Submitted:
12 April 2024
Posted:
17 April 2024
You are already at the latest version
Abstract
Keywords:
Introduction and Definitions
Donor-Derived Cell-Free DNA (dd-cfDNA)
Gene Expression Profile as Biomarkers
Urinary RNA Profile for the Diagnosis of Rejection
Conclusions
Author Contributions
Conflict of interest statement
References
- Naesens, M.; Anglicheau, D. Precision Transplant Medicine: Biomarkers to the Rescue. J Am Soc Nephrol. 2018, 29, 24–34. [Google Scholar] [CrossRef]
- Salvadori, M.; Tsalouchos, A. Microbiota, renal disease and renal transplantation. World J Transplant. 2021, 11, 16–36. [Google Scholar] [CrossRef] [PubMed]
- Anglicheau, D.; Naesens, M.; Essig, M.; Gwinner, W.; Marquet, P. Establishing Biomarkers in Transplant Medicine: A Critical Review of Current Approaches. Transplantation. 2016, 100, 2024–2038. [Google Scholar] [CrossRef]
- Suthanthiran, M.; Schwartz, J.E.; Ding, R.; Abecassis, M.; Dadhania, D.; Samstein, B.; Knechtle, S.J.; Friedewald, J.; Becker, Y.T.; Sharma, V.K.; Williams, N.M.; Chang, C.S.; Hoang, C.; Muthukumar, T.; August, P.; Keslar, K.S.; Fairchild, R.L.; Hricik, D.E.; Heeger, P.S.; Han, L.; Liu, J.; Riggs, M.; Ikle, D.N.; Bridges, N.D.; Shaked, A. Clinical Trials in Organ Transplantation 04 (CTOT-04) Study Investigators. Urinary-cell mRNA profile and acute cellular rejection in kidney allografts. Transplantation. 2012, 93, 1136–1146. [Google Scholar]
- Roedder, S.; Sigdel, T.; Salomonis, N.; Hsieh, S.; Dai, H.; Bestard, O.; Metes, D.; Zeevi, A.; Gritsch, A.; Cheeseman, J.; Macedo, C.; Peddy, R.; Medeiros, M.; Vincenti, F.; Asher, N.; Salvatierra, O.; Shapiro, R.; Kirk, A.; Reed, E.F.; Sarwal, M.M. The kSORT assay to detect renal transplant patients at high risk for acute rejection: results of the multicenter AART study. PLoS Med. 2014, 11, e1001759. [Google Scholar] [CrossRef] [PubMed]
- Kurian, S.M.; Williams, A.N.; Gelbart, T.; Campbell, D.; Mondala, T.S.; Head, S.R.; Horvath, S.; Gaber, L.; Thompson, R.; Whisenant, T.; Lin, W.; Langfelder, P.; Robison, E.H.; Schaffer, R.L.; Fisher, J.S.; Friedewald, J.; Flechner, S.M.; Chan, L.K.; Wiseman, A.C.; Shidban, H.; Mendez, R.; Heilman, R.; Abecassis, M.M.; Marsh, C.L.; Salomon, D.R. Molecular classifiers for acute kidney transplant rejection in peripheral blood by whole genome gene expression profiling. Am J Transplant. 2014, 14, 1164–1172. [Google Scholar] [CrossRef] [PubMed]
- Loupy, A.; Lefaucheur, C.; Vernerey, D.; Prugger, C.; Duong van Huyen, J.P.; Mooney, N.; Suberbielle, C.; Frémeaux-Bacchi, V.; Méjean, A.; Desgrandchamps, F.; Anglicheau, D.; Nochy, D.; Charron, D.; Empana, J.P.; Delahousse, M.; Legendre, C.; Glotz, D.; Hill, G.S.; Zeevi, A.; Jouven, X. Complement-binding anti-HLA antibodies and kidney-allograft survival. N Engl J Med. 2013, 369, 1215–1226. [Google Scholar] [CrossRef]
- Sicard, A.; Ducreux, S.; Rabeyrin, M.; Couzi, L.; McGregor, B.; Badet, L.; Scoazec, J.Y.; Bachelet, T.; Lepreux, S.; Visentin, J.; Merville, P.; Fremeaux-Bacchi, V.; Morelon, E.; Taupin, J.L.; Dubois, V.; Thaunat, O. Detection of C3d-binding donor-specific anti-HLA antibodies at diagnosis of humoral rejection predicts renal graft loss. J Am Soc Nephrol. 2015, 26, 457–467. [Google Scholar] [CrossRef]
