Submitted:
12 July 2024
Posted:
12 July 2024
You are already at the latest version
Abstract
Keywords:
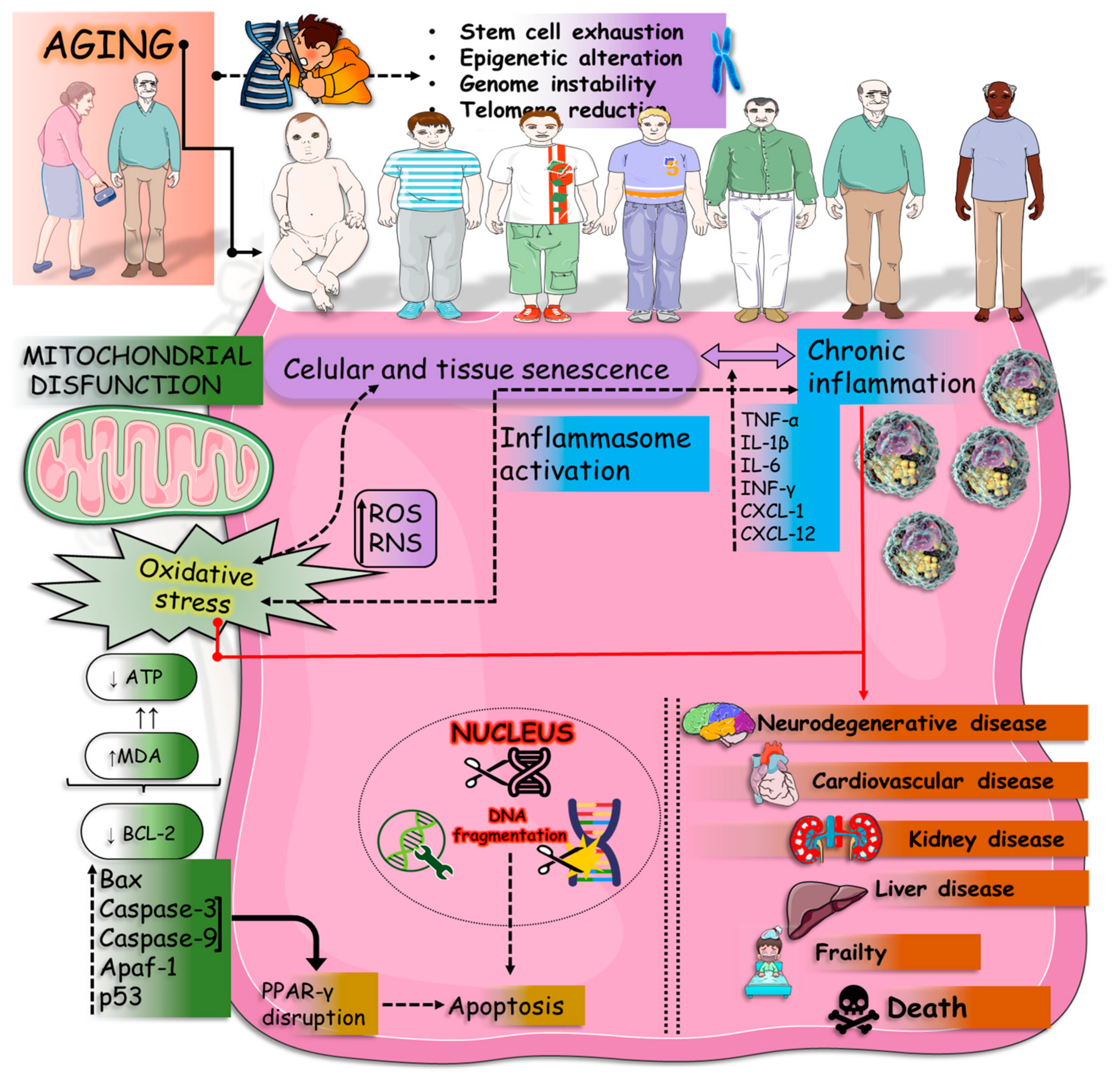
1. Introduction
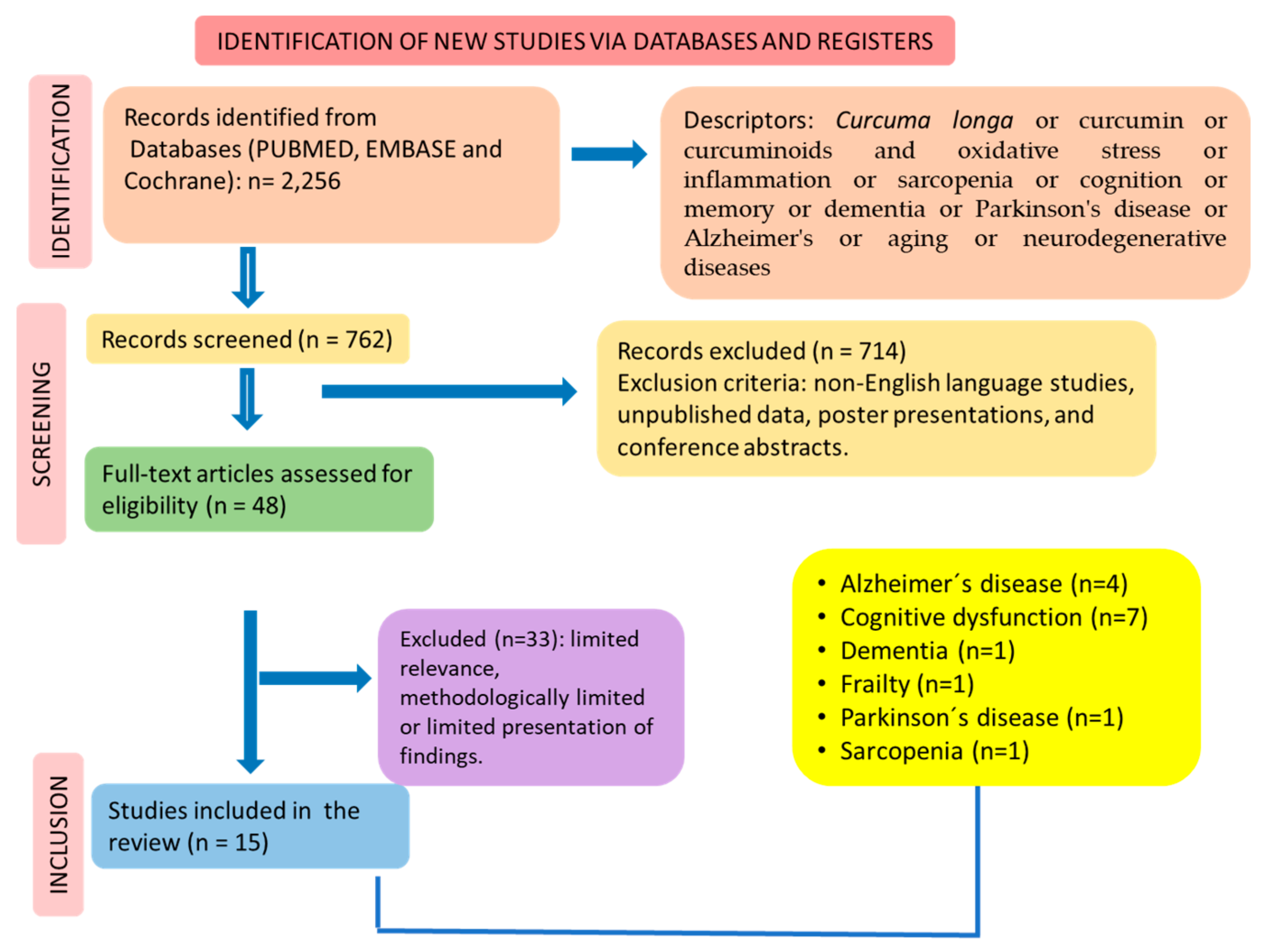
2. Materials and Methods
2.1. Focal Question
2.2. Language
2.3. Literature Search
2.4. Inclusion and Exclusion Criteria
2.5. Data Extraction
2.6. Study Selection
2.7. Quality Assessment
2.8. Registration
3. Results
4. Discussion
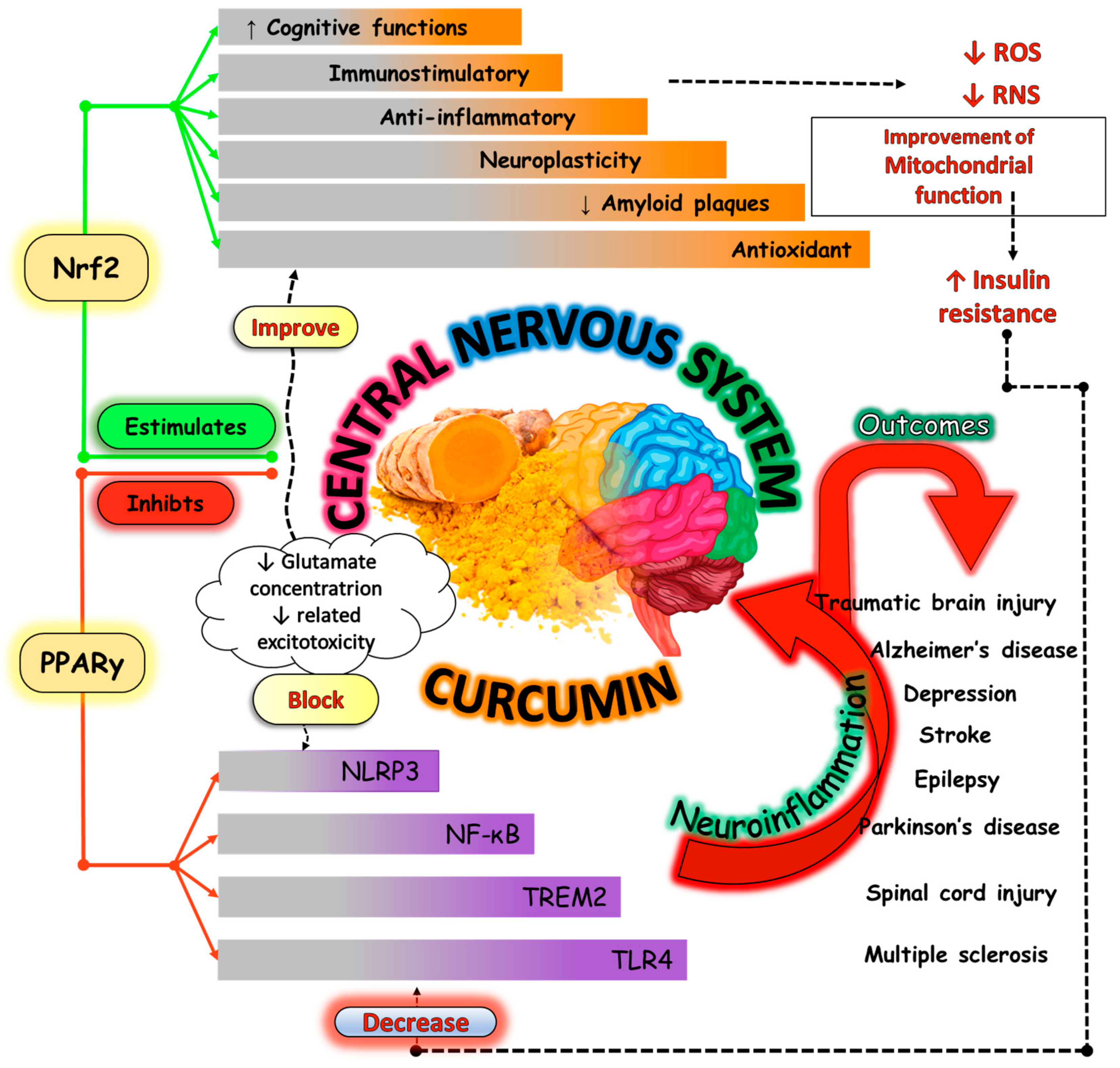
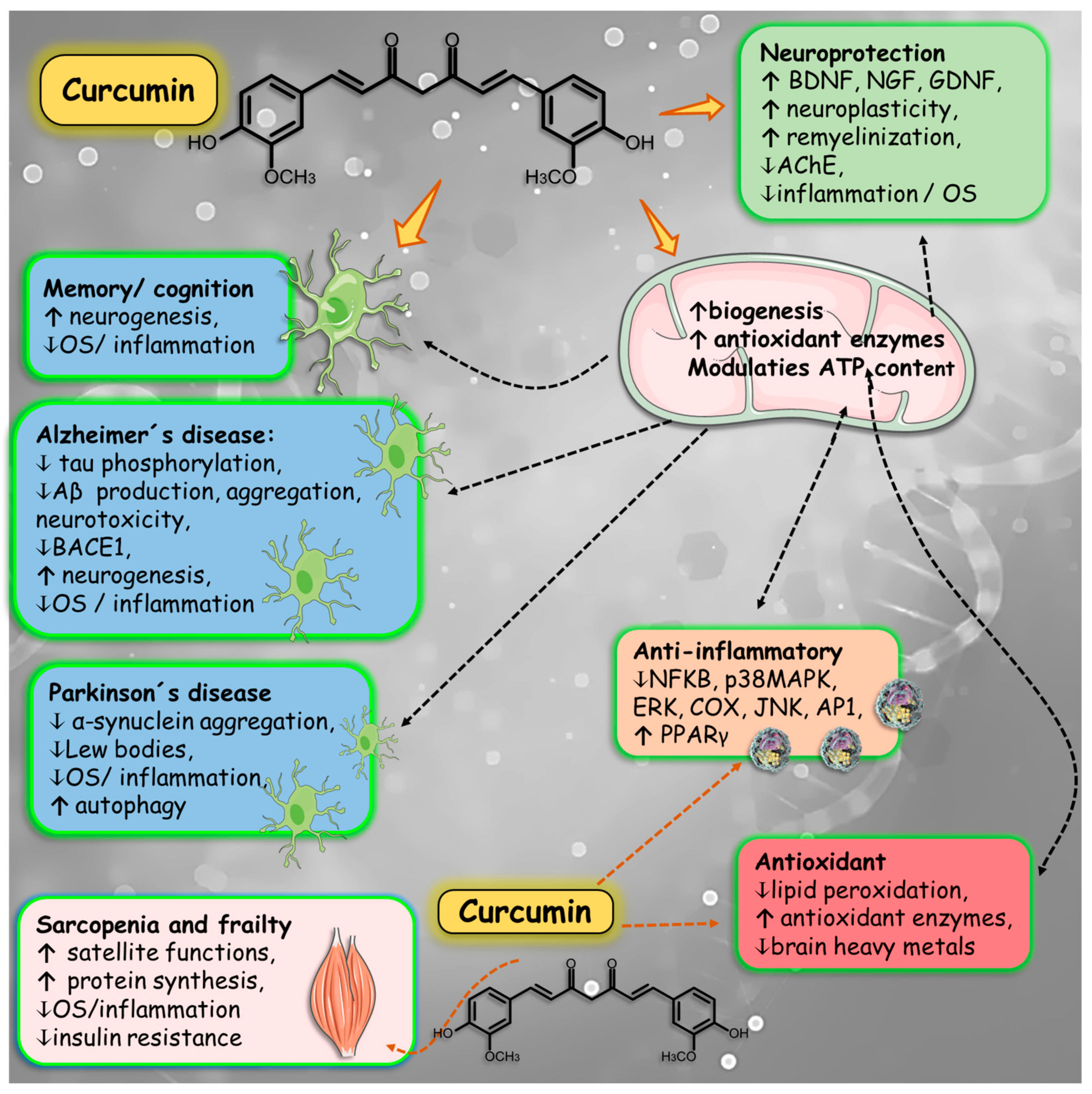
4.1. Beneficial Effects of Curcumin and Aging-Related Disorders
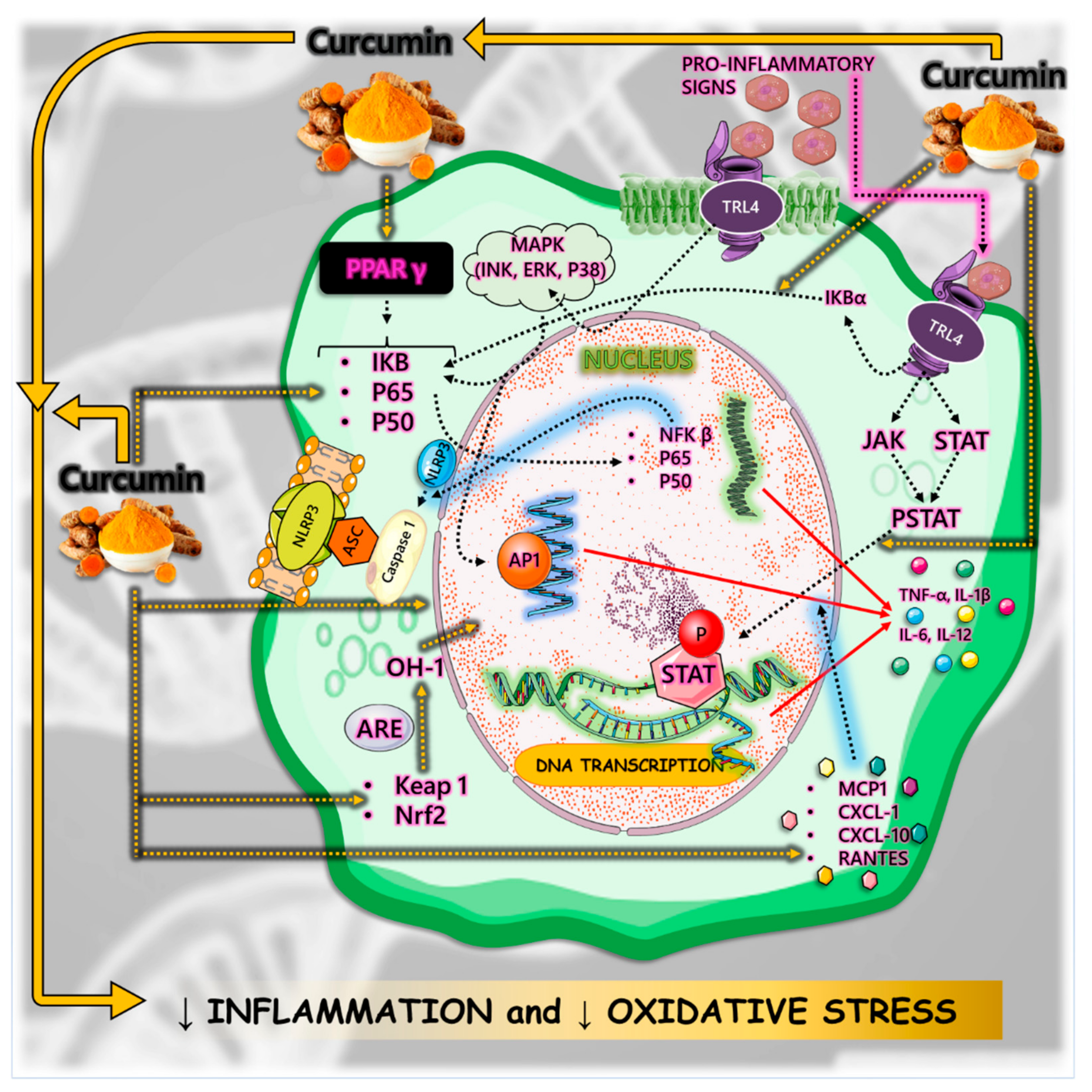
4.2. Inflammation
4.3. Oxidative Stress
4.4. Mitochondrial Dysfunction and Apoptosis
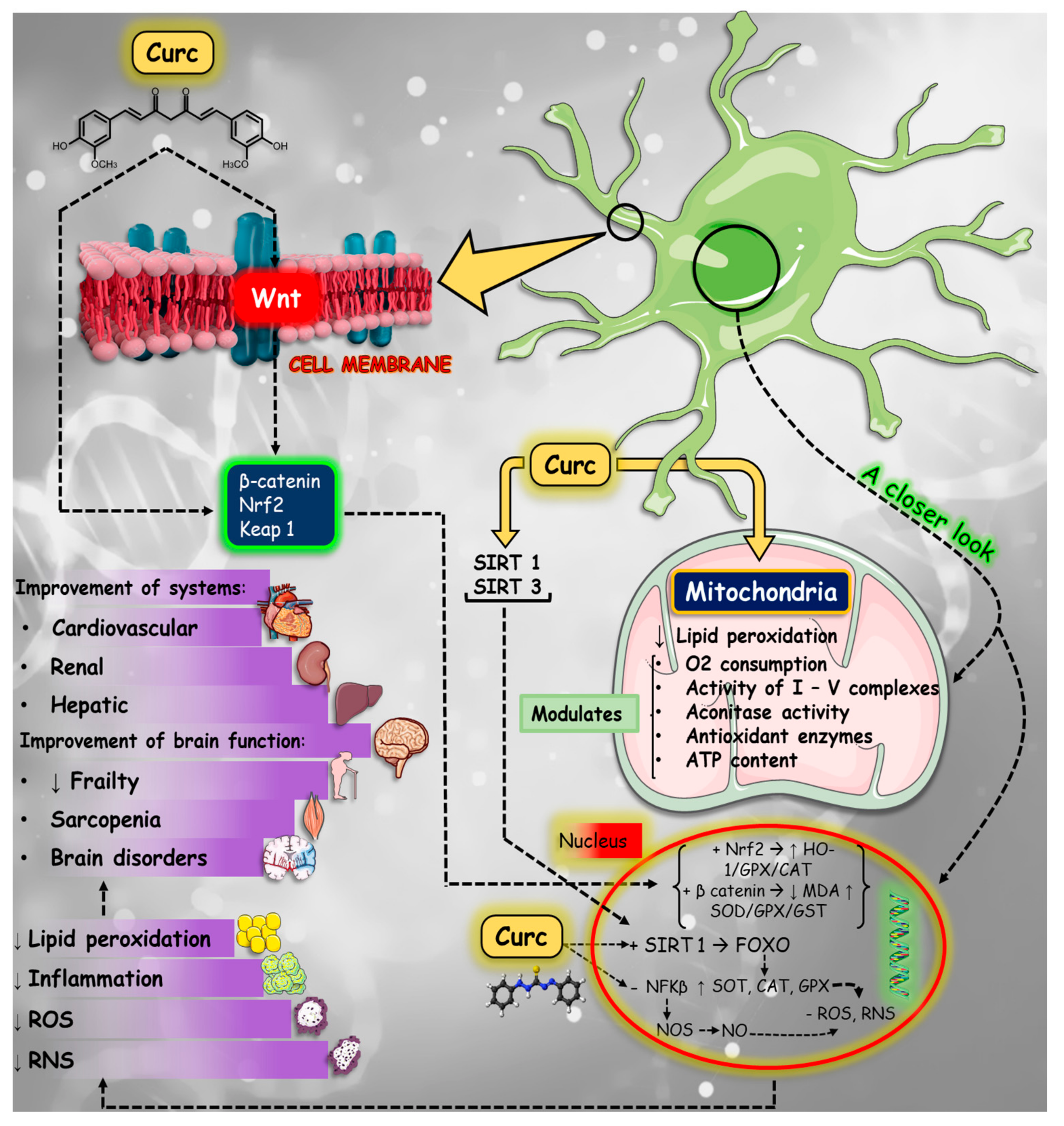
4.5. Neurodegenerative Diseases
4.5.1. Cognition
4.5.2. Memory
4.5.3. Alzheimer´s Disease
4.5.4. Parkinson’s Disease
4.6. Fragility
4.7. Sarcopenia
4.8. Clinical Trials Performed with Curcumin and Age-Related Disorders
5. Bioavailability and Safety
6. Synthesis and Future Research Endeavors
6.1. Advancing Curcumin Therapy: Exploring Formulations and Unraveling Mechanisms for Aging-Related Disorders
6.2. Unveiling Curcumin's Therapeutic Potential: Insights from Meticulous Clinical Trials and Advanced Neuroimaging Studies in Neurodegenerative Disorders
6.3. Unlocking Synergistic Therapeutic Strategies: Exploring Curcumin Combinations and Molecular Interactions in Disease Management
6.4. Fostering Collaboration for Curcumin Translation: Bridging Academia, Industry, Regulation, and Healthcare for Age-Related Disease Management
6.5. Unraveling the Genetic Basis of Curcumin Response: Genome-Wide Association Studies in Aging-Related Disease Management
7. Conclusion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
List of Abbreviations
| AChE | acetylcholinesterase |
| AD | Alzheimer´s disease |
| AMPK | adenosine 5′-monophosphate-activated protein kinase |
| APP | amyloid precursor protein |
| APPsw | APP Swedish Mutant |
| Bax | Bcl-2 associated protein X |
| Bcl-2 | B-cell lymphoma 2 |
| Cdk5 | cyclin-dependent kinase 5 |
| CNTMF | completely natural turmeric matrix formulation |
| COX-2 | cyclooxygenase 2 |
| DM2 | diabetes mellitus type 2 |
| DNA | deoxyribonucleic acid |
| FeONPs-Cur | iron oxide nanoparticles capped with curcumin |
| GSK-3β | glycogen synthase kinase-3β |
| HO-1 | heme oxygenase-1 |
| IL | interleukin |
| JAK/STAT | Janus kinase/Signal transducer and activator of transcription |
| JNK | c-Jun N-terminal kinase |
| Keap1 | Kelch-like ECH-associated protein 1 |
| MCT2 | monocarboxylate transporter 2 |
| mTOR | mammalian target of rapamycin |
| NADPH | nicotinamide adenine dinucleotide phosphate |
| NDs | neurodegenerative diseases |
| NF-κβ | nuclear factor-kappabeta |
| NO | nitric oxide |
| Nrf2 | nuclear factor erythroid 2–related factor 2 |
| OS | oxidative stress |
| PD | Parkinson's disease |
| PI3K | phosphoinositide 3-kinases |
| PI3K/AKT | phosphatidylinositol 3-kinase/protein kinase B |
| PPARγ | peroxisome proliferator-activated receptor gamma |
| RAGE | glycation end products |
| RNS | reactive nitrogen species |
| ROS | oxygen species |
| p- | phosphorylated |
| PPAR-γ | peroxisome proliferator-activated receptor gamma |
