INTRODUCTION
Adult cervical deformity (CD) is complex pathology characterized by interruption of the normal cervical vertebral alignment in the sagittal and/or coronal planes.[
1,
2] CD is a potentially debilitating disorder of multifactorial etiology that can cause severe discomfort and disability, and is associated with poor health-related quality of life metrics.[
3] Surgical intervention for CD can provide affected patients with significant improvements in quality of life.[
4,
5] However, it is complex surgery and is associated with considerable complication and revision rates.[
2,
5,
6]
Distal junctional kyphosis (DJK) is a mechanical failure complication which remains of particular concern following surgical correction for CD, and is a frequent reason for revision surgery.[
7,
8] DJK denotes a progression in the degree of kyphosis of the vertebral segment adjacent to the lower instrumented vertebra post-operatively.[
9] DJK can lead to considerable morbidity, including pain, imbalance and degenerative disc disease due to increased mechanical stress on adjacent vertebral segments.[
10,
11] Development of early DJK (within three months post-operatively) is associated with particularly more severe radiographic malalignment and neurologic decline.[
12] To our knowledge, there is limited information on the effect of early post-operative DJK on CD surgical recovery.
Mechanical failure complications following surgery to the thoracolumbar spine, such as proximal junctional kyphosis and proximal junctional failure, have been well-studied and literature exists which provides strategy for preventing such complications and identifying particularly at-risk patients.[
13,
14] DJK, which is the more likely mechanical complication following CD surgery has not been studied as extensively. In this context, this study aims to investigate the recovery course following CD surgery in patients who develop early DJK, particularly examining the variation in health-related quality of life metrics up to two years post-operatively.
METHODS
Data Source and Study Design
This is a retrospective analysis of a prospectively collected, single-center database containing adult cervical deformity (CD) patients treated between 2012 and 2019. Institutional Review Board (IRB) approval was obtained prior to patient enrollment and all patients provided informed consent. Patients enrolled in the database were older than 18 years of age and had a plan to undergo surgical correction for cervical deformity. Cervical deformity was defined as meeting at least one of the following radiographic parameters: C2-C7 sagittal kyphosis > 15°, T1 slope minus cervical lordosis (TS-CL) > 35°, C2-C7 sagittal vertical axis (cSVA) > 40 mm, chin-brow vertical angle (CBVA) > 25°, McGregor’s slope (MGS) > 20°, or segmental cervical kyphosis > 15° across any 3 vertebra between C2 and T1. The inclusion criteria of the present study required operative CD patients with complete radiographic and health related quality of life (HRQL) data preoperatively and at 2-years postoperatively.
Distal junctional kyphosis was defined by the development of an angle < -10° from the distal end of the fusion construct to the second adjacent distal vertebra, and/or a change in this angle by < -10° from baseline.[
15] “Early DJK” denoted patients developing this complication before three months post-operatively.
Data Collection and Radiographic Assessment
Standardized data collection forms assessed patient demographics, surgical parameters, and comorbidities at the initial presentation. HRQL metrics were collected via patient surveys at baseline and multiple follow-up time points, and included the Neck Disability Index (NDI), Numeric Rating Scale for the neck (NRS-Neck), EuroQol-5 Dimension (EQ-5D) and modified Japanese Orthopaedic Association (mJOA) assessment. The minimally clinically important difference (MCID) for the mJOA was set at 2 based on published values.[
16,
17] The MCID for Neck Disability Index was set as 15; this is double the published MCID value because our NDI score was collected on a 0-100 scale as opposed to 0-50.[
18,
19] The NRS-Neck MCID was set as 2 per previously published values.[
18,
20]
Lateral spine radiographs were used to assess radiographic parameters at baseline and follow-up intervals. All images were analyzed with SpineView® (ENSAM, Laboratory of Biomechanics, Paris, France). Spinopelvic radiographic parameters assessed included pelvic tilt (PT: the angle between the vertical and the line through the sacral midpoint to the center of the two femoral heads), the mismatch between pelvic incidence and lumbar lordosis (PI-LL), and the sagittal vertical axis (SVA: C7 plumb line relative to the posterosuperior corner of S1). Cervical spine parameters assessed included cervical lordosis (C2-C7 angle), cervical sagittal vertical axis (cSVA: C2 plumb line relative to the posterosuperior corner of C7), T1 slope (T1S), C2 slope (C2S), T1 slope minus cervical lordosis (TS-CL), and McGregor’s Slope (MGS).
