1. Introduction
Lumbar disc herniation (LDH) is a common condition that affects millions worldwide, leading to substantial pain and disability. The development of minimally invasive surgical techniques, such as transforaminal endoscopic lumbar discectomy (TELD), has revolutionized LDH treatment [
1,
2,
3,
4,
5,
6]. The effectiveness of TELD has been validated in several randomized controlled trials [
7,
8,
9,
10], and meta-analyses [
11,
12,
13,
14,
15,
16,
17,
18,
19]. TELD can be performed using a percutaneous posterolateral endoscopic approach under local anesthesia. However, access pain during the transforaminal approach poses a significant technical challenge in this minimally invasive procedure [
20,
21,
22], primarily attributed to the exiting nerve root (ENR) and other neural irritations. Various authors have demonstrated the anatomical configurations that determine access pain or neural irritation in LDH [
23,
24]. Recommendations from other researchers advocate for using surgical tips to reduce pain during the procedure [
20,
25]. Regarding common intracanal (subarticular or central) LDH, the transforaminal approach can be conducted through Kambin’s triangle or a designated safe working zone [
1,
26]. However, for foraminal or extraforaminal LDH, the endoscopic approach may be more challenging [
27]. The rate of significant access pain during TELD is reportedly higher in patients with foraminal LDH than in those with paramedian LDH [
27]. Mechanically, herniated disc fragments typically block or deviate Kambin’s triangle. Chemically, the landing point is inflamed and sensitized. Therefore, the ENR is vulnerable to instrumental manipulation, which may cause significant access pain. Severe access pain may delay the surgical approach and lead to failure. Understanding the factors that contribute to pain during TELD can help surgeons prevent or manage pain before and during the procedure, potentially improving patient outcomes. To our knowledge, no reliable predictive rules for access pain have been established for foraminal or extraforaminal LDH.
This study aimed to predict access pain during TELD for foraminal or extraforaminal LDH and discuss pain prevention and management before and during the procedure. We hypothesized that certain anatomical configurations and patient factors can predict access pain during TELD for foraminal or extraforaminal LDH.
2. Materials and Methods
2.1. Study Design and Patients
This observational study included 73 patients who underwent TELD for foraminal or extraforaminal LDH between January 2017 and December 2022. Patient data were prospectively registered, and their records were retrospectively evaluated. Approval for the study was obtained from our institutional review board (GDIRB2023-210, 24 June 2023), and written informed consent was obtained from the patients. The inclusion criteria were patients with single-level LDH despite >6 weeks of nonoperative treatment or those experiencing unbearable pain and progressive motor deficits. Enrollment of patients with foraminal or extraforaminal LDH was determined based on the LDH zone [
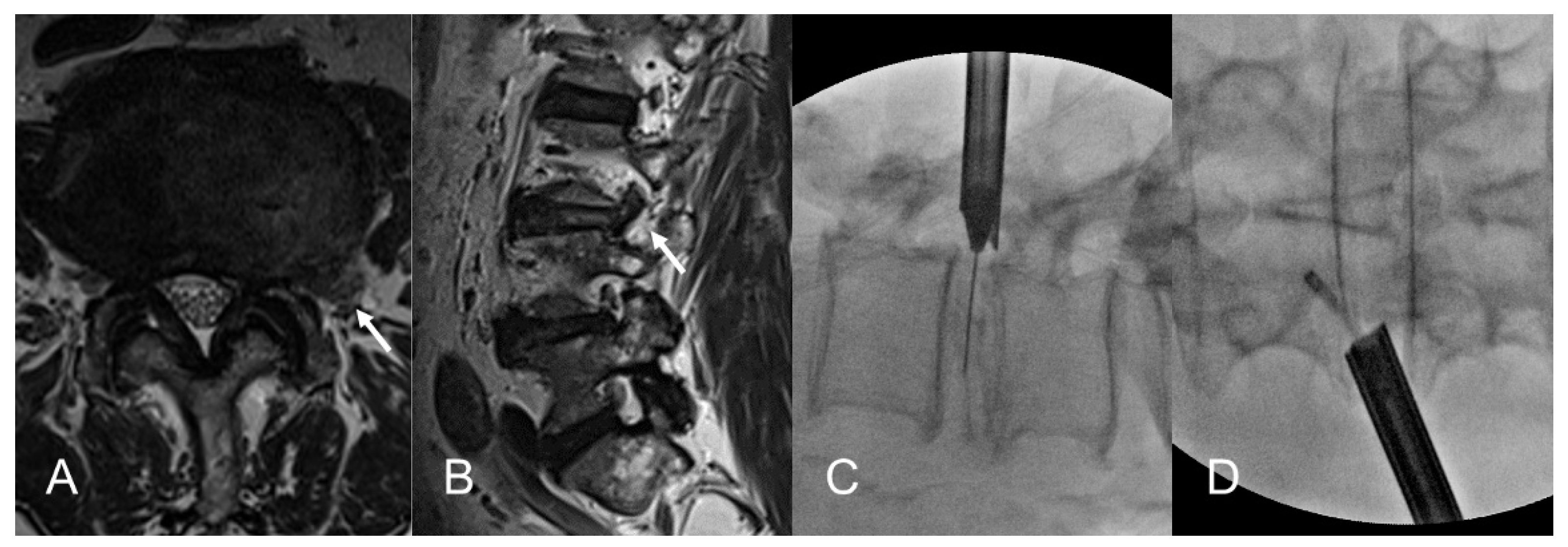
28]. Patients with subarticular or central LDH were excluded from the study. Other exclusion criteria comprised severe central stenosis, segmental instability (including spondylolisthesis), massive cauda equina syndrome, inflammatory disease, infectious disease, and spinal neoplasm. The radiculopathy symptoms were compatible with both the magnetic resonance imaging (MRI) and computed tomography (CT) scan findings (
Figure 1, A and B).
