Introduction:
The four territories of the thalamus’ vascular supply are the tuberothalamic, inferolateral, paramedian, and posterior choroidal [
1]. First described by Gérard Percheron in 1973, the Artery of Percheron Infarct (AOP) is a rare anatomical vascular variant supplying the paramedian thalamus and the rostral midbrain also. It arises from either proximal segment of the posterior cerebral artery (P1). According to estimates, 4-12% of the general population has AOP [
2] which is an uncommon cause of stroke that accounts for only 0.1–2% of ischemic strokes AOP infraction results in a characteristic pattern of paramedian thalamic infarcts with or without mesencephalic infections.
The four most prevalent patterns of AOP infarction that have been found are: bilateral paramedian thalamic infarction along with midbrain involvement (43%); bilateral paramedian thalamic infarction alone (38%); and bilateral paramedian thalamic infarction along with anterior thalamus involvement and midbrain (14%) and
bilateral paramedian thalamic with anterior thalamus without midbrain (5%) [
2]
It has a variable clinical presentation depending on the specific regions of the thalamus that are affected with or without upper midbrain involvement. Clinical presentation involves a spectrum of neurological deficits ranging from altered mental status and vertical gaze palsy to cognitive impairment and coma. Seizures, parkinsonism, and severe bradycardia are examples of uncommon symptoms [
3].
The diagnosis of this rare stroke is frequently delayed due to its heterogeneity and complex symptoms. Initial diagnosis is quite a challenge as is usually missed in CT scans and the majority of diagnoses are made outside of the thrombolytic window. Neuroimaging techniques such as MRI with diffusion-weighted imaging (DWI) are essential for confirming the diagnosis.
The presented case here of a 40-year-old female shows a clinical situation with difficulties associated with the diagnosis and management of this rare infarction.
Case Presentation:
A 40-year-old female coming from a lower socioeconomic class was presented to the emergency department of LG Hospital by her husband with chief complaints of new onset altered behavior and altered gaze associated with drowsiness for 3 days. The patient was relatively asymptomatic 3 days back, after which her husband noticed her talking irrelevant, which worsened to difficulty in arousing her from sleep in the morning.
There was no associated complaint of fever, headache, vomiting, or breathlessness. No history of seizure, loss of consciousness changes in sleep cycle, or any involuntary movements. No history of previous similar complaints.
Negative History of Alteration in smell, ptosis or any sensory abnormality on the face, any difficulty in hearing, tinnitus, vertigo, or diuresis, Regurgitation of food or fluid & no nasal twang of voice.
Past History:
The patient is a known case of hypertension for 5 years, which is well-controlled and under treatment.
Physical Examination:
Physical examination showed a temperature of 97.9 F, pulse rate of 86/min, blood pressure of 130/80mmHg, SpO2 97% on room air, and RBS of 110 mg/dl. Respiratory examination showed a respiratory rate of 18/min and bilateral equal air entry was present. S1S2 were present on cardiovascular examination. The patient was conscious and responding to verbal commands.
On Neurological examination, the Patient was conscious but disoriented to time, place, and person. Pupils were 2-3mm, bilaterally symmetrical, and reactive to light. vertical gaze palsy was seen along with abnormal gait and sensory ataxia. Deep tendon reflexes were normal with bilateral flexor plantar response. No significant family history was present.
Lab Investigations:
Blood examination, liver function test, renal function test, and lipid profile were normal [
Table 1,
Table 2,
Table 3 and
Table 4]. ECG showed normal sinus rhythm within normal limits.
Radiological Investigations:
The initial CT scan showed no pathological changes. The diagnosis was made the next day on MRI which showed bilateral thalamic, left cerebellar-vermis subacute infarcts with hemorrhagic foci in the right thalamic region, the possibility of artery of Percheron involvement. This was then followed by MR angiography which appeared unremarkable except for mild atherosclerotic changes and hypoplastic right vertebral artery.