| Th17 | T helper 17 |
| TNF | tumor necrosis factor |
| TNF-α | tumor necrosis factor-alpha |
| TLR | toll-like receptors |
References
- Cai, Y.; Song, W.; Li, J.; Jing, Y.; Liang, C.; Zhang, L.; Zhang, X.; Zhang, W.; Liu, B.; An, Y.; et al. The landscape of aging. Sci China Life Sci 2022, 65, 2354–2454. [Google Scholar] [CrossRef] [PubMed]
- Baig, J.; Sawant, N.; Rawat, P.; Reddy, A.P.; Reddy, P.H.; Kshirsagar, S. Abnormal interaction of Rlip with mutant APP/Abeta and phosphorylated tau reduces wild-type Rlip levels and disrupt Rlip function in Alzheimer's disease. Biochimica et biophysica acta. Molecular basis of disease 2023. [Google Scholar] [CrossRef] [PubMed]
- Chiu, C.C.; Cheng, K.C.; Lin, Y.H.; He, C.X.; Bow, Y.D.; Li, C.Y.; Wu, C.Y.; Wang, H.D.; Sheu, S.J. Prolonged Exposure to High Glucose Induces Premature Senescence Through Oxidative Stress and Autophagy in Retinal Pigment Epithelial Cells. Archivum immunologiae et therapiae experimentalis 2023, 71, 21. [Google Scholar] [CrossRef] [PubMed]
- Sheng, Y.; Zhu, X.; Wei, L.; Zou, Y.; Qi, X.; Shi, R.; Xu, W.; Wang, X.; Ding, G.; Duan, Y. Aberrant expression of thyroidal hormone receptor α exasperating mitochondrial dysfunction induced sarcopenia in aged mice. Aging 2024, 16. [Google Scholar] [CrossRef] [PubMed]
- Lagunas-Rangel, F.A. SIRT7 in the aging process. Cellular and molecular life sciences : CMLS 2022, 79, 297. [Google Scholar] [CrossRef] [PubMed]
- Rosen, R.S.; Yarmush, M.L. Current Trends in Anti-Aging Strategies. Annual review of biomedical engineering 2023, 25, 363–385. [Google Scholar] [CrossRef] [PubMed]
- Zamboni, G.; Maramotti, R.; Salemme, S.; Tondelli, M.; Adani, G.; Vinceti, G.; Carbone, C.; Filippini, T.; Vinceti, M.; Pagnoni, G.; et al. Age-specific prevalence of the different clinical presentations of AD and FTD in young-onset dementia. Journal of neurology 2024. [Google Scholar] [CrossRef] [PubMed]
- Guilbaud, E.; Sarosiek, K.A.; Galluzzi, L. Inflammation and mitophagy are mitochondrial checkpoints to aging. Nature communications 2024, 15, 3375. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, M.; Tuka, B.; Vécsei, L. Navigating the Neurobiology of Migraine: From Pathways to Potential Therapies. Multidisciplinary Digital Publishing Institute: 2024; Vol. 13, p 1098.
- Ropert, B.; Gallrein, C.; Schumacher, B. DNA repair deficiencies and neurodegeneration. DNA repair 2024, 138, 103679. [Google Scholar] [CrossRef] [PubMed]
- McClarty, B.M.; Rodriguez, G.; Dong, H. Class 1 histone deacetylases differentially modulate memory and synaptic genes in a spatial and temporal manner in aged and APP/PS1 mice. Brain research 2024. [Google Scholar] [CrossRef]
- Kong, L.; Liu, Y.; Li, J.; Wang, Y.; Ji, P.; Shi, Q.; Han, M.; Xu, H.; Li, W.; Li, W. Ginsenoside Rg1 alleviates chronic inflammation-induced neuronal ferroptosis and cognitive impairments via regulation of AIM2 - Nrf2 signaling pathway. Journal of ethnopharmacology 2024. [Google Scholar] [CrossRef] [PubMed]
- Battaglia, S.; Avenanti, A.; Vécsei, L.; Tanaka, M. Neurodegeneration in cognitive impairment and mood disorders for experimental, clinical and translational neuropsychiatry. MDPI: 2024; Vol. 12, p 574.
