Submitted:
27 May 2024
Posted:
28 May 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
1.1. Fasting: An Hystorical and Social View
1.2. A General View of IF Approaches
2. Food Intake Restriction: An In-Depth Outlook
2.1. Examples of Clinical Trials Showing ADF-Based Approach as Primary Dietary Intervention
3. Conclusions and Future Perspectives
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- de Cabo, R.; Mattson, M.P. Effects of Intermittent Fasting on Health, Aging, and Disease. N Engl J Med 2019, 381, 2541–2551. [Google Scholar] [CrossRef] [PubMed]
- Sainsbury, A.; Wood, R.E.; Seimon, R.V.; Hills, A.P.; King, N.A.; Gibson, A.A.; Byrne, N.M. Rationale for novel intermittent dieting strategies to attenuate adaptive responses to energy restriction. Obes Rev 2018, 19 Suppl 1, 47–60. [Google Scholar] [CrossRef]
- Mattson, M.P.; Longo, V.D.; Harvie, M. Impact of intermittent fasting on health and disease processes. Ageing Res Rev 2017, 39, 46–58. [Google Scholar] [CrossRef] [PubMed]
- Vasim, I.; Majeed, C.N.; DeBoer, M.D. Intermittent Fasting and Metabolic Health. Nutrients 2022, 14. [Google Scholar] [CrossRef] [PubMed]
- Longo, V.D.; Mattson, M.P. Fasting: molecular mechanisms and clinical applications. Cell Metab 2014, 19, 181–192. [Google Scholar] [CrossRef]
- O'Connor, S.G.; Boyd, P.; Bailey, C.P.; Shams-White, M.M.; Agurs-Collins, T.; Hall, K.; Reedy, J.; Sauter, E.R.; Czajkowski, S.M. Perspective: Time-Restricted Eating Compared with Caloric Restriction: Potential Facilitators and Barriers of Long-Term Weight Loss Maintenance. Adv Nutr 2021, 12, 325–333. [Google Scholar] [CrossRef]
- Dansinger, M.L.; Gleason, J.A.; Griffith, J.L.; Selker, H.P.; Schaefer, E.J. Comparison of the Atkins, Ornish, Weight Watchers, and Zone diets for weight loss and heart disease risk reduction: a randomized trial. JAMA 2005, 293, 43–53. [Google Scholar] [CrossRef] [PubMed]
- Anderson, J.W.; Konz, E.C.; Frederich, R.C.; Wood, C.L. Long-term weight-loss maintenance: a meta-analysis of US studies. Am J Clin Nutr 2001, 74, 579–584. [Google Scholar] [CrossRef] [PubMed]
- Del Corral, P.; Chandler-Laney, P.C.; Casazza, K.; Gower, B.A.; Hunter, G.R. Effect of dietary adherence with or without exercise on weight loss: a mechanistic approach to a global problem. J Clin Endocrinol Metab 2009, 94, 1602–1607. [Google Scholar] [CrossRef]
- Varady, K.A. Intermittent versus daily calorie restriction: which diet regimen is more effective for weight loss? Obes Rev 2011, 12, e593–601. [Google Scholar] [CrossRef]
- Pannen, S.T.; Maldonado, S.G.; Nonnenmacher, T.; Sowah, S.A.; Gruner, L.F.; Watzinger, C.; Nischwitz, K.; Ulrich, C.M.; Kaaks, R.; Schubel, R. , et al. Adherence and Dietary Composition during Intermittent vs. Continuous Calorie Restriction: Follow-Up Data from a Randomized Controlled Trial in Adults with Overweight or Obesity. Nutrients 2021, 13. [Google Scholar] [CrossRef] [PubMed]
- Trepanowski, J.F.; Kroeger, C.M.; Barnosky, A.; Klempel, M.C.; Bhutani, S.; Hoddy, K.K.; Gabel, K.; Freels, S.; Rigdon, J.; Rood, J. , et al. Effect of Alternate-Day Fasting on Weight Loss, Weight Maintenance, and Cardioprotection Among Metabolically Healthy Obese Adults: A Randomized Clinical Trial. JAMA Intern Med 2017, 177, 930–938. [Google Scholar] [CrossRef] [PubMed]
- Halpern, B.; Mendes, T.B. Intermittent fasting for obesity and related disorders: unveiling myths, facts, and presumptions. Arch Endocrinol Metab 2021, 65, 14–23. [Google Scholar] [CrossRef] [PubMed]
- Rajpal, A.; Ismail-Beigi, F. Intermittent fasting and 'metabolic switch': Effects on metabolic syndrome, prediabetes and type 2 diabetes. Diabetes Obes Metab 2020, 22, 1496–1510. [Google Scholar] [CrossRef]
- Attina, A.; Leggeri, C.; Paroni, R.; Pivari, F.; Dei Cas, M.; Mingione, A.; Dri, M.; Marchetti, M.; Di Renzo, L. Fasting: How to Guide. Nutrients 2021, 13. [Google Scholar] [CrossRef]
- Skiadas, P.K.; Lascaratos, J.G. Dietetics in ancient Greek philosophy: Plato's concepts of healthy diet. Eur J Clin Nutr 2001, 55, 532–537. [Google Scholar] [CrossRef] [PubMed]
- Fidanza, F. Diets and dietary recommendations in ancient Greece and Rome and the school of Salerno. Prog Food Nutr Sci 1979, 3, 79–99. [Google Scholar] [PubMed]
- Waterlow, J.C. Diet of the classical period of Greece and Rome. Eur J Clin Nutr 1989, 43 Suppl 2, 3–12. [Google Scholar]
- Kerndt, P.R.; Naughton, J.L.; Driscoll, C.E.; Loxterkamp, D.A. Fasting: the history, pathophysiology and complications. West J Med 1982, 137, 379–399. [Google Scholar]
- Trepanowski, J.F.; Bloomer, R.J. The impact of religious fasting on human health. Nutr J 2010, 9, 57. [Google Scholar] [CrossRef]
- Galassi, F.M.; Bender, N.; Habicht, M.E.; Armocida, E.; Toscano, F.; Menassa, D.A.; Cerri, M. St. Catherine of Siena (1347-1380 AD): one of the earliest historic cases of altered gustatory perception in anorexia mirabilis. Neurol Sci 2018, 39, 939–940. [Google Scholar] [CrossRef] [PubMed]
- Arbesmann, R. Fasting and Prophecy in Pagan and Christian Antiquity. Traditio 2017, 7, 1–71. [Google Scholar] [CrossRef]
- Harris, J.C. Anorexia nervosa and anorexia mirabilis: Miss K. R--and St Catherine Of Siena. JAMA Psychiatry 2014, 71, 1212–1213. [Google Scholar] [CrossRef] [PubMed]
- Visioli, F.; Mucignat-Caretta, C.; Anile, F.; Panaite, S.A. Traditional and Medical Applications of Fasting. Nutrients 2022, 14. [Google Scholar] [CrossRef] [PubMed]
- Venegas-Borsellino, C.; Sonikpreet; Martindale, R.G. From Religion to Secularism: the Benefits of Fasting. Current Nutrition Reports 2018, 7, 131–138. [Google Scholar] [CrossRef] [PubMed]
- Persynaki, A.; Karras, S.; Pichard, C. Unraveling the metabolic health benefits of fasting related to religious beliefs: A narrative review. Nutrition 2017, 35, 14–20. [Google Scholar] [CrossRef] [PubMed]
- Roky, R.; Chapotot, F.; Hakkou, F.; Benchekroun, M.T.; Buguet, A. Sleep during Ramadan intermittent fasting. J Sleep Res 2001, 10, 319–327. [Google Scholar] [CrossRef] [PubMed]
- Fedail, S.S.; Murphy, D.; Salih, S.Y.; Bolton, C.H.; Harvey, R.F. Changes in certain blood constituents during Ramadan. Am J Clin Nutr 1982, 36, 350–353. [Google Scholar] [CrossRef] [PubMed]
- Kul, S.; Savas, E.; Ozturk, Z.A.; Karadag, G. Does Ramadan fasting alter body weight and blood lipids and fasting blood glucose in a healthy population? A meta-analysis. J Relig Health 2014, 53, 929–942. [Google Scholar] [CrossRef]
- Sadeghirad, B.; Motaghipisheh, S.; Kolahdooz, F.; Zahedi, M.J.; Haghdoost, A.A. Islamic fasting and weight loss: a systematic review and meta-analysis. Public Health Nutr 2014, 17, 396–406. [Google Scholar] [CrossRef]
- Fakhrzadeh, H.; Larijani, B.; Sanjari, M.; Baradar-Jalili, R.; Amini, M.R. Effect of Ramadan fasting on clinical and biochemical parameters in healthy adults. Ann Saudi Med 2003, 23, 223–226. [Google Scholar] [CrossRef] [PubMed]
- Sarraf-Zadegan, N.; Atashi, M.; Naderi, G.A.; Baghai, A.M.; Asgary, S.; Fatehifar, M.R.; Samarian, H.; Zarei, M. The effect of fasting in Ramadan on the values and interrelations between biochemical, coagulation and hematological factors. Ann Saudi Med 2000, 20, 377–381. [Google Scholar] [CrossRef] [PubMed]
- Maislos, M.; Khamaysi, N.; Assali, A.; Abou-Rabiah, Y.; Zvili, I.; Shany, S. Marked increase in plasma high-density-lipoprotein cholesterol after prolonged fasting during Ramadan. Am J Clin Nutr 1993, 57, 640–642. [Google Scholar] [CrossRef] [PubMed]
- Ziaee, V.; Razaei, M.; Ahmadinejad, Z.; Shaikh, H.; Yousefi, R.; Yarmohammadi, L.; Bozorgi, F.; Behjati, M.J. The changes of metabolic profile and weight during Ramadan fasting. Singapore Med J 2006, 47, 409–414. [Google Scholar] [PubMed]
- Ahmed, N.; Farooq, J.; Siddiqi, H.S.; Meo, S.A.; Kulsoom, B.; Laghari, A.H.; Jamshed, H.; Pasha, F. Impact of Intermittent Fasting on Lipid Profile-A Quasi-Randomized Clinical Trial. Front Nutr 2020, 7, 596787. [Google Scholar] [CrossRef] [PubMed]
- Ramadan, J. Does fasting during Ramadan alter body composition, blood constituents and physical performance? Med Princ Pract 2002, 11 Suppl 2, 41–46. [Google Scholar] [CrossRef]
- Jack, H.A. The Gandhi Reader: A Sourcebook of His Life and Writings; Grove Press: 1994.