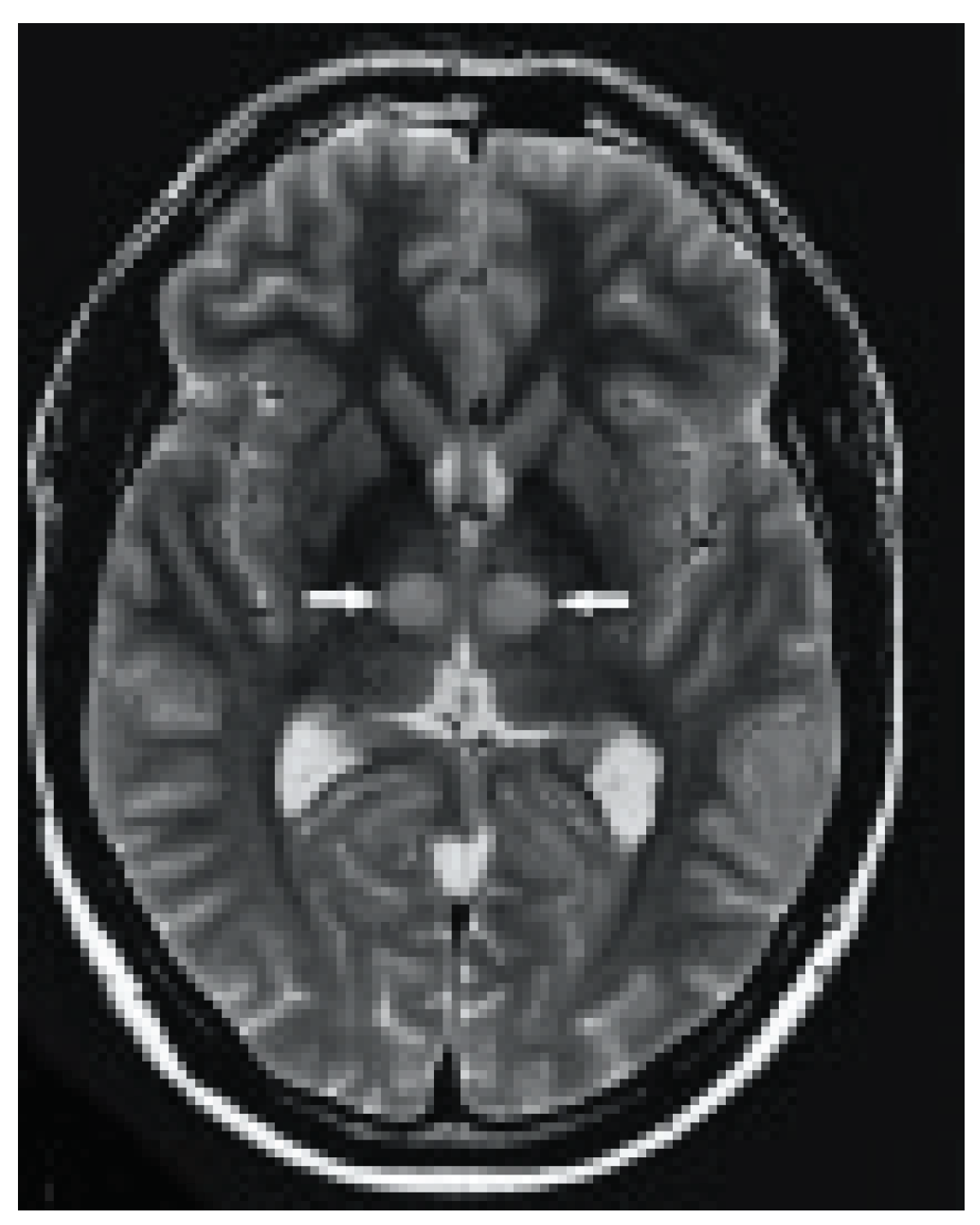
Figure 1.
Axial MRI images showing bilateral high-signal intensity on paramedian thalami in fast spin echo T2 sequence (white arrows).
Figure 1.
Axial MRI images showing bilateral high-signal intensity on paramedian thalami in fast spin echo T2 sequence (white arrows).
Figure 2.
Axial MRI images showing bilateral high-signal intensity on paramedian thalami in FLAIR sequence (black arrows).
Figure 2.
Axial MRI images showing bilateral high-signal intensity on paramedian thalami in FLAIR sequence (black arrows).