Development of the Normalized Integrated Health State
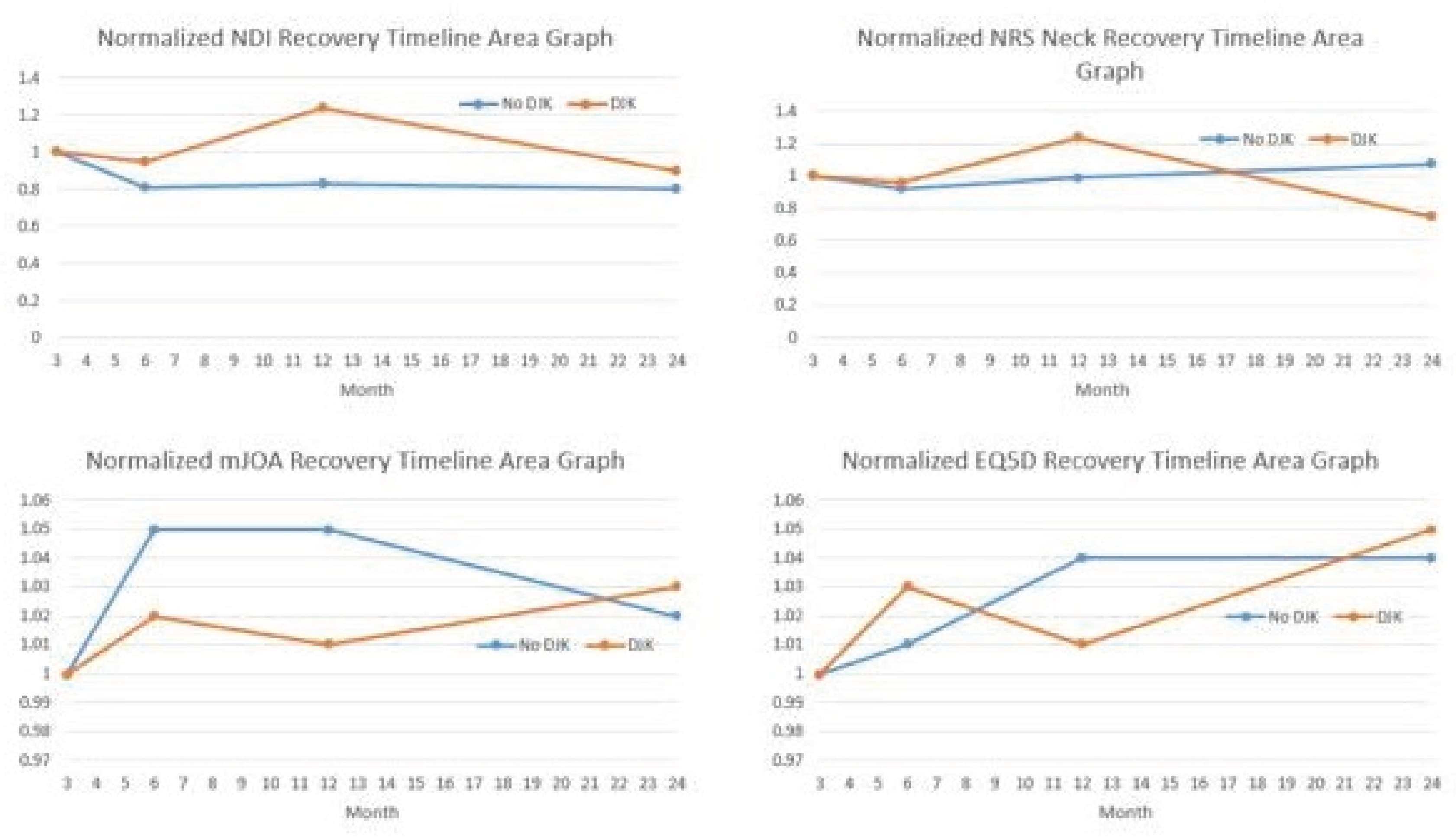
Normalized HRQLs were developed and analyzed, permitting the calculation of an integrated health state using the following validated novel area-under-the-curve methodology.[
21,
22] All reported preoperative and postoperative (3-month, 6-month, 1-year, 2-year) values for each outcome measure were divided by the corresponding preoperative score for each patient. The resulting preoperative normalized HRQL score for all patients was therefore 1, with any follow-up normalized HRQL scores being >1, equal to 1, or <1, depending on whether the patient improved or deteriorated relative to baseline. Normalized HRQL scores were then plotted on an area graph, with the x-axis representing time (in months, starting at the preoperative interval) and the y-axis representing normalized HRQL scores (
Figure 1). Regarding Integrated Health State values for varying outcome metrics, lower NDI Integrated Health State Scores indicate a better outcome (better recovery process), and higher NRS Total scores indicated a better outcome (better recovery process).
