again worsen but not as much, for people diagnosed with Parkinson’s for 20 years or more. This corroborates with our finding of inverted-parabolic relationship of QoL and wellbeing with age. However, life satisfaction worsens with every one sd for additional years of living with Parkinson’s since diagnosis. QoL, VAS and wellbeing scores worsen between 0.14 to 0.20 sd with each sd in additional visit to health services. Number of medications is a part of healthcare expenses. Number of medications means the number of prescribed medications; 38% PwP were on one of two medications, while 1.5% were not prescribed any medication. This is despite 6.19% PwP had other long-term conditions (LTCs) but not on medications. On the other extreme, 4% were prescribed more than 10 medications. This is because 39.56% PwP were being treated for other LTCs like diabetes, blood pressure, angina, and other cardiovascular diseases. There is no significant effect of number of medications on either of these QoL or wellbeing scores.
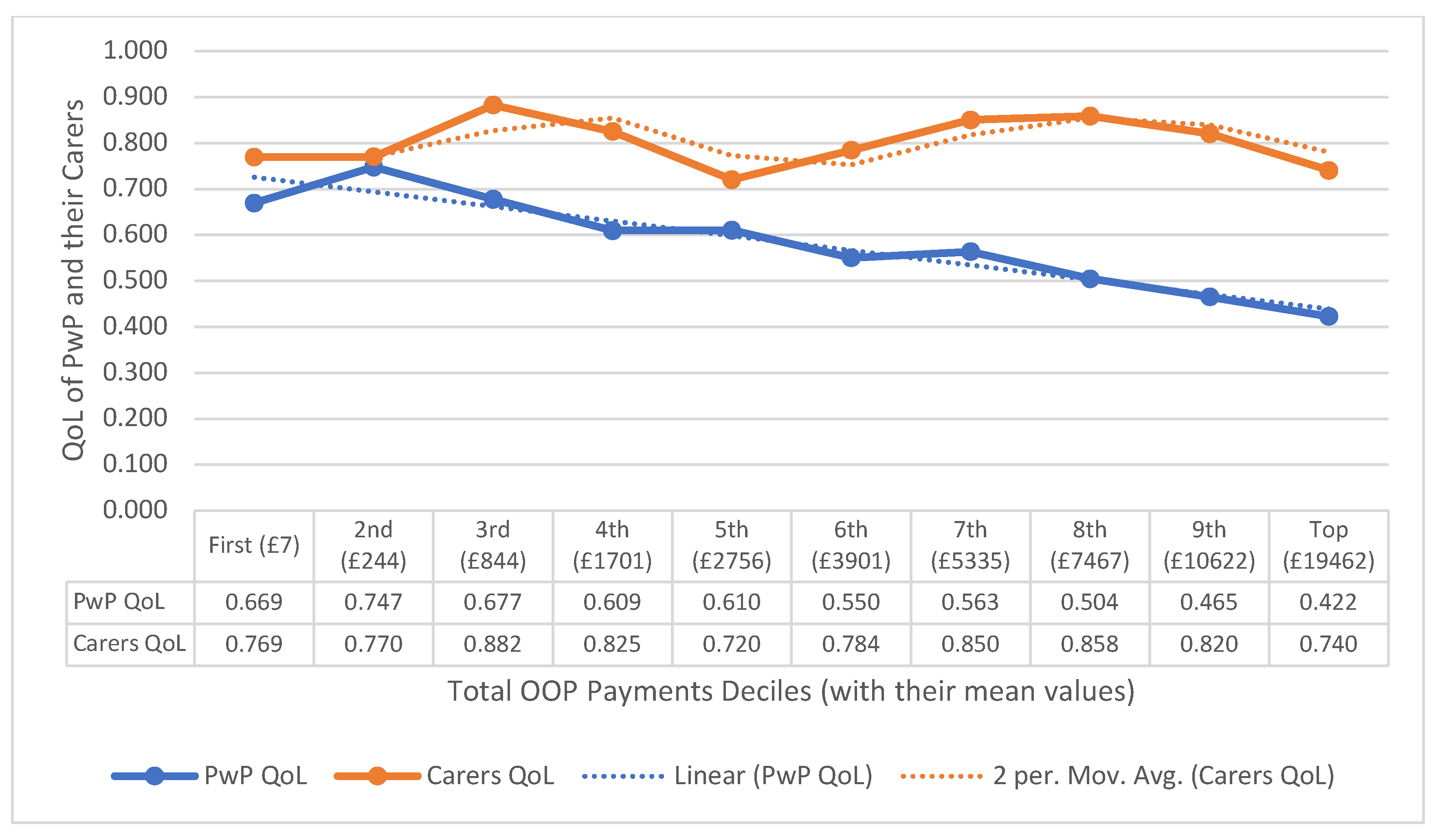
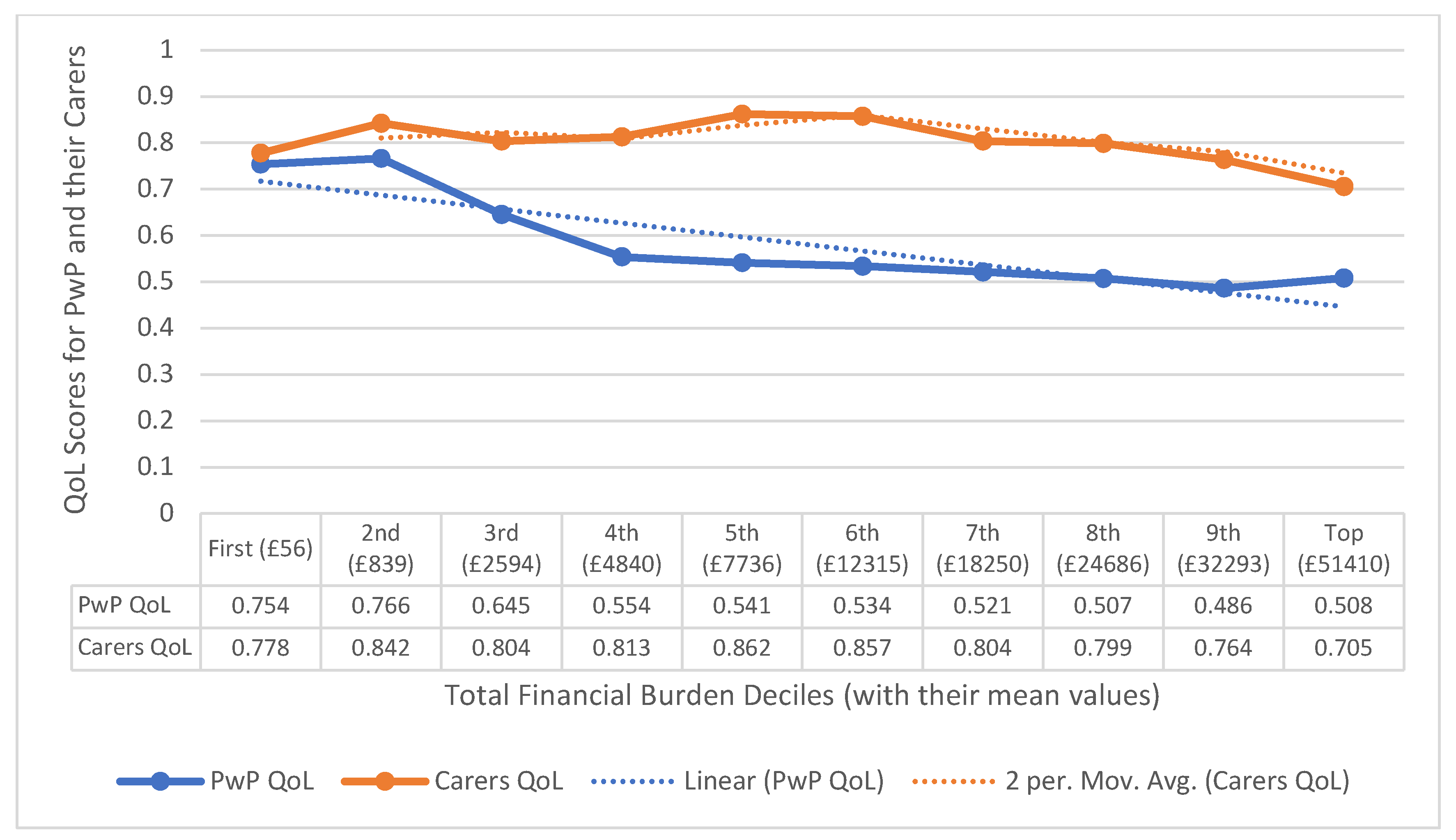
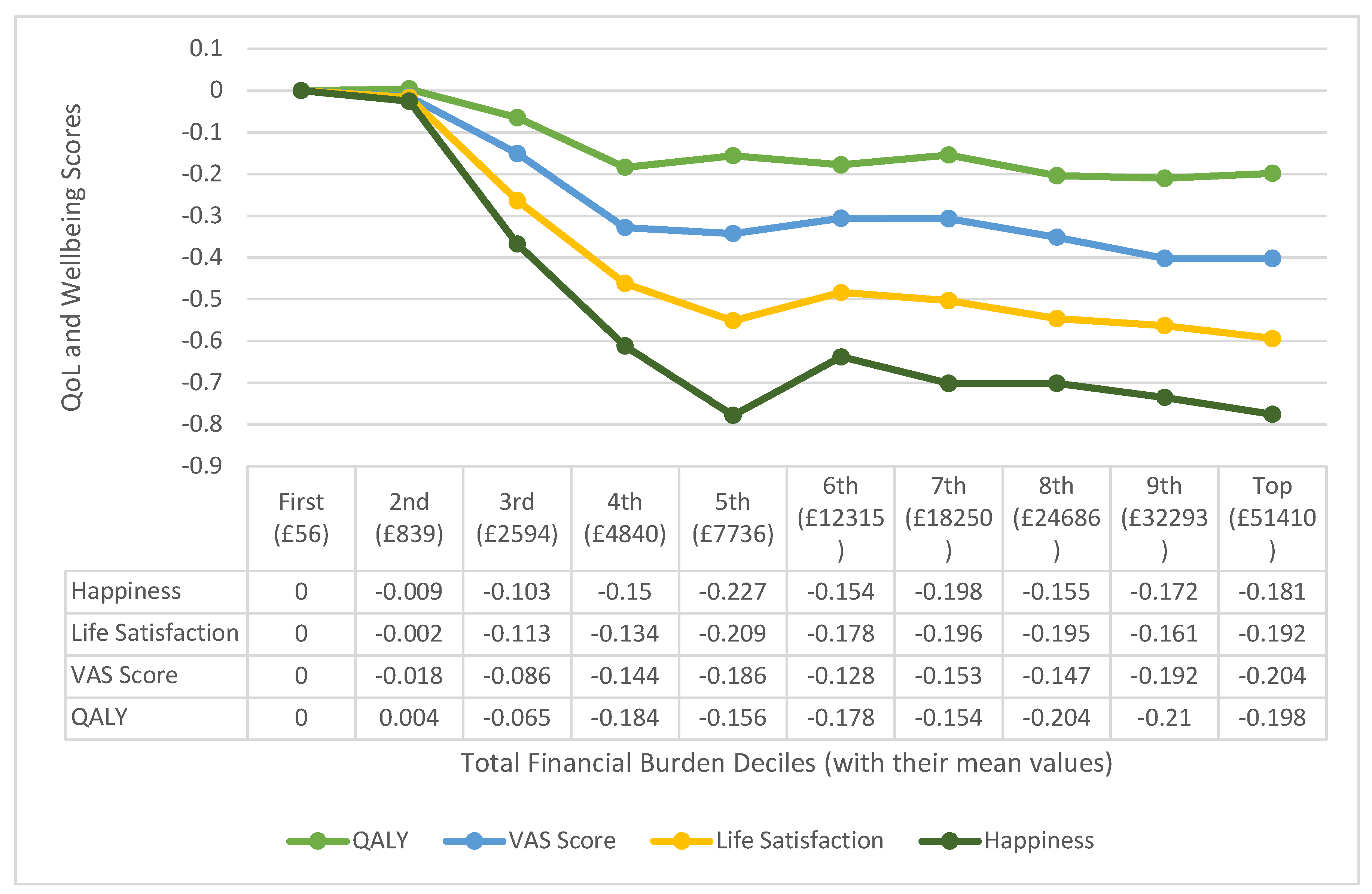
Financial Distress: Average financial burden to PwP works out to £16,582 per year per household. However, for the regression purpose, we categorised the financial burden into deciles; the mid-points (mean values) of financial burden for each decile is shown against the decile in
Figure 5 (legend on X-axis).