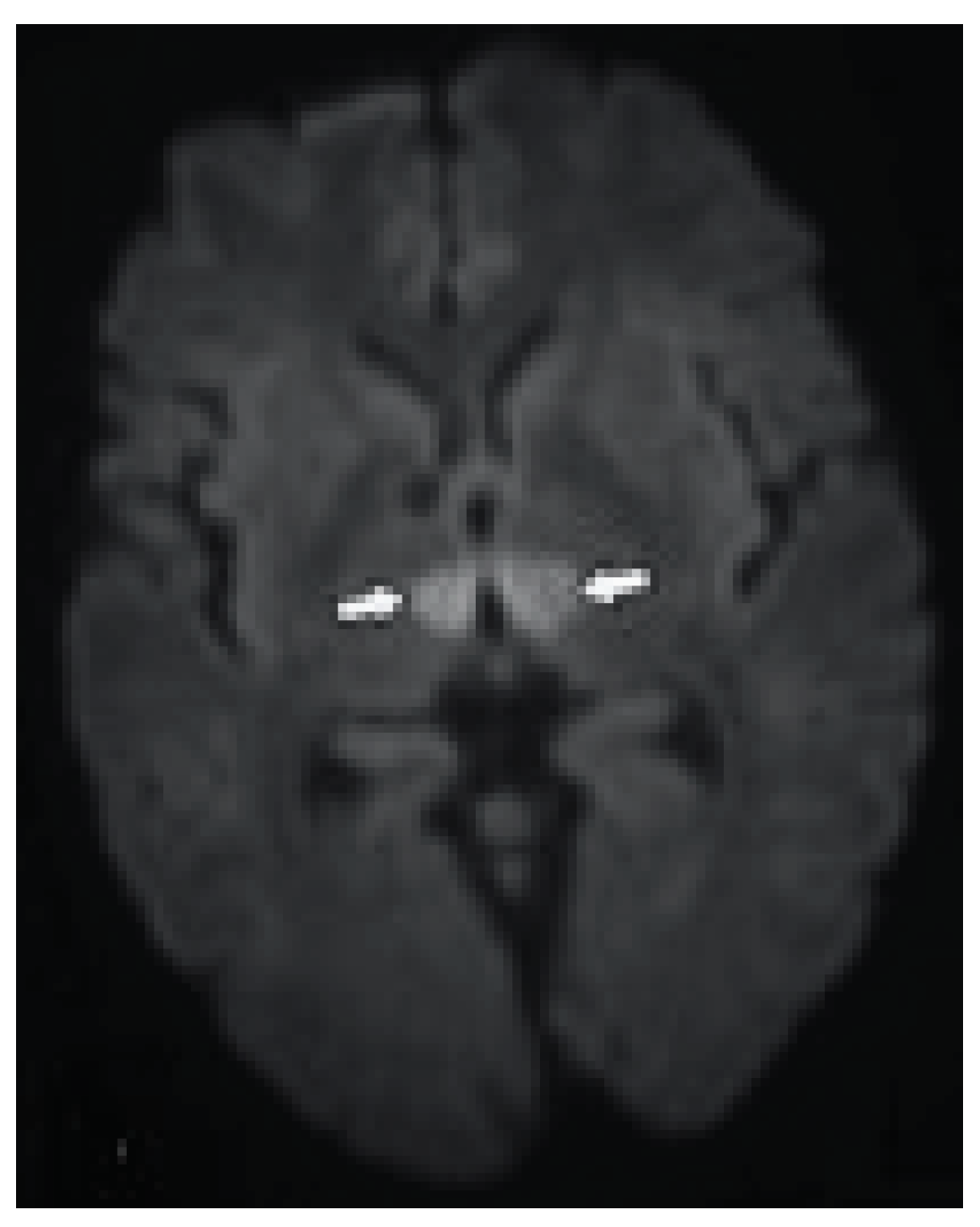
Figure 3.
DW axial image demonstrates bilateral paramedian thalamic hyperintense signal due to restricted diffusion (arrows).
Figure 3.
DW axial image demonstrates bilateral paramedian thalamic hyperintense signal due to restricted diffusion (arrows).