- Einecke, G.; Reeve, J.; Sis, B.; Mengel, M.; Hidalgo, L.; Famulski, K.S.; Matas, A.; Kasiske, B.; Kaplan, B.; Halloran, P.F. A molecular classifier for predicting future graft loss in late kidney transplant biopsies. J Clin Invest. 2010, 120, 1862–1872. [Google Scholar] [CrossRef]
- Loupy, A.; Lefaucheur, C.; Vernerey, D.; Chang, J.; Hidalgo, L.G.; Beuscart, T.; Verine, J.; Aubert, O.; Dubleumortier, S.; Duong van Huyen, J.P.; Jouven, X.; Glotz, D.; Legendre, C.; Halloran, P.F. Molecular microscope strategy to improve risk stratification in early antibody-mediated kidney allograft rejection. J Am Soc Nephrol. 2014, 25, 2267–2277. [Google Scholar] [CrossRef]
- O‘Connell, P.J.; Zhang, W.; Menon, M.C.; Yi, Z.; Schröppel, B.; Gallon, L.; Luan, Y.; Rosales, I.A.; Ge, Y.; Losic, B.; Xi, C.; Woytovich, C.; Keung, K.L.; Wei, C.; Greene, I.; Overbey, J.; Bagiella, E.; Najafian, N.; Samaniego, M.; Djamali, A.; Alexander, S.I.; Nankivell, B.J.; Chapman, J.R.; Smith, R.N.; Colvin, R.; Murphy, B. Biopsy transcriptome expression profiling to identify kidney transplants at risk of chronic injury: a multicentre, prospective study. Lancet. 2016, 388, 983–993. [Google Scholar] [CrossRef] [PubMed]
- Gielis, E.M.; Ledeganck, K.J.; De Winter, B.Y.; Del Favero, J.; Bosmans, J.L.; Claas, F.H.; Abramowicz, D.; Eikmans, M. Cell-Free DNA: An Upcoming Biomarker in Transplantation. Am J Transplant. 2015, 15, 2541–2551. [Google Scholar] [CrossRef] [PubMed]
- Beck, J.; Bierau, S.; Balzer, S.; Andag, R.; Kanzow, P.; Schmitz, J.; Gaedcke, J.; Moerer, O.; Slotta, J.E.; Walson, P.; Kollmar, O.; Oellerich, M.; Schütz, E. Digital droplet PCR for rapid quantification of donor DNA in the circulation of transplant recipients as a potential universal biomarker of graft injury. Clin Chem. 2013, 59, 1732–1741. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Tong, K.L.; Li, P.K.; Chan, A.Y.; Yeung, C.K.; Pang, C.C.; Wong, T.Y.; Lee, K.C.; Lo, Y.M. Presence of donor- and recipient-derived DNA in cell-free urine samples of renal transplantation recipients: urinary DNA chimerism. Clin Chem. 1999, 45, 1741–1746. [Google Scholar] [CrossRef] [PubMed]
- García Moreira, V.; Prieto García, B.; Baltar Martín, J.M.; Ortega Suárez, F.; Alvarez, F.V. Cell-free DNA as a noninvasive acute rejection marker in renal transplantation. Clin Chem. 2009, 55, 1958–1966. [Google Scholar] [CrossRef] [PubMed]
- Sigdel, T.K.; Vitalone, M.J.; Tran, T.Q.; Dai, H.; Hsieh, S.C.; Salvatierra, O.; Sarwal, M.M. A rapid noninvasive assay for the detection of renal transplant injury. Transplantation. 2013, 96, 97–101. [Google Scholar] [CrossRef] [PubMed]
- Botezatu, I.; Serdyuk, O.; Potapova, G.; Shelepov, V.; Alechina, R.; Molyaka, Y.; Ananév, V.; Bazin, I.; Garin, A.; Narimanov, M.; Knysh, V.; Melkonyan, H.; Umansky, S.; Lichtenstein, A. Genetic analysis of DNA excreted in urine: a new approach for detecting specific genomic DNA sequences from cells dying in an organism. Clin Chem. 2000, 46, 1078–1084. [Google Scholar] [CrossRef]
- Osmanodja, B.; Akifova, A.; Budde, K.; Choi, M.; Oellerich, M.; Schütz, E.; Beck, J. Absolute or Relative Quantification of Donor-derived Cell-free DNA in Kidney Transplant Recipients: Case Series. Transplant Direct. 2021, 7, e778. [Google Scholar] [CrossRef]
