Submitted:
25 June 2024
Posted:
26 June 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
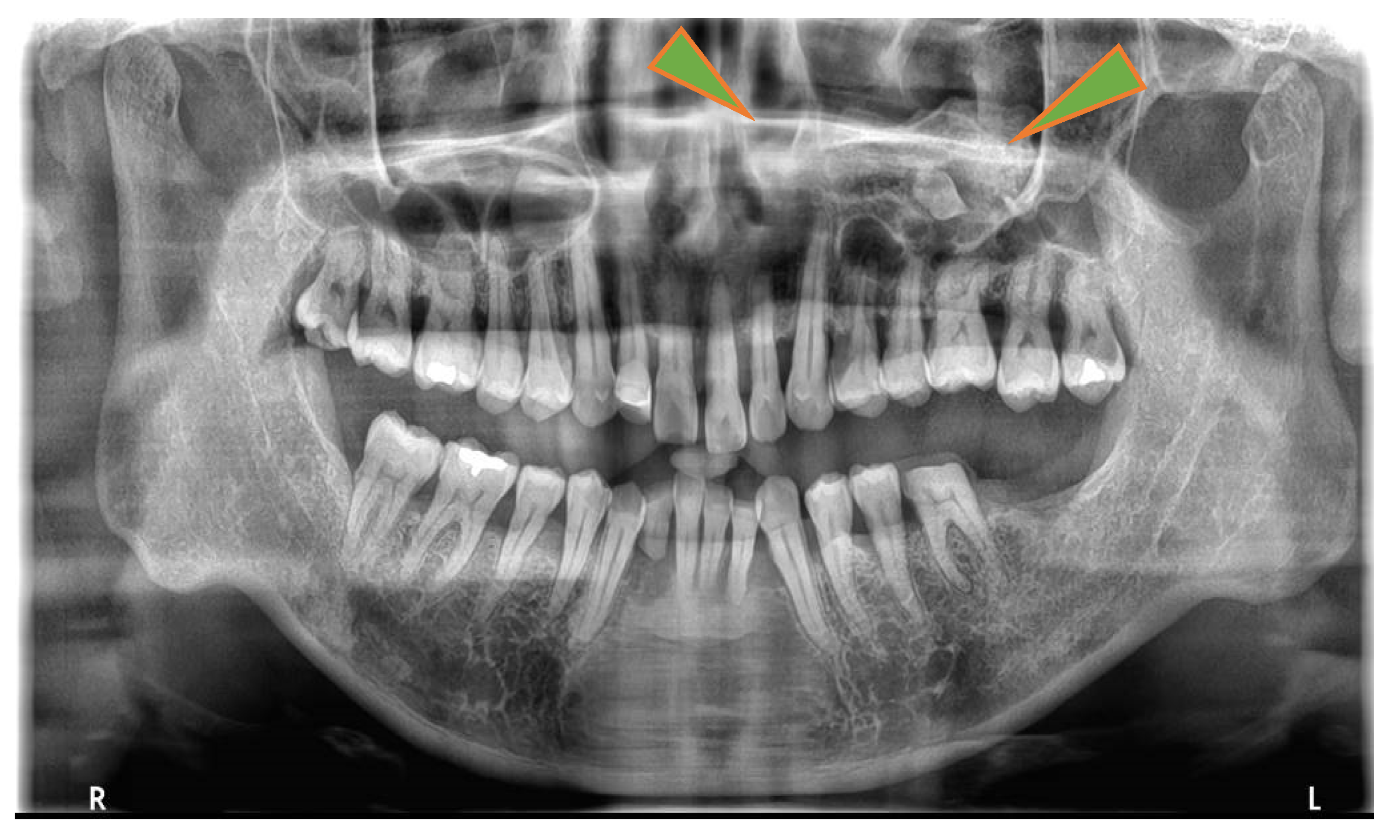
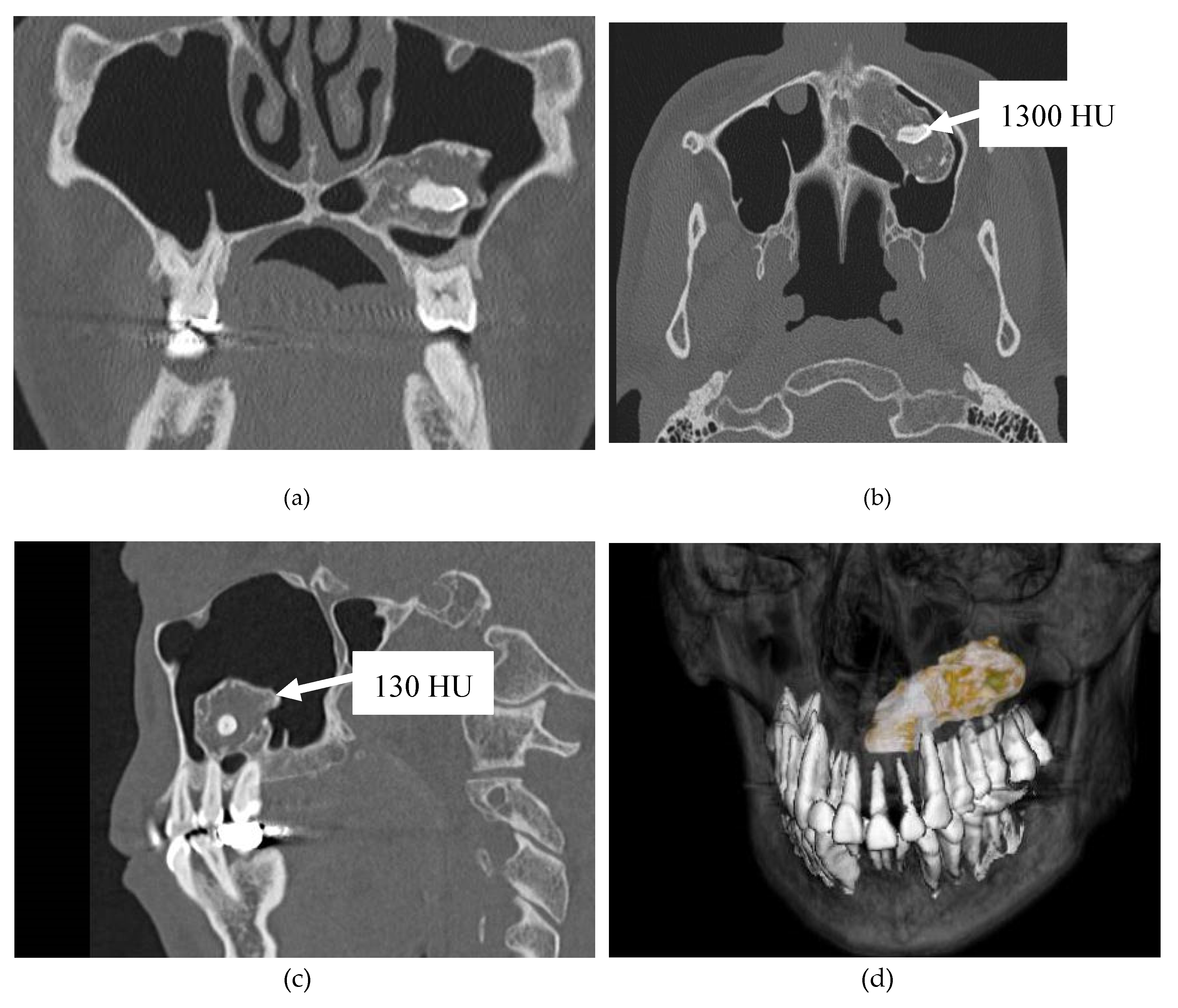
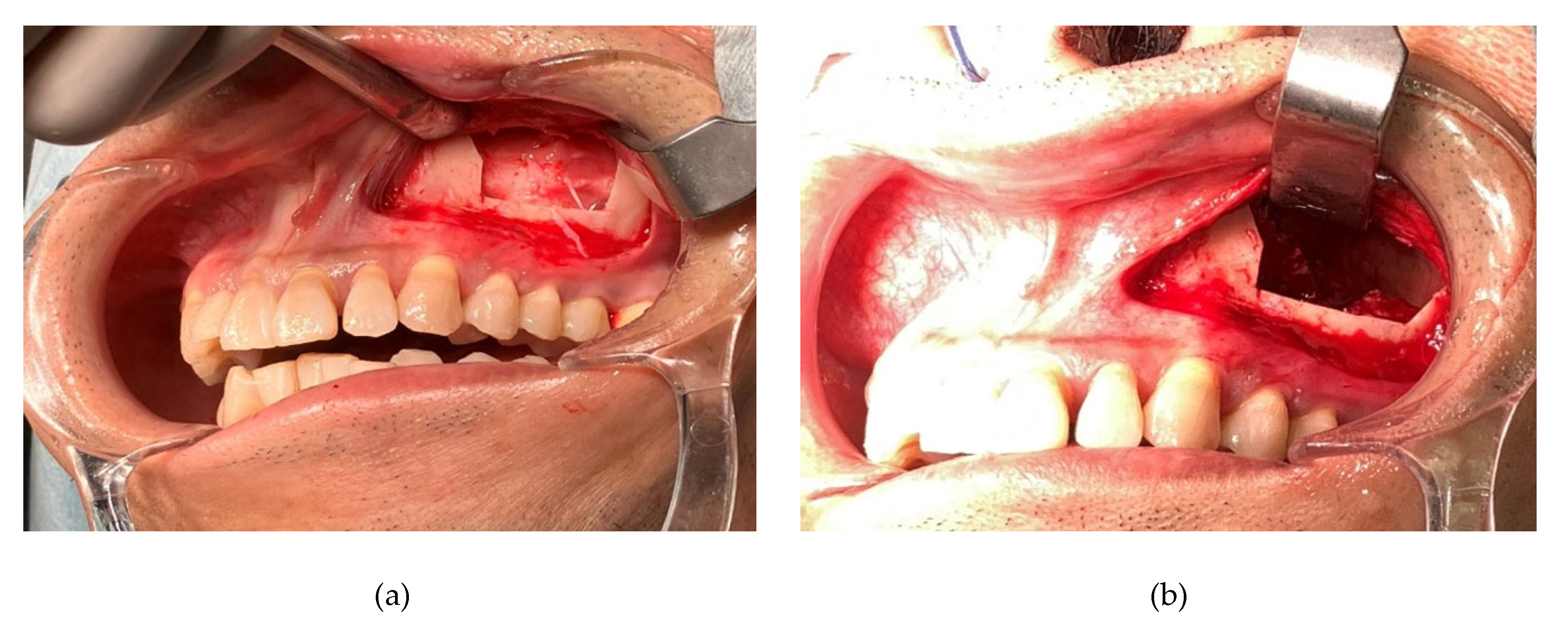
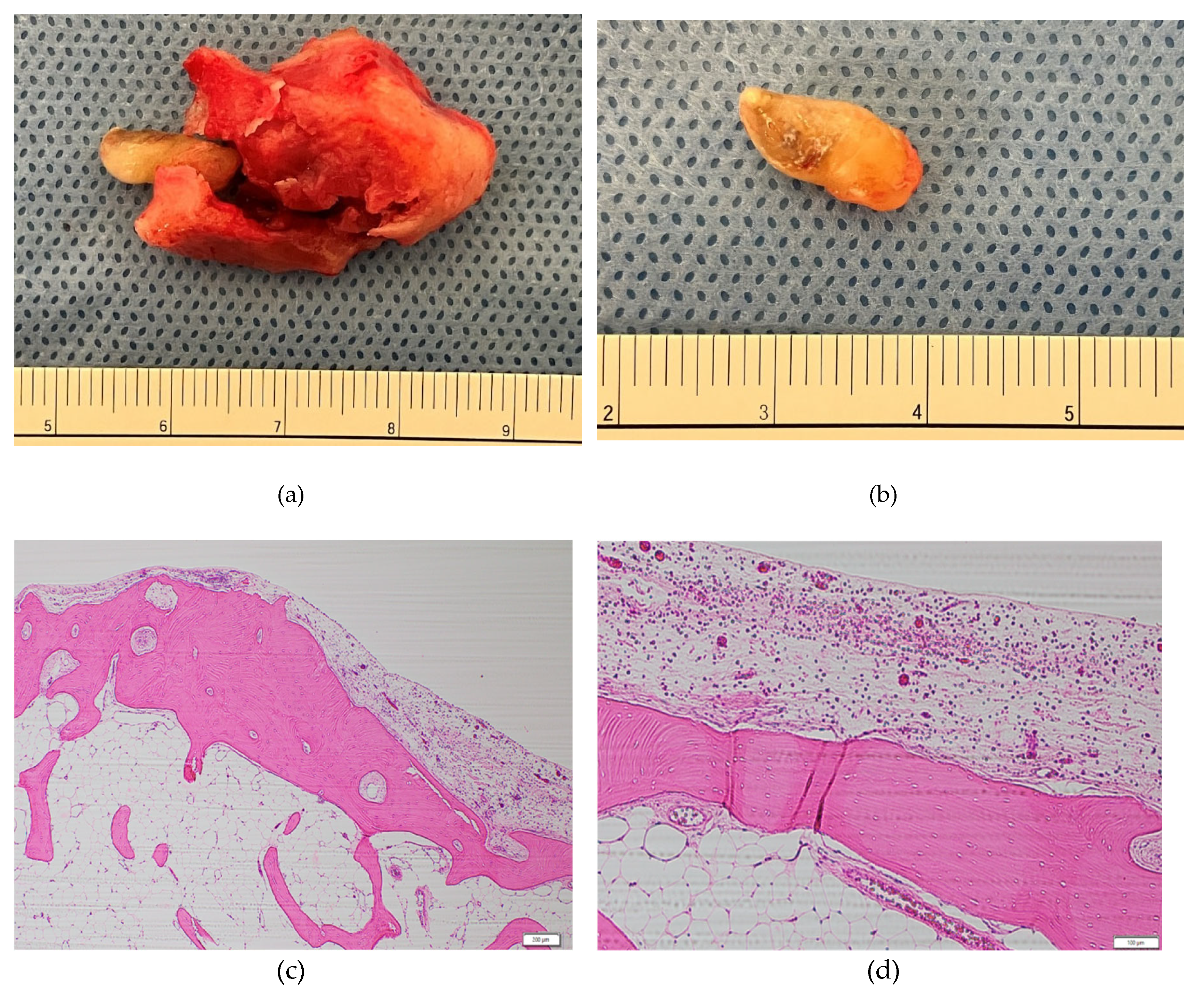
3. Case Presentation
3. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lombroni, L.G.; Farronato, G.; Santamaria, G.; Lombroni, D.M.; Gatti, P.; Capelli, M. Ectopic teeth in the maxillary sinus: A case report and literature review. Indian J Dent Res 2018, 29, 667–671. [Google Scholar] [PubMed]
- Magboul, N.A.; Al-Ahmari, M.S.; Alzahrani, M.A.; Dlboh, S.S. Fibro-osseous lesion of the nose and paranasal sinus: A retrospective study with literature review. Cureus 2022, 14, e27229. [Google Scholar] [CrossRef] [PubMed]
- Baykul, T.; Doğru, H.; Yasan, H.; Cina Aksoy, M. Clinical impact of fibro sinus. Auris Nasus Larynx 2006, 33, 277–281, (Epub 3 May 2006). [Google Scholar] [CrossRef] [PubMed]
- Buyuklu, F.; Akdogan, M.V.; Ozer, C.; Cakmak, O. Growth characteristics and clinical manifestations of the paranasal sinus osteomas. Otolaryngol Head Neck Surg 2011, 145, 319–323. [Google Scholar] [CrossRef] [PubMed]