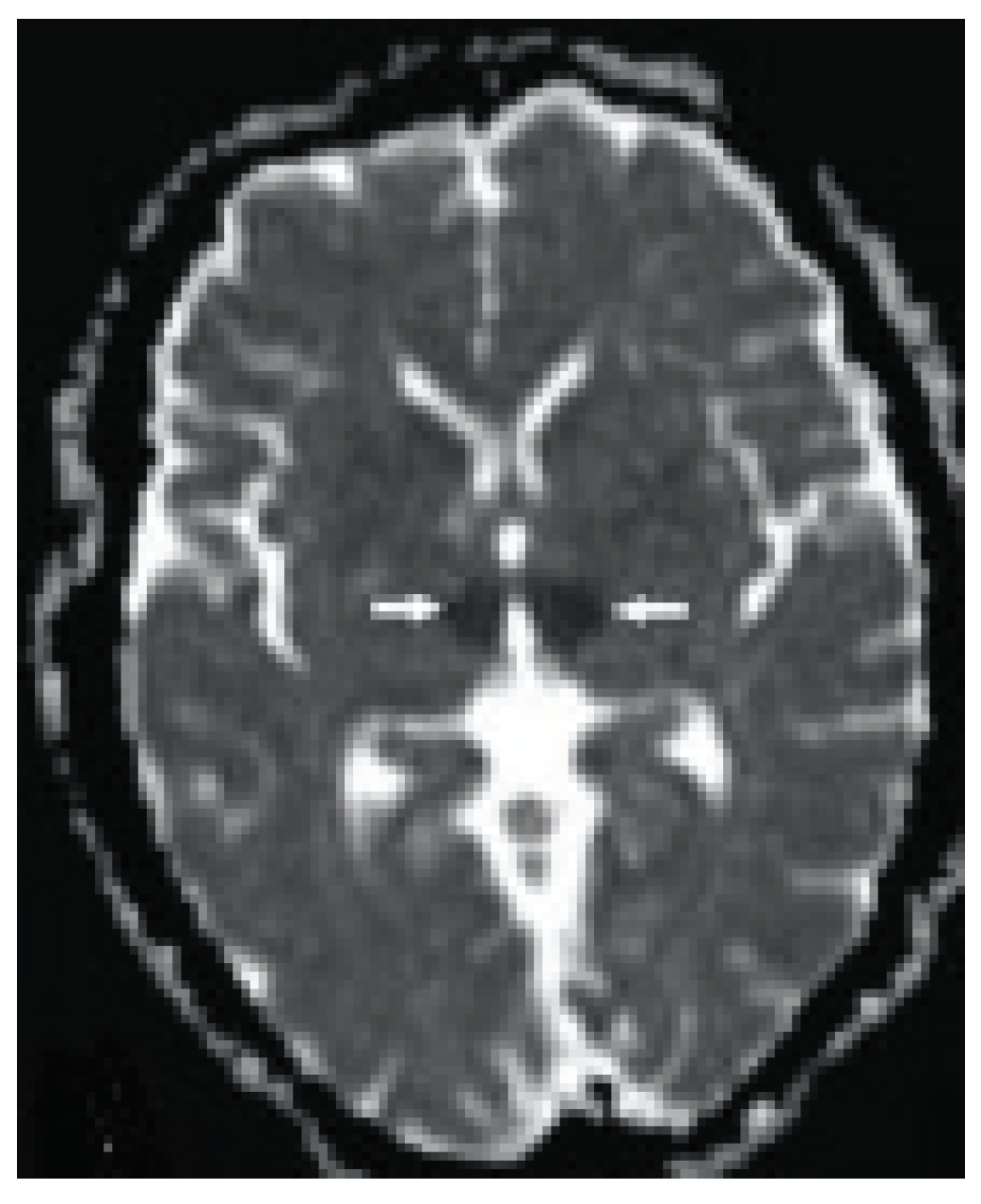
Figure 4.
Apparent diffusion coefficient demonstrates hypointense signal (arrows).
Figure 4.
Apparent diffusion coefficient demonstrates hypointense signal (arrows).
Management:
Primarily, after the initial evaluation the patient was treated with Injectable Mannitol which showed an improvement in the consciousness of the patient.
The patient was treated with Dual antiplatelet therapy (DAPT) and statins. DAPT included Ecosprin 150 mg once a day & clopidogrel and Atorvastatin 40 mg once a day. Supportive therapy like Pantoprazole 40 mg once a day was also given. For hypertension, she was given Amlodipine 5mg twice a day and a tablet of Metropolol 25mg twice a day. The patient was discharged after her condition stabilized and her symptoms improved within 3 days with persistent gaze palsy. DAPT and statins were continued even after the discharge.
