Submitted:
12 June 2024
Posted:
13 June 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Pharmacology of Aspirin: Joys And Sorrows
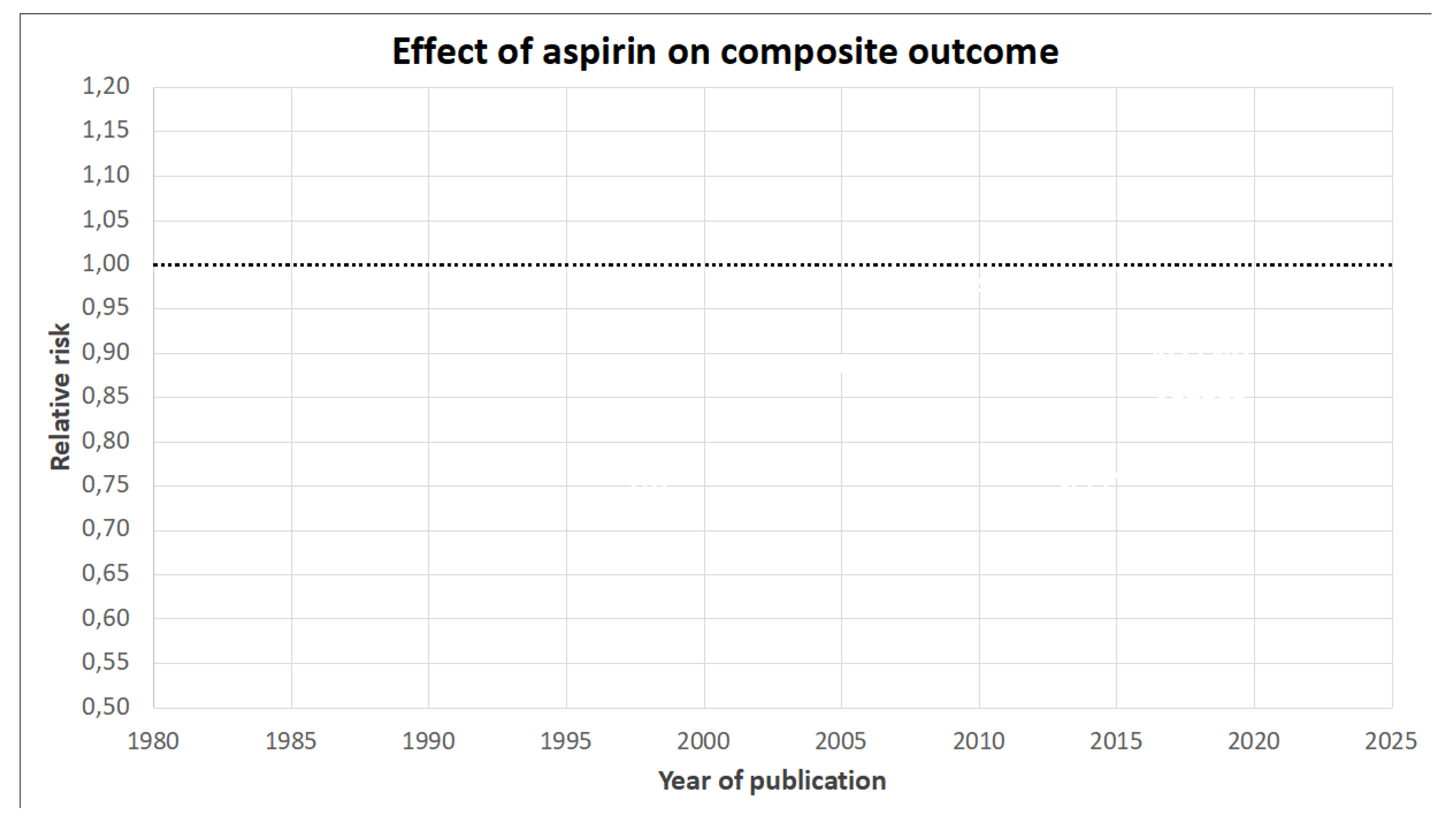
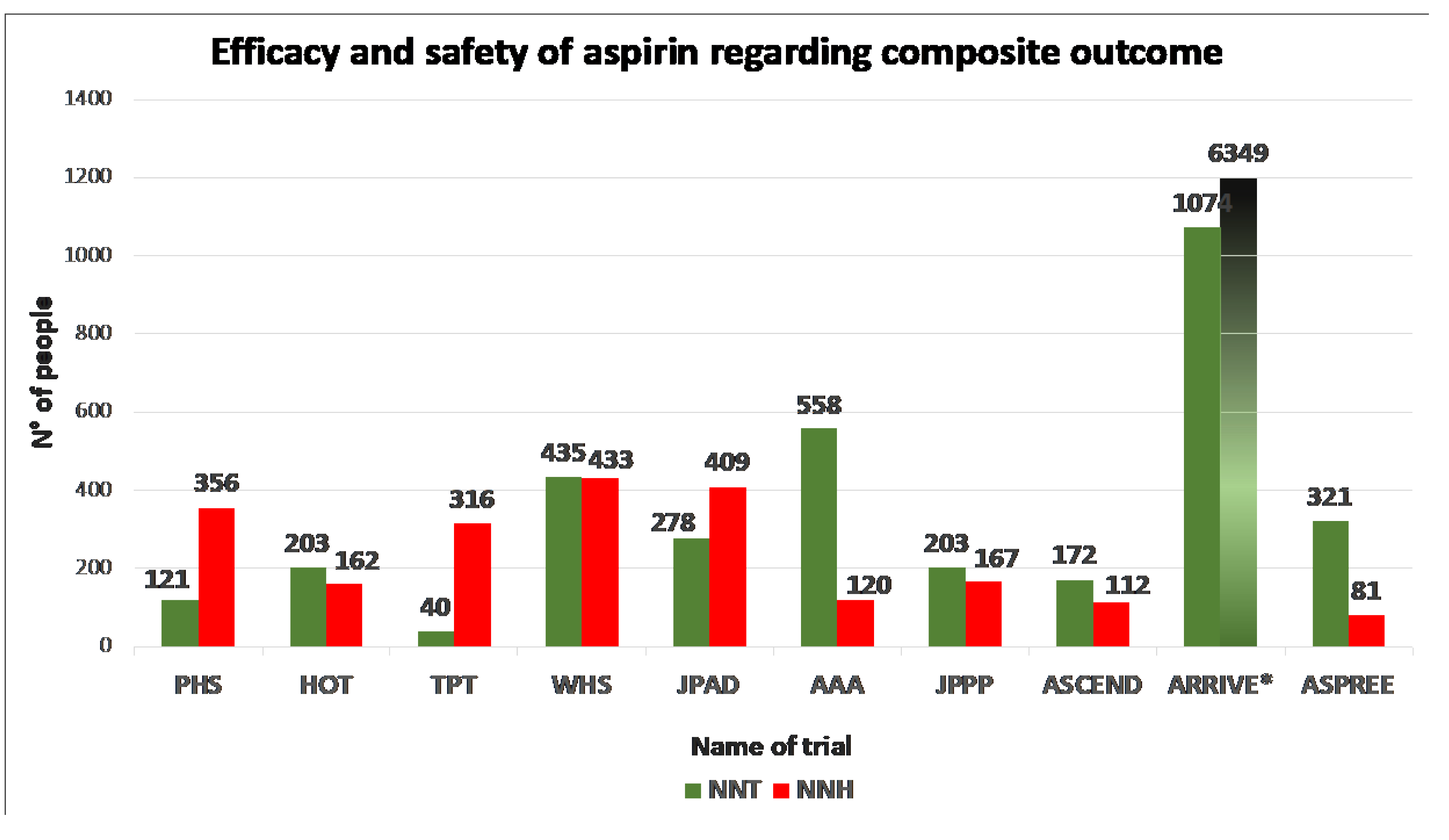
3. Deep Diving in Data: How Effective and Safe is Aspirin?
4. Looking for a Scapegoat: Can Subgroup Effects Account for the Lack of Benefit?
4.1. Diabetics
4.2. Obese
4.3. Women
5. Aspirin in Primary Prevention and Cancer
6. Guidelines Recommendations
7. Considerations for a Modern Approach to Cardiovascular Primary Prevention
7.1. Defining the Threshold of Intervention
7.2. Competing Benefit of Alternative Therapies
7.3. Potential “Facilitators” of Aspirin-Based Primary Prevention
8. Conclusion
Author Contributions
Conflicts of Interest
References
- Edney, P.; Jackson, P.; Burrell, B.; Lawton, N.; Leigh, N.; Lindsay McLellan, P.; Newman, C.; Pickard, J.; Weiser, R.; Williams, S.; et al. Secondary Prevention of Vascular Disease by Prolonged Antiplatelet Treatment. Br Med J (Clin Res Ed) 1988, 296, 320. [Google Scholar] [CrossRef]
- Benenati, S.; Galli, M.; Marzo, V. De; Pescetelli, F.; Toma, M.; Andreotti, F.; Della Bona, R.; Canepa, M.; Ameri, P.; Crea, F.; et al. Very Short vs. Long Dual Antiplatelet Therapy after Second Generation Drug-Eluting Stents in 35 785 Patients Undergoing Percutaneous Coronary Interventions: A Meta-Analysis of Randomized Controlled Trials. Eur Heart J Cardiovasc Pharmacother 2021, 7, 86–93. [Google Scholar] [CrossRef] [PubMed]
- Benenati, S.; Crimi, G.; Canale, C.; Pescetelli, F.; De Marzo, V.; Vergallo, R.; Galli, M.; Della Bona, R.; Canepa, M.; Ameri, P.; et al. Duration of Dual Antiplatelet Therapy and Subsequent Monotherapy Type in Patients Undergoing Drug-Eluting Stent Implantation: A Network Meta-Analysis. Eur Heart J Cardiovasc Pharmacother 2022, 8, 56–64. [Google Scholar] [CrossRef] [PubMed]
- O’Brien, C.W.; Juraschek, S.P.; Wee, C.C. Prevalence of Aspirin Use for Primary Prevention of Cardiovascular Disease in the United States: Results From the 2017 National Health Interview Survey. Ann Intern Med 2019, 171, 596. [Google Scholar] [CrossRef] [PubMed]
- Capodanno, D.; Angiolillo, D.J. Aspirin for Primary Cardiovascular Risk Prevention and Beyond in Diabetes Mellitus. Circulation 2016, 134, 1579–1594. [Google Scholar] [CrossRef] [PubMed]
- Patrono, C.; García Rodríguez, L.A.; Landolfi, R.; Baigent, C. Low-Dose Aspirin for the Prevention of Atherothrombosis. N Engl J Med 2005, 353, 2373–2383. [Google Scholar] [CrossRef] [PubMed]
- FitzGerald, G.A. Mechanisms of Platelet Activation: Thromboxane A2 as an Amplifying Signal for Other Agonists. Am J Cardiol 1991, 68, B11–B15. [Google Scholar] [CrossRef]
- Moncada, S.; Vane, J.R. Arachidonic Acid Metabolites and the Interactions between Platelets and Blood-Vessel Walls. N Engl J Med 1979, 300, 1142–1147. [Google Scholar] [CrossRef]
- Kobayashi, T.; Tahara, Y.; Matsumoto, M.; Iguchi, M.; Sano, H.; Murayama, T.; Arai, H.; Oida, H.; Yurugi-Kobayashi, T.; Yamashita, J.K.; et al. Roles of Thromboxane A(2) and Prostacyclin in the Development of Atherosclerosis in ApoE-Deficient Mice. J Clin Invest 2004, 114, 784–794. [Google Scholar] [CrossRef]
- Patrignani, P.; Filabozzi, P.; Patrono, C. Selective Cumulative Inhibition of Platelet Thromboxane Production by Low-Dose Aspirin in Healthy Subjects. J Clin Invest 1982, 69, 1366–1372. [Google Scholar] [CrossRef]
- Mcadam, B.F.; Catella-Lawson, F.; Mardini, I.A.; Kapoor, S.; Lawson, J.A.; Fitzgerald, G.A. Systemic Biosynthesis of Prostacyclin by Cyclooxygenase (COX)-2: The Human Pharmacology of a Selective Inhibitor of COX-2. Proc Natl Acad Sci U S A 1999, 96, 272–277. [Google Scholar] [CrossRef] [PubMed]
- FitzGerald, G.A.; Oates, J.A.; Hawiger, J.; Maas, R.L.; Roberts, L.J.; Lawson, J.A.; Brash, A.R. Endogenous Biosynthesis of Prostacyclin and Thromboxane and Platelet Function during Chronic Administration of Aspirin in Man. J Clin Invest 1983, 71, 676–688. [Google Scholar] [CrossRef] [PubMed]
- Patrono, C.; Ciabarroni, G.; Patrignani, P.; Pugliese, F.; Filabozzi, P.; Catella, F.; Davi, G.; Forni, L. Clinical Pharmacology of Platelet Cyclooxygenase Inhibition. Circulation 1985, 72, 1177–1184. [Google Scholar] [CrossRef] [PubMed]
- Hansson, L.; Zanchetti, A.; Carruthers, S.G.; Dahlöf, B.; Elmfeldt, D.; Julius, S.; Ménard, J.; Rahn, K.H.; Wedel, H.; Westerling, S. Effects of Intensive Blood-Pressure Lowering and Low-Dose Aspirin in Patients with Hypertension: Principal Results of the Hypertension Optimal Treatment (HOT) Randomised Trial. Lancet 1998, 351, 1755–1762. [Google Scholar] [CrossRef] [PubMed]
