Submitted:
31 May 2024
Posted:
31 May 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Proteomic Tools
2.1. General Remarks
2.2. From Protein Sequencing to Proteomics
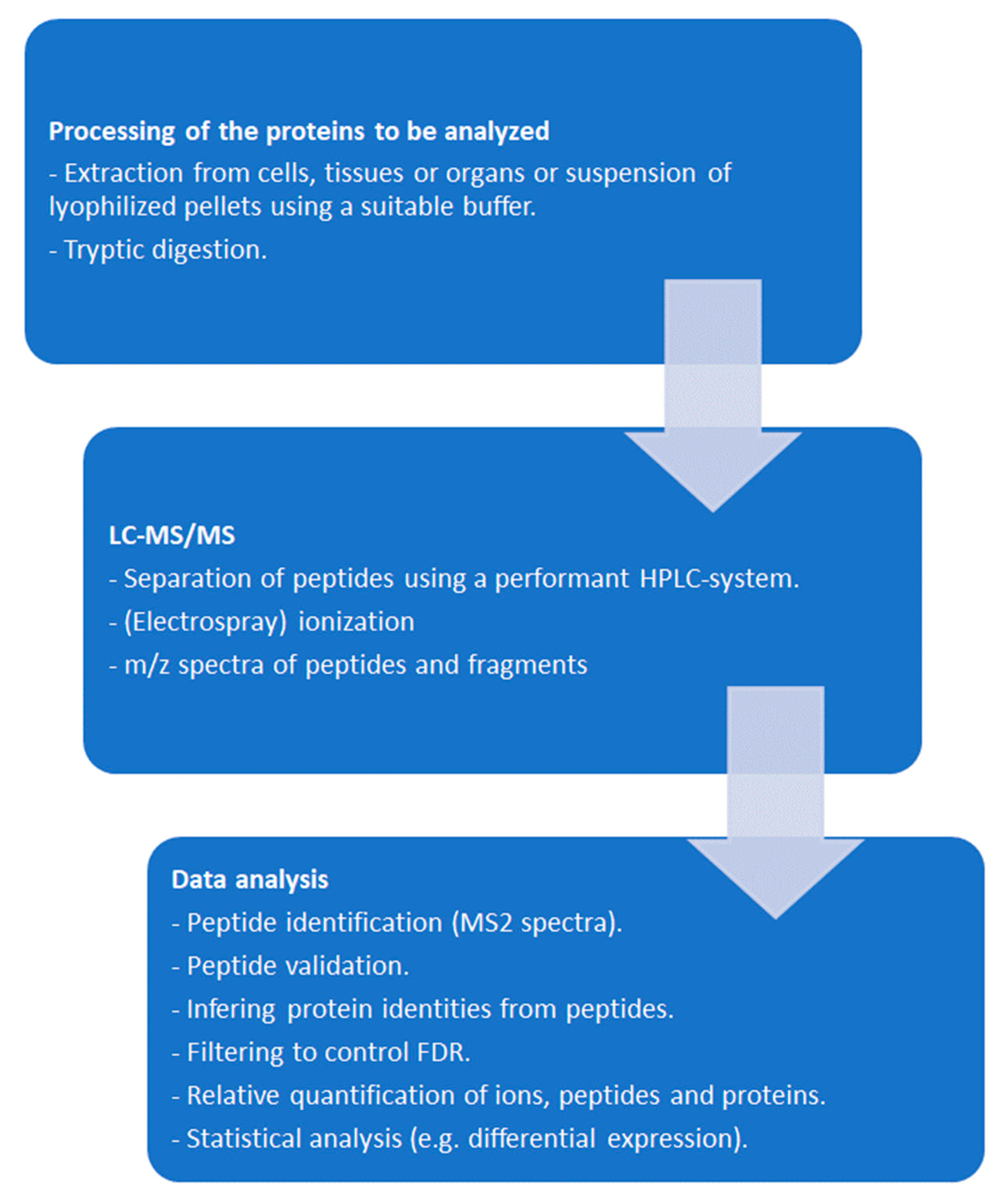
2.3. From Mass Spectra to Protein Data
3. Affinity Based Target Deconvolution
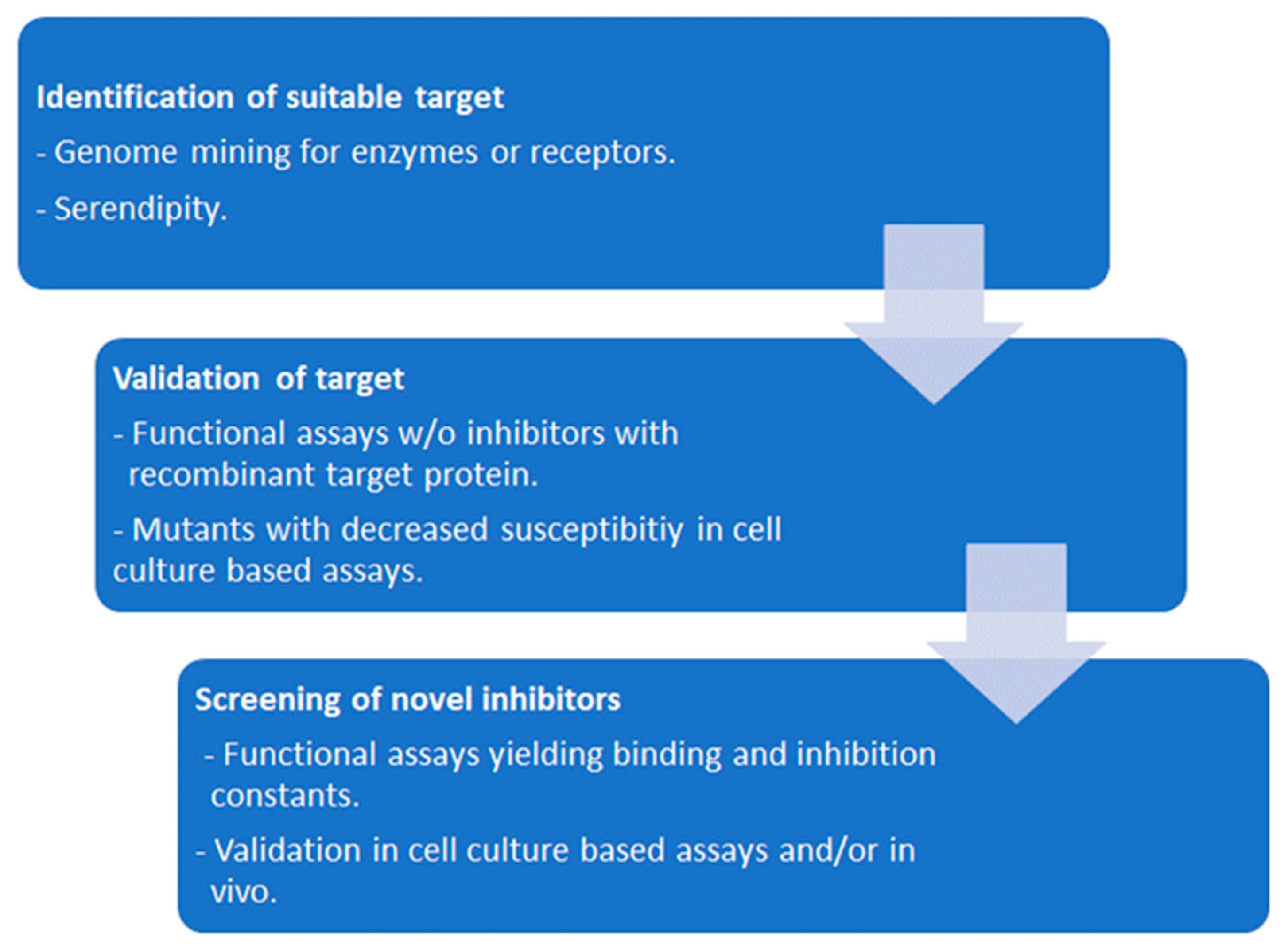
3.1. Functional and Binding Assays Using Isolated Proteins
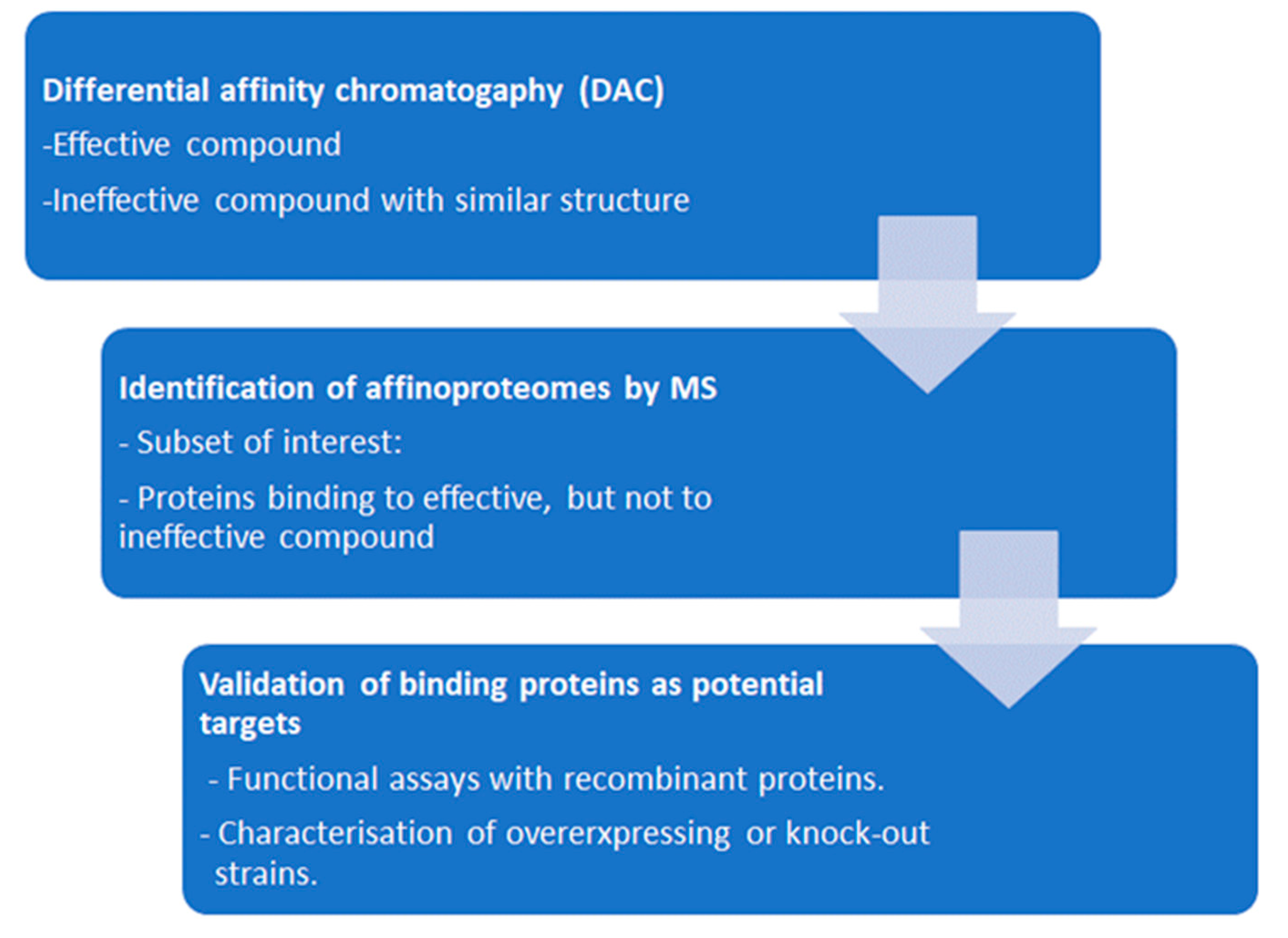
3.2. Affinity Chromatography
3.3. In-Situ-Binding
3.4. Thermal Proteome Profiling
4. Analysis of Resistant Strains
4.1. General Considerations
4.2. Resistance of Transgenic Strains
4.3. Differential Analysis of the Proteomes of Susceptible vs Resistant Strains
5. Combining Evidence from Chemoproteomics and Whole-Cell Proteomics
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lindsay, M.A. Target discovery. Nat Rev Drug Discov 2003, 2, 831–838. [Google Scholar] [CrossRef] [PubMed]
- Paananen, J.; Fortino, V. An omics perspective on drug target discovery platforms. Brief Bioinform 2020, 21, 1937–1953. [Google Scholar] [CrossRef] [PubMed]
- Tsukidate, T.; Li, Q.; Hang, H.C. Targeted and proteome-wide analysis of metabolite-protein interactions. Curr Opin Chem Biol 2020, 54, 19–27. [Google Scholar] [CrossRef] [PubMed]
- Dixon, B.R. Giardia duodenalis in humans and animals - Transmission and disease. Res Vet Sci 2021, 135, 283–289. [Google Scholar] [CrossRef] [PubMed]
- Matta, S.K.; Rinkenberger, N.; Dunay, I.R.; Sibley, L.D. Toxoplasma gondii infection and its implications within the central nervous system. Nat Rev Microbiol 2021, 19, 467–480. [Google Scholar] [CrossRef] [PubMed]
- Ryan, U.M.; Feng, Y.; Fayer, R.; Xiao, L. Taxonomy and molecular epidemiology of Cryptosporidium and Giardia - a 50 year perspective (1971-2021). Int J Parasitol 2021, 51, 1099–1119. [Google Scholar] [CrossRef] [PubMed]
- Marin-Garcia, P.J.; Planas, N.; Llobat, L. Toxoplasma gondii in foods: prevalence, control, and safety. Foods 2022, 11. [Google Scholar] [CrossRef] [PubMed]
- Nayeri, T.; Moosazadeh, M.; Sarvi, S.; Daryani, A. Neospora caninum infection in aborting bovines and lost fetuses: A systematic review and meta-analysis. PLoS One 2022, 17, e0268903. [Google Scholar] [CrossRef] [PubMed]
- Reichel, M.P.; Wahl, L.C.; Ellis, J.T. Research into Neospora caninum-What Have We Learnt in the Last Thirty Years? Pathogens 2020, 9. [Google Scholar] [CrossRef] [PubMed]
- Greenwood, B.M.; Bojang, K.; Whitty, C.J.; Targett, G.A. Malaria. Lancet 2005, 365, 1487–1498. [Google Scholar] [CrossRef] [PubMed]
- Bird, A. Understanding the replication crisis as a base rate fallacy. British Journal for the Philosophy of Science 2021, 72, 965–993. [Google Scholar] [CrossRef]
- Edman, P. A method for the determination of amino acid sequence in peptides. Arch Biochem 1949, 22, 475. [Google Scholar]
- Rabilloud, T. Paleoproteomics explained to youngsters: how did the wedding of two-dimensional electrophoresis and protein sequencing spark proteomics on: let there be light. J Proteomics 2014, 107, 5–12. [Google Scholar] [CrossRef] [PubMed]
- Downard, K.M. Historical account: Francis William Aston: the man behind the mass spectrograph. Eur J Mass Spectrom (Chichester) 2007, 13, 177–190. [Google Scholar] [CrossRef] [PubMed]
- Biemann, K.; Seibl, J.; Gapp, F. Mass spectrometric identification of amino acids. Biochemical and Biophysical Research Communications 1959, 1, 307–311. [Google Scholar] [CrossRef]
- Karas, M.; Bachmann, D.; Hillenkamp, F. Influence of the wavelength in high-irradiance ultraviolet-laser desorption mass-spectrometry of organic-molecules. Analytical Chemistry 1985, 57, 2935–2939. [Google Scholar] [CrossRef]
- Shimada, T.; Toyama, A.; Aoki, C.; Aoki, Y.; Tanaka, K.; Sato, T.A. Direct antigen detection from immunoprecipitated beads using matrix-assisted laser desorption/ionization time-of-flight mass spectrometry; a new method for immunobeads-mass spectrometry (iMS). Rapid Commun Mass Spectrom 2011, 25, 3521–3526. [Google Scholar] [CrossRef] [PubMed]
- Sedo, O.; Roblickova, A.; Jezek, F.; Gintar, P.; Kamenik, J.; Zdrahal, Z. Discriminatory power of MALDI-TOF MS protein profiling analysis of pork meat and meat products. Food Chem 2024, 449, 139155. [Google Scholar] [CrossRef] [PubMed]
- Sun, X.; Wu, P.; Zhao, C.; Zheng, F.; Hu, C.; Lu, X.; Xu, G. Protein profiling analysis based on matrix-assisted laser desorption/ionization-Fourier transform ion cyclotron resonance mass spectrometry and its application in typing Streptomyces isolates. Talanta 2020, 208, 120439. [Google Scholar] [CrossRef] [PubMed]
- Horisawa, S.; Iwamoto, K. Identification and typing of strains of wood-rotting basidiomycetes by protein profiling using MALDI-TOF MS. BioTech (Basel) 2022, 11. [Google Scholar] [CrossRef] [PubMed]
- Chivte, P.; LaCasse, Z.; Seethi, V.D.R.; Bharti, P.; Bland, J.; Kadkol, S.S.; Gaillard, E.R. MALDI-ToF protein profiling as a potential rapid diagnostic platform for COVID-19. J Mass Spectrom Adv Clin Lab 2021, 21, 31–41. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Y.; Tan, C.; Zenobi, R. Rapid profiling of the glycosylation effects on the binding of SARS-CoV-2 spike protein to angiotensin-converting enzyme 2 using MALDI-MS with high mass detection. Anal Chem 2024, 96, 1898–1905. [Google Scholar] [CrossRef] [PubMed]
- Ryan, D.J.; Spraggins, J.M.; Caprioli, R.M. Protein identification strategies in MALDI imaging mass spectrometry: a brief review. Curr Opin Chem Biol 2019, 48, 64–72. [Google Scholar] [CrossRef] [PubMed]
- James, P.; Quadroni, M.; Carafoli, E.; Gonnet, G. Protein identification by mass profile fingerprinting. Biochem Biophys Res Commun 1993, 195, 58–64. [Google Scholar] [CrossRef] [PubMed]