Follow Up:
This patient was followed up after 15 days, and there has been no recurrence or aggravation
Diagnosis:
The patient was diagnosed with an artery of Percheron infarct based on the clinical presentation, imaging results, and response to dual antiplatelet therapy and statins.
Discussion:
According to a recently published review in Neurology, just 14 verified cases of AOP were discovered during an eight-year evaluation of a single institution’s neuroimaging database [
4]. The median age of presentation was 67.5 years, and 57% of the participants were female [
4]. Even though AOP infarcts are known to result in long-term impairments, it is clear that most cases manifest late in the clinical course, which reduces the likelihood of receiving thrombolysis treatment [
5]. Because of the vessel’s small diameter, endovascular therapy is frequently not an option [
6]. In addition to usually occurring outside of the thrombolysis window, AOP infarctions can be challenging to diagnose clinically due to their wide range of symptoms.
The thalamus is a significant gray matter component of the diencephalon that forms the third ventricle’s lateral boundary and contains more than 100 nuclei that act as the last hub for afferent and efferent neurons to transmit information [
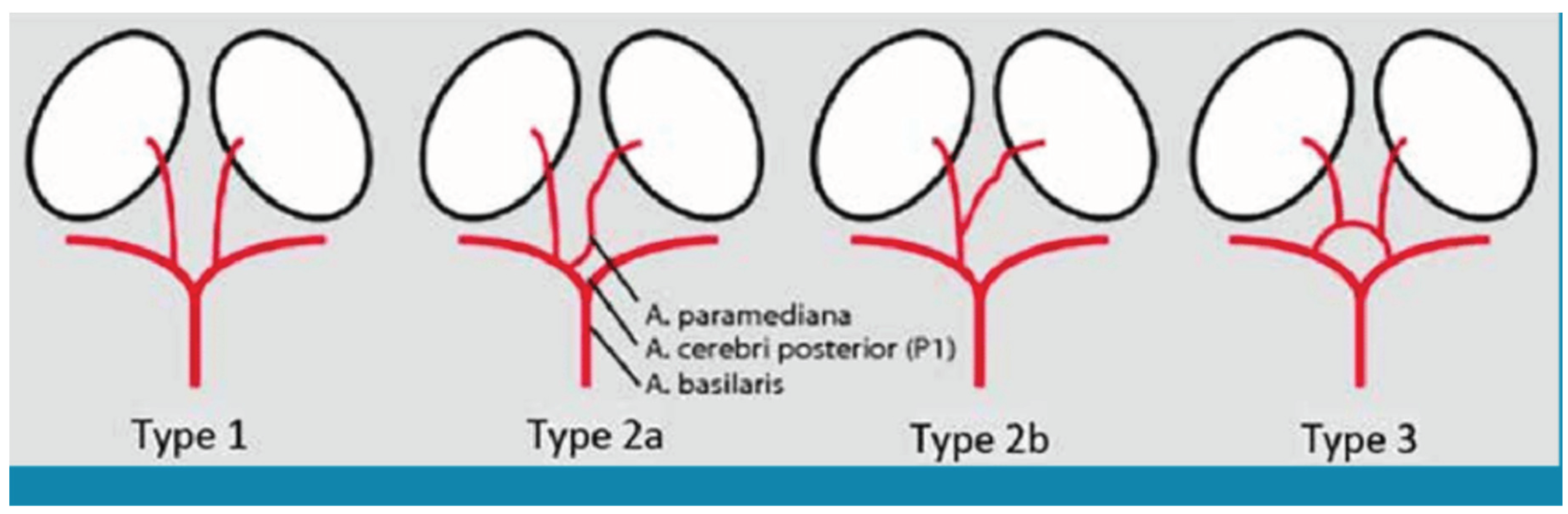
7]. There are four variants of the perforator artery supplying the thalamus and rostral midbrain as described by French neurologist Gerard Percheron. The most common type is type I, in which each posterior cerebral artery’s P1 segment gives birth to two paramedian arteries. Both paramedian arteries emerge from the left or right posterior cerebral arteries (P1 segment) in type IIa. The Artery of Percheron, or Type IIb, is a single trunk that bifurcates to supply the paramedian thalamus and bilateral rostral midbrain. It originates unilaterally from one of the posterior cerebral arteries (P1 segment). The paramedian arteries arise from the proximal aspect (P1 segments) of the left and right posterior cerebral arteries, and type III refers to the presence of a connecting artery between them (
Figure 5) [
8] (Figure 6) [
9]. Between 4% and 18% of the population have Type IIb AOP, however this number may be overestimated [
10].