Statistical Analysis
Frequency distributions and summary statistics were calculated for all demographic, clinical, surgical, and radiographic variables. Cross-tabulations with Pearson chi-square tests were used to assess categorical variables. Independent t-tests were used to assess differences in continuous variables. Multivariable logistic regression analysis assessed differences in patient outcomes adjusting for age, levels fused, and frailty. All analyses were performed using SPSS software (IBM Corp. IBM SPSS Statistics for Windows, v28.0. Armonk, NY, USA). Statistical tests were two-tailed with significance set to p < 0.05.
RESULTS
Cohort Overview
There were 113 patients included in this study. The mean age in this cohort was 61.1 years, 65% were female, mean body mass index (BMI) was 27.1 ± 5.7 kg/m2, and the mean Charlson Comorbidity Index (CCI) was 0.75 ± 0.5.
Surgical Descriptors
In terms of surgical characteristics, mean levels fused was 5.2 ± 3.5, mean estimated blood loss (EBL) was 894 ± 564 mL, and mean operative time was 405.0 ± 185.1 min. By surgical approach, 7.0% of patients underwent an anterior-only approach, 59.7% underwent posterior-only, and 31.3% underwent a combined approach. The most common upper instrumented vertebra (UIV) was C3, and most common lower instrumented vertebra (LIV) was C7. Overall, 60.4% underwent an osteotomy as part of their procedure (
Table 1).
Postoperative Distal Junctional Kyphosis
Of the 113 patients included in the analysis, 17 developed DJK and 96 did not. Comparing those that developed DJK and those who did not; age (60.3 vs 62.2), gender (F: 71.0% vs 61.0%), BMI (27.0 vs 28.3 kg/m2), CCI (0.77 vs 0.98), operating time (484.0 vs 556.5 min), EBL (1028.3 vs 843.9 mL), and presenting neurologic symptoms (70.6% vs 76.0%) were similar between groups (P > 0.05). Patients who developed early DJK were more likely to have pre-op sagittal malalignment (cervical sagittal vertical axis {cSVA}: 59.0 vs 43.9 mm, p = 0.031), underwent more osteotomies (76.5% vs 49.0%, p = 0.005) and underwent more combined approaches (64.7% vs 26.0%, p = 0.002). Posterior approaches, decompressions, and levels fused were similar between groups (p > 0.05). Following surgery, the rate of complications and development of neurological symptoms were similar between groups, except that DJK patients experienced more dysphagia (17.7% vs 4.2%; p = 0.034). DJK patients also remained more malaligned in cSVA through 2-yr follow-up (73% vs 45%, p = 0.001).
Recovery Kinetics
There were no significant differences between DJK and non-DJK patients at baseline in NDI, NRS-Neck, mJOA and EQ5D scores (
Table 3). Logistic regression analyses controlling for preop cSVA malalignment and surgical invasiveness revealed that patients experiencing DJK were more likely to experience worsening in NDI score post-operatively by one year (OR 1.25, 95% CI: 1.05-1.49, p = 0.035). DJK patients exhibited worse neck disability (NDI) Integrated Health State recovery from 3 months to 1 year (p = 0.014), but these differences subsided when following patients through 2 years (p = 0.232). DJK patients had worse NDI, NRS and mJOA scores at one year, but these differences subsided by 2-year follow up (
Figure 1).
DISCUSSION
The frequency of surgical intervention for CD surgery is increasing due to advancements in technique and patient selection.[
23] With the increased frequency of cervical vertebra instrumentation, mechanical failure complications such as distal junctional kyphosis (DJK) are becoming more notable.[
24] In the cervical spine specifically, DJK has been defined by the development of an angle < -10° from the distal end of the fusion construct to the second adjacent distal vertebra, and/or a change in this angle by < -10° from baseline.[
15] DJK is an important issue to address as it can significantly impact affected patients’ surgical journey; potentially resulting in increased overall cost and also deterioration in achieved clinical and radiographic improvements. Therefore this study aimed to investigate the differences between patients developing post-operative DJK and their unaffected counterparts, with a view to assessing if DJK patients eventually experienced similar levels of improvements as the non-DJK patients.
