Submitted:
20 August 2024
Posted:
21 August 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
1.1. Work-Related Disorders and Work Technique Training in Manual Handling
1.2. Current Research on the Effectivness of Sensor-Based Augmented Feedback Training
1.3. Aim
2. Materials and Methods
2.1. Eligibility Criteria
| Eligibility criteria | Descriptions |
|---|---|
| Studies evaluating sensor-based instruments or systems that monitor biomechanical exposure targeting the upper body and provide augmented feedback to the wearer based on this information. | Various biomechanical exposures are targeted, including posture, movement, and muscle activity etc. The primary body segments targeted include the neck (e.g., head inclination), spine (cervical to lumbosacral segments), arms (upper and lower), and wrists/hands. Only instruments or systems providing direct feedback to the wearer were considered. For example, evaluations on the effectiveness of an instructor assisted by sensor-based data are outside the scope. The focus on sensor-based augmented feedback excludes other types of augmented feedback, such as from athletic tapes. |
| Studies aiming to reduce adverse biomechanical exposure with the long-term objective of preventing or reducing work-related musculoskeletal disorders (WMSDs). | The study should report (at least briefly) how the reduction of the targeted biomechanical exposure can potentially mitigate adverse health effects, including WMSDs.Studies aiming to increase biomechanical exposure to achieve health benefits, such as interrupting prolonged sustained postures with increase physical activity, are excluded. |
| Studies evaluating augmented feedback on manual handling tasks performed in real work environments or those that simulate work-related manual handling tasks or single operations in controlled settings. | Manual handling operations encompass tasks such as lifting, pushing, pulling, and holding. This review excludes studies focused on predominantly sedentary jobs or tasks involving a significant proportion of static (isometric) postures, such as computer typing, dentistry, or surgical work. Additionally, the emphasis on work-related manual handling tasks excludes studies involving the manipulation of non-physical (virtual) objects. |
| Studies evaluating augmented feedback on adults (18–67 years) from regular working populations or student populations. | If the sample includes participants older or younger than 18–67 years, the data on the effect of feedback must be reported separately for those aged 18–67 years. The focus on regular working populations and student populations means that specific patient populations, such as those with medical conditions that hinder task performance, are excluded. |
| Studies evaluating augmented feedback on at least 8 participants per group receiving the feedback, and where the effect of the feedback is tested statistically | A sample size of fewer than 8 participants per group is acceptable only if justified by power calculations, including descriptions of the assumed effect size. The number of participants refers to those included in the final analysis. |
2.2. Search Strategy
2.3. Study Selection
2.4. Methodological Quality Assessment
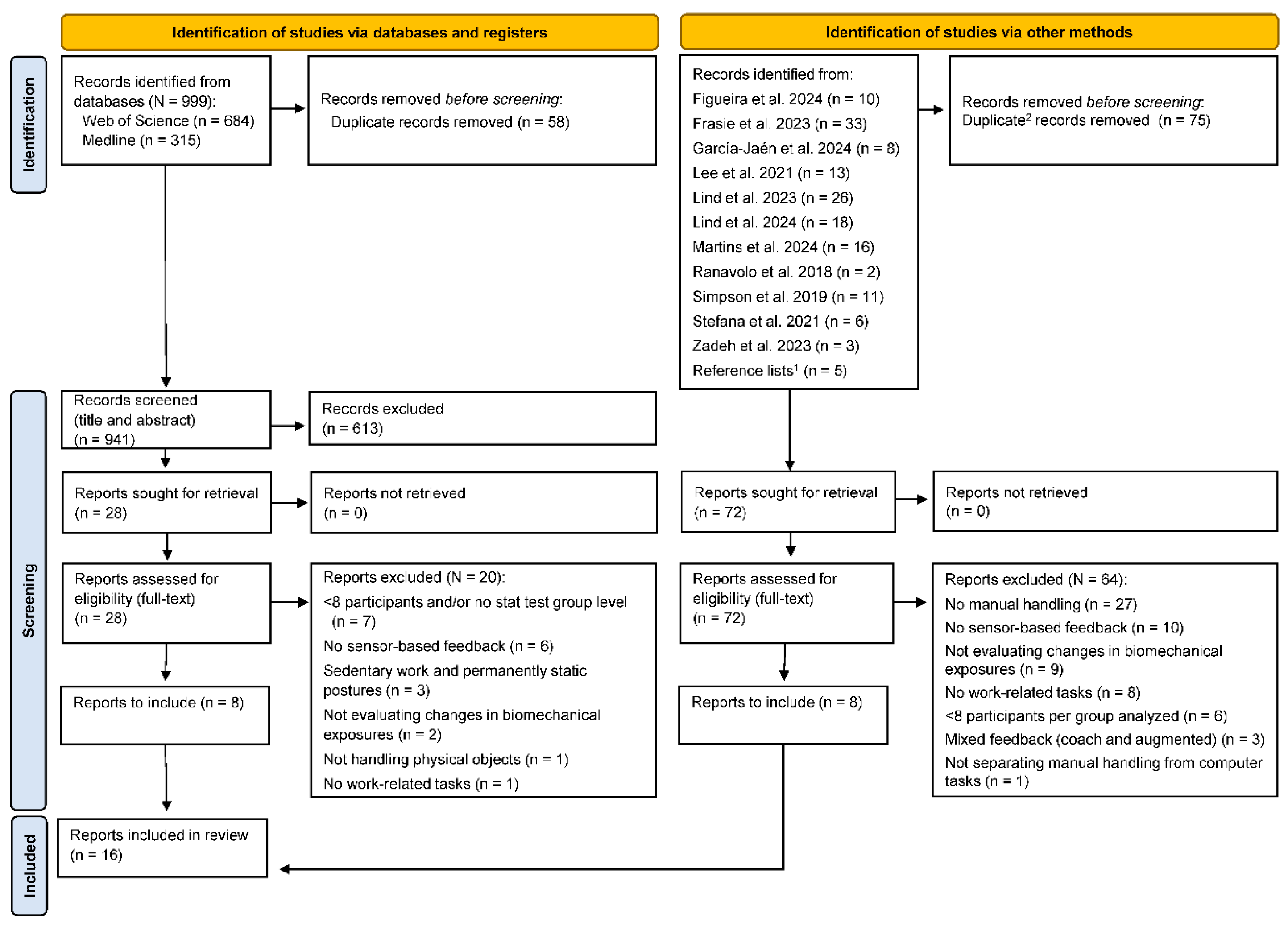
2.5. Strength of Evidence Assessment
| Strength of evidence | Criteria |
|---|---|
| Strong evidence | Consistent findings among three or more studies of at least moderate quality, including at least two of high quality. |
| Moderate evidence | Consistent findings among two or more studies of at least moderate quality, including at least one of high quality. |
| Limited evidence | Findings from at least one study of high quality or two studies of moderate quality. |
| Very limited evidence | Findings from one study of moderate quality. |
| Inconsistent evidence | Inconsistent findings among multiple studies, such as one or multiple studies of at least moderate quality reporting significant result, whereas one or multiple studies of at least moderate quality reporting no significant result. |
| Conflicting evidence | Conflicting results between studies, such as one or multiple studies of at least moderate quality reporting significant result in one direction, whereas one or multiple studies of at least moderate quality reporting significant result in the other direction. |
| No evidence | Insignificant results derived from multiple studies of high or moderate quality. |
2.6. Data Extraction
- Targeted outcome
- Study design (including the use of a control group)
- Setting and tasks performed
- Participants’ characteristics (sex, age, and eligibility)
- Feedback evaluation and duration of the retention tests
- Feedback characteristics (type and modality, targeted body region, and feedback trig-ger)
- Equipment for collecting and analyzing exposure data (including if it is ambulatory)
| Duration Classification | Criteria (time elapsed after feedback administration) | Abbreviated names |
|---|---|---|
| During feedback | Simultaneous to feedback administration | During feedback |
| Directly after | Directly after, and up to 8 hours after | Directly after (≤8 hours) |
| Very short term | >8 hours, and up to ≤1 week after | Very short term (≤1 week) |
| Short term | >1 week, and up to ≤1 month after | Short term (≤1 month) |
| Midterm | >1 month, and up to <6 months after | Midterm (<6 months) |
| Long term | 6 months or more after | Long term (≥6 months) |
3. Results
3.1. Quality Assessment
- Not reporting the participation rate of eligible persons of the identified pool of eligible persons (n = 15) (Criterion 3).
- Not blinding (or reporting blinding) of assessors to the participants' group allocation (n = 15) (Criterion 12).
- No clear justification of the sample size to detect difference in the outcome with at least 80% power (n = 13) (Criterion 5).
