Introduction
Burns are the main cause of death and disability among the pediatric population.[
1,
2] They represent nearly 180,000 deaths annually, and it´s the fifth cause of non-fatal injuries in children.[
1,
3] According to the WHO “Global Burn Registry”, pediatric patients represent 42% of all burn injuries of which preschool-age children (1 – 5 years) represent the larges percentage (62%).[
1,
3] The management of burned pediatric patients deserves special attention, since there is a generalized deficiency in the overall capacity to treat burn injuries, specially in this age group. In pediatric patients the skin is thinner, which predisposes them to deeper and more extensive burns: as well as greater morbidity due to scar contractures.[
1,
4] A comprehensive treatment of burn injuries consists of an adequate management of the airway, sedation, surgical debridement, reconstruction of the burned areas, adequate nutritional support and rehabilitation.[
1,
5] Regarding the surgical management of the burned patient, this includes early debridement and timely skin coverage of the wounds through the usage of adequate dressings, skin grafts or flaps.[
1,
6] Dressings are defined as any healing or protective material that is applied to a wound, in this case a burned area, and imitate a component of the skin and its function. Their basic principle is to absorb exudate, serve as an antimicrobial barrier and against foreign bodies, preventing the development of infections and inflammation. Currently there is a large number of “advanced” dressings composed of different biomaterials and bioactive principles, which accelerate the epithelialization and healing process.[
7] Epifast ® (Bioskinco S.A. de C.V. Estado de México, México) is a special and advanced dressing used in the coverage of burned areas, which consists of a sheet of human keratinocytes cultured and grown in vitro. Its function is that of an allograft of bio-preserved human epidermis, and its mechanism, is based on growth factors. This dressing stimulates cell migration accelerating the formation of granulation tissue through the deposition of “tenascin, type IV collagen and laminin” by fibroblasts, resulting in a reduction in epithelialization time (up to 50%) as well as a faster recovery time, decrease in fibrosis and pain, and as a barrier protecting against infections.[
8,
9,
10]
The principle is that cells from human epidermis allografts cultivated, once applied to the wound bed, they have a very short life and are quickly displaced by local keratinocytes. The application of culture temporarily replaces skin functions and the growth factors they contain, stimulate the cells for the repair and closure of wounds stimulating migration, mitosis, maturation and differentiation of the autogenous keratinocytes of the edges and the remaining epithelial elements in the wound bed; They also act on host fibroblasts, improving collagen production.[
11] Allogeneic transplantation of cells, tissues or organs, require treatment to prevent rejection, but implanted cultured human epidermis allografts have an antigenic response very low and a very short life, so immunosuppressive therapy is not necessary to allow its long-term integration and function and compared to autografts.[
12] Considering that availability is greater and in less time, This makes it a great tool for managing complex wounds such as burns.
Alvarez Díaz et cols. Conducted a study concluding that deep partial-thickness burns treated with cryopreserved epidermal allograft (CEA) cultures healed in 5.6 days, compared with 12.2 days in the control group treated with Vaseline-impregnated gauze.[
13]
Rodriguez-Ferreyra P et cols. reported similar results in a retrospective study of 297 pediatric burn patients, with an average epithelialization time after CEA of 7.55 days in superficial and deep second-degree burns. Most patients required only one application of Epifast® CEA. The safety was also demonstrated, as none of the adverse events reported weres causally related to CEA treatment.[
10]
H. Yanaga et al. conducted a study were deep partial-thickness burn wounds (DDB) and split-thickness skin donor sites of pediatric patients were treated with cryopreserved cultured epidermal allografts, reporting the number of days until epithelialization was 9.1 ± 3.6 (earlier than the usual healing period of DDB, up to 3 weeks). Donor site also reporting early wound closure. The period to heal in the grafted area was 7.0 ± 2.3 days, minimizing scaring with better aesthetic results. Concluding cryopreserved cultured epidermal allografts could prevent donor scars and also minimize scarring on the recipient site, emphasizing the advantages of the allograft;
it is frozen stored, and can be used anytime when necessary, it brings about early closure of wounds, it can be applied repeatedly, and a donor is not required.[
14]
Objectives:
Describe the epidemiology of burns that require in-hospital management in the pediatric population.
Analyze and compare the results obtained from the treatment of burn wounds by using the bio-preserved human epidermis allograft (BHEA) and other types of dressings
Analyze and compare the relationship between the use of BHEA and other dressings with further need of a skin graft.