- Michalski, A.; Cox, J.; Mann, M. More than 100,000 detectable peptide species elute in single shotgun proteomics runs but the majority is inaccessible to data-dependent LC-MS/MS. J Proteome Res 2011, 10, 1785–1793. [Google Scholar] [CrossRef] [PubMed]
- Michalski, A.; Damoc, E.; Lange, O.; Denisov, E.; Nolting, D.; Muller, M.; Viner, R.; Schwartz, J.; Remes, P.; Belford, M.; et al. Ultra high resolution linear ion trap Orbitrap mass spectrometer (Orbitrap Elite) facilitates top down LC MS/MS and versatile peptide fragmentation modes. Mol Cell Proteomics 2012, 11, O111–013698. [Google Scholar] [CrossRef] [PubMed]
- Shishkova, E.; Hebert, A.S.; Coon, J.J. Now, more than ever, proteomics needs better chromatography. Cell Syst 2016, 3, 321–324. [Google Scholar] [CrossRef]
- May, J.C.; Goodwin, C.R.; McLean, J.A. Ion mobility-mass spectrometry strategies for untargeted systems, synthetic, and chemical biology. Curr Opin Biotechnol 2015, 31, 117–121. [Google Scholar] [CrossRef] [PubMed]
- Orsburn, B.C. Single cell proteomics by mass spectrometry reveals deep epigenetic insight and new targets of a class specific histone deacetylase inhibitor. bioRxiv 2024. [Google Scholar] [CrossRef] [PubMed]
- Robertson, J.W.F.; Reiner, J.E. The utility of nanopore technology for protein and peptide sensing. Proteomics 2018, 18, e1800026. [Google Scholar] [CrossRef] [PubMed]
- Wei, X.; Penkauskas, T.; Reiner, J.E.; Kennard, C.; Uline, M.J.; Wang, Q.; Li, S.; Aksimentiev, A.; Robertson, J.W.F.; Liu, C. Engineering biological nanopore approaches toward protein sequencing. ACS Nano 2023, 17, 16369–16395. [Google Scholar] [CrossRef] [PubMed]
- Pan, S.; Aebersold, R.; Chen, R.; Rush, J.; Goodlett, D.R.; McIntosh, M.W.; Zhang, J.; Brentnall, T.A. Mass spectrometry based targeted protein quantification: methods and applications. J Proteome Res 2009, 8, 787–797. [Google Scholar] [CrossRef] [PubMed]
- Shuken, S.R. An Introduction to mass spectrometry-based proteomics. J Proteome Res 2023, 22, 2151–2171. [Google Scholar] [CrossRef] [PubMed]
- Yu, F.; Haynes, S.E.; Teo, G.C.; Avtonomov, D.M.; Polasky, D.A.; Nesvizhskii, A.I. Fast quantitative analysis of timsTOF PASEF data with MSFragger and IonQuant. Molecular and Cellular Proteomics 2020, 19, 1575–1585. [Google Scholar] [CrossRef] [PubMed]
- Tyanova, S.; Temu, T.; Cox, J. The MaxQuant computational platform for mass spectrometry-based shotgun proteomics. Nat Protoc 2016, 11, 2301–2319. [Google Scholar] [CrossRef] [PubMed]
- Savitski, M.M.; Wilhelm, M.; Hahne, H.; Kuster, B.; Bantscheff, M. A scalable approach for protein false discovery rate estimation in large proteomic data sets. Mol Cell Proteomics 2015, 14, 2394–2404. [Google Scholar] [CrossRef] [PubMed]
- Yang, K.L.; Yu, F.; Teo, G.C.; Li, K.; Demichev, V.; Ralser, M.; Nesvizhskii, A.I. MSBooster: improving peptide identification rates using deep learning-based features. Nat Commun 2023, 14, 4539. [Google Scholar] [CrossRef] [PubMed]
- Adams, C.; Gabriel, W.; Laukens, K.; Picciani, M.; Wilhelm, M.; Bittremieux, W.; Boonen, K. Fragment ion intensity prediction improves the identification rate of non-tryptic peptides in timsTOF. Nat Commun 2024, 15, 3956. [Google Scholar] [CrossRef] [PubMed]
- Braga-Lagache, S.; Buchs, N.; Iacovache, M.I.; Zuber, B.; Jackson, C.B.; Heller, M. Robust label-free, quantitative profiling of circulating plasma microparticle (MP) associated proteins. Mol Cell Proteomics 2016, 15, 3640–3652. [Google Scholar] [CrossRef] [PubMed]
- Fabre, B.; Lambour, T.; Bouyssié, D.; Menneteau, T.; Monsarrat, B.; Burlet-Schiltz, O.; Bousquet-Dubouch, M.-P. Comparison of label-free quantification methods for the determination of protein complexes subunits stoichiometry. EuPA Open Proteomics 2014, 4, 82–86. [Google Scholar] [CrossRef]
- Macleod, A.K.; Zang, T.; Riches, Z.; Henderson, C.J.; Wolf, C.R.; Huang, J.T. A targeted in vivo SILAC approach for quantification of drug metabolism enzymes: regulation by the constitutive androstane receptor. J Proteome Res 2014, 13, 866–874. [Google Scholar] [CrossRef] [PubMed]
- Dayon, L.; Sanchez, J.C. Relative protein quantification by MS/MS using the tandem mass tag technology. Methods Mol Biol 2012, 893, 115–127. [Google Scholar] [CrossRef] [PubMed]
- Stepath, M.; Zulch, B.; Maghnouj, A.; Schork, K.; Turewicz, M.; Eisenacher, M.; Hahn, S.; Sitek, B.; Bracht, T. Systematic Comparison of Label-Free, SILAC, and TMT Techniques to Study Early Adaption toward Inhibition of EGFR Signaling in the Colorectal Cancer Cell Line DiFi. J Proteome Res 2020, 19, 926–937. [Google Scholar] [CrossRef] [PubMed]
- Tyanova, S.; Temu, T.; Sinitcyn, P.; Carlson, A.; Hein, M.Y.; Geiger, T.; Mann, M.; Cox, J. The Perseus computational platform for comprehensive analysis of (prote)omics data. Nat Methods 2016, 13, 731–740. [Google Scholar] [CrossRef] [PubMed]
- Heller, M.; Braga, S.; Müller, N.; Müller, J. Transfection with plasmid causing stable expression of a foreign gene affects general proteome pattern in Giardia lamblia trophozoites. Front Cell Infect Microbiol 2020, 10, 602756. [Google Scholar] [CrossRef] [PubMed]
- Uldry, A.C.; Maciel-Dominguez, A.; Jornod, M.; Buchs, N.; Braga-Lagache, S.; Brodard, J.; Jankovic, J.; Bonadies, N.; Heller, M. Effect of sample transportation on the proteome of human circulating blood extracellular vesicles. Int J Mol Sci 2022, 23. [Google Scholar] [CrossRef] [PubMed]
- Waduge, P.; Tian, H.; Webster, K.A.; Li, W. Profiling disease-selective drug targets: From proteomics to ligandomics. Drug Discov Today 2023, 28, 103430. [Google Scholar] [CrossRef] [PubMed]
- Neun, S.; Zurek, P.J.; Kaminski, T.S.; Hollfelder, F. Ultrahigh throughput screening for enzyme function in droplets. Methods Enzymol 2020, 643, 317–343. [Google Scholar] [CrossRef] [PubMed]