- Sayan, N.B.; Uçok, C.; Karasu, H.A.; Günhan, O. Peripheral osteoma of the oral and maxillofacial region: a study of 35 new cases. J Oral Maxillofac Surg 2002, 60, 1299–1301. [Google Scholar] [CrossRef] [PubMed]
- Larrea-Oyarbide, N.; Valmaseda-Castellón, E.; Berini-Aytés, L.; Gay-Escoda, C. Osteomas of the craniofacial region. Review of 106 cases. J Oral Pathol Med 2008, 37, 38–42. [Google Scholar] [CrossRef] [PubMed]
- Johann, A.C.; de Freitas, J.B.; de Aguiar, M.C.; de Araújo, N.S.; Mesquita, R.A. Peripheral osteoma of the mandible: case report and review of the literature. J Craniomaxillofac Surg 2005, 33, 276–281. [Google Scholar] [CrossRef] [PubMed]
- Park, W.; Kim, H.S. Osteoma of maxillary sinus: A case report. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2006, 102, e26–e27. [Google Scholar] [CrossRef] [PubMed]
- Çelenk, F.; Baysal, E.; Karata, Z.A.; Durucu, C.; Mumbuç, S.; Kanlıkama, M. Paranasal sinus osteomas. J Craniofac Surg 2012, 23, e433–e437. [Google Scholar] [CrossRef] [PubMed]
- Borumandi, F.; Lukas, H.; Yousefi, B.; Gaggl, A. Maxillary sinus osteoma: from incidental finding to surgical management. J Oral Maxillofac Pathol 2013, 17, 318. [Google Scholar] [CrossRef] [PubMed]
