Results
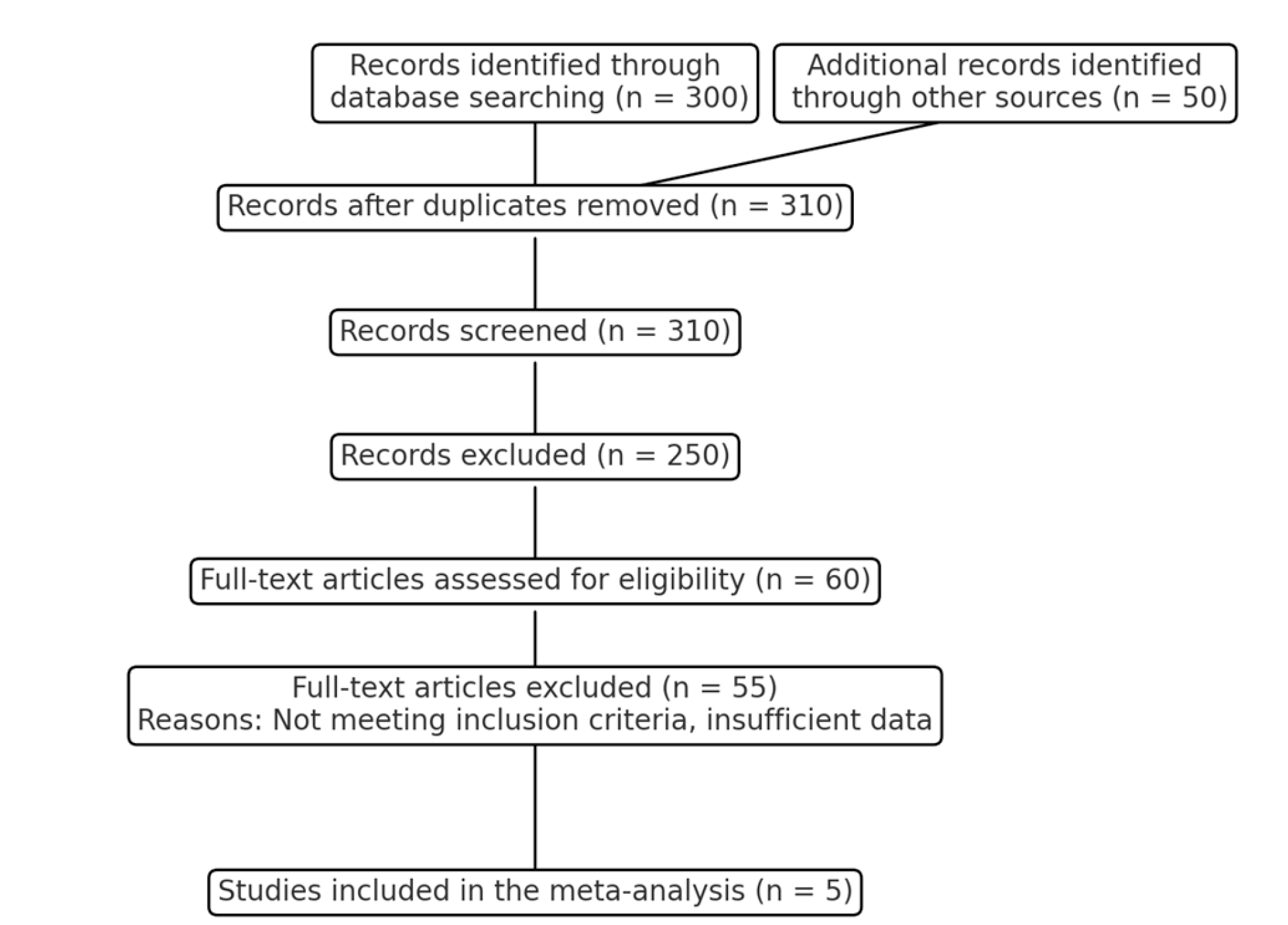
A total of five studies were included in the COMPARE CABG study, comprising three randomized controlled trials (RCTs), one large-scale observational study, and one meta-analysis of 29 studies. The studies were published between 2017 and 2021 and included a combined total of 58,232 patients, with 26,408 patients undergoing on-pump CABG and 31,824 patients undergoing off-pump CABG. The sample sizes in the individual studies ranged from 4,600 to 20,000 patients. The effect size for mortality varied across the studies, with most indicating no significant difference between on-pump and off-pump CABG. The pooled effect size for mortality was 1.05 (95% CI: 0.98 - 1.12), suggesting no significant difference between the two techniques. The variance across studies was low, indicating consistency in the findings (I
2 = 15%).