Methodology
A retrospective cross-sectional study was carried out whose population of study were burned patients under 18 years old and were hospitalized for their treatment in a period of time between 2022 and 2023. The patients were grouped into categories based on their age: infants (< 1 year old), preschoolers (1-5 years old), schoolchildren (6-12 years old) and adolescents (13-18 years old). Descriptive statistics were used to represent the epidemiological characteristics, dividing the mechanisms of injury into 6 categories: scald, flame, contact, electrical, chemical and friction. Likewise, a description of full extension, depth and anatomical site of the burned areas was made, comparing the treatment between two groups: 1) the patients who used the special dressing in study with “bio-preserved human epidermis allograft” Epifast ® (
Figure 1 and
Figure 2) the patients where other dressings were used. The study evaluates the time of complete epithelializacion of the burned wound areas, in-hospital stay and the need for skin grafts. Inferential statistics were used to determine the relationship between the use of BHEA and the need for skin grafts compared to the group that did not use the BHEA.
Results
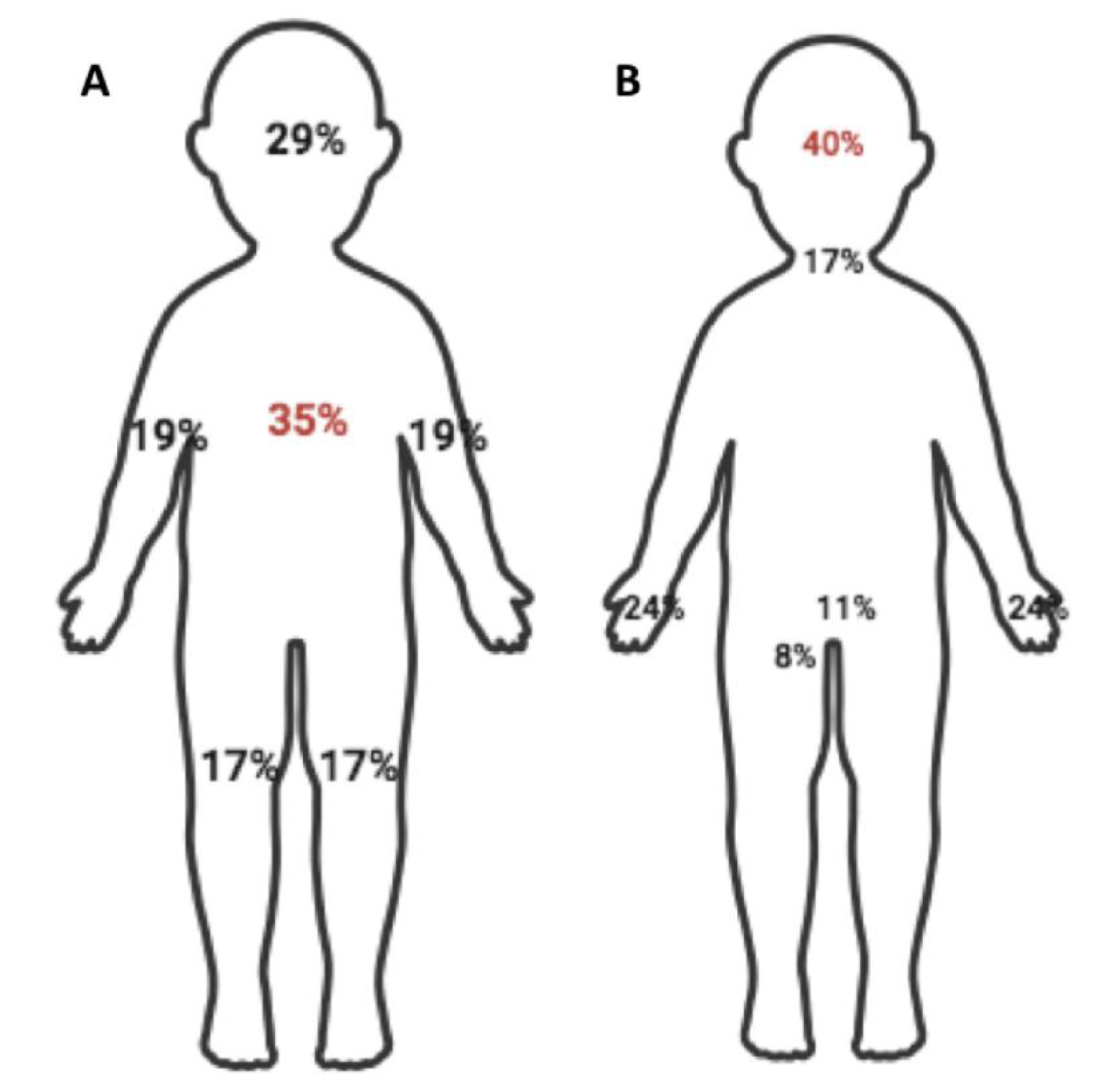
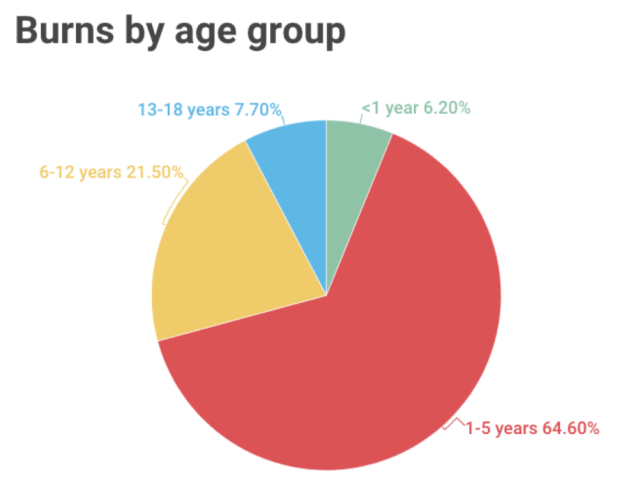
A total population of 65 patients was obtained. The average age of the patients was 4.5 years (±3.8), being preschoolers (1-5 years old) the most frequent category with a population in this range of 42 patient (64%) (
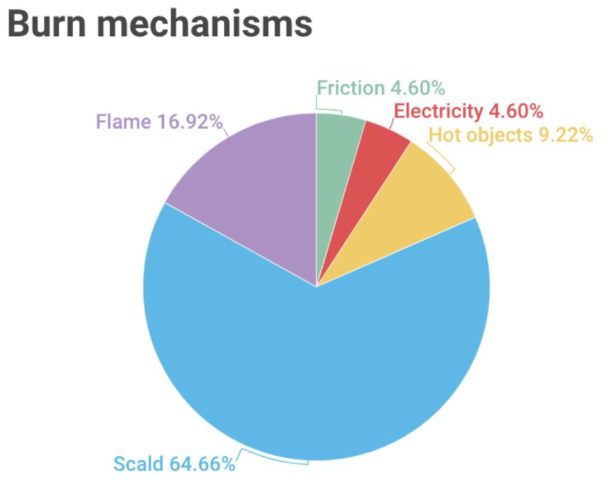
Table 1). The predominant sex were male patients with 61% (n=40). The most frequent mechanism of injury was scald with 64% (n=42) (
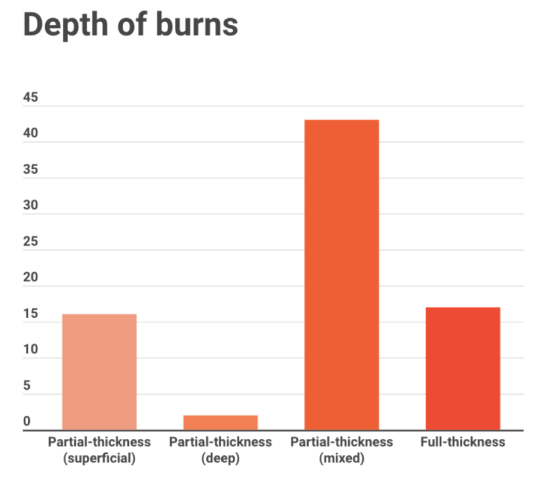