- Cho, J.; Higgason, N.; Rothman, J.; Safford, M.; Pinheiro, L.C. "Should I Prioritize My Cancer or My Diabetes?": Patient-Perceived Barriers to Co-Managing Cancer and Diabetes Mellitus. Journal of cancer education : the official journal of the American Association for Cancer Education 2024. [Google Scholar] [CrossRef] [PubMed]
- Ottosson, F.; Engström, G.; Orho-Melander, M.; Melander, O.; Nilsson, P.M.; Johansson, M. Plasma Metabolome Predicts Aortic Stiffness and Future Risk of Coronary Artery Disease and Mortality After 23 Years of Follow-Up in the General Population. Journal of the American Heart Association 2024. [Google Scholar] [CrossRef] [PubMed]
- Huang, Z.; Zhuang, Y.; Li, W.; Ma, M.; Lei, F.; Qu, Y.; Li, J.; Luo, H.; Li, C.; Lu, L.; et al. Apoptotic vesicles are required to repair DNA damage and suppress premature cellular senescence. Journal of extracellular vesicles 2024, 13, e12428. [Google Scholar] [CrossRef] [PubMed]
- Peng, L.N.; Lin, M.H.; Tseng, S.H.; Yen, K.H.; Lee, H.F.; Hsiao, F.Y.; Chen, L.K. Protein-enriched soup and weekly exercise improve muscle health: A randomized trial in mid-to-old age with inadequate protein intake. Journal of cachexia, sarcopenia and muscle 2024. [Google Scholar] [CrossRef] [PubMed]
- Bults, M.; van Leersum, C.M.; Olthuis, T.J.J.; Siebrand, E.; Malik, Z.; Liu, L.; Miguel-Cruz, A.; Jukema, J.S.; den Ouden, M.E.M. Acceptance of a Digital Assistant (Anne4Care) for Older Adult Immigrants Living With Dementia: Qualitative Descriptive Study. JMIR aging 2024, 7, e50219. [Google Scholar] [CrossRef] [PubMed]
- Karimi, H.; Mahdavi, S.; Moghaddam, S.S.; Abbasi-Kangevari, M.; Soleimani, Z.; Esfahani, Z.; Masinaei, M.; Fateh, S.M.; Golestani, A.; Dilmaghani-Marand, A.; et al. Unveiling the lead exposure attributed burden in Iran from 1990 to 2019 through the lens of the Global Burden of Disease study 2019. Scientific reports 2024, 14, 8688. [Google Scholar] [CrossRef] [PubMed]
- Laurindo, L.F.; de Carvalho, G.M.; de Oliveira Zanuso, B.; Figueira, M.E.; Direito, R.; de Alvares Goulart, R.; Buglio, D.S.; Barbalho, S.M. Curcumin-Based Nanomedicines in the Treatment of Inflammatory and Immunomodulated Diseases: An Evidence-Based Comprehensive Review. Pharmaceutics 2023, 15. [Google Scholar] [CrossRef] [PubMed]
- Pagotto, G.L.d.O.; Santos, L.M.O.d.; Osman, N.; Lamas, C.B.; Laurindo, L.F.; Pomini, K.T.; Guissoni, L.M.; Lima, E.P.d.; Goulart, R.d.A.; Catharin, V.M.S. Ginkgo biloba: A Leaf of Hope in the Fight against Alzheimer’s Dementia: Clinical Trial Systematic Review. Antioxidants 2024, 13, 651. [Google Scholar] [CrossRef] [PubMed]
- Valotto Neto, L.J.; Reverete de Araujo, M.; Moretti Junior, R.C.; Mendes Machado, N.; Joshi, R.K.; dos Santos Buglio, D.; Barbalho Lamas, C.; Direito, R.; Fornari Laurindo, L.; Tanaka, M. Investigating the Neuroprotective and Cognitive-Enhancing Effects of Bacopa monnieri: A Systematic Review Focused on Inflammation, Oxidative Stress, Mitochondrial Dysfunction, and Apoptosis. Antioxidants 2024, 13, 393. [Google Scholar] [CrossRef] [PubMed]
- Kasprzak-Drozd, K.; Oniszczuk, T.; Gancarz, M.; Kondracka, A.; Rusinek, R.; Oniszczuk, A. Curcumin and Weight Loss: Does It Work? Int J Mol Sci 2022, 23. [Google Scholar] [CrossRef] [PubMed]
- Razavi, B.M.; Ghasemzadeh Rahbardar, M.; Hosseinzadeh, H. A review of therapeutic potentials of turmeric (Curcuma longa) and its active constituent, curcumin, on inflammatory disorders, pain, and their related patents. Phytother Res 2021, 35, 6489–6513. [Google Scholar] [CrossRef] [PubMed]
- Scazzocchio, B.; Minghetti, L.; D'Archivio, M. Interaction between Gut Microbiota and Curcumin: A New Key of Understanding for the Health Effects of Curcumin. Nutrients 2020, 12. [Google Scholar] [CrossRef] [PubMed]
- Moskwa, J.; Bronikowska, M.; Socha, K.; Markiewicz-Żukowska, R. Vegetable as a Source of Bioactive Compounds with Photoprotective Properties: Implication in the Aging Process. Nutrients 2023, 15. [Google Scholar] [CrossRef] [PubMed]
- Ren, Y.; Qu, S. Constituent isoflavones of Puerariae radix as a potential neuroprotector in cognitive impairment: Evidence from preclinical studies. Ageing research reviews 2023, 90, 102040. [Google Scholar] [CrossRef] [PubMed]
- Chainoglou, E.; Hadjipavlou-Litina, D. Curcumin in Health and Diseases: Alzheimer's Disease and Curcumin Analogues, Derivatives, and Hybrids. Int J Mol Sci 2020, 21. [Google Scholar] [CrossRef] [PubMed]
- Budhathoki, R.; Timilsina, A.P.; Regmi, B.P.; Sharma, K.R.; Aryal, N.; Parajuli, N. Metabolome Mining of Curcuma longa L. Using HPLC-MS/MS and Molecular Networking. Metabolites 2023, 13. [Google Scholar] [CrossRef] [PubMed]
- Cacciola, N.A.; Cuciniello, R.; Petillo, G.D.; Piccioni, M.; Filosa, S.; Crispi, S. An Overview of the Enhanced Effects of Curcumin and Chemotherapeutic Agents in Combined Cancer Treatments. International journal of molecular sciences 2023, 24. [Google Scholar] [CrossRef] [PubMed]
- Zhi, H.W.; Jia, Y.Z.; Bo, H.Q.; Li, H.T.; Zhang, S.S.; Wang, Y.H.; Yang, J.; Hu, M.Z.; Wu, H.Y.; Cui, W.Q.; et al. Curcumin alleviates orofacial allodynia and improves cognitive impairment via regulating hippocampal synaptic plasticity in a mouse model of trigeminal neuralgia. Aging 2023, 15. [Google Scholar] [CrossRef] [PubMed]
- Marton, L.T.; Barbalho, S.M.; Sloan, K.P.; Sloan, L.A.; Goulart, R.A.; Araújo, A.C.; Bechara, M.D. Curcumin, autoimmune and inflammatory diseases: going beyond conventional therapy - a systematic review. Critical reviews in food science and nutrition 2022, 62, 2140–2157. [Google Scholar] [CrossRef] [PubMed]
- Akaberi, M.; Sahebkar, A.; Emami, S.A. Turmeric and Curcumin: From Traditional to Modern Medicine. Adv Exp Med Biol 2021, 1291, 15–39. [Google Scholar] [CrossRef] [PubMed]
- Wong, S.C.; Kamarudin, M.N.A.; Naidu, R. Anticancer Mechanism of Curcumin on Human Glioblastoma. Nutrients 2021, 13. [Google Scholar] [CrossRef] [PubMed]
- Den Hartogh, D.J.; Gabriel, A.; Tsiani, E. Antidiabetic Properties of Curcumin I: Evidence from In Vitro Studies. Nutrients 2020, 12. [Google Scholar] [CrossRef] [PubMed]
- Górka, M.; Białoń, N.; Bieczek, D.; Górka, D. [Neuroprotective effect of curcumin and its potential use in the treatment of neurodegenerative diseases]. Postepy biochemii 2023, 69, 18–25. [Google Scholar] [CrossRef] [PubMed]
- Jafari-Nozad, A.M.; Jafari, A.; Yousefi, S.; Bakhshi, H.; Farkhondeh, T.; Samarghandian, S. Anti-gout and urate-lowering potentials of curcumin: A review from bench to beside. Current medicinal chemistry 2023. [Google Scholar] [CrossRef] [PubMed]
- Boonla, O.; Kukongviriyapan, U.; Pakdeechote, P.; Kukongviriyapan, V.; Pannangpetch, P.; Prachaney, P.; Greenwald, S.E. Curcumin improves endothelial dysfunction and vascular remodeling in 2K-1C hypertensive rats by raising nitric oxide availability and reducing oxidative stress. Nitric Oxide 2014, 42, 44–53. [Google Scholar] [CrossRef] [PubMed]
- Izadi, M.; Sadri, N.; Abdi, A.; Zadeh, M.M.R.; Jalaei, D.; Ghazimoradi, M.M.; Shouri, S.; Tahmasebi, S. Longevity and anti-aging effects of curcumin supplementation. GeroScience 2024, 46, 2933–2950. [Google Scholar] [CrossRef] [PubMed]
- Xu, J.; Du, P.; Liu, X.; Xu, X.; Ge, Y.; Zhang, C. Curcumin supplementation increases longevity and antioxidant capacity in Caenorhabditis elegans. Frontiers in pharmacology 2023, 14, 1195490. [Google Scholar] [CrossRef] [PubMed]
- Kumar, A.; Prakash, A.; Dogra, S. Protective effect of curcumin (Curcuma longa) against D-galactose-induced senescence in mice. Journal of Asian natural products research 2011, 13, 42–55. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.; Kim, Y.S.; Kim, E.; Kim, Y.; Kim, Y.J.N.R. Practice. Curcumin and hesperetin attenuate D-galactose-induced brain senescence in vitro and in vivo. 2020, 14, 438.
- Li, J.H.; Wei, T.T.; Guo, L.; Cao, J.H.; Feng, Y.K.; Guo, S.N.; Liu, G.H.; Ding, Y.; Chai, Y.R. Curcumin protects thymus against D-galactose-induced senescence in mice. Naunyn-Schmiedeberg's archives of pharmacology 2021, 394, 411–420. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Group, P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA Statement. Open Med 2009, 3, e123–130. [Google Scholar] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. Cochrane handbook for systematic reviews of interventions; John Wiley & Sons: 2019.
- Peng, Y.; Ao, M.; Dong, B.; Jiang, Y.; Yu, L.; Chen, Z.; Hu, C.; Xu, R. Anti-inflammatory effects of curcumin in the inflammatory diseases: Status, limitations and countermeasures. Drug design, development and therapy 2021, 4503-4525.
- Derochette, S.; Franck, T.; Mouithys-Mickalad, A.; Ceusters, J.; Deby-Dupont, G.; Lejeune, J.-P.; Neven, P.; Serteyn, D. Curcumin and resveratrol act by different ways on NADPH oxidase activity and reactive oxygen species produced by equine neutrophils. Chemico-biological interactions 2013, 206, 186–193. [Google Scholar] [CrossRef] [PubMed]
- Cordero-Herrera, I.; Martín, M.A.; Goya, L.; Ramos, S. Cocoa flavonoids protect hepatic cells against high-glucose-induced oxidative stress: Relevance of MAPKs. Molecular nutrition & food research 2015, 59, 597–609. [Google Scholar]
- He, Y.; Yue, Y.; Zheng, X.; Zhang, K.; Chen, S.; Du, Z. Curcumin, inflammation, and chronic diseases: how are they linked? Molecules 2015, 20, 9183–9213. [Google Scholar] [CrossRef] [PubMed]
- Pirunkaset, E.; Boonyarat, C.; Maneenet, J.; Khamphukdee, C.; Daodee, S.; Monthakantirat, O.; Awale, S.; Kijjoa, A.; Chulikhit, Y. Effect of Diacetylcurcumin Manganese Complex on Rotenone-Induced Oxidative Stress, Mitochondria Dysfunction, and Inflammation in the SH-SY5Y Parkinson's Disease Cell Model. Molecules (Basel, Switzerland) 2024, 29. [Google Scholar] [CrossRef] [PubMed]
- Nair, B.; Adithya, J.K.; Chandrababu, G.; Lakshmi, P.K.; Koshy, J.J.; Manoj, S.V.; Ambiliraj, D.B.; Vinod, B.S.; Sethi, G.; Nath, L.R. Modulation of carcinogenesis with selected GRAS nutraceuticals via Keap1-Nrf2 signaling pathway. Phytotherapy research : PTR 2023, 37, 4398–4413. [Google Scholar] [CrossRef]
- Matias, J.N.; Achete, G.; Campanari, G.; Guiguer, É.L.; Araújo, A.C.; Buglio, D.S.; Barbalho, S.M. A systematic review of the antidepressant effects of curcumin: Beyond monoamines theory. The Australian and New Zealand journal of psychiatry 2021, 55, 451–462. [Google Scholar] [CrossRef] [PubMed]
- Cunha Neto, F.; Marton, L.T.; de Marqui, S.V.; Lima, T.A.; Barbalho, S.M. Curcuminoids from Curcuma Longa: New adjuvants for the treatment of crohn's disease and ulcerative colitis? Critical reviews in food science and nutrition 2019, 59, 2136–2143. [Google Scholar] [CrossRef] [PubMed]
- Mazieiro, R.; Frizon, R.R.; Barbalho, S.M.; Goulart, R.A. Is Curcumin a Possibility to Treat Inflammatory Bowel Diseases? Journal of medicinal food 2018, 21, 1077–1085. [Google Scholar] [CrossRef] [PubMed]
- Goulart, R.A.; Barbalho, S.M.; Lima, V.M.; Souza, G.A.; Matias, J.N.; Araújo, A.C.; Rubira, C.J.; Buchaim, R.L.; Buchaim, D.V.; Carvalho, A.C.A.; et al. Effects of the Use of Curcumin on Ulcerative Colitis and Crohn's Disease: A Systematic Review. Journal of medicinal food 2021, 24, 675–685. [Google Scholar] [CrossRef] [PubMed]
- Hu, P.; Li, K.; Peng, X.-X.; Kan, Y.; Yao, T.-J.; Wang, Z.-Y.; Li, Z.; Liu, H.-Y.; Cai, D. Curcumin derived from medicinal homologous foods: its main signals in immunoregulation of oxidative stress, inflammation, and apoptosis. Frontiers in Immunology 2023, 14, 1233652. [Google Scholar] [CrossRef]
- Cai, Z.; Wang, W.; Zhang, Y.; Zeng, Y. Curcumin alleviates imiquimod-induced psoriasis-like inflammation and regulates gut microbiota of mice. Immunity, Inflammation and Disease 2023, 11, e967. [Google Scholar] [CrossRef] [PubMed]
- Barbalho, S.M.; de Sousa Gonzaga, H.F.; de Souza, G.A.; de Alvares Goulart, R.; de Sousa Gonzaga, M.L.; de Alvarez Rezende, B. Dermatological effects of Curcuma species: a systematic review. Clinical and experimental dermatology 2021, 46, 825–833. [Google Scholar] [CrossRef]
- Islam, T.; Koboziev, I.; Albracht-Schulte, K.; Mistretta, B.; Scoggin, S.; Yosofvand, M.; Moussa, H.; Zabet-Moghaddam, M.; Ramalingam, L.; Gunaratne, P.H. Curcumin reduces adipose tissue inflammation and alters gut microbiota in diet-induced obese male mice. Molecular nutrition & food research 2021, 65, 2100274. [Google Scholar]
- Gao, J.; Liu, Y.; Chen, J.; Tong, C.; Wang, Q.; Piao, Y. Curcumin treatment attenuates cisplatin-induced gastric mucosal inflammation and apoptosis through the NF-κ B and MAPKs signaling pathway. Human & Experimental Toxicology 2022, 41, 09603271221128738. [Google Scholar]
- Rathore, A.S.; Singh, S.S.; Birla, H.; Zahra, W.; Keshri, P.K.; Dilnashin, H.; Singh, R.; Singh, S.; Singh, S.P. Curcumin Modulates p62-Keap1-Nrf2-Mediated Autophagy in Rotenone-Induced Parkinson's Disease Mouse Models. ACS chemical neuroscience 2023. [Google Scholar] [CrossRef] [PubMed]
- Chauhan, W.; Zennadi, R. Keap1-Nrf2 Heterodimer: A Therapeutic Target to Ameliorate Sickle Cell Disease. Antioxidants (Basel, Switzerland) 2023, 12. [Google Scholar] [CrossRef] [PubMed]
- Devita, M.; Debiasi, G.; Anglani, M.; Ceolin, C.; Mazzonetto, I.; Begliomini, C.; Cauzzo, S.; Raffaelli, C.; Lazzarin, A.; Ravelli, A.; et al. The Role of Cognitive Reserve in Protecting Cerebellar Volumes of Older Adults with mild Cognitive Impairment. Cerebellum (London, England) 2024. [Google Scholar] [CrossRef] [PubMed]
- Csiszar, A.; Ungvari, A.; Patai, R.; Gulej, R.; Yabluchanskiy, A.; Benyo, Z.; Kovacs, I.; Sotonyi, P.; Kirkpartrick, A.C.; Prodan, C.I.; et al. Atherosclerotic burden and cerebral small vessel disease: exploring the link through microvascular aging and cerebral microhemorrhages. GeroScience 2024. [Google Scholar] [CrossRef] [PubMed]
