1. Introduction
Orthodontic clear aligners offer superior aesthetics and improved hygiene compared to bracket systems. They also demand less chair time and fewer clinical visits, making them more convenient for clinicians. As a result, there is significant current demand for aligners, leading to their widespread use in the dental market [
1,
2]. However, attaining optimal clinical outcomes with aligners relies on optimizing various factors [
3,
4]; including material type [
5], thickness [
6], edge shape, extension [
7], and the degree of activation [
8]. Therefore, enhancing the biomechanical understanding of applied forces is crucial for improving the safety and predictability of aligner treatments, especially considering observed discrepancies between planned and actual outcomes, which may result from inaccuracies in predicting forces applied to teeth [
4]. Furthermore, it is imperative to carefully consider each single factor during manufacturing and application of aligner, based on well-established scientific evidence. This approach will lead to the development of a standardized method for practitioners and companies, ensuring the best treatment outcomes. Additionally, standardizing all studies in the literature will facilitate the comparison of similar research endeavors.
The predominant method of aligner manufacturing in the industry involves deep drawing of a thermoplastic sheet onto a 3D-printed model. This thermoforming process has been noted to significantly influence material properties [
9] and may lead to the thinning of sheets over the model [
10]. A direct relationship has been identified between aligner thickness and force generation [
8,
11]. Various research methods have been employed to assess the mechanics of orthodontic aligners. Pressure-sensitive films have gained broad acceptance in literature and have been used in numerous studies to quantify contact force between aligners and teeth [
