Submitted:
07 April 2024
Posted:
10 April 2024
You are already at the latest version
Abstract
Keywords:
Introduction
Methods
Results
Discussion
Conclusion
Limitations of the Study
Strengths of the Study
Acknowledgments
Statement of Ethics
Conflicts of Interest
Funding
Author Contributions
Data availability
Ethical approval
References
- Haneke E. Epidemiology and pathology of the onychomycoses. In: Nolting S, Korting HC: Onychomycoses - Local Antimycotic Treatment. Springer, Berlin Heidelberg New York, 1990: 1-11.
- Gawdzik A, Nowogrodzka K, Hryncewicz-Gwóźdź A, Szepietowski J, Maj J, Jankowska-Konsur A. Epidemiology of dermatophytoses in paediatric population in Southwestern Poland, 2011-2016. Postepy Dermatol Alergol. 2021;38(2):91-95. [CrossRef]
- Kromer C, Celis D, Hipler UC, Zampeli VA, Mößner R, Lippert U. Dermatophyte infections in children compared to adults in Germany: a retrospective multicenter study in Germany. J Dtsch Dermatol Ges. 2021;19(7):993-1001. [CrossRef]
- Gupta AK, Venkataraman M, Shear NH, Piguet V. Onychomycosis in children - review on treatment and management strategies. J Dermatolog Treat. 2022;33(3):1213-1224. [CrossRef]
- Lecerf P, Abdy S, Vollono L, Pastushenko I, Richert B, André J. Direct examination, histopathology and fungal culture for the diagnosis of onychomycosis: A retrospective, comparative study on 2245 specimens. Mycoses. 2021;64(2):187-193. [CrossRef]
- Gupta AK, Taborda VBA, Taborda PRO, Shemer A, Summerbell RC, Nakrieko KA. High prevalence of mixed infections in global onychomycosis. PLoS One. 2020;15(9):e0239648. [CrossRef]
- Haneke E (1999) Achilles foot-screening project: Background, objectives and design. J Eur Acad Dermatol Venereol 12: Suppl 1:S2-S5.
- Haneke E, Roseeuw D (1999) The scope of onychomycosis: epidemiology and clinical features. Int J Dermatol 38: Suppl 2:7-12.
- English MP. Trichophyton rubrum infections in families. Br Med J 1957;2:744-746.
- Zaias N, Tosti A, Rebell G, Morelli R, Bardazzi F, Bieley H, Zaiac M, Glick B, Paley B, Allevato M, Baran R. Autosomal dominant pattern of distal subungual onychomycosis caused by Trichophyton rubrum. J Am Acad Dermatol. 1996;34(2 Pt 1):302-304. [CrossRef]
- Jazdarehee A, Malekafzali L, Lee J, Lewis R, Mukovozov I. Transmission of onychomycosis and dermatophytosis between household members: A scoping review. J Fungi (Basel). 2022;8(1):60. [CrossRef]
- Zaias N, Rebell G, Escovar S. Asymmetric gait nail unit syndrome: the most common worldwide toenail abnormality and onychomycosis. Skinmed. 2014;12(4):217-223.
- Zaias N, Escovar SX, Rebell G. Opportunistic toenail onychomycosis. The fungal colonization of an available nail unit space by non-dermatophytes is produced by the trauma of the closed shoe by an asymmetric gait or other trauma. A plausible theory. J Eur Acad Dermatol Venereol. 2014;28(8):1002-6. [CrossRef]
- Haneke E. Toenails: Where orthopedics and onychology meet. In Baran R, ed. Advances in Nail Disease and Management. Springer Nature Switzerland 2021:71-86.
- Haneke E. Foot, toe and nail changes – are they interdependent? Skin Append Disord 2024, accepted.
- Haneke E. Fungal infections of the nail. Semin Dermatol. 1991;10(1):41-53.
- Ogawa T, Matsuda A, Ogawa Y, Tanaka R. Risk factors for the development of tinea pedis and onychomycosis: Real-world evidence from a single-podiatry center, large-scale database in Japan. J Dermatol. 2024;51(1):30-39. [CrossRef]
- Roseeuw D. Achilles foot screening project: preliminary results of patients screened by dermatologists. J Eur Acad Dermatol Venereol. 1999;12 Suppl 1:S6-9; discussion S17.