- Snowden, S.; Nelson, R. The Effects of Nonsteroidal Anti-Inflammatory Drugs on Blood Pressure in Hypertensive Patients. Cardiol Rev 2011, 19, 184–191. [Google Scholar] [CrossRef]
- FitzGerald, G.A.; Oates, J.A.; Hawiger, J.; Maas, R.L.; Roberts, L.J.; Lawson, J.A.; Brash, A.R. Endogenous Biosynthesis of Prostacyclin and Thromboxane and Platelet Function during Chronic Administration of Aspirin in Man. J Clin Invest 1983, 71, 676–688. [Google Scholar] [CrossRef] [PubMed]
- Reilly, I.; FitzGerald, G. Inhibition of Thromboxane Formation In Vivo and Ex Vivo: Implications for Therapy With Platelet Inhibitory Drugs. Blood 1987, 69, 180–186. [Google Scholar] [CrossRef] [PubMed]
- Maree, A.O.; Curtin, R.J.; Dooley, M.; Conroy, R.M.; Crean, P.; Cox, D.; Fitzgerald, D.J. Platelet Response to Low-Dose Enteric-Coated Aspirin in Patients With Stable Cardiovascular Disease. J Am Coll Cardiol 2005, 46, 1258–1263. [Google Scholar] [CrossRef] [PubMed]
- Denis, M.M.; Tolley, N.D.; Bunting, M.; Schwertz, H.; Jiang, H.; Lindemann, S.; Yost, C.C.; Rubner, F.J.; Albertine, K.H.; Swoboda, K.J.; et al. Escaping the Nuclear Confines: Signal-Dependent Pre-MRNA Splicing in Anucleate Platelets. Cell 2005, 122, 379–391. [Google Scholar] [CrossRef]
- Evangelista, V.; Manarini, S.; Di Santo, A.; Capone, M.L.; Ricciotti, E.; Di Francesco, L.; Tacconelli, S.; Sacchetti, A.; D’Angelo, S.; Scilimati, A.; et al. De Novo Synthesis of Cyclooxygenase-1 Counteracts the Suppression of Platelet Thromboxane Biosynthesis by Aspirin. Circ Res 2006, 98, 593–595. [Google Scholar] [CrossRef]
- Cagnina, A.; Chabot, O.; Davin, L.; Lempereur, M.; Maréchal, P.; Oury, C.; Lancellotti, P. Atherosclerosis — An Inflammatory Disease 1999, 77, 302-309. 10.1056/NEJM199901143400207. [CrossRef]
- Lindemann, S.; Tolley, N.D.; Dixon, D.A.; McIntyre, T.M.; Prescott, S.M.; Zimmerman, G.A.; Weyrich, A.S. Activated Platelets Mediate Inflammatory Signaling by Regulated Interleukin 1β Synthesis. Journal of Cell Biology 2001, 154, 485–490. [Google Scholar] [CrossRef] [PubMed]
- Brown, J.R.; DuBois, R.N. COX-2: A Molecular Target for Colorectal Cancer Prevention. J Clin Oncol 2005, 23, 2840–2855. [Google Scholar] [CrossRef]
- Thun, M.J.; Jacobs, E.J.; Patrono, C. The Role of Aspirin in Cancer Prevention. Nat Rev Clin Oncol 2012, 9, 259–267. [Google Scholar] [CrossRef] [PubMed]
- Peto, R.; Gray, R.; Collins, R.; Wheatley, K.; Hennekens, C.; Jamrozik, K.; Warlow, C.; Hafner, B.; Thompson, E.; Norton, S.; et al. Randomised Trial of Prophylactic Daily Aspirin in British Male Doctors. Br Med J (Clin Res Ed) 1988, 296, 313–316. [Google Scholar] [CrossRef] [PubMed]
- Steering Committee of the Physicians’ Health Study Research Group Final Report on the Aspirin Component of the Ongoing Physicians’ Health Study. N Engl J Med 1989, 321, 129–135. [CrossRef] [PubMed]
- Meade, T.W.; Wilkes, H.C.; Kelleher, C.C.; Roderick, P.J.; Brennan, P.J.; Wilson, C.W.; Howarth, D.J.; Stirling, Y.; Garrow, K.; Dickinson, C.J.; et al. Thrombosis Prevention Trial: Randomised Trial of Low-Intensity Oral Anticoagulation with Warfarin and Low-Dose Aspirin in the Primary Prevention of Ischaemic Heart Disease in Men at Increased Risk. Lancet 1998, 351, 233–241. [Google Scholar] [CrossRef]
- Sacco, M.; Pellegrini, F.; Roncaglioni, M.C.; Avanzini, F.; Tognoni, G.; Nicolucci, A. Primary Prevention of Cardiovascular Events with Low-Dose Aspirin and Vitamin E in Type 2 Diabetic Patients: Results of the Primary Prevention Project (PPP) Trial. Diabetes Care 2003, 26, 3264–3272. [Google Scholar] [CrossRef] [PubMed]
- Ridker, P.M.; Cook, N.R.; Lee, I.-M.; Gordon, D.; Gaziano, J.M.; Manson, J.E.; Hennekens, C.H.; Buring, J.E. A Randomized Trial of Low-Dose Aspirin in the Primary Prevention of Cardiovascular Disease in Women. N Engl J Med 2005, 352, 1293–1304. [Google Scholar] [CrossRef] [PubMed]
- Belch, J.; MacCuish, A.; Campbell, I.; Cobbe, S.; Taylor, R.; Prescott, R.; Lee, R.; Bancroft, J.; MacEwan, S.; Shepherd, J.; et al. The Prevention of Progression of Arterial Disease and Diabetes (POPADAD) Trial: Factorial Randomised Placebo Controlled Trial of Aspirin and Antioxidants in Patients with Diabetes and Asymptomatic Peripheral Arterial Disease. BMJ 2008, 337. [Google Scholar] [CrossRef]
- Ogawa, H.; Nakayama, M.; Morimoto, T.; Uemura, S.; Kanauchi, M.; Doi, N.; Jinnouchi, H.; Sugiyama, S.; Saito, Y. Low-Dose Aspirin for Primary Prevention of Atherosclerotic Events in Patients With Type 2 Diabetes: A Randomized Controlled Trial. JAMA 2008, 300, 2134–2141. [Google Scholar] [CrossRef]
- Collins, R.; Peto, R.; Hennekens, C.; Doll, R.; Bubes, V.; Buring, J.; Dushkesas, R.; Gaziano, M.; Brennan, P.; Meade, T.; et al. Aspirin in the Primary and Secondary Prevention of Vascular Disease: Collaborative Meta-Analysis of Individual Participant Data from Randomised Trials. Lancet 2009, 373, 1849. [Google Scholar] [CrossRef] [PubMed]
