Submitted:
29 April 2024
Posted:
30 April 2024
You are already at the latest version
Abstract
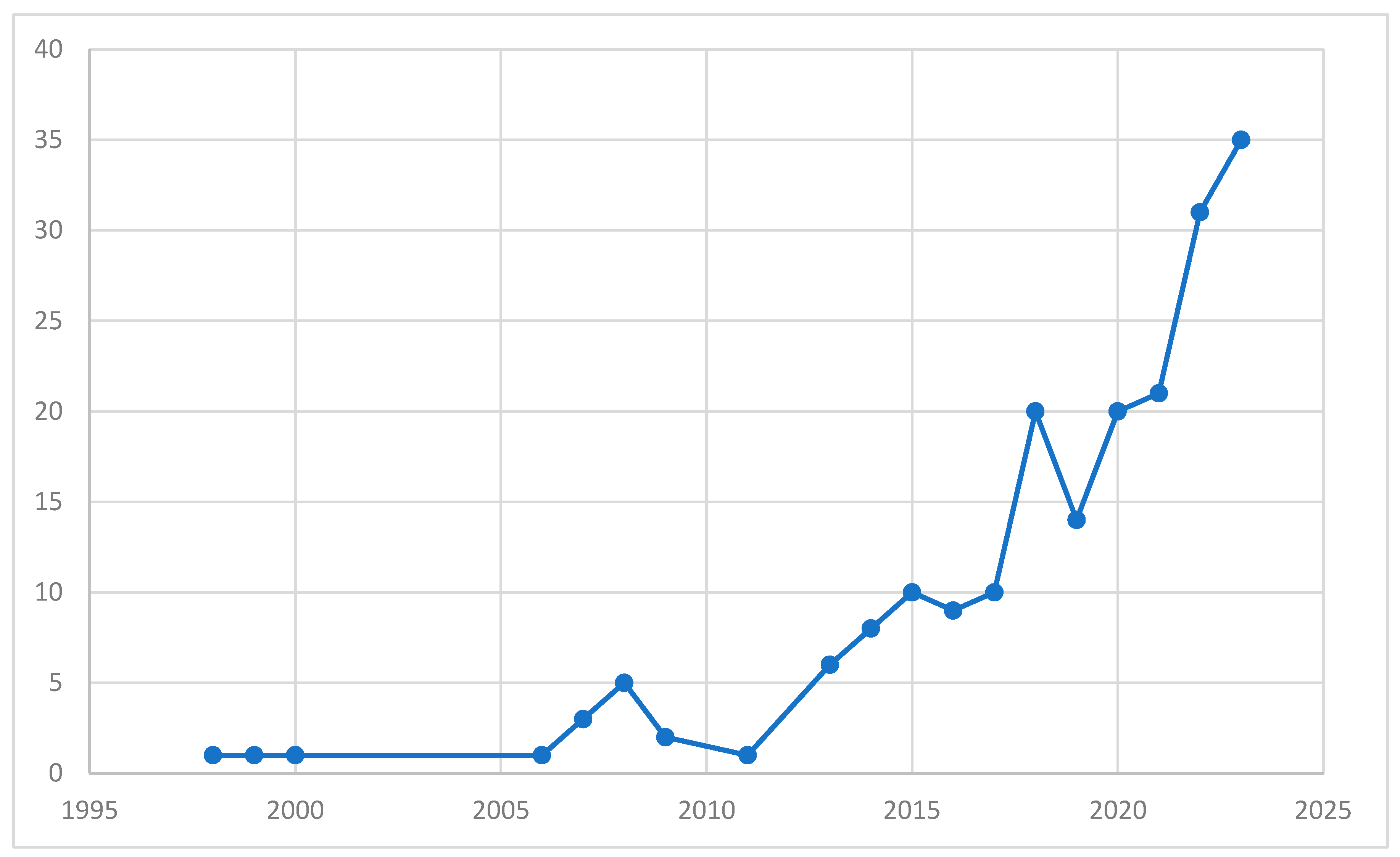
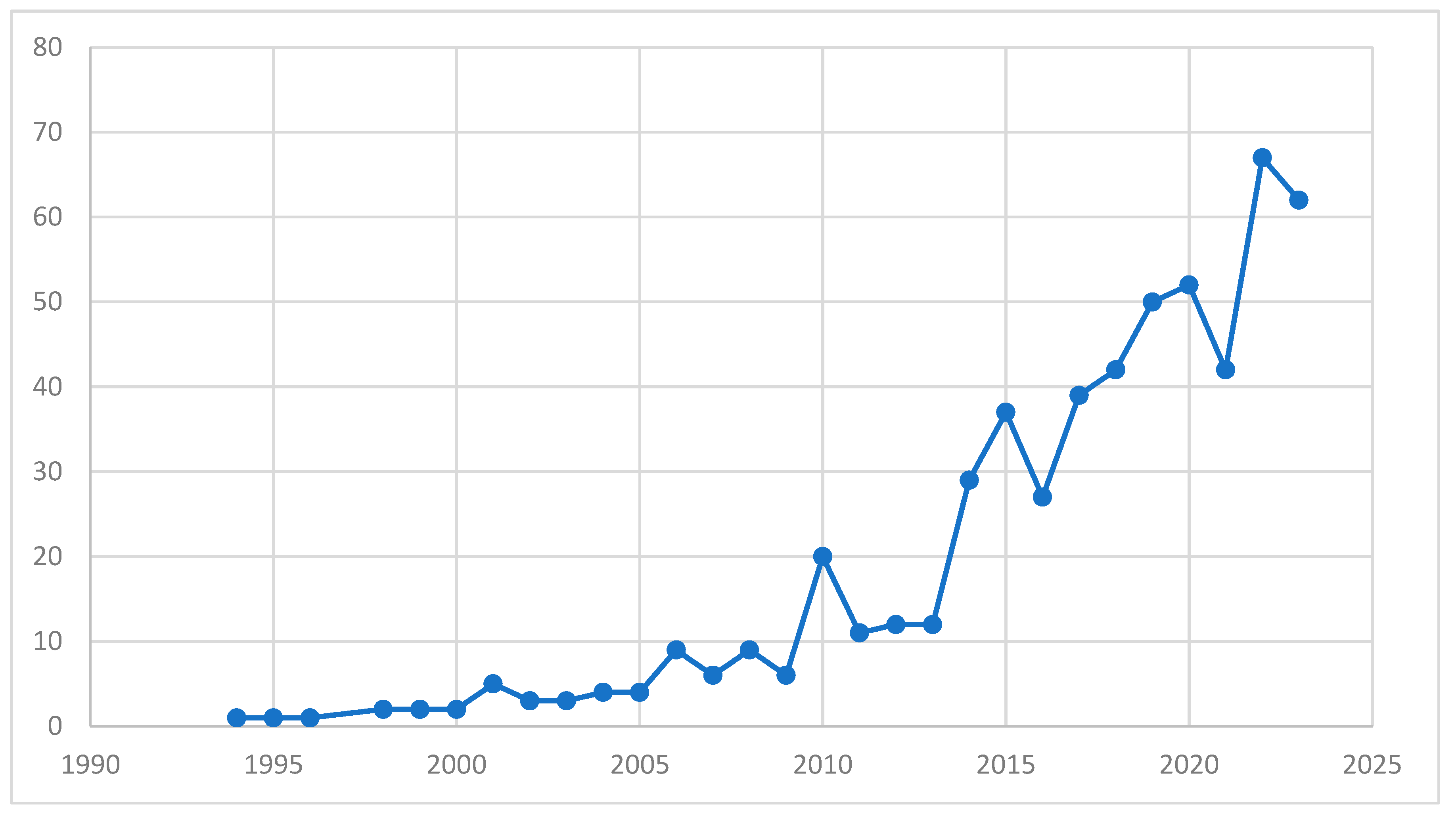
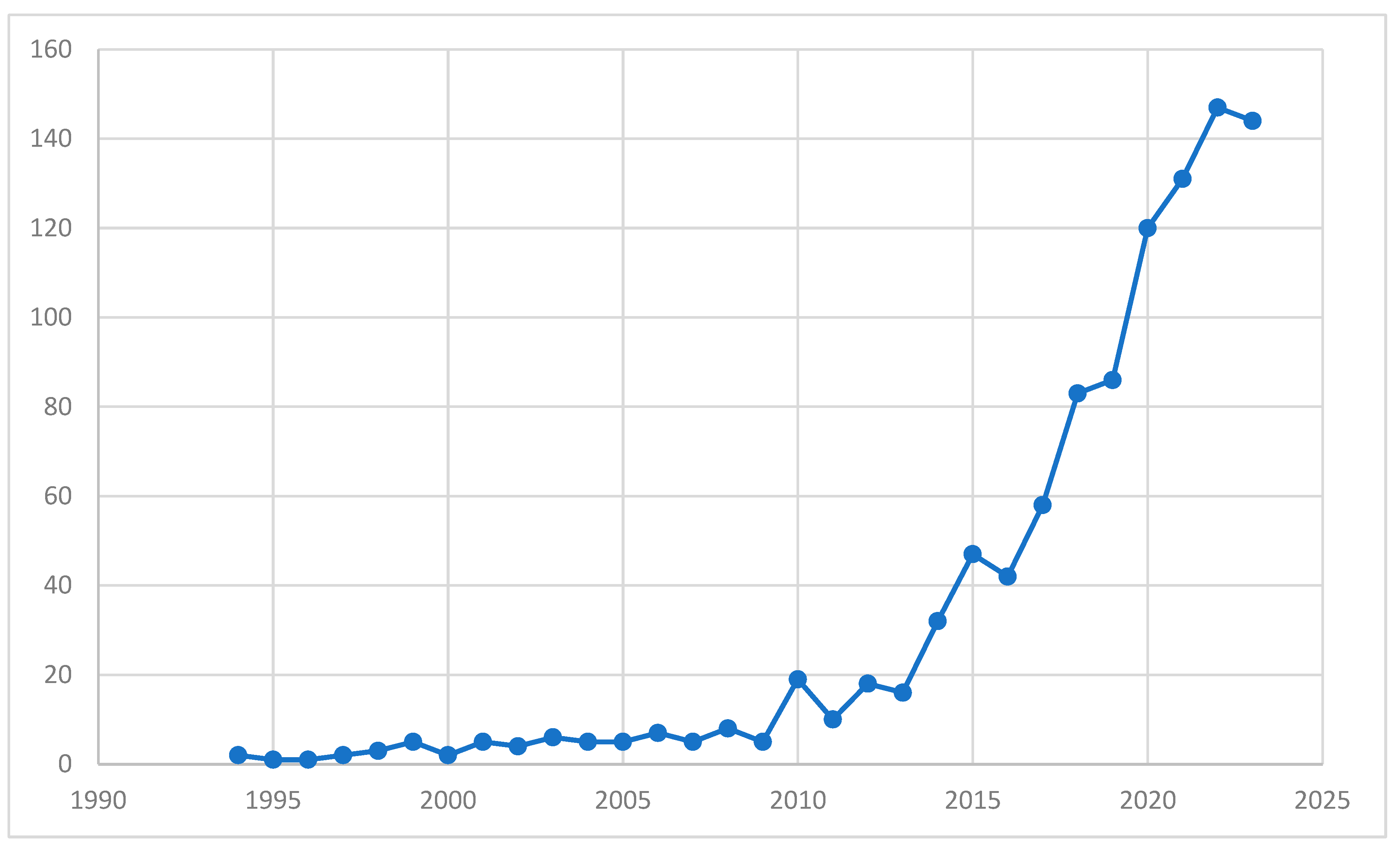
Introduction: The aim is to investigate the possibility of altering the delusional perceptions of psychotic patients by exposing them to a cognitively flexible virtual environment. A flexible vir-tual reality (VR) environment could challenge and enhance the ability to adapt to changing situa-tions and generate novel solutions to core psychotic symptoms. Materials and methods: A systematic review was conducted using different combinations of keywords in different databases. This study was conducted using the PRISMA statement. Results: There is a growing literature on the use of VR to manipulate and normalise perceptual distortions in psychosis. Over the last decade, the number of published studies on VR in mental health has increased 14-fold. Conclusions: A cognitive flexibility virtual environment can alter delusional perception by ex-posing the person to different scenarios that require them to question their assumptions, test their hypotheses, and revise their beliefs. Commonly used biosensors measure heart rate, skin con-ductance and body temperature in relation to different emotional states. Recently, there has been a major shift towards the use of neuroimaging techniques to better understand the pathophysiology of mental disorders. This is where the new wave of biosensor-integrated virtual reality (VR) sys-tems comes in.