2.2. Surgical Procedure
2.2.1. Patient Preparation
The endoscopic procedure was performed under local anesthesia with conscious sedation according to the standard TELD technique [
3,
20,
27,
29]. Premedication included intramuscular administration of midazolam (0.05 mg/kg) and intravenous administration of fentanyl (0.8 μg/kg). Additional fentanyl doses were administered as necessary, depending on the patient’s vital signs and sedation level. The patient was then positioned prone on a radiolucent spine table.
2.2.2. Transforaminal Approach under Fluoroscopic Guidance
An 18-G needle was percutaneously inserted posterolaterally with about a 45º angle under fluoroscopic guidance. The approach angle and insertion point were determined based on the body size and zone of the LDH. The primary goal of this posterolateral approach is safe landing close to the herniated disc fragment with minimal access pain. The needle was inserted into the disc through the foraminal window to prevent ENR irritation after a preemptive epidural block. Intraoperative discography was performed using contrast medium and indigo carmine to stain the nucleus and herniated fragments. Subsequently, a sequential dilation technique was used until the working sheath was docked at the foraminal zone, outside, or inside the disc surface (
Figure 1, C and D).
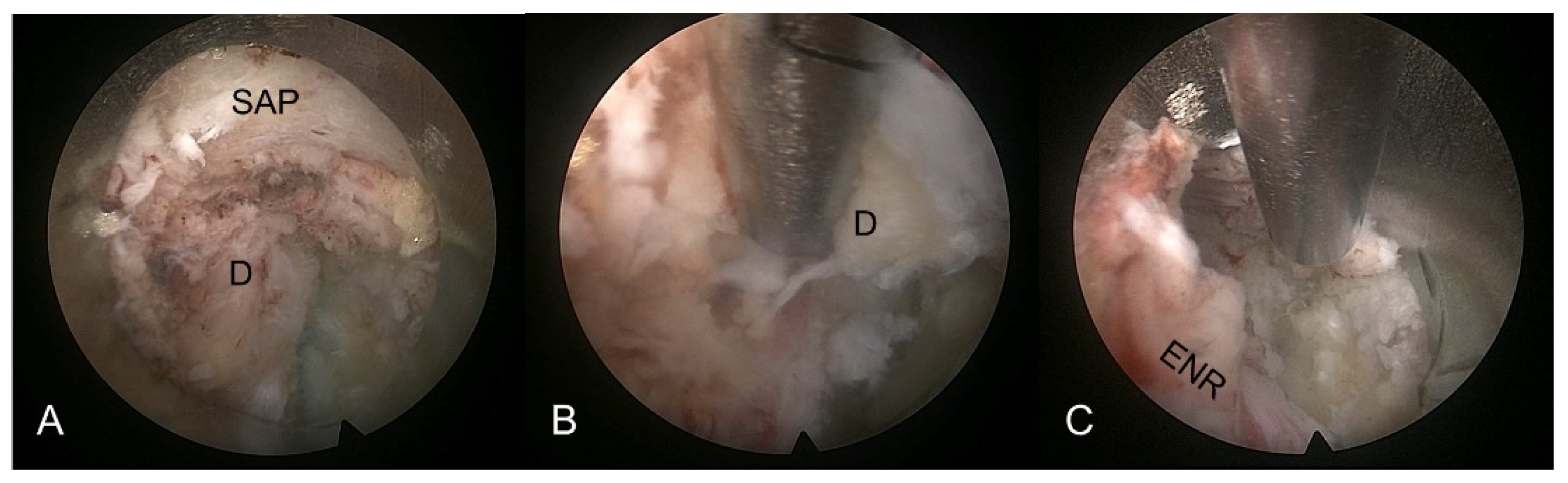
2.2.3. Selective Discectomy under Endoscopic Visualization
An oval-shaped working channel endoscope was introduced through the working sheath, initiating selective discectomy under endoscopic visualization. Decompression was performed by visualizing anatomical structures from the posterolateral aspect. The initial view included the foraminal disc surface, perineural fat, and the ENR course. The herniated disc fragment and neural tissues could be visualized and distinguished using instrumental dissection with a probe, forceps, and a radiofrequency tip. The herniated fragment compressing the nerve root usually adhered to the tenacious fibrotic annular anchorage. After delicately releasing the annular anchorage, the herniated disc fragment was freed and removed using grasping forceps and radiofrequency. During selective discectomy, epidural bleeding or inflamed tissues were controlled using radiofrequency coagulation and hemostatic agents. As the dissection and removal maneuvers proceeded, the nerve root and dural sac were visualized and released. The entire fragment, including the hidden intradiscal portion, was removed. Any remaining fragment of the “iceberg” may cause an incomplete decompression or postoperative recurrence. Sufficient annular release and removal of the entire herniated disc are primary keys to success (
Figure 2).
2.2.4. Postoperative Management