- Yi, Y.; Zankharia, U.; Cassel, J.A.; Lu, F.; Salvino, J.M.; Lieberman, P.M.; Collman, R.G. A high-throughput screening assay for silencing established HIV-1 macrophage infection identifies nucleoside analogs that perturb H3K9me3 on proviral genomes. J Virol 2023, 97, e0065323. [Google Scholar] [CrossRef] [PubMed]
- Taoda, Y.; Sugiyama, S.; Seki, T. New designs for HIV-1 integrase inhibitors: a patent review (2018-present). Expert Opin Ther Pat 2023, 33, 51–66. [Google Scholar] [CrossRef] [PubMed]
- Montalbano, A.; Sala, C.; Altadonna, G.C.; Becchetti, A.; Arcangeli, A. High throughput clone screening on overexpressed hERG1 and Kv1. 3 potassium channels using ion channel reader (ICR) label free technology. Heliyon 2023, 9, e20112. [Google Scholar] [CrossRef] [PubMed]
- Diaz, G.J.; Daniell, K.; Leitza, S.T.; Martin, R.L.; Su, Z.; McDermott, J.S.; Cox, B.F.; Gintant, G.A. The [3H]dofetilide binding assay is a predictive screening tool for hERG blockade and proarrhythmia: Comparison of intact cell and membrane preparations and effects of altering [K+]o. J Pharmacol Toxicol Methods 2004, 50, 187–199. [Google Scholar] [CrossRef] [PubMed]
- Sichler, S.; Hofner, G.; Nitsche, V.; Niessen, K.V.; Seeger, T.; Worek, F.; Paintner, F.F.; Wanner, K.T. Screening for new ligands of the MB327-PAM-1 binding site of the nicotinic acetylcholine receptor. Toxicol Lett 2024. [Google Scholar] [CrossRef] [PubMed]
- Loo, C.S.; Lam, N.S.; Yu, D.; Su, X.Z.; Lu, F. Artemisinin and its derivatives in treating protozoan infections beyond malaria. Pharmacol Res 2017, 117, 192–217. [Google Scholar] [CrossRef] [PubMed]
- Tu, Y. The discovery of artemisinin (qinghaosu) and gifts from Chinese medicine. Nat Med 2011, 17, 1217–1220. [Google Scholar] [CrossRef] [PubMed]
- Müller, J.; Hemphill, A. Toxoplasma gondii infection: novel emerging therapeutic targets. Expert Opin Ther Targets 2023, 27, 293–304. [Google Scholar] [CrossRef] [PubMed]
- Kurganov, B.I. Kinetics of protein aggregation. Quantitative estimation of the chaperone-like activity in test-systems based on suppression of protein aggregation. Biochemistry (Mosc) 2002, 67, 409–422. [Google Scholar] [CrossRef] [PubMed]
- Kassack, M.U. Quantitative comparison of functional screening by measuring intracellular Ca2+ with radioligand binding at recombinant human dopamine receptors. AAPS PharmSci 2002, 4, E31. [Google Scholar] [CrossRef] [PubMed]
- Oostendorp, J.; Meurs, H.; Adriaan Nelemans, S.; Zaagsma, J.; Kauffman, H.F.; Postma, D.S.; Boddeke, H.W.; Biber, K. Cloning, pharmacological characterization, and polymorphism screening of the guinea pig beta(2)-adrenoceptor. Eur J Pharmacol 2002, 457, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Tamaki, F.; Fisher, F.; Milne, R.; Teran, F.S.; Wiedemar, N.; Wrobel, K.; Edwards, D.; Baumann, H.; Gilbert, I.H.; Baragana, B.; et al. High-throughput screening platform to identify inhibitors of protein synthesis with potential for the treatment of malaria. Antimicrob Agents Chemother 2022, 66, e0023722. [Google Scholar] [CrossRef] [PubMed]
- Ojo, K.K.; Larson, E.T.; Keyloun, K.R.; Castaneda, L.J.; Derocher, A.E.; Inampudi, K.K.; Kim, J.E.; Arakaki, T.L.; Murphy, R.C.; Zhang, L.; et al. Toxoplasma gondii calcium-dependent protein kinase 1 is a target for selective kinase inhibitors. Nature Structural & Molecular Biology 2010, 17, 602–607. [Google Scholar] [CrossRef] [PubMed]
- Johnson, S.M.; Murphy, R.C.; Geiger, J.A.; DeRocher, A.E.; Zhang, Z.; Ojo, K.K.; Larson, E.T.; Perera, B.G.; Dale, E.J.; He, P.; et al. Development of Toxoplasma gondii calcium-dependent protein kinase 1 (TgCDPK1) inhibitors with potent anti-toxoplasma activity. J Med Chem 2012, 55, 2416–2426. [Google Scholar] [CrossRef] [PubMed]
- Vanichtanankul, J.; Yoomuang, A.; Taweechai, S.; Saeyang, T.; Pengon, J.; Yuvaniyama, J.; Tarnchompoo, B.; Yuthavong, Y.; Kamchonwongpaisan, S. Structural insight into effective inhibitors binding to Toxoplasma gondii dihydrofolate reductase thymidylate synthase. ACS Chem Biol 2022, 17, 1691–1702. [Google Scholar] [CrossRef] [PubMed]
- Djapa, L.Y.; Basco, L.K.; Zelikson, R.; Rosowsky, A.; Djaman, J.A.; Yonkeu, J.N.; Bolotin-Fukuhara, M.; Mazabraud, A. Antifolate screening using yeast expressing Plasmodium vivax dihydrofolate reductase and in vitro drug susceptibility assay for Plasmodium falciparum. Mol Biochem Parasitol 2007, 156, 89–92. [Google Scholar] [CrossRef]
- Jelenska, J.; Sirikhachornkit, A.; Haselkorn, R.; Gornicki, P. The carboxyltransferase activity of the apicoplast acetyl-CoA carboxylase of Toxoplasma gondii is the target of aryloxyphenoxypropionate inhibitors. J Biol Chem 2002, 277, 23208–23215. [Google Scholar] [CrossRef] [PubMed]
- Goo, Y.K.; Yamagishi, J.; Ueno, A.; Terkawi, M.A.; Aboge, G.O.; Kwak, D.; Hong, Y.; Chung, D.I.; Igarashi, M.; Nishikawa, Y.; et al. Characterization of Toxoplasma gondii glyoxalase 1 and evaluation of inhibitory effects of curcumin on the enzyme and parasite cultures. Parasit Vectors 2015, 8, 654. [Google Scholar] [CrossRef] [PubMed]
- Lin, S.S.; Kerscher, S.; Saleh, A.; Brandt, U.; Gross, U.; Bohne, W. The Toxoplasma gondii type-II NADH dehydrogenase TgNDH2-I is inhibited by 1-hydroxy-2-alkyl-4(1H)quinolones. Biochim Biophys Acta 2008, 1777, 1455–1462. [Google Scholar] [CrossRef] [PubMed]
- Harada, M.; Nagai, J.; Kurata, R.; Shimizu, K.; Cui, X.; Isagawa, T.; Semba, H.; Ishihara, J.; Yoshida, Y.; Takeda, N.; et al. Establishment of novel high-standard chemiluminescent assay for NTPase in two protozoans and its high-throughput screening. Mar Drugs 2020, 18. [Google Scholar] [CrossRef] [PubMed]
- Razakantoanina, V.; Florent, I.; Jaureguiberry, G. Plasmodium falciparum: functional mitochondrial ADP/ATP transporter in Escherichia coli plasmic membrane as a tool for selective drug screening. Exp Parasitol 2008, 118, 181–187. [Google Scholar] [CrossRef] [PubMed]