- https://www.washingtonpost.com/archive/politics/1981/10/04/prisoners-end-fasting-in-belfast/; accessed on 23 May 2024.
- http://news.bbc.co.uk/2/hi/americas/8533350.stm; acceseed on 23 May 2024.
- https://www.cubacenter.org/archives/2023/5/25/cubabrief-cuban-student-leader-pedro-luis-boitel-martyred-51-years-ago-today-eu-high-representative-begins-high-level-visit-to-cuba-ngos-call-on-eu-to-address-cubas-human-rights-crisis; accessed on 23May 2024.
- https://www.ilsecoloxix.it/italia/2016/05/19/news/pannella-46-anni-di-digiuni-il-primo-nel-1969-1.37958505; accessed on 23 May 2024.
- Stella, A. SCRITTI DI ALDO CAPITINI. Annali della Scuola Normale Superiore di Pisa. Classe di Lettere e Filosofia 1975, 5, 379–412. [Google Scholar]
- https://www.corriere.it/cronache/17_luglio_05/sardegna-morto-sciopero-fame-l-indipendentista-doddore-4037bca8-618d-11e7-bdfb-e027df3feb8d.shtml; accessed on 23 May 2024.
- Oswald, J.A. Yours for Health: The Life and Times of Herbert M. Shelton; Franklin Books: 1989.
- Shelton, H.M. The Science and Fine Art of Fasting; Martino Fine Books: 2013.
- Shelton, H.M.G.; Cridland, R.G. Fasting Can Save Your Life; American Natural Hygiene Society: 1996.
- McCay, C.M.; Crowell, M.F.; Maynard, L.A. The Effect of Retarded Growth Upon the Length of Life Span and Upon the Ultimate Body Size. The Journal of Nutrition 1935, 10, 63–79. [Google Scholar] [CrossRef]
- McCay, C.M.; Crowell, M.F.; Maynard, L.A. The effect of retarded growth upon the length of life span and upon the ultimate body size. 1935. Nutrition 1989, 5, 155–171. [Google Scholar]
- McDonald, R.B.; Ramsey, J.J. Honoring Clive McCay and 75 years of calorie restriction research. J Nutr 2010, 140, 1205–1210. [Google Scholar] [CrossRef]
- Santos, H.O.; Genario, R.; Tinsley, G.M.; Ribeiro, P.; Carteri, R.B.; Coelho-Ravagnani, C.F.; Mota, J.F. A scoping review of intermittent fasting, chronobiology, and metabolism. Am J Clin Nutr 2022, 115, 991–1004. [Google Scholar] [CrossRef]
- Jensen, M.D.; Ryan, D.H.; Apovian, C.M.; Ard, J.D.; Comuzzie, A.G.; Donato, K.A.; Hu, F.B.; Hubbard, V.S.; Jakicic, J.M.; Kushner, R.F. , et al. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. Circulation 2014, 129, S102–138. [Google Scholar] [CrossRef]
- Moreira, E.A.; Most, M.; Howard, J.; Ravussin, E. Dietary adherence to long-term controlled feeding in a calorie-restriction study in overweight men and women. Nutr Clin Pract 2011, 26, 309–315. [Google Scholar] [CrossRef] [PubMed]
- Sacks, F.M.; Bray, G.A.; Carey, V.J.; Smith, S.R.; Ryan, D.H.; Anton, S.D.; McManus, K.; Champagne, C.M.; Bishop, L.M.; Laranjo, N. , et al. Comparison of weight-loss diets with different compositions of fat, protein, and carbohydrates. N Engl J Med 2009, 360, 859–873. [Google Scholar] [CrossRef] [PubMed]
- Das, S.K.; Gilhooly, C.H.; Golden, J.K.; Pittas, A.G.; Fuss, P.J.; Cheatham, R.A.; Tyler, S.; Tsay, M.; McCrory, M.A.; Lichtenstein, A.H. , et al. Long-term effects of 2 energy-restricted diets differing in glycemic load on dietary adherence, body composition, and metabolism in CALERIE: a 1-y randomized controlled trial. Am J Clin Nutr 2007, 85, 1023–1030. [Google Scholar] [CrossRef]
- Gu, L.; Fu, R.; Hong, J.; Ni, H.; Yu, K.; Lou, H. Effects of Intermittent Fasting in Human Compared to a Non-intervention Diet and Caloric Restriction: A Meta-Analysis of Randomized Controlled Trials. Front Nutr 2022, 9, 871682. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Green, S. Cochrane Handbook for Systematic Reviews of Interventions; Wiley: 2011.
