Submitted:
30 June 2024
Posted:
01 July 2024
Read the latest preprint version here
Abstract
Keywords:
1. Introduction
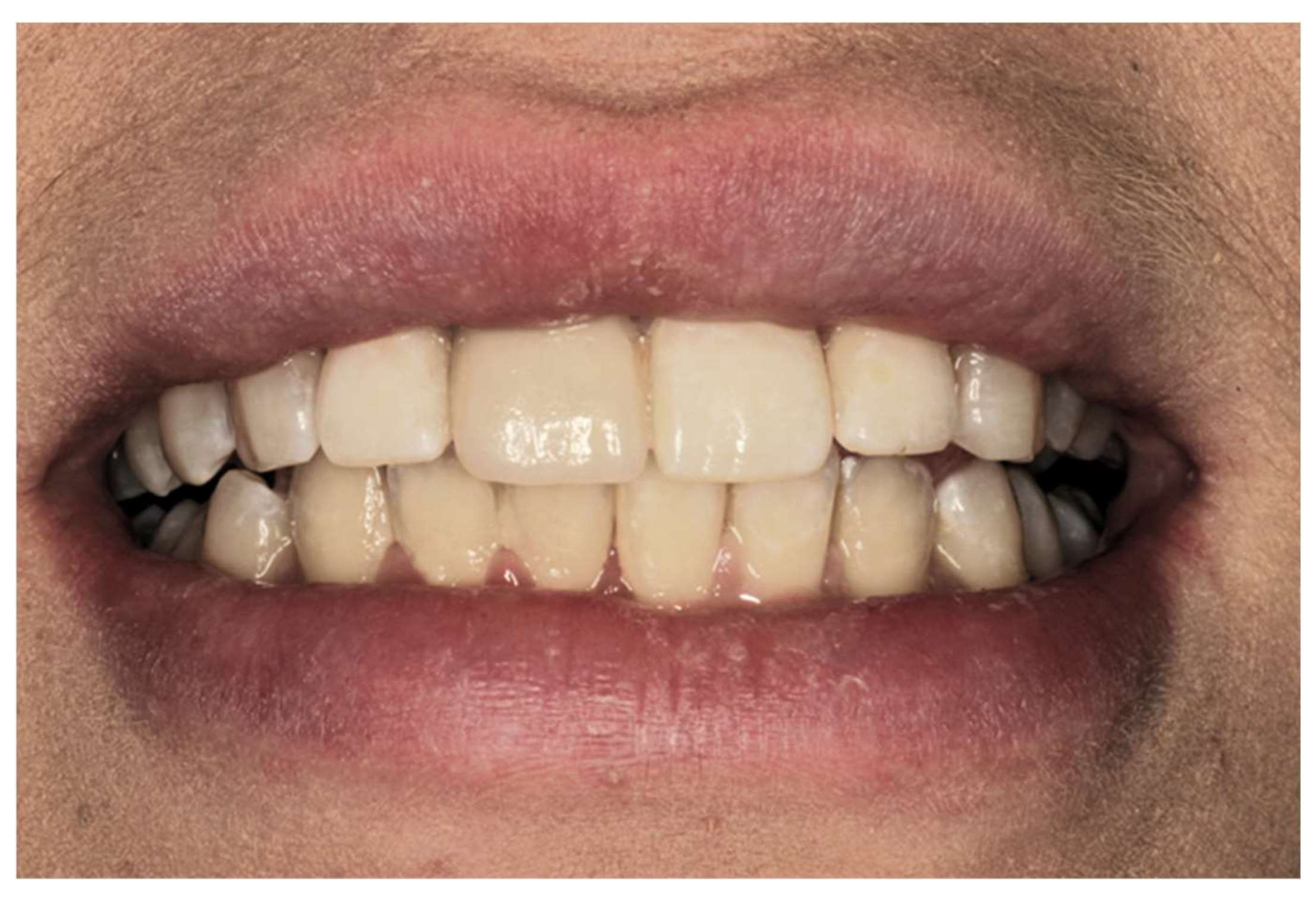
2. Clinical Case
3. Discussion
4. Conclusions
- Ceramic veneers provide a reliable and conservative alternative for the aesthetic restoration of endodontically treated teeth that have undergone discoloration.
- For better aesthetic results, in cases of intrinsic discoloration, an internal tooth whitening procedure may precede.
- Considering bonding and cementation, adhesively cemented high translucency monolithic zirconia seems to be a suitable option for veneers.
Author Contributions
Funding
Institutional Review Board Statement
Conflicts of Interest
References
- Fradeani, M.; Redemagni, M.; Corrado, M. Porcelain laminate veneers: 6-12year clinical evaluation-a retrospective study. Int J Periodontics Restorative Dent 2005, 25(1), 9–17. [Google Scholar] [PubMed]
- Calamia, JR. Etched porcelain veneers: the current state of the art. Quintessence Int 1985, 16(1), 5–12. [Google Scholar] [PubMed]
- Galiatsatos, A.; Bergou, D. Five-year clinical performance pf porcelain laminate veneers. Quintessence Int 2002, 33, 185–189. [Google Scholar]
- Dumfahrt, H.; Schaffer, H. Porcelain laminate veneers. A retrospective evaluation after 1 to 10 years of service: part II-clinical results. Int J Prosthodont 2000, 13(1),9-18.