| Study | Criteria | Quality | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | ||
| Agruss et al. [77] | 1 | 1 | NR | 1 | NR | 1 | 1 | 1 | 1 | 0 | 1 | NR | 1 | 1 | Moderate |
| Boocock et al. [78] | 1 | 1 | NR | 1 | 1 | NA | 1 | 1 | 1 | 1 | 1 | NR | 1 | 1 | High |
| Bootsman et al. [79] | 1 | 1 | NR | NA | NR | 1 | 1 | 1 | 0 | 1 | 1 | NR | 1 | 0 | Moderate |
| Brandl et al. [67] | 1 | 1 | NR | 1 | NR | 0 | 0 | 1 | 1 | 0 | 0 | NR | 1 | 0 | Low |
| Kamachi et al. [80] | 1 | 1 | NR | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | NR | 1 | 1 | High |
| Kernozek et al. [81] | 0 | 0 | NR | 1 | NR | 1 | 1 | 1 | 1 | 0 | 1 | NR | 1 | 1 | Moderate |
| Langenskiöld et al. [72] | 1 | 1 | NR | NA | NR | 1 | 1 | 1 | 0 | 1 | 1 | NR | 1 | 0 | Moderate |
| Lim et al. [71] | 1 | 1 | NR | NA | NR | 1 | 1 | 1 | 1 | 1 | 1 | NR | 1 | 1 | High |
| Lind et al. [82] Sens | 1 | 1 | NR | NA | NR | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 1 | 0 | Moderate |
| Lind et al. [69] AE | 1 | 1 | NR | NA | NR | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | High |
| Lind et al. [73] Erg | 1 | 1 | 1 | NA | NR | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | High |
| Oppici et al. [83] | 1 | 1 | NR | NA | NR | 1 | 1 | 1 | 1 | 1 | 1 | NR | 1 | 1 | High |
| Owlia et al. [68] | 1 | 1 | NR | 1 | NR | 1 | 1 | 1 | 0 | 1 | 1 | NR | 1 | 0 | Moderate |
| Punt et al. [66] | 1 | 0 | NR | NR | NR | 1 | 1 | 1 | 1 | 1 | 1 | NR | 1 | 1 | Moderate |
| Ribeiro et al. [84] | 1 | 1 | NR | 0 | NR | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | Low |
| Ribeiro et al. [70] | 1 | 1 | NR | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | High |
| Study | Criteria | Quality | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | ||
| Ribeiro et al. [84] | 1 | 0 | 0 | 0 | NR | 0 | 0 | 1 | NR | NR | 0 | 0 | NR | 1 | Low |
| Ribeiro et al. [70] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | NR | NR | 1 | 1 | 1 | 1 | High |
3.2. Study Design, Methodology, and Instruments
3.2.1. Study Design, Settings, Tasks and Participants
| Study | Targeted outcome | Study design | Control group | Setting |
|---|---|---|---|---|
| Agruss et al. [77] | Reduce peak lumbosacral compression | CS | Yes | Cont. |
| Boocock et al. [78] | Reduce lumbosacral posture and trunk flexion | CS | Yes | Cont. |
| Bootsman et al. [79] | Reduce episodes of lower back flexion | CS | No | Real |
| Kamachi et al. [80] | Reduce time in end-range lumbar spine flexion | CS/SLN | Yes | Cont. 1 |
| Kernozek et al. [81] | Reduce peak lumbosacral moment | CS | Yes | Cont. |
| Langenskiöld et al. [72] | Reduce time in adverse trunk inclination and arm elevation | CS | No | Cont. |
| Lim et al. [71] | Reduce sagittal trunk flexion angles | CS | No | Cont. |
| Lind et al. [82] | Reduce time in adverse arm elevation | CS | No | Cont. |
| Lind et al. [69] | Reduce time in adverse trunk inclination and arm elevation | CS | No | Cont. 2 |
| Lind et al. [73] | Reduce time in adverse trunk inclination | CS/SLN | No | Real |
| Oppici et al. [83] | Reduce spine flexion | CS | No | Cont. |
| Owlia et al. [68] | Reduce peak lumbar spine flexion | CS | Yes | Cont. 1 |
| Punt et al. [66] | Reduce low-back load (L5/S1 net moment, trunk inclination and lumbar flexion) | CS | Yes | Cont. |
| Ribeiro et al. [70] | Reduce occurrence of trunk inclination | cluster RCT | Yes | Real |
| Study | Force demands | Task complexity | Tasks | Description | |
|---|---|---|---|---|---|
| Agruss et al. [77] | H | L | Lifting | Symmetrical sagittal plane lifts of boxes ('maximum safe load'1) from pallet height to knuckle height at 30-second intervals. | |
| Boocock et al. [78] | H | L | Lifting and lowering | Lifting and lowering a 13-kg box (30×25×25.5 cm) with handles (10 lifts/min) from a platform (height: 15 cm) to an upright standing position, holding it still, and then lowering the box back to the platform. | |
| Bootsman et al. [79] | L–H | H | Health care and home care tasks | Various intensive care and home care tasks. | |
| Kamachi et al. [80] | H | M–H | Patient transfer | A series of simulated patient transfer activities of a patient actor (87 kg), e.g., transfer patient from bed to wheelchair, from wheelchair to couch, and assist patient to stand, don pants and transfer to wheelchair. Additional skill transfer task: patient sling insertion task. |
|
| Kernozek et al. [81] | H | L | Lifting and lowering | Lifting cases of bananas (mean: 18 kg) and various items (13.6–18.1 kg). Items lifted from pallet on the floor to a 2.1-meter height location and from a 2.1-meter height location to the pallet. | |
| Langenskiöld et al. [72] | L–M | L–M | Office-type of manual handling | Organizing 38 documents, lifting 8 large empty boxes, relocating 8 ring binders, and lifting 10 small empty boxes. | |
| Lim et al. [71] | M–H | M | Construction activities | Lifting pouches (25×36 cm, 4.5 kg) from floor height, carrying them 1.2 m, and lowering them. Transferring the pouches using a shovel to a location 1.2 m away. Simulated rebar tying tasks. | |
| Lind et al. [82] | L | L | Mail (letter) sorting | Sorting 30 randomly ordered letters (marked 0–9) to their corresponding letter tray (marked 0–9). | |
| Lind et al. [69] | L–M | M–H | Order picking | Simulated order-picking task resembling real order-picking, with items (0.1–3.1 kg) located in seven positions (heights: 0.15–1.3 m). | |
| Lind et al. [73] | M–H | H | Order picking | Sorting of packages (3–15 kg, 3–6 packages/min) from a container to a storage container (height: 0.3–1.1 m). Handling of containers was also included (including pushing) and registering each handled item. | |
| Oppici et al. [83] | H | L | Lifting and lowering | Lifting (symmetrical sagittal plane lift) a 7.5-kg box from floor height to knuckle height and lowering it back to floor height (10 lifts/min). | |
| Owlia et al. [68] | H | M–H | Patient transfer | A series of simulated patient transfer activities of a patient actor (82 kg), e.g., transfer patient from bed to wheelchair, from wheelchair to couch, and assist patient to stand, don pants and transfer to wheelchair. | |
| Punt et al. [66] | H | L | Lifting and lowering | Lifting and lowering a 10-kg box to three locations: a left/center/right positions and two depth (far and nearby) positions. | |
| Ribeiro et al. [70] | L–H | H | Health care activities | Various health care activities performed within aged care institutions and hospitals. |
| Study | Participants: sex, age (mean, SD) and eligibility |
|---|---|
| Agruss et al. [77] | 28 college students (10 men; 18 women), 23.2 (3.4) years. Verbal acceleration feedback group: n = 9; 24.1 (4.8) years. EMG feedback group: n = 10; 22.8 (2.5) years. Control group; n = 9; 22.7 (2.4) years. Eligibility (health status): no having acute or chronic back pain. |
| Boocock et al. [78] | 36 university students1 (sex: NR). Feedback group: (n = 18); 25.7 (4.6) years. Control group: (n = 16); 25.6 (5.1) years.Eligibility (health status): no back injury or complaint in the past 6 months; no history of spinal surgery; without any cardiovascular or neurological conditions; no existing musculoskeletal injury. Other 2: not experienced in manual handling or performed regular handling in their work. |
| Bootsman et al. [79] | 13 nurses (all women); 40 (14) yearsEligibility (health status): no LBP. Other: not having a sedentary job |
| Kamachi et al. [80] | 20 participants (10 men; 10 women). Feedback group (5 female; 5 male); 24 (4) years. Control group (5 female; 5 male); 24 (3) years. Eligibility (health status): no back pain in the last 6 months or any MSDs or issues related to the spine. Other: no previous experience in caregiving or healthcare; able to understand and speak English. |
| Kernozek et al. [81] | 22 warehouse workers (all men); age: NR. Feedback training group (n=11); control group (n = 11). Eligibility (health status): NR. Other 2: regularly performing warehouse lifting or lowering tasks. |
| Langenskiöld et al. [72] | 10 participants3,4 (2 men; 8 women); 43.9 (12.0) years. Eligibility (health status): Not having pain or restrictions in movement. |
| Lim et al. [71] | 14 participants (all men); 26 (5) years.Eligibility (health status): without MSDs. Other: 18–35 years age; no previous experience of construction; no previous training on safe construction work techniques. |
| Lind et al. [82] | 16 university staff/students (7 men; 9 women); 25 (8) years.Eligibility (health status): no musculoskeletal discomfort or disorders that could hinder the manual handling task. |
| Lind et al. [69] | 155 warehouse workers (12 men; 3 women); 39 (12) years.Eligibility (health status): no musculoskeletal discomfort or disorders that could hinder the manual handling task. |
| Lind et al. [73] | 15 warehouse workers (14 men; 1 women) 6; 31 (12) years. Eligibility (health status): no disorders or pain that prevent performing daily work. Other: currently working as order picker. |
| Oppici et al. [83] | 20 university students (13 men; 7 women); 30 ± 6 years. Eligibility (health status): Not having back injury or pain in the last year, undergoing spinal surgery, or any cardiovascular, neurological or musculoskeletal condition at the time of the study, or allergy to adhesives. |
| Owlia et al. [68] | 20 participants (10 men; 10 women). Feedback training group: (6 men; 4 women); 28 (6) years. Control group: (4 men; 6 women); 25 (3) years. Eligibility (health status) 2: no history of back pain in the last six months and no musculoskeletal issues related to the spine. Other 2: adult s (i.e., ≥18 years); having no formal training in caregiving or patient handling; able to understand and speak English. |
| Punt et al. [66] | Control group: 14 participants (7 men and 7 women); 23.7 ± 8 years. Feedback moment group: 29 participants (22 men and 7 women); 25.7 ± 4 years. Feedback inclination group: 28 participants (13 men and 15 women); 24.9 ± 7 years. Feedback lumbar flexion group: 21 participants (15 7 men and 7 7 women); 25.9 ± 10 years. Eligibility (health status) 2: no recent history of low back pain. Other 2: no previously knowledge about the biomechanics of lifting; not having participated in any other studies related to lifting and biomechanics. |
| Ribeiro et al. [70] | 130 healthcare workers (20 men; 110 women); 45 (13) years. Feedback group (10 men; 53 women); 48 (range: 37–55) years. Control group (10 men; 57 women); 47 (range: 32–56) years.Eligibility (health status): performing regular work activities without any limitations such as due to LBP or LBP symptoms. Other: adult health care worker; working at least 20 hours/week. |
3.2.2. Feedback Characteristics and Distribution, and Equipment
| Study | Feedback evaluation | Feedback distribution |
|---|---|---|
| Agruss et al. [77] | During feedback 1 Very short term (≤1 week) |
Baseline – All lifting two 5-min sets (each 10 lifts) without feedback; instructions from video on basics of safe lifting mechanics (all participants) Week 1 – CG: 40 lifts without feedback; FBGs A and B: 10 lifts without feedback; 10 lifts (100% feedback); 10 lifts (50% feedback); 10 lifts without feedback. Week 2 – CG: 40 lifts without feedback; FBGs A and B: 10 lifts without feedback; 5 lifts (100% feedback); 15 lifts (33% feedback); 10 lifts without feedback. Week 3 – All: lifting two 5 min sets (each 10 lifts) without feedback Feedback session duration: ~15 minutes |