10,
12,
13,
14]. Moreover, in several studies [
15,
16], micro-computed tomography (µ-CT) was utilized to achieve precise measurements of aligner thickness.
To date, there is a lack of existing literature documenting the effect of 3D-printed model height, used in deep drawing if orthodontic aligner sheets, on the thermoformed aligner thickness and the force transmitted to the malaligned tooth. Therefore, the originality of the present study lies in addressing this gap through the utilization of pressure-sensitive films, a digital caliper, and µ-CT imaging, and establishing a link among these methods.
2. Materials and Methods
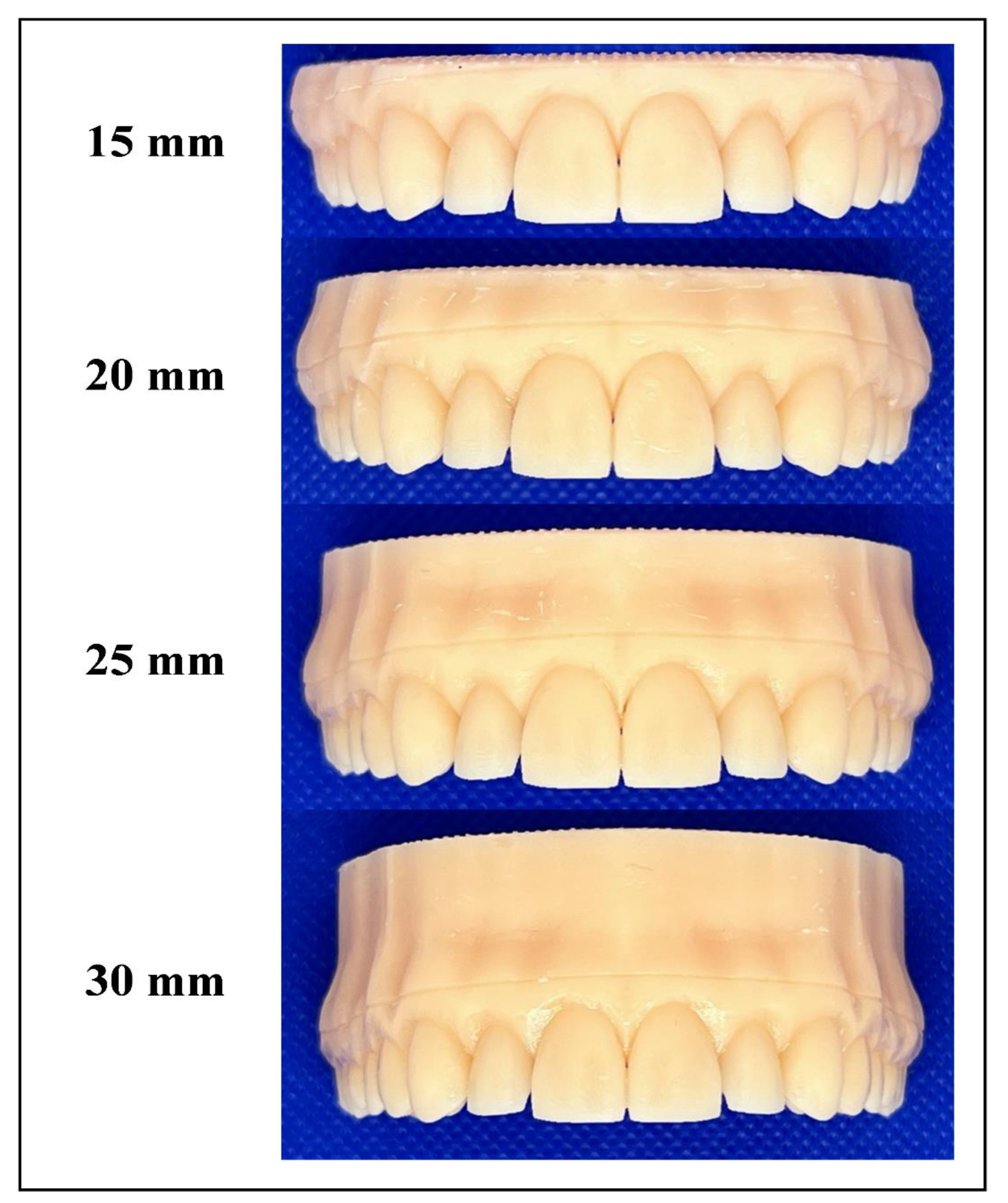
A digital model of an upper full-dentate jaw (Digimation Corp., St Rose, Louisiana, USA) was imported into image processing software (3-matic 17.0; Materialise, Leuven, Belgium). This model served as the basis for designing five distinct models. Four were with aligned teeth, designed for thermoforming purposes, but each had a different height from the occlusal table to the model base, specifically: 15, 20, 25, 30 mm (
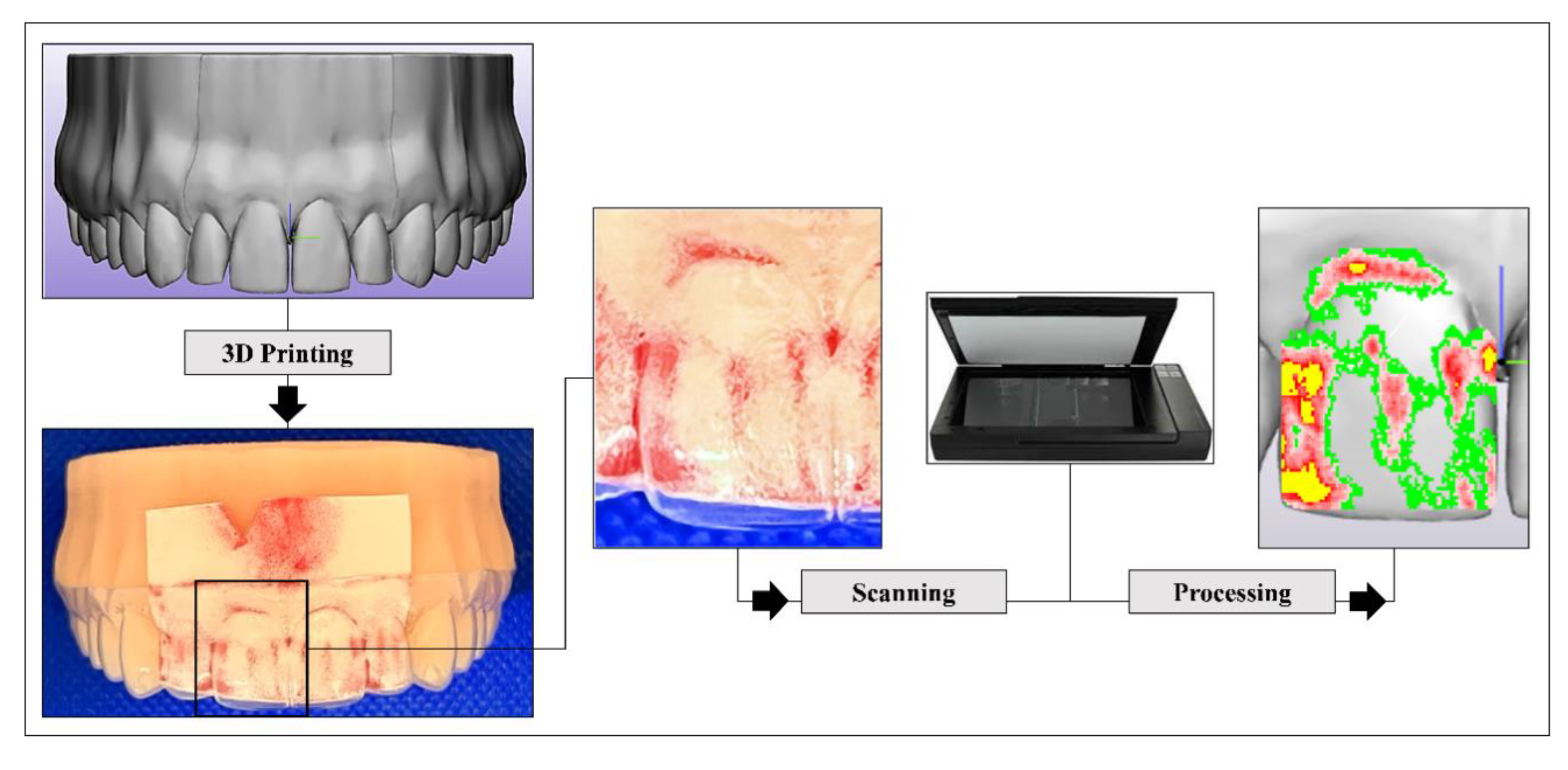
Figure 1). The fifth model, designed for force measurement purposes, intentionally introduced malalignment in the upper right central incisor (Tooth 11), moving it bodily translated facially by 0.2 mm toward the facial side. In this malaligned model, a 100 µm space was incorporated around the four incisors and their corresponding gingival area (housing space) to eliminate the influence of the inherent thickness of the pressure-sensitive films used for force measurements (
Figure 2). All five digital models were exported as STL files to a digital light processing (DLP) 3D printer (P20+; Straumann, Basel, Switzerland) and printed using dental model resin (P pro resin; Straumann, Basel, Switzerland).