The endpoint of the procedure was determined by free mobilization and pulsation of the nerve root and dural sac after sufficient discectomy. After the procedure, patients were checked for adverse events before discharge. Postoperative MRI or CT scans can be considered as required.
2.3. Evaluation
Patient demographic data, including age, sex, body mass index (BMI), and symptom duration, were documented. Preoperative radiographic information included the level, zone (foraminal or extraforaminal), degree of disc herniation (bulging or diffuse herniation, protrusion, extrusion, and sequestration), and presence of neural anomalies (conjoined nerve root or low-lying nerve root). The foraminal nerve root impingement grade was measured using the Lee classification system [
30,
31].
The primary outcome was access pain, which was prospectively evaluated in all patients. Access pain was defined as mechanical or neural pain experienced during the transforaminal approach under local anesthesia. Such pain may have been caused by irritation of the ENR by the approaching needle, dilators, or working sheath when they touch or pass through a foraminal window. Pain intensity of the access pain during TELD was classified into a four-point scale according to a published article [
27]: 1) minimal (no or negligible irritation response), 2) mild (mild but tolerable, visual analog scale (VAS) 1–3), 3) moderate (definitive complaint of pain, VAS 4–6), and 4) severe (screaming and twisting in pain, VAS >6). Moderate or severe pain was considered “significant.”
Operative data, including operative time, length of hospital stay, and adverse events, were documented as secondary outcomes. The clinical outcomes were assessed using patient-based outcome questionnaires. These questionnaires were administered during outpatient office visits and telephone interviews. Global clinical outcomes were evaluated using the modified MacNab criteria [
3,
32].
2.4. Statistical Analysis
When analyzing the association between access pain and other variables, the independent t-test was performed for continuous variables and the chi-square test or Fisher's exact test was performed for categorical variables.
Simple multiple logistic regression analysis was conducted to analyze the effects of the significant variables on access pain and the impact of access pain on clinical outcomes, including the modified MacNab criteria and complications. Simple multiple linear regression analysis was performed to analyze the effect of access pain on the operative time and hospital stay. Statistical analysis was conducted using SPSS (version 22.0; IBM Corp., Armonk, NY, USA) and R 4.3.1(R Foundation for Statistical Computing, Vienna, Austria), with two-sided tests performed at a significance level of 5%.