- Koivunen, P.; Löppönen, H.; Fors, A.P.; Jokinen, K. The growth rate of osteomas of the paranasal sinuses. Clin Otolaryngol Allied Sci 1997, 22, 111–114. [Google Scholar] [CrossRef] [PubMed]
- Oner, A.Y.; Pocan, S. Gardner’s syndrome: a case report. Br Dent J 2006, 200, 666–667. [Google Scholar] [CrossRef] [PubMed]
- Osma, U.; Yaldiz, M.; Tekin, M.; Topcu, I. Giant ethmoid osteoma with orbital extension presenting with epiphora. Rhinology 2003, 41, 122–124. [Google Scholar]
- Lee, J.J.; Ryu, G.; Lee, K.E.; Hong, S.D.; Jung, Y.G.; Kim, H.Y.; Dhong, H.J.; Chung, S.K. Long-term clinical course of benign fibro-osseous lesions in the paranasal sinuses. Clin Exp Otorhinolaryngol 2021, 14, 374–381. [Google Scholar] [CrossRef] [PubMed]
- Moreano, E.H.; Zich, D.K.; Goree, J.C.; Graham, S.M. Nasal tooth. Am J Otolaryngol 1998, 19, 124–126. [Google Scholar] [CrossRef] [PubMed]
- Abdollahifakhim, S.; Mousaviagdas, M. Ectopic molar with maxillary sinus drainage obstruction and oroantral fistula. Iran J Otorhinolaryngol 2013, 25, 187–192. [Google Scholar] [PubMed]