- Adams C, Athanasoula E, Lee W, Mahmudova N, Vlahovic TC. Environmental and genetic factors on the development of onychomycosis. J Fungi (Basel). 2015;1(2):211-216. [CrossRef]
- Gupta AK, Sibbald RG, Lynde CW, Hull PR, Prussick R, Shear NH, De Doncker P, Daniel CR 3rd, Elewski BE. Onychomycosis in children: prevalence and treatment strategies. J Am Acad Dermatol. 1997;36(3 Pt 1):395-402. [CrossRef]
- Jha B, Sharma M, Gc S, Sapkota J. Onychomycosis among clinically suspected cases attending the dermatology out-patient department of a tertiary care centre: A descriptive cross-sectional study. JNMA J Nepal Med Assoc. 2021;59(237):450-453. [CrossRef]
- Gupta AK, Wang T, Cooper EA, Lincoln SA, Foreman HC, Scherer WP, Bakotic WL. Clinical diagnosis and laboratory testing of abnormal appearing toenails: a retrospective assessment of confirmatory testing for onychomycosis in the United States, 2022-2023. J Fungi (Basel). 2024 Feb 13;10(2):149. [CrossRef]
- Walshe MM, English MP. Fungi in nails. Br J Dermatol. 1966;78(4):198-207. [CrossRef]
- English MP. Nails and fungi. Br J Dermatol. 1976 Jun;94(6):697-701. [CrossRef]
- Gudnadóttir G, Hilmarsdóttir I, Sigurgeirsson B. Onychomycosis in Icelandic swimmers. Acta Derm Venereol. 1999;79(5):376-7. [CrossRef]
- Möhrenschlager M, Seidl HP, Schnopp C, Ring J, Abeck D. Professional ice hockey players: a high-risk group for fungal infection of the foot? Dermatology. 2001;203(3):271. [CrossRef]
- Caputo R, De Boulle K, Del Rosso J, Nowicki R. Prevalence of superficial fungal infections among sports-active individuals: results from the Achilles survey, a review of the literature. J Eur Acad Dermatol Venereol. 2001;15(4):312-316.
- Jenkins DW, Cooper K, O'Connor R, Watanabe L, Wills C. Prevalence of podiatric conditions seen in Special Olympics athletes: Structural, biomechanical and dermatological findings. Foot (Edinb). 2011;21(1):15-25. [CrossRef]
- Buder V, Augustin M, Schäfer I, Welsch G, Catala-Lehnen P, Herberger K. Prävalenz von Dermatomykosen bei Profifußballspielern : Untersuchung im Rahmen der Bundesligatauglichkeitsuntersuchung (2013–2015) im Vergleich mit Daten der Allgemeinbevölkerung [Prevalence of dermatomycoses in professional football players : A study based on data of German Bundesliga fitness check-ups (2013-2015) compared to data of the general population]. Hautarzt. 2018 May;69(5):401-407. German. [CrossRef]
- Kubec K. Vascular factor in onychomycosis. Acta Univ Carol Med (Praha). 1979;25(5-6):247-333.
- Shemer A, Nathansohn N, Kaplan B, Trau H. Toenail abnormalities and onychomycosis in chronic venous insufficiency of the legs: should we treat? J Eur Acad Dermatol Venereol. 2008;22(3):279-82. [CrossRef]
- Rocha N, Velho G, Horta M, Martins A, Massa A. Cutaneous manifestations of familial amyloidotic polyneuropathy. J Eur Acad Dermatol Venereol. 2005;19(5):605-607. [CrossRef]
- Rich P. Special patient populations: onychomycosis in the diabetic patient. J Am Acad Dermatol. 1996;35(3 Pt 2):S10-2. [CrossRef]
- Dogra S, Kumar B, Bhansali A, Chakrabarty A. Epidemiology of onychomycosis in patients with diabetes mellitus in India. Int J Dermatol. 2002;41(10):647-51. [CrossRef]
- Muniz EC, Rocha RM, Reis ML, Santos VL, Grossi SA. Neuropathic and ischemic changes of the foot in Brazilian patients with diabetes. Ostomy Wound Manage. 2003;49(8):60-70, 72-3.