Table 2). Regarding the burn extent, the average total body surface area burned (TBSAB) was 10.8% (± 9.2) with a range between 1 – 40%. The most reported degree of burn injury was mixed partial thickness (superficial and deep) with a 55% (
Table 3). The most affected anatomical area was the trunk with 35% (n=52) (
Figure 3 and
Figure 4-A). In reference to “special areas”, burn injuries in the face were the most frequent with a 40% (n=30) (
Figure 2 and
Figure 4-B). Twenty-six percent of the population (n=17) had burn injuries affecting ≥15% TBSAB, and 23% of this population (n=15) required management in the pediatric intensive care unit. No deaths were reported. The average epithelialization time of the burned injuries was 18.8 days (± 12.8); with an average hospital stay time of 12.8 days (± 11.1). Within the 65 patients, only 32.2 % of the population (n=21) used BHEA as treatment of the burned wounds, and the rest of the population 67.7% (n=44) used another type of dressing as treatment and coverage of the burned area. The average time of epithelialization of the group that used BHEA was 8 days (±7.2), and their average hospital stay time was 7 days (±5.7) (
Figure 2 and
Figure 3). In the group that did not used BHEA, the average epithelialization time of the burned wounds was 18 days (±13.6), and their average hospital stay time was 11 days (±12.6). Fifty percent (n=22) of the patients that did not used BHEA required surgical management for the coverage of the burned areas that did not epithelialize using skin grafts. In the group that BHEA was used, only 19% of the population (n=4) required surgical procedures for skin grafts. An OR of 0.23 and CI of 95% (0.06 – 0.81) were obtained and a p value of (0.017) for the need of skin grafts after de use of BHEA.