3. Results
3.1. Demographics
The study comprised 73 patients with a mean follow-up period of 31.6 months (range: 12–64 months). Among them, 23 (31.51%) were male and 50 (68.49%) were female, with a mean age of 61.05 years (range, 21–83 years). Evaluation based on the four-point classification of transforaminal access pain revealed no or minimal pain in 46 (63.01%) patients, mild pain in 17 (23.29%), moderate pain in 6 (8.22%), and severe pain in 4 (5.48%). Therefore, the rate of significant (moderate to severe) access pain was 13.70% (10 of 73 patients). The zones of disc herniation were foraminal in 53 patients (72.60%) and extraforaminal in 20 (27.40%). The operative level was L2–3 in 3 (4.11%), L3–4 in 12 (16.44%), L4–5 in 29 (39.73%), and L5–S1 in 29 (39.73). The mean operative time was 62.71 minutes (range, 30–120 minutes). The mean length of hospital stay was 2.29 days (range, 1–9 days). Evaluation based on the modified MacNab criteria indicated excellent outcomes in 12 patients (16.44%), good outcomes in 47 (64.38%), fair outcomes in 11 (15.07%), and poor outcomes in 3 (4.11%). The symptomatic improvement and success (good or excellent) rates were 95.89% and 80.82%, respectively. Postoperative dysesthesia was observed in six patients (8.22%), managed through medication alone or in combination with nerve root block. No instances of postoperative infection or hematoma were reported. Three patients with poor outcomes underwent revision surgery (decompression with fusion) during follow-up. The demographic characteristics are summarized in
Table 1.
3.2. Predictive Factors for access Pain during TELD
Extraforaminal LDH tended to cause more severe pain than foraminal LDH during the transforaminal approach under local anesthesia (p < 0.001). Univariate analysis revealed a significant association between the herniation zone and access pain. Significant access pain occurred in 5.66% of foraminal LDH cases and 35% of extraforaminal LDH cases (p = 0.0032;
Table 1). Other factors including age, sex, BMI, symptom duration, level, side, herniation type, and foraminal stenosis grade were not associated with access pain (
Table 1). According to the multiple logistic regression analysis, the herniation zone was also strongly associated with significant access pain (odds ratio = 6.264, 95% confidence interval, 1.056–37.164; p = 0.043;
Table 2).
3.3. Access Pain and Clinical Outcomes
Analysis of the impact of access pain on operative results showed that access pain affected operative time and hospital stay. Significant access pain tends to prolong operative time and length of hospital stay. The mean operative time was 59.57 ± 16.21 min in the minimal pain group and 82.50 ± 26.06 min in the significant pain group (p < 0.001;
Table 3). The mean length of hospital stay was 2.10 ± 1.42 days in the minimal pain group and 3.50 ± 2.51 days in the significant group (p = 0.012;
Table 3). Access pain did not affect other outcome parameters, including complications, postoperative dysesthesia, and the modified MacNab criteria (
Table 3). Excellent or good outcomes were observed in 82.54% of the minimal pain group and 70% of the significant pain group, showing no statistical difference.
Multiple linear regression analysis showed that significant access pain was strongly associated with a longer operative time (B = 21.839, standard error = 6.707; p = 0.002;
Table 4). Significant access pain was also associated with a longer hospital stay (B = 1.106, standard error = 0.518; p = 0.036;
Table 5).
4. Discussion
4.1. Importance of access Pain during TELD under Local Anesthesia
TELD has emerged as an efficient surgical alternative for treating LDH by using a percutaneous transforaminal endoscopic approach. Its effectiveness has been validated in randomized trials and meta-analyses [
7,
8,
9,
10,
11,
12,
13,
14,
15,
16,
17,
18,
19]. Endoscopic spine surgeons can perform this technique with the typical benefits of minimally invasive procedures, including muscle preservation and avoidance of unnecessary laminofacetectomy under local anesthesia. A direct posterolateral approach to the spinal canal through the foraminal safety zone and selective discectomy are feasible for typical intracanal (central or subarticular) LDH. However, the transforaminal approach may encounter considerable access pain in cases of foraminal or extraforaminal LDH, stemming from nerve root irritation, potentially jeopardizing the procedure’s success.
27 Therefore, prediction and prevention strategies for access pain are essential for aspiring endoscopic spinal surgeons.