| Boocock et al. [78] | During feedback | Order (no baseline): Lifting for 20 min (FBG: with feedback; CG: without feedback) Feedback session duration: ~20 min |
| Bootsman et al. [79] | During feedback Directly after (≤8 hours) |
Order: Baseline (30 min, no feedback); Feedback session 1 (60 min, feedback); Retention test session (60 min, no feedback); Feedback 2 session (60 min, feedback3) Feedback session duration: ~120 min |
| Kamachi et al. [80] | Directly after (≤8 hours) 4 Short term (≤1 month) Midterm (≤6 months) |
Session 1: FBG+CG (no feedback); FBG+CG video training Sessions 2 and 3: FBG (100%8 feedback); CG: (no feedback) Sessions 4 and 6: FBG+CG (no feedback) Sessions 6 and 7: FBG (50%8 feedback); CG (no feedback) Session 8: FBG+CG (no feedback) Retention tests (sessions 9 and 10): previous tasks and a new task to test the skill transfer Sessions 9 (after 2 weeks): FBG+CG (no feedback) Sessions 10 (after 2 months): FBG+CG (no feedback) Feedback session duration: ~60 minutes. Session duration: about 15 min each for session 1–8 (session 1–4 performed on day 1 and session 5–8 on day 2) |
| Kernozek et al. [81] | Short term (≤1 month) | Week 1 (baseline): Lifting 2 (both groups: without feedback) Weeks 2 and 4: Lifting 2 (feedback group: with feedback; control group: not lifting) Weeks 6: Lifting 2 (both groups: without feedback) Feedback session duration: ~30 minutes |
| Langenskiöld et al. [72] | During feedback Directly after (≤8 hours) |
Order: Practice session; Baseline (4-6 min, no feedback); Feedback session (8-12 min, feedback); Retention session (4-6 min, no feedback). Feedback session duration: ~8–12 min |
| Lim et al. [71] | During feedback | Random order: 3 feedback sessions each performed in 3 tasks. Feedback condition: no feedback; feedback from device on the back or the wrist. Tasks: lifting/lowering (mean: 3.4 min); shoveling (mean: 7.2 min); rebar tying (mean: 6.9 min) Feedback session duration: ~35 min |
| Lind et al. [82] | During feedback | Order: Practice session (no feedback); b) Baseline (no feedback); Ergonomics instruction session 1 (no feedback); Feedback session 1 (feedback); Ergonomics instruction session 2 (no feedback); Feedback session 2 (feedback). Session duration: all sessions but practice session (~1 min) Feedback session duration: ~2 min |
| Lind et al. [69] | During feedback Directly after (≤8 hours) |
Order: Practice session (no feedback); Baseline (no feedback); Feedback session 1 (feedback); Feedback session 2 (feedback); post-Feedback session (no feedback). Session duration: all sessions but practice session (~6 min) Feedback session duration: ~12 min |
| Lind et al. [73] | During feedback Directly after (≤8 hours) Very short term (≤1 week) Short term (≤1 month) |
Order: Baseline (no feedback): Feedback session 1 (2 days after baseline; feedback); Feedback session 2 (~7 days after baseline; feedback); post-Feedback session (directly after Feedback session 2; no feedback); Retention session 1 (~1 week after Feedback session 2; no feedback); Retention session 2 (~3 weeks after Feedback session 2; no feedback). Session duration: Baseline (~45 min); Feedback sessions and post-Feedback session (~30 min); Retention sessions (~45 min) Feedback session duration: ~60 min |
| Oppici et al. [83] | During feedback Directly after (≤8 hours) |
All conditions: 30 lifts/lower; 6 min rest; retention test (5 lifts/lower) Order (2 min break between condition): Baseline, Feedback condition (A or B), Feedback condition (B or A) Feedback was not provided during retention test Feedback session duration: ~3 minutes each with audio- and tactile feedback |
| Owlia et al. [68] | Directly after (≤8 hours) 3 | Day 1 – Session 1 (no feedback); Video training (only FBG); Session 2 (no feedback); Sessions 3 and 4 (FBG: feedback; CG no feedback); Day 2 – Session 5 (no feedback); Sessions 6 and 7 (FBG: feedback; CG no feedback); Session 8 (no feedback) Session duration: session 1–7 (~10 min) Feedback session duration: ~about 40 minutes |
| Punt et al. [66] | During feedback Directly after (≤8 hours) |
All sessions: 12 lifts/lower Session 1 (Baseline): no feedback Sessions 2 and 3: feedback for feedback groups; no feedback for control group. Session 4 (retention test): no feedback Feedback session duration: NR |
| Ribeiro et al. [70] | During feedback Very short term (≤1 week) Short term (≤1 month) Midterm (≤6 months) Long term (≥ 12 months) |
Baseline Intervention (for 4 weeks) Retention tests after: 1 week, 1 month, 3 months, 6 months, 12 months. Feedback session duration: 4 work weeks |
| Study | Feedback type |
Feedback modality | Primary body region(s) | Feedback trigger |
|---|---|---|---|---|
| Agruss et al. [77] | System-initiated Corrective fading Concurrent or terminal1 |
A: audio B: audio (verbal) |
Lumbosacral spine | Gradually increased feedback intensity: Group A: muscle activity (electromyographic) Group B: acceleration index (difference between the dynamically and statically determined lumbosacral peak compression forces) |
| Boocock et al. [78] | System-initiated Concurrent corrective | Audio | Lumbosacral spine | 1 feedback level: >80% of maximum lumbosacral range-of-motion |
| Bootsman et al. [79] | System-initiated Concurrent cumulative) corrective |
Audio and Vibration 2 + Visual 3 |
Lumbosacral spine | 1 feedback level: >20° lower back flexion for >1.5 s (max 1 notification / 5 min) |
| Kamachi et al. [80] | System-initiated Concurrent and fading 4 corrective | Audio | Lumbosacral spine | 2 feedback levels: 20° less than 70% max forward lumbar flexion (intermittent tone); >70% of max forward lumbar flexion (continuous tone). |
| Kernozek et al. [81] | System-initiated Concurrent corrective | Audio | Lumbosacral spine | Gradually increased feedback intensity with increased spinal moments (L5/S1) |
| Langenskiöld et al. [72] | System-initiated Terminal corrective and reinforcing | Vibration | Spine (thoracic–lumbosacral) Upper arm |
1 feedback level per body region: >30° trunk inclination for >10% of the time. >30° arm elevation for >30% of the time. |
| Lim et al. [71] | System-initiated Concurrent (cumulative) corrective | Vibration | Spine (thoracic–lumbosacral) | 2 feedback levels: >45° trunk inclination (3 intermittent vibrations). 3 s continuous vibration if the criteria was reached >2 times within 2 min. |
| Lind et al. [82] | System-initiated Concurrent corrective | Vibration | Upper arm |
2 feedback levels: Arm elevation ≥30° and ≥60° |
| Lind et al. [69] | System-initiated Concurrent corrective | Vibration | Spine (thoracic–lumbosacral) Upper arm |
2 feedback levels per body region: Arm elevation ≥30° and ≥60° Trunk inclination ≥20° and ≥45° |
| Lind et al. [73] | System-initiated Concurrent corrective | Vibration | Spine (thoracic–lumbosacral) | 2 feedback levels: Trunk inclination >30° and >45° |
| Oppici et al. [83] | System-initiated Concurrent corrective 5 | Audio | Lumbosacral spine | Gradually increased feedback amplitude and modulation frequency with increased spine flexion angle. |
| Owlia et al. [68] | System-initiated Concurrent corrective | Audio | Lumbosacral spine | 2 feedback levels: 20° less than 70% of maximum forward lumbar flexion; 70% of maximum forward lumbar flexion. |
| Punt et al. [66] | System-initiated Concurrent corrective | Audio | Lumbosacral spine | Gradually increased feedback intensity. A 6 80% of the average peak sagittal plane moments during baseline. B 7 80% of the average peak trunk inclination angles during baseline. C 8 70% of the average of the observed peak lumbar flexion angles during baseline |
| Ribeiro et al. [70] | System-initiated Concurrent cumulative corrective | Audio | Lumbosacral spine | 2 feedback levels: ≥45° lumbopelvic forward bend (continuous >5 s) ≥45° lumbopelvic forward bending (occurring within 25 s after condition 1). |
| Study | Equipment (exposure analysis; feedback trigger) | Motion sensor | Ambulatory |
|---|---|---|---|
| Agruss et al. [77] | Group A: NR Group B: Custom |
Prototype version of the video analysis system the V-Task. 6 reflective markers on the wrist, elbow, shoulder, hip, knee, and ankle joint. Group A: additionally, an EMG-system (name and location: NR) |
No |
| Boocock et al. [78] | Custom: custom-designed software (LabView) | 2 IMUs (Shimmer Sensing, Ireland) Location: 1st lumbar spinous process and sacral body (S1) |
Partly |
| Bootsman et al. [79] | Custom: smartphone Android application | 2 IMUs (LSM9DSO, STMicroelectronics, Sweden) Location: 1st and 5th lumbar spine vertebrae |
Yes |
| Kamachi et al. [80] | Custom: PostureCoach v0.2 | 2 IMUs (MTi-3, Xsens Technologies, Enschede, Netherlands) Location: (back) thoracic vertebrae (T10) and approx. to sacrum |
Yes |
| Kernozek et al. [81] | Custom and commercial: motion Monitor software (Innovative Sports Training, Inc., IL, USA); Custom Matlab programs (Version 6.5, The Mathworks Inc., MA, USA); Motion Monitor software. Auditory feedback was controlled by the LiftTrainerTM software. | Ascension Electromagnetic Tracking Device (Ascension Technology Corporation, Burlington,USA) Sensor location: forearms, upper arm, back of the head, cervical (C4) and sacral (S1) region of the spine. |
No |
| Langenskiöld et al. [72] | Custom: Smartphone Android application (ErgoRiskLogger) | 2 IMUs (LPMS-B2 IMU, LP Research, Tokyo, Japan) Location about at the level of 1–2 thoracic vertebrae, and distal part of m. deltoideus. |
Yes |
| Lim et al. [71] | Custom: custom-designed software with hardware Raspberry Pi 3 board and PC | 4 IMUs (Mbientlab MetaMotionR+) Location: 6th thoracic vertebra, right thigh, right shin and dominant wrist |
Partly |
| Lind et al. [82] | Custom: smartphone Android application (ErgoRiskLogger ) | 1 IMU (LPMS-B2 IMU, LP Research, Tokyo, Japan) Location: distal part of m. deltoideus |
Yes |
| Lind et al. [69] | Custom: smartphone Android application (ErgoRiskLogger) | 2 IMUs (LPMS-B2 IMU, LP Research, Tokyo, Japan) Location: 1–2 thoracic vertebrae, and distal part of m. deltoideus |
Yes |
| Lind et al. [73] | Custom: smartphone Android application (ErgoRiskLogger) | 1 IMU (LPMS-B2 IMU, LP Research, Tokyo, Japan) Location: 1–2 thoracic vertebrae |
Yes |
| Oppici et al. [83] | Custom: Visual3D software (CMotion, Inc.) and custom script in MATLAB (The Mathworks Inc., MA, USA); Pure Data via Open Sound Control protocol. | 10-camera motion capture system (Qualisys AB, Gothenburg, Sweden) with 36 reflective markers attached to the trunk, pelvis, thighs, shanks and feet. |
No |
| Owlia et al. [68] | Custom: PostureCoach v0.2 | 2 IMUs (MTi-3, Xsens Technologies, Enschede, Netherlands) Location: 10th thoracic vertebrae and approx. to sacrum |
Yes |
| Punt et al. [66] | Custom: custom-made Matlab (The Mathworks Inc., MA, USA) program | 3 camera arrays of a 3D motion capture system (Optotrak Certus system; Norton Digital Inc.). Light emitting diodes markers attached: both shanks and thighs, pelvis (sacrum) and thorax (T6 spinous process). |
No |
| Ribeiro et al. [70] | Commercial: Spineangel (Movement Metrics Ltd, Hamilton, New Zealand) | 1 triaxial accelerometer (Spineangel) Location: lateral around the hip |