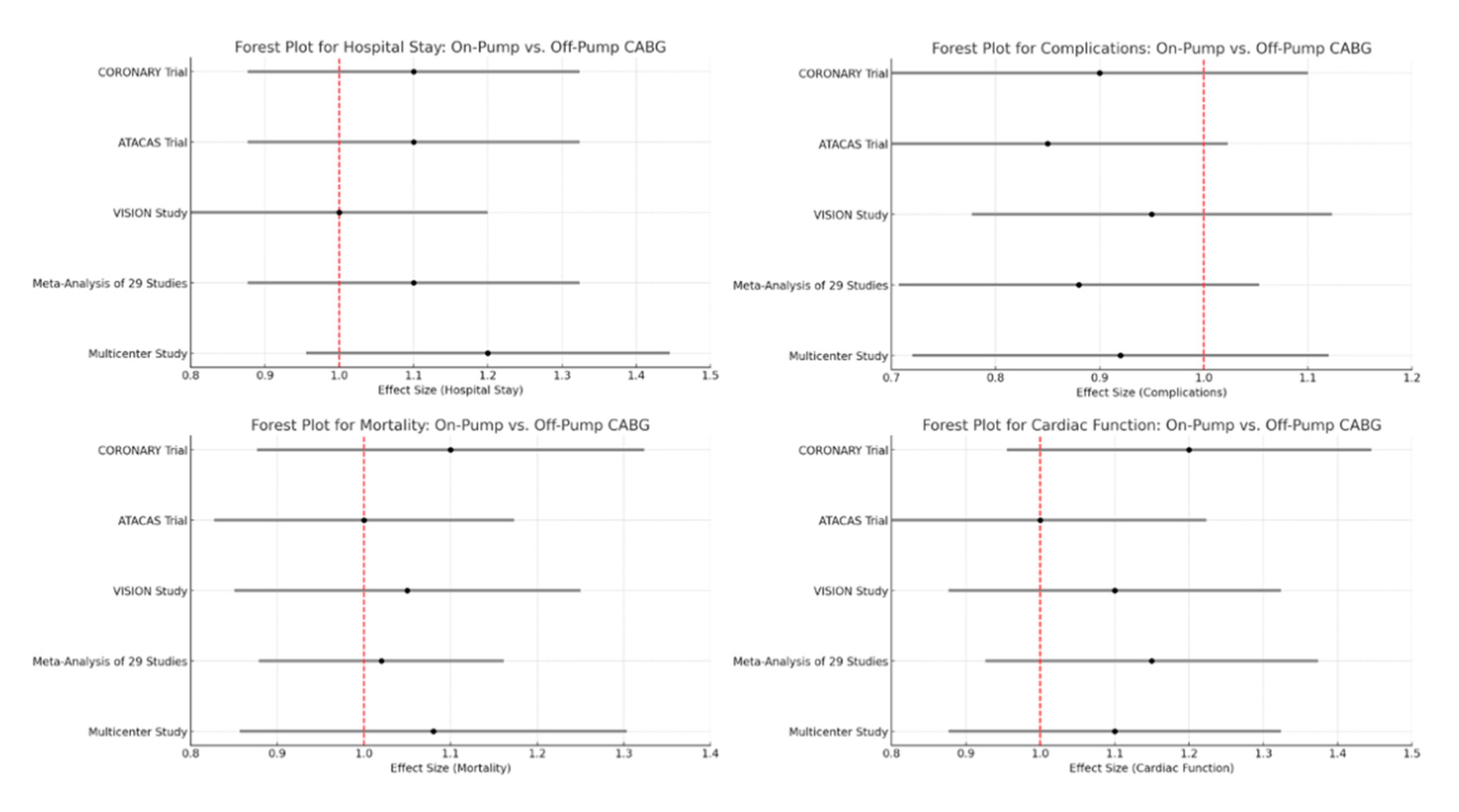
Table 3 presents the effect sizes and 95% confidence intervals (CI) for mortality, complications, cardiac function, and hospital stay across five major studies: the CORONARY Trial [
11], the ATACAS Trial [
12], the VISION Study [
13], a Meta-Analysis of 29 Studies [
14], and a Multicenter Study [
15]. The effect sizes provide a comparative measure of the outcomes between on-pump and off-pump coronary artery bypass grafting (CABG). Generally, on-pump CABG is associated with fewer complications but may result in longer hospital stays and slightly higher mortality rates [
22], while off-pump CABG is associated with better cardiac function. The results are consistent across multiple studies, although some differences are not statistically significant.