- Arora, P.; Nair, M.K.; Liang, H.; Patel, P.B.; Wright, J.M.; Tahmasbi-Arashlow, M. Ectopic teeth with disparate migration: A literature review and new case series. Imaging Sci Dent 2023, 53, 229–238. [Google Scholar] [CrossRef] [PubMed]
- Srinivasa Prasad, T.; Sujatha, G.; Niazi, T.M.; Rajesh, P. Dentigerous cyst associated with an ectopic third molar in the maxillary sinus: a rare entity. Indian J Dent Res 2007, 18, 141–143. [Google Scholar] [CrossRef] [PubMed]
- Alfuriji, S.; Alamro, H.; Kentab, J.; Alosail, L.; Alali, L.; Altuwaijri, N.; Alalwan, R. Ectopic permanent molars: a review. Dent J (Basel) 2023, 11, 206. [Google Scholar] [CrossRef] [PubMed]
- Dalben, G.d.S.; das Neves, L.T.; Gomide, M.R. Oral findings in patients with Apert syndrome. J Appl Oral Sci 2006, 14, 465–469. [Google Scholar] [CrossRef] [PubMed]
- Helm, A.; Martín-Vacas, A.; Molinero-Mourelle, P.; Caleya, A.M.; Gallardo, N.E.; Mourelle-Martínez, M.R. Ectopic eruption of maxillary first permanent molars: preliminary results of prevalence and dentoskeletal characteristics in Spanish paediatric population. Children (Basel) 2021, 8, 479. [Google Scholar] [CrossRef] [PubMed]