Yes |
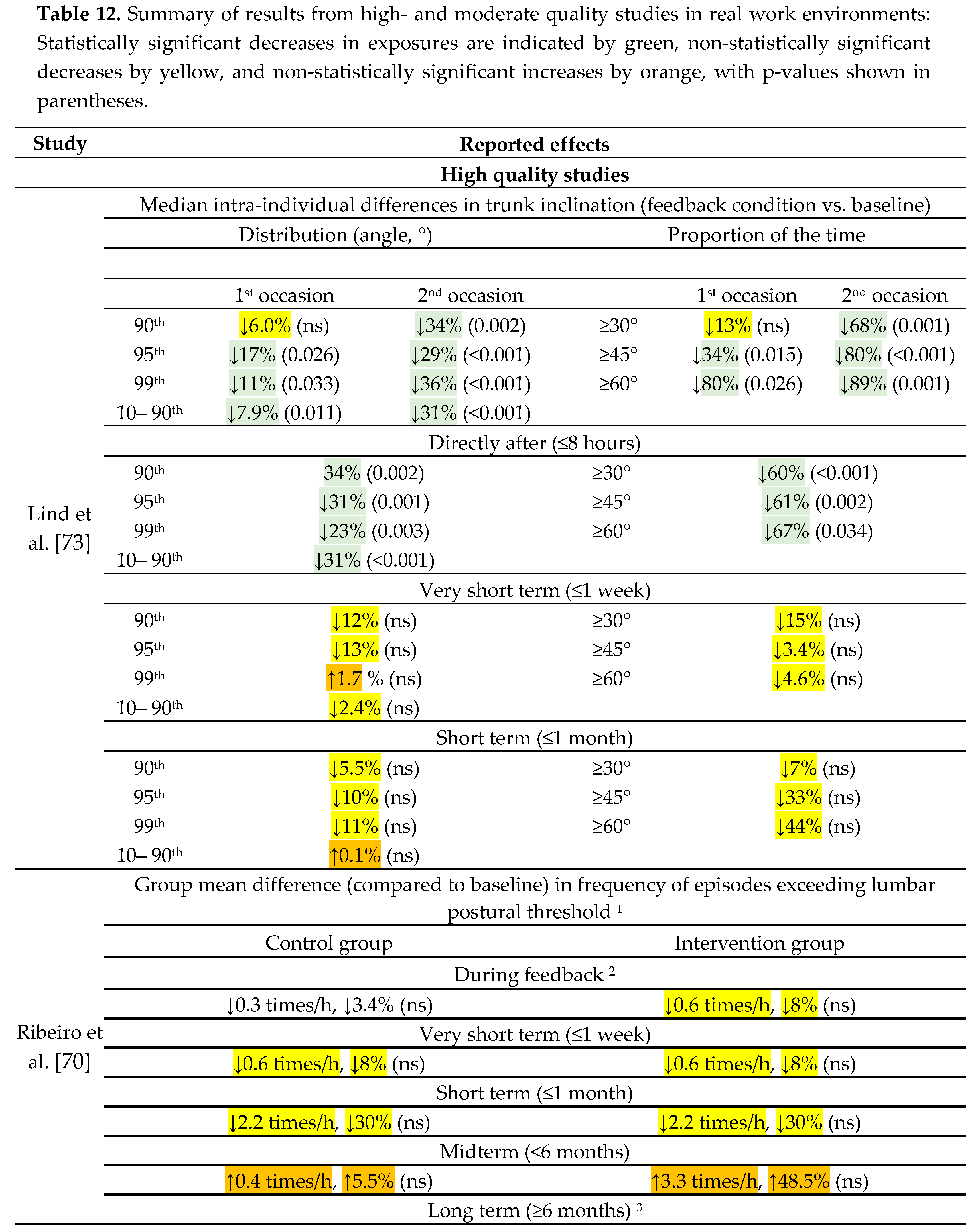
3.3. Effectiveness of Feedback in Real Work Environments
3.3.1. Effect during Feedback Administration
3.3.2. Effect Directly after Feedback Administration
3.3.3. Retained Effects: Very Short and Short Term
3.3.4. Retained Effects: Midterm and Long Term
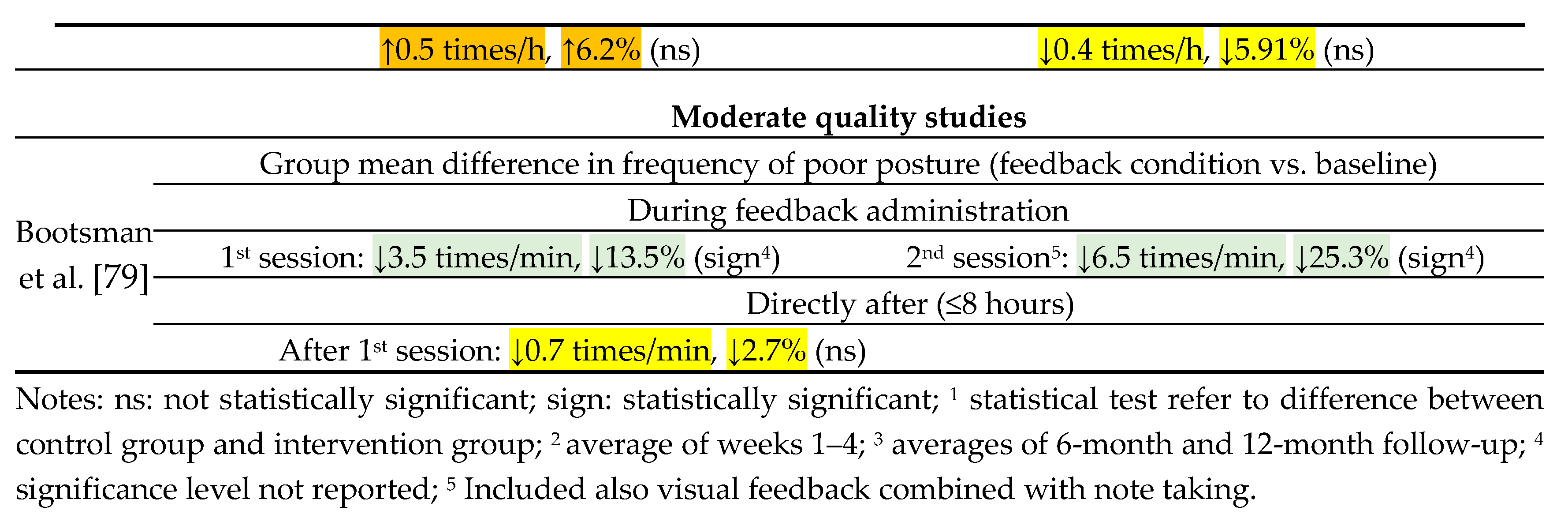
3.4. Effectiveness of Feedback in Controlled Settings
3.4.1. Effect during Feedback Administration
3.4.2. Effect Directly after Feedback Administration
3.4.3. Retained Effects: Short and Midterm
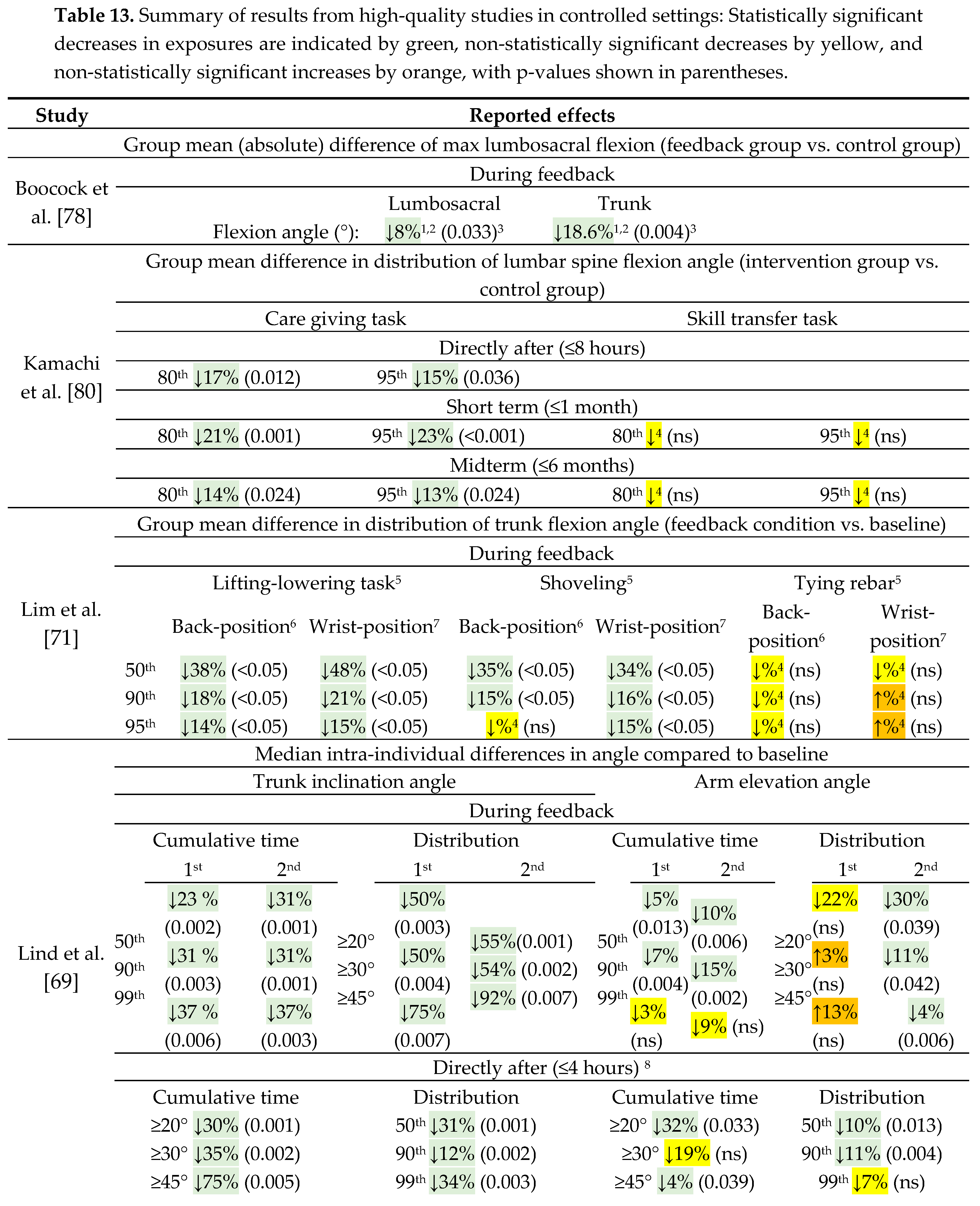
3.5. Summary of the Effectiveness of Feedback in Real Work Environments and in Controlled Settings.
| Study | During feedback | Directly after (≤8 hours) | Very short term (≤1 week) | Short term (≤1 month) |
Midterm (≤6 months) | Long term (≥ 6 months) |
|---|---|---|---|---|---|---|
| Real work environments | ||||||
| Strength of Evidence |
Inconsistent | Very limited | No evidence | No evidence | No evidence | No evidence |
| High quality studies | ||||||
| Lind et al. [73] | ++ | ++ | (+)/= | (+)/= | ||
| Ribeiro et al. [70] | = | = | = | = | = | |
| Moderate quality studies | ||||||
| Bootsman et al. [79] | ++ | (+)/= | ||||
| Controlled settings | ||||||
| Strength of Evidence |
Strong | Strong4 | Limited1 / No evidence2 | Limited1 / No evidence2 | ||
| High quality studies | ||||||
| Boocock et al. [78] | ++ | |||||
| Kamachi et al. [80] | ++ | ++ 1 / = 2 | ++ 1 / = 2 | |||
| Lim et al. [71] | + | |||||
| Lind et al. [69] | ++ | ++ | ||||
| Oppici et al. [83] | ++ | ++ | ||||
| Moderate quality studies | ||||||
| Agruss et al. [77] | +/= | |||||
| Kernozek et al. [81] | * | |||||
| Langenskiöld et al. [72] | + | ++ | ||||
| Lind et al. [82] | ++ | |||||
| Owlia et al. [68] | ++ 3 /= 4 | |||||
| Punt et al. [66] | ++ / + | ++ / + | ||||
4. Discussion
4.1. General Summary of the Findings
4.2. General Interpretation of the Results
4.2.1. Feedback Modalities and Sensors
4.3. Limitations
4.3.1. Limitations of the Evidence
4.3.2. Limitations of the Review Processes
4.4. Practical Implications and Future Research
5. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A. Search Strings in the Literature Search
| "feedback" OR "biofeedback" AND “posture$” OR “postural” OR “movement$” OR “muscle activity” OR “EMG” AND “neck” OR “trunk” OR “spine” OR "back" OR “arm$” or “wrist$” OR “hand$” The following terms were excluded “gait”, “child*”, “rehab*”, “parkinson”, “stroke*”, “cerebral palsy”, “spinal cord injury”, “prosthesis”, and “therap*”. The first two search strings were applied “all fields” while the third as well the exclusion were applied to the abstract. Articles in other language than English was excluded. The search covered the period 2020-01-01 to 2024-06-09. |
| "feedback" OR "biofeedback" AND “posture$” OR “postural” OR “movement$” OR “muscle activity” OR “EMG” AND “neck” OR “trunk” OR “spine” OR "upper back" OR "lower back" OR “arm$” or “wrist$” OR “hand$” The following terms were excluded: “gait”, “child”, “rehab”, “parkinson”, “stroke*”, “cerebral palsy”, “spinal cord injury”, “prosthesis”, “therap*”. The search terms were applied to the abstract. Review articles were excluded. Articles in other language than English was excluded. The search covered the period 2020-01-01 to 2024-06-09. |
Appendix B. The Criteria to Assess the Methodological Quality
| Item | Criteria |
| 1. Clear research question | Clearly stated research question or study objective including a description of the outcome (dependent variable) |
| 2. Clear study population | Clearly defined study population and inclusion/exclusion criteria, and consistently applied inclusion/exclusion criteria |
| 3. Participation rate | Participation rate ≥50% of eligible persons of the identified pool of eligible persons |
| 4. Subjects recruitment | Subjects recruited from the same/similar populations, with uniformly applied inclusion/exclusion criteria |
| 5. Justified sample size | Sample size sufficiently justified, and large enough to detect difference in the outcome with at least 80% power |
| 6. Temporality of exposure(s) and outcome(s) | Exposure(s) measured before outcome(s) |
| 7. Sufficient time | Timeframe for feedback described and sufficient long to induce behavioral changes |
| 8. Dependent variable scaling | Dependent variable (e.g., posture, movements or muscle activity) assessed on a continuous or categorical scale |
| 9. Independent variables treatment | Relevant independent variables controlled or measured (as minimum. the amount of work performed per time unit, and clearly defined and consistently implemented feedback trigger) |
| 10. Assessment of dependent variable | Dependent variable(s) assessed more than one time |
| 11.Assessment of dependent variable | Dependent variable clearly defined and adequately assessed |
| 12. Blinding | Assessors blinded to the participants' group allocation |
| 13. Loss to follow-up | Data from at least 80% of participants were included in the final analysis |
| 14. Control of confounders | Key confounding variables that could alter the outcome results were adjusted for |
| Item | Criteria |
| 1. Study description | Study described as a randomized controlled trial and provides adequate details of the study design |
| 2. Randomization | Suitable randomization was employed, such as computer-generated random allocation of participants |
| 3. Concealed allocation | Concealed process of assigning participants to group allocation |
| 4. Blinding (providers and participants) | Blinding (group assignment) of both administrator of the intervention and the participants receiving the intervention |
| 5. Blinding (assessors) | Blinding of assessors evaluating outcomes to participants' group allocation |
| 6. Baseline characteristics | Baseline characteristics reported and balanced between groups, such as age, gender, experience, occupation, job exposure, and disorders |
| 7. Endpoint dropout | The dropout rate ≤20% at the end of the study for each group |
| 8. Endpoint dropout (between groups) | Dropout rate ≤15% between groups at the end of the study |
| 9. Adherence | Adherence to the intervention protocol by participants in all group |
| 10. Confounding interventions | No additional interventions that could confound the study results were occurring, or any such interventions were similar between groups |
| 11. Quality of outcomes assessment | Dependent variable(s) measured using accurate and precise tools/methods |
| 12. Justified sample size | Sample size sufficiently justified, and large enough to detect difference in the outcome between groups with at least 80% power |
| 13. Prespecified analysis | Predetermined analysis of the outcomes |
| 14. Group assignment | Participants analyzed based on their original group allocation |
References
- WHO. Musculoskeletal health. Availabe online: https://www.who.int/news-room/fact-sheets/detail/musculoskeletal-conditions. (accessed on 23 November 2022).
- Kassebaum, N.J.; Arora, M.; Barber, R.M.; Bhutta, Z.A.; Brown, J.; Carter, A.; Casey, D.C.; Charlson, F.J.; Coates, M.M.; Coggeshall, M. , et al. Global, regional, and national disability-adjusted life-years (DALYs) for 315 diseases and injuries and healthy life expectancy (HALE), 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. The Lancet 2016, 388, 1603–1658. [Google Scholar] [CrossRef]
- Tompa, E.; Mofidi, A.; van den Heuvel, S.; van Bree, T.; Michaelsen, F.; Jung, Y.; Porsch, L.; van Emmerik, M. The value of occupational safety and health and the societal costs of work-related injuries and diseases; Publications Office of the European Union: Luxembourg (LU), 2019. [Google Scholar] [CrossRef]