- Graver, A.S.; Lee, D.; Power, D.A.; Whitlam, J.B. Understanding Donor-derived Cell-free DNA in Kidney Transplantation: An Overview and Case-based Guide for Clinicians. Transplantation. 2023, 107, 1675–1686. [Google Scholar] [CrossRef]
- Sigdel, T.K.; Archila, F.A.; Constantin, T.; Prins, S.A.; Liberto, J.; Damm, I.; Towfighi, P.; Navarro, S.; Kirkizlar, E.; Demko, Z.P.; Ryan, A.; Sigurjonsson, S.; Sarwal, R.D.; Hseish, S.C.; Chan-On, C.; Zimmermann, B.; Billings, P.R.; Moshkevich, S.; Sarwal, M.M. Optimizing Detection of Kidney Transplant Injury by Assessment of Donor-Derived Cell-Free DNA via Massively Multiplex PCR. J Clin Med. 2018, 8, 19. [Google Scholar] [CrossRef]
- Bloom, R.D.; Bromberg, J.S.; Poggio, E.D.; Bunnapradist, S.; Langone, A.J.; Sood, P.; Matas, A.J.; Mehta, S.; Mannon, R.B.; Sharfuddin, A.; Fischbach, B.; Narayanan, M.; Jordan, S.C.; Cohen, D.; Weir, M.R.; Hiller, D.; Prasad, P.; Woodward, R.N.; Grskovic, M.; Sninsky, J.J.; Yee, J.P.; Brennan, D.C. Circulating Donor-Derived Cell-Free DNA in Blood for Diagnosing Active Rejection in Kidney Transplant Recipients (DART) Study Investigators. Cell-Free DNA and Active Rejection in Kidney Allografts. J Am Soc Nephrol. 2017, 28, 2221–2232. [Google Scholar] [CrossRef]
- Wijtvliet, V.P.W.M.; Plaeke, P.; Abrams, S.; Hens, N.; Gielis, E.M.; Hellemans, R.; Massart, A.; Hesselink, D.A.; De Winter, B.Y.; Abramowicz, D.; Ledeganck, K.J. Donor-derived cell-free DNA as a biomarker for rejection after kidney transplantation: a systematic review and meta-analysis. Transpl Int. 2020, 33, 1626–1642. [Google Scholar] [CrossRef]
- Xiao, H.; Gao, F.; Pang, Q.; Xia, Q.; Zeng, X.; Peng, J.; Fan, L.; Liu, J.; Wang, Z.; Li, H. Diagnostic Accuracy of Donor-derived Cell-free DNA in Renal-allograft Rejection: A Meta-analysis. Transplantation. 2021, 105, 1303–1310. [Google Scholar] [CrossRef] [PubMed]
- Oellerich, M.; Shipkova, M.; Asendorf, T.; Walson, P.D.; Schauerte, V.; Mettenmeyer, N.; Kabakchiev, M.; Hasche, G.; Gröne, H.J.; Friede, T.; Wieland, E.; Schwenger, V.; Schütz, E.; Beck, J. Absolute quantification of donor-derived cell-free DNA as a marker of rejection and graft injury in kidney transplantation: Results from a prospective observational study. Am J Transplant. 2019, 19, 3087–3099. [Google Scholar] [CrossRef]
- Whitlam, J.B.; Ling, L.; Skene, A.; Kanellis, J.; Ierino, F.L.; Slater, H.R.; Bruno, D.L.; Power, D.A. Diagnostic application of kidney allograft-derived absolute cell-free DNA levels during transplant dysfunction. Am J Transplant. 2019, 19, 1037–1049. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.; Zheng, C.; Li, X.; Fu, Q.; Li, J.; Su, Q.; Zeng, L.; Liu, Z.; Wang, J.; Huang, H.; Xu, B.; Ye, M.; Liu, L.; Wang, C. Diagnostic Performance of Donor-Derived Plasma Cell-Free DNA Fraction for Antibody-Mediated Rejection in Post Renal Transplant Recipients: A Prospective Observational Study. Front Immunol. 2020, 11, 342. [Google Scholar] [CrossRef]