Forty aligner sheets made from 0.76 mm thick multilayered thermoplastic sheets (Zendura FLX; Bay Materials LLC, Fremont, CA, USA), were deep-drawn over the four models (n=10) using a thermoforming device (Biostar; Scheu-Dental GmbH, Iserlohn, Germany), and following the manufacturer's guidelines (Code 162; heating for 50 seconds at 220 °C and pressure-forming at 4.8 bar, then cooling for 60 seconds). All aligners were trimmed by a single trained investigator into a straight 2-mm extended design, guided by a shallow pre-designed groove in the model (
Figure 1).
The local normal contact force transmitted by each aligner to the crown of Tooth 11 was recorded using Low Pressure (LW) pressure-sensitive films (Fuji
® Prescale Film; Fuji Film, Tokyo, Japan), following parameters and steps detailed in a recent study [
10]. The films were cautiously seated in the pre-designed housing space in the malaligned model, and then the aligner was inserted carefully to avoid undesirable pressure. Subsequently, each pressurized film was scanned using a specialized scanner (EPSON Perfection V300 series; SEIKO Epson CORPORATION, Japan). Digitalization and quantification of force were performed using specialized software (FPD-8010E analysis system; Fuji® Film, Tokyo, Japan) (
Figure 2).
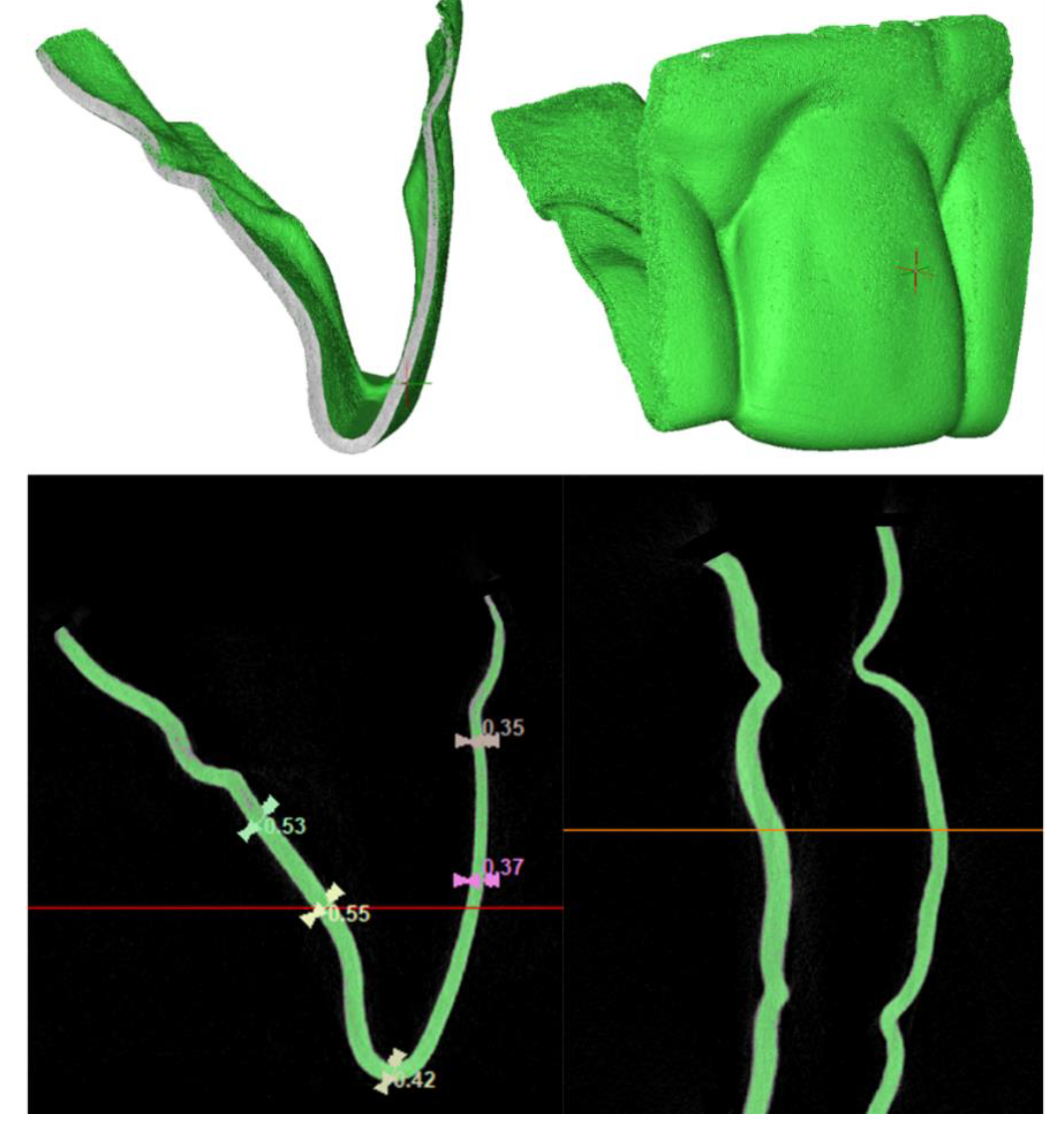
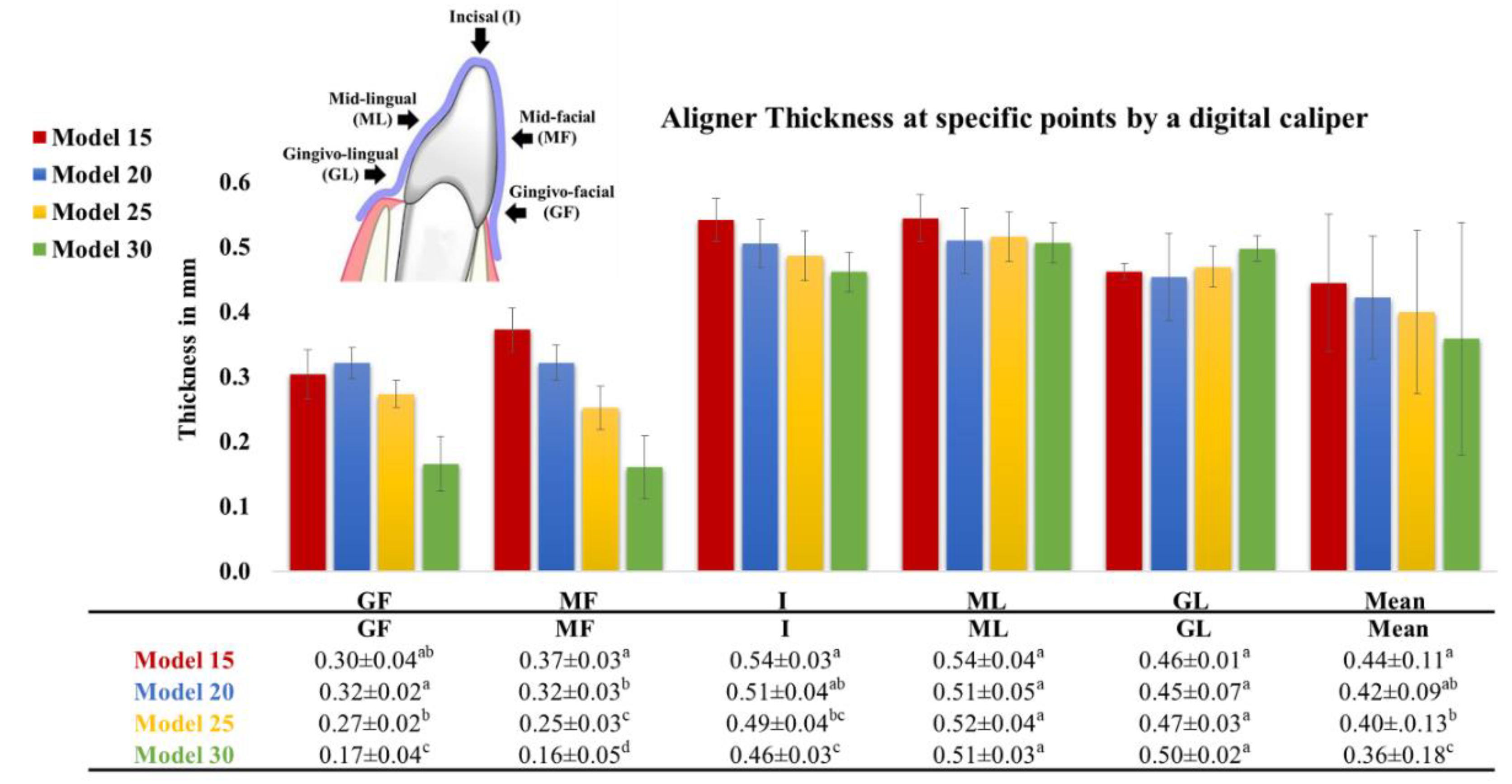
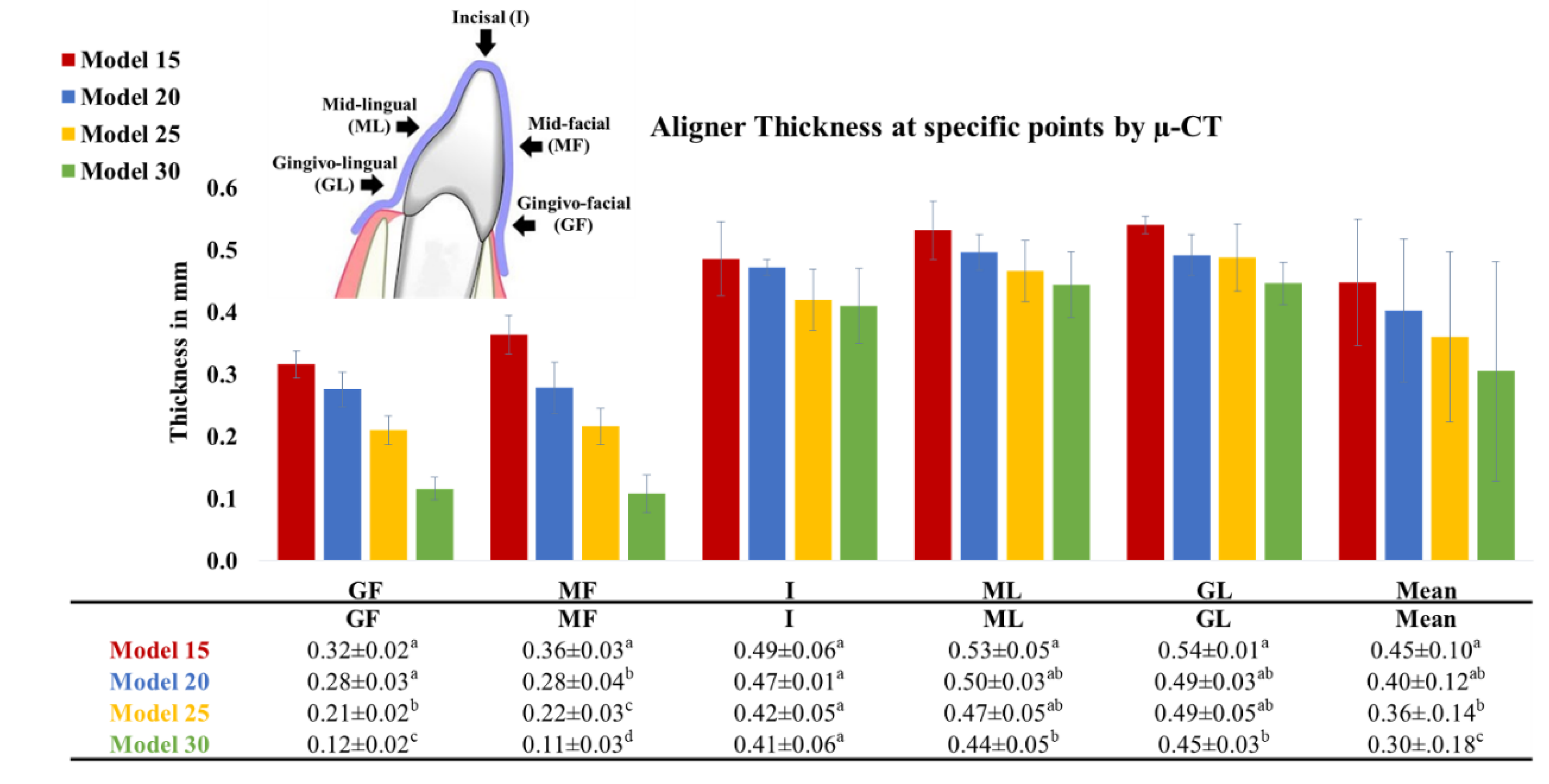
The thickness of the aligners was measured at various reference points (Gingivo-facial (GF), Mid-facial (MF), Incisal (I), Mid-lingual (ML), Gingivo-lingual (GL)) along the midline of the aligner part covering the crown of Tooth 11. Two measurement methods were employed. The first method used a digital caliper (Dial Caliper D; Aura-Dental GmbH, Aura an der Saale, Germany), while the second method employed µ-CT (Skyscan 1174; Skyscan, Kontich, Belgium), with a resolution of 22 μm, an accelerating voltage of 50 kVp, a beam current of 800 μA, an exposure time of 22 seconds, a rotation of 360° at 0.4° angular step, and without using filters. The mean total number of slices was 1018, and the average scanning time was one and a half hours. The 2D data were transferred as DICOM files into a 3D interactive medical image processing system (Mimics 25.0; Materialise, Leuven, Belgium). Mimics provided advanced visualization and segmentation capabilities through image radio-opacity thresholding. An automated process within Mimics allowed the generation of a 3D model for each specimen by expanding a threshold region across the complete stack of scans (
Figure 3). Identifying the optimal radio-opacity threshold was a crucial and highly sensitive step in determining and analyzing the 3D objects.
3. Statistical Analysis
Normality was assessed by examining the data distribution and conducting the Shapiro-Wilk test. The data exhibited a parametric distribution and was presented as mean values with corresponding standard deviations. Statistical analysis was conducted using a one-way ANOVA, followed by post-hoc Tukey HSD Test. The significance level (α) was set at p≤0.05. The statistical analysis was carried out using IBM SPSS Statistics version 25 for Windows (IBM, Endicott, NY, USA).