Our study reports a DJK rate of 15% among the patients included in analysis. Perhaps unsurprisingly, patients who developed DJK had significantly worse cervical sagittal malalignment pre-operatively. Excess pre-operative malalignment has previously been reported to be predictive of DJK development.[
10,
15,
24,
25] Passias
et al. studied 101 patients undergoing CD surgery and reported that excessive malalignment beyond certain thresholds (preoperative cervical lordosis < -12°, preoperative cSVA > 56.3 mm, and preoperative cervical lordosis minus T1 slope > 36.4°) resulted in a five to six times increased risk for DJK.[
15] Patients who developed DJK also underwent a significantly higher frequency of osteotomies and combined surgical approaches, compared to non-DJK patients. Combined surgical approaches and the Smith Peterson osteotomy have previously been reported as notable predictors of DJK.[
12,
15]
Predictably, patients in our study who developed early DJK still exhibited significantly worse cervical sagittal malalignment (cSVA) than their unaffected counterparts at two years. Both pre-operative and post-operative malalignment have been associated with increased rates of DJK.[
26] These patients also exhibited consistently worse HRQL metrics (NDI and EQ-5D) at follow up till one year. Interestingly, these differences were insignificant at two years post-operatively. This indicates that despite these patients still displaying radiographic evidence of malalignment after two years, their overall levels of disability and symptomaticity had eventually improved to comparable levels with their non-DJK counterparts. This was especially evident in the patients who underwent revision surgery due to DJK, who also achieved comparable HRQL outcomes at two years. We have not been able to identify factors contributing to this improvement between one year and two years post-operatively. Previous studies into mechanical failure after cervical vertebra instrumentation predominantly involved follow up till one-year post-operatively.[
7,
11,
15,
26] Future studies will need to include longer-term follow up in order to further shed light on this.
This study is not without limitation. The retrospective nature combined with relatively small sample sizes may limit generalizability of findings. The sample size might also create potential for restricted clinical variation and truncation in certain areas. Further, as CD is a heterogeneous condition, the radiographic parameters used to analyze CD may be limited in their application. The heterogeneous nature of CD also does not allow for more in-depth analysis of focal pre-operative malalignments. We have also not included an analysis of additional therapeutic modalities used post-operatively. Such an analysis may have shed some light on the HRQL improvements noted in the DJK patients between one and two years post-operatively.
CONCLUSIONS
Despite exhibiting similar pre-operative health-related quality of life metrics, patients who developed early post-operative DJK exhibited worse post-operative neck disability following the development of their DJK, when compared with their unaffected. These differences had subsided by 2-year follow-up, highlighting the prolonged but eventual successful course of many DJK patients after CD surgery.
Conflicts of Interest
none.
Ethical Review Committee Statement
Institutional Review Board approval was obtained before enrolling patients in the prospective database. Informed consent was obtained from each patient prior to enrollment.
References