- Walunj, S.B.; Dias, M.M.; Kaur, C.; Wagstaff, K.M.; Dey, V.; Hick, C.; Patankar, S.; Jans, D.A. High-throughput screening to identify inhibitors of Plasmodium falciparum importin alpha. Cells 2022, 11. [Google Scholar] [CrossRef] [PubMed]
- Radke, J.B.; Melillo, B.; Mittal, P.; Sharma, M.; Sharma, A.; Fu, Y.; Uddin, T.; Gonse, A.; Comer, E.; Schreiber, S.L.; et al. Bicyclic azetidines target acute and chronic stages of Toxoplasma gondii by inhibiting parasite phenylalanyl t-RNA synthetase. Nat Commun 2022, 13, 459. [Google Scholar] [CrossRef]
- Bosch, S.S.; Lunev, S.; Batista, F.A.; Linzke, M.; Kronenberger, T.; Domling, A.S.S.; Groves, M.R.; Wrenger, C. Molecular target validation of aspartate transcarbamoylase from Plasmodium falciparum by Torin 2. ACS Infect Dis 2020, 6, 986–999. [Google Scholar] [CrossRef] [PubMed]
- Batista, F.A.; Gyau, B.; Vilacha, J.F.; Bosch, S.S.; Lunev, S.; Wrenger, C.; Groves, M.R. New directions in antimalarial target validation. Expert Opin Drug Discov 2020, 15, 189–202. [Google Scholar] [CrossRef] [PubMed]
- Xu, F.; Jex, A.; Svard, S.G. A chromosome-scale reference genome for Giardia intestinalis WB. Sci Data 2020, 7, 38. [Google Scholar] [CrossRef] [PubMed]
- Kunz, S.; Balmer, V.; Sterk, G.J.; Pollastri, M.P.; Leurs, R.; Müller, N.; Hemphill, A.; Spycher, C. The single cyclic nucleotide-specific phosphodiesterase of the intestinal parasite Giardia lamblia represents a potential drug target. PLoS Negl Trop Dis 2017, 11, e0005891. [Google Scholar] [CrossRef] [PubMed]
- Müller, J.; Braga, S.; Uldry, A.C.; Heller, M.; Müller, N. Comparative proteomics of three Giardia lamblia strains: investigation of antigenic variation in the post-genomic era. Parasitology 2020, 147, 1008–1018. [Google Scholar] [CrossRef] [PubMed]
- Zheng, Y.; Müller, J.; Kunz, S.; Siderius, M.; Maes, L.; Caljon, G.; Müller, N.; Hemphill, A.; Sterk, G.J.; Leurs, R. 3-nitroimidazo[1,2-b]pyridazine as a novel scaffold for antiparasitics with sub-nanomolar anti-Giardia lamblia activity. Int J Parasitol Drugs Drug Resist 2022, 19, 47–55. [Google Scholar] [CrossRef] [PubMed]
- Leitsch, D. A review on metronidazole: an old warhorse in antimicrobial chemotherapy. Parasitology 2017, 146, 1167–1178. [Google Scholar] [CrossRef] [PubMed]
- Bailey, B.L.; Nguyen, W.; Cowman, A.F.; Sleebs, B.E. Chemo-proteomics in antimalarial target identification and engagement. Med Res Rev 2023, 43, 2303–2351. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Zhang, J.; Li, M.; Qiao, Y.; Wang, W.; Ma, L.; Liu, K. Target discovery of bioactive natural products with native-compound-coupled CNBr-activated Sepharose 4B beads (NCCB): Applications, mechanisms and outlooks. Bioorg Med Chem 2023, 96, 117483. [Google Scholar] [CrossRef] [PubMed]
- Lechner, S.; Malgapo, M.I.P.; Gratz, C.; Steimbach, R.R.; Baron, A.; Ruther, P.; Nadal, S.; Stumpf, C.; Loos, C.; Ku, X.; et al. Target deconvolution of HDAC pharmacopoeia reveals MBLAC2 as common off-target. Nat Chem Biol 2022, 18, 812–820. [Google Scholar] [CrossRef] [PubMed]
- O’Carra, P.; Barry, S.; Griffin, T. Spacer arms in affinity chromatography: use of hydrophilic arms to control or eliminate nonbiospecific adsorption effects. FEBS Lett 1974, 43, 169–175. [Google Scholar] [CrossRef] [PubMed]
- Spratt, B.G.; Pardee, A.B. Penicillin-binding proteins and cell shape in E. coli. Nature 1975, 254, 516–517. [Google Scholar] [CrossRef] [PubMed]
- Spratt, B.G. Distinct penicillin binding proteins involved in the division, elongation, and shape of Escherichia coli K12. Proc Natl Acad Sci U S A 1975, 72, 2999–3003. [Google Scholar] [CrossRef] [PubMed]
- Curtis, S.J.; Strominger, J.L. Purification of penicillin-binding protein 2 of Escherichia coli. J Bacteriol 1981, 145, 398–403. [Google Scholar] [CrossRef] [PubMed]
- Knockaert, M.; Gray, N.; Damiens, E.; Chang, Y.T.; Grellier, P.; Grant, K.; Fergusson, D.; Mottram, J.; Soete, M.; Dubremetz, J.F.; et al. Intracellular targets of cyclin-dependent kinase inhibitors: identification by affinity chromatography using immobilised inhibitors. Chem Biol 2000, 7, 411–422. [Google Scholar] [CrossRef] [PubMed]
- Graves, P.R.; Kwiek, J.J.; Fadden, P.; Ray, R.; Hardeman, K.; Coley, A.M.; Foley, M.; Haystead, T.A. Discovery of novel targets of quinoline drugs in the human purine binding proteome. Mol Pharmacol 2002, 62, 1364–1372. [Google Scholar] [CrossRef] [PubMed]
- Morita, M.; Sanai, H.; Hiramoto, A.; Sato, A.; Hiraoka, O.; Sakura, T.; Kaneko, O.; Masuyama, A.; Nojima, M.; Wataya, Y.; et al. Plasmodium falciparum endoplasmic reticulum-resident calcium binding protein is a possible target of synthetic antimalarial endoperoxides, N-89 and N-251. J Proteome Res 2012, 11, 5704–5711. [Google Scholar] [CrossRef]
- Müller, J.; Wastling, J.; Sanderson, S.; Müller, N.; Hemphill, A. A novel Giardia lamblia nitroreductase, GlNR1, interacts with nitazoxanide and other thiazolides. Antimicrob Agents Chemother 2007, 51, 1979–1986. [Google Scholar] [CrossRef] [PubMed]
- Müller, J.; Rout, S.; Leitsch, D.; Vaithilingam, J.; Hehl, A.; Müller, N. Comparative characterisation of two nitroreductases from Giardia lamblia as potential activators of nitro compounds. Int J Parasitol Drugs Drug Resist 2015, 5, 37–43. [Google Scholar] [CrossRef] [PubMed]
- Müller, J.; Müller, N. Nitroreductases of bacterial origin in Giardia lamblia: Potential role in detoxification of xenobiotics. Microbiologyopen 2019, e904. [Google Scholar] [CrossRef] [PubMed]
- Müller, J.; Sidler, D.; Nachbur, U.; Wastling, J.; Brunner, T.; Hemphill, A. Thiazolides inhibit growth and induce glutathione-S-transferase Pi (GSTP1)-dependent cell death in human colon cancer cells. Int J Cancer 2008, 123, 1797–1806. [Google Scholar] [CrossRef] [PubMed]