4. Results
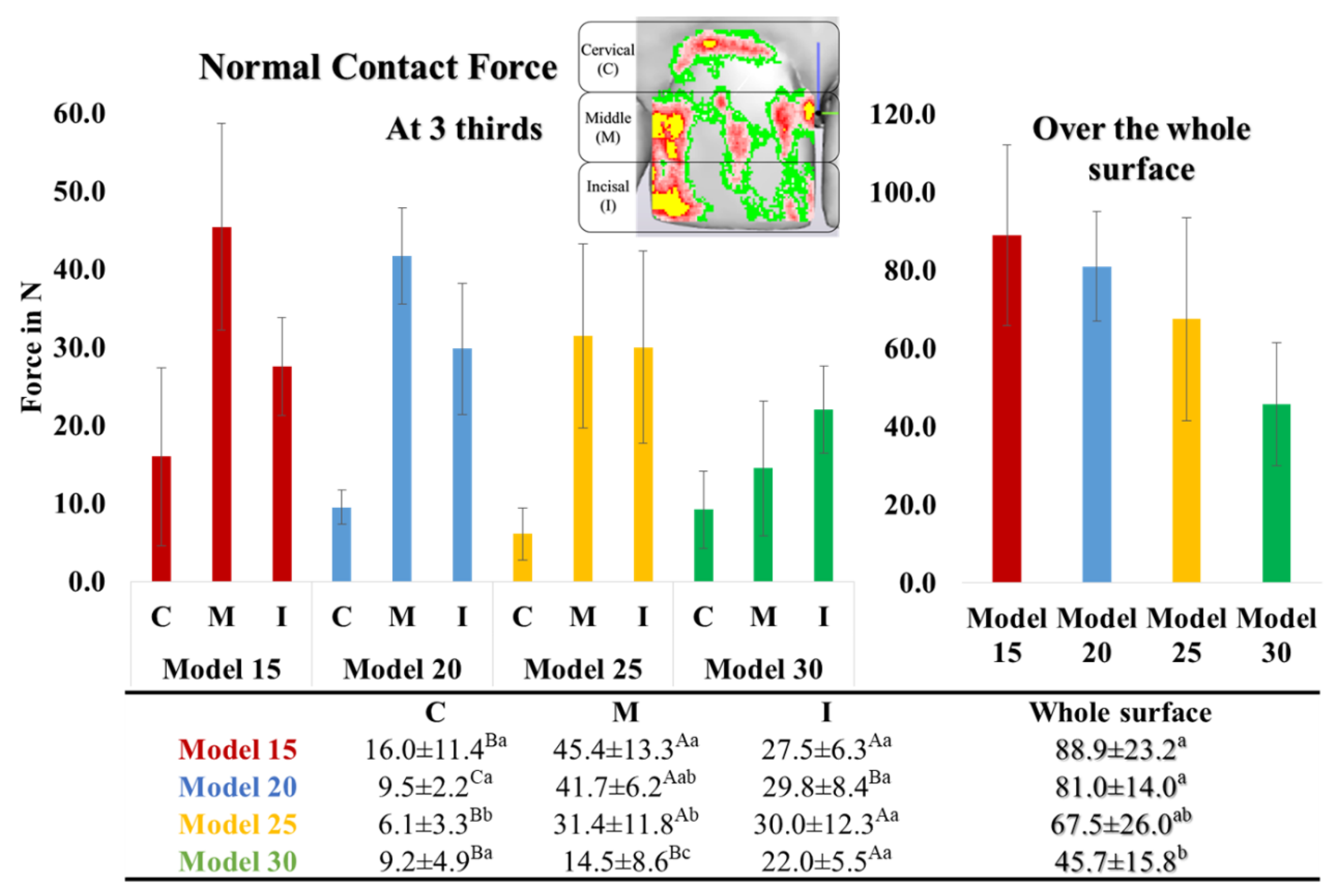
Figure 4 illustrates the local normal contact force across the entire facial surface of the crown of Tooth 11. The pressure-sensitive films recorded force values between 45.7 N to 88.9 N. Among the thermoformed aligners, those made over Model 15 exhibited the highest force, followed by Models 20 and 25, with no statistically significant differences between them. Aligners thermoformed over Model 30 showed the lowest contact force. The distribution of normal contact force was uneven, with certain areas experiencing higher forces than others. When the tooth surface was divided into three equal thirds, it was observed that the normal contact force at the cervical third (F
C) was the lowest. The force at the middle third (F
M) was significantly higher than the force at the incisal third (F
I) and F
C, except in the case of Model 30, in which F
I was the highest (
Figure 4).
As depicted in
Figure 5 and
Figure 6, the thickness measurements obtained using the digital caliper and µ-CT were consistent and mutually validated. The initial thickness of the aligner sheets (0.75 mm) underwent a substantial reduction after thermoforming across the entire tooth surface, averaging between 0.3 to 0.5 mm (33-60% thinning). The least thinning occurred at the incisal edge (I) (0.4-0.5 mm; 30-50% thinning), while the most significant thinning was observed at the gingivo-facial part (GF) (0.1-0.3 mm; 60-85% thinning). Aligner thinning increased notably with increasing model height. There were noticeable differences in aligner thickness across various model heights on the facial surface, however, the differences in aligner thickness were less pronounced at the incisal tip and lingual surface.
5. Discussion
With the widespread utilization of orthodontic aligners, studying their biomechanics becomes crucial to address certain drawbacks and limitations associated with their use. Adopting a scientifically grounded approach in aligner manufacturing and application is essential for achieving optimal treatment outcomes. This study specifically explores the influence of model height, used in thermoforming of aligner sheets, on both force transmission to Tooth 11 and aligner thickness.
Tooth 11 was chosen for this study due to its prevalence in experimental studies reporting forces. This allows for comparisons with other reports in the literature. Aligner treatment achieves incremental tooth movement through a series of aligner splints, each splint is capable of progressively repositioning the target teeth by approximately 0.2 mm for translations. The geometry of the aligner splint has a crucial role in determining the direction and extent of tooth movement. A predefined mismatch between the crown of the treated tooth and the splint generates force in three dimensions exerted on the contact surface between the aligner and the tooth [
4]. However, in this study, the pressure-sensitive films could only measure a one-dimensional normal contact force, which may explain the high recorded force values compared to those documented in the literature (0.5-1.5 N) [
17]. Furthermore, the absence of the periodontal ligament (PDL) and bone in experimental studies contributes to increased force generation. Nevertheless, these factors could be ignored, since all groups were evaluated under the same standard conditions.
A clinical study by Barbagallo et al. [
12] documented force values of approximately 28.0 N when using pressure-sensitive films. The presence of the PDL acts as a cushion that absorbs force, explaining the disparity between clinical and experimental outcomes. An experimental study by Cervinara et al. [
13] reported pressure values around 3.3 MPa, which is comparable to the findings in this study, assuming that the force values result from the product of pressure (MPa) and area (mm
2), and the measured area in the current study was around 40 mm
2. Yet, discrepancies observed across studies may be attributed to differences in material composition [
5], trimming line design [
10], extent and type of tooth activation, and aligner thickness [
8].