- Lamb, J.F.; Husein, O.F.; Spiess, A.C. Ectopic molar in the maxillary sinus precipitating a mucocele: a case report and literature review. Ear Nose Throat J 2009, 88, E6–E11. [Google Scholar] [PubMed]
- Mucedero, M.; Rozzi, M.; Cardoni, G.; Ricchiuti, M.R.; Cozza, P. Dentoskeletal features in individuals with ectopic eruption of the permanent maxillary first molar. Korean J Orthod 2015, 45, 190–197. [Google Scholar] [CrossRef] [PubMed]
- Erkmen, N.; Olmez, S.; Onerci, M. Supernumerary tooth in the maxillary sinus: case report. Aust Dent J 1998, 43, 385–386. [Google Scholar] [CrossRef] [PubMed]
- Kayabasoglu, G. 2 Murat Karaman, 1 Recep Kaymaz, 1 Alpen Nacar. A rare entity causing chronic sinusitis: ectopic tooth in maxillary sinus. Eur J Gen Med 2015, 12, 86–89. [Google Scholar]
- Lai, Y.T.; Luk, Y.S.; Fung, K.H. Anomalous morphology of an ectopic tooth in the maxillary sinus on three-dimensional computed tomography images. J Radiol Case Rep 2013, 7, 11–16. [Google Scholar] [CrossRef] [PubMed]
- Aydın, Ü.; Aşık, B.; Ahmedov, A.; Durmaz, A. Osteoma and ectopic tooth of the left maxillary sinus: A unique coexistence. Balkan Med J 2016, 33, 473–476. [Google Scholar] [CrossRef] [PubMed]