4.2. Higher Risk of access Pain for Extraforaminal LDH
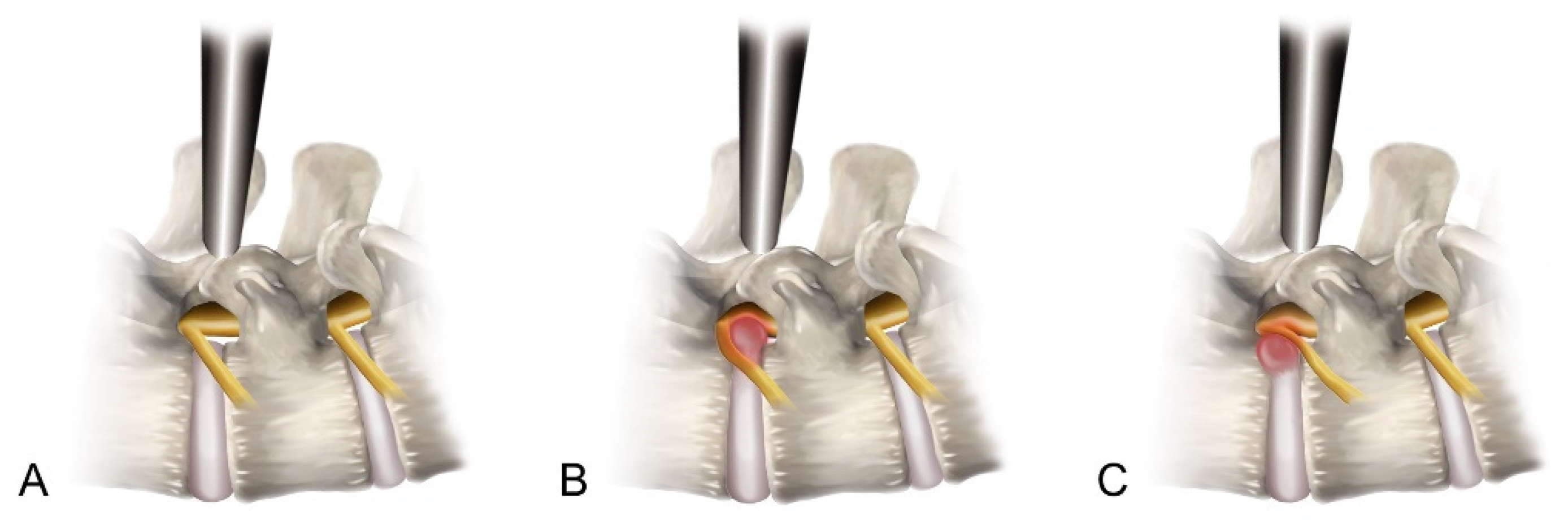
Our data revealed a significant association between the herniation zone and access pain experienced during the transforaminal approach. Extraforaminal LDH, whether with or without sequestered fragments, tended to cause significant access pain (p < 0.01). We postulated that this correlation is closely related to the safety zone of the transforaminal approach (
Figure 3). In cases of foraminal LDH, as the disc material extrudes, the ENR usually deviates anteriorly, allowing for the maintenance or widening of the Kambin’s triangle space utilized in the transforaminal approach. However, in instances of extraforaminal LDH, the extruded disc material can directly exert lateral pressure on the ENR. Therefore, the ENR can be located in the middle of the approach trajectory, leading to a subsequent narrowing of the safety zone. Under such circumstances, the risk of experiencing significant nerve root irritation pain may increase, even with a careful outside-in approach.
4.3. Access Pain May Prolong Operative Time and Hospital Stay
In our study, access pain during TELD tended to lead to a longer operative time (p < 0.01) and a longer hospital stay (p < 0.05). However, other clinical outcomes, including the modified MacNab criteria, postoperative dysesthesia, and other complications were not significantly associated with access pain during TELD. However, caution should be exercised when interpreting these findings. First, the skill and experience of the operating surgeon can influence the outcomes of endoscopic spinal procedures. The senior surgeon involved in this study possessed extensive expertise in transforaminal endoscopic spine surgery, potentially mitigating surgical failures or complications. The observed outcomes may not be generalizable to cases handled by less-experienced practitioners. Second, patients may retain painful memories, impacting their long-term satisfaction, regardless of pain scores or functional improvements. Therefore, access pain may affect both global outcomes and recovery time. Proactive measures to predict and minimize access pain during TELD under local anesthesia are essential for achieving clinical success.
4.4. Technical Keys to Avoid Access Pain
The primary goal of the transforaminal endoscopic approach is to dock the obturator and working sheath in the foraminal zone while avoiding ENR irritation. Accomplishing this objective may involve employing specific technical insights and strategies.
First, the outside-in approach is superior to the inside-out technique. The herniated disc fragment tightly compresses the nerve root. Therefore, passing through the disc may increase the probability of nerve root irritation. In contrast, adopting an outside-in approach can minimize neural irritation or damage during the approach process.
Second, implanting a preemptive epidural block in the foraminal zone can reduce pain caused by neural irritation. Several authors have reported the efficacy of preemptive blocks during the transforaminal endoscopic approach [
22]. The administration of block medications may widen the working space.
Third, the landing point should be as far away from the ENR as possible. The target is recommended to be located at the caudal part of the disc to avoid ENR. Regarding Kambin's triangle, the safe working space at the caudal level of the disc was larger than that at the cranial level.