- Saunte DM, Holgersen JB, Haedersdal M, Strauss G, Bitsch M, Svendsen OL, Arendrup MC, Svejgaard EL. Prevalence of toe nail onychomycosis in diabetic patients. Acta Derm Venereol. 2006;86(5):425-8. [CrossRef]
- Eckhard M, Lengler A, Liersch J, Bretzel RG, Mayser P. Fungal foot infections in patients with diabetes mellitus--results of two independent investigations. Mycoses. 2007;50 Suppl 2:14-9. [CrossRef]
- Dumont IJ. Diagnosis and prevalence of onychomycosis in diabetic neuropathic patients: an observational study. J Am Podiatr Med Assoc. 2009;99(2):135-9. [CrossRef]
- Lauterbach S, Kostev K, Becker R. Characteristics of diabetic patients visiting a podiatry practice in Germany. J Wound Care. 2010;19(4):140, 142, 144 passim. [CrossRef]
- Navarro-Pérez D, Tardáguila-García A, García-Oreja S, López-Moral M, García-Madrid M, Lázaro-Martínez JL. Onychomycosis associated with diabetic foot syndrome: A systematic review. Mycoses. 2023;66(6):459-466. [CrossRef]
- Kuvandik G, Cetin M, Genctoy G, Horoz M, Duru M, Akcali C, Satar S, Kiykim AA, Kaya H. The prevalance, epidemiology and risk factors for onychomycosis in hemodialysis patients. BMC Infect Dis. 2007 Aug 30;7:102. [CrossRef]
- Filho AMS, Ventura CG, Criado PR, Del Negro GB, Freitas RS, Luiz OC, Giudice MC, Neto ED, Benard G. Hemodialysis and kidney transplantation as predisposing conditions to onychomycosis. Nephron. 2017;137(1):38-46. [CrossRef]
- Bersano JMQB, Cordeiro MG, Marson FAL. Prevalence and risk predictors of onychomycosis in patients on hemodialysis: an observation, prospective, and unicenter study in Brazil. Front Med (Lausanne). 2023;10:1268324. [CrossRef]
- Eftekhari H, Haghdar Saheli Y, Ashoobi MT, Mahjoob M, Kazemnezhad Leyli E, Bagheri Toolaroud P. The prevalence of onychomycosis in patients with chronic renal failure undergoing dialysis: A cross-sectional study. Heliyon. 2024 Feb 11;10(4):e25737. [CrossRef]
- Howard J, Sattler F, Mahon R, Sperling J, Leedom J. Clinical features of 100 human immunodeficiency virus antibody-positive individuals from an alternate test site. Arch Intern Med. 1987;147(12):2131-2133.
- Dompmartin D, Dompmartin A, Deluol AM, Grosshans E, Coulaud JP. Onychomycosis and AIDS. Clinical and laboratory findings in 62 patients. Int J Dermatol. 1990;29(5):337-9. [CrossRef]
- Daniel CR 3rd, Norton LA, Scher RK. The spectrum of nail disease in patients with human immunodeficiency virus infection. J Am Acad Dermatol. 1992;27(1):93-97. [CrossRef]
- Castro LÁ, Álvarez MI. Nail dermatophytoma in HIV-infected patients in Cali, Colombia. J Mycol Med. 2021;31(3):101172. [CrossRef]
- Gómez-Moyano E, Crespo-Erchiga V. HIV infection manifesting as proximal white onychomycosis. N Engl J Med. 2017;377(18):e26. [CrossRef]
- Levy LA. Epidemiology of onychomycosis in special-risk populations. J Am Podiatr Med Assoc. 1997;87(12):546-50. [CrossRef]
- Faergemann J, Baran R. Epidemiology, clinical presentation and diagnosis of onychomycosis. Br J Dermatol. 2003;149 Suppl 65:1-4. [CrossRef]
- Borba OSM, Ogawa MM, Kirsztajn GM, Tomimori J. Onychomycosis in immunocompromised population: Phenotypic and molecular identification. Mycoses. 2023;66(11):1018-1024. [CrossRef]
- Al-Mutairi N, Nour T, Al-Rqobah D. Onychomycosis in patients of nail psoriasis on biologic therapy: a randomized, prospective open label study comparing Etanercept, Infliximab and Adalimumab. Expert Opin Biol Ther. 2013;13(5):625-9. [CrossRef]
- Andersen PL, Henning MAS, Jemec GBE, Arendrup MC, Saunte DM. Two cases of proximal subungual onychomycosis caused by trichophyton rubrum in HIV-negative patients during treatment with TNF-α inhibitors combined with methotrexate. Acta Dermatovenerol Croat. 2018;26(4):304-306.