- Sundstrup, E.; Andersen, L.L. Joint association of physical and psychosocial working conditions with risk of long-term sickness absence: Prospective cohort study with register follow-up. Scand J Public Health 2021, 49, 132–140. [Google Scholar] [CrossRef] [PubMed]
- Pedersen, J.; Bjorner, J.B.; Andersen, L.L. Physical work demands and expected labor market affiliation (ELMA): Prospective cohort with register-follow-up among 46 169 employees. Scand J Work Environ Health 2022, 48, 641–650. [Google Scholar] [CrossRef]
- Badarin, K.; Hemmingsson, T.; Hillert, L.; Kjellberg, K. The impact of musculoskeletal pain and strenuous work on self-reported physical work ability: a cohort study of Swedish men and women. Int Arch Occup Environ Health 2022, 95, 939–952. [Google Scholar] [CrossRef] [PubMed]
- NRC. Musculoskeletal disorders and the workplace: low back and upper extremities; National Academies Press: Washington (DC), 2001. [Google Scholar]
- Widanarko, B.; Legg, S.; Devereux, J.; Stevenson, M. The combined effect of physical, psychosocial/organisational and/or environmental risk factors on the presence of work-related musculoskeletal symptoms and its consequences. Appl Ergon 2014, 45, 1610–1621. [Google Scholar] [CrossRef] [PubMed]
- Hauke, A.; Flintrop, J.; Brun, E.; Rugulies, R. The impact of work-related psychosocial stressors on the onset of musculoskeletal disorders in specific body regions: A review and metaanalysis of 54 longitudinal studies. Work Stress 2011, 25, 243–256. [Google Scholar] [CrossRef]
- NIOSH. Musculoskeletal Disorders and Workplace Factors.; National Institute for Occupational Safety and Health: Cincinnati, 1997. [Google Scholar]
- van Rijn, R.M.; Huisstede, B.M.; Koes, B.W.; Burdorf, A. Associations between work-related factors and the carpal tunnel syndrome--a systematic review. Scand J Work Environ Health 2009, 35, 19–36. [Google Scholar] [CrossRef]
- da Costa, B.R.; Vieira, E.R. Risk factors for work-related musculoskeletal disorders: A systematic review of recent longitudinal studies. Am J Ind Med 2010, 53, 285–323. [Google Scholar] [CrossRef]
- Garg, A.; Boda, S.; Hegmann, K.T.; Moore, J.S.; Kapellusch, J.M.; Bhoyar, P.; Thiese, M.S.; Merryweather, A.; Deckow-Schaefer, G.; Bloswick, D. , et al. The NIOSH lifting equation and low-back pain, part 1: Association with low-back pain in the BackWorks prospective cohort study. Hum Factors 2014, 56, 6–28. [Google Scholar] [CrossRef]
- Garg, A.; Kapellusch, J.M.; Hegmann, K.T.; Moore, J.S.; Boda, S.; Bhoyar, P.; Thiese, M.S.; Merryweather, A.; Deckow-Schaefer, G.; Bloswick, D. , et al. The NIOSH lifting equation and low-back pain, Part 2: Association with seeking care in the backworks prospective cohort study. Hum Factors 2014, 56, 44–57. [Google Scholar] [CrossRef]
- Hoozemans, M.J.; Knelange, E.B.; Frings-Dresen, M.H.; Veeger, H.E.; Kuijer, P.P. Are pushing and pulling work-related risk factors for upper extremity symptoms? A systematic review of observational studies. Occup Environ Med 2014, 71, 788–795. [Google Scholar] [CrossRef] [PubMed]
- Kozak, A.; Schedlbauer, G.; Wirth, T.; Euler, U.; Westermann, C.; Nienhaus, A. Association between work-related biomechanical risk factors and the occurrence of carpal tunnel syndrome: An overview of systematic reviews and a meta-analysis of current research. BMC Musculoskelet Disord 2015, 16. [Google Scholar] [CrossRef] [PubMed]
- Fox, R.R.; Lu, M.L.; Occhipinti, E.; Jaeger, M. Understanding outcome metrics of the revised NIOSH lifting equation. Appl Ergon 2019, 81, 102897. [Google Scholar] [CrossRef]
- Jahn, A.; Andersen, J.H.; Christiansen, D.H.; Seidler, A.; Dalbøge, A. Occupational mechanical exposures as risk factor for chronic low-back pain: a systematic review and meta-analysis. Scand J Work Environ Health 2023, 49, 453–465. [Google Scholar] [CrossRef]
- Hoogendoorn, W.E.; Bongers, P.M.; de Vet, H.C.; Douwes, M.; Koes, B.W.; Miedema, M.C.; Ariëns, G.A.; Bouter, L.M. Flexion and rotation of the trunk and lifting at work are risk factors for low back pain: results of a prospective cohort study. Spine (Phila Pa 1976) 2000, 25, 3087–3092. [Google Scholar] [CrossRef]
- Gupta, N.; Bjerregaard, S.S.; Yang, L.; Forsman, M.; Rasmussen, C.L.; Rasmussen, C.D.N.; Clays, E.; Holtermann, A. Does occupational forward bending of the back increase long-term sickness absence risk? A 4-year prospective register-based study using device-measured compositional data analysis. Scand J Work Environ Health 2022, 48, 651–661. [Google Scholar] [CrossRef] [PubMed]
- Gupta, N.; Rasmussen, C.L.; Forsman, M.; Søgaard, K.; Holtermann, A. How does accelerometry-measured arm elevation at work influence prospective risk of long-term sickness absence? Scand J Work Environ Health 2022, 48, 137–147. [Google Scholar] [CrossRef]
- Versloot, A.H.C.; Jackson, J.A.; van Rijn, R.M.; Elbers, R.G.; Søgaard, K.; Macri, E.M.; Koes, B.; Burdorf, A.; Chiarotto, A.; Gerger, H. Physical and psychosocial work-related exposures and the occurrence of disorders of the shoulder: A systematic review update. Appl Ergon 2024, 118, 104277. [Google Scholar] [CrossRef]
- Nilsson, T.; Wahlström, J.; Burström, L. Hand-arm vibration and the risk of vascular and neurological diseases-A systematic review and meta-analysis. PLoS One 2017, 12, e0180795. [Google Scholar] [CrossRef]
- Burström, L.; Nilsson, T.; Wahlström, J. Whole-body vibration and the risk of low back pain and sciatica: a systematic review and meta-analysis. Int Arch Occup Environ Health 2015, 88, 403–418. [Google Scholar] [CrossRef]
- Lind, C.M.; Rose, L.M. Shifting to proactive risk management: Risk communication using the RAMP tool. Agron Res 2016, 14, 513–524. [Google Scholar]
- Lind, C.M.; Forsman, M.; Rose, L.M. Development and evaluation of RAMP I - a practitioner's tool for screening of musculoskeletal disorder risk factors in manual handling. Int J Occup Saf Ergon 2019, 25, 165–180. [Google Scholar] [CrossRef]
- Lind, C.M.; Forsman, M.; Rose, L.M. Development and evaluation of RAMP II - a practitioner’s tool for assessing musculoskeletal disorder risk factors in industrial manual handling. Ergonomics 2020, 63, 477–504. [Google Scholar] [CrossRef]
- Macdonald, W.; Oakman, J. The problem with "ergonomics injuries": What can ergonomists do? Appl Ergon 2022, 103, 103774. [Google Scholar] [CrossRef] [PubMed]
- Rose, L.M.; Eklund, J.; Nord Nilsson, L.; Barman, L.; Lind, C.M. The RAMP package for MSD risk management in manual handling – A freely accessible tool, with website and training courses. Appl Ergon 2020, 86, 103101. [Google Scholar] [CrossRef]
- Eliasson, K.; Lind, C.M.; Nyman, T. Factors influencing ergonomists' use of observation-based risk-assessment tools. Work 2019, 64, 93–106. [Google Scholar] [CrossRef] [PubMed]
- Abdul Halim, N.S.S.; Ripin, Z.M.; Ridzwan, M.I.Z. Effects of patient transfer devices on the risk of work-related musculoskeletal disorders: a systematic review. Int J Occup Saf Ergon 2023, 29, 494–514. [Google Scholar] [CrossRef] [PubMed]
- van der Molen, H.F.; Sluiter, J.K.; Hulshof, C.T.; Vink, P.; Frings-Dresen, M.H. Effectiveness of measures and implementation strategies in reducing physical work demands due to manual handling at work. Scand J Work Environ Health 2005, 31 Suppl 2, 75–87. [Google Scholar]
- Marras, W.S.; Allread, W.G.; Burr, D.L.; Fathallah, F.A. Prospective validation of a low-back disorder risk model and assessment of ergonomic interventions associated with manual materials handling tasks. Ergonomics 2000, 43, 1866–1886. [Google Scholar] [CrossRef]
- Zare, M.; Black, N.; Sagot, J.-C.; Hunault, G.; Roquelaure, Y. Ergonomics interventions to reduce musculoskeletal risk factors in a truck manufacturing plant. Int J Ind Ergon 2020, 75, 102896. [Google Scholar] [CrossRef]