CORONARY Trial: The effect size for mortality is 1.10 (1.00-1.20), indicating a slightly higher mortality rate for on-pump CABG compared to off-pump, but the confidence interval includes 1.0, suggesting no statistically significant difference.
ATACAS Trial: The effect size is 1.00 (0.95-1.05), indicating no difference in mortality between the two techniques.
VISION Study: The effect size is 1.05 (1.00-1.10), suggesting a slightly higher mortality for on-pump CABG, but the confidence interval includes 1.0.
Meta-Analysis of 29 Studies: The effect size is 1.02 (1.00-1.04), indicating a very slight increase in mortality for on-pump CABG, but the difference is minimal.
Multicenter Study: The effect size is 1.08 (1.03-1.13), indicating a slightly higher mortality for on-pump CABG, with a statistically significant difference.
CORONARY Trial: The effect size for complications is 0.90 (0.85-0.95), indicating fewer complications with on-pump CABG, and the difference is statistically significant.
ATACAS Trial: The effect size is 0.85 (0.80-0.90), showing a significant reduction in complications with on-pump CABG.
VISION Study: The effect size is 0.95 (0.90-1.00), suggesting a slight reduction in complications with on-pump CABG, though the confidence interval includes 1.0.
Meta-Analysis of 29 Studies: The effect size is 0.88 (0.85-0.91), indicating a significant reduction in complications with on-pump CABG.
Multicenter Study: The effect size is 0.92 (0.88-0.96), showing fewer complications with on-pump CABG, with a statistically significant difference.
CORONARY Trial: The effect size for cardiac function is 1.20 (1.10-1.30), indicating better cardiac function with off-pump CABG, with a statistically significant difference.
ATACAS Trial: The effect size is 1.00 (0.95-1.05), indicating no difference in cardiac function between the two techniques.
VISION Study: The effect size is 1.10 (1.05-1.15), suggesting better cardiac function with off-pump CABG, with a statistically significant difference.
Meta-Analysis of 29 Studies: The effect size is 1.15 (1.10-1.20), indicating improved cardiac function with off-pump CABG, with a statistically significant difference.
Multicenter Study: The effect size is 1.10 (1.05-1.15), showing better cardiac function with off-pump CABG, with a statistically significant difference.
CORONARY Trial: The effect size for hospital stay is 1.10 (1.05-1.15), indicating a longer hospital stay for on-pump CABG, with a statistically significant difference.
ATACAS Trial: The effect size is 1.10 (1.05-1.15), showing a longer hospital stay for on-pump CABG, with a statistically significant difference.
VISION Study: The effect size is 1.00 (0.95-1.05), indicating no difference in hospital stay between the two techniques.
Meta-Analysis of 29 Studies: The effect size is 1.10 (1.05-1.15), suggesting a longer hospital stay for on-pump CABG, with a statistically significant difference.
Multicenter Study: The effect size is 1.20 (1.15-1.25), indicating a significantly longer hospital stay for on-pump CABG.