Beta coefficients also show that age has the strongest impact on all the QoL and wellbeing scores. QoL and VAS are also affected by more number of years elapsed since diagnosis and higher deciles of financial burden. Life satisfaction and happiness are influenced the most by the financial distress.
The effect sizes of all the four QoL as well as wellbeing indicators with financial burden is shown in
Figure 5. It can be seen that except for the 2
nd and 3
rd deciles for both QALY and VAS, the coefficients are statistically significant for all other deciles of financial burden. It can also be observed that the QoL for PwP in 8
th and 9
th deciles are the worst affected in comparison with that of those in the first decile (the reference group). VAS is worst affected for 9
th and 10
th deciles. The coefficients for life satisfaction and happiness scores are statistically significant for all deciles of financial burden, except the 2
nd.
Figure 5 further shows that life satisfaction score is affected the most for PwP in 5
th, 7
th and 8
th deciles of financial burden. Happiness scores are worst affected for the PwP in the 5
th decile of financial burden. Overall, it can be seen that all the scores – QoL, VAS and wellbeing – largely worsen with increase in financial burden, 4
th decile onwards.
Limitations of the Study
This study in a community setting has adopted a household-based approach and therefore, PwP living in institutional settings such as rehabilitation centres, hospitals and care homes could not be included. These are largely PwP with severe conditions. Therefore, there is an under-representation of PwP with severe conditions in this study. As a result there is an under-estimation of such associated institutional and personal cost. The study has also not computed any cost of premature mortality due to Parkinson’s and thus the economic and financial burden is entirely based on the survived PwP and the management of their disease condition.
Carers might have an increased need for healthcare services, as compared to them not having the caring responsibility. Carers have reported increased morbidity and deterioration of QoL because of caring responsibilities. This could be because of additional work burden and emotional distress. This can have a negative multiplier effect on costs of healthcare. In this study, we have not taken into consideration, these consequential costs.
Key Findings and Policy Recommendations
Annual average cost of Parkinson's care is £16,582, and that is a huge strain on their limited income. Most PwP households surveyed had an annual income under £30,000. Financial distress caused by this income-expenditure gap can significantly affect the treatment and management of Parkinson's in the UK, resulting in further deterioration of quality of life and wellbeing of PwP. The findings of this study show that there is an increased impact on the QoL of PwP with the progression of Parkinson’s. Also, both QoL and wellbeing scores have negative association with the financial burden, implying a deteriorated quality of life and wellbeing of PwP with increase in financial burden.
There is no known cure for Parkinson’s. Therefore, addressing financial barriers is essential for ensuring equitable access to quality care for PwP. Various support programs like employment and support allowance, and carer’s allowance are already available to assist PwP with financial constraints. Charities could be encouraged to offer assistance programs for PwP, by introducing government schemes to provide financial aid. Social workers and healthcare professionals could be encouraged to help PwP navigate available resources.
Financial distress can lead to anxiety, depression, and overall mental health decline in people with Parkinson's. Comprehensive care for Parkinson's should include mental health support alongside medical treatment. Pontone et al., (2019) has found that raising awareness of mental healthcare needs, and promoting integrated speciality mental healthcare would help improve the QoL of PwP. Comprehensive support programs, advocacy efforts, and mental health services are key components in addressing financial distress in Parkinson's treatment.
Advocacy efforts are crucial also for raising awareness about the financial challenges faced by PwP, and the already available benefits for PwP with financial needs. Collaboration between PwP and their carers, advocacy groups, healthcare providers, and policymakers is essential to access the demand and supply of financial support, estimate the gap and take necessary steps to reduce the gap. Policy provisions to improve access to healthcare should aim at reducing out-of-pocket medication expenses and travel costs of healthcare visits.
Considering that Parkinson’s is not curable, continued research and innovation in Parkinson's treatment may focus on more affordable, accessible and effective therapies. Dodel et al., (2021) estimated that treatment intervention for Parkinson’s had a cost savings between €1800 and €7600 with 0.10 QALY for the United Kingdom. They estimated the incremental cost effectiveness ratio (ICER) of adequate treatment availability to be €15,000 to €32,600 across country
4 settings. Target adherence to treatment would save €917,000–€2,980,000 (UK) for every 1,000 patients treated adequately. Ensuring effective and adequate treatment, augmented with lifestyle changes can help further slow the progression and eventually, reduce the financial distress. Studies (Janssen Daalen et al., 2022; Marras et al., 2019; Veronese et al., 2024) have examined and identified some lifestyle factors that helps in progression of prodromal to manifest Parkinson’s, and progression of Parkinson’s.