Fourth, a serial dilation technique, starting from thin to larger dilators, may also reduce mechanical pain and create a smooth route in the back muscles. In contrast, blunt pressure caused by a large-headed dilator may cause severe pain on the inflamed disc surface.
Fifth, using a bevel-ended working sheath is more valuable than using a non-bevel-ended working sheath. The sloping edge enables precise foraminal landing while protecting the ENR. To avoid ENR irritation, the sharp edge of the working sheath is directed towards the caudal part of the foramen. During this step, the obturator and working sheath should not be inserted into the disc space because blunt insertion of the devices can cause severe neural damage or irritation.
Finally, the working sheath can be engaged in the bony foramen with delicate mallet tapping. This allows the working sheath to be placed firmly without a handgrip, and the percutaneous transforaminal approach can be completed. A working-channel endoscope can then be introduced through the working sheath for adequate decompression.
4.5. Limitations of the Study
This study had some inherent limitations. First, despite the inclusion of consecutive cases, its retrospective nature may have introduced considerable bias in assessing the effect of access pain on long-term clinical outcomes and patient satisfaction. Second, in addition to ENR irritation, the severity of access pain might be influenced by other factors, such as personal disposition, depth of sedation, premedication, and the surgeon’s skill. Our measurement was confined to the global pain response of the patients, preventing the evaluation of potential additional factors. Third, the grade of access pain was determined arbitrarily using a four-point grading system. An agreement study on the degree of access pain was not conducted. Therefore, our subsequent study will focus on developing a more objective and reliable grading system for access pain or nerve irritation during the percutaneous transforaminal approach under local anesthesia through a prospective study. Furthermore, future studies should evaluate the relationship between the radiographic dimensions of Kambin’s safety zone and access pain or neural irritation.
5. Conclusions
TELD can serve as an effective surgical option for treating foraminal/extraforaminal LDH using the percutaneous transforaminal approach under local anesthesia. This local procedure may be beneficial, particularly in medically compromised or elderly patients. However, access pain during the transforaminal approach can result in surgical failure and other adverse events. In our study, significant access pain developed during TELD for extraforaminal LDH compared to foraminal LDH, leading to prolonged operative time and length of hospital stay. The extraforaminal component of LDH can narrow the safety working zone for the transforaminal approach. Thus, addressing specialized technical considerations is imperative to ensure the clinical success of TELD.
Author Contributions
Conceptualization, Y.A. and J.-E.C.; methodology, Y.A. and S.L..; software, S.L.; validation, Y.A. and J.-E.C.; formal analysis, Y.A., J.-E.C. and S.L.; investigation, J.-E.C.; resources, Y.A.; data curation, Y.A. and J.-E.C.; writing—original draft preparation, Y.A.; writing—review and editing, Y.A., J.-E.C. and S.L.; visualization, Y.A.; supervision, Y.A.; project administration, Y.A. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the institutional Review Board of Gachon University Gil Medical Center (GDIRB2023-210).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Acknowledgments
The authors would like to thank Chae-Yeon Nam and Jae Min Son for their support and assistance with this manuscript.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Kambin, P.; Sampson, S. Posterolateral percutaneous suction-excision of herniated lumbar intervertebral discs. Report of interim results. Clin. Orthop. Relat. Res. 1986, 207, 37–43. [Google Scholar] [CrossRef]