- Alves NCPOP, Moreira TA, Malvino LDS, Rodrigues JJ, Ranza R, de Araújo LB, Pedroso RDS. Onychomycosis in Psoriatic Patients with Nail Disorders: Aetiological Agents and Immunosuppressive Therapy. Dermatol Res Pract. 2020;2020:7209518. [CrossRef]
- Chularojanamontri L, Pattanaprichakul P, Leeyaphan C, Suphatsathienkul P, Wongdama S, Bunyaratavej S. Overall prevalence and prevalence compared among psoriasis treatments of onychomycosis in patients with nail psoriasis and fungal involvement. Biomed Res Int. 2021;2021:9113418. [CrossRef]
- Zaias N, Escovar SX, Zaiac MN, Edwards R, Dutra M, Pona A, Rio ED, Jungcharoensukying P. Onychomycosis, the active invasion of a normal nail unit by a dermatophytic versus the colonization of an existing abnormal nail unit by environmental fungus. Skinmed. 2020;18(1):18-22.
- Murray SC, Dawber RP. Onychomycosis of toenails: orthopaedic and podiatric considerations. Australas J Dermatol. 2002;43(2):105-112. [CrossRef]
- McGonagle D, Tan AL, Benjamin M. The nail as a musculoskeletal appendage--implications for an improved understanding of the link between psoriasis and arthritis. Dermatology. 2009;218(2):97-102. [CrossRef]
- Ash Z, McGonagle D. Joint appendages: the structures which have historically been overlooked in arthritis research and therapy development. Best Pract Res Clin Rheumatol. 2011;25(6):779-784. [CrossRef]
- Haneke E. Anatomy of the nail unit and the nail biopsy. Semin Cutan Med Surg. 2015 Jun;34(2):95-100. [CrossRef]
- Braswell MA, Daniel CR 3rd, Brodell RT. Beau lines, onychomadesis, and retronychia: A unifying hypothesis. J Am Acad Dermatol. 2015 Nov;73(5):849-55. [CrossRef]
- Buttars B, Scott SG, Glinka D, Daniel CR, Brodell RT, Braswell MA. Congenital malalignment of the great toenail, the disappearing nail bed, and distal phalanx deviation: A review. Skin Appendage Disord. 2022;8(1):8-12. [CrossRef]
- Arai H, Arai T, Nakajima H, Haneke E. Formable acrylic treatment for ingrowing nail with gutter splint and sculptured nail. Int J Dermatol. 2004;43(10):759-765. [CrossRef]
- Haneke E. Controversies in the treatment of ingrown nails. Dermatol Res Pract. 2012;2012:783924. [CrossRef]
- Daniel CR 3rd, Tosti A, Iorizzo M, Piraccini BM. The disappearing nail bed: a possible outcome of onycholysis. Cutis. 2005;76(5):325-327.
- Kim JK, Chung HC, Chun EJ, Kim S, Kim CW. Correlation between nail thickness and onychomycosis: misuse of antifungal agents in patients with thick nails. Ann Dermatol. 2024;36(2):123-124 . [CrossRef]
- Drake LA, Patrick Dl, Fleckman P, Andre J, Baran R, Haneke E, Sapede C, Tosti A (1999) The impact of onychomycosis on quality of life: Development of an international onychomycosis-specific questionnaire to measure patient quality of life. J Am Acad Dermatol 41:189-196.
- Vlahovic TC. Onychomycosis: Evaluation, treatment options, managing recurrence, and patient outcomes. Clin Podiatr Med Surg. 2016;33(3):305-18. [CrossRef]
- Sommer S, Sheehan-Dare RA, Goodfield MJ, Evans EG. Prediction of outcome in the treatment of onychomycosis. Clin Exp Dermatol. 2003;28(4):425-8. [CrossRef]
- Evans EG. The rationale for combination therapy. Br J Dermatol. 2001;145 Suppl 60:9-13.