Provision for person-centered care (PCC) at home is advocated for PwP. This helps people at different stages of Parkinson’s, from different ethnicities and cultures to access care suited to their needs. PCC could apparently appear to be expensive, but it could increase the quality of life and wellbeing of a PwP, resulting in slow progression of Parkinson’s, which could lead to reduced costs over the lifetime of a PwP.
Bhimani, (2014) further observes the need for reposing trust in palliative care. Caring for PwP in advance stages could affect QoL and wellbeing of carers. Our study shows that a majority of the carers are spouses, who not only get physically distressed but also emotionally disturbed seeing their loved ones in advanced stages of Parkinson’s. Since Parkinson’s progresses with age, the spouses also age alongside their PwP partners. Affordable and reliable palliative care can help improve the QoL and wellbeing of both PwP and their carers.
While this study is focused on examining the effect of financial distress on QoL and wellbeing of PwP, we also broadly looked at the QoL of carers with increased out-of-pocket payments and overall financial burden. Our study shows that QoL of carers seem to decline after an unbearable threshold level of financial burden experienced. Additionally, carers were also found to have an average wellbeing score lower as compared to that of general population because they too experience financial stress and burden (Gumber et al., 2017). We recommend providing financial resources and support also for carers of PwP. Respite care services and caregiver assistance programmes are required to be implemented, to alleviate financial strain. Giles et al., (2015) have observed that there is a huge demand-supply gap for respite care, especially for PwP in moderate and advance stages. The need for respite care would increase by the number of years and stage of Parkinson’s. However, Rosqvist et al., (2022) found that there is a demand for respite care but people prefer the informal care route for respite because of their apprehensions about the quality of care in respite care facilities. Bhimani, (2014) observes that respite care is often not sought for, because of the additional costs. As discussed, PwP already bear the burden of increased expenditure because of their condition. The demand-supply gap for respite care could be bridged partially by making it affordable and accessible. Undertaking measures to reposing trust about respite care could help PwP and their carers avail of these services, thereby, reducing fatigue and improving their QoL and wellbeing.
In nutshell, Parkinson’s is a progressive neurodegenerative condition, which deteriorates with age, resulting in reduced quality of life and wellbeing of PwP and their caregivers. This also results in increased financial burden to PwP household. Financial distress arising out of out-of-pocket expenditure can add to deterioration of QoL and wellbeing of PwP and their carers and consequently drag them into vicious circle of distress. Appropriate policy measures like financial support programmes, respite care for carers, creating awareness about lifestyle factors for prevention and slowing down the progression of Parkinson’s as well as person-centric care could be some responses to address financial distress and improve the QoL and wellbeing of PwP and their caregivers.
References
- Bhimani, R. (2014). Understanding the Burden on Caregivers of People with Parkinson’s: A Scoping Review of the Literature. Rehabilitation Research and Practice, 2014(1), 718527. [CrossRef]
- Chaudhuri, K. R., Azulay, J.-P., Odin, P., Lindvall, S., Domingos, J., Alobaidi, A., Kandukuri, P. L., Chaudhari, V. S., Parra, J. C., Yamazaki, T., Oddsdottir, J., Wright, J., & Martinez-Martin, P. (2024). Economic Burden of Parkinson’s Disease: A Multinational, Real-World, Cost-of-Illness Study. Drugs - Real World Outcomes, 11(1), 1–11. [CrossRef]
- Cholewa, J., Gorzkowska, A., Szepelawy, M., Nawrocka, A., & Cholewa, J. (2014). Influence of functional movement rehabilitation on quality of life in people with Parkinson’s disease. Journal of Physical Therapy Science, 26(9), 1329–1331. [CrossRef]
- Devlin, N. J., & Brooks, R. (2017). EQ-5D and the EuroQol Group: Past, Present and Future. Applied Health Economics and Health Policy, 15(2), 127–137. [CrossRef]
- Devlin, N., Shah, K., Feng, Y., Mulhern, B., & van Hout, B. (2016). Valuing Health-Related Quality of Life: An EQ-5D-5L Value Set for England: Vol. Research Paper 16/01. Office of Health Economics.