- Kim, H.J.; Virk, S.; Elysee, J.; Passias, P.; Ames, C.; Shaffrey, C.I.; Mundis, G.; Protopsaltis, T.; Gupta, M.; Klineberg, E.; et al. The morphology of cervical deformities: a two-step cluster analysis to identify cervical deformity patterns. J. Neurosurgery: Spine SPI 2020, 32, 353–359. [Google Scholar] [CrossRef]
- Koller, H.; Ames, C.; Mehdian, H.; Bartels, R.; Ferch, R.; Deriven, V.; Toyone, H.; Shaffrey, C.; Smith, J.; Hitzl, W.; et al. Characteristics of deformity surgery in patients with severe and rigid cervical kyphosis (CK): results of the CSRS-Europe multi-centre study project. Eur. Spine J. 2018, 28, 324–344. [Google Scholar] [CrossRef]
- Smith, J.S.; Line, B.; Bess, S.; Shaffrey, C.I.; Kim, H.J.; Mundis, G.; Scheer, J.K.; Klineberg, E.; O’brien, M.; Hostin, R.; et al. The Health Impact of Adult Cervical Deformity in Patients Presenting for Surgical Treatment: Comparison to United States Population Norms and Chronic Disease States Based on the EuroQuol-5 Dimensions Questionnaire. Neurosurgery 2017, 80, 716–725. [Google Scholar] [CrossRef]
- Ailon, T.; Smith, J.S.; I Shaffrey, C.; Kim, H.J.; Mundis, G.; Gupta, M.; Klineberg, E.; Schwab, F.; Lafage, V.; Lafage, R.; et al. Outcomes of Operative Treatment for Adult Cervical Deformity: A Prospective Multicenter Assessment With 1-Year Follow-up. Neurosurgery 2017, 83, 1031–1039. [Google Scholar] [CrossRef]
- Zuckerman, S.L.; Devin, C.J. Outcomes and value in elective cervical spine surgery: an introductory and practical narrative review. J. Spine Surg. 2020, 6, 89–105. [Google Scholar] [CrossRef]
- Passias, P.G.; Oh, C.; Horn, S.R.; Kim, H.J.; Hamilton, D.K.; Sciubba, D.M.; Neuman, B.J.; Buckland, A.J.; Poorman, G.W.; Segreto, F.A.; et al. Predicting the occurrence of complications following corrective cervical deformity surgery: Analysis of a prospective multicenter database using predictive analytics. J. Clin. Neurosci. 2018, 59, 155–161. [Google Scholar] [CrossRef]
- Passias PG, Horn SR, Oh C, et al. Predicting the Occurrence of Postoperative Distal Junctional Kyphosis in Cervical Deformity Patients. Neurosurgery. 2020;86(1):E38-E46.
- Zileli, M.; Akıntürk, N.; Yaman, O. Complications of adult spinal deformity surgery: A literature review. J. Craniovertebral Junction Spine 2022, 13, 17–26. [Google Scholar] [CrossRef]
- Wang, P.-Y.; Chen, C.-W.; Lee, Y.-F.; Hu, M.-H.; Wang, T.-M.; Lai, P.-L.; Yang, S.-H. Distal Junctional Kyphosis after Posterior Spinal Fusion in Lenke 1 and 2 Adolescent Idiopathic Scoliosis-Exploring Detailed Features of the Sagittal Stable Vertebra Concept. Glob. Spine J. 2021, 13, 1112–1119. [Google Scholar] [CrossRef]
- Lee, J.J.; Park, J.H.; Oh, Y.G.; Shin, H.K.; Park, B.G. Change in the Alignment and Distal Junctional Kyphosis Development after Posterior Cervical Spinal Fusion Surgery for Cervical Spondylotic Myelopathy – Risk Factor Analysis. J. Korean Neurosurg. Soc. 2022, 65, 549–557. [Google Scholar] [CrossRef]
- Lafage, R.; Smith, J.S.; Soroceanu, A.; Ames, C.; Passias, P.; Shaffrey, C.; Mundis, G.; Alshabab, B.S.; Protopsaltis, T.; Klineberg, E.; et al. Predicting Mechanical Failure Following Cervical Deformity Surgery: A Composite Score Integrating Age-Adjusted Cervical Alignment Targets. Glob. Spine J. 2022, 13, 2432–2438. [Google Scholar] [CrossRef]
- Pierce KE, Passias PG, Lafage V, et al. P48. Disparities in etiology, clinical presentation and determinants for distal junctional kyphosis based on timing of occurrence: are we treating two separate issues? The Spine Journal. 2020;20(9, Supplement):S169.