- Hoe, V.C.; Urquhart, D.M.; Kelsall, H.L.; Sim, M.R. Ergonomic design and training for preventing work-related musculoskeletal disorders of the upper limb and neck in adults. Cochrane Database Syst Rev 2012, 2012, Cd008570. [Google Scholar] [CrossRef]
- Ouellet, S.; Vézina, N. Work training and MSDs prevention: Contribution of ergonomics. Int J Ind Ergon 2014, 44, 24–31. [Google Scholar] [CrossRef]
- Denis, D.; St-Vincent, M.; Imbeau, D.; Jetté, C.; Nastasia, I. Intervention practices in musculoskeletal disorder prevention: a critical literature review. Appl Ergon 2008, 39, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Denis, D.; Gonella, M.; Comeau, M.; Lauzier, M. Questioning the value of manual material handling training: a scoping and critical literature review. Appl Ergon 2020, 89, 103186. [Google Scholar] [CrossRef] [PubMed]
- EU. Council Directive 90/269/EEC of 29 May 1990 on the minimum health and safety requirements for the manual handling of loads where there is a risk particularly of back injury to workers.; Publications Office of the European Union: Luxemburg (LU), 1990. [Google Scholar]
- McGill, S.M. Evolving ergonomics? Ergonomics 2009, 52, 80–86. [Google Scholar] [CrossRef] [PubMed]
- Plamondon, A.; Denis, D.; Delisle, A.; Lariviere, C.; Salazar, E. Biomechanical differences between expert and novice workers in a manual material handling task. Ergonomics 2010, 53, 1239–1253. [Google Scholar] [CrossRef]
- Marras, W.S.; Walter, B.A.; Purmessur, D.; Mageswaran, P.; Wiet, M.G. The Contribution of Biomechanical-Biological Interactions of the Spine to Low Back Pain. Hum Factors 2016, 58, 965–975. [Google Scholar] [CrossRef]
- Kumar, S. Ergonomics and biology of spinal rotation. Ergonomics 2004, 47, 370–415. [Google Scholar] [CrossRef]
- Clemes, S.A.; Haslam, C.O.; Haslam, R.A. What constitutes effective manual handling training? A systematic review. Occup Med (Lond) 2010, 60, 101–107. [Google Scholar] [CrossRef]
- Verbeek, J.H.; Martimo, K.P.; Karppinen, J.; Kuijer, P.P.; Viikari-Juntura, E.; Takala, E.P. Manual material handling advice and assistive devices for preventing and treating back pain in workers. Cochrane Database Syst Rev 2011. [Google Scholar] [CrossRef]
- Hogan, D.A.; Greiner, B.A.; O'Sullivan, L. The effect of manual handling training on achieving training transfer, employee's behaviour change and subsequent reduction of work-related musculoskeletal disorders: a systematic review. Ergonomics 2014, 57, 93–107. [Google Scholar] [CrossRef]
- Lind, C.M.; Abtahi, F.; Forsman, M. Wearable Motion Capture Devices for the Prevention of Work-Related Musculoskeletal Disorders in Ergonomics-An Overview of Current Applications, Challenges, and Future Opportunities. Sensors (Basel) 2023, 23. [Google Scholar] [CrossRef] [PubMed]
- Ranavolo, A.; Draicchio, F.; Varrecchia, T.; Silvetti, A.; Iavicoli, S. Wearable monitoring devices for biomechanical risk assessment at work: Current status and future challenges-a systematic review. Int J Environ Res Public Health 2018, 15. [Google Scholar] [CrossRef] [PubMed]
- Stefana, E.; Marciano, F.; Rossi, D.; Cocca, P.; Tomasoni, G. Wearable Devices for Ergonomics: A Systematic Literature Review. Sensors (Basel) 2021, 21. [Google Scholar] [CrossRef]
- Figueira, V.; Silva, S.; Costa, I.; Campos, B.; Salgado, J.; Pinho, L.; Freitas, M.; Carvalho, P.; Marques, J.; Pinho, F. Wearables for Monitoring and Postural Feedback in the Work Context: A Scoping Review. Sensors (Basel) 2024, 24. [Google Scholar] [CrossRef] [PubMed]
- Thomas, R.E.; Vaidya, S.C.; Herrick, R.T.; Congleton, J.J. The effects of biofeedback on carpal tunnel syndrome. Ergonomics 1993, 36, 353–361. [Google Scholar] [CrossRef]
- Akamatsu, M.; MacKenzie, I.S.; Hasbroucq, T. A comparison of tactile, auditory, and visual feedback in a pointing task using a mouse-type device. Ergonomics 1995, 38, 816–827. [Google Scholar] [CrossRef]
- Faucett, J.; Garry, M.; Nadler, D.; Ettare, D. A test of two training interventions to prevent work-related musculoskeletal disorders of the upper extremity. Appl Ergon 2002, 33, 337–347. [Google Scholar] [CrossRef]
- De Kraker, H.; De Korte, E.; Van Mil, F.; Rijs, B.; Bongers, P. The effect of a feedback signal in a computer mouse on hovering behaviour, productivity, comfort and usability in a field study. Ergonomics 2008, 51, 140–155. [Google Scholar] [CrossRef]
- Lindegård, A.; Grimby-Ekman, A.; Wahlström, J.; Gustafsson, E. Can biofeedback training in combination with ergonomic information reduce pain among young adult computer users with neck and upper extremity symptoms? - A randomized controlled intervention study. Appl Ergon 2024, 114, 104155. [Google Scholar] [CrossRef]
- Bazazan, A.; Dianat, I.; Feizollahi, N.; Mombeini, Z.; Shirazi, A.M.; Castellucci, H.I. Effect of a posture correction-based intervention on musculoskeletal symptoms and fatigue among control room operators. Appl Ergon 2019, 76, 12–19. [Google Scholar] [CrossRef] [PubMed]
- King, T.K.; Severin, C.N.; Van Eerd, D.; Ibrahim, S.; Cole, D.; Amick, B., 3rd; Steenstra, I.A. A pilot randomised control trial of the effectiveness of a biofeedback mouse in reducing self-reported pain among office workers. Ergonomics 2013, 56, 59–68. [Google Scholar] [CrossRef]
- Meijer, E.M.; Sluiter, J.K.; Frings-Dresen, M.H. Effectiveness of a feedback signal in a computer mouse on upper extremity musculoskeletal symptoms: a randomised controlled trial with an 8-month follow-up. Occup Environ Med 2009, 66, 305–311. [Google Scholar] [CrossRef] [PubMed]
- Zadeh, S.M.; MacDermid, J.; Johnson, J.; Birmingham, T.B.; Shafiee, E. Applications of wearable sensors in upper extremity MSK conditions: a scoping review. J Neuroeng Rehabil 2023, 20, 158. [Google Scholar] [CrossRef]
- Martins, D.R.; Cerqueira, S.M.; Santos, C.P. Combining inertial-based ergonomic assessment with biofeedback for posture correction: A narrative review. Comput Ind Eng 2024, 190, 110037. [Google Scholar] [CrossRef]
- García-Jaén, M.; Sebastia-Amat, S.; Sanchis-Soler, G.; Cortell-Tormo, J.M. Lumbo-Pelvic Rhythm Monitoring Using Wearable Technology with Sensory Biofeedback: A Systematic Review. Healthc Inform Res 2024, 12, 758. [Google Scholar] [CrossRef] [PubMed]
- Frasie, A.; Houry, M.; Plourde, C.; Robert, M.T.; Bouyer, L.J.; Roy, J.S. Feedback for the prevention and rehabilitation of work-related musculoskeletal disorders: A systematic review. Work 2023, 76, 61–94. [Google Scholar] [CrossRef] [PubMed]
- Lind, C.M. A Rapid Review on the Effectiveness and Use of Wearable Biofeedback Motion Capture Systems in Ergonomics to Mitigate Adverse Postures and Movements of the Upper Body. Sensors (Basel) 2024, 24, 3345. [Google Scholar] [CrossRef]
- Simpson, L.; Maharaj, M.M.; Mobbs, R.J. The role of wearables in spinal posture analysis: a systematic review. BMC Musculoskelet Disord 2019, 20, 55. [Google Scholar] [CrossRef]
- Lee, R.; James, C.; Edwards, S.; Skinner, G.; Young, J.L.; Snodgrass, S.J. Evidence for the Effectiveness of Feedback from Wearable Inertial Sensors during Work-Related Activities: A Scoping Review. Sensors (Basel) 2021, 21. [Google Scholar] [CrossRef]
- Punt, M.; Nematimoez, M.; van Dieën, J.H.; Kingma, I. Real-time feedback to reduce low-back load in lifting and lowering. J Biomech 2020, 102, 109513. [Google Scholar] [CrossRef] [PubMed]
- Brandl, C.; Brunner, O.; Marzaroli, P.; Hellig, T.; Johnen, L.; Mertens, A.; Tarabini, M.; Nitsch, V. Using real-time feedback of L5/S1 compression force based on markerless optical motion capture to improve the lifting technique in manual materials handling. Int J Ind Ergon 2022, 91, 103350. [Google Scholar] [CrossRef]