- Dodel, R., Tinelli, M., Deuschl, G., Petersen, G., Oertel, W., & Ahmerkamp-Böhme, J. (2021). The economic benefit of timely, adequate, and adherence to Parkinson’s disease treatment: The Value of Treatment Project 2. European Journal of Neurology, 28(2), 707–716. [CrossRef]
- EuroQol Research Foundation. (2019). EQ-5D-5L User Guide [Dataset]. https://euroqol.org/publications/user-guides.
- Findley, L., Aujla, M., Bain, P. G., Baker, M., Beech, C., Bowman, C., Holmes, J., Kingdom, W. K., MacMahon, D. G., Peto, V., & Playfer, J. R. (2003). Direct economic impact of Parkinson’s disease: A research survey in the United Kingdom. Movement Disorders, 18(10), 1139–1145. [CrossRef]
- Findley, L. J. (2007). The economic impact of Parkinson’s disease. Parkinson’s Disease: From Premotor Symptoms to New Treatment Strategies, 13, S8–S12. [CrossRef]
- Findley, L. J., Wood, E., Lowin, J., Roeder, C., Bergman, A., & Schifflers, M. (2011). The economic burden of advanced Parkinson’s disease: An analysis of a UK patient dataset. Journal of Medical Economics, 14(1), 130–139. [CrossRef]
- Giles, M., Thomas, M., & Lewin, G. (2015). Ageing Intensifies the Care Needs of Adults Living with Parkinson ’s Disease and their Carers. Ageing International, 40(4), 338–352. [CrossRef]
- Gumber, A., Ramaswamy, B., Ibbotson, R., Ismail, M., Thongchundee, O., Harrop, D., Allmark, P., & Rauf, A. (2017). Economic, Social and Financial Cost of Parkinson’s on Individuals, Carers and their Families in the UK. Centre for Health and Social Care Research, Sheffield Hallam University.
- Gumber, A., Ramaswamy, B., & Thongchundee, O. (2019). Effects of Parkinson’s on employment, cost of care, and quality of life of people with condition and family caregivers in the UK: a systematic literature review. Patient Related Outcome Measures, 10(null), 321–333. [CrossRef]
- Henry, R. S., Lageman, S. K., & Perrin, P. B. (2020). The relationship between Parkinson’s disease symptoms and caregiver quality of life. Rehabilitation Psychology, 65(2), 137–144. [CrossRef]
- Janssen Daalen, J. M., Schootemeijer, S., Richard, E., Darweesh, S. K. L., & Bloem, B. R. (2022). Lifestyle Interventions for the Prevention of Parkinson Disease. Neurology, 99(7_Supplement_1), 42–51. [CrossRef]
- Marras, C., Canning, C. G., & Goldman, S. M. (2019). Environment, lifestyle, and Parkinson’s disease: Implications for prevention in the next decade. Movement Disorders, 34(6), 801–811. [CrossRef]
- McCrone, P., Allcock, L. M., & Burn, D. J. (2007). Predicting the cost of Parkinson’s disease. Movement Disorders, 22(6), 804–812. [CrossRef]
- Modugno, N., Antonini, A., Tessitore, A., Marano, P., Pontieri, F. E., Tambasco, N., Canesi, M., Fabbrini, G., Sensi, M., Quatrale, R., Solla, P., Defazio, G., Melzi, G., Gualberti, G., & Lopiano, L. (2020). Impact of Supporting People with Advanced Parkinson’s Disease on Carer’s Quality of Life and Burden. Neuropsychiatric Disease and Treatment, 16(null), 2899–2912. [CrossRef]
- Moreira, R. C., Zonta, M. B., Araújo, A. P. S. de, Israel, V. L., & Teive, H. A. G. (2017). Quality of life in Parkinson’s disease patients: Progression markers of mild to moderate stages. Arquivos de Neuro-Psiquiatria, 75.
- Office for National Statistics. (2012). First Annual ONS Experimental Subjective Well-being Results. https://webarchive.nationalarchives.gov.uk/ukgwa/20160106195128/http://www.ons.gov.uk/ons/rel/wellbeing/measuring-subjective-wellbeing-in-the-uk/first-annual-ons-experimental-subjective-well-being-results/first-ons-annual-experimental-subjective-well-being-results.html.