- Sidler, D.; Brockmann, A.; Müller, J.; Nachbur, U.; Corazza, N.; Renzulli, P.; Hemphill, A.; Brunner, T. Thiazolide-induced apoptosis in colorectal cancer cells is mediated via the Jun kinase-Bim axis and reveals glutathione-S-transferase P1 as Achilles’ heel. Oncogene 2012, 31, 4095–4106. [Google Scholar] [CrossRef] [PubMed]
- Müller, J.; Hemphill, A. Identification of a host cell target for the thiazolide class of broad-spectrum anti-parasitic drugs. Exp Parasitol 2011, 128, 145–150. [Google Scholar] [CrossRef] [PubMed]
- Basto, A.P.; Müller, J.; Rubbiani, R.; Stibal, D.; Giannini, F.; Suss-Fink, G.; Balmer, V.; Hemphill, A.; Gasser, G.; Furrer, J. Characterization of the activities of dinuclear thiolato-bridged arene ruthenium complexes against Toxoplasma gondii. Antimicrob Agents Chemother 2017, 61. [Google Scholar] [CrossRef] [PubMed]
- Anghel, N.; Müller, J.; Serricchio, M.; Jelk, J.; Butikofer, P.; Boubaker, G.; Imhof, D.; Ramseier, J.; Desiatkina, O.; Paunescu, E.; et al. Cellular and molecular targets of nucleotide-tagged trithiolato-bridged arene ruthenium complexes in the protozoan parasites Toxoplasma gondii and Trypanosoma brucei. Int J Mol Sci 2021, 22. [Google Scholar] [CrossRef] [PubMed]
- Müller, J.; Boubaker, G.; Imhof, D.; Hanggeli, K.; Haudenschild, N.; Uldry, A.C.; Braga-Lagache, S.; Heller, M.; Ortega-Mora, L.M.; Hemphill, A. Differential affinity chromatography coupled to mass spectrometry: A suitable tool to identify common binding proteins of a broad-range antimicrobial peptide derived from leucinostatin. Biomedicines 2022, 10. [Google Scholar] [CrossRef] [PubMed]
- Müller, J.; Anghel, N.; Imhof, D.; Hänggeli, K.; Uldry, A.C.; Braga-Lagache, S.; Heller, M.; Ojo, K.K.; Ortega-Mora, L.M.; Van Voorhis, W.C.; et al. Common molecular targets of a quinoline based bumped kinase inhibitor in Neospora caninum and Danio rerio. Int J Mol Sci 2022, 23, 2381–2399. [Google Scholar] [CrossRef] [PubMed]
- Ajiboye, J.; Uldry, A.C.; Heller, M.; Naguleswaran, A.; Fan, E.; Van Voorhis, W.C.; Hemphill, A.; Müller, J. Molecular targets of the 5-amido-carboxamide bumped kinase inhibitor BKI-1748 in Cryptosporidium parvum and HCT-8 Host Cells. Int J Mol Sci 2024, 25. [Google Scholar] [CrossRef]
- Yang, K.S.; Budin, G.; Tassa, C.; Kister, O.; Weissleder, R. Bioorthogonal approach to identify unsuspected drug targets in live cells. Angew Chem Int Ed Engl 2013, 52, 10593–10597. [Google Scholar] [CrossRef] [PubMed]
- Kusza, D.A.; Hunter, R.; Schafer, G.; Smith, M.; Katz, A.A.; Kaschula, C.H. Activity-based proteomic identification of the S-thiolation targets of ajoene in MDA-MB-231 breast cancer cells. J Agric Food Chem 2022, 70, 14679–14692. [Google Scholar] [CrossRef] [PubMed]
- Tang, J.; Sun, Q.; Xie, Y.; Zheng, Q.; Ding, Y. Virus-like iron-gold heterogeneous nanoparticles for drug target screening. Anal Chem 2023, 95, 17187–17192. [Google Scholar] [CrossRef] [PubMed]
- Seo, S.Y.; Corson, T.W. Small molecule target identification using photo-affinity chromatography. Methods Enzymol 2019, 622, 347–374. [Google Scholar] [CrossRef] [PubMed]
- Penarete-Vargas, D.M.; Boisson, A.; Urbach, S.; Chantelauze, H.; Peyrottes, S.; Fraisse, L.; Vial, H.J. A chemical proteomics approach for the search of pharmacological targets of the antimalarial clinical candidate albitiazolium in Plasmodium falciparum using photocrosslinking and click chemistry. PLoS One 2014, 9, e113918. [Google Scholar] [CrossRef] [PubMed]
- Ismail, H.M.; Barton, V.; Phanchana, M.; Charoensutthivarakul, S.; Wong, M.H.; Hemingway, J.; Biagini, G.A.; O’Neill, P.M.; Ward, S.A. Artemisinin activity-based probes identify multiple molecular targets within the asexual stage of the malaria parasites Plasmodium falciparum 3D7. Proc Natl Acad Sci U S A 2016, 113, 2080–2085. [Google Scholar] [CrossRef]
- Lubin, A.S.; Rueda-Zubiaurre, A.; Matthews, H.; Baumann, H.; Fisher, F.R.; Morales-Sanfrutos, J.; Hadavizadeh, K.S.; Nardella, F.; Tate, E.W.; Baum, J.; et al. Development of a photo-cross-linkable diaminoquinazoline inhibitor for target identification in Plasmodium falciparum. ACS Infect Dis 2018, 4, 523–530. [Google Scholar] [CrossRef] [PubMed]
- Lisauskaite, M.; Nixon, G.L.; Woodley, C.M.; Berry, N.G.; Coninckx, A.; Qie, L.C.; Leung, S.C.; Taramelli, D.; Basilico, N.; Parapini, S.; et al. Design, synthesis and modelling of photoreactive chemical probes for investigating target engagement of plasmepsin IX and X in Plasmodium falciparum. RSC Chem Biol 2024, 5, 19–29. [Google Scholar] [CrossRef] [PubMed]
- Luan, C.H.; Light, S.H.; Dunne, S.F.; Anderson, W.F. Ligand screening using fluorescence thermal shift analysis (FTS). Methods Mol Biol 2014, 1140, 263–289. [Google Scholar] [CrossRef] [PubMed]
- Jafari, R.; Almqvist, H.; Axelsson, H.; Ignatushchenko, M.; Lundback, T.; Nordlund, P.; Martinez Molina, D. The cellular thermal shift assay for evaluating drug target interactions in cells. Nat Protoc 2014, 9, 2100–2122. [Google Scholar] [CrossRef] [PubMed]
- Molina, D.M.; Jafari, R.; Ignatushchenko, M.; Seki, T.; Larsson, E.A.; Dan, C.; Sreekumar, L.; Cao, Y.H.; Nordlund, P. Monitoring drug target engagement in cells and tissues using the cellular thermal shift assay. Science 2013, 341, 84–87. [Google Scholar] [CrossRef] [PubMed]
- Muroi, M.; Osada, H. Two-dimensional electrophoresis-cellular thermal shift assay (2DE-CETSA) for target identification of bioactive compounds. Methods Enzymol 2022, 675, 425–437. [Google Scholar] [CrossRef] [PubMed]
- Friman, T. Mass spectrometry-based cellular thermal shift assay (CETSA(R)) for target deconvolution in phenotypic drug discovery. Bioorg Med Chem 2020, 28, 115174. [Google Scholar] [CrossRef] [PubMed]