- Friedman, M. A 15-year review of porcelain veneer failure – A clinician’s observations. Compend Contn Educ Dent 1998, 19, 625–628. [Google Scholar]
- Edward, J.; Swift, Jr.; Mark, J.; Friedman. Critical appraisal porcelain veneer outcomes, part I. J Esthet Restor Dent 2006, 18(1),54-157.
- Maciej Zarow, Louis Hardan, Katarzyna Szczeklik. Porcelain veneers in vital vs non-vital teeth: a retrospective clinical evaluation. Bioengineering (Basel)2023,10(2),168-175.
- Amrani Alaoui, Y.; Hicham, S.; Amal, EY. Veneers on Devitalized Teeth: The Role of Adhesive Dentistry in Aesthetic and Functional Therapies. Integr J Med Sci 2024, 11, 1–5. [Google Scholar] [CrossRef]
- Freire, A.; Regina Archegas, L. Porcelain Laminate Veneer on a Highly Discoloured Tooth: A Case Report. J Can Dent Assoc 2010, 76, 305. [Google Scholar]
- Chen, J.; Shi, C.; Wang, M.; Zhao, S.; Wang, H. Clinical Evaluation of 546 Tetracycline-Stained Teeth Treated with Porcelain Laminate Veneers. J Dent 2005, 33, 3–8. [Google Scholar] [CrossRef] [PubMed]
- Kelleher, M.G.D.; Roe, F.J.C. The safety-in-use of 10% carbamide peroxide (Opalescence) for bleaching teeth under the supervision of a dentist. Br Dent J 1999, 187, 190–194. [Google Scholar] [CrossRef] [PubMed]
- Davis, L.G.; Ashworth, P.D.; Spriggs, L.S. Psychological effects of aesthetic dental treatment. J Dent 1998, 26, 547–554. [Google Scholar] [CrossRef] [PubMed]
- Watts, A. ; Addy M: Tooth discoloration and staining: a review of the literature. Br Dent J 2001, 190, 309–316. [Google Scholar] [CrossRef] [PubMed]
- van der Burgdt, T.P.; Plasschaert, A.J.M. Bleaching of Tooth Discoloration caused by endodontic sealers. J Endod 1986, 12, 231–234. [Google Scholar] [CrossRef] [PubMed]
- Leendert, B.; Jordan, RE. ; Skinner DH: A conservative bleaching treatment for the non-vital discolored tooth. Compendium of Continuing Education in Dentistry 1984, 5, 471–5. [Google Scholar]
- Dahl, JE. Tooth bleaching-A critical review of the biological aspects. Crit Rev Oral Biol Med 2003, 14, 292–304. [Google Scholar] [CrossRef] [PubMed]
- Attin, T.; Paqué, F.; Ajam, F.; Lennon, AM. Review of the current status of tooth whitening with the walking bleach technique. Int Endod J 2003, 36, 313–329. [Google Scholar] [CrossRef] [PubMed]
- Poyser, N.J.; Kelleher, M.G.D.; Briggs, P.F.A. Managing discoloured non-vital teeth: The inside/outside bleaching technique. Dent Update 2004, 31, 204–214. [Google Scholar] [CrossRef] [PubMed]
- Harlan, AW. The removal of stains from teeth caused by administration of medical agents and the bleaching of a pulpless tooth. Am J Dent Sci 1884/1885, 18:521.
- Cotton, FA.; Wilkinson, G. Oxygen. In: Advances in inorganic chemistry. A comprehensive text. Cotton FA, Wilkinson G, editors. Interscience Publisher. New York, 1972; p.403-420.
- Gregus, Z.; Klaassen CD: Mechanisms of toxicity. In: Cassarett and Doull’s toxicology, the basic science of poisons. Klaassen CD, editor. McGraw-Hill Companies Inc. New York: 1995; p.35-74.