- Gaziano, J.M.; Brotons, C.; Coppolecchia, R.; Cricelli, C.; Darius, H.; Gorelick, P.B.; Howard, G.; Pearson, T.A.; Rothwell, P.M.; Ruilope, L.M.; et al. Use of Aspirin to Reduce Risk of Initial Vascular Events in Patients at Moderate Risk of Cardiovascular Disease (ARRIVE): A Randomised, Double-Blind, Placebo-Controlled Trial. Lancet 2018, 392, 1036–1046. [Google Scholar] [CrossRef] [PubMed]
- McNeil, J.J.; Wolfe, R.; Woods, R.L.; Tonkin, A.M.; Donnan, G.A.; Nelson, M.R.; Reid, C.M.; Lockery, J.E.; Kirpach, B.; Storey, E.; et al. Effect of Aspirin on Cardiovascular Events and Bleeding in the Healthy Elderly. New England Journal of Medicine 2018, 379, 1509–1518. [Google Scholar] [CrossRef] [PubMed]
- Bowman, L.; Mafham, M.; Wallendszus, K.; Stevens, W. ; and the ASCEND Study Collaborative Group Effects of Aspirin for Primary Prevention in Persons with Diabetes Mellitus. New England Journal of Medicine 2018, 379, 1529–1539. [Google Scholar] [CrossRef] [PubMed]
- Zheng, S.L.; Roddick, A.J. Association of Aspirin Use for Primary Prevention With Cardiovascular Events and Bleeding Events: A Systematic Review and Meta-Analysis. JAMA 2019, 321, 277–287. [Google Scholar] [CrossRef]
- Shah, R.; Khan, B.; Latham, S.B.; Khan, S.A.; Rao, S. V. A Meta-Analysis of Aspirin for the Primary Prevention of Cardiovascular Diseases in the Context of Contemporary Preventive Strategies. Am J Med 2019, 132, 1295–1304. [Google Scholar] [CrossRef]
- Galli, M.; Andreotti, F.; D’amario, D.; Vergallo, R.; Montone, R.A.; Porto, I.; Crea, F. Aspirin in Primary Prevention of Cardiovascular Disease in the Elderly. Eur Heart J Cardiovasc Pharmacother 2020, 6, 326–327. [Google Scholar] [CrossRef]
- Guirguis-Blake, J.M.; Evans, C. V.; Perdue, L.A.; Bean, S.I.; Senger, C.A. Aspirin Use to Prevent Cardiovascular Disease and Colorectal Cancer: Updated Evidence Report and Systematic Review for the US Preventive Services Task Force. JAMA 2022, 327, 1585–1597. [Google Scholar] [CrossRef]
- Saito, Y.; Okada, S.; Ogawa, H.; Soejima, H.; Sakuma, M.; Nakayama, M.; Doi, N.; Jinnouchi, H.; Waki, M.; Masuda, I.; et al. Low-Dose Aspirin for Primary Prevention of Cardiovascular Events in Patients With Type 2 Diabetes Mellitus: 10-Year Follow-Up of a Randomized Controlled Trial. Circulation 2017, 135, 659–670. [Google Scholar] [CrossRef]
- Cook, N.R.; Cole, S.R.; Buring, J.E. Aspirin in the Primary Prevention of Cardiovascular Disease in the Women’s Health Study: Effect of Noncompliance. Eur J Epidemiol 2012, 27, 431. [Google Scholar] [CrossRef]
- Ardeshna, D.; Khare, S.; Jagadish, P.S.; Bhattad, V.; Cave, B.; Khouzam, R.N. The Dilemma of Aspirin Resistance in Obese Patients. Ann Transl Med 2019, 7, 404–404. [Google Scholar] [CrossRef] [PubMed]
- Dal Canto, E.; Ceriello, A.; Rydén, L.; Ferrini, M.; Hansen, T.B.; Schnell, O.; Standl, E.; Beulens, J.W.J. Diabetes as a Cardiovascular Risk Factor: An Overview of Global Trends of Macro and Micro Vascular Complications. Eur J Prev Cardiol 2019, 26, 25–32. [Google Scholar] [CrossRef] [PubMed]
- Capodanno, D.; Patel, A.; Dharmashankar, K.; Ferreiro, J.L.; Ueno, M.; Kodali, M.; Tomasello, S.D.; Capranzano, P.; Seecheran, N.; Darlington, A.; et al. Pharmacodynamic Effects of Different Aspirin Dosing Regimens in Type 2 Diabetes Mellitus Patients with Coronary Artery Disease. Circ Cardiovasc Interv 2011, 4, 180–187. [Google Scholar] [CrossRef] [PubMed]
- Spectre, G.; Arnetz, L.; Östenson, C.G.; Brismar, K.; Li, N.; Hjemdahl, P. Twice Daily Dosing of Aspirin Improves Platelet Inhibition in Whole Blood in Patients with Type 2 Diabetes Mellitus and Micro-or Macrovascular Complications. Thromb Haemost 2011, 106, 491–499. [Google Scholar] [CrossRef] [PubMed]
- DiChiara, J.; Bliden, K.P.; Tantry, U.S.; Hamed, M.S.; Antonino, M.J.; Suarez, T.A.; Bailon, O.; Singla, A.; Gurbel, P.A. The Effect of Aspirin Dosing on Platelet Function in Diabetic and Nondiabetic Patients: An Analysis from the Aspirin-Induced Platelet Effect (ASPECT) Study. Diabetes 2007, 56, 3014–3019. [Google Scholar] [CrossRef] [PubMed]
- Gurbel, P.A.; Bliden, K.P.; DiChiara, J.; Newcomer, J.; Weng, W.; Neerchal, N.K.; Gesheff, T.; Chaganti, S.K.; Etherington, A.; Tantry, U.S. Evaluation of Dose-Related Effects of Aspirin on Platelet Function: Results from the Aspirin-Induced Platelet Effect (ASPECT) Study. Circulation 2007, 115, 3156–3164. [Google Scholar] [CrossRef]