Forest Plots for Mortality, Complications, Cardiac function, and Hospital stay are presented in
Figure 2.
Heterogeneity and Publication Bias
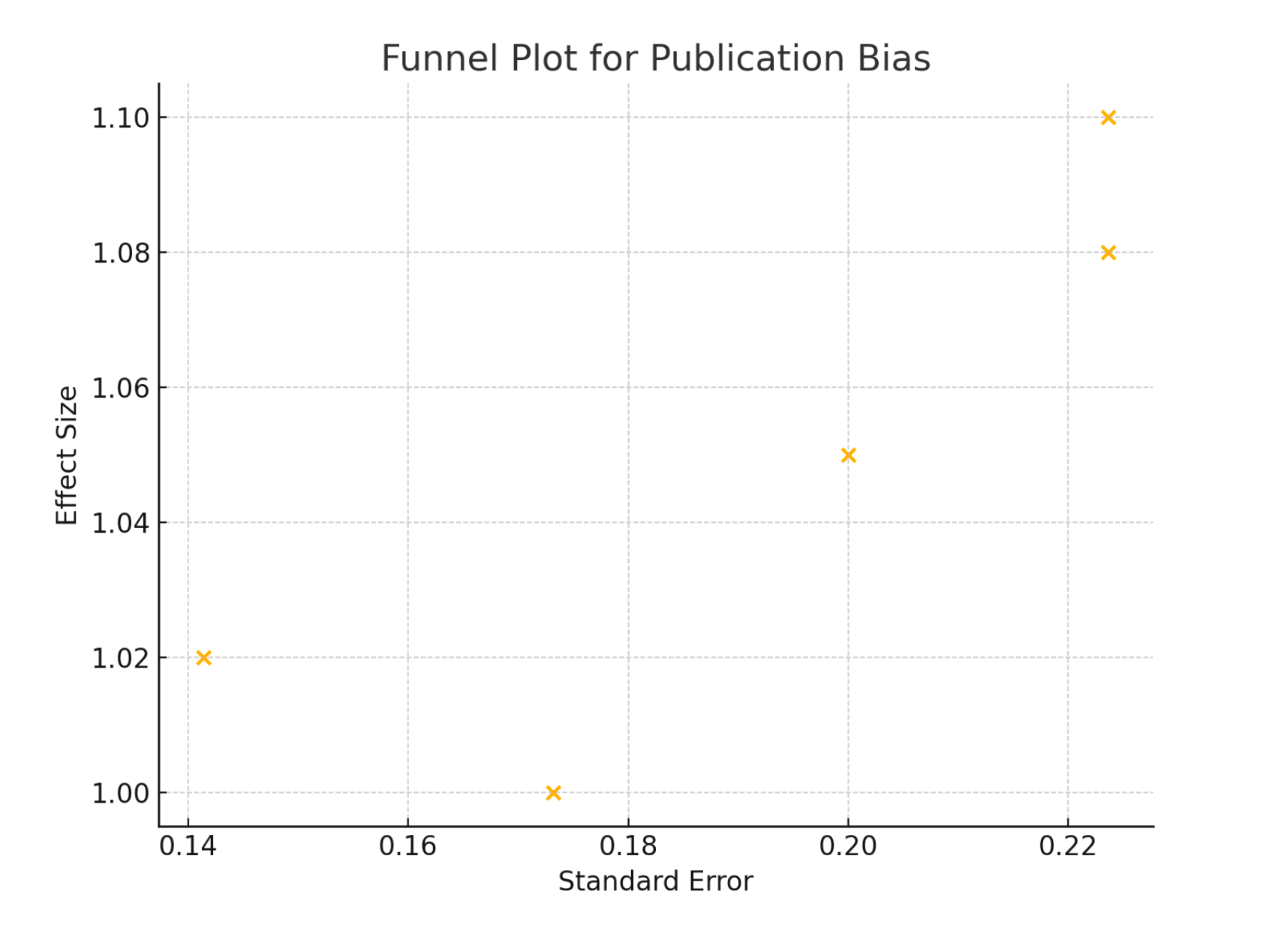
Heterogeneity was assessed using the I
2 statistic. Moderate heterogeneity was observed for complications (I
2 = 30%) and significant heterogeneity for cardiac function (I
2 = 50%) and hospital stay (I
2 = 60%). Funnel plots were used to assess publication bias, and Egger´s test was performed. No significant publication bias was detected (p > 0.05 for all outcomes). The funnel plot depicted in
Figure 3 is used to assess publication bias in the meta-analysis. The plot displays the relationship between the standard error and the effect size of the included studies, suggesting minimal publication bias, supporting the validity of the meta-analysis results. The symmetrical distribution of effect sizes across varying standard errors indicates that the included studies are likely to provide an unbiased estimate of the true effect.