- Sauer, P.; Bantscheff, M. Thermal proteome profiling for drug target identification and probing of protein states. Methods Mol Biol 2023, 2718, 73–98. [Google Scholar] [CrossRef] [PubMed]
- George, A.L.; Sidgwick, F.R.; Watt, J.E.; Martin, M.P.; Trost, M.; Marin-Rubio, J.L.; Duenas, M.E. Comparison of quantitative mass spectrometric methods for drug target identification by thermal proteome profiling. J Proteome Res 2023, 22, 2629–2640. [Google Scholar] [CrossRef] [PubMed]
- Shi, Z.; Ren, Y.; Li, S.; Hao, P. Identifying drug targets with thermal proteome profiling using IBT-16plex. Rapid Commun Mass Spectrom 2024, 38, e9673. [Google Scholar] [CrossRef] [PubMed]
- Savitski, M.M.; Reinhard, F.B.M.; Franken, H.; Werner, T.; Savitski, M.F.; Eberhard, D.; Molina, D.M.; Jafari, R.; Dovega, R.B.; Klaeger, S.; et al. Tracking cancer drugs in living cells by thermal profiling of the proteome. Science 2014, 346, 55-+, ARTN 1255784. [Google Scholar] [CrossRef]
- Ball, K.A.; Webb, K.J.; Coleman, S.J.; Cozzolino, K.A.; Jacobsen, J.; Jones, K.R.; Stowell, M.H.B.; Old, W.M. An isothermal shift assay for proteome scale drug-target identification. Commun Biol 2020, 3, 75. [Google Scholar] [CrossRef] [PubMed]
- Zijlmans, D.W.; Hernandez-Quiles, M.; Jansen, P.; Becher, I.; Stein, F.; Savitski, M.M.; Vermeulen, M. STPP-UP: An alternative method for drug target identification using protein thermal stability. J Biol Chem 2023, 299, 105279. [Google Scholar] [CrossRef] [PubMed]
- Kalxdorf, M.; Gunthner, I.; Becher, I.; Kurzawa, N.; Knecht, S.; Savitski, M.M.; Eberl, H.C.; Bantscheff, M. Cell surface thermal proteome profiling tracks perturbations and drug targets on the plasma membrane. Nat Methods 2021, 18, 84–91. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Hu, L.; Ye, M. Solvent-induced protein precipitation for drug target discovery. Methods Mol Biol 2023, 2554, 35–45. [Google Scholar] [CrossRef] [PubMed]
- Paradela, L.S.; Wall, R.J.; Carvalho, S.; Chemi, G.; Corpas-Lopez, V.; Moynihan, E.; Bello, D.; Patterson, S.; Guther, M.L.S.; Fairlamb, A.H.; et al. Multiple unbiased approaches identify oxidosqualene cyclase as the molecular target of a promising anti-leishmanial. Cell Chem Biol 2021, 28, 711–721 e718. [Google Scholar] [CrossRef] [PubMed]
- Corpas-Lopez, V.; Wyllie, S. Utilizing thermal proteome profiling to identify the molecular targets of anti-leishmanial compounds. STAR Protoc 2021, 2, 100704. [Google Scholar] [CrossRef] [PubMed]
- Ibarra-Meneses, A.V.; Corbeil, A.; Wagner, V.; Beaudry, F.; do Monte-Neto, R.L.; Fernandez-Prada, C. Exploring direct and indirect targets of current antileishmanial drugs using a novel thermal proteomics profiling approach. Front Cell Infect Microbiol 2022, 12, 954144. [Google Scholar] [CrossRef] [PubMed]
- Dziekan, J.M.; Wirjanata, G.; Dai, L.; Go, K.D.; Yu, H.; Lim, Y.T.; Chen, L.; Wang, L.C.; Puspita, B.; Prabhu, N.; et al. Cellular thermal shift assay for the identification of drug-target interactions in the Plasmodium falciparum proteome. Nat Protoc 2020, 15, 1881–1921. [Google Scholar] [CrossRef] [PubMed]
- Herneisen, A.L.; Sidik, S.M.; Markus, B.M.; Drewry, D.H.; Zuercher, W.J.; Lourido, S. Identifying the target of an antiparasitic compound in Toxoplasma using thermal proteome profiling. ACS Chem Biol 2020, 15, 1801–1807. [Google Scholar] [CrossRef] [PubMed]
- Becher, I.; Andres-Pons, A.; Romanov, N.; Stein, F.; Schramm, M.; Baudin, F.; Helm, D.; Kurzawa, N.; Mateus, A.; Mackmull, M.T.; et al. Pervasive protein thermal stability variation during the cell cycle. Cell 2018, 173, 1495–1507 e1418. [Google Scholar] [CrossRef] [PubMed]
- Müller, J.; Hemphill, A. In vitro screening technologies for the discovery and development of novel drugs against Toxoplasma gondii. Expert Opin Drug Discov 2024, 19, 97–109. [Google Scholar] [CrossRef] [PubMed]
- Tjorve, K.M.C.; Tjorve, E. The use of Gompertz models in growth analyses, and new Gompertz-model approach: An addition to the Unified-Richards family. PLoS One 2017, 12, e0178691. [Google Scholar] [CrossRef] [PubMed]
- Brauner, A.; Fridman, O.; Gefen, O.; Balaban, N.Q. Distinguishing between resistance, tolerance and persistence to antibiotic treatment. Nat Rev Microbiol 2016, 14, 320–330. [Google Scholar] [CrossRef] [PubMed]
- Müller, J.; Hemphill, A.; Müller, N. Physiological aspects of nitro drug resistance in Giardia lamblia. Int J Parasitol Drugs Drug Resist 2018, 8, 271–277. [Google Scholar] [CrossRef] [PubMed]
- Müller, J.; Schlange, C.; Heller, M.; Uldry, A.C.; Braga-Lagache, S.; Haynes, R.K.; Hemphill, A. Proteomic characterization of Toxoplasma gondii ME49 derived strains resistant to the artemisinin derivatives artemiside and artemisone implies potential mode of action independent of ROS formation. Int J Parasitol Drugs Drug Resist 2022, 21, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Wellems, T.E.; Sá, J.M.; Su, X.Z.; Connelly, S.V.; Ellis, A.C. ’Artemisinin Resistance’: Something New or Old? Something of a Misnomer? Trends in Parasitology 2020, 36, 735–744. [Google Scholar] [CrossRef] [PubMed]
- Yu, X.; Wang, C.; Zhao, Y.; Tang, J.; Zhu, M.; Platon, L.; Culleton, R.; Zhu, G.; Menard, D.; Zhang, Q.; et al. Ring-stage growth arrest: Metabolic basis of artemisinin tolerance in Plasmodium falciparum. iScience 2023, 26, 105725. [Google Scholar] [CrossRef] [PubMed]
- Winzer, P.; Anghel, N.; Imhof, D.; Balmer, V.; Ortega-Mora, L.M.; Ojo, K.K.; Van Voorhis, W.C.; Müller, J.; Hemphill, A. Neospora caninum: Structure and Fate of Multinucleated Complexes Induced by the Bumped Kinase Inhibitor BKI-1294. Pathogens 2020, 9. [Google Scholar] [CrossRef] [PubMed]
- Winzer, P.; Müller, J.; Imhof, D.; Ritler, D.; Uldry, A.C.; Braga-Lagache, S.; Heller, M.; Ojo, K.K.; Van Voorhis, W.C.; Ortega-Mora, L.M.; et al. Neospora caninum: Differential Proteome of Multinucleated Complexes Induced by the Bumped Kinase Inhibitor BKI-1294. Microorganisms 2020, 8. [Google Scholar] [CrossRef]