The inner surface of the aligner should closely contact the teeth surface to ensure the application of clinically effective force. However, in the present study, the force distribution demonstrated pressure and relief areas on the facial surface of the tooth. This resulted in variations in force levels across different points, aligning with observations from previous reports [
10,
13], This uneven contact and force distribution may be attributed to the topography of the tooth surface, which can differ from one tooth to another.
Consistent with prior studies [
10,
16,
18], the current outcomes showed significant material thinning (60-85%) after the thermoforming process, particularly at the gingival third [
15,
19], and less thinning at the incisal edge. Increased thinning of the aligner contributes to undesirable flexibility and weakening of the margins. Moreover, an increase in model height results in increased thinning of the thermoformed aligner, especially in the cervical areas. This leads to a significant reduction in transmitted force and a modification in force distribution, affecting both the magnitude and type of tooth movement. Principally, a 10% reduction in aligner material thickness could theoretically decrease exerted forces by up to 30%. This is because the moment of inertia is calculated using the third power of the material thickness in the direction of the acting forces [
8,
15].
Reducing of the applied force on the tooth near the gingival area, closer to the center of resistance of the tooth, diminishes the likelihood of accomplishing bodily translation. Conversely, maintaining an appropriate aligner thickness at the gingival margins enhances stiffness, retention, and gingival adaptation. This, in turn, leads to improved force distribution and better control of tooth movement, allowing for greater force application at the gingival area potentially enhancing control over bodily tooth movement [
10,
20,
21]. To prevent additional weakening of the aligner margins, a straight extended trimming line was implemented instead of a scalloped design [
10].
It's worth noting that this experimental study has certain limitations, including the investigation of only one type of aligner material (Zendura FLX, thermoplastic polyurethane-based multilayer sheets). Future studies may consider exploring different materials with varying compositions and thicknesses. Additionally, thickness values may vary depending on the types of teeth and the measurement locations [
15]. Furthermore, factor such as material deformation during aligner placement and material swelling due to exposure to saliva were not considered.
To achieve desired and predictable outcomes, adjustments in aligner thickness throughout the treatment course are recommended. The use of 3D-printed aligners is also suggested to ensure a consistently uniform thickness across the entire surface and allow for intentional control over the aligner thickness [
22]. The current methodology will be employed in subsequent studies to investigate the 3D-printed aligners.
6. Conclusion
The current in vitro study showed the following observations:
Thermoplastic aligner sheets experience substantial thinning by thermoforming.
Aligner thinning varies across the aligner splint covering the tooth, being minimal at the incisal part (30%) and maximal at the gingival section of the facial surface (85%).
Increased aligner thinning corresponds to lower force transmission.
Decreasing the model height diminishes the thinning effect, thereby preserving the thickness at the cervical part to enhance force application and promote bodily tooth movement.
The model height utilized for aligner thermoforming is recommended to be within the range of 15 mm from the occlusal table to the base.
Clinical Relevance: The present findings provide clinicians and aligner manufacturers with evidence-based guidance regarding the optimal model height for deep drawing aligner sheets. It is recommended that the model height for aligner thermoforming falls within the range of 15 mm. This ensures the maintenance of sufficient aligner thickness, thereby delivering adequate force for effective teeth movement.
Author Contributions
Conceptualization, Tarek Elshazly; Data curation, Abdulaziz Alhotan and Tarek Elshazly; Formal analysis, Mostafa Aldesoki and Tarek Elshazly; Funding acquisition, Christoph Bourauel and Abdulaziz Alhotan; Investigation, Omar Ghoraba, Lamia Singer and Ahmed Ismail; Methodology, Omar Ghoraba, Ahmed Ismail, Hanaa Elattar and Abdulaziz Alhotan; Project administration, Christoph Bourauel and Tarek Elshazly; Resources, Hanaa Elattar and Abdulaziz Alhotan; Software, Omar Ghoraba, Mostafa Aldesoki, Lamia Singer, Ahmed Ismail and Tarek Elshazly; Supervision, Christoph Bourauel; Validation, Omar Ghoraba, Mostafa Aldesoki, Ahmed Ismail, Hanaa Elattar and Tarek Elshazly; Visualization, Christoph Bourauel and Tarek Elshazly; Writing – original draft, Tarek Elshazly; Writing – review & editing, Omar Ghoraba, Christoph Bourauel, Mostafa Aldesoki, Lamia Singer, Ahmed Ismail, Hanaa Elattar, Abdulaziz Alhotan and Tarek Elshazly.
Funding
The authors did not receive support from any organization for the submitted work.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
During the preparation of this work the authors used ChatGPT AI tool in order to improve the readability of the English language. After using this tool, the authors reviewed and edited the content as needed and take full responsibility for the content of the publication.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Acknowledgments
The authors thank the Researchers Supporting Project Number (RSPD2024R790), King Saud University, Riyadh, Saudi Arabia.
Conflicts of Interest
The authors have no relevant financial or non-financial interests to disclose.