- Bromberg, J.S.; Brennan, D.C.; Poggio, E.; Bunnapradist, S.; Langone, A.; Sood, P.; Matas, A.J.; Mannon, R.B.; Mehta, S.; Sharfuddin, A.; Fischbach, B.; Narayanan, M.; Jordan, S.C.; Cohen, D.J.; Zaky, Z.S.; Hiller, D.; Woodward, R.N.; Grskovic, M.; Sninsky, J.J.; Yee, J.P.; Bloom, R.D. Biological Variation of Donor-Derived Cell-Free DNA in Renal Transplant Recipients: Clinical Implications. J Appl Lab Med. 2017, 2, 309–321. [Google Scholar] [CrossRef]
- Huang, E.; Sethi, S.; Peng, A.; Najjar, R.; Mirocha, J.; Haas, M.; Vo, A.; Jordan, S.C. Early clinical experience using donor-derived cell-free DNA to detect rejection in kidney transplant recipients. Am J Transplant. 2019, 19, 1663–1670. [Google Scholar] [CrossRef] [PubMed]
- Stroup, D.F.; Berlin, J.A.; Morton, S.C.; Olkin, I.; Williamson, G.D.; Rennie, D.; Moher, D.; Becker, B.J.; Sipe, T.A.; Thacker, S.B. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000, 283, 2008–2012. [Google Scholar] [CrossRef]
- Lefaucheur, C.; Loupy, A. Antibody-Mediated Rejection of Solid-Organ Allografts. N Engl J Med. 2018, 379, 2580–2582. [Google Scholar]
- Haas, M.; Loupy, A.; Lefaucheur, C.; Roufosse, C.; Glotz, D.; Seron, D.; Nankivell, B.J.; Halloran, P.F.; Colvin, R.B.; Akalin, E.; Alachkar, N.; Bagnasco, S.; Bouatou, Y.; Becker, J.U.; Cornell, L.D.; Duong van Huyen, J.P.; Gibson, I.W.; Kraus, E.S.; Mannon, R.B.; Naesens, M.; Nickeleit, V.; Nickerson, P.; Segev, D.L.; Singh, H.K.; Stegall, M.; Randhawa, P.; Racusen, L.; Solez, K.; Mengel, M. The Banff 2017 Kidney Meeting Report: Revised diagnostic criteria for chronic active T cell-mediated rejection, antibody-mediated rejection, and prospects for integrative endpoints for next-generation clinical trials. Am J Transplant. 2018, 18, 293–307. [Google Scholar] [CrossRef] [PubMed]
- Stites, E.; Kumar, D.; Olaitan, O.; John Swanson, S.; Leca, N.; Weir, M.; Bromberg, J.; Melancon, J.; Agha, I.; Fattah, H.; Alhamad, T.; Qazi, Y.; Wiseman, A.; Gupta, G. High levels of dd-cfDNA identify patients with TCMR 1A and borderline allograft rejection at elevated risk of graft injury. Am J Transplant. 2020, 20, 2491–2498. [Google Scholar] [CrossRef]
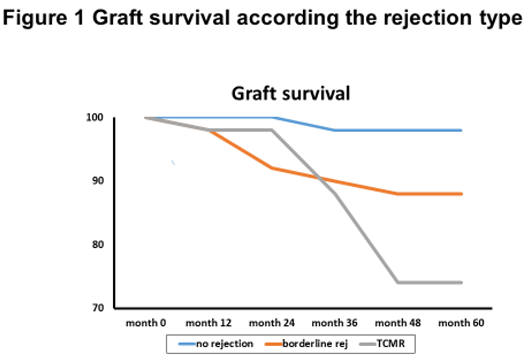
- Pallardó Mateu, L.M.; Sancho Calabuig, A.; Capdevila Plaza, L.; Franco Esteve, A. Acute rejection and late renal transplant failure: risk factors and prognosis. Nephrol Dial Transplant, 2004; 19, (Suppl. 3), iii38–42. [Google Scholar]
- Jevnikar, A.M.; Mannon, R.B. Late kidney allograft loss: what we know about it, and what we can do about it. Clin J Am Soc Nephrol. 2008, 3 (Suppl. 2), S56–S67. [Google Scholar] [CrossRef] [PubMed]
- Cooper, J.E.; Gralla, K.; Chan, K. Clinical significance of post kidney transplant de novo DSA in otherwise stable grafts. Clin Transpl 2011, 35, 359–364. [Google Scholar]
- Bu, L.; Gupta, G.; Pai, A.; Anand, S.; Stites, E.; Moinuddin, I.; Bowers, V.; Jain, P.; Axelrod, D.A.; Weir, M.R.; Wolf-Doty, T.K.; Zeng, J.; Tian, W.; Qu, K.; Woodward, R.; Dholakia, S.; De Golovine, A.; Bromberg, J.S.; Murad, H.; Alhamad, T. Clinical outcomes from the Assessing Donor-derived cell-free DNA Monitoring Insights of kidney Allografts with Longitudinal surveillance (ADMIRAL) study. Kidney Int. 2022, 101, 793–803. [Google Scholar] [CrossRef]