- Addad, F.; Chakroun, T.; Elalamy, I.; Abderazek, F.; Chouchene, S.; Dridi, Z.; Gerotziafas, G.T.; Hatmi, M.; Hassine, M.; Gamra, H. Antiplatelet Effect of Once- or Twice-Daily Aspirin Dosage in Stable Coronary Artery Disease Patients with Diabetes. Int J Hematol 2010, 92, 296–301. [Google Scholar] [CrossRef]
- Dillinger, J.G.; Drissa, A.; Sideris, G.; Bal Dit Sollier, C.; Voicu, S.; Manzo Silberman, S.; Logeart, D.; Drouet, L.; Henry, P. Biological Efficacy of Twice Daily Aspirin in Type 2 Diabetic Patients with Coronary Artery Disease. Am Heart J 2012, 164. [Google Scholar] [CrossRef]
- Bethel, M.A.; Harrison, P.; Sourij, H.; Sun, Y.; Tucker, L.; Kennedy, I.; White, S.; Hill, L.; Oulhaj, A.; Coleman, R.L.; et al. Randomized Controlled Trial Comparing Impact on Platelet Reactivity of Twice-Daily with Once-Daily Aspirin in People with Type 2 Diabetes. Diabetic Medicine 2016, 33, 224–230. [Google Scholar] [CrossRef]
- Jones, W.S.; Mulder, H.; Wruck, L.M.; Pencina, M.J.; Kripalani, S.; Muñoz, D.; Crenshaw, D.L.; Effron, M.B.; Re, R.N.; Gupta, K.; et al. Comparative Effectiveness of Aspirin Dosing in Cardiovascular Disease. New England Journal of Medicine 2021, 384, 1981–1990. [Google Scholar] [CrossRef]
- Pulcinelli, F.M.; Biasucci, L.M.; Riondino, S.; Giubilato, S.; Leo, A.; Di Renzo, L.; Trifir, E.; Mattiello, T.; Pitocco, D.; Liuzzo, G.; et al. COX-1 Sensitivity and Thromboxane A2 Production in Type 1 and Type 2 Diabetic Patients under Chronic Aspirin Treatment. Eur Heart J 2009, 30, 1279–1286. [Google Scholar] [CrossRef]
- Santilli, F.; Vazzana, N.; Liani, R.; Guagnano, M.T.; Davì, G. Platelet Activation in Obesity and Metabolic Syndrome. Obes Rev 2012, 13, 27–42. [Google Scholar] [CrossRef]
- Cox, D.; Maree, A.O.; Dooley, M.; Conroy, R.; Byrne, M.F.; Fitzgerald, D.J. Effect of Enteric Coating on Antiplatelet Activity of Low-Dose Aspirin in Healthy Volunteers. Stroke 2006, 37, 2153–2158. [Google Scholar] [CrossRef] [PubMed]
- Norgard, N.B.; Monte, S. V.; Fernandez, S.F.; Ma, Q. Aspirin Responsiveness Changes in Obese Patients Following Bariatric Surgery. Cardiovasc Ther 2017, 35. [Google Scholar] [CrossRef]
- Petrucci, G.; Zaccardi, F.; Giaretta, A.; Cavalca, V.; Capristo, E.; Cardillo, C.; Pitocco, D.; Porro, B.; Schinzari, F.; Toffolo, G.; et al. Obesity Is Associated with Impaired Responsiveness to Once-Daily Low-Dose Aspirin and in Vivo Platelet Activation. J Thromb Haemost 2019, 17, 885–895. [Google Scholar] [CrossRef] [PubMed]
- Becker, D.M.; Segal, J.; Vaidya, D.; Yanek, L.R.; Herrera-Galeano, J.E.; Bray, P.F.; Moy, T.F.; Becker, L.C.; Faraday, N. Sex Differences in Platelet Reactivity and Response to Low-Dose Aspirin Therapy. JAMA 2006, 295, 1420–1427. [Google Scholar] [CrossRef] [PubMed]
- Qayyum, R.; Becker, D.M.; Yanek, L.R.; Moy, T.F.; Becker, L.C.; Faraday, N.; Vaidya, D. Platelet Inhibition by Aspirin 81 and 325 Mg/Day in Men versus Women without Clinically Apparent Cardiovascular Disease. Am J Cardiol 2008, 101, 1359–1363. [Google Scholar] [CrossRef]
- Kim, S.P.; Ryu, J.; Kim, S.H.; Yoon, H.J. Low-Dose Aspirin in the Primary Prevention of Cardiovascular Diseases: A Retrospective, Propensity Score Matched Study. Atherosclerosis 2023, 371, 54–60. [Google Scholar] [CrossRef] [PubMed]
- Cattaneo, M.; Faioni, E.M. Why Does Ticagrelor Induce Dyspnea? Thromb Haemost 2012, 108, 1031–1036. [Google Scholar] [CrossRef] [PubMed]
- Benenati, S.; Canale, C.; De Marzo, V.; Della Bona, R.; Rosa, G.M.; Porto, I. Atrial Fibrillation and Alzheimer’s Disease: A Conundrum. Eur J Clin Invest 2021, 51. [Google Scholar] [CrossRef]
- Pollard, M.; Luckert, P.H. Effect of Indomethacin on Intestinal Tumors Induced in Rats by the Acetate Derivative of Dimethylnitrosamine. Science (1979) 1981, 214, 558–559. [Google Scholar] [CrossRef] [PubMed]
- Thun, M.J.; Namboodiri, M.M.; Heath, C.W. Aspirin Use and Reduced Risk of Fatal Colon Cancer. N Engl J Med 1991, 325, 1593–1596. [Google Scholar] [CrossRef] [PubMed]
- Kune, G.; Kune, S.; Watson, L.F. Colorectal Cancer Risk, Chronic Illnesses, Operations, and Medications: Case Control Results from the Melbourne Colorectal Cancer Study. Cancer research (Baltimore) 1988, 48, 4399–4404. [Google Scholar] [CrossRef] [PubMed]
- Gann, P.H.; Manson, J.E.; Glynn, R.J.; Buring, J.E.; Hennekens, C.H. Low-Dose Aspirin and Incidence of Colorectal Tumors in a Randomized Trial. J Natl Cancer Inst 1993, 85, 1220–1224. [Google Scholar] [CrossRef] [PubMed]
- Burn, J.; Bishop, D.T.; Mecklin, J.-P.; Macrae, F.; Möslein, G.; Olschwang, S.; Bisgaard, M.-L.; Ramesar, R.; Eccles, D.; Maher, E.R.; et al. Effect of Aspirin or Resistant Starch on Colorectal Neoplasia in the Lynch Syndrome. New England Journal of Medicine 2008, 359, 2567–2578. [Google Scholar] [CrossRef] [PubMed]