- Elortegui Pascual, P.; Rolands, M.R.; Eldridge, A.L.; Kassis, A.; Mainardi, F.; Le, K.A.; Karagounis, L.G.; Gut, P.; Varady, K.A. A meta-analysis comparing the effectiveness of alternate day fasting, the 5:2 diet, and time-restricted eating for weight loss. Obesity (Silver Spring) 2023, 31 Suppl 1, 9–21. [Google Scholar] [CrossRef]
- Schroor, M.M.; Joris, P.J.; Plat, J.; Mensink, R.P. Effects of Intermittent Energy Restriction Compared with Those of Continuous Energy Restriction on Body Composition and Cardiometabolic Risk Markers - A Systematic Review and Meta-Analysis of Randomized Controlled Trials in Adults. Adv Nutr 2024, 15, 100130. [Google Scholar] [CrossRef]
- Cheung, K.; Chan, V.; Chan, S.; Wong, M.M.H.; Chung, G.K.; Cheng, W.Y.; Lo, K.; Zeng, F. Effect of Intermittent Fasting on Cardiometabolic Health in the Chinese Population: A Meta-Analysis of Randomized Controlled Trials. Nutrients 2024, 16. [Google Scholar] [CrossRef] [PubMed]
- Wang, W.; Wei, R.; Pan, Q.; Guo, L. Beneficial effect of time-restricted eating on blood pressure: a systematic meta-analysis and meta-regression analysis. Nutr Metab (Lond) 2022, 19, 77. [Google Scholar] [CrossRef]
- Wilhelmi de Toledo, F.; Grundler, F.; Bergouignan, A.; Drinda, S.; Michalsen, A. Safety, health improvement and well-being during a 4 to 21-day fasting period in an observational study including 1422 subjects. PLoS One 2019, 14, e0209353. [Google Scholar] [CrossRef]
- Kim, K.-K.; Kang, J.-H.; Kim, E.M. Updated Meta-Analysis of Studies from 2011 to 2021 Comparing the Effectiveness of Intermittent Energy Restriction and Continuous Energy Restriction. Journal of Obesity & Metabolic Syndrome 2022, 31, 230–244. [Google Scholar] [CrossRef]
- Schoonakker, M.P.; van den Burg, E.L.; van Peet, P.G.; Lamb, H.J.; Numans, M.E.; Pijl, H. Chapter 21 - Intermittent fasting. In Visceral and Ectopic Fat; Lamb, H.J., Ed.; Elsevier, 2023; pp. 307–319. [Google Scholar] [CrossRef]
- Cui, Y.; Cai, T.; Zhou, Z.; Mu, Y.; Lu, Y.; Gao, Z.; Wu, J.; Zhang, Y. Health Effects of Alternate-Day Fasting in Adults: A Systematic Review and Meta-Analysis. Front Nutr 2020, 7, 586036. [Google Scholar] [CrossRef] [PubMed]
- Brandhorst, S.; Choi, I.Y.; Wei, M.; Cheng, C.W.; Sedrakyan, S.; Navarrete, G.; Dubeau, L.; Yap, L.P.; Park, R.; Vinciguerra, M. , et al. A Periodic Diet that Mimics Fasting Promotes Multi-System Regeneration, Enhanced Cognitive Performance, and Healthspan. Cell Metab 2015, 22, 86–99. [Google Scholar] [CrossRef] [PubMed]
- Wei, M.; Brandhorst, S.; Shelehchi, M.; Mirzaei, H.; Cheng, C.W.; Budniak, J.; Groshen, S.; Mack, W.J.; Guen, E.; Di Biase, S. , et al. Fasting-mimicking diet and markers/risk factors for aging, diabetes, cancer, and cardiovascular disease. Sci Transl Med 2017, 9. [Google Scholar] [CrossRef]
- Wang, R.; Lv, X.; Xu, W.; Li, X.; Tang, X.; Huang, H.; Yang, M.; Ma, S.; Wang, N.; Niu, Y. Effects of the periodic fasting-mimicking diet on health, lifespan, and multiple diseases: a narrative review and clinical implications. Nutr Rev 2024. [Google Scholar] [CrossRef] [PubMed]
- Longo, V.D.; Panda, S. Fasting, Circadian Rhythms, and Time-Restricted Feeding in Healthy Lifespan. Cell Metab 2016, 23, 1048–1059. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Song, Y. Early Time-Restricted Eating Reduces Weight and Improves Glycemic Response in Young Adults: A Pre-Post Single-Arm Intervention Study. Obes Facts 2023, 16, 69–81. [Google Scholar] [CrossRef]
- Lynch, S.; Johnston, J.D.; Robertson, M.D. Early versus late time-restricted feeding in adults at increased risk of developing type 2 diabetes: Is there an optimal time to eat for metabolic health? Nutr Bull 2021, 46, 69–76. [Google Scholar] [CrossRef]
- Tinsley, G.M.; La Bounty, P.M. Effects of intermittent fasting on body composition and clinical health markers in humans. Nutr Rev 2015, 73, 661–674. [Google Scholar] [CrossRef]
- Di Francesco, A.; Di Germanio, C.; Bernier, M.; de Cabo, R. A time to fast. Science 2018, 362, 770–775. [Google Scholar] [CrossRef]
- Kalam, F.; Gabel, K.; Cienfuegos, S.; Ezpeleta, M.; Wiseman, E.; Varady, K.A. Alternate Day Fasting Combined with a Low Carbohydrate Diet: Effect on Sleep Quality, Duration, Insomnia Severity and Risk of Obstructive Sleep Apnea in Adults with Obesity. Nutrients 2021, 13. [Google Scholar] [CrossRef]
- Varady, K.A.; Cienfuegos, S.; Ezpeleta, M.; Gabel, K. Clinical application of intermittent fasting for weight loss: progress and future directions. Nat Rev Endocrinol 2022, 18, 309–321. [Google Scholar] [CrossRef]
- Varady, K.A.; Gabel, K. Safety and efficacy of alternate day fasting. Nat Rev Endocrinol 2019, 15, 686–687. [Google Scholar] [CrossRef]
- Klempel, M.C.; Kroeger, C.M.; Varady, K.A. Alternate day fasting increases LDL particle size independently of dietary fat content in obese humans. Eur J Clin Nutr 2013, 67, 783–785. [Google Scholar] [CrossRef]
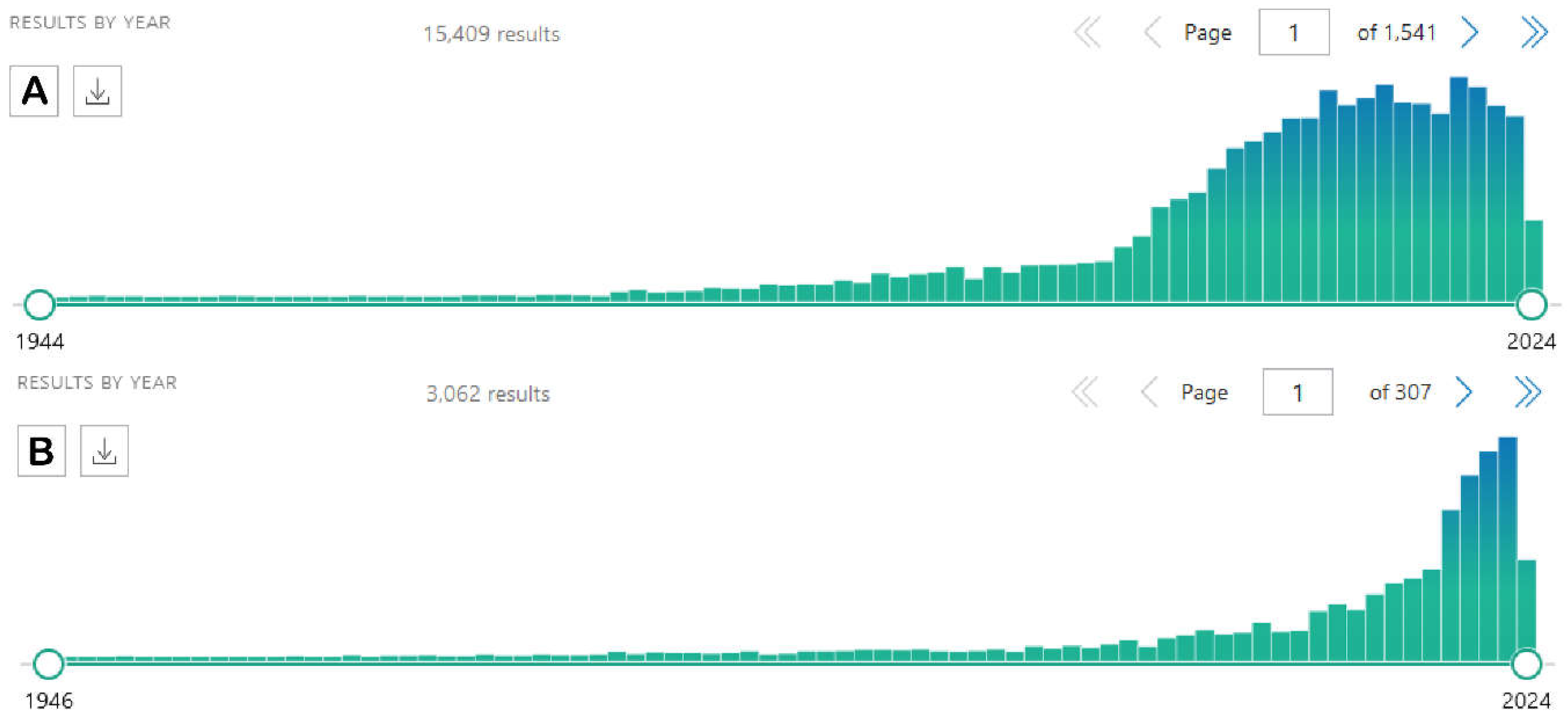
- Chen, S.; Han, R.; Liu, H. A Bibliometric and Visualization Analysis of Intermittent Fasting. Front Public Health 2022, 10, 946795. [Google Scholar] [CrossRef]
- Alhamdan, B.A.; Garcia-Alvarez, A.; Alzahrnai, A.H.; Karanxha, J.; Stretchberry, D.R.; Contrera, K.J.; Utria, A.F.; Cheskin, L.J. Alternate-day versus daily energy restriction diets: which is more effective for weight loss? A systematic review and meta-analysis. Obes Sci Pract 2016, 2, 293–302. [Google Scholar] [CrossRef]
- Heilbronn, L.K.; Smith, S.R.; Martin, C.K.; Anton, S.D.; Ravussin, E. Alternate-day fasting in nonobese subjects: effects on body weight, body composition, and energy metabolism. Am J Clin Nutr 2005, 81, 69–73. [Google Scholar] [CrossRef]
- Patterson, R.E.; Laughlin, G.A.; LaCroix, A.Z.; Hartman, S.J.; Natarajan, L.; Senger, C.M.; Martinez, M.E.; Villasenor, A.; Sears, D.D.; Marinac, C.R. , et al. Intermittent Fasting and Human Metabolic Health. J Acad Nutr Diet 2015, 115, 1203–1212. [Google Scholar] [CrossRef]
- Mosley, M.; Spencer, M. The FastDiet-revised & updated: lose weight, stay healthy, and live longer with the simple secret of intermittent fasting; Simon and Schuster: 2015.