- Guo, X.; Xin, Q.; Wei, P.; Hua, Y.; Zhang, Y.; Su, Z.; She, G.; Yuan, R. Antioxidant and anti-aging activities of Longan crude and purified polysaccharide (LP-A) in nematode Caenorhabditis elegans. International journal of biological macromolecules 2024. [Google Scholar] [CrossRef]
- Xu, M.; Wang, W.; Cheng, J.; Qu, H.; Xu, M.; Wang, L. Effects of mitochondrial dysfunction on cellular function: Role in atherosclerosis. Biomedicine & pharmacotherapy = Biomedecine & pharmacotherapie 2024, 174, 116587. [Google Scholar] [CrossRef]
- Kong, J.; Fan, R.; Zhang, Y.; Jia, Z.; Zhang, J.; Pan, H.; Wang, Q. Oxidative stress in the brain-lung crosstalk: cellular and molecular perspectives. Frontiers in aging neuroscience 2024, 16, 1389454. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, M.; Vécsei, L. Monitoring the redox status in multiple sclerosis. Biomedicines 2020, 8, 406. [Google Scholar] [CrossRef] [PubMed]
- Stolp, H.B.; Solito, E. Developmental priming of early cerebrovascular ageing: Implications across a lifetime. International journal of geriatric psychiatry 2024, 39, e6090. [Google Scholar] [CrossRef] [PubMed]
- Hirunsai, M.; Srikuea, R. Differential effects of cholecalciferol and calcitriol on muscle proteolysis and oxidative stress in angiotensin II-induced C2C12 myotube atrophy. Physiological reports 2024, 12, e16011. [Google Scholar] [CrossRef] [PubMed]
- Li, S.; Liu, Y.; Lu, S.; Xu, J.; Liu, X.; Yang, D.; Yang, Y.; Hou, L.; Li, N. A crazy trio in Parkinson's disease: metabolism alteration, α-synuclein aggregation, and oxidative stress. Molecular and cellular biochemistry 2024. [Google Scholar] [CrossRef]
- Duan, D.; Li, H.; Chai, S.; Zhang, L.; Fan, T.; Hu, Z.; Feng, Y. The relationship between cardiac oxidative stress, inflammatory cytokine response, cardiac pump function, and prognosis post-myocardial infarction. Scientific reports 2024, 14, 8985. [Google Scholar] [CrossRef] [PubMed]
- Muhammad, I.; Khan, A.; Mustafa, A.; Elshikh, M.S.; Shen, W. Elucidating the modulatory effect of melatonin on enzyme activity and oxidative stress in wheat: a global meta-analysis. Physiologia plantarum 2024, 176, e14294. [Google Scholar] [CrossRef]
- Ezim, O.E.; Nyeche, J.; Nebeolisa, C.E.; Belonwu, C.D.; Abarikwu, S.O. Ascorbic acid attenuates gasoline-induced testicular toxicity, sperm quality deterioration, and testosterone imbalance in rats. Toxicology and industrial health 2024. [Google Scholar] [CrossRef]
- Fišar, Z.; Hroudová, J. CoQ(10) and Mitochondrial Dysfunction in Alzheimer's Disease. Antioxidants (Basel, Switzerland) 2024, 13. [Google Scholar] [CrossRef]
- Speers, A.B.; Wright, K.M.; Brandes, M.S.; Kedjejian, N.; Matthews, D.G.; Caruso, M.; Harris, C.J.; Koike, S.; Nguyen, T.; Quinn, J.F.; et al. Mode of administration influences plasma levels of active Centella asiatica compounds in 5xFAD mice while markers of neuroinflammation remain unaltered. Frontiers in neuroscience 2024, 18, 1277626. [Google Scholar] [CrossRef] [PubMed]
- Ferrara, F.; Yan, X.; Pecorelli, A.; Guiotto, A.; Colella, S.; Pasqui, A.; Ivarrson, J.; Lynch, S.; Anderias, S.; Choundhary, H.; et al. Combined exposure to UV and PM affect skin oxinflammatory responses and it is prevented by antioxidant mix topical application: Evidences from clinical study. Journal of cosmetic dermatology, 2024. [Google Scholar] [CrossRef]
- Novoselova, E.G.; Lunin, S.M.; Khrenov, M.O.; Glushkova, O.V.; Novoselova, T.V.; Parfenyuk, S.B. Pancreas Β-Cells in Type 1 and Type 2 Diabetes: Cell Death, Oxidative Stress and Immune Regulation. Recently Appearing Changes in Diabetes Consequences. Cellular physiology and biochemistry : international journal of experimental cellular physiology, biochemistry, and pharmacology 2024, 58, 144–155. [Google Scholar] [CrossRef] [PubMed]
- Uysal, F.; Sukur, G.; Bozdemir, N.; Cinar, O. Antioxidant supplementation may effect DNA methylation patterns, apoptosis, and ROS levels in developing mouse embryos. Histochemistry and cell biology 2024. [Google Scholar] [CrossRef] [PubMed]
- Zia, A.; Farkhondeh, T.; Pourbagher-Shahri, A.M.; Samarghandian, S. The role of curcumin in aging and senescence: Molecular mechanisms. Biomedicine & Pharmacotherapy 2021, 134, 111119. [Google Scholar]
- Ren, L.; Zhan, P.; Wang, Q.; Wang, C.; Liu, Y.; Yu, Z.; Zhang, S. Curcumin upregulates the Nrf2 system by repressing inflammatory signaling-mediated Keap1 expression in insulin-resistant conditions. Biochemical and biophysical research communications 2019, 514, 691–698. [Google Scholar] [CrossRef] [PubMed]
- Scuto, M.C.; Mancuso, C.; Tomasello, B.; Ontario, M.L.; Cavallaro, A.; Frasca, F.; Maiolino, L.; Salinaro, A.T.; Calabrese, E.J.; Calabrese, V. Curcumin, hormesis and the nervous system, Nutrients 11 (2019).
- Méndez-García, L.A.; Martinez-Castillo, M.; Villegas-Sepúlveda, N.; Orozco, L.; Córdova, E.J. Curcumin induces p53-independent inactivation of Nrf2 during oxidative stress–induced apoptosis. Human & experimental toxicology 2019, 38, 951–961. [Google Scholar]
- Azzini, E.; Peña-Corona, S.I.; Hernández-Parra, H.; Chandran, D.; Saleena, L.A.K.; Sawikr, Y.; Peluso, I.; Dhumal, S.; Kumar, M.; Leyva-Gómez, G.; et al. Neuroprotective and anti-inflammatory effects of curcumin in Alzheimer's disease: Targeting neuroinflammation strategies. Phytotherapy research : PTR 2024. [Google Scholar] [CrossRef] [PubMed]
- Hou, D.; Liao, H.; Hao, S.; Liu, R.; Huang, H.; Duan, C. Curcumin simultaneously improves mitochondrial dynamics and myocardial cell bioenergy after sepsis via the SIRT1-DRP1/PGC-1α pathway. Heliyon 2024, 10, e28501. [Google Scholar] [CrossRef] [PubMed]
- Osawa, T.; Kato, Y. Protective role of antioxidative food factors in oxidative stress caused by hyperglycemia. Annals of the New York Academy of Sciences 2005, 1043, 440–451. [Google Scholar] [CrossRef] [PubMed]
- Méndez-García, L.A.; Martínez-Castillo, M.; Villegas-Sepúlveda, N.; Orozco, L.; Córdova, E.J. Curcumin induces p53-independent inactivation of Nrf2 during oxidative stress-induced apoptosis. Human & experimental toxicology 2019, 38, 951–961. [Google Scholar] [CrossRef]
- Amalraj, A.; Pius, A.; Gopi, S.; Gopi, S. Biological activities of curcuminoids, other biomolecules from turmeric and their derivatives - A review. Journal of traditional and complementary medicine 2017, 7, 205–233. [Google Scholar] [CrossRef] [PubMed]
- Kocaadam, B.; Şanlier, N.J.C.r.i.f.s.; nutrition. Curcumin, an active component of turmeric (Curcuma longa), and its effects on health. 2017, 57, 2889-2895.
- Nazarian, M.; Aramjoo, H.; Roshanravan, B.; Samarghandian, S.; Farkhondeh, T. Protective Effects of Curcumin and Nanomicelle Curcumin on Chlorpyrifos-induced Oxidative Damage and Inflammation in the Uterus, Ovary and Brain of Rats. Current pharmaceutical biotechnology 2024. [Google Scholar] [CrossRef] [PubMed]
- Farkhondeh, T.; Zardast, M.; Rajabi, S.; Abdollahi-Karizno, M.; Roshanravan, B.; Havangi, J.; Aschner, M.; Samarghandian, S. Neuroprotective Effects of Curcumin against Chronic ChlorpyrifosInduced Oxidative Damage in Rat Brain Tissue. Current aging science 2024. [Google Scholar] [CrossRef]
- Zhang, M.W.; Sun, X.; Xu, Y.W.; Meng, W.; Tang, Q.; Gao, H.; Liu, L.; Chen, S.H. Curcumin relieves oxaliplatin-induced neuropathic pain via reducing inflammation and activating antioxidant response. Cell biology international 2024. [Google Scholar] [CrossRef] [PubMed]
- Sathyabhama, M.; Priya Dharshini, L.C.; Karthikeyan, A.; Kalaiselvi, S.; Min, T. The credible role of curcumin in oxidative stress-mediated mitochondrial dysfunction in mammals. Biomolecules 2022, 12, 1405. [Google Scholar] [CrossRef]
- Liu, Y.; Zeng, J.M.; Zhao, H.; Ao, C.Y.; Ao, L.H.; Ban, J.Q.; Li, J. Mechanism of KAT2A regulation of H3K36ac in manganese-induced oxidative damage to mitochondria in the nervous system and intervention by curcumin. Ecotoxicology and environmental safety 2024, 273, 116155. [Google Scholar] [CrossRef]
- Wang, D.; Yang, Y.; Zou, X.; Zheng, Z.; Zhang, J. Curcumin ameliorates CKD-induced mitochondrial dysfunction and oxidative stress through inhibiting GSK-3β activity. The Journal of Nutritional Biochemistry 2020, 83, 108404. [Google Scholar] [CrossRef] [PubMed]
- Saghari, Y.; Movahedi, M.; Tebianian, M.; Entezari, M. The Neuroprotective Effects of Curcumin Nanoparticles on The Cerebral Ischemia-Reperfusion Injury in The Rats-The Roles of The Protein Kinase RNA-Like ER Kinase/Extracellular Signal-Regulated Kinase and Transcription Factor EB proteins. Cell journal 2024, 26, 62–69. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Zhang, Y.; Yang, Y.; Zhang, W.; Luo, L.; Han, F.; Guan, H.; Tao, K.; Hu, D. Curcumin pretreatment protects against hypoxia/reoxgenation injury via improvement of mitochondrial function, destabilization of HIF-1α and activation of Epac1-Akt pathway in rat bone marrow mesenchymal stem cells. Biomedicine & Pharmacotherapy 2019, 109, 1268–1275. [Google Scholar]
- Liu, J.; Hu, S.; Zhu, B.; Shao, S.; Yuan, L. Grape seed procyanidin suppresses inflammation in cigarette smoke-exposed pulmonary arterial hypertension rats by the PPAR-γ/COX-2 pathway. Nutrition, metabolism, and cardiovascular diseases : NMCD 2020, 30, 347–354. [Google Scholar] [CrossRef]
- Hu, P.; Li, K.; Peng, X.X.; Kan, Y.; Yao, T.J.; Wang, Z.Y.; Li, Z.; Liu, H.Y.; Cai, D. Curcumin derived from medicinal homologous foods: its main signals in immunoregulation of oxidative stress, inflammation, and apoptosis. Frontiers in immunology 2023, 14, 1233652. [Google Scholar] [CrossRef] [PubMed]
- Chiu, Y.J.; Yang, J.S.; Tsai, F.J.; Chiu, H.Y.; Juan, Y.N.; Lo, Y.H.; Chiang, J.H. Curcumin suppresses cell proliferation and triggers apoptosis in vemurafenib-resistant melanoma cells by downregulating the EGFR signaling pathway. Environmental toxicology 2022, 37, 868–879. [Google Scholar] [CrossRef] [PubMed]
- Petiti, J.; Rosso, V.; Lo Iacono, M.; Panuzzo, C.; Calabrese, C.; Signorino, E.; Pironi, L.; Cartellà, A.; Bracco, E.; Pergolizzi, B.; et al. Curcumin induces apoptosis in JAK2-mutated cells by the inhibition of JAK2/STAT and mTORC1 pathways. Journal of cellular and molecular medicine 2019, 23, 4349–4357. [Google Scholar] [CrossRef] [PubMed]
- Ren, B.C.; Zhang, Y.F.; Liu, S.S.; Cheng, X.J.; Yang, X.; Cui, X.G.; Zhao, X.R.; Zhao, H.; Hao, M.F.; Li, M.D.; et al. Curcumin alleviates oxidative stress and inhibits apoptosis in diabetic cardiomyopathy via Sirt1-Foxo1 and PI3K-Akt signalling pathways. Journal of cellular and molecular medicine 2020, 24, 12355–12367. [Google Scholar] [CrossRef]
- Zhu, H.; Wang, X.; Wang, X.; Liu, B.; Yuan, Y.; Zuo, X. Curcumin attenuates inflammation and cell apoptosis through regulating NF-κB and JAK2/STAT3 signaling pathway against acute kidney injury. Cell cycle (Georgetown, Tex.) 2020, 19, 1941–1951. [Google Scholar] [CrossRef]
- Souza, P.V.S.d.; Pinto, W.B.V.d.R.; Oliveira, A.S.B. C9orf72-related disorders: expanding the clinical and genetic spectrum of neurodegenerative diseases. Arquivos de Neuro-psiquiatria 2015, 73, 246–256. [Google Scholar] [CrossRef] [PubMed]
- Bulle Oliveira, A.S.; Batista Pereira, R.D. AMYOTROPHIC LATERAL SCLEROSIS (ALS): THREE LETTERS THAT CHANGE THE PEOPLE'S LIFE. Arquivos de neuro-psiquiatria 2009, 67, 750–782. [Google Scholar] [CrossRef] [PubMed]
- Song, J.; Li, J.; Pei, X.; Chen, J.; Wang, L. Identification of cuproptosis-realated key genes and pathways in Parkinson's disease via bioinformatics analysis. PloS one 2024, 19, e0299898. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Y.; Sanchez, V.B.; Xu, P.; Roule, T.; Flores-Mendez, M.; Ciesielski, B.; Yoo, D.; Teshome, H.; Jimenez, T.; Liu, S.; et al. Altered lipid homeostasis is associated with cerebellar neurodegeneration in SNX14 deficiency. JCI insight, 2024. [Google Scholar] [CrossRef]
- Kovalová, M.; Gottfriedová, N.; Mrázková, E.; Janout, V.; Janoutová, J. Cognitive impairment, neurodegenerative disorders, and olfactory impairment: A literature review. Otolaryngologia polska = The Polish otolaryngology 2024, 78, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Bássoli, R.; Audi, D.; Ramalho, B.; Audi, M.; Quesada, K.; Barbalho, S. The Effects of Curcumin on Neurodegenerative Diseases: a Systematic Review. Journal of Herbal Medicine 2023, 42, 100771. [Google Scholar] [CrossRef]
- Gunnarsson, L.-G.; Bodin, L. Occupational exposures and neurodegenerative diseases—a systematic literature review and meta-analyses. International journal of environmental research and public health 2019, 16, 337. [Google Scholar] [CrossRef] [PubMed]
- Rekatsina, M.; Paladini, A.; Piroli, A.; Zis, P.; Pergolizzi, J.V.; Varrassi, G. Pathophysiology and therapeutic perspectives of oxidative stress and neurodegenerative diseases: a narrative review. Advances in therapy 2020, 37, 113–139. [Google Scholar] [CrossRef] [PubMed]
- Katsnelson, A.; De Strooper, B.; Zoghbi, H.Y. Neurodegeneration: From cellular concepts to clinical applications. Science translational medicine 2016, 8, 364ps318–364ps318. [Google Scholar] [CrossRef] [PubMed]
- Yadav, S.; Mansoori, A.; Sisodiya, J. Current pathologic determinants of complex neurodegenerative diseases: a review. Int J Pharm Technol 2013, 5, 2607–2621. [Google Scholar]
- Jette, N.; Maxwell, C.J.; Fiest, K.M.; Hogan, D.B. Systematic reviews and meta-analyses of the incidence and prevalence of dementia and its commoner neurodegenerative causes. Canadian Journal of Neurological Sciences 2016, 43, S1–S2. [Google Scholar] [CrossRef] [PubMed]
- González, H.; Pacheco, R. T-cell-mediated regulation of neuroinflammation involved in neurodegenerative diseases. Journal of neuroinflammation 2014, 11, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, M.; Chen, C. Towards a mechanistic understanding of depression, anxiety, and their comorbidity: Perspectives from cognitive neuroscience. Frontiers Media SA: 2023; Vol. 17, p 1268156.