- Clayton, P.A.; Lim, W.H.; Wong, G.; Chadban, S.J. Relationship between eGFR Decline and Hard Outcomes after Kidney Transplants. J Am Soc Nephrol. 2016, 27, 3440–3446. [Google Scholar] [CrossRef] [PubMed]
- Faddoul, G.; Nadkarni, G.N.; Bridges, N.D.; Goebel, J.; Hricik, D.E.; Formica, R.; Menon, M.C.; Morrison, Y.; Murphy, B.; Newell, K.; Nickerson, P.; Poggio, E.D.; Rush, D.; Heeger, P.S. CTOT-17 consortium. Analysis of Biomarkers Within the Initial 2 Years Posttransplant and 5-Year Kidney Transplant Outcomes: Results From Clinical Trials in Organ Transplantation-17. Transplantation. 2018, 102, 673–680. [Google Scholar] [CrossRef] [PubMed]
- Nankivell, B.J.; Agrawal, N.; Sharma, A.; Taverniti, A.; P‘Ng, C.H.; Shingde, M.; Wong, G.; Chapman, J.R. The clinical and pathological significance of borderline T cell-mediated rejection. Am J Transplant. 2019, 19, 1452–1463. [Google Scholar] [CrossRef] [PubMed]
- Seifert, M.E.; Yanik, M.V.; Feig, D.I.; Hauptfeld-Dolejsek, V.; Mroczek-Musulman, E.C.; Kelly, D.R.; Rosenblum, F.; Mannon, R.B. Subclinical inflammation phenotypes and long-term outcomes after pediatric kidney transplantation. Am J Transplant. 2018, 18, 2189–2199. [Google Scholar] [CrossRef]
- Mehta, R.; Bhusal, S.; Randhawa, P.; Sood, P.; Cherukuri, A.; Wu, C.; Puttarajappa, C.; Hoffman, W.; Shah, N.; Mangiola, M.; Zeevi, A.; Tevar, A.D.; Hariharan, S. Short-term adverse effects of early subclinical allograft inflammation in kidney transplant recipients with a rapid steroid withdrawal protocol. Am J Transplant. 2018, 18, 1710–1717. [Google Scholar] [CrossRef]
- Friedewald, J.J.; Kurian, S.M.; Heilman, R.L.; Whisenant, T.C.; Poggio, E.D.; Marsh, C.; Baliga, P.; Odim, J.; Brown, M.M.; Ikle, D.N.; Armstrong, B.D.; Charette, J.I.; Brietigam, S.S.; Sustento-Reodica, N.; Zhao, L.; Kandpal, M.; Salomon, D.R.; Abecassis, M.M. Clinical Trials in Organ Transplantation 08 (CTOT-08). Development and clinical validity of a novel blood-based molecular biomarker for subclinical acute rejection following kidney transplant. Am J Transplant. 2019, 19, 98–109. [Google Scholar] [CrossRef] [PubMed]
- Hricik, D.E.; Nickerson, P.; Formica, R.N.; Poggio, E.D.; Rush, D.; Newell, K.A.; Goebel, J.; Gibson, I.W.; Fairchild, R.L.; Riggs, M.; Spain, K.; Ikle, D.; Bridges, N.D.; Heeger, P.S. CTOT-01 consortium.Multicenter validation of urinary CXCL9 as a risk-stratifying biomarker for kidney transplant injury. Am J Transplant. 2013, 13, 2634–2644. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.; Yi, Z.; Keung, K.L.; Shang, H.; Wei, C.; Cravedi, P.; Sun, Z.; Xi, C.; Woytovich, C.; Farouk, S.; Huang, W.; Banu, K.; Gallon, L.; Magee, C.N.; Najafian, N.; Samaniego, M.; Djamali, A.; Alexander, S.I.; Rosales, I.A.; Smith, R.N.; Xiang, J.; Lerut, E.; Kuypers, D.; Naesens, M.; O‘Connell, P.J.; Colvin, R.; Menon, M.C.; Murphy, B. A Peripheral Blood Gene Expression Signature to Diagnose Subclinical Acute Rejection. J Am Soc Nephrol. 2019, 30, 1481–1494. [Google Scholar] [CrossRef] [PubMed]
- Yazdani, S.; Naesens, M. Foretelling Graft Outcome by Molecular Evaluation of Renal Allograft Biopsies: The GoCAR Study. Transplantation. 2017, 101, 5–7. [Google Scholar] [CrossRef] [PubMed]