- Owlia, M.; Kamachi, M.; Dutta, T. Reducing lumbar spine flexion using real-time biofeedback during patient handling tasks. Work 2020, 66, 41–51. [Google Scholar] [CrossRef] [PubMed]
- Lind, C.M.; Yang, L.; Abtahi, F.; Hanson, L.; Lindecrantz, K.; Lu, K.; Forsman, M.; Eklund, J. Reducing postural load in order picking through a smart workwear system using real-time vibrotactile feedback. Appl Ergon 2020, 89, 103188. [Google Scholar] [CrossRef]
- Ribeiro, D.C.; Milosavljevic, S.; Terry, J.; Abbott, J.H. Effectiveness of a lumbopelvic monitor and feedback device to change postural behaviour: the ELF cluster randomised controlled trial. Occup Environ Med 2020, 77, 462–469. [Google Scholar] [CrossRef]
- Lim, S.; Yang, X. Real-time vibrotactile feedback system for reducing trunk flexion exposure during construction tasks. Appl Ergon 2023, 110, 104019. [Google Scholar] [CrossRef]
- Langenskiöld, C.; Berg, A.; Yang, L. The Effect of Corrective and Encouraging Accumulated Vibrotactile Feedback on Work Technique Training and Motivation-A Pilot Study. Int J Environ Res Public Health 2023, 20. [Google Scholar] [CrossRef]
- Lind, C.M.; De Clercq, B.; Forsman, M.; Grootaers, A.; Verbrugghe, M.; Van Dyck, L.; Yang, L. Effectiveness and usability of real-time vibrotactile feedback training to reduce postural exposure in real manual sorting work. Ergonomics 2023, 66, 198–216. [Google Scholar] [CrossRef]
- Garritty, C.; Gartlehner, G.; Nussbaumer-Streit, B.; King, V.J.; Hamel, C.; Kamel, C.; Affengruber, L.; Stevens, A. Cochrane Rapid Reviews Methods Group offers evidence-informed guidance to conduct rapid reviews. J Clin Epidemiol 2021, 130, 13–22. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E. , et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- National Heart, Lung, and Blood Institute (NHLBI), Study Quality Assessment Tools. Availabe online: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools. (accessed on 20 November 2023).
- Agruss, C.D.; Williams, K.; Fathallah, F.A. The effect of feedback training on lumbosacral compression during simulated occupational lifting. Ergonomics 2004, 47, 1103–1115. [Google Scholar] [CrossRef]
- Boocock, M.; Naudé, Y.; Taylor, S.; Kilby, J.; Mawston, G. Influencing lumbar posture through real-time biofeedback and its effects on the kinematics and kinetics of a repetitive lifting task. Gait Posture 2019, 73, 93–100. [Google Scholar] [CrossRef]
- Bootsman, R.; Markopoulos, P.; Qi, Q.; Wang, Q.; Timmermans, A.A.A. Wearable technology for posture monitoring at the workplace. Int J Hum Comput Stud 2019, 132, 99–111. [Google Scholar] [CrossRef]
- Kamachi, M.; Owlia, M.; Dutta, T. Evaluating a wearable biofeedback device for reducing end-range sagittal lumbar spine flexion among home caregivers. Appl Ergon 2021, 97, 103547. [Google Scholar] [CrossRef] [PubMed]
- Kernozek, T.; Iwasaki, M.; Fater, D.; Durall, C.; Langenhorst, B. Movement-based feedback may reduce spinal moments in male workers during lift and lowering tasks. Physiother Res Int 2006, 11, 140–147. [Google Scholar] [CrossRef] [PubMed]
- Lind, C.M.; Diaz-Olivares, J.A.; Lindecrantz, K.; Eklund, J. A Wearable Sensor System for Physical Ergonomics Interventions Using Haptic Feedback. Sensors (Basel) 2020, 20, 6010. [Google Scholar] [CrossRef] [PubMed]
- Oppici, L.; Grütters, K.; Garofolini, A.; Rosenkranz, R.; Narciss, S. Deliberate Practice and Motor Learning Principles to Underpin the Design of Training Interventions for Improving Lifting Movement in the Occupational Sector: A Perspective and a Pilot Study on the Role of Augmented Feedback. Frontiers in sports and active living 2021, 3, 746142. [Google Scholar] [CrossRef] [PubMed]
- Ribeiro, D.C.; Sole, G.; Abbott, J.H.; Milosavljevic, S. The effectiveness of a lumbopelvic monitor and feedback device to change postural behavior: a feasibility randomized controlled trial. J Orthop Sports Phys Ther 2014, 44, 702–711. [Google Scholar] [CrossRef]
- Marras, W.S.; Schoenmarclin, R.W. Wrist motions in industry. Ergonomics 1993, 36, 341–351. [Google Scholar] [CrossRef]
- Marras, W.S.; Lavender, S.A.; Leurgans, S.E.; Rajulu, S.L.; Allread, W.G.; Fathallah, F.A.; Ferguson, S.A. The role of dynamic three-dimensional trunk motion in occupationally-related low back disorders. The effects of workplace factors, trunk position, and trunk motion characteristics on risk of injury. Spine (Phila Pa 1976) 1993, 18, 617–628. [Google Scholar] [CrossRef]
- Nordander, C.; Ohlsson, K.; Akesson, I.; Arvidsson, I.; Balogh, I.; Hansson, G.; Strömberg, U.; Rittner, R.; Skerfving, S. Exposure-response relationships in work-related musculoskeletal disorders in elbows and hands - A synthesis of group-level data on exposure and response obtained using uniform methods of data collection. Appl Ergon 2013, 44, 241–253. [Google Scholar] [CrossRef] [PubMed]
- Nordander, C.; Hansson, G.Å.; Ohlsson, K.; Arvidsson, I.; Balogh, I.; Strömberg, U.; Rittner, R.; Skerfving, S. Exposure–response relationships for work-related neck and shoulder musculoskeletal disorders – Analyses of pooled uniform data sets. Appl Ergon 2016, 55, 70–84. [Google Scholar] [CrossRef] [PubMed]
- Balogh, I.; Arvidsson, I.; Björk, J.; Hansson, G.Å.; Ohlsson, K.; Skerfving, S.; Nordander, C. Work-related neck and upper limb disorders - Quantitative exposure-response relationships adjusted for personal characteristics and psychosocial conditions. BMC Musculoskelet Disord 2019, 20. [Google Scholar] [CrossRef] [PubMed]
- Arvidsson, I.; Dahlqvist, C.; Enquist, H.; Nordander, C. Action Levels for the Prevention of Work-Related Musculoskeletal Disorders in the Neck and Upper Extremities: A Proposal. Ann Work Expo Health 2021, 65, 741–747. [Google Scholar] [CrossRef]
- Fan, X.; Lind, C.M.; Rhen, I.M.; Forsman, M. Effects of Sensor Types and Angular Velocity Computational Methods in Field Measurements of Occupational Upper Arm and Trunk Postures and Movements. Sensors (Basel) 2021, 21. [Google Scholar] [CrossRef]
- Forsman, M.; Fan, X.; Rhén, I.M.; Lind, C.M. Concerning a Work Movement Velocity Action Level Proposed in "Action Levels for the Prevention of Work-Related Musculoskeletal Disorders in the Neck and Upper Extremities: A Proposal" by Inger Arvidsson et al. (2021). Ann Work Expo Health 2022, 66, 130–131. [Google Scholar] [CrossRef]
- Forsman, M.; Fan, X.; Rhen, I.-M.; Lind, C.M. Mind the gap – development of conversion models between accelerometer- and IMU-based measurements of arm and trunk postures and movements in warehouse work. Appl Ergon 2022, 105, 103841. [Google Scholar] [CrossRef]
- Lavender, S.A.; Lorenz, E.; Andersson, G.B.J. Training in lifting. Prof Saf 2002, 47, 30–35. [Google Scholar]
- Lavender, S.A.; Lorenz, E.P.; Andersson, G.B. Can a new behaviorally oriented training process to improve lifting technique prevent occupationally related back injuries due to lifting? Spine (Phila Pa 1976) 2007, 32, 487–494. [Google Scholar] [CrossRef]
- Doss, R.; Robathan, J.; Abdel-Malek, D.; Holmes, M.W.R. Posture Coaching and Feedback during Patient Handling in a Student Nurse Population. IISE Trans Occup Ergon Hum Factors 2018, 6, 116–127. [Google Scholar] [CrossRef]
- van Tulder, M.; Furlan, A.; Bombardier, C.; Bouter, L. Updated method guidelines for systematic reviews in the Cochrane Collaboration Back Review Group. Spine (Phila Pa 1976) 2003, 28, 1290–1299. [Google Scholar] [CrossRef] [PubMed]
- Furlan, A.D.; Malmivaara, A.; Chou, R.; Maher, C.G.; Deyo, R.A.; Schoene, M.; Bronfort, G.; van Tulder, M.W. 2015 Updated Method Guideline for Systematic Reviews in the Cochrane Back and Neck Group. Spine (Phila Pa 1976) 2015, 40, 1660–1673. [Google Scholar] [CrossRef] [PubMed]