- Hijikata, S. Percutaneous nucleotomy. A new concept technique and 12 years' experience. Clin. Orthop. Relat. Res. 1989, 238, 9–23. [Google Scholar] [CrossRef]
- Yeung, A.T.; Tsou, P.M. Posterolateral endoscopic excision for lumbar disc herniation: Surgical technique, outcome, and complications in 307 consecutive cases. Spine (Phila Pa 1976) 2002, 27, 722–731. [Google Scholar] [CrossRef]
- Ahn, Y.; Lee, S.H.; Park, W.M.; Lee, H.Y.; Shin, S.W.; Kang, H.Y. Percutaneous endoscopic lumbar discectomy for recurrent disc herniation: surgical technique, outcome, and prognostic factors of 43 consecutive cases. Spine (Phila Pa 1976) 2004, 29, E326–E32. [Google Scholar] [CrossRef] [PubMed]
- Birkenmaier, C.; Komp, M.; Leu, H.F.; Wegener, B.; Ruetten, S. The current state of endoscopic disc surgery: review of controlled studies comparing full-endoscopic procedures for disc herniations to standard procedures. Pain Physician 2013, 16, 335–344. [Google Scholar] [CrossRef]
- Hofstetter, C.P.; Ahn, Y.; Choi, G.; Gibson, J.N.A.; Ruetten, S.; Zhou, Y.; Li, Z.Z.; Siepe, C.J.; Wagner, R.; Lee, J.H.; et al. AOSpine consensus paper on nomenclature for working-channel endoscopic spinal procedures. Global Spine J. 2020, 10, 111S–121S. [Google Scholar] [CrossRef] [PubMed]
- Mayer, H.M.; Brock, M. Percutaneous endoscopic discectomy: surgical technique and preliminary results compared to microsurgical discectomy. J. Neurosurg. 1993, 78, 216–225. [Google Scholar] [CrossRef] [PubMed]
- Hermantin, F.U.; Peters, T.; Quartararo, L.; Kambin, P. A prospective, randomized study comparing the results of open discectomy with those of video-assisted arthroscopic microdiscectomy. J. Bone Joint Surg. Am. 1999, 81, 958–965. [Google Scholar] [CrossRef] [PubMed]
- Hoogland, T.; Schubert, M.; Miklitz, B.; Ramirez, A. Transforaminal posterolateral endoscopic discectomy with or without the combination of a low-dose chymopapain: a prospective randomized study in 280 consecutive cases. Spine (Phila Pa 1976) 2006, 31, E890–E897. [Google Scholar] [CrossRef]
- Ruetten, S.; Komp, M.; Merk, H.; Godolias, G. Full-endoscopic interlaminar and transforaminal lumbar discectomy versus conventional microsurgical technique: a prospective, randomized, controlled study. Spine (Phila Pa 1976) 2008, 33, 931–939. [Google Scholar] [CrossRef]
- Nellensteijn, J.; Ostelo, R.; Bartels, R.; Peul, W.; van Royen, B.; van Tulder, M. Transforaminal endoscopic surgery for symptomatic lumbar disc herniations: a systematic review of the literature. Eur. Spine J. 2010, 19, 181–204. [Google Scholar] [CrossRef] [PubMed]
- Cong, L.; Zhu, Y.; Tu, G. A meta-analysis of endoscopic discectomy versus open discectomy for symptomatic lumbar disk herniation. Eur. Spine J. 2016, 25, 134–143. [Google Scholar] [CrossRef] [PubMed]
- Li, X.C.; Zhong, C.F.; Deng, G.B.; Liang, R.W.; Huang, C.M. Full-Endoscopic procedures versus traditional discectomy surgery for discectomy: a systematic review and meta-analysis of current global clinical trials. Pain Physician 2016, 19, 103–118. [Google Scholar]
- Ruan, W.; Feng, F.; Liu, Z.; Xie, J.; Cai, L.; Ping, A. Comparison of percutaneous endoscopic lumbar discectomy versus open lumbar microdiscectomy for lumbar disc herniation: a meta-analysis. Int. J. Surg. 2016, 31, 86–92. [Google Scholar] [CrossRef]
- Ding, W.; Yin, J.; Yan, T.; Nong, L.; Xu, N. Meta-analysis of percutaneous transforaminal endoscopic discectomy vs. fenestration discectomy in the treatment of lumbar disc herniation. Orthopade 2018, 47, 574–584. [Google Scholar] [CrossRef] [PubMed]
- Zhang, B.; Liu, S.; Liu, J.; Yu, B.; Guo, W.; Li, Y.; Liu, Y.; Ruan, W.; Ning, G.; Feng, S. Transforaminal endoscopic discectomy versus conventional microdiscectomy for lumbar discherniation: a systematic review and meta-analysis. J. Orthop. Surg. Res. 2018, 13, 169. [Google Scholar] [CrossRef] [PubMed]
- Barber, S.M.; Nakhla, J.; Konakondla, S.; Fridley, J.S.; Oyelese, A.A.; Gokaslan, Z.L.; Telfeian, A.E. Outcomes of endoscopic discectomy compared with open microdiscectomy and tubular microdiscectomy for lumbar disc herniations: a meta-analysis. J. Neurosurg. Spine 2019, 31, 802–815. [Google Scholar] [CrossRef]