- Cook, F.; Langdon-Daly, J.; Serpell, L. Compliance of participants undergoing a '5-2' intermittent fasting diet and impact on body weight. Clin Nutr ESPEN 2022, 52, 257–261. [Google Scholar] [CrossRef]
- Hajek, P.; Przulj, D.; Pesola, F.; McRobbie, H.; Peerbux, S.; Phillips-Waller, A.; Bisal, N.; Myers Smith, K. A randomised controlled trial of the 5:2 diet. PLoS One 2021, 16, e0258853. [Google Scholar] [CrossRef]
- Witjaksono, F.; Prafiantini, E.; Rahmawati, A. Effect of intermittent fasting 5:2 on body composition and nutritional intake among employees with obesity in Jakarta: a randomized clinical trial. BMC Res Notes 2022, 15, 323. [Google Scholar] [CrossRef]
- Fudla, H.; Mudjihartini, N.; Khusun, H. Effect of four weeks of 5:2 intermittent fasting on energy intake and body mass index among obese male students aged 18-25. Obes Med 2021, 25, 100353. [Google Scholar] [CrossRef]
- Kord Varkaneh, H.; Salehi Sahlabadi, A.; Gaman, M.A.; Rajabnia, M.; Sedanur Macit-Celebi, M.; Santos, H.O.; Hekmatdoost, A. Effects of the 5:2 intermittent fasting diet on non-alcoholic fatty liver disease: A randomized controlled trial. Front Nutr 2022, 9, 948655. [Google Scholar] [CrossRef]
- Rothschild, J.; Hoddy, K.K.; Jambazian, P.; Varady, K.A. Time-restricted feeding and risk of metabolic disease: a review of human and animal studies. Nutr Rev 2014, 72, 308–318. [Google Scholar] [CrossRef]
- Moro, T.; Tinsley, G.; Bianco, A.; Marcolin, G.; Pacelli, Q.F.; Battaglia, G.; Palma, A.; Gentil, P.; Neri, M.; Paoli, A. Effects of eight weeks of time-restricted feeding (16/8) on basal metabolism, maximal strength, body composition, inflammation, and cardiovascular risk factors in resistance-trained males. J Transl Med 2016, 14, 290. [Google Scholar] [CrossRef]
- Gabel, K.; Hoddy, K.K.; Haggerty, N.; Song, J.; Kroeger, C.M.; Trepanowski, J.F.; Panda, S.; Varady, K.A. Effects of 8-hour time restricted feeding on body weight and metabolic disease risk factors in obese adults: A pilot study. Nutr Healthy Aging 2018, 4, 345–353. [Google Scholar] [CrossRef]
- Cienfuegos, S.; Gabel, K.; Kalam, F.; Ezpeleta, M.; Wiseman, E.; Pavlou, V.; Lin, S.; Oliveira, M.L.; Varady, K.A. Effects of 4- and 6-h Time-Restricted Feeding on Weight and Cardiometabolic Health: A Randomized Controlled Trial in Adults with Obesity. Cell Metab 2020, 32, 366–378 e363. [Google Scholar] [CrossRef]
- Liu, D.; Huang, Y.; Huang, C.; Yang, S.; Wei, X.; Zhang, P.; Guo, D.; Lin, J.; Xu, B.; Li, C. , et al. Calorie Restriction with or without Time-Restricted Eating in Weight Loss. N Engl J Med 2022, 386, 1495–1504. [Google Scholar] [CrossRef] [PubMed]
- Pavlou, V.; Cienfuegos, S.; Lin, S.; Ezpeleta, M.; Ready, K.; Corapi, S.; Wu, J.; Lopez, J.; Gabel, K.; Tussing-Humphreys, L. , et al. Effect of Time-Restricted Eating on Weight Loss in Adults With Type 2 Diabetes: A Randomized Clinical Trial. JAMA Netw Open 2023, 6, e2339337. [Google Scholar] [CrossRef] [PubMed]
- Tsameret, S.; Chapnik, N.; Froy, O. Effect of early vs. late time-restricted high-fat feeding on circadian metabolism and weight loss in obese mice. Cell Mol Life Sci 2023, 80, 180. [Google Scholar] [CrossRef] [PubMed]
- Hutchison, A.T.; Regmi, P.; Manoogian, E.N.C.; Fleischer, J.G.; Wittert, G.A.; Panda, S.; Heilbronn, L.K. Time-Restricted Feeding Improves Glucose Tolerance in Men at Risk for Type 2 Diabetes: A Randomized Crossover Trial. Obesity (Silver Spring) 2019, 27, 724–732. [Google Scholar] [CrossRef] [PubMed]
- Sutton, E.F.; Beyl, R.; Early, K.S.; Cefalu, W.T.; Ravussin, E.; Peterson, C.M. Early Time-Restricted Feeding Improves Insulin Sensitivity, Blood Pressure, and Oxidative Stress Even without Weight Loss in Men with Prediabetes. Cell Metab 2018, 27, 1212–1221. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Yi, P.; Liu, F. The Effect of Early Time-Restricted Eating vs Later Time-Restricted Eating on Weight Loss and Metabolic Health. J Clin Endocrinol Metab 2023, 108, 1824–1834. [Google Scholar] [CrossRef] [PubMed]
- https://www.abstractsonline.com/pp8/#!/20343/presentation/379; accessed on 23 May 2024.
- https://newsroom.heart.org/news/8-hour-time-restricted-eating-linked-to-a-91-higher-risk-of-cardiovascular-death; accessed on 23 May 2024.