- Cook, N.R.; Lee, I.M.; Zhang, S.M.; Moorthy, M.V.; Buring, J.E. Alternate-Day, Low-Dose Aspirin and Cancer Risk: Long-Term Observational Follow-up of a Randomized Trial. Ann Intern Med 2013, 159, 77–85. [Google Scholar] [CrossRef] [PubMed]
- Burn, J.; Gerdes, A.M.; MacRae, F.; Mecklin, J.P.; Moeslein, G.; Olschwang, S.; Eccles, D.; Evans, D.G.; Maher, E.R.; Bertario, L.; et al. Long-Term Effect of Aspirin on Cancer Risk in Carriers of Hereditary Colorectal Cancer: An Analysis from the CAPP2 Randomised Controlled Trial. Lancet 2011, 378, 2081–2087. [Google Scholar] [CrossRef] [PubMed]
- Rothwell, P.M.; Wilson, M.; Elwin, C.E.; Norrving, B.; Algra, A.; Warlow, C.P.; Meade, T.W. Long-Term Effect of Aspirin on Colorectal Cancer Incidence and Mortality: 20-Year Follow-up of Five Randomised Trials. Lancet 2010, 376, 1741–1750. [Google Scholar] [CrossRef] [PubMed]
- Rothwell, P.M.; Wilson, M.; Price, J.F.; Belch, J.F.F.; Meade, T.W.; Mehta, Z. Effect of Daily Aspirin on Risk of Cancer Metastasis: A Study of Incident Cancers during Randomised Controlled Trials. Lancet 2012, 379, 1591–1601. [Google Scholar] [CrossRef]
- Wang, L.; Zhang, R.; Yu, L.; Xiao, J.; Zhou, X.; Li, X.; Song, P.; Li, X. Aspirin Use and Common Cancer Risk: A Meta-Analysis of Cohort Studies and Randomized Controlled Trials. Front Oncol 2021, 11. [Google Scholar] [CrossRef]
- Bibbins-Domingo, K.; Grossman, D.C.; Curry, S.J.; Davidson, K.W.; Epling, J.W.; García, F.A.R.; Gillman, M.; Harper, D.M.; Kemper, A.R.; Krist, A.H.; et al. Aspirin Use for the Primary Prevention of Cardiovascular Disease and Colorectal Cancer: U.S. Preventive Services Task Force Recommendation Statement. Ann Intern Med 2016, 164, 836–845. [Google Scholar] [CrossRef] [PubMed]
- Mcneil, J.J.; Gibbs, P.; Orchard, S.G.; Lockery, J.E.; Bernstein, W.B.; Cao, Y.; Ford, L.; Haydon, A.; Kirpach, B.; Macrae, F.; et al. Effect of Aspirin on Cancer Incidence and Mortality in Older Adults. J Natl Cancer Inst 2021, 113, 258–265. [Google Scholar] [CrossRef] [PubMed]
- National Institute for Health and Care Effectiveness of Aspirin in the Prevention of Colorectal Cancer in People with Lynch Syndrome; National Institute for Health and Care Excellence (NICE), 2020;
- Di Fusco, S.A.; Cianfrocca, C.; Bisceglia, I.; Spinelli, A.; Alonzo, A.; Mocini, E.; Gulizia, M.M.; Gabrielli, D.; Oliva, F.; Imperoli, G.; et al. Potential Pathophysiologic Mechanisms Underlying the Inherent Risk of Cancer in Patients with Atherosclerotic Cardiovascular Disease. Int J Cardiol 2022, 363, 190–195. [Google Scholar] [CrossRef] [PubMed]
- Giovannucci, E.; Egan, K.M.; Hunter, D.J.; Stampfer, M.J.; Colditz, G.A.; Willett, W.C.; Speizer, F.E. Aspirin and the Risk of Colorectal Cancer in Women. New England Journal of Medicine 1995, 333, 609–614. [Google Scholar] [CrossRef] [PubMed]
- Giovannucci, E.; Rimm, E.B.; Stampfer, M.J.; Colditz, G.A.; Ascherio, A.; Willett, W.C. Aspirin Use and the Risk for Colorectal Cancer and Adenoma in Male Health Professionals. Ann Intern Med 1994, 121, 241–246. [Google Scholar] [CrossRef] [PubMed]
- Chan, A.T.; Ogino, S.; Fuchs, C.S. Aspirin and the Risk of Colorectal Cancer in Relation to the Expression of COX-2. New England Journal of Medicine 2007, 356, 2131–2142. [Google Scholar] [CrossRef]
- Shechan, K.M.; Shcahan, K.; O’Donoghue, P.; Imacswecney, F.; Conroy, R.M.; Fitzgerald, D.J.; Murray, F.E. The Relationship Between Cyclooxygenase-2 Expression and Colorectal Cancer. JAMA 1999, 282, 1254–1257. [Google Scholar] [CrossRef]
- Ogino, S.; Kirkner, G.J.; Nosho, K.; Irahara, N.; Kure, S.; Shima, K.; Hazra, A.; Chan, A.T.; Dehari, R.; Giovannucci, E.L.; et al. Cyclooxygenase-2 Expression Is an Independent Predictor of Poor Prognosis in Colon Cancer. Clinical Cancer Research 2008, 14, 8221–8227. [Google Scholar] [CrossRef]
- González-Pérez, A.; García Rodríguez, L.A.; López-Ridaura, R. Effects of Non-Steroidal Anti-Inflammatory Drugs on Cancer Sites Other than the Colon and Rectum: A Metal-Analysis. BMC Cancer 2003, 3, 1–12. [Google Scholar] [CrossRef]
- Arnett, D.K.; Blumenthal, R.S.; Albert, M.A.; Buroker, A.B.; Goldberger, Z.D.; Hahn, E.J.; Himmelfarb, C.D.; Khera, A.; Lloyd-Jones, D.; McEvoy, J.W.; et al. 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 2019, 140, e596–e646. [Google Scholar] [CrossRef]
- Davidson, K.W.; Barry, M.J.; Mangione, C.M.; Cabana, M.; Chelmow, D.; Coker, T.R.; Davis, E.M.; Donahue, K.E.; Jaén, C.R.; Krist, A.H.; et al. Aspirin Use to Prevent Cardiovascular Disease: US Preventive Services Task Force Recommendation Statement. JAMA 2022, 327, 1577–1584. [Google Scholar] [CrossRef]