- Gadjradj, P.S.; Harhangi, B.S.; Amelink, J.; van Susante, J.; Kamper, S.; van Tulder, M.; Peul, W.C.; Vleggeert-Lankamp, C.; Rubinstein, S.M. Percutaneous transforaminal endoscopic discectomy versus open microdiscectomy for lumbar disc herniation: a systematic review and meta-analysis. Spine (Phila Pa 1976) 2021, 46, 538–549. [Google Scholar] [CrossRef]
- Li, W.S.; Yan, Q.; Cong, L. Comparison of endoscopic discectomy versus non-endoscopic discectomy for symptomatic lumbar disc herniation: a systematic review and meta-analysis. Global Spine J. 2022, 12, 1012–1026. [Google Scholar] [CrossRef]
- Ahn, Y. Transforaminal percutaneous endoscopic lumbar discectomy: technical tips to prevent complications. Expert Rev. Med. Devices 2012, 9, 361–366. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.J.; Chen, B.H.; Wang, P.; Liu, C.S.; Yu, J.M.; Ma, X.X. The effect of percutaneous endoscopic lumbar discectomy under different anesthesia on pain and immunity of patients with prolapse of lumbar intervertebral disc. Eur. Rev. Med. Pharmacol. Sci. 2017, 21, 2793–2799. [Google Scholar] [PubMed]
- Sang, X.; Shan, H.; Hu, J.; Wu, M. The efficacy of bilateral intervertebral foramen block for pain management in percutaneous endoscopic lumbar discectomy: a protocol for randomized controlled trial. Medicine (Baltimore) 2020, 99, e22693. [Google Scholar] [CrossRef]
- Choi, I.; Ahn, J.O.; So, W.S.; Lee, S.J.; Choi, I.J.; Kim, H. Exiting root injury in transforaminal endoscopic discectomy: preoperative image considerations for safety. Eur. Spine J. 2013, 22, 2481–2487. [Google Scholar] [CrossRef] [PubMed]
- Pairaiturkar, P.P.; Sudame, O.S.; Pophale, C.S. Evaluation of dimensions of Kambin's triangle to calculate maximum permissible cannula diameter for percutaneous endoscopic lumbar discectomy : a 3-dimensional magnetic resonance imaging based study. J. Korean Neurosurg. Soc. 2019, 62, 414–421. [Google Scholar] [CrossRef] [PubMed]
- Cho, J.Y.; Lee, S.H.; Lee, H.Y. Prevention of development of postoperative dysesthesia in transforaminal percutaneous endoscopic lumbar discectomy for intracanalicular lumbar disc herniation: floating retraction technique. Minim. Invasive Neurosurg. 2011, 54, 214–218. [Google Scholar] [CrossRef]
- Kambin, P.; Brager, M.D. Percutaneous posterolateral discectomy. Anatomy and mechanism. Clin. Orthop. Relat. Res. 1987, 223, 145–154. [Google Scholar] [CrossRef]
- Ahn, Y.; Yoo, B.R.; Jung, J.M. The irony of the transforaminal approach: a comparative cohort study of transforaminal endoscopic lumbar discectomy for foraminal versus paramedian lumbar disc herniation. Medicine (Baltimore) 2021, 100, e27412. [Google Scholar] [CrossRef]
- Fardon, D.F.; Milette, P.C.; Combined Task Forces of the North American Spine Society, American Society of Spine Radiology, and American Society of Neuroradiology. Nomenclature and classification of lumbar disc pathology. Recommendations of the Combined task Forces of the North American Spine Society, American Society of Spine Radiology, and American Society of Neuroradiology. Spine (Phila Pa 1976) 2001, 26, E93–E113. [Google Scholar] [CrossRef]
- Kambin, P.; O'Brien, E.; Zhou, L.; Schaffer, J.L. Arthroscopic microdiscectomy and selective fragmentectomy. Clin. Orthop. Relat. Res. 1998, 347, 150–167. [Google Scholar] [CrossRef]
- Lee, S.; Lee, J.W.; Yeom, J.S.; Kim, K.J.; Kim, H.J.; Chung, S.K.; Kang, H.S. A practical MRI grading system for lumbar foraminal stenosis. AJR Am. J. Roentgenol. 2010, 194, 1095–1098. [Google Scholar] [CrossRef] [PubMed]
- Park, H.J.; Kim, S.S.; Lee, S.Y.; Park, N.H.; Rho, M.H.; Hong, H.P.; Kwag, H.J.; Kook, S.H.; Choi, S.H. Clinical correlation of a new MR imaging method for assessing lumbar foraminal stenosis. AJNR Am. J. Neuroradiol. 2012, 33, 818–822. [Google Scholar] [CrossRef] [PubMed]
- Macnab, I. Negative disc exploration. An analysis of the causes of nerve-root involvement in sixty-eight patients. J. Bone Joint Surg. Am. 1971, 53, 891–903. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).