- Rynders, C.A.; Thomas, E.A.; Zaman, A.; Pan, Z.; Catenacci, V.A.; Melanson, E.L. Effectiveness of Intermittent Fasting and Time-Restricted Feeding Compared to Continuous Energy Restriction for Weight Loss. Nutrients 2019, 11. [Google Scholar] [CrossRef]
- Patikorn, C.; Roubal, K.; Veettil, S.K.; Chandran, V.; Pham, T.; Lee, Y.Y.; Giovannucci, E.L.; Varady, K.A.; Chaiyakunapruk, N. Intermittent Fasting and Obesity-Related Health Outcomes: An Umbrella Review of Meta-analyses of Randomized Clinical Trials. JAMA Netw Open 2021, 4, e2139558. [Google Scholar] [CrossRef]
- Varady, K.A.; Hellerstein, M.K. Alternate-day fasting and chronic disease prevention: a review of human and animal trials. Am J Clin Nutr 2007, 86, 7–13. [Google Scholar] [CrossRef] [PubMed]
- Heilbronn, L.K.; Ravussin, E. Calorie restriction and aging: review of the literature and implications for studies in humans. Am J Clin Nutr 2003, 78, 361–369. [Google Scholar] [CrossRef]
- Kritchevsky, D. Caloric restriction and cancer. J Nutr Sci Vitaminol (Tokyo) 2001, 47, 13–19. [Google Scholar] [CrossRef]
- Manco, M.; Mingrone, G. Effects of weight loss and calorie restriction on carbohydrate metabolism. Curr Opin Clin Nutr Metab Care 2005, 8, 431–439. [Google Scholar] [CrossRef]
- Minamiyama, Y.; Bito, Y.; Takemura, S.; Takahashi, Y.; Kodai, S.; Mizuguchi, S.; Nishikawa, Y.; Suehiro, S.; Okada, S. Calorie restriction improves cardiovascular risk factors via reduction of mitochondrial reactive oxygen species in type II diabetic rats. J Pharmacol Exp Ther 2007, 320, 535–543. [Google Scholar] [CrossRef]
- Heilbronn, L.K.; Civitarese, A.E.; Bogacka, I.; Smith, S.R.; Hulver, M.; Ravussin, E. Glucose tolerance and skeletal muscle gene expression in response to alternate day fasting. Obes Res 2005, 13, 574–581. [Google Scholar] [CrossRef]
- Halberg, N.; Henriksen, M.; Soderhamn, N.; Stallknecht, B.; Ploug, T.; Schjerling, P.; Dela, F. Effect of intermittent fasting and refeeding on insulin action in healthy men. J Appl Physiol (1985) 2005, 99, 2128–2136. [Google Scholar] [CrossRef]
- Hsieh, E.A.; Chai, C.M.; Hellerstein, M.K. Effects of caloric restriction on cell proliferation in several tissues in mice: role of intermittent feeding. Am J Physiol Endocrinol Metab 2005, 288, E965–972. [Google Scholar] [CrossRef]
- Anson, R.M.; Guo, Z.; de Cabo, R.; Iyun, T.; Rios, M.; Hagepanos, A.; Ingram, D.K.; Lane, M.A.; Mattson, M.P. Intermittent fasting dissociates beneficial effects of dietary restriction on glucose metabolism and neuronal resistance to injury from calorie intake. Proc Natl Acad Sci U S A 2003, 100, 6216–6220. [Google Scholar] [CrossRef] [PubMed]
- Hohn, S.; Dozieres-Puyravel, B.; Auvin, S. History of dietary treatment: Guelpa & Marie first report of intermittent fasting for epilepsy in 1911. Epilepsy Behav 2019, 94, 277–280. [Google Scholar] [CrossRef]
- Wiersielis, K.; Yasrebi, A.; Degroat, T.J.; Knox, N.; Rojas, C.; Feltri, S.; Roepke, T.A. Intermittent fasting disrupts hippocampal-dependent memory and norepinephrine content in aged male and female mice. Physiol Behav 2024, 275, 114431. [Google Scholar] [CrossRef] [PubMed]
- Fernandez-Rodriguez, R.; Martinez-Vizcaino, V.; Mesas, A.E.; Notario-Pacheco, B.; Medrano, M.; Heilbronn, L.K. Does intermittent fasting impact mental disorders? A systematic review with meta-analysis. Crit Rev Food Sci Nutr 2023, 63, 11169–11184. [Google Scholar] [CrossRef] [PubMed]
- Barati, M.; Ghahremani, A.; Namdar Ahmadabad, H. Intermittent fasting: A promising dietary intervention for autoimmune diseases. Autoimmun Rev 2023, 22, 103408. [Google Scholar] [CrossRef]
- Catenacci, V.A.; Pan, Z.; Ostendorf, D.; Brannon, S.; Gozansky, W.S.; Mattson, M.P.; Martin, B.; MacLean, P.S.; Melanson, E.L.; Troy Donahoo, W. A randomized pilot study comparing zero-calorie alternate-day fasting to daily caloric restriction in adults with obesity. Obesity (Silver Spring) 2016, 24, 1874–1883. [Google Scholar] [CrossRef]
- Varady, K.A.; Bhutani, S.; Church, E.C.; Klempel, M.C. Short-term modified alternate-day fasting: a novel dietary strategy for weight loss and cardioprotection in obese adults. Am J Clin Nutr 2009, 90, 1138–1143. [Google Scholar] [CrossRef] [PubMed]
- Hoddy, K.K.; Kroeger, C.M.; Trepanowski, J.F.; Barnosky, A.; Bhutani, S.; Varady, K.A. Meal timing during alternate day fasting: Impact on body weight and cardiovascular disease risk in obese adults. Obesity (Silver Spring) 2014, 22, 2524–2531. [Google Scholar] [CrossRef] [PubMed]
- Trepanowski, J.F.; Kroeger, C.M.; Barnosky, A.; Klempel, M.; Bhutani, S.; Hoddy, K.K.; Rood, J.; Ravussin, E.; Varady, K.A. Effects of alternate-day fasting or daily calorie restriction on body composition, fat distribution, and circulating adipokines: Secondary analysis of a randomized controlled trial. Clin Nutr 2018, 37, 1871–1878. [Google Scholar] [CrossRef] [PubMed]
- Conley, M.; Le Fevre, L.; Haywood, C.; Proietto, J. Is two days of intermittent energy restriction per week a feasible weight loss approach in obese males? A randomised pilot study. Nutr Diet 2018, 75, 65–72. [Google Scholar] [CrossRef]
- Kalam, F.; Gabel, K.; Cienfuegos, S.; Wiseman, E.; Ezpeleta, M.; Steward, M.; Pavlou, V.; Varady, K.A. Alternate day fasting combined with a low-carbohydrate diet for weight loss, weight maintenance, and metabolic disease risk reduction. Obes Sci Pract 2019, 5, 531–539. [Google Scholar] [CrossRef] [PubMed]
- Hutchison, A.T.; Liu, B.; Wood, R.E.; Vincent, A.D.; Thompson, C.H.; O'Callaghan, N.J.; Wittert, G.A.; Heilbronn, L.K. Effects of Intermittent Versus Continuous Energy Intakes on Insulin Sensitivity and Metabolic Risk in Women with Overweight. Obesity (Silver Spring) 2019, 27, 50–58. [Google Scholar] [CrossRef] [PubMed]
- Sundfor, T.M.; Svendsen, M.; Tonstad, S. Effect of intermittent versus continuous energy restriction on weight loss, maintenance and cardiometabolic risk: A randomized 1-year trial. Nutr Metab Cardiovasc Dis 2018, 28, 698–706. [Google Scholar] [CrossRef] [PubMed]
- Cho, A.R.; Moon, J.Y.; Kim, S.; An, K.Y.; Oh, M.; Jeon, J.Y.; Jung, D.H.; Choi, M.H.; Lee, J.W. Effects of alternate day fasting and exercise on cholesterol metabolism in overweight or obese adults: A pilot randomized controlled trial. Metabolism 2019, 93, 52–60. [Google Scholar] [CrossRef] [PubMed]