Keywords:
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
Acknowledgments
Conflicts of Interest
References
- Miller ML, Strassnig MT, Bromet E, Depp CA, Jonas K, Lin W, Moore RC, Patterson TL, Penn DL, Pinkham AE, Kotov RA, Harvey PD. Performance-based assessment of social skills in a large sample of participants with schizophrenia, bipolar disorder and healthy controls: Correlates of social competence and social appropriateness. Schizophr Res. 2021 Oct;236:80-86. Epub 2021 Aug 20. [CrossRef] [PubMed] [PubMed Central]
- Grossman MJ, Doell FK, Watson-Gaze J, Baer LH, Martins F, Kidd SA. Increasing Access to CBT for Psychosis: Development, Feasibility, and Acceptability of a Specialized Outpatient Service. Community Ment Health J. 2022 Nov;58(8):1448-1456. Epub 2022 Mar 17. [CrossRef] [PubMed]
- Hazell CM, Hayward M, Cavanagh K, Strauss C. A systematic review and meta-analysis of low intensity CBT for psychosis. Clin Psychol Rev. 2016 Apr;45:183-92. Epub 2016 Mar 23. [CrossRef] [PubMed]
- Rees, S.N., Crowe, M. and Harris, S., 2021. The lesbian, gay, bisexual and transgender communities’ mental health care needs and experiences of mental health services: An integrative review of qualitative studies. Journal of Psychiatric and Mental Health Nursing, 28(4), pp.578-589.
- Kohn, L., Christiaens, W., Detraux, J., De Lepeleire, J., De Hert, M., Gillain, B., Delaunoit, B., Savoye, I., Mistiaen, P. and Jespers, V., 2022. Barriers to somatic health care for persons with severe mental illness in Belgium: a qualitative study of patients’ and healthcare professionals’ perspectives. Frontiers in Psychiatry, 12, p.798530. frontiersin.org.
- Chevance, A., Gourion, D., Hoertel, N., Llorca, P.M., Thomas, P., Bocher, R., Moro, M.R., Laprévote, V., Benyamina, A., Fossati, P. and Masson, M., 2020. Ensuring mental health care during the SARS-CoV-2 epidemic in France: A narrative review. L’encephale, 46(3), pp.193-201.
- Lee, E.E., Torous, J., De Choudhury, M., Depp, C.A., Graham, S.A., Kim, H.C., Paulus, M.P., Krystal, J.H. and Jeste, D.V., 2021. Artificial intelligence for mental health care: clinical applications, barriers, facilitators, and artificial wisdom. Biological Psychiatry: Cognitive Neuroscience and Neuroimaging, 6(9), pp.856-864.
- Kritikos J, Alevizopoulos G, Koutsouris D. Personalized Virtual Reality Human-Computer Interaction for Psychiatric and Neurological Illnesses: A Dynamically Adaptive Virtual Reality Environment That Changes According to Real-Time Feedback From Electrophysiological Signal Responses. Front Hum Neurosci. 2021 Feb 12;15:596980. [CrossRef] [PubMed] [PubMed Central]
- Market Analysis Report. Augmented Reality & Virtual Reality In Healthcare Market Size, Share & Trends Analysis Report By Component (Hardware, Software, Service), By Technology (Augmented Reality, Virtual Reality), By Region, And Segment Forecasts, 2023 – 2030. Report ID: GVR-1-68038-855-8.
- Gega L, White R, Clarke T, Turner R, Fowler D. Virtual environments using video capture for social phobia with psychosis. Cyberpsychol Behav Soc Netw. 2013 Jun;16(6):473-9. Epub 2013 May 9. [CrossRef] [PubMed] [PubMed Central]
- Pot-Kolder RMCA, Geraets CNW, Veling W, van Beilen M, Staring ABP, Gijsman HJ, Delespaul PAEG, van der Gaag M. Virtual-reality-based cognitive behavioural therapy versus waiting list control for paranoid ideation and social avoidance in patients with psychotic disorders: a single-blind randomised controlled trial. Lancet Psychiatry. 2018 Mar;5(3):217-226. Epub 2018 Feb 9. [CrossRef] [PubMed]
- Freeman D, Bradley J, Antley A, Bourke E, DeWeever N, Evans N, Černis E, Sheaves B, Waite F, Dunn G, Slater M, Clark DM. Virtual reality in the treatment of persecutory delusions: randomised controlled experimental study testing how to reduce delusional conviction. Br J Psychiatry. 2016 Jul;209(1):62-7. Epub 2016 May 5. [CrossRef] [PubMed] [PubMed Central]