- Jerlström-Hultqvist, J.; Stadelmann, B.; Birkestedt, S.; Hellman, U.; Svärd, S.G. Plasmid vectors for proteomic analyses in Giardia: purification of virulence factors and analysis of the proteasome. Eukaryot Cell 2012, 11, 864–873. [Google Scholar] [CrossRef] [PubMed]
- Meissner, M.; Breinich, M.S.; Gilson, P.R.; Crabb, B.S. Molecular genetic tools in Toxoplasma and Plasmodium: achievements and future needs. Curr Opin Microbiol 2007, 10, 349–356. [Google Scholar] [CrossRef] [PubMed]
- Carucci, D.J. Technologies for the study of gene and protein expression in Plasmodium. Philos Trans R Soc Lond B Biol Sci 2002, 357, 13–16. [Google Scholar] [CrossRef]
- Donald, R.G.; Roos, D.S. Stable molecular transformation of Toxoplasma gondii: a selectable dihydrofolate reductase-thymidylate synthase marker based on drug-resistance mutations in malaria. Proc Natl Acad Sci U S A 1993, 90, 11703–11707. [Google Scholar] [CrossRef] [PubMed]
- Howe, D.K.; Sibley, L.D. Development of molecular genetics for Neospora caninum: A complementary system to Toxoplasma gondii. Methods 1997, 13, 123–133. [Google Scholar] [CrossRef] [PubMed]
- Ullu, E.; Tschudi, C.; Chakraborty, T. RNA interference in protozoan parasites. Cell Microbiol 2004, 6, 509–519. [Google Scholar] [CrossRef] [PubMed]
- Sidik, S.M.; Hackett, C.G.; Tran, F.; Westwood, N.J.; Lourido, S. Efficient genome engineering of Toxoplasma gondii using CRISPR/Cas9. PLoS One 2014, 9, e100450. [Google Scholar] [CrossRef] [PubMed]
- Shen, B.; Brown, K.M.; Lee, T.D.; Sibley, L.D. Efficient gene disruption in diverse strains of Toxoplasma gondii using CRISPR/CAS9. MBio 2014, 5, e01114–01114. [Google Scholar] [CrossRef] [PubMed]
- Sidik, S.M.; Huet, D.; Ganesan, S.M.; Huynh, M.H.; Wang, T.; Nasamu, A.S.; Thiru, P.; Saeij, J.P.; Carruthers, V.B.; Niles, J.C.; et al. A Genome-wide CRISPR screen in Toxoplasma Identifies essential apicomplexan genes. Cell 2016, 166, 1423–1435 e1412. [Google Scholar] [CrossRef] [PubMed]
- Castaneda-Barba, S.; Top, E.M.; Stalder, T. Plasmids, a molecular cornerstone of antimicrobial resistance in the One Health era. Nat Rev Microbiol 2024, 22, 18–32. [Google Scholar] [CrossRef] [PubMed]
- Leitsch, D.; Williams, C.F.; Hrdy, I. Redox pathways as drug targets in microaerophilic parasites. Trends Parasitol 2018, 34, 576–589. [Google Scholar] [CrossRef] [PubMed]
- Müller, J.; Heller, M.; Uldry, A.C.; Braga, S.; Müller, N. Nitroreductase activites in Giardia lamblia: ORF 17150 encodes a quinone reductase with nitroreductase activity. Pathogens 2021, 10. [Google Scholar] [CrossRef] [PubMed]
- Palmer, A.C.; Kishony, R. Opposing effects of target overexpression reveal drug mechanisms. Nat Commun 2014, 5, 4296. [Google Scholar] [CrossRef] [PubMed]
- Hanggeli, K.P.A.; Hemphill, A.; Müller, N.; Heller, M.; Uldry, A.C.; Braga-Lagache, S.; Müller, J.; Boubaker, G. Comparative proteomic analysis of Toxoplasma gondii RH wild-type and four SRS29B (SAG1) knock-out clones reveals significant differences between individual strains. Int J Mol Sci 2023, 24. [Google Scholar] [CrossRef] [PubMed]
- Freisleben, F.; Behrmann, L.; Thaden, V.; Muschhammer, J.; Bokemeyer, C.; Fiedler, W.; Wellbrock, J. Downregulation of GLI3 expression mediates chemotherapy resistance in acute myeloid leukemia. Int J Mol Sci 2020, 21. [Google Scholar] [CrossRef] [PubMed]
- de Koning, H.P. Drug resistance in protozoan parasites. Emerg Top Life Sci 2017, 1, 627–632. [Google Scholar] [CrossRef] [PubMed]
- Gardner, M.J.; Hall, N.; Fung, E.; White, O.; Berriman, M.; Hyman, R.W.; Carlton, J.M.; Pain, A.; Nelson, K.E.; Bowman, S.; et al. Genome sequence of the human malaria parasite Plasmodium falciparum. Nature 2002, 419, 498–511. [Google Scholar] [CrossRef] [PubMed]
- Cooper, R.A.; Carucci, D.J. Proteomic approaches to studying drug targets and resistance in Plasmodium. Curr Drug Targets Infect Disord 2004, 4, 41–51. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.; Huang, F.; Yan, H.; Yin, J.; Xia, Z. A review of malaria molecular markers for drug resistance in Plasmodium falciparum and Plasmodium vivax in China. Front Cell Infect Microbiol 2023, 13, 1167220. [Google Scholar] [CrossRef] [PubMed]
- Pandit, K.; Surolia, N.; Bhattacharjee, S.; Karmodiya, K. The many paths to artemisinin resistance in Plasmodium falciparum. Trends Parasitol 2023, 39, 1060–1073. [Google Scholar] [CrossRef] [PubMed]
- Platon, L.; Menard, D. Plasmodium falciparum ring-stage plasticity and drug resistance. Trends Parasitol 2024, 40, 118–130. [Google Scholar] [CrossRef] [PubMed]
- Müller, J.; Ley, S.; Felger, I.; Hemphill, A.; Müller, N. Identification of differentially expressed genes in a Giardia lamblia WB C6 clone resistant to nitazoxanide and metronidazole. J Antimicrob Chemother 2008, 62, 72–82. [Google Scholar] [CrossRef] [PubMed]
- Townson, S.M.; Laqua, H.; Upcroft, P.; Boreham, P.F.; Upcroft, J.A. Induction of metronidazole and furazolidone resistance in Giardia. Trans R Soc Trop Med Hyg 1992, 86, 521–522. [Google Scholar] [CrossRef] [PubMed]
- Müller, J.; Sterk, M.; Hemphill, A.; Müller, N. Characterization of Giardia lamblia WB C6 clones resistant to nitazoxanide and to metronidazole. J Antimicrob Chemother 2007, 60, 280–287. [Google Scholar] [CrossRef] [PubMed]
- Brown, D.M.; Upcroft, J.A.; Edwards, M.R.; Upcroft, P. Anaerobic bacterial metabolism in the ancient eukaryote Giardia duodenalis. Int J Parasitol 1998, 28, 149–164. [Google Scholar] [CrossRef] [PubMed]
- Müller, J.; Braga, S.; Heller, M.; Müller, N. Resistance formation to nitro drugs in <italic>Giardia lamblia</italic>: No common markers identified by comparative proteomics Int J Parasitol: Drugs Drug Resist 2019, 9, 112-119.