- Bagheri, H.; Ghasemi, F.; Barreto, G.E.; Rafiee, R.; Sathyapalan, T.; Sahebkar, A. Effects of curcumin on mitochondria in neurodegenerative diseases. Biofactors 2020, 46, 5–20. [Google Scholar] [CrossRef] [PubMed]
- Kobayashi, H.; Ohnishi, T.; Nakagawa, R.; Yoshizawa, K. The comparative efficacy and safety of cholinesterase inhibitors in patients with mild-to-moderate Alzheimer's disease: a Bayesian network meta-analysis. International journal of geriatric psychiatry 2016, 31, 892–904. [Google Scholar] [CrossRef] [PubMed]
- Mehla, J.; Gupta, P.; Pahuja, M.; Diwan, D.; Diksha, D. Indian medicinal herbs and formulations for Alzheimer’s disease, from traditional knowledge to scientific assessment. Brain sciences 2020, 10, 964. [Google Scholar] [CrossRef] [PubMed]
- Popa-Wagner, A.; Dumitrascu, D.I.; Capitanescu, B.; Petcu, E.B.; Surugiu, R.; Fang, W.-H.; Dumbrava, D.-A. Dietary habits, lifestyle factors and neurodegenerative diseases. Neural regeneration research 2020, 15, 394–400. [Google Scholar] [CrossRef] [PubMed]
- Fasihi, M.; Samimi-Badabi, M.; Robat-Jazi, B.; Bitarafan, S.; Moghadasi, A.N.; Mansouri, F.; Yekaninejad, M.S.; Izad, M.; Saboor-Yaraghi, A.A. Immunoregulatory Effects of the Active Form of Vitamin D (Calcitriol), Individually and in Combination with Curcumin, on Peripheral Blood Mononuclear Cells (PBMCs) of Multiple Sclerosis (MS) Patients. Anti-inflammatory & anti-allergy agents in medicinal chemistry 2024. [Google Scholar] [CrossRef]
- Chae, J.; Choi, Y.; Hong, J.; Kim, N.; Kim, J.; Lee, H.Y.; Choi, J. Anticancer and Antibacterial Properties of Curcumin-Loaded Mannosylated Solid Lipid Nanoparticles for the Treatment of Lung Diseases. ACS applied bio materials 2024, 7, 2175–2185. [Google Scholar] [CrossRef] [PubMed]
- Guo, J.; Tang, X.; Deng, P.; Hui, H.; Chen, B.; An, J.; Zhang, G.; Shi, K.; Wang, J.; He, Y.; et al. Interleukin-4 from curcumin-activated OECs emerges as a central modulator for increasing M2 polarization of microglia/macrophage in OEC anti-inflammatory activity for functional repair of spinal cord injury. Cell communication and signaling : CCS 2024, 22, 162. [Google Scholar] [CrossRef]
- Harada, C.N.; Natelson Love, M.C.; Triebel, K.L. Normal cognitive aging. Clin Geriatr Med 2013, 29, 737–752. [Google Scholar] [CrossRef] [PubMed]
- Bliss, E.S.; Wong, R.H.; Howe, P.R.; Mills, D.E. Benefits of exercise training on cerebrovascular and cognitive function in ageing. J Cereb Blood Flow Metab 2021, 41, 447–470. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, M. Protective effects of curcumin against lithium-pilocarpine induced status epilepticus, cognitive dysfunction and oxidative stress in young rats. Saudi J Biol Sci 2013, 20, 155–162. [Google Scholar] [CrossRef]
- Sarker, M.R.; Franks, S.F. Efficacy of curcumin for age-associated cognitive decline: a narrative review of preclinical and clinical studies. Geroscience 2018, 40, 73–95. [Google Scholar] [CrossRef] [PubMed]
- Zhi, H.W.; Jia, Y.Z.; Bo, H.Q.; Li, H.T.; Zhang, S.S.; Wang, Y.H.; Yang, J.; Hu, M.Z.; Wu, H.Y.; Cui, W.Q.; et al. Curcumin alleviates orofacial allodynia and improves cognitive impairment via regulating hippocampal synaptic plasticity in a mouse model of trigeminal neuralgia. Aging (Albany NY) 2023, 15, 8458–8470. [Google Scholar] [CrossRef] [PubMed]
- Cho, J.A.; Park, S.H.; Cho, J.; Kim, J.O.; Yoon, J.H.; Park, E. Exercise and Curcumin in Combination Improves Cognitive Function and Attenuates ER Stress in Diabetic Rats. Nutrients 2020, 12. [Google Scholar] [CrossRef] [PubMed]
- Kodali, M.; Hattiangady, B.; Shetty, G.A.; Bates, A.; Shuai, B.; Shetty, A.K. Curcumin treatment leads to better cognitive and mood function in a model of Gulf War Illness with enhanced neurogenesis, and alleviation of inflammation and mitochondrial dysfunction in the hippocampus. Brain Behav Immun 2018, 69, 499–514. [Google Scholar] [CrossRef] [PubMed]
- Grimm, A.; Eckert, A. Brain aging and neurodegeneration: from a mitochondrial point of view. J Neurochem 2017, 143, 418–431. [Google Scholar] [CrossRef] [PubMed]
- Ionescu-Tucker, A.; Cotman, C.W. Emerging roles of oxidative stress in brain aging and Alzheimer's disease. Neurobiol Aging 2021, 107, 86–95. [Google Scholar] [CrossRef] [PubMed]
- Yi, L.T.; Dong, S.Q.; Wang, S.S.; Chen, M.; Li, C.F.; Geng, D.; Zhu, J.X.; Liu, Q.; Cheng, J. Curcumin attenuates cognitive impairment by enhancing autophagy in chemotherapy. Neurobiol Dis 2020, 136, 104715. [Google Scholar] [CrossRef] [PubMed]
- Rueda, N.; Vidal, V.; García-Cerro, S.; Puente, A.; Campa, V.; Lantigua, S.; Narcís, O.; Bartesaghi, R.; Martínez-Cué, C. Prenatal, but not Postnatal, Curcumin Administration Rescues Neuromorphological and Cognitive Alterations in Ts65Dn Down Syndrome Mice. J Nutr 2020, 150, 2478–2489. [Google Scholar] [CrossRef] [PubMed]
- Noorafshan, A.; Abdollahifar, M.A.; Karbalay-Doust, S.; Asadi-Golshan, R.; Rashidian-Rashidabadi, A. Protective effects of curcumin and sertraline on the behavioral changes in chronic variable stress-induced rats. Exp Neurobiol 2013, 22, 96–106. [Google Scholar] [CrossRef] [PubMed]
- Sorrenti, V.; Contarini, G.; Sut, S.; Dall'Acqua, S.; Confortin, F.; Pagetta, A.; Giusti, P.; Zusso, M. Curcumin Prevents Acute Neuroinflammation and Long-Term Memory Impairment Induced by Systemic Lipopolysaccharide in Mice. Front Pharmacol 2018, 9, 183. [Google Scholar] [CrossRef] [PubMed]
- Vorhees, C.V.; Williams, M.T. Tests for learning and memory in rodent regulatory studies. Curr Res Toxicol 2024, 6, 100151. [Google Scholar] [CrossRef] [PubMed]
- Lang, B.; Kahnau, P.; Hohlbaum, K.; Mieske, P.; Andresen, N.P.; Boon, M.N.; Thöne-Reineke, C.; Lewejohann, L.; Diederich, K. Challenges and advanced concepts for the assessment of learning and memory function in mice. Front Behav Neurosci 2023, 17, 1230082. [Google Scholar] [CrossRef] [PubMed]
- Denninger, J.K.; Smith, B.M.; Kirby, E.D. Novel Object Recognition and Object Location Behavioral Testing in Mice on a Budget. J Vis Exp, 2018. [Google Scholar] [CrossRef]
- Battaglia, S.; Avenanti, A.; Vécsei, L.; Tanaka, M. Neural correlates and molecular mechanisms of memory and learning. MDPI: 2024; Vol. 25, p 2724.
- Changlek, S.; Rana, M.N.; Phyu, M.P.; Karim, N.; Majima, H.J.; Tangpong, J. Curcumin Suppresses Lead-Induced Inflammation and Memory Loss in Mouse Model and In Silico Molecular Docking. Foods 2022, 11. [Google Scholar] [CrossRef] [PubMed]
- Lu, W.T.; Sun, S.Q.; Li, Y.; Xu, S.Y.; Gan, S.W.; Xu, J.; Qiu, G.P.; Zhuo, F.; Huang, S.Q.; Jiang, X.L.; et al. Curcumin Ameliorates Memory Deficits by Enhancing Lactate Content and MCT2 Expression in APP/PS1 Transgenic Mouse Model of Alzheimer's Disease. Anat Rec (Hoboken) 2019, 302, 332–338. [Google Scholar] [CrossRef] [PubMed]
- Sarlak, Z.; Oryan, S.; Moghaddasi, M. Interaction between the antioxidant activity of curcumin and cholinergic system on memory retention in adult male Wistar rats. Iran J Basic Med Sci 2015, 18, 398–403. [Google Scholar] [PubMed]
- Ikram, M.; Saeed, K.; Khan, A.; Muhammad, T.; Khan, M.S.; Jo, M.G.; Rehman, S.U.; Kim, M.O. Natural Dietary Supplementation of Curcumin Protects Mice Brains against Ethanol-Induced Oxidative Stress-Mediated Neurodegeneration and Memory Impairment via Nrf2/TLR4/RAGE Signaling. Nutrients 2019, 11. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Fang, Y.; Xu, Y.; Lian, Y.; Xie, N.; Wu, T.; Zhang, H.; Sun, L.; Zhang, R.; Wang, Z. Curcumin Improves Amyloid β-Peptide (1-42) Induced Spatial Memory Deficits through BDNF-ERK Signaling Pathway. PLoS One 2015, 10, e0131525. [Google Scholar] [CrossRef] [PubMed]
- Gouras, G.K.; Olsson, T.T.; Hansson, O. β-Amyloid peptides and amyloid plaques in Alzheimer's disease. Neurotherapeutics 2015, 12, 3–11. [Google Scholar] [CrossRef]
- Serrano-Pozo, A.; Frosch, M.P.; Masliah, E.; Hyman, B.T. Neuropathological alterations in Alzheimer disease. Cold Spring Harb Perspect Med 2011, 1, a006189. [Google Scholar] [CrossRef] [PubMed]
- Metaxas, A.; Kempf, S.J. Neurofibrillary tangles in Alzheimer's disease: elucidation of the molecular mechanism by immunohistochemistry and tau protein phospho-proteomics. Neural Regen Res 2016, 11, 1579–1581. [Google Scholar] [CrossRef] [PubMed]
- Minter, M.R.; Taylor, J.M.; Crack, P.J. The contribution of neuroinflammation to amyloid toxicity in Alzheimer's disease. J Neurochem 2016, 136, 457–474. [Google Scholar] [CrossRef] [PubMed]
- Trejo-Lopez, J.A.; Yachnis, A.T.; Prokop, S. Neuropathology of Alzheimer's Disease. Neurotherapeutics 2022, 19, 173–185. [Google Scholar] [CrossRef] [PubMed]
- Domingues, C.; da Cruz E Silva, O.A.B.; Henriques, A.G. Impact of Cytokines and Chemokines on Alzheimer's Disease Neuropathological Hallmarks. Curr Alzheimer Res 2017, 14, 870–882. [Google Scholar] [CrossRef] [PubMed]
- Al-Ghraiybah, N.F.; Wang, J.; Alkhalifa, A.E.; Roberts, A.B.; Raj, R.; Yang, E.; Kaddoumi, A. Glial Cell-Mediated Neuroinflammation in Alzheimer's Disease. Int J Mol Sci 2022, 23. [Google Scholar] [CrossRef] [PubMed]
- Twarowski, B.; Herbet, M. Inflammatory Processes in Alzheimer's Disease-Pathomechanism, Diagnosis and Treatment: A Review. Int J Mol Sci 2023, 24. [Google Scholar] [CrossRef] [PubMed]
- González-Reyes, R.E.; Nava-Mesa, M.O.; Vargas-Sánchez, K.; Ariza-Salamanca, D.; Mora-Muñoz, L. Involvement of Astrocytes in Alzheimer's Disease from a Neuroinflammatory and Oxidative Stress Perspective. Front Mol Neurosci 2017, 10, 427. [Google Scholar] [CrossRef] [PubMed]
- Ono, K.; Hasegawa, K.; Naiki, H.; Yamada, M. Curcumin has potent anti-amyloidogenic effects for Alzheimer's beta-amyloid fibrils in vitro. J Neurosci Res 2004, 75, 742–750. [Google Scholar] [CrossRef] [PubMed]
- Lim, G.P.; Chu, T.; Yang, F.; Beech, W.; Frautschy, S.A.; Cole, G.M. The curry spice curcumin reduces oxidative damage and amyloid pathology in an Alzheimer transgenic mouse. J Neurosci 2001, 21, 8370–8377. [Google Scholar] [CrossRef] [PubMed]
- Hoppe, J.B.; Coradini, K.; Frozza, R.L.; Oliveira, C.M.; Meneghetti, A.B.; Bernardi, A.; Pires, E.S.; Beck, R.C.; Salbego, C.G. Free and nanoencapsulated curcumin suppress β-amyloid-induced cognitive impairments in rats: involvement of BDNF and Akt/GSK-3β signaling pathway. Neurobiol Learn Mem 2013, 106, 134–144. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Alloza, M.; Borrelli, L.A.; Rozkalne, A.; Hyman, B.T.; Bacskai, B.J. Curcumin labels amyloid pathology in vivo, disrupts existing plaques, and partially restores distorted neurites in an Alzheimer mouse model. J Neurochem 2007, 102, 1095–1104. [Google Scholar] [CrossRef] [PubMed]
- Goozee, K.G.; Shah, T.M.; Sohrabi, H.R.; Rainey-Smith, S.R.; Brown, B.; Verdile, G.; Martins, R.N. Examining the potential clinical value of curcumin in the prevention and diagnosis of Alzheimer's disease. Br J Nutr 2016, 115, 449–465. [Google Scholar] [CrossRef]
- Tiwari, S.K.; Agarwal, S.; Seth, B.; Yadav, A.; Nair, S.; Bhatnagar, P.; Karmakar, M.; Kumari, M.; Chauhan, L.K.; Patel, D.K.; et al. Curcumin-loaded nanoparticles potently induce adult neurogenesis and reverse cognitive deficits in Alzheimer's disease model via canonical Wnt/β-catenin pathway. ACS Nano 2014, 8, 76–103. [Google Scholar] [CrossRef] [PubMed]
- Martos, D.; Lőrinczi, B.; Szatmári, I.; Vécsei, L.; Tanaka, M. The Impact of C-3 Side Chain Modifications on Kynurenic Acid: A Behavioral Analysis of Its Analogs in the Motor Domain. International journal of molecular sciences 2024, 25, 3394. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, M.; Bohár, Z.; Vécsei, L. Are kynurenines accomplices or principal villains in dementia? Maintenance of kynurenine metabolism. Molecules 2020, 25, 564. [Google Scholar] [CrossRef] [PubMed]
- Yang, F.; Lim, G.P.; Begum, A.N.; Ubeda, O.J.; Simmons, M.R.; Ambegaokar, S.S.; Chen, P.P.; Kayed, R.; Glabe, C.G.; Frautschy, S.A.; et al. Curcumin inhibits formation of amyloid beta oligomers and fibrils, binds plaques, and reduces amyloid in vivo. J Biol Chem 2005, 280, 5892–5901. [Google Scholar] [CrossRef] [PubMed]
- Pan, R.; Qiu, S.; Lu, D.X.; Dong, J. Curcumin improves learning and memory ability and its neuroprotective mechanism in mice. Chin Med J (Engl) 2008, 121, 832–839. [Google Scholar] [CrossRef]
- Xie, Y.; Zhao, Q.Y.; Li, H.Y.; Zhou, X.; Liu, Y.; Zhang, H. Curcumin ameliorates cognitive deficits heavy ion irradiation-induced learning and memory deficits through enhancing of Nrf2 antioxidant signaling pathways. Pharmacol Biochem Behav 2014, 126, 181–186. [Google Scholar] [CrossRef] [PubMed]
- Hacioglu, C.; Kar, F.; Kar, E.; Kara, Y.; Kanbak, G. Effects of Curcumin and Boric Acid Against Neurodegenerative Damage Induced by Amyloid Beta (1-42). Biol Trace Elem Res 2021, 199, 3793–3800. [Google Scholar] [CrossRef] [PubMed]
- Ahlijanian, M.K.; Barrezueta, N.X.; Williams, R.D.; Jakowski, A.; Kowsz, K.P.; McCarthy, S.; Coskran, T.; Carlo, A.; Seymour, P.A.; Burkhardt, J.E.; et al. Hyperphosphorylated tau and neurofilament and cytoskeletal disruptions in mice overexpressing human p25, an activator of cdk5. Proc Natl Acad Sci U S A 2000, 97, 2910–2915. [Google Scholar] [CrossRef] [PubMed]
- Chow, H.M.; Guo, D.; Zhou, J.C.; Zhang, G.Y.; Li, H.F.; Herrup, K.; Zhang, J. CDK5 activator protein p25 preferentially binds and activates GSK3β. Proc Natl Acad Sci U S A 2014, 111, E4887–4895. [Google Scholar] [CrossRef] [PubMed]
- Alamro, A.A.; Alsulami, E.A.; Almutlaq, M.; Alghamedi, A.; Alokail, M.; Haq, S.H. Therapeutic Potential of Vitamin D and Curcumin in an. J Cent Nerv Syst Dis 2020, 12, 1179573520924311. [Google Scholar] [CrossRef] [PubMed]
- Das, T.K.; Jana, P.; Chakrabarti, S.K.; Abdul Hamid, M.R.W. Curcumin Downregulates GSK3 and Cdk5 in Scopolamine-Induced Alzheimer's Disease Rats Abrogating Aβ. J Alzheimers Dis Rep 2019, 3, 257–267. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Li, J.; Li, S.; Wang, X.; Liu, B.; Fu, Q.; Ma, S. Curcumin attenuates glutamate neurotoxicity in the hippocampus by suppression of ER stress-associated TXNIP/NLRP3 inflammasome activation in a manner dependent on AMPK. Toxicol Appl Pharmacol 2015, 286, 53–63. [Google Scholar] [CrossRef] [PubMed]