- Craig TK, Rus-Calafell M, Ward T, Leff JP, Huckvale M, Howarth E, Emsley R, Garety PA. AVATAR therapy for auditory verbal hallucinations in people with psychosis: a single-blind, randomised controlled trial. Lancet Psychiatry. 2018 Jan;5(1):31-40. Epub 2017 Nov 23. Erratum in: Lancet Psychiatry. 2017 Nov 29. [CrossRef] [PubMed] [PubMed Central]
- Lan L, Sikov J, Lejeune J, Ji C, Brown H, Bullock K, Spencer AE. A Systematic Review of using Virtual and Augmented Reality for the Diagnosis and Treatment of Psychotic Disorders. Curr Treat Options Psychiatry. 2023 Jun 14:1-21. Epub ahead of print. [CrossRef] [PubMed] [PubMed Central]
- Chan KC, Hui CL, Suen YN, Lee EH, Chang WC, Chan SK, Chen EY. Application of Immersive Virtual Reality for Assessment and Intervention in Psychosis: A Systematic Review. Brain Sci. 2023 Mar 10;13(3):471. [CrossRef] [PubMed] [PubMed Central]
- Shen ZH, Liu MH, Wu Y, Lin QQ, Wang YG. Virtual-reality-based social cognition and interaction training for patients with schizophrenia: A preliminary efficacy study. Front Psychiatry. 2022 Nov 17;13:1022278. [CrossRef] [PubMed] [PubMed Central]
- Baghaei N, Liang H-N, Billinghurst M, Naslund J and Oyekoya O (2022) Editorial: Virtual Reality and Mental Health: Opportunities to Advance Research and Practice. Front. Virtual Real. 3:838036. [CrossRef]
- BMJ 2021;372:n71. [CrossRef]
- Goharinejad, S., Goharinejad, S., Hajesmaeel-Gohari, S. et al. The usefulness of virtual, augmented, and mixed reality technologies in the diagnosis and treatment of attention deficit hyperactivity disorder in children: an overview of relevant studies. BMC Psychiatry 22, 4 (2022). [CrossRef]
- Jahn Frida Simon, Skovbye Marie, Kia Obenhausen, Andreas Elleby Jespersen, Kamilla Woznica Miskowiak, Cognitive training with fully immersive virtual reality in patients with neurological and psychiatric disorders: A systematic review of randomized controlled trials, Psychiatry Research, Volume 300,2021,113928,ISSN 0165-1781, doi.org/10.1016/j.psychres.2021.113928.
- Martingano, A. J., Hererra, F., & Konrath, S. (2021). Virtual reality improves emotional but not cognitive empathy: A meta-analysis. Technology, Mind, and Behavior, 2(1). [CrossRef]
- Martens MA, Antley A, Freeman D, Slater M, Harrison PJ, Tunbridge EM. It feels real: physiological responses to a stressful virtual reality environment and its impact on working memory. J Psychopharmacol. 2019 Oct;33(10):1264-1273. [CrossRef]
- Mazurek J, Kiper P, Cieślik B, Rutkowski S, Mehlich K, Turolla A, Szczepańska-Gieracha A. Virtual reality in medicine: a brief overview and future research directions. Hum Mov. 2019;20(3):16–22; doi.org/10.5114/hm.2019.83529.
- Valmaggia LR, Day F, Rus-Calafell M. Using virtual reality to investigate psychological processes and mechanisms associated with the onset and maintenance of psychosis: a systematic review. Soc Psychiatry Psychiatr Epidemiol. 2016 Jul;51(7):921-36. Epub 2016 Jun 4. [CrossRef] [PubMed]
- Lee TY, Lee SS, Gong B-g and Kwon JS (2022) Research Trends in Individuals at High Risk for Psychosis: A Bibliometric Analysis. Front. Psychiatry 13:853296. [CrossRef]
- Gutiérrez-Maldonado, J. The Use of Virtual Reality Technology in the Treatment of Psychopathological Disorders. J. Clin. Med. 2022, 11, 5358. [Google Scholar] [CrossRef] [PubMed]
- Fernández-Caballero A, Navarro E, Fernández-Sotos P, González P, Ricarte JJ, Latorre JM, Rodriguez-Jimenez R. Human-Avatar Symbiosis for the Treatment of Auditory Verbal Hallucinations in Schizophrenia through Virtual/Augmented Reality and Brain-Computer Interfaces. Front Neuroinform. 2017 Nov 21;11:64. [CrossRef]
- Alevizopoulos A, Kritikos J, Alevizopoulos G. Intelligent machines and mental health in the era of COVID-19. Psychiatriki. 2021 Jul 10;32(2):99-102. Greek, Modern, English. Epub 2021 May 28. [CrossRef] [PubMed]