- Visseren, F.L.J.; MacH, F.; Smulders, Y.M.; Carballo, D.; Koskinas, K.C.; Bäck, M.; Benetos, A.; Biffi, A.; Boavida, J.M.; Capodanno, D.; et al. 2021 ESC Guidelines on Cardiovascular Disease Prevention in Clinical PracticeDeveloped by the Task Force for Cardiovascular Disease Prevention in Clinical Practice with Representatives of the European Society of Cardiology and 12 Medical Societies With the Special Contribution of the European Association of Preventive Cardiology (EAPC). Eur Heart J 2021, 42, 3227–3337. [Google Scholar] [CrossRef]
- Committee, A.D.A.P.P. 10. Cardiovascular Disease and Risk Management: Standards of Medical Care in Diabetes—2022. Diabetes Care 2022, 45, S144–S174. [Google Scholar] [CrossRef] [PubMed]
- Aboyans, V.; Ricco, J.B.; Bartelink, M.L.E.L.; Björck, M.; Brodmann, M.; Cohnert, T.; Collet, J.P.; Czerny, M.; De Carlo, M.; Debus, S.; et al. 2017 ESC Guidelines on the Diagnosis and Treatment of Peripheral Arterial Diseases, in Collaboration with the European Society for Vascular Surgery (ESVS)Document Covering Atherosclerotic Disease of Extracranial Carotid and Vertebral, Mesenteric, Renal, Upper and Lower Extremity ArteriesEndorsed by: The European Stroke Organization (ESO)The Task Force for the Diagnosis and Treatment of Peripheral Arterial Diseases of the European Society of Cardiology (ESC) and of the European Society for Vascul. Eur Heart J 2018, 39, 763–816. [Google Scholar] [CrossRef]
- Ahmadi, S.F.; Streja, E.; Zahmatkesh, G.; Streja, D.; Kashyap, M.; Moradi, H.; Molnar, M.Z.; Reddy, U.; Amin, A.N.; Kovesdy, C.P.; et al. Reverse Epidemiology of Traditional Cardiovascular Risk Factors in the Geriatric Population. J Am Med Dir Assoc 2015, 16, 933. [Google Scholar] [CrossRef]
- Vaes, B.; Depoortere, D.; Van Pottelbergh, G.; Matheï, C.; Neto, J.; Degryse, J. Association between Traditional Cardiovascular Risk Factors and Mortality in the Oldest Old: Untangling the Role of Frailty. BMC Geriatr 2017, 17, 1–8. [Google Scholar] [CrossRef]
- SCORE2 working group and ESC Cardiovascular risk collaboration; Hageman, S. ; Pennells, L.; Ojeda, F.; Kaptoge, S.; Kuulasmaa, K.; de Vries, T.; Xu, Z.; Kee, F.; Chung, R.; et al. SCORE2 Risk Prediction Algorithms: New Models to Estimate 10-Year Risk of Cardiovascular Disease in Europe. Eur Heart J 2021, 42, 2439–2454. [Google Scholar] [CrossRef]
- SCORE2-OP working group and ESC Cardiovascular risk collaboration; de Vries, T. I.; Cooney, M.T.; Selmer, R.M.; Hageman, S.H.J.; Pennells, L.A.; Wood, A.; Kaptoge, S.; Xu, Z.; Westerink, J.; et al. SCORE2-OP Risk Prediction Algorithms: Estimating Incident Cardiovascular Event Risk in Older Persons in Four Geographical Risk Regions. Eur Heart J 2021, 42, 2455–2467. [Google Scholar] [CrossRef]
- Pennells, L.; Kaptoge, S.; Østergaard, H.B.; Read, S.H.; Carinci, F.; Franch-Nadal, J.; Petitjean, C.; Taylor, O.; Hageman, S.H.J.; Xu, Z.; et al. SCORE2-Diabetes: 10-Year Cardiovascular Risk Estimation in Type 2 Diabetes in Europe. Eur Heart J 2023, 44, 2544–2556. [Google Scholar] [CrossRef] [PubMed]
- Montone, R.A.; Camilli, M.; Calvieri, C.; Magnani, G.; Bonanni, A.; Bhatt, D.L.; Rajagopalan, S.; Crea, F.; Niccoli, G. Exposome in Ischaemic Heart Disease: Beyond Traditional Risk Factors. Eur Heart J 2024, 45, 419–438. [Google Scholar] [CrossRef] [PubMed]
- Khan, S.S.; Coresh, J.; Pencina, M.J.; Ndumele, C.E.; Rangaswami, J.; Chow, S.L.; Palaniappan, L.P.; Sperling, L.S.; Virani, S.S.; Ho, J.E.; et al. Novel Prediction Equations for Absolute Risk Assessment of Total Cardiovascular Disease Incorporating Cardiovascular-Kidney-Metabolic Health: A Scientific Statement From the American Heart Association. Circulation 2023, 148, 1982–2004. [Google Scholar] [CrossRef]
- Di Fusco, S.A.; Arca, M.; Scicchitano, P.; Alonzo, A.; Perone, F.; Gulizia, M.M.; Gabrielli, D.; Oliva, F.; Imperoli, G.; Colivicchi, F. Lipoprotein(a): A Risk Factor for Atherosclerosis and an Emerging Therapeutic Target. Heart 2022, 109, 18–25. [Google Scholar] [CrossRef]
- Reyes-Soffer, G.; Ginsberg, H.N.; Berglund, L.; Duell, P.B.; Heffron, S.P.; Kamstrup, P.R.; Lloyd-Jones, D.M.; Marcovina, S.M.; Yeang, C.; Koschinsky, M.L. Lipoprotein(a): A Genetically Determined, Causal, and Prevalent Risk Factor for Atherosclerotic Cardiovascular Disease: A Scientific Statement From the American Heart Association. Arterioscler Thromb Vasc Biol 2022, 42, E48–E60. [Google Scholar] [CrossRef]
- Bhatia, H.S.; Trainor, P.; Carlisle, S.; Tsai, M.Y.; Criqui, M.H.; Defilippis, A.; Tsimikas, S. Aspirin and Cardiovascular Risk in Individuals With Elevated Lipoprotein(a): The Multi-Ethnic Study of Atherosclerosis. J Am Heart Assoc 2024, 13, 33562. [Google Scholar] [CrossRef]