- Aldren, C.P.; Soames, J.V.; Birchall, J.P. Bony remodelling in an osteoma of the paranasal sinuses. J Laryngol Otol 1993, 107, 633–635. [Google Scholar] [CrossRef] [PubMed]
- Viterbo, S.; Griffa, A.; Boffano, P. Endoscopic removal of an ectopic tooth in maxillary sinus. J Craniofac Surg 2013, 24, e46–e48. [Google Scholar] [CrossRef] [PubMed]
- Litvin, M.; Caprice, D.; Infranco, L. Dentigerous cyst of the maxilla with impacted tooth displaced into orbital rim and floor. Ear Nose Throat J 2008, 87, 160–162. [Google Scholar] [CrossRef] [PubMed]
- Masalha, M.; Schneider, S.; Kassem, F.; Koren, I.; Eliashar, R.; Margulis, A.; Landsberg, R. Endoscopic treatment of ectopic teeth in the maxillary sinus. J Clin Exp Dent 2021, 13, e227–e233. [Google Scholar] [CrossRef] [PubMed]
- Chiapasco, M.; Felisati, G.; Zaniboni, M.; Pipolo, C.; Borloni, R.; Lozza, P. The treatment of sinusitis following maxillary sinus grafting with the association of functional endoscopic sinus surgery (FESS) and an intra-oral approach. Clin Oral Implants Res 2013, 24, 623–629. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).