- Soares, PV.; Spini, PH.; Carvalho, VF.; Souza, PG.; Gonzaga, RC.; Tolentino, AB.; Machado, AC. Esthetic rehabilitation with laminated ceramic veneers reinforced by lithium disilicate. Quintessence Int 2014, 45(2), 129–133. [Google Scholar] [PubMed]
- Conrad, HJ.; Seong, WJ.; Pesun, IJ. Current ceramic materials and systems with clinical recommendations: A systematic review. J Prosthet Dent 2007, 98(5), 389–404. [Google Scholar] [CrossRef] [PubMed]
- Trinkner, TF.; Roberts, M. Fluorapatite-leucite glass ceramic veneers for aesthetic anterior restorations. Pract Proced Aesthet Dent 2001, 13(1), 37–41. [Google Scholar] [PubMed]
- Manicone, PF.; Lammetti, RP.; Raffaelli, L. An overview of zirconia ceramics: Basic properties and clinical applications. J Dent 2007, 35(11), 819–26. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y. Making yttria-stabilized tetragonal zirconia. Dent Mater 2014, 30(10), 1195–203. [Google Scholar] [CrossRef] [PubMed]
- Harada, K.; Raigrodski, AJ.; Chung, KH.; Flinn, BD.; Dogan, S.; Mancl, LA. A comparative evaluation of the translucency of zirconia and lithium disilicate for monolithic restorations. J Prosthet Dent 2016, 116, 257–63. [Google Scholar] [CrossRef] [PubMed]
- Kolakarnprasert, N.; Kaizer, M.R.; Kim, D.K.; Zhang, Y. New multi-layered zirconia: Composition, microstructure and translucency. Dent Mater 2019, 35, 797–806. [Google Scholar] [CrossRef] [PubMed]
- Alrabeah, G.; Al-Sowygh, A.H.; Almarshedy, S. Use of Ultra-Translucent Monolithic Zirconia as Esthetic Dental Restorative Material: A Narrative Review. Ceramics 2024, 7, 264–275. [Google Scholar] [CrossRef]
- Toma, F.R.; Porojan, S.D.; Vasiliu, R.D.; Porojan, L. The effect of polishing, glazing, and aging on optical characteristics of multi-layered dental zirconia with different degrees of translucency. J Funct Biomater 2023, 14, 68. [Google Scholar] [CrossRef] [PubMed]
- Kongkiatkamon, S.; Rokaya, D.; Kengtanyakich, S.; Peampring, C. Current classification of zirconia in dentistry: An updated review. Peer J 2023, 11, e15669. [Google Scholar] [CrossRef] [PubMed]
- Kolakarnprasert, N.; Kaizer, M.R.; Kim, D.K.; Zhang, Y. New multi-layered zirconia: Composition, microstructure and translucency. Dent Mater 2019, 35, 797–806. [Google Scholar] [CrossRef] [PubMed]
- Matsuzaki, F.; Sekine, H.; Honma, S.; Takanashi, T.; Furuya, K.; Yajima, Y.; Yoshinari, M. Translucency and flexural strength of monolithic translucent zirconia and porcelain-layered zirconia. Dent Mater J 2015, 34(6), 910–7. [Google Scholar] [CrossRef] [PubMed]
- Koizumi, H.; Nakayama, D.; Komine, F.; Blatz, MB.; Matsumura, H. Bonding of resin-based luting cements to zirconia with and without the use of ceramic priming agents. J Adhes Dent 2012,14:385-92.
- Inokoshi, M.; De Munck, J.; Minakuchi, S.; Van Meerbeek, B. Meta-analysis of bonding effectiveness to zirconia ceramics. J Dent Res 2014, 93, 329–34. [Google Scholar] [CrossRef] [PubMed]
- Özcan, M.; Bernasconi, M. Adhesion to zirconia used for dental restorations: A systematic review and meta-analysis. J Adhes Dent 2015, 17, 7–26. [Google Scholar] [PubMed]
- Kern, M.; Thompson, VP. Sandblasting and silica coating of a glass-infiltrated alumina ceramic: Volume loss, morphology, and changes in the surface composition. J Prosthet Dent 1994, 71, 453–61. [Google Scholar] [CrossRef] [PubMed]
- Blatz, M.B.; Conejo, J. cementation and bonding of zirconia restorations. Compend Contin Educ Dent 2018, 39 (Suppl. S4), 9–13. [Google Scholar] [PubMed]
- Silva, N.R.; Araújo, G.D.; Moura, D.M.; Araújo, L.D.; Gurgel, B.D.; Melo, R.M.; Bottino, M.A.; Özcan, M.; Zhang, Y.; Souza, R.O. Clinical Performance of Minimally Invasive Monolithic Ultratranslucent Zirconia Veneers: A Case Series up to Five Years of Follow-up. Oper Dent 2023, 48, 606–617. [Google Scholar] [CrossRef] [PubMed]
- Dikicier, S.; Korkmaz, C.; Atay, A. Surface roughness and characteristics of CAD/CAM zirconia and glass ceramics after combined treatment procedures. BMC Oral Health 2022, 22, 524. [Google Scholar] [CrossRef] [PubMed]
- Shetty, R.; Pinge, SS.; Shetty, S.; Banga, P.; Zahid, M. Zirconia monolithic veneers: A durable and cosmetic alternative to regular veneers; Adv Hum Biol 2022, 12,22-5.
- Papia, E.; Larsson, C.; du Toit, M.; Vult von Steyern, P. Bonding between oxide ceramics and adhesive cement systems: A systematic review. J Biomed Mater Res B Appl Biomater 2014, 102, 395-413. [Google Scholar] [CrossRef] [PubMed]



Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).