- Razavi, A.C.; Richardson, L.C.; Coronado, F.; Dzaye, O.; Bhatia, H.S.; Mehta, A.; Quyyumi, A.A.; Vaccarino, V.; Budoff, M.J.; Nasir, K.; et al. Aspirin Use for Primary Prevention Among US Adults With and Without Elevated Lipoprotein(a). Am J Prev Cardiol 2024, 100674. [Google Scholar] [CrossRef]
- Agatston, A.S.; Janowitz, W.R.; Hildner, F.J.; Zusmer, N.R.; Viamonte, M.; Detrano, R. Quantification of Coronary Artery Calcium Using Ultrafast Computed Tomography. J Am Coll Cardiol 1990, 15, 827–832. [Google Scholar] [CrossRef]
- Arad, Y.; Spadaro, L.A.; Goodman, K.; Newstein, D.; Guerci, A.D. Prediction of Coronary Events with Electron Beam Computed Tomography. J Am Coll Cardiol 2000, 36, 1253–1260. [Google Scholar] [CrossRef]
- Detrano, R.; Guerci, A.D.; Carr, J.J.; Bild, D.E.; Burke, G.; Folsom, A.R.; Liu, K.; Shea, S.; Szklo, M.; Bluemke, D.A.; et al. Coronary Calcium as a Predictor of Coronary Events in Four Racial or Ethnic Groups. 2008, 358, 1336-1345. 10.1056/NEJMOA072100. [CrossRef]
- Razavi, A.C.; Shaw, L.J.; Berman, D.S.; Budoff, M.J.; Wong, N.D.; Vaccarino, V.; van Assen, M.; De Cecco, C.N.; Quyyumi, A.A.; Mehta, A.; et al. Left Main Coronary Artery Calcium and Diabetes Confer Very-High-Risk Equivalence in Coronary Artery Calcium >1,000. Cardiovascular Imaging 2023. [Google Scholar] [CrossRef]
- Miedema, M.D.; Duprez, D.A.; Misialek, J.R.; Blaha, M.J.; Nasir, K.; Silverman, M.G.; Blankstein, R.; Budoff, M.J.; Greenland, P.; Folsom, A.R. Use of Coronary Artery Calcium Testing to Guide Aspirin Utilization for Primary Prevention: Estimates From the Multi-Ethnic Study of Atherosclerosis. Circ Cardiovasc Qual Outcomes 2014, 7, 453–460. [Google Scholar] [CrossRef] [PubMed]
- Nasir, K.; Bittencourt, M.S.; Blaha, M.J.; Blankstein, R.; Agatson, A.S.; Rivera, J.J.; Miemdema, M.D.; Sibley, C.T.; Shaw, L.J.; Blumenthal, R.S.; et al. Implications of Coronary Artery Calcium Testing Among Statin Candidates According to American College of Cardiology/American Heart Association Cholesterol Management Guidelines: MESA (Multi-Ethnic Study of Atherosclerosis). J Am Coll Cardiol 2015, 66, 1657–1668. [Google Scholar] [CrossRef] [PubMed]
- Cainzos-Achirica, M.; Miedema, M.D.; McEvoy, J.W.; Al Rifai, M.; Greenland, P.; Dardari, Z.; Budoff, M.; Blumenthal, R.S.; Yeboah, J.; Duprez, D.A.; et al. Coronary Artery Calcium for Personalized Allocation of Aspirin in Primary Prevention of Cardiovascular Disease in 2019. Circulation 2020, 141, 1541–1553. [Google Scholar] [CrossRef]
- Alam, S.; Mansour, K.; Taher, A.T.; Musallam, K.M. Aspirin Resistance. Adv Hematol 2009, 2009. [Google Scholar] [CrossRef]
- Galli, M.; Benenati, S.; Capodanno, D.; Franchi, F.; Rollini, F.; D’Amario, D.; Porto, I.; Angiolillo, D.J. Guided versus Standard Antiplatelet Therapy in Patients Undergoing Percutaneous Coronary Intervention: A Systematic Review and Meta-Analysis. The Lancet 2021, 397, 1470–1483. [Google Scholar] [CrossRef]
- Galli, M.; Benenati, S.; Franchi, F.; Rollini, F.; Capodanno, D.; Biondi-Zoccai, G.; Vescovo, G.M.; Cavallari, L.H.; Bikdeli, B.; Ten Berg, J.; et al. Comparative Effects of Guided vs. Potent P2Y12 Inhibitor Therapy in Acute Coronary Syndrome: A Network Meta-Analysis of 61 898 Patients from 15 Randomized Trials. Eur Heart J 2022, 43, 959–967. [Google Scholar] [CrossRef]
- Akintoye, E.; Afonso, L.; Jayanna, M.B.; Bao, W.; Briasoulis, A.; Robinson, J. Prognostic Utility of Risk Enhancers and Coronary Artery Calcium Score Recommended in the 2018 ACC/AHA Multisociety Cholesterol Treatment Guidelines Over the Pooled Cohort Equation: Insights From 3 Large Prospective Cohorts. Journal of the American Heart Association: Cardiovascular and Cerebrovascular Disease 2021, 10, 19589. [Google Scholar] [CrossRef]
- Yusuf, S.; Joseph, P.; Dans, A.; Gao, P.; Teo, K.; Xavier, D.; López-Jaramillo, P.; Yusoff, K.; Santoso, A.; Gamra, H.; et al. Polypill with or without Aspirin in Persons without Cardiovascular Disease. New England Journal of Medicine 2021, 384, 216–228. [Google Scholar] [CrossRef]
- Safi U. Khan, M.M.; Ahmad N. Lone, M.; Neal S. Kleiman, M.; Adeel Arshad, M.; Vardhmaan Jain, M.; Mahmoud Al Rifai, M.M.; Hassaan B. Arshad, M.; Sourbha S. Dani, M.Ms.; Amit Khera, M.; Pamela B. Morris, M.; et al. Aspirin With or Without Statin in Individuals Without Atherosclerotic Cardiovascular Disease Across Risk Categories. JACC: Advances , 100197. [CrossRef]
- Lanas, A.; Fuentes, J.; Benito, R.; Serrano, P.; Bajador, E.; Sáinz, R. Helicobacter Pylori Increases the Risk of Upper Gastrointestinal Bleeding in Patients Taking Low-Dose Aspirin. Aliment Pharmacol Ther 2002, 16, 779–786. [Google Scholar] [CrossRef]
- Steffel, J.; Eikelboom, J.W.; Anand, S.S.; Shestakovska, O.; Yusuf, S.; Fox, K.A.A. The COMPASS Trial: Net Clinical Benefit of Low-Dose Rivaroxaban plus Aspirin as Compared with Aspirin in Patients with Chronic Vascular Disease. Circulation 2020, 40–48. [Google Scholar] [CrossRef]