- Adamovich SV, August K, Merians A, Tunik E. A virtual reality-based system integrated with fMRI to study neural mechanisms of action observation-execution: a proof of concept study. Restor Neurol Neurosci. 2009;27(3):209-23. [CrossRef]
- Roberts G, Holmes N, Alexander N, Boto E, Leggett J, Hill RM, Shah V, Rea M, Vaughan R, Maguire EA, Kessler K, Beebe S, Fromhold M, Barnes GR, Bowtell R, Brookes MJ. Towards OPM-MEG in a virtual reality environment. Neuroimage. 2019 Oct 1;199:408-417. [CrossRef]
- Dordevic M, Maile O, Das A, Kundu S, Haun C, Baier B, Müller NG. A Comparison of Immersive vs. Non-Immersive Virtual Reality Exercises for the Upper Limb: A Functional Near-Infrared Spectroscopy Pilot Study with Healthy Participants. J Clin Med. 2023 Sep 5;12(18):5781. [CrossRef]
- Yunxiang Zhang, Benjamin Liang, Boyuan Chen, Paul M. Torrens, S. Farokh Atashzar, Dahua Lin, and Qi Sun. 2022. Force-Aware Interface via Electromyography for Natural VR/AR Interaction. ACM Trans. Graph. 41, 6, Article 268 (December 2022), 18 pages. [CrossRef]
- Parida K, H. Bark, P. S. Lee, Emerging Thermal Technology Enabled Augmented Reality. Adv. Funct. Mater. 2021, 31, 2007952. [CrossRef]
- Martin Kocur, Lukas Jackermeier, Valentin Schwind, and Niels Henze. 2023. The Effects of Avatar and Environment on Thermal Perception and Skin Temperature in Virtual Reality. In Proceedings of the 2023 CHI Conference on Human Factors in Computing Systems (CHI ’23), April 23–28, 2023, Hamburg, Germany. ACM, New York, NY, USA, 15 pages. [CrossRef]
- Floris C, Solbiati S, Landreani F, Damato G, Lenzi B, Megale V, Caiani EG. Feasibility of Heart Rate and Respiratory Rate Estimation by Inertial Sensors Embedded in a Virtual Reality Headset. Sensors. 2020; 20(24):7168. [CrossRef]
- Stramba-Badiale C, Mancuso V, Cavedoni S, Pedroli E, Cipresso P and Riva G (2020) Transcranial Magnetic Stimulation Meets Virtual Reality: The Potential of Integrating Brain Stimulation With a Simulative Technology for Food Addiction. Front. Neurosci. 14:720. [CrossRef]
- Stramba-Badiale C, Mancuso V, Cavedoni S, Pedroli E, Cipresso P and Riva G (2020) Transcranial Magnetic Stimulation Meets Virtual Reality: The Potential of Integrating Brain Stimulation With a Simulative Technology for Food Addiction. Front. Neurosci. 14:720. [CrossRef]
- Rizzo, A.“S.”, Schultheis, M. T., & Rothbaum, B. O. (2002). Ethical issues for the use of virtual reality in the psychological sciences. In S. S. Bush & M. L. Drexler (Eds.), Ethical issues in clinical neuropsychology (pp. 243–277). Swets & Zeitlinger Publishers.
- Lavoie, R., Main, K., King, C. et al. Virtual experience, real consequences: the potential negative emotional consequences of virtual reality gameplay. Virtual Reality 25, 69–81 (2021). [CrossRef]
- Ahrens S, Twanow JD, Vidaurre J, Gedela S, Moore-Clingenpeel M, Ostendorf AP. Electroencephalography Technologist Inter-rater Agreement and Interpretation of Pediatric Critical Care Electroencephalography. Pediatr Neurol. 2021 Feb;115:66-71. [CrossRef]
- Dzardanova E, Kasapakis V, Gavalas D, Sylaiou S. Virtual reality as a communication medium: a comparative study of forced compliance in virtual reality versus physical world. Virtual Real. 2022;26(2):737-757. [CrossRef]
- Freeman D, Rosebrock L, Waite F, Loe BS, Kabir T, Petit A, Dudley R, Chapman K, Morrison A, O’Regan E, Aynsworth C, Jones J, Murphy E, Powling R, Peel H, Walker H, Byrne R, Freeman J, Rovira A, Galal U, Yu LM, Clark DM, Lambe S. Virtual reality (VR) therapy for patients with psychosis: satisfaction and side effects. Psychol Med. 2023 Jul;53(10):4373-4384. [CrossRef]
- Takahashi K, Meilinger T, Watanabe K, Bülthoff HH. Psychological influences on distance estimation in a virtual reality environment. Front Hum Neurosci. 2013 Sep 18;7:580. [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).