- Li, C.; Sadraie, B.; Steckhan, N.; Kessler, C.; Stange, R.; Jeitler, M.; Michalsen, A. Effects of A One-week Fasting Therapy in Patients with Type-2 Diabetes Mellitus and Metabolic Syndrome - A Randomized Controlled Explorative Study. Exp Clin Endocrinol Diabetes 2017, 125, 618–624. [Google Scholar] [CrossRef]
- Corley, B.T.; Carroll, R.W.; Hall, R.M.; Weatherall, M.; Parry-Strong, A.; Krebs, J.D. Intermittent fasting in Type 2 diabetes mellitus and the risk of hypoglycaemia: a randomized controlled trial. Diabet Med 2018, 35, 588–594. [Google Scholar] [CrossRef]
- Gabel, K.; Kroeger, C.M.; Trepanowski, J.F.; Hoddy, K.K.; Cienfuegos, S.; Kalam, F.; Varady, K.A. Differential Effects of Alternate-Day Fasting Versus Daily Calorie Restriction on Insulin Resistance. Obesity (Silver Spring) 2019, 27, 1443–1450. [Google Scholar] [CrossRef] [PubMed]
- Parvaresh, A.; Razavi, R.; Abbasi, B.; Yaghoobloo, K.; Hassanzadeh, A.; Mohammadifard, N.; Safavi, S.M.; Hadi, A.; Clark, C.C.T. Modified alternate-day fasting vs. calorie restriction in the treatment of patients with metabolic syndrome: A randomized clinical trial. Complement Ther Med 2019, 47, 102187. [Google Scholar] [CrossRef] [PubMed]
- Guo, Y.; Luo, S.; Ye, Y.; Yin, S.; Fan, J.; Xia, M. Intermittent Fasting Improves Cardiometabolic Risk Factors and Alters Gut Microbiota in Metabolic Syndrome Patients. J Clin Endocrinol Metab 2021, 106, 64–79. [Google Scholar] [CrossRef] [PubMed]
- Kroemer, G.; Lopez-Otin, C.; Madeo, F.; de Cabo, R. Carbotoxicity-Noxious Effects of Carbohydrates. Cell 2018, 175, 605–614. [Google Scholar] [CrossRef]
- Tang, D.; Tao, S.; Chen, Z.; Koliesnik, I.O.; Calmes, P.G.; Hoerr, V.; Han, B.; Gebert, N.; Zornig, M.; Loffler, B. , et al. Dietary restriction improves repopulation but impairs lymphoid differentiation capacity of hematopoietic stem cells in early aging. J Exp Med 2016, 213, 535–553. [Google Scholar] [CrossRef] [PubMed]
- Villareal, D.T.; Fontana, L.; Das, S.K.; Redman, L.; Smith, S.R.; Saltzman, E.; Bales, C.; Rochon, J.; Pieper, C.; Huang, M. , et al. Effect of Two-Year Caloric Restriction on Bone Metabolism and Bone Mineral Density in Non-Obese Younger Adults: A Randomized Clinical Trial. J Bone Miner Res 2016, 31, 40–51. [Google Scholar] [CrossRef] [PubMed]
- Ballon, A.; Neuenschwander, M.; Schlesinger, S. Breakfast Skipping Is Associated with Increased Risk of Type 2 Diabetes among Adults: A Systematic Review and Meta-Analysis of Prospective Cohort Studies. J Nutr 2019, 149, 106–113. [Google Scholar] [CrossRef] [PubMed]
- Sievert, K.; Hussain, S.M.; Page, M.J.; Wang, Y.; Hughes, H.J.; Malek, M.; Cicuttini, F.M. Effect of breakfast on weight and energy intake: systematic review and meta-analysis of randomised controlled trials. BMJ 2019, 364, l42. [Google Scholar] [CrossRef] [PubMed]
- Stekovic, S.; Hofer, S.J.; Tripolt, N.; Aon, M.A.; Royer, P.; Pein, L.; Stadler, J.T.; Pendl, T.; Prietl, B.; Url, J. , et al. Alternate Day Fasting Improves Physiological and Molecular Markers of Aging in Healthy, Non-obese Humans. Cell Metab 2019, 30, 462–476 e466. [Google Scholar] [CrossRef] [PubMed]
- Kang, S.M.; Yoon, J.W.; Ahn, H.Y.; Kim, S.Y.; Lee, K.H.; Shin, H.; Choi, S.H.; Park, K.S.; Jang, H.C.; Lim, S. Android fat depot is more closely associated with metabolic syndrome than abdominal visceral fat in elderly people. PLoS One 2011, 6, e27694. [Google Scholar] [CrossRef]
- Kelli, H.M.; Corrigan, F.E., 3rd; Heinl, R.E.; Dhindsa, D.S.; Hammadah, M.; Samman-Tahhan, A.; Sandesara, P.; O'Neal, W.T.; Al Mheid, I.; Ko, Y.A. , et al. Relation of Changes in Body Fat Distribution to Oxidative Stress. Am J Cardiol 2017, 120, 2289–2293. [Google Scholar] [CrossRef] [PubMed]
- Schafer, A.L. Decline in Bone Mass During Weight Loss: A Cause for Concern? J Bone Miner Res 2016, 31, 36–39. [Google Scholar] [CrossRef] [PubMed]
- Meydani, S.N.; Das, S.K.; Pieper, C.F.; Lewis, M.R.; Klein, S.; Dixit, V.D.; Gupta, A.K.; Villareal, D.T.; Bhapkar, M.; Huang, M. , et al. Long-term moderate calorie restriction inhibits inflammation without impairing cell-mediated immunity: a randomized controlled trial in non-obese humans. Aging (Albany NY) 2016, 8, 1416–1431. [Google Scholar] [CrossRef] [PubMed]
- Newman, J.C.; Covarrubias, A.J.; Zhao, M.; Yu, X.; Gut, P.; Ng, C.P.; Huang, Y.; Haldar, S.; Verdin, E. Ketogenic Diet Reduces Midlife Mortality and Improves Memory in Aging Mice. Cell Metab 2017, 26, 547–557 e548. [Google Scholar] [CrossRef]
- Rozing, M.P.; Westendorp, R.G.; de Craen, A.J.; Frolich, M.; Heijmans, B.T.; Beekman, M.; Wijsman, C.; Mooijaart, S.P.; Blauw, G.J.; Slagboom, P.E. , et al. Low serum free triiodothyronine levels mark familial longevity: the Leiden Longevity Study. J Gerontol A Biol Sci Med Sci 2010, 65, 365–368. [Google Scholar] [CrossRef]
| IF method | Features | References |
|---|---|---|
| ADF Alternate day fasting |
A day of eating is alternate to a day ad libitum is alternate to a day of fasting (25% of usual food intake, approximately 500 kcal) | [64] |
| IF 5:2 | A five-days with normal eating and two days of severe fasting (food intake restricted to 500 - 800 cal) | [57] |
| FMD Fasting-mimicking diet |
A five-day fasting dietary regimen centered around natural, healthful items and ingredients (healthy fats and fiber-rich carbohydrate) with no refined carbohydrate (25% of usual food intake and less than 10% of protein) | [65,66] |
| PF Periodic fasting |
Water-only fasting or FMD for at least two days in succession repeated each month (involves a maximum daily energy intake of 250 kcal for about one week – 5-day diet affording 750-1100 kcal) | [67] |
| TRF Time-restricting feeding |
Daily no energy intake (or restricted amount) for 12 - 20 h, with eating window of 4 - 12 h (reduction of at least 20% of caloric intake) | [68] |
| eTRF Early time-restricting feeding |
Modified TRF in which calories restriction occurs in the first 6 -8 h of the day (i.e., eating window starts at 08:00 a. m. to at the maximum 02:00 p.m.) | [69] |
| lTRF Late time-restricting feeding |
Modified TRF in which the eating window starts late in the day, usually from 02:00 p. m. to at the maximum 08:00 p.m.) | [70] |
| Clinical trial | Participants | Trials weeks | Intervention |
Body weight (kg) |
WC |
Blood pressure (mmHg) |
Plasma lipids (mg/dL) |
Glucoregulatory factors (mg/dL) |