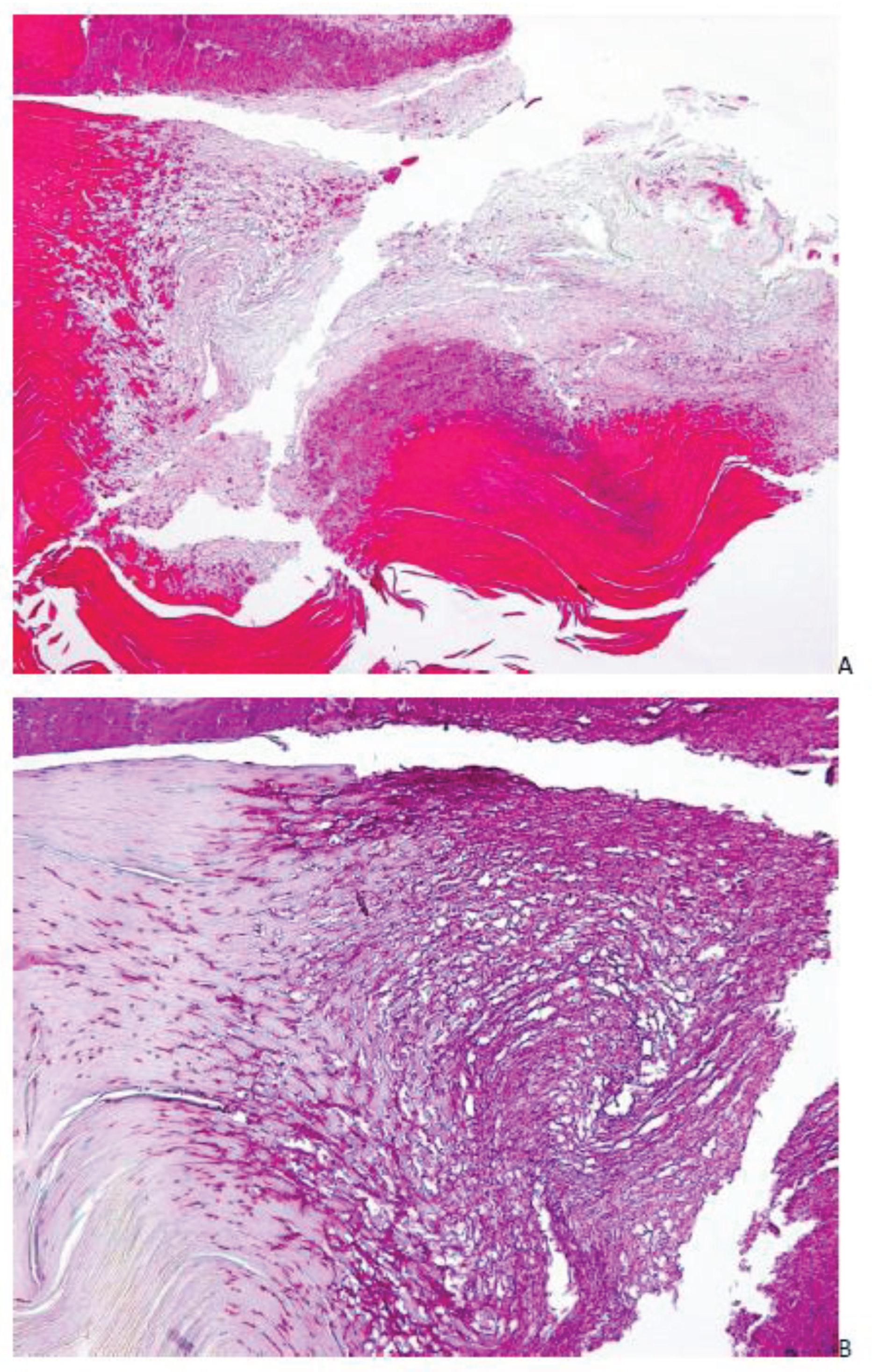
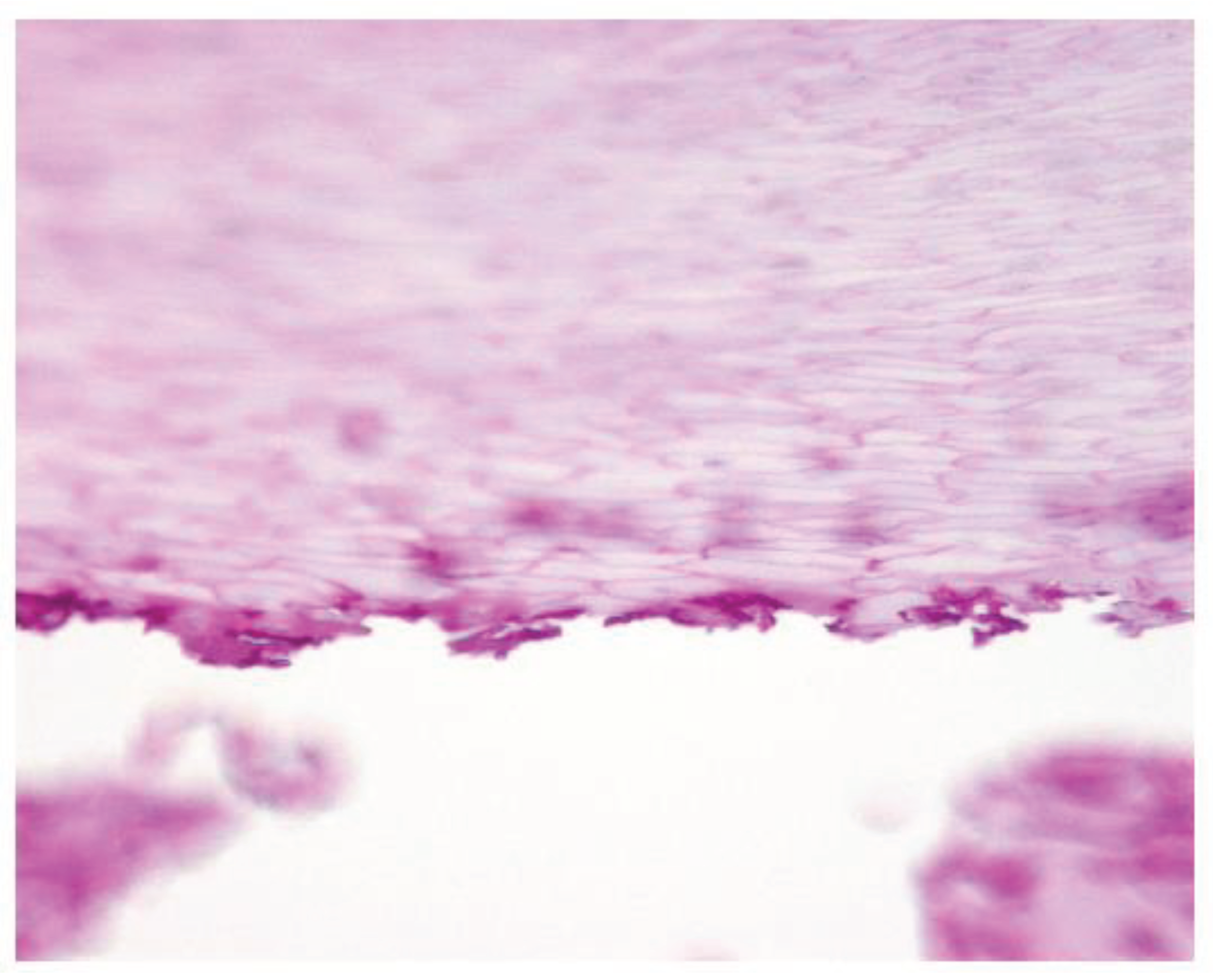
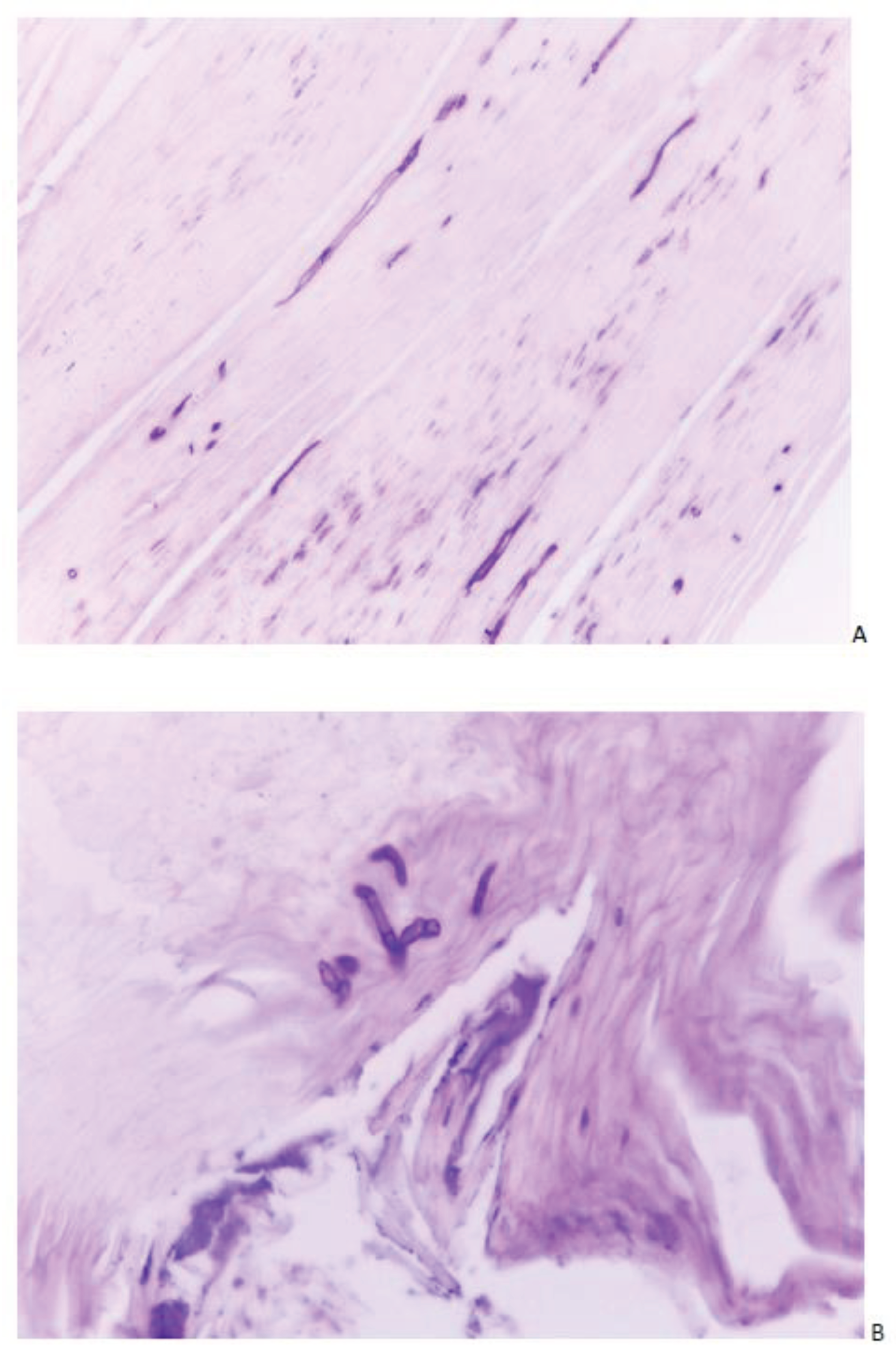
- Roberts DT, Evans EG. Subungual dermatophytoma complicating dermatophyte onychomycosis. Br J Dermatol. 1998;138(1):189-90. [CrossRef]
- Burkhart CN, Burkhart CG, Gupta AK. Dermatophytoma: Recalcitrance to treatment because of existence of fungal biofilm. J Am Acad Dermatol. 2002 Oct;47(4):629-31. [CrossRef]
- Markantonatou AM, Samaras K, Vyzantiadis TA. Dermatophytic biofilms: Characteristics, significance and treatment approaches. J Fungi (Basel). 2023;9(2):228. [CrossRef]
- Haneke E. Nail psoriasis: clinical features, pathogenesis, differential diagnoses, and management. Psoriasis (Auckl) 2017;7:51-63.
- Haneke E. Differential diagnosis of nail psoriasis and onychomycoses: A report based on 40 years of specialised nail consultations. EMJ Dermatol 2020. [CrossRef]
- Aldana-Caballero A, Mayordomo R, Marcos-Tejedor F. Assessment of visual diagnosis by podiatrists for HPV and onychomycosis: the need for complementary tests. J Fungi (Basel). 2022;8(2):135. [CrossRef]














Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).