- Marsh, C.L.; Kurian, S.M.; Rice, J.C.; Whisenant, T.C.; David, J.; Rose, S.; Schieve, C.; Lee, D.; Case, J.; Barrick, B.; Peddi, V.R.; Mannon, R.B.; Knight, R.; Maluf, D.; Mandelbrot, D.; Patel, A.; Friedewald, J.J.; Abecassis, M.M.; First, M.R. Application of TruGraf v1: A Novel Molecular Biomarker for Managing Kidney Transplant Recipients With Stable Renal Function. Transplant Proc. 2019, 51, 722–728. [Google Scholar] [CrossRef] [PubMed]
- Heilman, R.L.; Fleming, J.N.; Mai, M.; Smith, B.; Park, W.D.; Holman, J.; Stegall, M.D. Multiple abnormal peripheral blood gene expression assay results are correlated with subsequent graft loss after kidney transplantation. Clin Transplant. 2023, 37, e14987. [Google Scholar] [CrossRef] [PubMed]
- Park, S.; Guo, K.; Heilman, R.L.; Poggio, E.D.; Taber, D.J.; Marsh, C.L.; Kurian, S.M.; Kleiboeker, S.; Weems, J.; Holman, J.; Zhao, L.; Sinha, R.; Brietigam, S.; Rebello, C.; Abecassis, M.M.; Friedewald, J.J. Combining Blood Gene Expression and Cellfree DNA to Diagnose Subclinical Rejection in Kidney Transplant Recipients. Clin J Am Soc Nephrol. 2021, 16, 1539–1551. [Google Scholar] [CrossRef] [PubMed]
- Li, B.; Hartono, C.; Ding, R.; Sharma, V.K.; Ramaswamy, R.; Qian, B.; Serur, D.; Mouradian, J.; Schwartz, J.E.; Suthanthiran, M. Noninvasive diagnosis of renal-allograft rejection by measurement of messenger RNA for perforin and granzyme B in urine. N Engl J Med. 2001, 344, 947–954. [Google Scholar] [CrossRef] [PubMed]
- Suthanthiran, M.; Schwartz, J.E.; Ding, R.; Abecassis, M.; Dadhania, D.; Samstein, B.; Knechtle, S.J.; Friedewald, J.; Becker, Y.T.; Sharma, V.K.; Williams, N.M.; Chang, C.S.; Hoang, C.; Muthukumar, T.; August, P.; Keslar, K.S.; Fairchild, R.L.; Hricik, D.E.; Heeger, P.S.; Han, L.; Liu, J.; Riggs, M.; Ikle, D.N.; Bridges, N.D.; Shaked, A. Clinical Trials in Organ Transplantation 04 (CTOT-04) Study Investigators. Urinary-cell mRNA profile and acute cellular rejection in kidney allografts. N Engl J Med. 2013, 369, 20–31. [Google Scholar] [CrossRef]
- Muthukumar, T.; Dadhania, D.; Ding, R.; Snopkowski, C.; Naqvi, R.; Lee, J.B.; Hartono, C.; Li, B.; Sharma, V.K.; Seshan, S.V.; Kapur, S.; Hancock, W.W.; Schwartz, J.E.; Suthanthiran, M. Messenger RNA for FOXP3 in the urine of renal-allograft recipients. N Engl J Med. 2005, 353, 2342–2351. [Google Scholar] [CrossRef]
- Ho, J.; Wiebe, C.; Gibson, I.W.; Rush, D.N.; Nickerson, P.W. Immune monitoring of kidney allografts. Am J Kidney Dis. 2012, 60, 629–640. [Google Scholar] [CrossRef] [PubMed]
- Panzer, U.; Reinking, R.R.; Steinmetz, O.M.; Zahner, G.; Sudbeck, U.; Fehr, S.; Pfalzer, B.; Schneider, A.; Thaiss, F.; Mack, M.; Conrad, S.; Huland, H.; Helmchen, U.; Stahl, R.A. CXCR3 and CCR5 positive T-cell recruitment in acute human renal allograft rejection. Transplantation. 2004, 78, 1341–1350. [Google Scholar] [CrossRef] [PubMed]
- Qin, S.; Rottman, J.B.; Myers, P.; Kassam, N.; Weinblatt, M.; Loetscher, M.; Koch, A.E.; Moser, B.; Mackay, C.R. The chemokine receptors CXCR3 and CCR5 mark subsets of T cells associated with certain inflammatory reactions. J Clin Invest. 1998, 101, 746–754. [Google Scholar] [CrossRef] [PubMed]