Adherence and tolerability | Ref | ||
| Overweight and obese | UIC-004-2009 | 16 obese subjects (12 females, 4 males); age 35–65 y, BMI 30 -39.9 kg/m2 | 10 | 3 intervention phases: • 2-w pre-loss control phase (usual eating and exercise habits) • 4-w weight loss/ADF controlled food intake phase (25% of energy needs on the fast day (24 h) and ad libitum food on each alternate feed day (24 h)) • 4-w weight loss/ADF self-selected food intake phase (25% of energy needs on the fast day and ad libitum food on the feed day) |
-5.8 | NA | SBP -9.5 | TG -38 | FI NA |
No drop in adherence during the different phases | [115] | |
| TC -37 | ||||||||||||
| FPG NA |
||||||||||||
| DBP -1.5 | ||||||||||||
| LDL-C -29 | ||||||||||||
| HOMA-IR NA |
||||||||||||
| HDL-C +2 | ||||||||||||
| Randomized, parallel-arm feeding trial | 74 subjects with BMI 30 - 39.9 kg/m2; age 25 - 65 y | 10 | ADF lunch (ADF-L): 25% of baseline energy needs on the fast day (24 h), and ad libitum on each alternating feed day (24 h) |
-3.5 | NA | SBP -2 | TG -6 | FI 0 μIU/mL |
Adherence to the fast day energy goal was similar for each group . Compliance of ADF meal was high in each intervention group | [116] | ||
| TC -1 | ||||||||||||
| FPG -2 | ||||||||||||
| DBP -1 | LDL-C -2 | |||||||||||
| HOMA-IR -0.3 |
||||||||||||
| HDL-C -2 | ||||||||||||
| ADF dinner (ADF-D): 25% of baseline energy needs on the fast day (24 h), and ad libitum on each alternating feed day (24 h) |
-4.1kg | NA | SBP -5 | TG -9 | FI -2 μIU/mL |
|||||||
| TC -5 | ||||||||||||
| FPG -1 | ||||||||||||
| DBP -3 | LDL-C 0 | |||||||||||
| HOMA-IR -0.8 |
||||||||||||
| HDL-C 0 | ||||||||||||
| ADF-small meals (ADF-SM): 25% of baseline energy needs on the fast day (24 h), and ad libitum on each alternating feed day (24 h) |
-4kg | NA | SBP -6 | TG -1 | FI -2 μIU/mL |
|||||||
| TC -1 | ||||||||||||
| FPG -2 | ||||||||||||
| DBP -1 | LDL-C +1 | |||||||||||
| HOMA-IR -0.8 |
||||||||||||
| HDL-C -1 | ||||||||||||
| Pilot study | 26 subjects, aged 18 -55 y; BMI 30 kg/m2 | 8 | zero-calorie ADF (n =14) | -8.2 | NA | SBP NA | TG -25 | FI +3 μU/mL FPG +6 HOMA-IR NA |
No relevant safety changes over the 8-w; zero-cal ADF is safe and tolerable and not associated with weight regain after 24 w of follow-up | [114] | ||
| TC -31.8 | ||||||||||||
| DBP NA | LDL-C -22.6 |
|||||||||||
| HDL-C -4.2 |
||||||||||||
| CR (n=12): -400 kcal/day | -7.1 | NA | SBP NA |
TG -2.8 | FI -0.2 μU/mL FPG +3.3mg/dl HOMA-IR NA |
|||||||
| TC -21.7 | ||||||||||||
| DBP NA |
LDL-C -16.9 |
|||||||||||
| HDL-C -4.2 |
||||||||||||
| Randomized controlled trial NCT00960505. |
79 subjects, BMI 25 -40 kg/m2; men and women aged 18-65 y | 24 (12 Control feeding period, 12 self-selected feeding) |
ADF (n=25) alternating every 24-h between consuming 25% or 125% of energy needs |
NA | NA | SBP NA |
TG NA |
FI -7.4 μIU/mL |
NA | [117] | ||
| TC NA |
||||||||||||
| FPG 0 | ||||||||||||
| DBP NA |
LDL-C NA |
|||||||||||
|
HOMA-IR -1.88 |
||||||||||||
| HDL-C NA |
||||||||||||
| CR(n=29) consuming 75% of needs every day |
NA | NA | SBP NA |
TG NA |
FI -4.4 μIU/mL |
|||||||
| TC NA |
||||||||||||
| FPG +5.2 | ||||||||||||
| DBP NA |
LDL-C NA |
|||||||||||
| HOMA-IR -0.79 |
||||||||||||
| HDL-C NA |
||||||||||||
| CONTROL (n=25) consuming 100% of needs every day |
NA | NA | SBP NA |
TG NA |
FI +0.6 μIU/mL |
|||||||
| TC NA |
||||||||||||
| FPG +5.2 |
||||||||||||
| DBP NA |
LDL-C NA |
|||||||||||
| HOMA-IR +0.5 |
||||||||||||
| HDL-C NA |
||||||||||||
| Randomized, controlled, long-term study www.clinicaltrials.gov NCT02480504. |
112 subjects, aged 21-70 y; BMI 30-45 kg/m2 | 1 y (6 months weight loss, 6 months weight maintenance) |
5:2 approach consumption of 400/600 kcal (female/male) on each of two nonconsecutive days a week and to consume food as usual the remaining five days a week |
-9.1 | -8 | SBP -1.9 | TG -0.31 mmol/L |
FI NA |
None of the participants withdrew. Participants in the IF group reported stronger feelings of hunger. Adverse events and larger weight regain than in the CR group |
[121] | ||
| TC +0.7 mmol/L |
||||||||||||
| FPG -0.2 mmol/L |
||||||||||||
| DBP -3 | ||||||||||||
| LDL-C -0.03 mmol/L |
||||||||||||
| HOMA-IR NA |
||||||||||||
| HDL-C +0.13 mmol/L |
||||||||||||
| CR reduction of energy intake seven days a week |
-9.4 | -9.2 | SBP -3.6 | TG -0.11 mmol/L |
FI NA |
|||||||
| TC +0.17 mmol/L |
||||||||||||
| FPG 0 mmol/L |
||||||||||||
| DBP -2.9 | ||||||||||||
| LDL-C +0.08 mmol/L |
||||||||||||
| HOMA-IR NA |
||||||||||||
| HDL-C +0.13 mmol/L |
||||||||||||
| Single-centre, parallel group randomized controlled trial ACTRN12614000396628 |
23 males, aged 55–75 y, BMI ≥ 30 kg/m2 | 6 months | 5:2 approach n=11 restricted daily calorie intake to 600 cal on the fast day for two non-consecutive days per week and eat ad libitum on the remaining 5 days |
-5.3 | -8 | SBP -14 | TG -0.3 mmol/L |
FI NA |
No adverse side effects experienced in either dietary group. Over half of participants on the 5:2 diet experienced hunger after 2 w with slight progress over time- Compliance rates were similar in both dietary groups |
[118] | ||
| TC 0 mmol/L |
||||||||||||
| FPG -0.1 mmol/L |
||||||||||||
| DBP -0.2 | LDL-C -0.09 mml/L |
|||||||||||
| HOMA-IR NA |
||||||||||||
| HDL-C +0.04 mmol/L |
||||||||||||
| SERD (standard energy-reduced diet) n=12continuous daily energy-restricted diet (500- cal daily reduction from average requirement) | -5.5 | -6.4 | SBP -10.2 | TG -0.2 mmol/L |
FI NA |
|||||||
| TC +0.2 mmol/L |
||||||||||||
| FPG -0.2 mmol/L |
||||||||||||
| DBP -3.7 | LDL-C -0.45 mmol/L |
|||||||||||
| HOMA-IR NA |
||||||||||||
| HDL-C 0 mmol/L |
||||||||||||
| Randomized, controlled, parallel-arm diet trial NCT0365253 | 31 subjects, aged 20–65 y; BMI >23 kg/m2 | 8 | E-ADF (ADF and exercise) 25% of daily recommended energy intake (approximately 500 kcal) on each fast day (24 h), and food ad libitum on each feed day (24 h). The fast day and feed day were repeated every other day, and the fast day occurred 3 days per week. Exercise - training and aerobic exercise. |
-3.9 | NA | SBP NA |
TG -43.6 | FI -3.87 μIU/mL |
NA | [122] | ||
| TC +15.1 | ||||||||||||
| FPG -14.1 |
||||||||||||
| DBP NA |
LDL-C +17.8 | |||||||||||
| HOMA-IR -1.12 |
||||||||||||
| HDL-C +6 | ||||||||||||