- Guyatt, G.H.; Oxman, A.D.; Vist, G.E.; Kunz, R.; Falck-Ytter, Y.; Alonso-Coello, P.; Schünemann, H.J. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008, 336, 924–926. [Google Scholar] [CrossRef]
- Humadi, A.; Nazarahari, M.; Ahmad, R.; Rouhani, H. In-field instrumented ergonomic risk assessment: Inertial measurement units versus Kinect V2. Int J Ind Ergon 2021, 84, 103147. [Google Scholar] [CrossRef]
- Marras, W.S. The complex spine: The multidimensional system of causal pathways for low-back disorders. Hum Factors 2012, 54, 881–889. [Google Scholar] [CrossRef]
- Gallagher, S.; Marras, W.S.; Litsky, A.S.; Burr, D. Torso flexion loads and the fatigue failure of human lumbosacral motion segments. Spine (Phila Pa 1976) 2005, 30, 2265–2273. [Google Scholar] [CrossRef]
- Andersen, J.H.; Kaergaard, A.; Mikkelsen, S.; Jensen, U.F.; Frost, P.; Bonde, J.P.; Fallentin, N.; Thomsen, J.F. Risk factors in the onset of neck/shoulder pain in a prospective study of workers in industrial and service companies. Occup Environ Med 2003, 60, 649–654. [Google Scholar] [CrossRef]
- Ariëns, G.A.; Bongers, P.M.; Hoogendoorn, W.E.; van der Wal, G.; van Mechelen, W. High physical and psychosocial load at work and sickness absence due to neck pain. Scand J Work Environ Health 2002, 28, 222–231. [Google Scholar] [CrossRef]
- Mayer, J.; Kraus, T.; Ochsmann, E. Longitudinal evidence for the association between work-related physical exposures and neck and/or shoulder complaints: a systematic review. Int Arch Occup Environ Health 2012, 85, 587–603. [Google Scholar] [CrossRef]
- Baer, J.L.; Vasavada, A.; Cohen, R.G. Posture biofeedback increases cognitive load. Psychological research 2022, 86, 1892–1903. [Google Scholar] [CrossRef]
- Padula, R.S.; Comper, M.L.C.; Sparer, E.H.; Dennerlein, J.T. Job rotation designed to prevent musculoskeletal disorders and control risk in manufacturing industries: A systematic review. Appl Ergon 2017, 58, 386–397. [Google Scholar] [CrossRef]
- Wong, W.C.; Cheung, C.S.; Hart, G.J. Development of a quality assessment tool for systematic reviews of observational studies (QATSO) of HIV prevalence in men having sex with men and associated risk behaviours. Emerging themes in epidemiology 2008, 5, 23. [Google Scholar] [CrossRef] [PubMed]
- Breen, P.P.; Nisar, A.; Olaighin, G. Evaluation of a single accelerometer based biofeedback system for real-time correction of neck posture in computer users. Annu Int Conf IEEE Eng Med Biol Soc 2009, 2009, 7269–7272. [Google Scholar] [CrossRef]
- Tino, A.; Carvalho, M.; Preto, N.F.; McConville, K.M. Wireless vibrotactile feedback system for postural response improvement. Annu Int Conf IEEE Eng Med Biol Soc 2011, 2011, 5203–5206. [Google Scholar] [CrossRef] [PubMed]
- Vignais, N.; Miezal, M.; Bleser, G.; Mura, K.; Gorecky, D.; Marin, F. Innovative system for real-time ergonomic feedback in industrial manufacturing. Appl Ergon 2013, 44, 566–574. [Google Scholar] [CrossRef] [PubMed]
- Hermanis, A.; Nesenbergs, K.; Cacurs, R.; Greitans, M.J.J.o.m.; bioengineering. Wearable Posture Monitoring System with Biofeedback via Smartphone. J Biomed Eng 2013, 2, 40–44. [Google Scholar] [CrossRef]
- Cerqueira, S.M.; Silva, A.F.D.; Santos, C.P. Smart Vest for Real-Time Postural Biofeedback and Ergonomic Risk Assessment. IEEE Access 2020, 8, 107583–107592. [Google Scholar] [CrossRef]
- Ferrone, A.; García Patiño, A.; Menon, C. Low Back Pain-Behavior Correction by Providing Haptic Feedbacks: A Preliminary Investigation. Sensors (Basel) 2021, 21. [Google Scholar] [CrossRef] [PubMed]
- Kim, W.; Ruiz Garate, V.; Gandarias, J.M.; Lorenzini, M.; Ajoudani, A. A Directional Vibrotactile Feedback Interface for Ergonomic Postural Adjustment. IEEE Trans Haptics 2022, 15, 200–211. [Google Scholar] [CrossRef]
- Lind, C.M.; Sandsjö, L.; Mahdavian, N.; Högberg, D.; Hanson, L.; Diaz Olivares, J.A.; Yang, L.; Forsman, M. Prevention of Work-Related Musculoskeletal Disorders Using Smart Workwear – The Smart Workwear Consortium. In Human Systems Engineering and Design, Ahram, T., Karwowski, W., Taiar, R., Eds. Springer: Cham, 2019; Vol. 876, pp. 477-483.
- Lind, C.M.; De Clercq, B.; Forsman, M.; Grootaers, A.; Verbrugghe, M.; Van Dyck, L.; Yang, L. Reducing postural exposure in real manual sorting work by means of real time vibrotactile feedback training. Saf Health Work 2022, 13, S147–S148. [Google Scholar] [CrossRef]
- Lind, C.M.; Forsman, M.; Lindecrantz, K.; Eklund, J.A.E. Reducing postural exposure in manual handling – effects of vibrotactile feedback and verbal instructions. In Proceedings of the 50th Nordic Ergonomics and Human Factors Society Conference, Lindblom, J., Österman, C., Eds. Technical University of Denmark: Elsinore, Denmark, 2019.
- Ailneni, R.C.; Syamala, K.R.; Kim, I.S.; Hwang, J. Influence of the wearable posture correction sensor on head and neck posture: Sitting and standing workstations. Work 2019, 62, 27–35. [Google Scholar] [CrossRef] [PubMed]
- Kuo, Y.L.; Huang, K.Y.; Kao, C.Y.; Tsai, Y.J. Sitting Posture during Prolonged Computer Typing with and without a Wearable Biofeedback Sensor. Int J Environ Res Public Health 2021, 18. [Google Scholar] [CrossRef] [PubMed]
- Thanathornwong, B.; Suebnukarn, S.; Ouivirach, K. A system for predicting musculoskeletal disorders among dental students. Int J Occup Saf Ergon 2014, 20, 463–475. [Google Scholar] [CrossRef] [PubMed]
- Thanathornwong, B.; Suebnukarn, S. The Improvement of Dental Posture Using Personalized Biofeedback. Stud Health Technol Inform 2015, 216, 756–760. [Google Scholar] [CrossRef]
- Thanathornwong, B.; Jalayondeja, W. Vibrotactile -Feedback Device for Postural Balance Among Malocclusion Patients. IEEE journal of translational engineering in health and medicine 2020, 8, 2100406. [Google Scholar] [CrossRef]
- Thanathornwong, B.; Suebnukarn, S. A Personalized Pre-operative and Intra-operative Ergonomic Feedback to Improve the Dental Work Posture. Int J Hum Comput 2021, 37, 528–533. [Google Scholar] [CrossRef]
- Pinto, B.L.; Beaudette, S.M.; Brown, S.H.M. Tactile cues can change movement: An example using tape to redistribute flexion from the lumbar spine to the hips and knees during lifting. Hum Mov Sci 2018, 60, 32–39. [Google Scholar] [CrossRef]
- Larson, D.J.; Brown, S.H.M. Effects of trunk extensor muscle fatigue on repetitive lift (re)training using an augmented tactile feedback approach. Ergonomics 2023, 66, 1919–1934. [Google Scholar] [CrossRef]
- Grütters, K.; Narciss, S.; Beaudette, S.M.; Oppici, L. Reducing Lumbar Flexion in a Repetitive Lifting Task: Comparison of Leukotape and Kinesio Tape and Their Effect on Lumbar Proprioception. 2023, 13, 5908. [CrossRef]
- Chan, V.C.H.; Welsh, T.N.; Tremblay, L.; Frost, D.M.; Beach, T.A.C. A comparison of augmented feedback and didactic training approaches to reduce spine motion during occupational lifting tasks. Appl Ergon 2022, 99, 103612. [Google Scholar] [CrossRef]
- NIOSH. Hierarchy of Controls. Availabe online: https://www.cdc.gov/niosh/topics/hierarchy/default.html. (accessed on 3 November 2022).
- Lind, C.M. Assessment and design of industrial manual handling to reduce physical ergonomics hazards – use and development of assessment tools; KTH Royal Institute of Technology: Stockholm, 2017. [Google Scholar]
- Sabino, I.; Fernandes, M.d.C.; Cepeda, C.; Quaresma, C.; Gamboa, H.; Nunes, I.L.; Gabriel, A.T. Application of wearable technology for the ergonomic risk assessment of healthcare professionals: A systematic literature review. Int J Ind Ergon 2024, 100, 103570. [Google Scholar] [CrossRef]
- Schall, M.C., Jr.; Sesek, R.F.; Cavuoto, L.A. Barriers to the Adoption of Wearable Sensors in the Workplace: A Survey of Occupational Safety and Health Professionals. Hum Factors 2018, 60, 351–362. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