Discussion
Based on the results obtained in the study, the average age was 4.5 years (±3.8) and the predominant sex were males with 61%. These results are similar to the ones reported by the “WHO Global Burn Registry” (GBR), who is in charge of describing the global epidemiology of pediatric burned patients. GBR reports an average age of 5.3 years with a 60% predominant male population.[
1] In a national study, where the reported average age was 3.7 years and a predominant 55% male population.[
10] The most frequent age group was preschoolers (1-5 years) with 64%, and in second place, the age group of schoolers (6-12 years) with 21%; this data compares to what was reported by the GBR with 62% y 20%, respectively to each age group. There was also a national study in which the most prevalent age group were preschoolers.[
1,
10]
Regarding the extent and depth of the burn injuries, the average TBSAB in this study was 10.8% with a range of 1-40%. There was also a higher frecuency of mixed pattern partial thickness burns (55%), being similar to the data reported in a national study, mentioning TBSAB of 12.2% and a range of 2-30% and a 64% being mixed pattern partial thickness burns.[
10] Talking about the mechanism of injury, burn from scald was reported the most frequent with 64% and by flame in second place (17%); being equivalent to what was reported in an international report with 64% and 27%, respectively.[
1] In a national study, the report was 86% by scald and 12.8% by flame.[
10] the most affected anatomical site was the head, contrasting with what was reported by the GBR, where the trunk is reported as the most affected area. [
10] Twenty-three percent had major burns (≥15 % TBSAB), which constrasts with the 52% reported in the international literature. [
1,
15]
The average epithelialization time of the patients who were treated with BHEA was 8 days (±7.2), which is similar to the reported in the study of
Rodriguez-Ferreyra P et cols where the time reported is 7.5 days (± 4.2)[
10]. Eighty percent of the patients treated with BHEA had epithelialized at 15 days; the remaining 20% epithelilized at 21 days due to more extensive and full thickness burns that required skin grafts. The average hospital stay was 7 days (±5.7), compared with patients where another dressing coverage method was used and epithelialization time was 18 days (±13.6) with a hospital stay of 11 days (±12.6). In conclusion, the use of BHEA dressings reduces the time of eputhelialization and hospital stay. Fifty percent of the patients that did not used the BHEA dressings required skin grafts to cover the burned area. In the group where BHEA dressgins were used, only 19% (n=4) required skin grafts, adressing that the burn wounds treated and coverd with BHEA dressings had a faster epithelialization rate and less risk of deepening of the burns. An OR of 0.23 and a CI of 95% (0.06 – 0.81) with a p value of (0.017) for the need of skin grafts after the use of BHEA, it can be established that the use of this dressing reduces de risk of requiring a skin graft for management of the burned wounds.
Conclusions
The study of the epidemiological characteristics of burn injuries is important to be able to carry out interventions in terms of prevention and management. With the acquired knowledge, it will help estimate care costs, the need for specialists in burn management and to guide resources for the treatment of this pathology. Taking into account its high morbidity and mortality in the pediatric population, this study demonstrates the epidemiological trends of our population are similar to the trends reported nationally and internationally. The use of crio-preserved human epidermis allograft (Epifast®) proved to be a good option for the management of partial thickness burns and burns in transition, promoting timely epithelilization and avoiding deepening of the burns while reducing morbidity, hospital stay and care costs.
Funding Declaration. This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Competing Interest declaration. The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Data availability. Data generated at a central, large-scale facility, available upon request. HEBM*.
Protection of humans and animals. The authors declare that no experiments on humans or animals have been performed for this research.
Confidentiality of data. We have a consent for publication signed by the legal representatives of patients.
Right to privacy and informed consent. We have a consent for publication signed by the legal representatives of patients.
Use of artificial intelligence to generate texts. The authors declare that they have not used any type of generative artificial intelligence in the writing of this manuscript or for the creation of figures, graphs, tables, or their corresponding captions or legends.