| ADF 25% of daily energy intake (approximately 500 kcal) on each fast day (24 h), and food ad libitum on each feed day (24 h). The fast day and feed day were repeated every other day, and the fast day occurred 3 days per week |
-3.9 | NA | SBP NA |
TG +12.6 | FI +3.21 μIU/mL |
|||||||
| TC +5.4 | ||||||||||||
| FPG -9.7 |
||||||||||||
| DBP NA |
||||||||||||
| LDL-C 0 |
||||||||||||
| HOMA-IR +0.68 |
||||||||||||
| HDL-C +2.9 |
||||||||||||
| EXERCISE exercise intervention included resistance training and aerobic exercise. |
-2 | NA | SBP NA |
TG -87.9l | FI +0.04 μIU/mL |
|||||||
| TC +20.3 | ||||||||||||
| FPG -1.3 |
||||||||||||
| DBP NA |
LDL-C +26.7 |
|||||||||||
| HOMA-IR +0.01 |
||||||||||||
| HDL-C +11.2 |
||||||||||||
| CONTROL | -0.2 | NA | SBP NA |
TG +53.2 |
FI +5.19 μIU/mL |
|||||||
| TC +33.2 |
||||||||||||
| FPG -4 |
||||||||||||
| DBP NA |
LDL-C +16.9 |
|||||||||||
| HOMA-IR +1.10 |
||||||||||||
| HDL-C +5.7 |
||||||||||||
| Longitudinal study | 31 subjects, BMI 30-49.9 kg/m2; aged 18 - 65 y | 6 months (3 months weight-loss, 3 months weight-maintenance) | ADF low-carbohydrate intervention | -5.5 | NA | SBP -7 | TG -14 | FI -4 μIU/mL |
Adherence was high amongst those who completed the study. High dropout (40%), particularly in the first few months of intervention | [119] | ||
| TC -12 | ||||||||||||
| FPG 0 |
||||||||||||
| DBP -4 | LDL-C -10l |
|||||||||||
| HOMA-IR -0.7 |
||||||||||||
| HDL-C -2 |
||||||||||||
| T2DM | Non-blinded randomized parallel group interventional trial ACTRN12614000402640 | 37 subjects aged >18 y with T2DM treated with metformin and/or any combination of hypoglycemic agents, HbA1c 50–86 mmol/mol; 15 females and 22 males. | 12 | Diet with consecutive fasting days (n = 18) |
-3.1 | -1.6 | SBP -3 | TG +0.1 mmol/dL | FI NA |
Hypoglycemic events (53) during 84 days of observation affecting 15 participants which required further medication adjustments in 9 out of 37 subjects | [124] | |
| TC +0.1 mmol/dL | ||||||||||||
| FPG -1.3 mmol/dL |
||||||||||||
| DBP -2 | LDL-C +0.15 mmol/dL |
|||||||||||
| HOMA-IR NA |
||||||||||||
| HDL-C +0.1 mmol/dL |
||||||||||||
| Diet with non-consecutive fasting days (n = 19) |
-3.6 | -3.4 | SBP -4 | TG 0.1 mmol/dL |
FI NA |
|||||||
| TC -0.4 mmol/dL |
||||||||||||
| FPG -1.1 mmol/dL |
||||||||||||
| DBP -3 | ||||||||||||
| LDL-C -0.1 mmol/dL |
||||||||||||
| HOMA-IR NA |
||||||||||||
| HDL-C 0 mmol/dL |
||||||||||||
| NCT00960505. | 43 insulin-resistant individuals, aged 18 - 65 y, BMI 25-39.9 kg/m2 | 12 months | ADF (n=11) • 6 months weight-loss: 25% of baseline energy needs as a lunch on fast days and 125% of baseline energy needs over three meals on alternating feast days • 6 months maintenance phase: 50% of energy needs as a lunch on fast days and 150% of energy needs over three meals on alternating feast days |
-8 | NA | SBP -9 | TG -27 | FI -12 μIU/mL |
ADF participants consumed almost twice as many calories on fast days but still observed greater metabolic effects compared with CR participants | [125] | ||
| TC +4 | ||||||||||||
| FPG -3 |
||||||||||||
| DBP -5 | LDL-C +7 |
|||||||||||
| HOMA-IR -3 |
||||||||||||
| HDL-C +3 |
||||||||||||
| CR (n=17) • 6 months weight-loss: 75% of baseline energy needs over three meals every day • 6 months maintenance phase: 100% of energy needs over three meals every day |
-5 | NA | SBP -7mmHg |
TG -6 | FI -1 μIU/mL |
|||||||
| TC -6 | ||||||||||||
| FPG -4 |
||||||||||||
| DBP -2 | LDL-C -6 |
|||||||||||
| HOMA-IR -0.9 |
||||||||||||
| HDL-C +2 |
||||||||||||
| CONTROL (n=15) not changing usual eating and activity habits |
0kg | NA | SBP -1 | TG -8 | FI -3 μIU/mL |
|||||||
| TC -1 | ||||||||||||
| FPG +4 |
||||||||||||
| DBP -3 | LDL-C 0 |
|||||||||||
| HOMA-IR 0.5 |
||||||||||||
| HDL-C +2 |
||||||||||||
| Randomized controlled clinical pilot study | 32 subjects, aged 25 - 75 y with a manifest and treated T2DM | 7 days of intervention 4 months trial |
ADF n=16 2 pre-fasting days with moderate caloric restriction (approx. 1200 kcal) followed by 7 modified fasting days with nutritional energy intake of 300 kcal/day by liquids only and subsequent stepwise re-introduction of ordinary food items over 3 days |
-3.5 | -4.4 | SBP -13.9 | TG -26.6 | FI -3.5 μU/mL |
Fasting was well accepted, no serious adverse events. | [123] | ||
| TC -0.5 | ||||||||||||
| FPG -10.6 |
||||||||||||
| DBP -9 | LDL-C -2.6 l |
|||||||||||
| HOMA-IR -1.5 |
||||||||||||
| HDL-C +6.5 |
||||||||||||
| CONTROL n=16 following the principles of a Mediterranean diet |
-2 | -0.3 | SPB +0.4 | TG -2.5 | FI -0.2 μU/mL |
|||||||
| TC -15.5 | ||||||||||||
| FPG -38.4 |
||||||||||||
| DBP +3.2 | LDL-C -7.8 |
|||||||||||
| HOMA-IR -1.5 |
||||||||||||
| HDL-C -2.3 |
||||||||||||
| Metabolic syndrome | Single-center, randomized clinical trial IRCT201509092395N8 | 69 subjects, aged 25–60 y overweight (BMI 25-40 kg/m2), 41 males and 28 femalesdiagnosed with MetS | 8 - |
ADF n=35 75% energy restriction during 3 fast days and 100% of energy needs on feed day |
-4.1 | -4 | SBP -13 | TG -52 | FI -2.41 μU/mL |
no complaint due to difficulties with diet adherence |
[126] | |
| TC -11 | ||||||||||||
| FPG -5 |
||||||||||||
| DBP -8 | LDL-C -5 |
|||||||||||
| HOMA-IR -0.72 |
||||||||||||
| HDL-C 0 |
||||||||||||
| CR n=34 75% of energy needs each day |
-1.7 | -1 | SBP -1 |
TG -40 | FI -1.56 μU/mL |
No complaint due to difficulties with diet adherence | ||||||
| TC -8 | ||||||||||||
| FPG 0 |
||||||||||||
| DBP -5 | LDL-C -1 |
|||||||||||
| HOMA-IR -0.39 |
||||||||||||
| HDL-C 0 |
||||||||||||
| Randomized controlled trial NCT03608800 | 39 subjects with MetS, 21 males and 18 femalesaged 30 - 50 y | 8 | ADF n= 21 75% energy restriction for 2 non-consecutive days a week and an ad libitum diet the other 5 days |
-3.5 | -2.5 | SBP -5.3 |
TG –0.22 | FI NA |
91.3% of participants were compliant | [127] | ||
| TC –0.04 | ||||||||||||
| FGP NA |
||||||||||||
| DBP -2.5 | LDL-C +0.02 |
|||||||||||
| HOMA-IR -0.75 |
||||||||||||
| HDL-C +0.5 |
||||||||||||
| CONTROL n= 18 routine diet without dietary instructions |
-1.2 | -1.1 | SBP -4.9 | TG 0 | FI NA |
78.3% of participants were compliant | ||||||
| TC -0.27 | ||||||||||||
| FGP NA |
||||||||||||
| DBP -2.1 | LDL-C +0.55 |
|||||||||||
| HOMA-IR -0.09 |
||||||||||||
| HDL-C +0.16 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