- Zhou, J.; Wu, N.; Lin, L. Curcumin Suppresses Apoptosis and Inflammation in Hypoxia/Reperfusion-Exposed Neurons via Wnt Signaling Pathway. Med Sci Monit 2020, 26, e920445. [Google Scholar] [CrossRef] [PubMed]
- Park, J.S.; Lee, W.K.; Kim, H.S.; Seo, J.A.; Kim, D.H.; Han, H.C.; Min, B.H. Clusterin overexpression protects against western diet-induced obesity and NAFLD. Sci Rep 2020, 10, 17484. [Google Scholar] [CrossRef] [PubMed]
- Shao, S.; Ye, X.; Su, W.; Wang, Y. Curcumin alleviates Alzheimer's disease by inhibiting inflammatory response, oxidative stress and activating the AMPK pathway. J Chem Neuroanat 2023, 134, 102363. [Google Scholar] [CrossRef] [PubMed]
- Yavarpour-Bali, H.; Ghasemi-Kasman, M.; Pirzadeh, M. Curcumin-loaded nanoparticles: a novel therapeutic strategy in treatment of central nervous system disorders. Int J Nanomedicine 2019, 14, 4449–4460. [Google Scholar] [CrossRef] [PubMed]
- Panzarini, E.; Mariano, S.; Tacconi, S.; Carata, E.; Tata, A.M.; Dini, L. Novel Therapeutic Delivery of Nanocurcumin in Central Nervous System Related Disorders. Nanomaterials (Basel) 2020, 11. [Google Scholar] [CrossRef] [PubMed]
- Ruan, Y.; Xiong, Y.; Fang, W.; Yu, Q.; Mai, Y.; Cao, Z.; Wang, K.; Lei, M.; Xu, J.; Liu, Y.; et al. Highly sensitive Curcumin-conjugated nanotheranostic platform for detecting amyloid-beta plaques by magnetic resonance imaging and reversing cognitive deficits of Alzheimer's disease via NLRP3-inhibition. J Nanobiotechnology 2022, 20, 322. [Google Scholar] [CrossRef] [PubMed]
- Cheng, K.K.; Yeung, C.F.; Ho, S.W.; Chow, S.F.; Chow, A.H.; Baum, L. Highly stabilized curcumin nanoparticles tested in an in vitro blood-brain barrier model and in Alzheimer's disease Tg2576 mice. AAPS J 2013, 15, 324–336. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.-Y.; Chun, Y.-S.; Kim, J.-K.; Lee, J.-O.; Ku, S.-K.; Shim, S.-M. Curcumin attenuates sarcopenia in chronic forced exercise executed aged mice by regulating muscle degradation and protein synthesis with antioxidant and anti-inflammatory effects. Journal of Agricultural and Food Chemistry 2021, 69, 6214–6228. [Google Scholar] [CrossRef] [PubMed]
- Miller, D.B.; O’Callaghan, J.P. Biomarkers of Parkinson’s disease: present and future. Metabolism 2015, 64, S40–S46. [Google Scholar] [CrossRef] [PubMed]
- Cabreira, V.; Massano, J. Doença de Parkinson: Revisão clínica e atualização [Parkinson's disease: Clinical review and update]. Acta Med Port 2019, 32, 661–670. [Google Scholar] [CrossRef]
- Solleiro-Villavicencio, H.; Rivas-Arancibia, S. Effect of chronic oxidative stress on neuroinflammatory response mediated by CD4+ T cells in neurodegenerative diseases. Frontiers in cellular neuroscience 2018, 12, 114. [Google Scholar] [CrossRef] [PubMed]
- Puspita, L.; Chung, S.Y.; Shim, J.-w. Oxidative stress and cellular pathologies in Parkinson’s disease. Molecular brain 2017, 10, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Martinez, B.; Peplow, P.V. Neuroprotection by immunomodulatory agents in animal models of Parkinson’s disease. Neural Regeneration Research 2018, 13, 1493–1506. [Google Scholar] [PubMed]
- Achete de Souza, G.; de Marqui, S.V.; Matias, J.N.; Guiguer, E.L.; Barbalho, S.M. Effects of Ginkgo biloba on Diseases Related to Oxidative Stress. Planta medica 2020, 86, 376–386. [Google Scholar] [CrossRef]
- de Oliveira Zanuso, B.; de Oliveira Dos Santos, A.R.; Miola, V.F.B.; Guissoni Campos, L.M.; Spilla, C.S.G.; Barbalho, S.M. Panax ginseng and aging related disorders: A systematic review. Experimental gerontology 2022, 161, 111731. [Google Scholar] [CrossRef] [PubMed]
- Barbalho, S.M.; Direito, R.; Laurindo, L.F.; Marton, L.T.; Guiguer, E.L.; Goulart, R.A.; Tofano, R.J.; Carvalho, A.C.A.; Flato, U.A.P.; Capelluppi Tofano, V.A.; et al. Ginkgo biloba in the Aging Process: A Narrative Review. Antioxidants (Basel, Switzerland) 2022, 11. [Google Scholar] [CrossRef] [PubMed]
- Dhouib, I.B.; Annabi, A.; Doghri, R.; Rejeb, I.; Dallagi, Y.; Bdiri, Y.; Lasram, M.M.; Elgaaied, A.; Marrakchi, R.; Fazaa, S. Neuroprotective effects of curcumin against acetamiprid-induced neurotoxicity and oxidative stress in the developing male rat cerebellum: biochemical, histological, and behavioral changes. Environmental Science and Pollution Research 2017, 24, 27515–27524. [Google Scholar] [CrossRef] [PubMed]
- Mamun, A.A.; Shao, C.; Geng, P.; Wang, S.; Xiao, J. Polyphenols Targeting NF-κB Pathway in Neurological Disorders: What We Know So Far? International journal of biological sciences 2024, 20, 1332–1355. [Google Scholar] [CrossRef] [PubMed]
- Reglodi, D.; Renaud, J.; Tamas, A.; Tizabi, Y.; Socías, S.B.; Del-Bel, E.; Raisman-Vozari, R. Novel tactics for neuroprotection in Parkinson's disease: role of antibiotics, polyphenols and neuropeptides. Progress in neurobiology 2017, 155, 120–148. [Google Scholar] [CrossRef] [PubMed]
- Bhat, A.; Mahalakshmi, A.M.; Ray, B.; Tuladhar, S.; Hediyal, T.A.; Manthiannem, E.; Padamati, J.; Chandra, R.; Chidambaram, S.B.; Sakharkar, M.K. Benefits of curcumin in brain disorders. BioFactors 2019, 45, 666–689. [Google Scholar] [CrossRef] [PubMed]
- Sharma, N.; Nehru, B.J.I. Curcumin affords neuroprotection and inhibits α-synuclein aggregation in lipopolysaccharide-induced Parkinson’s disease model. 2018, 26, 349-360.
- Khadrawy, Y.A.; Hosny, E.N.; Eldein Mohamed, H.S. Assessment of the neuroprotective effect of green synthesized iron oxide nanoparticles capped with curcumin against a rat model of Parkinson's disease. Iranian journal of basic medical sciences 2024, 27, 81–89. [Google Scholar] [CrossRef] [PubMed]
- Bandeen-Roche, K.; Seplaki, C.L.; Huang, J.; Buta, B.; Kalyani, R.R.; Varadhan, R.; Xue, Q.-L.; Walston, J.D.; Kasper, J.D. Frailty in older adults: a nationally representative profile in the United States. Journals of Gerontology Series A: Biomedical Sciences and Medical Sciences 2015, 70, 1427–1434. [Google Scholar] [CrossRef] [PubMed]
- Proietti, M.; Cesari, M. Frailty: what is it? Frailty and Cardiovascular Diseases: Research into an Elderly Population 2020, 1-7.
- Cesari, M.; Calvani, R.; Marzetti, E. Frailty in older persons. Clinics in geriatric medicine 2017, 33, 293–303. [Google Scholar] [CrossRef] [PubMed]
- Asavamongkolkul, A.; Adulkasem, N.; Chotiyarnwong, P.; Vanitcharoenkul, E.; Chandhanayingyong, C.; Laohaprasitiporn, P.; Soparat, K.; Unnanuntana, A. Prevalence of osteoporosis, sarcopenia, and high falls risk in healthy community-dwelling Thai older adults: a nationwide cross-sectional study. JBMR plus 2024, 8, ziad020. [Google Scholar] [CrossRef] [PubMed]
- Hoogendijk, E.O.; Afilalo, J.; Ensrud, K.E.; Kowal, P.; Onder, G.; Fried, L.P. Frailty: implications for clinical practice and public health. The Lancet 2019, 394, 1365–1375. [Google Scholar] [CrossRef] [PubMed]
- Bandeen-Roche, K.; Xue, Q.-L.; Ferrucci, L.; Walston, J.; Guralnik, J.M.; Chaves, P.; Zeger, S.L.; Fried, L.P. Phenotype of frailty: characterization in the women's health and aging studies. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences 2006, 61, 262–266. [Google Scholar] [CrossRef] [PubMed]
- Xue, Q.-L.; Walston, J.D.; Fried, L.P.; Beamer, B.A. Prediction of risk of falling, physical disability, and frailty by rate of decline in grip strength: the women's health and aging study. Archives of Internal Medicine 2011, 171, 1119–1121. [Google Scholar] [CrossRef] [PubMed]
- Ensrud, K.E.; Ewing, S.K.; Taylor, B.C.; Fink, H.A.; Stone, K.L.; Cauley, J.A.; Tracy, J.K.; Hochberg, M.C.; Rodondi, N.; Cawthon, P.M. Frailty and risk of falls, fracture, and mortality in older women: the study of osteoporotic fractures. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences 2007, 62, 744–751. [Google Scholar] [CrossRef] [PubMed]
- Makary, M.A.; Segev, D.L.; Pronovost, P.J.; Syin, D.; Bandeen-Roche, K.; Patel, P.; Takenaga, R.; Devgan, L.; Holzmueller, C.G.; Tian, J. Frailty as a predictor of surgical outcomes in older patients. Journal of the American College of Surgeons 2010, 210, 901–908. [Google Scholar] [CrossRef] [PubMed]
- McAdams-DeMarco, M.A.; Suresh, S.; Law, A.; Salter, M.L.; Gimenez, L.F.; Jaar, B.G.; Walston, J.D.; Segev, D.L. Frailty and falls among adult patients undergoing chronic hemodialysis: a prospective cohort study. BMC nephrology 2013, 14, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Cawthon, P.M.; Marshall, L.M.; Michael, Y.; Dam, T.T.; Ensrud, K.E.; Barrett-Connor, E.; Orwoll, E.S.; Group, O.F.i.M.R. Frailty in older men: prevalence, progression, and relationship with mortality. Journal of the American Geriatrics Society 2007, 55, 1216–1223. [Google Scholar] [CrossRef] [PubMed]
- Collard, R.M.; Boter, H.; Schoevers, R.A.; Oude Voshaar, R.C. Prevalence of frailty in community-dwelling older persons: a systematic review. Journal of the american geriatrics society 2012, 60, 1487–1492. [Google Scholar] [CrossRef] [PubMed]
- Santos-Eggimann, B.; Cuénoud, P.; Spagnoli, J.; Junod, J. Prevalence of frailty in middle-aged and older community-dwelling Europeans living in 10 countries. Journals of Gerontology Series A: Biomedical Sciences and Medical Sciences 2009, 64, 675–681. [Google Scholar] [CrossRef] [PubMed]
- Ikegami, S.; Uehara, M.; Tokida, R.; Nishimura, H.; Sakai, N.; Horiuchi, H.; Kato, H.; Takahashi, J. Male-female disparity in clinical features and significance of mild vertebral fractures in community-dwelling residents aged 50 and over. Scientific reports 2024, 14, 5602. [Google Scholar] [CrossRef]
- Nicol, L.M.; Rowlands, D.S.; Fazakerly, R.; Kellett, J. Curcumin supplementation likely attenuates delayed onset muscle soreness (DOMS). European journal of applied physiology 2015, 115, 1769–1777. [Google Scholar] [CrossRef] [PubMed]
- Drobnic, F.; Riera, J.; Appendino, G.; Togni, S.; Franceschi, F.; Valle, X.; Pons, A.; Tur, J. Reduction of delayed onset muscle soreness by a novel curcumin delivery system (Meriva®): a randomised, placebo-controlled trial. Journal of the International Society of Sports Nutrition 2014, 11, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Perna, S.; Alalwan, T.A.; Al-Thawadi, S.; Negro, M.; Parimbelli, M.; Cerullo, G.; Gasparri, C.; Guerriero, F.; Infantino, V.; Diana, M. Evidence-based role of nutrients and antioxidants for chronic pain management in musculoskeletal frailty and sarcopenia in aging. Geriatrics 2020, 5, 16. [Google Scholar] [CrossRef] [PubMed]
- Mankowski, R.T.; Sibille, K.T.; Leeuwenburgh, C.; Lin, Y.; Hsu, F.C.; Qiu, P.; Sandesara, B.; Anton, S.D. Effects of Curcumin C3 Complex® on Physical Function in Moderately Functioning Older Adults with Low-Grade Inflammation - A Pilot Trial. The Journal of frailty & aging 2023, 12, 143–149. [Google Scholar] [CrossRef]
- Saud Gany, S.L.; Chin, K.-Y.; Tan, J.K.; Aminuddin, A.; Makpol, S. Curcumin as a therapeutic agent for sarcopenia. Nutrients 2023, 15, 2526. [Google Scholar] [CrossRef] [PubMed]
- Cruz-Jentoft, A.J.; Baeyens, J.P.; Bauer, J.M.; Boirie, Y.; Cederholm, T.; Landi, F.; Martin, F.C.; Michel, J.-P.; Rolland, Y.; Schneider, S.M. Sarcopenia: European consensus on definition and diagnosis: Report of the European Working Group on Sarcopenia in Older People. Age and ageing 2010, 39, 412–423. [Google Scholar] [CrossRef] [PubMed]
- Morley, J.E.; Abbatecola, A.M.; Argiles, J.M.; Baracos, V.; Bauer, J.; Bhasin, S.; Cederholm, T.; Coats, A.J.S.; Cummings, S.R.; Evans, W.J. Sarcopenia with limited mobility: an international consensus. Journal of the American Medical Directors Association 2011, 12, 403–409. [Google Scholar] [CrossRef] [PubMed]
- Studenski, S.A.; Peters, K.W.; Alley, D.E.; Cawthon, P.M.; McLean, R.R.; Harris, T.B.; Ferrucci, L.; Guralnik, J.M.; Fragala, M.S.; Kenny, A.M. The FNIH sarcopenia project: rationale, study description, conference recommendations, and final estimates. Journals of Gerontology Series A: Biomedical Sciences and Medical Sciences 2014, 69, 547–558. [Google Scholar] [CrossRef] [PubMed]
- Mellen, R.H.; Girotto, O.S.; Marques, E.B.; Laurindo, L.F.; Grippa, P.C.; Mendes, C.G.; Garcia, L.N.H.; Bechara, M.D.; Barbalho, S.M.; Sinatora, R.V.; et al. Insights into Pathogenesis, Nutritional and Drug Approach in Sarcopenia: A Systematic Review. Biomedicines 2023, 11. [Google Scholar] [CrossRef]
- Minniti, G.; Pescinini-Salzedas, L.M.; Minniti, G.; Laurindo, L.F.; Barbalho, S.M.; Vargas Sinatora, R.; Sloan, L.A.; Haber, R.S.A.; Araújo, A.C.; Quesada, K.; et al. Organokines, Sarcopenia, and Metabolic Repercussions: The Vicious Cycle and the Interplay with Exercise. International journal of molecular sciences 2022, 23. [Google Scholar] [CrossRef] [PubMed]
- Barbalho, S.M.; Flato, U.A.P.; Tofano, R.J.; Goulart, R.A.; Guiguer, E.L.; Detregiachi, C.R.P.; Buchaim, D.V.; Araújo, A.C.; Buchaim, R.L.; Reina, F.T.R.; et al. Physical Exercise and Myokines: Relationships with Sarcopenia and Cardiovascular Complications. International journal of molecular sciences 2020, 21. [Google Scholar] [CrossRef] [PubMed]
- Park, J.; Park, S. Association of Handgrip Strength and Cardiovascular Disease Risk Among Middle-Aged Postmenopausal Women: An Analysis of the Korea National Health and Nutrition Examination Survey 2014-2019. Vascular health and risk management 2024, 20, 183–194. [Google Scholar] [CrossRef] [PubMed]
- Ferri, E.; Marzetti, E.; Calvani, R.; Picca, A.; Cesari, M.; Arosio, B. Role of age-related mitochondrial dysfunction in sarcopenia. International journal of molecular sciences 2020, 21, 5236. [Google Scholar] [CrossRef]
- Dong, H.; Ni, W.; Bai, Y.; Yuan, X.; Zhang, Y.; Zhang, H.; Sun, Y.; Xu, J.J.S.r. Cross-sectional and longitudinal associations of apolipoprotein A1 and B with glycosylated hemoglobin in Chinese adults. 2022, 12, 1-8.