- Parkinson’s Community Help. (2021). "The Parkinson’s Journey: Understanding Progression” – Webinar Notes. Stanford Medicine: Stanford PD Community Blog. https://parkinsonsblog.stanford.edu/2021/09/the-parkinsons-journey-understanding-progression-webinar-notes/.
- Parkinson’s UK. (2023). The cost of Parkinson’s: The financial impact of living with the condition. https://www.parkinsons.org.uk/sites/default/files/2017-07/CS2547%20Cost%20of%20Parkinson%27s%20report%202017%20-%20UK_1.pdf.
- Pontone, G. M., Dissanayaka, N., Dobkin, R. D., Mari, L., Marsh, L., Vernaleo, B. A., Weintraub, D., & Mari, Z. (2019). Integration and Extension of Specialty Mental Healthcare Services to Community Practice in Parkinson Disease. Innovations and Challenges of Training in Geriatric Mental Health, 27(7), 712–719. [CrossRef]
- Rahman, S., Griffin, H. J., Quinn, N. P., & Jahanshahi, M. (2008). Quality of life in Parkinson’s disease: The relative importance of the symptoms. Movement Disorders, 23(10), 1428–1434. [CrossRef]
- Rosqvist, K., Schrag, A., Odin, P., & the CLaSP Consortium. (2022). Caregiver Burden and Quality of Life in Late Stage Parkinson’s Disease. Brain Sciences, 12(1). [CrossRef]
- Santos-García, D., de Deus Fonticoba, T., Cores Bartolomé, C., Íñiguez Alvarado, M. C., Feal Panceiras, M. J., Suárez Castro, E., Canfield, H., Martínez Miró, C., Jesús, S., Aguilar, M., Pastor, P., Planellas, L., Cosgaya, M., García Caldentey, J., Caballol, N., Legarda, I., Hernández Vara, J., Cabo, I., López Manzanares, L., … COPPADIS Study Group. (2022). Predictors of the change in burden, strain, mood, and quality of life among caregivers of Parkinson’s disease patients. International Journal of Geriatric Psychiatry, 37(6). [CrossRef]
- Schrag, A., Jahanshahi, M., & Quinn, N. (2000). What contributes to quality of life in patients with Parkinson’s disease? Journal of Neurology, Neurosurgery & Psychiatry, 69(3), 308. [CrossRef]
- Tomlinson, C. L., Patel, S., Meek, C., Herd, C. P., Clarke, C. E., Stowe, R., Shah, L., Sackley, C., Deane, K. H. O., Wheatley, K., & Ives, N. (2012). Physiotherapy intervention in Parkinson’s disease: Systematic review and meta-analysis. BMJ (Clinical Research Ed.), 345, e5004. [CrossRef]
- Trend, P., Kaye, J., Gage, H., Owen, C., & Wade, D. (2002). Short-term effectiveness of intensive multidisciplinary rehabilitation for people with Parkinson’s disease and their carers. Clinical Rehabilitation, 16(7), 717–725. [CrossRef]
- Veronese, N., Nova, A., Fazia, T., Riggi, E., Yang, L., Piccio, L., Huang, B.-H., Ahmadi, M., Barbagallo, M., Notarnicola, M., Giannelli, G., De Pergola, G., Stamatakis, E., Cereda, E., Bernardinelli, L., & Fontana, L. (2024). Contribution of Nutritional, Lifestyle, and Metabolic Risk Factors to Parkinson’s Disease. Movement Disorders, 39(7), 1203–1212. [CrossRef]
- Weir, S., Samnaliev, M., Kuo, T.-C., Tierney, T. S., Walleser Autiero, S., Taylor, R. S., & Schrag, A. (2018). Short- and long-term cost and utilization of health care resources in Parkinson’s disease in the UK. Movement Disorders, 33(6), 974–981. [CrossRef]
Notes
| 1 |
Informal carers are interchangeably referred to as carers or caregivers in this paper. |
| 2 |
Please refer this report for details on recruitment strategy (overall and for the booster sample) as well as other details of methodology. |
| 3 |
Life satisfaction score and happiness score are jointly referred to as the psychological wellbeing scores. |
| 4 |
Their study was undertaken for the United Kingdom and Germany. |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).