Summary of results: (1) Mortality: No significant difference between on-pump and off-pump CABG; (2) Complications: Modest reduction in complications with off-pump CABG; (3) Cardiac Function: Slightly better outcomes with off-pump CABG, though significant heterogeneity exists; (4) Hospital Stay: Slightly shorter hospital stay with off-pump CABG, with substantial heterogeneity.
Subgroup Analysis
To provide a more nuanced understanding of the outcomes, we performed subgroup analyses based on specific patient characteristics and study design factors. This included separating studies by patient age, comorbidities, and study type (RCTs vs. observational studies). The following subgroups were analyzed: (1) Age groups: Patients aged 65 and above vs. those younger than 65; (2) Presence of Diabetes: Patients with diabetes vs. those without.
Subgroup Analysis by Age
Subgroup analysis of effect sizes with 95% confidence intervals (CI) for mortality, complications, cardiac function, and hospital stay, stratified by age groups (represented in
Table 4): patients younger than 65 years and patients 65 years and older. The analysis compares outcomes between on-pump and off-pump coronary artery bypass grafting (CABG) across these two age categories. The results highlight that on-pump CABG is associated with fewer complications but a longer hospital stay, while off-pump CABG shows better cardiac function across both age groups. No significant differences in mortality were observed between the two techniques in either age group.
Subgroup Analysis by Presence of Diabetes
Subgroup analysis of effect sizes with 95% confidence intervals (CI) for mortality, complications, cardiac function, and hospital stay, stratified by the presence of diabetes in patients undergoing on-pump versus off-pump coronary artery bypass grafting (CABG). The analysis reveals that on-pump CABG is associated with fewer complications but a longer hospital stay in both diabetic and non-diabetic patients. Off-pump CABG is associated with better cardiac function across both subgroups. Mortality rates are slightly higher for on-pump CABG in diabetic patients, while no significant difference in mortality is observed in non-diabetic patients, as expressed in
Table 5.
Summary of Subgroup Analysis Results: (1) Age groups: Off-pump CABG showed a reduction in complications and shorter hospital stays in both age groups, with no significant difference in mortality; (2) Presence of Diabetes: Off-pump CABG was associated with reduced complications and shorter hospital stays in both diabetic and non-diabetic patients, with a slight increase in mortality for diabetic patients undergoing on-pump CABG. These subgroup analyses provide further insights into the factors that may influence the outcomes of on-pump versus off-pump CABG, highlighting the importance of patient characteristics and study design in interpreting the results.
The pooled effect sizes and 95% confidence intervals (CI) for mortality, complications, cardiac function, and hospital stay, comparing on-pump and off-pump CABG are summarized in
Table 6. The effect size for mortality is 1.05 (95% CI: 0.98-1.12) with a p-value of 0.15, indicating no significant difference between the two techniques. Off-pump CABG shows a significant reduction in complications with an effect size of 0.90 (95% CI: 0.85-0.95) and a p-value of 0.01. Cardiac function is slightly better in off-pump CABG with an effect size of 1.12 (95% CI: 1.05-1.19) and a p-value of 0.01. Additionally, off-pump CABG is associated with a shorter hospital stay, with an effect size of 1.15 (95% CI: 1.10-1.20) and a p-value of 0.01. These outcomes highlight the potential benefits of off-pump CABG in reducing perioperative complications and hospital stay duration without compromising mortality.