- Ticinesi, A.; Nouvenne, A.; Cerundolo, N.; Parise, A.; Meschi, T. Accounting gut microbiota as the mediator of beneficial effects of dietary (poly) phenols on skeletal muscle in aging. Nutrients 2023, 15, 2367. [Google Scholar] [CrossRef]
- Goates, S.; Du, K.; Arensberg, M.; Gaillard, T.; Guralnik, J.; Pereira, S.L. Economic impact of hospitalizations in US adults with sarcopenia. The Journal of frailty & aging 2019, 8, 93–99. [Google Scholar]
- Dalle, S.; Rossmeislova, L.; Koppo, K. The role of inflammation in age-related sarcopenia. Frontiers in physiology 2017, 8, 311540. [Google Scholar] [CrossRef] [PubMed]
- Bian, A.-L.; Hu, H.-Y.; Rong, Y.-D.; Wang, J.; Wang, J.-X.; Zhou, X.-Z. A study on relationship between elderly sarcopenia and inflammatory factors IL-6 and TNF-α. European journal of medical research 2017, 22, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Schaap, L.A.; Pluijm, S.M.; Deeg, D.J.; Visser, M. Inflammatory markers and loss of muscle mass (sarcopenia) and strength. The American journal of medicine 2006, 119, 526.e9–526.e17. [Google Scholar] [CrossRef] [PubMed]
- Baylis, D.; Bartlett, D.B.; Syddall, H.E.; Ntani, G.; Gale, C.R.; Cooper, C.; Lord, J.M.; Sayer, A.A. Immune-endocrine biomarkers as predictors of frailty and mortality: a 10-year longitudinal study in community-dwelling older people. Age 2013, 35, 963–971. [Google Scholar] [CrossRef] [PubMed]
- Aggarwal, B.B.; Kumar, A.; Bharti, A.C. Anticancer potential of curcumin: preclinical and clinical studies. Anticancer research 2003, 23, 363–398. [Google Scholar] [PubMed]
- Gorza, L.; Germinario, E.; Tibaudo, L.; Vitadello, M.; Tusa, C.; Guerra, I.; Bondì, M.; Salmaso, S.; Caliceti, P.; Vitiello, L. Chronic systemic curcumin administration antagonizes murine sarcopenia and presarcopenia. International Journal of Molecular Sciences 2021, 22, 11789. [Google Scholar] [CrossRef] [PubMed]
- Saud Gany, S.L.; Chin, K.Y.; Tan, J.K.; Aminuddin, A.; Makpol, S. Curcumin as a Therapeutic Agent for Sarcopenia. Nutrients 2023, 15. [Google Scholar] [CrossRef] [PubMed]
- Gorza, L.; Germinario, E.; Tibaudo, L.; Vitadello, M.; Tusa, C.; Guerra, I.; Bondì, M.; Salmaso, S.; Caliceti, P.; Vitiello, L.; et al. Chronic Systemic Curcumin Administration Antagonizes Murine Sarcopenia and Presarcopenia. International journal of molecular sciences 2021, 22. [Google Scholar] [CrossRef] [PubMed]
- Kawamori, T.; Lubet, R.; Steele, V.E.; Kelloff, G.J.; Kaskey, R.B.; Rao, C.V.; Reddy, B.S. Chemopreventive effect of curcumin, a naturally occurring anti-inflammatory agent, during the promotion/progression stages of colon cancer. Cancer research 1999, 59, 597–601. [Google Scholar] [PubMed]
- Asai, A.; Miyazawa, T. Occurrence of orally administered curcuminoid as glucuronide and glucuronide/sulfate conjugates in rat plasma. Life sciences 2000, 67, 2785–2793. [Google Scholar] [CrossRef] [PubMed]
- Öner-İyidoğan, Y.; Tanrıkulu-Küçük, S.; Seyithanoğlu, M.; Koçak, H.; Doğru-Abbasoğlu, S.; Aydin, A.F.; Beyhan-Özdaş, Ş.; Yapişlar, H.; Koçak-Toker, N. Effect of curcumin on hepatic heme oxygenase 1 expression in high fat diet fed rats: is there a triangular relationship? Can J Physiol Pharmacol 2014, 92, 805–812. [Google Scholar] [CrossRef] [PubMed]
- Receno, C.N.; Liang, C.; Korol, D.L.; Atalay, M.; Heffernan, K.S.; Brutsaert, T.D.; DeRuisseau, K.C. Effects of Prolonged Dietary Curcumin Exposure on Skeletal Muscle Biochemical and Functional Responses of Aged Male Rats. Int J Mol Sci 2019, 20. [Google Scholar] [CrossRef] [PubMed]
- Liang, Y.J.; Yang, I.H.; Lin, Y.W.; Lin, J.N.; Wu, C.C.; Chiang, C.Y.; Lai, K.H.; Lin, F.H. Curcumin-Loaded Hydrophobic Surface-Modified Hydroxyapatite as an Antioxidant for Sarcopenia Prevention. Antioxidants (Basel) 2021, 10. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.Y.; Chun, Y.S.; Kim, J.K.; Lee, J.O.; Ku, S.K.; Shim, S.M. Curcumin Attenuates Sarcopenia in Chronic Forced Exercise Executed Aged Mice by Regulating Muscle Degradation and Protein Synthesis with Antioxidant and Anti-inflammatory Effects. J Agric Food Chem 2021, 69, 6214–6228. [Google Scholar] [CrossRef] [PubMed]
- Sani, A.; Hasegawa, K.; Yamaguchi, Y.; Panichayupakaranant, P.; Pengjam, Y. Inhibitory effects of curcuminoids on dexamethasone-induced muscle atrophy in differentiation of C2C12 cells. Phytomedicine plus 2021, 1, 100012. [Google Scholar] [CrossRef]
- Varma, K.; Amalraj, A.; Divya, C.; Gopi, S. The Efficacy of the Novel Bioavailable Curcumin (Cureit) in the Management of Sarcopenia in Healthy Elderly Subjects: A Randomized, Placebo-Controlled, Double-Blind Clinical Study. J Med Food 2021, 24, 40–49. [Google Scholar] [CrossRef] [PubMed]
- Ghodsi, H.; Rahimi, H.R.; Aghili, S.M.; Saberi, A.; Shoeibi, A. Evaluation of curcumin as add-on therapy in patients with Parkinson's disease: A pilot randomized, triple-blind, placebo-controlled trial. Clinical neurology and neurosurgery 2022, 218, 107300. [Google Scholar] [CrossRef] [PubMed]
- Cox, K.H.; Pipingas, A.; Scholey, A.B. Investigation of the effects of solid lipid curcumin on cognition and mood in a healthy older population. Journal of psychopharmacology (Oxford, England) 2015, 29, 642–651. [Google Scholar] [CrossRef] [PubMed]
- Thota, R.N.; Acharya, S.H.; Garg, M.L. Curcumin and/or omega-3 polyunsaturated fatty acids supplementation reduces insulin resistance and blood lipids in individuals with high risk of type 2 diabetes: a randomised controlled trial. Lipids Health Dis 2019, 18, 31. [Google Scholar] [CrossRef] [PubMed]
- DiSilvestro, R.A.; Joseph, E.; Zhao, S.; Bomser, J. Diverse effects of a low dose supplement of lipidated curcumin in healthy middle aged people. Nutr J 2012, 11, 79. [Google Scholar] [CrossRef] [PubMed]
- Baum, L.; Cheung, S.K.; Mok, V.C.; Lam, L.C.; Leung, V.P.; Hui, E.; Ng, C.C.; Chow, M.; Ho, P.C.; Lam, S.; et al. Curcumin effects on blood lipid profile in a 6-month human study. Pharmacol Res 2007, 56, 509–514. [Google Scholar] [CrossRef] [PubMed]
- Khanna, A.; Das, S.S.; Kannan, R.; Swick, A.G.; Matthewman, C.; Maliakel, B.; Ittiyavirah, S.P.; Krishnakumar, I.M. The effects of oral administration of curcumin-galactomannan complex on brain waves are consistent with brain penetration: a randomized, double-blinded, placebo-controlled pilot study. Nutr Neurosci 2022, 25, 1240–1249. [Google Scholar] [CrossRef] [PubMed]
- Cox, K.H.M.; White, D.J.; Pipingas, A.; Poorun, K.; Scholey, A. Further Evidence of Benefits to Mood and Working Memory from Lipidated Curcumin in Healthy Older People: A 12-Week, Double-Blind, Placebo-Controlled, Partial Replication Study. Nutrients 2020, 12. [Google Scholar] [CrossRef]
- Kuszewski, J.C.; Wong, R.H.X.; Wood, L.G.; Howe, P.R.C. Effects of fish oil and curcumin supplementation on cerebrovascular function in older adults: A randomized controlled trial. Nutrition, metabolism, and cardiovascular diseases : NMCD 2020, 30, 625–633. [Google Scholar] [CrossRef] [PubMed]
- Small, G.W.; Siddarth, P.; Li, Z.; Miller, K.J.; Ercoli, L.; Emerson, N.D.; Martinez, J.; Wong, K.P.; Liu, J.; Merrill, D.A.; et al. Memory and Brain Amyloid and Tau Effects of a Bioavailable Form of Curcumin in Non-Demented Adults: A Double-Blind, Placebo-Controlled 18-Month Trial. The American journal of geriatric psychiatry : official journal of the American Association for Geriatric Psychiatry 2018, 26, 266–277. [Google Scholar] [CrossRef] [PubMed]
- Ross, S.M. Curcuma longa (Theracumin®): A Bioavailable Form of Curcumin and Its Cognitive Benefits. Holist Nurs Pract 2018, 32, 217–220. [Google Scholar] [CrossRef] [PubMed]
- Panahi, Y.; Badeli, R.; Karami, G.R.; Sahebkar, A. Investigation of the efficacy of adjunctive therapy with bioavailability-boosted curcuminoids in major depressive disorder. Phytotherapy research : PTR 2015, 29, 17–21. [Google Scholar] [CrossRef] [PubMed]
- Rainey-Smith, S.R.; Brown, B.M.; Sohrabi, H.R.; Shah, T.; Goozee, K.G.; Gupta, V.B.; Martins, R.N. Curcumin and cognition: a randomised, placebo-controlled, double-blind study of community-dwelling older adults. Br J Nutr 2016, 115, 2106–2113. [Google Scholar] [CrossRef] [PubMed]
- Baum, L.; Cheung, S.K.; Mok, V.C.; Lam, L.C.; Leung, V.P.; Hui, E.; Ng, C.C.; Chow, M.; Ho, P.C.; Lam, S.; et al. Curcumin effects on blood lipid profile in a 6-month human study. Pharmacol Res 2007, 56, 509–514. [Google Scholar] [CrossRef] [PubMed]
- Kucukgoncu, S.; Guloksuz, S.; Tek, C. Effects of Curcumin on Cognitive Functioning and Inflammatory State in Schizophrenia: A Double-Blind, Placebo-Controlled Pilot Trial. J Clin Psychopharmacol 2019, 39, 182–184. [Google Scholar] [CrossRef] [PubMed]
- Dei Cas, M.; Ghidoni, R. Dietary Curcumin: Correlation between Bioavailability and Health Potential. Nutrients 2019, 11. [Google Scholar] [CrossRef] [PubMed]
- Kunnumakkara, A.B.; Harsha, C.; Banik, K.; Vikkurthi, R.; Sailo, B.L.; Bordoloi, D.; Gupta, S.C.; Aggarwal, B.B. Is curcumin bioavailability a problem in humans: lessons from clinical trials. Expert opinion on drug metabolism & toxicology 2019, 15, 705–733. [Google Scholar] [CrossRef]
- Vashisht, M.; Rani, P.; Onteru, S.K.; Singh, D. Curcumin Encapsulated in Milk Exosomes Resists Human Digestion and Possesses Enhanced Intestinal Permeability in Vitro. Applied biochemistry and biotechnology 2017, 183, 993–1007. [Google Scholar] [CrossRef] [PubMed]
- Marton, L.T.; Pescinini, E.S.L.M.; Camargo, M.E.C.; Barbalho, S.M.; Haber, J.; Sinatora, R.V.; Detregiachi, C.R.P.; Girio, R.J.S.; Buchaim, D.V.; Cincotto Dos Santos Bueno, P. The Effects of Curcumin on Diabetes Mellitus: A Systematic Review. Frontiers in endocrinology 2021, 12, 669448. [Google Scholar] [CrossRef] [PubMed]
- Akuri, M.C.; Barbalho, S.M.; Val, R.M.; Guiguer, E.L. Reflections about Osteoarthritis and Curcuma longa. Pharmacognosy reviews 2017, 11, 8–12. [Google Scholar] [CrossRef] [PubMed]
- Gopi, S.; Jacob, J.; Varma, K.; Jude, S.; Amalraj, A.; Arundhathy, C.A.; George, R.; Sreeraj, T.R.; Divya, C.; Kunnumakkara, A.B.; et al. Comparative Oral Absorption of Curcumin in a Natural Turmeric Matrix with Two Other Curcumin Formulations: An Open-label Parallel-arm Study. Phytotherapy research : PTR 2017, 31, 1883–1891. [Google Scholar] [CrossRef] [PubMed]
- Kocher, A.; Bohnert, L.; Schiborr, C.; Frank, J. Highly bioavailable micellar curcuminoids accumulate in blood, are safe and do not reduce blood lipids and inflammation markers in moderately hyperlipidemic individuals. Molecular nutrition & food research 2016, 60, 1555–1563. [Google Scholar] [CrossRef]
- Sharifi-Rad, J.; Rayess, Y.E.; Rizk, A.A.; Sadaka, C.; Zgheib, R.; Zam, W.; Sestito, S.; Rapposelli, S.; Neffe-Skocińska, K.; Zielińska, D.; et al. Turmeric and Its Major Compound Curcumin on Health: Bioactive Effects and Safety Profiles for Food, Pharmaceutical, Biotechnological and Medicinal Applications. Frontiers in pharmacology 2020, 11, 01021. [Google Scholar] [CrossRef] [PubMed]
- Zeng, L.; Yang, T.; Yang, K.; Yu, G.; Li, J.; Xiang, W.; Chen, H. Efficacy and Safety of Curcumin and Curcuma longa Extract in the Treatment of Arthritis: A Systematic Review and Meta-Analysis of Randomized Controlled Trial. Frontiers in immunology 2022, 13, 891822. [Google Scholar] [CrossRef] [PubMed]
- Shep, D.; Khanwelkar, C.; Gade, P.; Karad, S. Safety and efficacy of curcumin versus diclofenac in knee osteoarthritis: a randomized open-label parallel-arm study. Trials 2019, 20, 214. [Google Scholar] [CrossRef] [PubMed]
- Pivari, F.; Mingione, A.; Piazzini, G.; Ceccarani, C.; Ottaviano, E.; Brasacchio, C.; Dei Cas, M.; Vischi, M.; Cozzolino, M.G.; Fogagnolo, P.; et al. Curcumin Supplementation (Meriva(®)) Modulates Inflammation, Lipid Peroxidation and Gut Microbiota Composition in Chronic Kidney Disease. Nutrients 2022, 14. [Google Scholar] [CrossRef] [PubMed]
- Panahi, Y.; Kianpour, P.; Mohtashami, R.; Jafari, R.; Simental-Mendía, L.E.; Sahebkar, A. Efficacy and Safety of Phytosomal Curcumin in Non-Alcoholic Fatty Liver Disease: A Randomized Controlled Trial. Drug research 2017, 67, 244–251. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, M.; Vécsei, L. A Decade of Dedication: Pioneering Perspectives on Neurological Diseases and Mental Illnesses. MDPI: 2024; Vol. 12, p 1083.