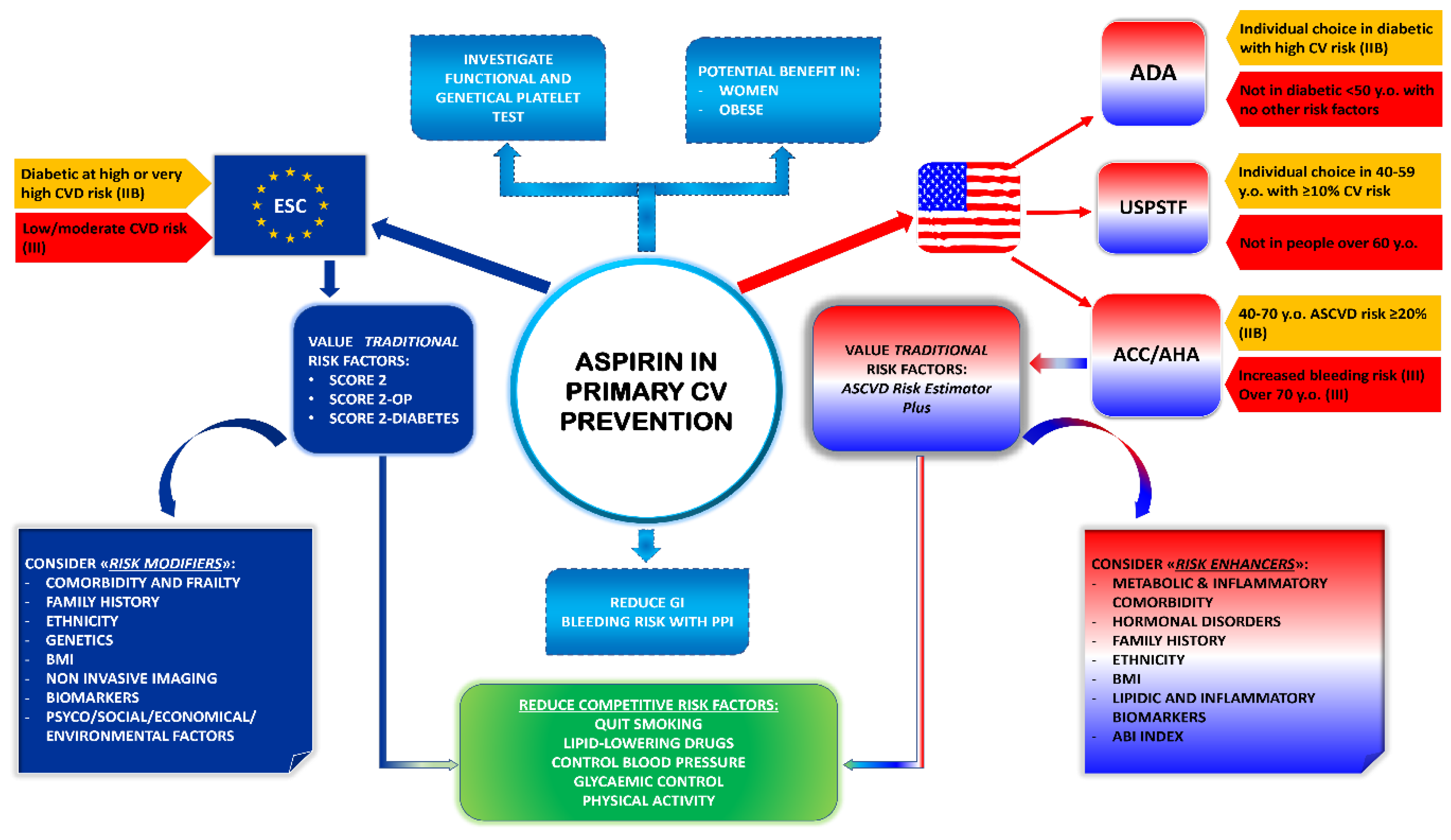
| Guidelines | Recommendation | Class | Level |
|---|---|---|---|
| 2019 American College of Cardiology/American Heart Association (ACC/AHA) Guideline on the Primary Prevention of Cardiovascular Disease | Low-dose aspirin (75-100 mg orally daily) might be considered for the primary prevention of ASCVD among select adults 40 to 70 years of age who are at higher ASCVD risk but not at increased bleeding risk | IIb | A |
| Low-dose aspirin (75-100 mg orally daily) should not be administered on a routine basis for the primary prevention of ASCVD among adults >70 years of age. | III | B-R | |
| Low-dose aspirin (75-100 mg orally daily) should not be administered for the primary prevention of ASCVD among adults of any age who are at increased risk of bleeding. | III | C-LD | |
| 2023 American Diabetes Association (ADA) “Standards of Medical Care in Diabetes” | Aspirin therapy (75–162 mg/day) may be considered as a primary prevention strategy in those with diabetes who are at increased cardiovascular risk, after a comprehensive discussion with the patient on the benefits versus the comparable increased risk of bleeding. | IIb | A |
| Aspirin is not recommended for those at low risk of ASCVD (such as men and women, aged <50 years old with diabetes with no other major ASCVD risk factors) as the low benefit is likely to be outweighed by the risks of bleeding. | III | N.A. | |
| 2022 Aspirin Use to Prevent Cardiovascular Disease: US Preventive Services Task Force (USPSTF) Recommendation Statement | The decision to initiate low-dose aspirin use for the primary prevention of CVD in adults aged 40 to 59 years old who have a 10% or greater 10-year CVD risk should be an individual one. Evidence indicates that the net benefit of aspirin use in this group is small. Persons who are not at increased risk for bleeding and are willing to take low-dose aspirin daily are more likely to benefit. | N.A. | C |
| The USPSTF recommends against initiating low-dose aspirin use for the primary prevention of CVD in adults 60 years or older. | III | D | |
| 2021 European Society of Cardiology (ESC) Guidelines on cardiovascular disease prevention in clinical practice | In patients with DM at high or very high CVD risk, low-dose aspirin may be considered for primary prevention in the absence of clear contraindications. | IIb | A |
| Antiplatelet therapy is not recommended in individuals with low/moderate CVD risk due to the increased risk of major bleeding. | III | A | |
| 2017 ESC Guidelines on the Diagnosis and Treatment of Peripheral Arterial Diseases, in collaboration with the European Society for Vascular Surgery (ESVS) | In patients with symptomatic carotid stenosis, long-term SAPT is recommended. | I | A |
| In patients with asymptomatic >50% carotid artery stenosis, long-term antiplatelet therapy (commonly low-dose aspirin) should be considered when the bleeding risk is low. | IIa | C | |
| Long-term SAPT is recommended in symptomatic patients with LEAD. | I | A | |
| Because of a lack of proven benefit, antiplatelet therapy is not routinely indicated in patients with isolated asymptomatic LEAD. | III | A |
| Traditional cardiovascular risk factors | |
|---|---|
| Age | Sex |
| Blood pressure | Blood cholesterol |
| Cigarette smoking | Diabetes Mellitus |
| Adiposity | Lifestyle (nutrition and physical activity) |
| 2019 ACC/AHA risk enhancers | 2021 ESC risk modifiers |
| Family history of premature ASCVD | Family history |
| Primary hypercholesterolemia | Genetics |
| Metabolic syndrome | Body composition |
| Chronic kidney disease | Frailty |
| History of premature menopause and history of pregnancy-associated conditions that increase later ASCVD risk | Imaging (CAC, CCTA, IMT, ABI) |
| High-risk race/ethnicity | Ethnicity |
| Chronic inflammatory conditions (psoriasis, lupus, RA, HIV/AIDS, etc.) | Biomarkers |
| Lipids/biomarkers: associated with increased ASCVD risk | Psychosocial factors |
| Persistently elevated, primary hypertriglyceridemia (≥175 mg/dL) | Socioeconomic determinants |
| Elevated high-sensitivity C-reactive protein (≥2.0 mg/L) | Environmental exposure |
| Elevated Lp(a): ≥50 mg/dL or ≥125 nmol/L constitutes a risk-enhancing factor especially at higher levels of Lp(a) | Clinical conditions (CKD, AF, COPD, Cancer, HF, inflamatory conditions, infections, sleeping and mental disorders) |
| Elevated apoB: ≥130 mg/dL corresponds to an LDL-C ≥160 mg/dL and constitutes a riskenhancing factor | |
| ABI <0.9 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