- Tinel, C.; Devresse, A.; Vermorel, A.; Sauvaget, V.; Marx, D.; Avettand-Fenoel, V.; Amrouche, L.; Timsit, M.O.; Snanoudj, R.; Caillard, S.; Moulin, B.; Olagne, J.; Essig, M.; Gwinner, W.; Naesens, M.; Marquet, P.; Legendre, C.; Terzi, F.; Rabant, M.; Anglicheau, D. Development and validation of an optimized integrative model using urinary chemokines for noninvasive diagnosis of acute allograft rejection. Am J Transplant. 2020, 20, 3462–3476. [Google Scholar] [CrossRef] [PubMed]
- Hirt-Minkowski, P.; Handschin, J.; Stampf, S.; Hopfer, H.; Menter, T.; Senn, L.; Hönger, G.; Wehmeier, C.; Amico, P.; Steiger, J.; Koller, M.; Dickenmann, M.; Schaub, S. Randomized Trial to Assess the Clinical Utility of Renal Allograft Monitoring by Urine CXCL10 Chemokine. J Am Soc Nephrol. 2023, 34, 1456–1469. [Google Scholar] [CrossRef]
- Hricik, D.E.; Formica, R.N.; Nickerson, P.; Rush, D.; Fairchild, R.L.; Poggio, E.D.; Gibson, I.W.; Wiebe, C.; Tinckam, K.; Bunnapradist, S.; Samaniego-Picota, M.; Brennan, D.C.; Schröppel, B.; Gaber, O.; Armstrong, B.; Ikle, D.; Diop, H.; Bridges, N.D.; Heeger, P.S. Clinical Trials in Organ Transplantation-09 Consortium. Adverse Outcomes of Tacrolimus Withdrawal in Immune-Quiescent Kidney Transplant Recipients. J Am Soc Nephrol. 2015, 26, 3114–3122. [Google Scholar] [CrossRef]
| Serum creatinine testing | Creatinine is a lagging and non-specific marker of injury |
| Urine testing | Non-specific |
| Transplant ultrasonography | Non-specific |
| Screening and monitoring donor specific antibodies (DSA) | Not all DSAs are overtly pathogenic, many unknown non-HLA Abs |
| Drug level monitoring | Non-specific |
| Renal biopsy | Expensive and not without complications Subject to sampling error and interpreter variability Histologic assessment has limitations |
| Biomarker Type | Biomarker Definition | Established Examples in Transplantation | Potential new Examples in Transplantation |
|---|---|---|---|
| Diagnostic biomarker | A biomarker used to identify individuals with the disease or condition of interest or define a subset of the disease | Serum creatinine Proteinuria Hematuria DSA Signs of hemolysis Renal ultrasound examination Protocol or for cause biopsy histology |
Urinary three gene mRNA expression signature and wide range of other suggested molecules [3,4] Wide range of urinary target proteins, like CXCL10 and CXCL9 [3] Blood 17-gene mRNA expression “kSORT” [5] Blood 200-gene mRNA expression “TruGraf” [6] Several blood and urine mRNAs [3] Molecular microscope for allograft pathology |
| Prognostic biomarker | A biomarker used to identify likelihood of a clinical event, disease recurrence, or progression | Serum creatinine Proteinuria DSA Protocol or for cause biopsy histology |
Complement-fixing characteristics of DSA [7,8] Edmonton classifier for graft loss [9] Edmonton ABMR molecular score [10]GOCAR 13-gene set [11] |
| Monitoring biomarker | A biomarker measured serially and used to detect a change in the degree or extent of disease; monitoring biomarkers may also be used to indicate toxicity, assess safety, or provide evidence of exposure, including exposures to medical products | Serum creatinine Proteinuria Hematuria Immunosuppressive drug levelsBKV/PCR Signs of hemolysis |