- Tanaka, M.; Battaglia, S.; Giménez-Llort, L.; Chen, C.; Hepsomali, P.; Avenanti, A.; Vécsei, L. Innovation at the intersection: emerging translational research in neurology and psychiatry. MDPI: 2024; Vol. 13, p 790.
- Tanaka, M.; Vécsei, L. From Lab to Life: Exploring Cutting-Edge Models for Neurological and Psychiatric Disorders. Biomedicines 2024, 12, 613. [Google Scholar] [CrossRef] [PubMed]
- Tajti, J.; Szok, D.; Csáti, A.; Szabó, Á.; Tanaka, M.; Vécsei, L. Exploring novel therapeutic targets in the common pathogenic factors in migraine and neuropathic pain. International Journal of Molecular Sciences 2023, 24, 4114. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, M.; Török, N.; Tóth, F.; Szabó, Á.; Vécsei, L. Co-players in chronic pain: neuroinflammation and the tryptophan-kynurenine metabolic pathway. Biomedicines 2021, 9, 897. [Google Scholar] [CrossRef]
- Battaglia, S.; Schmidt, A.; Hassel, S.; Tanaka, M. Case reports in neuroimaging and stimulation. Frontiers Media SA: 2023; Vol. 14, p 1264669.
- Balogh, L.; Tanaka, M.; Török, N.; Vécsei, L.; Taguchi, S. Crosstalk between existential phenomenological psychotherapy and neurological sciences in mood and anxiety disorders. Biomedicines 2021, 9, 340. [Google Scholar] [CrossRef] [PubMed]
- Jászberényi, M.; Thurzó, B.; Bagosi, Z.; Vécsei, L.; Tanaka, M. The Orexin/Hypocretin System, the Peptidergic Regulator of Vigilance, Orchestrates Adaptation to Stress. Biomedicines 2024, 12, 448. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, M.; Diano, M.; Battaglia, S. Insights into structural and functional organization of the brain: evidence from neuroimaging and non-invasive brain stimulation techniques. Frontiers Media SA: 2023; Vol. 14, p 1225755.
- Tanaka, M.; Szabó, Á.; Körtési, T.; Szok, D.; Tajti, J.; Vécsei, L. From CGRP to PACAP, VIP, and beyond: unraveling the next chapters in migraine treatment. Cells 2023, 12, 2649. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, M.; Szabó, Á.; Vécsei, L. Preclinical modeling in depression and anxiety: Current challenges and future research directions. Advances in Clinical and Experimental Medicine 2023, 32, 505–509. [Google Scholar] [CrossRef] [PubMed]
- Polyák, H.; Galla, Z.; Nánási, N.; Cseh, E.K.; Rajda, C.; Veres, G.; Spekker, E.; Szabó, Á.; Klivényi, P.; Tanaka, M. The tryptophan-kynurenine metabolic system is suppressed in cuprizone-induced model of demyelination simulating progressive multiple sclerosis. Biomedicines 2023, 11, 945. [Google Scholar] [CrossRef] [PubMed]
- Török, N.; Maszlag-Török, R.; Molnár, K.; Szolnoki, Z.; Somogyvári, F.; Boda, K.; Tanaka, M.; Klivényi, P.; Vécsei, L. Single Nucleotide Polymorphisms of Indoleamine 2, 3-Dioxygenase1 Influenced the Age Onset of Parkinson's Disease. Frontiers in Bioscience-Landmark 2022, 27, 1–11. [Google Scholar] [CrossRef]
- Tanaka, M.; Szabó, Á.; Vécsei, L.; Giménez-Llort, L. Emerging translational research in neurological and psychiatric diseases: From in vitro to in vivo models. MDPI: 2023; Vol. 24, p 15739.

| Reference | Model/Country | Population | Intervention/Comparison | Outcomes | Side Effects |
|---|---|---|---|---|---|
| Sarcopenia | |||||
| [240] | Randomized, placebo-controlled, double-blind clinical trial. India |
30 healthy elderly individuals, 13♂, 17♀, 69.8±5. | Participants received 500mg/day of Cureit or placebo for 3 months. | ↑ 1.43% in handgrip strength, a considerable increase of 6.08% in weightlifting strength, and a positive impact on the distance covered before feeling tired (↑ 1.15%, along with speed walking (5,51m)). | No adverse events were observed. |
| Parkinson's disease | |||||
| [241] | Pilot, randomized, triple-blind, placebo-controlled, add-on trial. Iran | 60 subjects, 45♂, 15♀, 58.2±11.2 y, with idiopathic PD | Subjects received curmin nanomicelles in capsules 80 mg/day or placebo /9 months. Then, the scores MDS-UPDRS and PDQ-39 were calculated at 3, 6, and 9 months. | Curcumin group did not have a significant improvement in MDS-UPDRS and PDQ-39 scores compared to placebo group. | Nausea, vomiting, and dyspepsia. |
| Frailty | |||||
| [212] | Pilot, 12-week, randomized trial/ United States of America | 17 subjects, 8♀, 9♂, 66-94y, moderately functioning and sedentary, with low-grade systemic inflammation. |
9 subjects were assigned to Curcumin C3 Complex®, receiving 1000mg/day or placebo. At 0 and at 12 weeks, patients underwent functional testing and lower-limb strength tenting. Also, at the begining of treatment, 4, 8, and 12 weeks, venous blood was collected for safety blood chemistry analyses and biomarkers of inflammation. | Curcumin C3 Complex® group demonstrated large effect sizes in the short physical performance battery (d=0.75), measures of knee extension (d=0.69), and flexion peak torque (d=0.82). Futhermore, effects in galectin-3 and IL-6 levels were smaller in curcumin group compared to placebo. | No adverse events were reported. |
| Dementia | |||||
| [242] | Randomized, double-blind, placebo-controlled parallel-groups trial. Australia |
60 healthy subjects, 22♂, 38♀, 60-85y. | Subjects were divided into curcumin group (80m solid lipid formulation (Longvida® Curcumin- 400mg) or placebo/ 1x/day/4 weeks. Participants performed 3 sets of computerized cognitive tasks preceded and followed by an evaluation of state mood. After the first set, a single treatment dose was used, then the assessment was repeated at 1 h and 3 h after dose administration. | The results showed that 1h after administration, curcumin group presented significantly enhanced performance on sustained attention and working memory tasks, compared with placebo. Also, working memory and mood were significantly better during chronic treatment (4 weeks). Furthermore, curcumin significantly reduced total cholesterol and LDL cholesterol levels. | No adverse events were reported. |
| Alzheimer's disease | |||||
| [243] | 12 week, 2 × 2 factorial, double-blinded, randomized controlled trial. Australia |
29 participants, 12♂ , 17♀ (52.3 ± 1.9y) at high risk of developing diabetes or with impaired fasting glucose | Participants were divided into 4 groups,: the placebo; curcumin (2x500mg of curcumin (Meriva®), providing 180 mg of curcumin plus 2x1000mg of corn oil/day); ω3, 2 x 1000 mg of fish oil + placebo or double active (1000 mg of curcumin (Meriva®) + 21000 mg of fish oil. | Curcumin reducted in triglyceride levels, fasting insulin, atherogenic index and the HOMA2-IR. There were no significant effects on CRP, TC, HDL-c, LDL-c; fasting glycemia, glycated hemoglobin, and body composition (body weight, muscle mass, body mass index, body fat percentage, circumference waist). | No adverse events were observed. |
| [252] | Randomised, double-blind, placebo-controlled of 12 months. Australia |
160 healthy individuals; 40–90 y, and no significant cerebral vascular disease; no significant cognitive impairments. | They were randomly assigned to treatment groups with BCM-95 ® CG (Biocurcumax TM) capsule 3x/day (1,500 mg/d) or placebo . | No differences were observed between the placebo and treatment groups in changes in cognitive performance. | Gastrointestinal complaints. |
| [244] | Prospective randomized, 4 weeks. United States of America |
19 healthy participants 17♀, 2 ♂ aged 40-60 y | The selected population was assigned to placebo interventions of starch x 80mg/day of curcumin for 4 weeks | There were no significant effects on TC, LDL-c, HDL-c, superoxide dismutase and glutathione peroxidase; significant reduction in the levels of TG, intercellular adhesion molecule, and plasma amyloid β protein content. Increased NO, myeloperoxidase, catalase activity, and elimination of free radicals. | No adverse events were observed. |
| [253] | Randomized, double-blind, placebo-controlled for 6 months. China. |
34 individuals 29%♂, 71%♀), aged 73.4 ± 8.8 (progressive decline in memory and cognitive function for at least 6 weeks or diagnosed with AD | They presented 3 groups, one consisting of 10 people (control), the second of 8 people (1g of curcumin), and the third (4g of curcumin). | There were no significant effects on the lipid profile (LDL-c, HDL-c, TG, and TC) in both groups receiving curcumin. | Constipation, more, diarrhea, and dizziness. |
| Cognition | |||||
| [246] | Randomized, 30-day, double-blind, placebo-controlled, 3-arm pilot study. India | 18 healthy participants, 12♂ and 6♀, 35-65 y. | Patients were randomized into 3 groups, CGM (500 mgx2/day for 30 days of curcuma-galactomannoside complex; UC (500mg 2x/day for 30 days of curcumin with 95% purity) or placebo | CGM : significant ↑↓in α and β waves, and in the α/β ratio compared to the unformulated curcumin and placebo groups. Furthermore, CGM showed a significant ↓ in audio reaction time (29.8;) compared with placebo and 24.6% with UC. Choice-based visual reaction time was also significantly ↓ (36%) in CGM compared to UC and placebo, which yielded 15.36% and 5.2%, respectively. | No adverse events were reported. |
| [247] | Double-blind, placebo-controlled, 12-week trial/ Australia. | 79 participants ♀ and ♂healthy, 50-85 y. | Participants were divided in curcumin group (400 mg Longvida© curcumin capsule with 80 mg of curcumin 1x/day / 12 weeks) or placebo. | Curcumin group showed better working memory performance at 12 weeks (Serial Threes, Serial Sevens, and performance on a virtual Morris Water Maze) and lower fatigue scores on the POMS at 4 and 12 weeks, and tension, anger, confusion and total mood disturbance in just 4 weeks. | No adverse events were reported. |
| [248] | 16-week double-blind, randomized placebo-controlled trial/ Australia. | 152 older sedentary overweight/obese adults, 50-80y. | Subjects were divided in 4 groups: fish oil + curcumin placebo, curcumin + fish oil placebo, fish oil + curcumin or placebo. Then patients ingested 6 capsules/ day consisting of 2 fish oil capsules and 400mg Longvida® Optimised Curcumin containing 80mg of curcumin, or placebo, 2xd. Then, an evaluation of Transcranial Doppler ultrasound, blood, glycemia, heart rate, arterial compliance, blood lipids, and C-RP was performed. | Curcumin did not significantly affect the performed parameters alone or in combination with fish oil. | Digestive problems and reflux. |
| [254] | Randomized, double-blind, placebo-controlled pilot clinical trial/ USA. | 12 participants 9♂ and 3♀ with chronic schizophrenia, 5-51y. |
Patietns were randomized into 2 groups: curcumin (180 mg/d) or placebo. A commercially available surface-controlled water-soluble form of 300 mg curcumin (30% formulation: 90 mg pure curcumin) or matching placebo capsules were provided. | Complementary curcumin treatment showed significant improvement in working memory (Z =2,200, P =0.028) and reduced IL-6 levels (Z =2,402, P =0.016) compared to placebo. No significant effect of curcumin on PANSS and Calgary Depression scores was found. | No adverse events were reported. |
| [249] | 18-month, randomized, double-blind, two-group parallel design | 40 non-demented adults, 22♀, 18♂ and 50-90y. | Subjects were divided into placebo group or Theracurmin group (90 mg of curcumin), 2 x/d/ 18months. Depression Inventory and neuropsychological test battery were applied. | Buschke-Fuld Selective Reminding Test presented a consistent long-term retrieval improvement with curcumin (ES = 0.63, p = 0.002). Curcumin also improved visual memory and attention. | Transient abdominal pain, gastritis, nausea and heat. |
| [250] | Randomized, 18-month, double-blind, placebo-controlled, parallel-group study. EUA | 40 participants, 51-84y, without dementia. | They were randomized into 2 groups: Theracurmin Group: 90mg of curcumin, 2xd 18 months or placebo group. | Curcumin significantly improved long-term recovery of SRT, visual memory and attention compared with placebo. Assessment of neurodegeneration using PET scans significantly ↆ in the amygdala with curcumin. | No adverse events were reported. |
| [251] | 6-week open study/ Tehran, Iran. | 111 participants, ♀ and ♂ diagnosed with Major Depressive Disorder | They were divided into Group standard antidepressant therapy + curcuminoids (1000mg/d - C3 Complex®) or standard antidepressant therapy alone / 6 weeks. | Both groups had a reduction in BDI-II total and subscale scores at the end of the study. Significantly greater ↓in HADS, anxiety and depression subscales in the curcuminoids versus control group (p<0.001). | Gastrointestinal symptons |
| Study | Question Focus |
Allocation Blinding |
Double- blind |
Losses (>20%) | Prognostic or demographic characteristics | Outcomes | Intention to treat analysis |
Sample calculation |
Adequate follow-up |
|---|---|---|---|---|---|---|---|---|---|
| [240] | Yes | Yes | Yes | No | Yes | Yes | No | Yes | Yes |
| [241] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| [212] | Yes | Yes | Yes | No | Yes | Yes | No | No | Yes |
| [242] | Yes | Yes | Yes | No | Yes | Yes | No | No | Yes |
| [243] | Yes | Yes | Yes | No | Yes | Yes | No | Yes | Yes |
| [252] | Yes | No | Yes | Yes | Yes | Yes | No | Yes | Yes |
| [244] | No | No | Yes | No | No | Yes | No | No | Yes |
| [253] | Yes | Yes | Yes | No | Yes | Yes | No | Yes | Yes |
| [246] | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes |
| [247] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| [248] | Yes | Yes | Yes | No | Yes | Yes | No | Yes | Yes |
| [254] | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| [249] | Yes | Yes | Yes | No | Yes | Yes | No | No | Yes |
| [250] | Yes | No | Yes | ? | Yes | Yes | Yes | No ? | Yes |
| [251] | Yes | No | No | No | Yes | Yes | Yes | Yes | Yes |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