References
- Papageorgiou SN, Koletsi D, Iliadi A, Peltomaki T, Eliades T. Treatment outcome with orthodontic aligners and fixed appliances: a systematic review with meta-analyses. European Journal of Orthodontics 2020; 42:331-343. [CrossRef]
- Macrì M, Murmura G, Varvara G, Traini T, Festa F. Clinical performances and biological features of clear aligners materials in orthodontics. Frontiers in Materials 2022; 9:819121. [CrossRef]
- Moutawakil A, Bennamar F, Aouame AEL, Alami S. Biomechanics of aligners: literature review. Adv Dent & Oral Health 2021; 13: 555872. DOI:10.19080/ADOH.2021.13.555872. [CrossRef]
- Upadhyay M, Arqub SA. Biomechanics of clear aligners: hidden truths & first principles. Journal of the World Federation of Orthodontists 2022; 11:12-21.
- Ho CT, Huang YT, Chao CW, Huang TH, Kao CT. Effects of different aligner materials and attachments on orthodontic behavior. Journal of dental sciences 2021; 16: 1001-1009. [CrossRef]
- Hahn W, Dathe H, Fialka-Fricke J, Fricke-Zech S, Zapf A, Kubein-Meesenburg D, Sadat-Khonsari R. Influence of thermoplastic appliance thickness on the magnitude of force delivered to a maxillary central incisor during tipping. American Journal of Orthodontics and Dentofacial Orthopedics 2009; 136:12.e1-12.e7.
- Cowley DP, Mah J, O’Toole B. The effect of gingival-margin design on the retention of thermoformed aligners. J. Clin. Orthod. 2012; 46:697.
- Elshazly TM, Bourauel C, Aldesoki M, Ghoneima A, Abuzayda M, Talaat W, Talaat S, Keilig L. Computer-aided finite element model for biomechanical analysis of orthodontic aligners. Clinical Oral Investigations 2023; 27:115-124. [CrossRef]
- Ryu JH, Kwon JS, Jiang HB, Cha JY, Kim KM. Effects of thermoforming on the physical and mechanical properties of thermoplastic materials for transparent orthodontic aligners. The Korean Journal of Orthodontics 2018; 48:316-325. [CrossRef]
- Elshazly TM, Keilig L, Salvatori D, Chavanne P, Aldesoki M, Bourauel C. Effect of trimming line design and edge extension of orthodontic aligners on force transmission: an in vitro study. Journal of Dentistry 2022; 125:104276. https://doi.org/10.1016/j.jdent.2022.104276. [CrossRef]
- Min S, Hwang CJ, Yu HS, Lee SB, Cha JY. The effect of thickness and deflection of orthodontic thermoplastic materials on its mechanical properties. Korean Journal of Orthodontics 2010; 40:16-26. [CrossRef]
- Barbagallo LJ, Shen G, Jones AS, Swain MV, Petocz P, Darendeliler MA. A novel pressure film approach for determining the force imparted by clear removable thermoplastic appliances. Annals of Biomedical Engineering 2008; 36:335-341. [CrossRef]
- Cervinara F, Cianci C, De Cillis F, Pappalettera G, Pappalettere C, Siciliani G, Lombardo L. Experimental study of the pressures and points of application of the forces exerted between aligner and tooth. Nanomaterials 2019; 9:1010. [CrossRef]
- Zamani NSM, Ashari A, Ali SHM, Gan KB, How RAWM, Wahab RMA, Mohamed AMFS, Sinnasamy S, Mokhtar MHH. Distributed Force Measurement and Mapping Using Pressure-Sensitive Film and Image Processing for Active and Passive Aligners on Orthodontic Attachments. IEEE Access 2022; 10:52853-52865. [CrossRef]
- Ihssen BA, Kerberger R, Rauch N, Drescher D, Becker K. Impact of dental model height on thermoformed PET-G aligner thickness—an in vitro micro-CT study. Applied Sciences 2021; 11:6674. [CrossRef]
- Lombardo L, Palone M, Longo M, Arveda N, Nacucchi M, De Pascalis F, Spedicato GA, Siciliani G. MicroCT X-ray comparison of aligner gap and thickness of six brands of aligners: an in-vitro study. Progress in Orthodontics 2020; 21:1-12. [CrossRef]
- Proffit WR, Fields HW, Larson B, Sarver DM. Contemporary orthodontics. Elsevier Health Sciences; 2000.
- Lee SY, Kim H, Kim HJ, Chung CJ, Choi YJ, Kim SJ, Cha JY. Thermo-mechanical properties of 3D printed photocurable shape memory resin for clear aligners. Scientific reports 2022; 12:6246. [CrossRef]
- Krey KF, Behyar M, Hartmann M, Corteville F, Ratzmann A. Behaviour of monolayer and multilayer foils in the aligner thermoforming process. J Aligner Orthod 2019; 3:139-145.
- Tuncay OC. The invisalign system. Quintessence Publishing Company; 2006.
- Elshazly TM, Salvatori D, Elattar H, Bourauel C, Keilig L. Effect of trimming line design and edge extension of orthodontic aligners on force transmission: A 3D finite element study. journal of the mechanical behavior of biomedical materials 2023; 140:105741. doi: https://doi.org/10.1016/j.jmbbm.2023.105741. [CrossRef]
- Park SY, Choi SH, Yu HS, Kim SJ, Kim H, Kim KB, Cha JY. Comparison of translucency, thickness, and gap width of thermoformed and 3D-printed clear aligners using micro-CT and spectrophotometer. Sci Rep 2023; 13:10921. https://doi.org/10.1038/s41598-023-36851-5. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).