- Echt, M.; Ranson, W.; Steinberger, J.; Yassari, R.; Cho, S.K. A Systematic Review of Treatment Strategies for the Prevention of Junctional Complications After Long-Segment Fusions in the Osteoporotic Spine. Glob. Spine J. 2020, 11, 792–801. [Google Scholar] [CrossRef]
- Zhao, J.; Chen, K.; Zhai, X.; Li, M.; Lu, Y. Incidence and risk factors of proximal junctional kyphosis after internal fixation for adult spinal deformity: a systematic evaluation and meta-analysis. Neurosurg. Rev. 2020, 44, 855–866. [Google Scholar] [CrossRef]
- Passias, P.G.; Vasquez-Montes, D.; Poorman, G.W.; Protopsaltis, T.; Horn, S.R.; Bortz, C.A.; Segreto, F.; Diebo, B.; Ames, C.; Smith, J.; et al. Predictive model for distal junctional kyphosis after cervical deformity surgery. Spine J. 2018, 18, 2187–2194. [Google Scholar] [CrossRef]
- Kato, S.; Oshima, Y.; Matsubayashi, Y.; Taniguchi, Y.; Tanaka, S.; Takeshita, K. Minimum Clinically Important Difference and Patient Acceptable Symptom State of Japanese Orthopaedic Association Score in Degenerative Cervical Myelopathy Patients. Spine 2019, 44, 691–697. [Google Scholar] [CrossRef]
- Soroceanu, A.; Lau, D.; Kelly, M.P.; Passias, P.G.; Protopsaltis, T.S.; Gum, J.L.; Lafage, V.; Kim, H.-J.; Scheer, J.K.; Gupta, M.; et al. Establishing the minimum clinically important difference in Neck Disability Index and modified Japanese Orthopaedic Association scores for adult cervical deformity. J. Neurosurgery: Spine 2020, 33, 441–445. [Google Scholar] [CrossRef]
- Carreon, L.Y.; Glassman, S.D.; Campbell, M.J.; Anderson, P.A. Neck Disability Index, short form-36 physical component summary, and pain scales for neck and arm pain: the minimum clinically important difference and substantial clinical benefit after cervical spine fusion. Spine J. 2010, 10, 469–474. [Google Scholar] [CrossRef]
- Young, B.A.; Walker, M.J.; Strunce, J.B.; Boyles, R.E.; Whitman, J.M.; Childs, J.D. Responsiveness of the Neck Disability Index in patients with mechanical neck disorders. Spine J. 2009, 9, 802–808. [Google Scholar] [CrossRef]
- Khan, I.; Pennings, J.S.; Devin, C.J.; Oleisky, E.R.; Bydon, M.; Asher, A.M.B.; Archer, K.R. Clinically Meaningful Improvement Following Cervical Spine Surgery: 30% Reduction Versus Absolute Point-change MCID Values. Spine 2020, 46, 717–725. [Google Scholar] [CrossRef]
- Liu, S.; Tetreault, L.; Fehlings, M.G.; Challier, V.; Smith, J.S.; Shaffrey, C.I.; Arnold, P.M.; Scheer, J.K.; Chapman, J.R.; Kopjar, B.; et al. Novel Method Using Baseline Normalization and Area Under the Curve to Evaluate Differences in Outcome Between Treatment Groups and Application to Patients With Cervical Spondylotic Myelopathy Undergoing Anterior Versus Posterior Surgery. Spine 2015, 40, E1299–E1304. [Google Scholar] [CrossRef]
- A Segreto, F.; Lafage, V.; Lafage, R.; Smith, J.S.; Line, B.G.; Eastlack, R.K.; Scheer, J.K.; Chou, D.; Frangella, N.J.; Horn, S.R.; et al. Recovery Kinetics: Comparison of Patients Undergoing Primary or Revision Procedures for Adult Cervical Deformity Using a Novel Area Under the Curve Methodology. Neurosurgery 2018, 85, E40–E51. [Google Scholar] [CrossRef]
- Smith, J.S.; Shaffrey, C.I.; Bess, S.; Shamji, M.F.; Brodke, D.; Lenke, L.G.; Fehlings, M.G.; Lafage, V.; Schwab, F.; Vaccaro, A.R.; et al. Recent and Emerging Advances in Spinal Deformity. Neurosurgery 2017, 80, S70–S85. [Google Scholar] [CrossRef]
- Lafage, R.; Smith, J.S.; Soroceanu, A.; Ames, C.; Passias, P.; Shaffrey, C.; Mundis, G.; Alshabab, B.S.; Protopsaltis, T.; Klineberg, E.; et al. Predicting Mechanical Failure Following Cervical Deformity Surgery: A Composite Score Integrating Age-Adjusted Cervical Alignment Targets. Glob. Spine J. 2022, 13, 2432–2438. [Google Scholar] [CrossRef]
- Smith, J.S.; Buell, T.J.; Shaffrey, C.I.; Kim, H.J.; Klineberg, E.; Protopsaltis, T.; Passias, P.; Mundis, G.M.; Eastlack, R.; Deviren, V.; et al. Prospective multicenter assessment of complication rates associated with adult cervical deformity surgery in 133 patients with minimum 1-year follow-up. J. Neurosurgery: Spine 2020, 33, 588–600. [Google Scholar] [CrossRef]
- Passias PG, Horn SR, Lafage V, et al. Effect of age-adjusted alignment goals and distal inclination angle on the fate of distal junctional kyphosis in cervical deformity surgery. Journal of craniovertebral junction & spine. 2021;12(1):65-71.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).