- Ansell, B.R.; Baker, L.; Emery, S.J.; McConville, M.J.; Svard, S.G.; Gasser, R.B.; Jex, A.R. Transcriptomics indicates active and passive metronidazole resistance mechanisms in three seminal Giardia lines. Front Microbiol 2017, 8, 398. [Google Scholar] [CrossRef] [PubMed]
- Emery, S.J.; Baker, L.; Ansell, B.R.E.; Mirzaei, M.; Haynes, P.A.; McConville, M.J.; Svard, S.G.; Jex, A.R. Differential protein expression and post-translational modifications in metronidazole-resistant Giardia duodenalis. Gigascience 2018, 7. [Google Scholar] [CrossRef] [PubMed]
- Koncarevic, S.; Bogumil, R.; Becker, K. SELDI-TOF-MS analysis of chloroquine resistant and sensitive Plasmodium falciparum strains. Proteomics 2007, 7, 711–721. [Google Scholar] [CrossRef] [PubMed]
- Doliwa, C.; Xia, D.; Escotte-Binet, S.; Newsham, E.L.; Sanya, J.S.; Aubert, D.; Randle, N.; Wastling, J.M.; Villena, I. Identification of differentially expressed proteins in sulfadiazine resistant and sensitive strains of Toxoplasma gondii using difference-gel electrophoresis (DIGE). Int J Parasitol Drugs Drug Resist 2013, 3, 35–44. [Google Scholar] [CrossRef] [PubMed]
- Müller, J.; Schlange, C.; Heller, M.; Uldry, A.C.; Braga-Lagache, S.; Haynes, R.K.; Hemphill, A. Proteomic characterization of Toxoplasma gondii ME49 derived strains resistant to the artemisinin derivatives artemiside and artemisone implies potential mode of action independent of ROS formation. Int J Parasitol Drugs Drug Resist 2023, 21, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Scheele, S.; Geiger, J.A.; DeRocher, A.E.; Choi, R.; Smith, T.R.; Hulverson, M.A.; Vidadala, R.S.R.; Barrett, L.K.; Maly, D.J.; Merritt, E.A.; et al. Toxoplasma calcium-dependent protein kinase 1 inhibitors: Probing activity and resistance using cellular thermal shift assays. Antimicrob Agents Chemother 2018, 62. [Google Scholar] [CrossRef] [PubMed]
- Burata, O.E.; Yeh, T.J.; Macdonald, C.B.; Stockbridge, R.B. Still rocking in the structural era: A molecular overview of the small multidrug resistance (SMR) transporter family. J Biol Chem 2022, 298, 102482. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Lin, Q. Chemical proteomics approach reveals the direct targets and the heme-dependent activation mechanism of artemisinin in Plasmodium falciparum using an artemisinin-based activity probe. Microb Cell 2016, 3, 230–231. [Google Scholar] [CrossRef] [PubMed]
- Rios-Barros, L.V.; Silva-Moreira, A.L.; Horta, M.F.; Gontijo, N.F.; Castro-Gomes, T. How to get away with murder: The multiple strategies employed by pathogenic protozoa to avoid complement killing. Mol Immunol 2022, 149, 27–38. [Google Scholar] [CrossRef] [PubMed]
- Prucca, C.G.; Lujan, H.D. Antigenic variation in Giardia lamblia. Cell Microbiol 2009, 11, 1706–1715. [Google Scholar] [CrossRef] [PubMed]
- Müller, N.; Gottstein, B. Antigenic variation and the murine immune response to Giardia lamblia. Int J Parasitol 1998, 28, 1829–1839. [Google Scholar] [CrossRef] [PubMed]
- Müller, J.; Vermathen, M.; Leitsch, D.; Vermathen, P.; Müller, N. Metabolomic profiling of wildtype and transgenic Giardia lamblia Strains by (1)H HR-MAS NMR Spectroscopy. Metabolites 2020, 10. [Google Scholar] [CrossRef] [PubMed]
| Protein Target for Inhibitor Screenings | Pathogen | Methodology | Reference |
|---|---|---|---|
| Protein biosynthesis | P. falciparum | Luciferase assay | [60] |
| Calcium-dependent protein kinase 1 | T. gondii | Kinase assay Cocrystallization |
[61,62] |
| Dihydrofolate reductase thymidylate synthase | T. gondii | Functional assay | [63] |
| Dihydrofolate reductase | P. vivax | Heterologous expression in yeast Growth assay |
[64] |
| Acetyl-CoA carboxylase | T. gondii | Functional assay | [65] |
| Glyoxalase 1 | T. gondii | Functional assay | [66] |
| Type-II NADH dehydrogenase | T. gondii | Functional assay | [67] |
| Nucleoside triphosphate hydrolase | N. caninum, T. gondii | Chemoluminescence assay | [68] |
| Mitochondrial ADP/ATP | P. falciparum | Heterologous expression in E. coli Radioactive uptake assay |
[69] |
| Importin alpha binding to nuclear localization signal | P. falciparum | Alpha screen binding assay | [70] |
| Phenylalanyl t-RNA synthetase | T. gondii | Functional assay | [71] |
| Aspartate transcarbamoylase | P. falciparum | Functional assay, protein interference assay | [72,73] |
| Antimalarial | Methodology | Remarks | Reference |
|---|---|---|---|
| Kinase inhibitors | Cell-free extracts from various cell types and organisms. DAC with active and inactive purines. SDS-PAGE followed by digestion of binding proteins and microsequencing of the peptides. | Detection of known kinases by Western Blotting. Some of the peptide sequences match to other kinases and other proteins. | [86] |
| Quinolines | Cell-free extracts of infected human erythrocytes. DAC with ATP as a control, elution with various quinoline antimalarials, SDS-PAGE followed by Edman mixed peptide sequencing. | Human aldehyde dehydrogenase 1 and quinone reductase 2 major BP. Validated as potential target by FA. | [87] |
| Endoperoxides | P. falciparum trophozoite lysates. AC with an artemisinin analog, followed by 2-D SDS-PAGE and MALDI-TOF MS. | Identification of 9 P. falciparum BPs. Major BP is a calcium binding protein. | [88] |
| Organism | Ligand | Methodology | Remarks | Reference |
|---|---|---|---|---|
| G. lamblia | Thiazolide | AC, elution with ligand, SDS-PAGE followed by LC-MS/MS. | Nitroreductase NR1 major BP. Validated as potential target by FA and in subsequent studies. | [89,90,91] |
|
H. sapiens Caco2 |
Thiazolide | AC, elution with ligand, SDS-PAGE followed by LC-MS/MS. | Human GSTP1 major BP. Validated as potential target by FA and in subsequent studies. | [92,93] |
|
H. sapiens Fibroblasts |
Thiazolide | AC, elution with ligand, SDS-PAGE followed by LC-MS/MS. | Human quinone reductase 1 major BP in N. caninum infected cells. Validation by FA. | [94] |
| T. gondii | Ruthenium complex | DAC with mock column only; elution by pH shift; SDS-PAGE followed by LC-MS/MS. | Translation elongation factor 1 alpha and two ribosomal proteins identified as binding proteins. |
[95] |
|
T. gondii T. brucei |
Ruthenium complex | Comparative DAC with two ineffective complexes in two pathogens, elution with pH shift, LC-MS/MS on entire eluates. | 128 specific T. gondii BPs and 46 specific T. brucei BPs. Major T. brucei BP mitochondrial ATP synthase subunit validated by FA. | [96] |
|
T. gondii M. musculus splenocytes |
Antimicrobial peptide | Comparative DAC with ineffective peptide, elution with pH shift, LC-MS/MS on entire eluates. | Several hundred BPs in eluates from both organisms suggesting common modes of action. | [97] |
|
N. caninum D. rerio |
Bumped kinase inhibitor with quinoline core | Comparative DAC with quinine, elution with pH shift, LC-MS/MS on entire eluates. | 12 specific N. caninum BPs and 13 specific D. rerio BPs. Many BPs in both organism in quinine eluates, as well. Majority involved in RNAbinding or modification. | [98] |
|
C. parvum H. sapiens HCT-8 cells |
Bumped kinase in-hibitor with quino-line core | Comparative DAC with quinine, elution with pH shift, LC-MS/MS on entire eluates. | No specific binding proteins in C. parvum, 25 specific BPs in host cells. 29 C. parvum and 224 host cell BPs also in quinine eluates. Common targets in RNA binding or modification. | [99] |
| Organism | Methodology | Remarks | Reference |
|---|---|---|---|
| Leishmania donovani | Classical CETSA-MS on promastigotes with an inhibitor of sterol biosynthesis. | Oxidosqualene cyclase identified as a target of this inhibitor. | [121,122] |
| L. infantum | Classical CETSA-MS on cell-free extracts of amphotericine B, antimony or miltefosine susceptible and resistant lines incubated with the respective drugs. | Up to several hundred proteins with altered melting profiles depending on the compound. Sb tend to stabilize ribosomal proteins. | [123] |
| P. falciparum | Comparison of classical and isothermal CETSA on intraerythrocytic stages using pyrimethamine as a proof of concept. | Conceptual study. No data on novel binding proteins directly available. | [124] |
| T. gondii | Classical CETSA-MS with calcium egress inhibitor ENH1 as ligand. | 82 proteins with enhanced thermal stability identified including Calcium dependent protein kinase 1. | [125] |
| Methodology | Advantages | Inconvenients |
|---|---|---|
| AC–elution with ligand | Well established. Does not need sophisticated equipment. Fast. | Modification of original ligand necessary to create column matrix. Identification of major binding proteins after PAGE, resulting in low yields, bias. Cell-free extracts. |
| DAC–unspecific elution | See above. LC-MS/MS if elution with compatible solvent. | Needs ineffective control compound with similar structure. Cell-free extracts. |
| Affinity labelling | Interaction occurs intracellularly, therefore under physiological conditions. Fast. | Modification of original ligand necessary to create compound for affinity labelling. Polishing of labelled proteins by PAGE, therefore low yields and bias. Label may interfere with subsequent MS. |
| TPP | Flexible, since interaction of proteomes and ligands are investigated under physiological conditions or in cell free extracts. Unmodified compounds may be used. | Time and cost intensive. Use of isobaric labels. Large data volumes needing appropriate bioinformatic tools. |
| Organism | Drug | Methodology | Remarks | Reference |
|---|---|---|---|---|
| G. lamblia | Metronidazole | Comparison of three resistant cell lines created by increasing drug concentrations plus UV irradiation with susceptible parental strains. Analysis of proteomes and post-translational modifications by broad panel of proteome analytical methods. | 265, 171, and 76 differentially expressed proteins depending on the strains. High isolate dependent variability of adaptation mechanisms. | [163] |
| G. lamblia | Nitazoxanide Metronidazole |
Comparison of a strain generated by increasing nitazoxanide concentrations and two metronidazole resistant strains from study quoted above with their corresponding wildtypes. All resistant strains were resistant to both drugs and were grown int the presence of either drug prior to analysis by shotgun LC/MS-MS. | 225, 248, and 304 differentially expressed proteins in the presence of nitazoxanide, 510, 287, and 216 in the presence of metronidazole. No common markers for nitro resistance. Common pattern of antigenic variation in all metronidazole resistant vs. susceptible strains. Strategies of coping with nitro reduction strain and drug dependent. | [161] |
| P. falciparum | Chloroquine | Comparison of two clinical isolates resistant to chloroquine with two susceptible isolates using SELDI-TOF. | Study focused on the methodology. One of the susceptible strains and both resistant strains are resistant to pyrimethamine, one resistant strain is resistant to quinine and sulfadoxine, as well. 10 “marker proteins” identified. | [164] |
|
T. gondii |
Sulfadizine | Resistant clinical isolates, susceptible reference strains. Comparison of proteomes by DIGE-MS. | 31 unique differential proteins were identified. |
[165] |
| T. gondii | Artemisone Artemiside |
Generation of resistant strains by treating the reference strain ME49 with increasing concentrations. Whole-cell-shotgun LC/MS-MS. | 215 proteins downregulated in the artemisone resistant strain, 8 proteins in the artemiside resistant strain. | [166] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