Justification: The following manuscript describes the epidemiological characteristics of burn injuries in pediatric patients in northeastern Mexico, specifically in one important referral center in the state of Monterrey. Also describing the reconstructive management of burn injuries with cryopreserved epidermal allograft, comparing it with other dressings.
Declaration: I declare that I have had no previous discussions with any member of the Editorial Board of Scientific Reports about the work described in the manuscript.
References
- Jordan KC, Di Gennaro JL, von Saint André-von Arnim A, Stewart BT. Global trends in pediatric burn injuries and care capacity from the World Health Organization Global Burn Registry. Front Pediatr. 2022;10:954995. [CrossRef]
- Atiyeh BS, Costagliola M, Hayek SN. Burn prevention mechanisms and outcomes: Pitfalls, failures and successes. Burns. (2009) 35:181–93. [CrossRef]
- World Health Organization. Burns. World Health Organization (2018). Available online at: https://www.who.int/news-room/fact-sheets/detail/burns (accessed March 30, 2022).
- Meng F, Zuo KJ, Amar-Zifkin A, Baird R, Cugno S, Poenaru D. Pediatric burn contractures in low- and lower middle-income countries: A systematic review of causes and factors affecting outcome. Burns. (2020) 46:993–1004. [CrossRef]
- Esparaz JR, Anderson SA, Chen MK, Beierle EA. Who manages burn injuries in children? A program director survey evaluating burn training during pediatric surgery fellowship. J Pediatr Surg. (2022) 57:127–9. [CrossRef]
- Tripathi S, Kaur H, Kashyap R, Dong Y, Gajic O, Murthy S. A survey on the resources and practices in pediatric critical care of resource-rich and resource-limited countries. J Intensive Care. (2015) 3:40. [CrossRef]
- Martínez-Correa E. Systemic classification of wound dressings: A review. Revista Mexicana de Ingenieria Biomedica; 2020.
- Información Técnica – BIOSKINCO [Internet]. Bioskinco.com. [cited 2024 Feb 6]. Available from: https://www.bioskinco.com/productos/epifast/informacion-tecnica/.
- Castellano Ramirez DK, Gonzalez Villordo D, Garcia Bravo D LJ. Manejo de heridas. Cirujano General. (2014) 36112-120.
- Rodriguez-Ferreyra P, Gayosso-Cerón O, Alonso-Campero R, Tellez-Tellez A, Balderas-Sánchez R, Funk M, et al. Experience with Epifast® cryopreserved epidermal allograft in the treatment of superficial and deep second-degree burns: Retrospective study of 297 cases, 2010–2015. Burns Open. 2019;3(3):116–20.
- Oliver AM, Kaawach W, Mithoff EW, Watt A, Abramovich DR, Rayner CR. The differentiation and proliferation of newly formed epidermis on wounds treated with cultured epithelial allografts. Br J Dermatol 1991; 125(2): 147-54.
- Madden MR, LaBruna AA, Hajjar DP, Staiano-Coico L. Transplantation of cryopreserved cultured epidermal allografts. J Trauma 1996; 40(5): 743-50.
- C. Alvarez-Díaz, J. Cuenca-Pardo, A. Sosa-Serrano, E. Juárez-Aguilar, M. Marsch-Moreno, W. Kuri-Harcuch Controlled clinical study of deep partial-thickness burns treated with frozen cultured human allogeneic epidermal sheets J Burn Care Rehabil, 21 (4) (2000), pp.
- Yanaga, H., Udoh, Y., Yamauchi, T., et al. Cryopreserved cultured epidermal allografts achieved early closure of wounds and reduced scar formation in deep partial-thickness burn wounds (DDB) and split-thickness skin donor sites of pediatric patients. Burns: Journal of the International Society for Burn Injuries, 27(7), 689–698.
- Johnson SA, Shi J, Groner JI, Thakkar RK, Fabia R, Besner GE, et al. Interfacility transfer of pediatric burn patients from U.S. Emergency Departments. Burns. (2016) 42:1413–22.
- Masse Sanchez A. Hernandez Aguilar G. 4.063 Pediatric Burns treated on an Outpatient Basis with excellent results with Epifast Cultured Skin Graft. Eur. Burn J. 2019.
- Zulema Cantu Catu M, Vazquez Balboa P. P.073 Surgical management of a paediatric patient with a 90% SCQ by electrical and deflagration burns with the support of cryopreserved cultured epidermal allograft, epifast® at 5 years of evolution Eur. Burn J. 2022.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).