There are currently no new monitoring biomarkers proposed in kidney transplantation |
| Pharmacodynamics/response biomarker | A biomarker used to show that a biologic response has occurred in an individual who has received an intervention or exposure | CD19/CD20 count with rituximab treatment DSA mean fluorescence index after AMMR treatment Post-treatment control biopsy histology |
There are currently no new pharmacodynamics/response biomarkers proposed in kidney transplantation |
| Potential Benefits | Pitfalls |
|---|---|
| Noninvasive blood biomarker | Fractional quantification affected by changes in rdcfDNA |
| Applicable to all solid organ transplantation | Does not exclude TCMR (if ddcfDNA normal) |
| Elevations may occur up to 30 days before histologic changes | Elevated in nonrejection pathologies associated with tissue injury (BKV, CVNI toxicity) |
| Absolute quantification of ddcfDNA not affected by changes in rdcfDNA | Not recommemded for use in early posttransplant period |
| Avoidance of protocol biopsy | No recommended flor use for 24 h post-biopsy |
| Avoidance of unnecessary biopsies | Confounded in pregnancy |
| Noninvasive diagnosis of AMR | Confounders in some repeat and multiorgan transplants |
| Assessment of response to rejection treatment | |
| Indicator for treatment of chronic active AMR |
| Acute rejection median | 2,32% |
| Non-acute rejection median | 0.47% |
| |
| Statistics | Low (dd-cfDNA <0.5% | Hgh (dd-cfDNA > 0.5% | p-value | |
|---|---|---|---|---|
| dd-cfDNA value (%) | Mean (SD) | 0.25 (0.087) | 1.76 (1.40) | - |
| Median | 0.21 (0.19, 0,29) | 1.40 (0.87, 2.02) | - | |
| Min, Max | 0.19, 0.49 | 0.52, 6.70 | - | |
|
% Change in eGFR |
Mean (SD) | -0.40 (18.149) | -8.64 (11.98) | 0.0040 |
| Median | 0.00 (-0.92, 4,76 | -7.50 (-16.22, -1.39) | ||
| Min, Max | -70.73, 33,.33 | -37-50, 32.65 | ||
| Presence of DSAs | 1/37 (2.7%) | 17/42 (40.5%) | <0.0001 | |
| Recurrent Rejection | 0/37 (0.0%) | 9/42 (21.4%) | 0.0028 |
| Symbol | RefSeq | Name | P-value |
|---|---|---|---|
| ZMAT1 | NM_001011657 | Zinc finger, matrin type 1 | 0.01 |
| ETAA1 | NM_019002 | Ewing tumor.associated antigen 1 | 0.04 |
| ZNF493 | NM_001076678 | Zinc finger protein 493 | 0.002 |
| CCDC82 | NM_024725 | Coiled-coil domain containing 82 | 0.02 |
| NFYB | NM_006166 | Nuclear transcription factor Y, β | 0.03 |
| SENP7 | NM_001077203 | SUMO1/sentrin specific peptidase 7 | <0.001 |
| CLK1 | NM_001162407 | CDC-like kinase 1 | 0.01 |
| SENP6 | NM_001100409 | SUMO1/sentrin specific peptidase 6 | 0.01 |
| C1GALT1C1 | NM_001011551 | C1GALT1-specific chaperone 1 | 0.01 |
| SPCS3 | NM_021928 | Signal peptidase complex subunit 3 homolog (S,. cerevisiae) | 0.03 |
| MAP1A | NM_002373 | Microtubule-associated protein 1A | 0.01 |
| EFTUD2 | NM_001142605 | Elongation factor Tu GTP binding domain containing 2 | 0.001 |
| AP1M1 | NM_001130524 | Adaptor-related protein complex 1, mu 1 subunit | <0001 |
| ANXA5 | NM_001154 | Annexin A5 | <0.001 |
| TSC22D1 | NM_001243797 | TSC22 domain family, member 1 | 0.01 |
| F13A1 | NM_000129 | Coagulation factor XIII, A1 polypeptide | 0.02 |
| TUBB1 | NM_030773 | Tubulin, β1 class VI | 0.03 |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