Infarction of AOP usually presents with the triad as follows (1) Vertical Gaze Palsy (2) Memory Impairments (3) Altered sensorium/Coma. The altered mental status is explained by the involvement of the reticular activating system. Disruption of cortical information that travels through the thalamus and reaches the rostral interstitial medial longitudinal fasciculus is the cause of vertical gaze palsy. It may also present with oculomotor nerve palsy if the involvement of the third cranial nerve. Additionally noticed are cognitive problems such as delirium, hypersexuality, psychosis, and emotional incontinence [
12] As overlapping of vascular supply is seen apart from bilateral paramedian thalamic lesions there are also rostral midbrain lesions producing a ‘mesencephalothalamic syndrome’ characterized by oculomotor disturbances, hemiplegia, cerebellar ataxia, and movement disorders.
The diagnosis of AOP infarction can be challenging due to the bilateral involvement of the thalami and the very small size of AOP infarction which may not be readily apparent on initial clinical assessment like a CT scan. Neuroimaging techniques such as MRI with diffusion-weighted imaging (DWI) are essential for confirming the diagnosis, but delays in obtaining or interpreting imaging studies can contribute to diagnostic delays. Moreover AOP infarction shares clinical features with other neurological conditions, such as metabolic encephalopathy, toxic-metabolic disorders, and bilateral thalamic lesions of different etiologies causing overlapping symptoms that may add further to diagnostic confusion and delay in considering AOP infarction as the underlying cause [
13]. The midbrain “V sign,” a hypertensive signal seen on FLAIR and DWI is a pathognomonic sign with 67% sensitivity to identify AOP infarction, was identified by Lazzaro et al. [
14].
When administered within the therapeutic window (4.5 hours), thrombolytic therapy is the most effective treatment for AOP infarction, as it is for any ischemic stroke. This indicates that the best possible treatment outcome depends on an early diagnosis [
15]. However, in our case, AOP infarction was diagnosed next and hence patient was out of the thrombolysis window and was treated with antiplatelets and statins. Patients recover partially with variable degrees of remaining neurological deficits.
Conclusions:
Artery of Percheron is used to refer to a single arterial branch that arises from one of the proximal segments of either posterior cerebral artery and supplies blood to the paramedian thalami. And the rostral midbrain bilaterally Our case highlights the unusual presentation and that an absence of evidence of AOP infarction in a CT scan does not exclude its diagnosis. The Artery of Percheron infarct requires a comprehensive clinical and radiological examination.
Funding
None of the authors are financially interested in any of the products, devices, or drugs mentioned in this manuscript.
Institutional Review Board Statement
Being a case report study, there were no ethical issues and the IRB was notified about the topic and the case. Still, no formal permission was required as this was a record-based case report. Permission from the patient for the article has been acquired and ensured that their information or identity is not disclosed.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Schmahmann, J.D. Vascular Syndromes of the Thalamus. Stroke 2003, 34, 2264–2278. [Google Scholar] [CrossRef] [PubMed]
- Lazzaro, N.; Wright, B.; Castillo, M.; Fischbein, N.; Glastonbury, C.; Hildenbrand, P.; Wiggins, R.; Quigley, E.; Osborn, A. Artery of Percheron Infarction: Imaging Patterns and Clinical Spectrum. Am. J. Neuroradiol. 2010, 31, 1283–1289. [Google Scholar] [CrossRef] [PubMed]
- Musa, J.; Rahman, M.; Guy, A.; Kola, E.; Guy, A.; Hyseni, F.; Cobo, A.; Saliaj, K.; Bushati, F.; Ahmetgjekaj, I. Artery of Percheron infarction: A case report and literature review. Radiol. Case Rep. 2021, 16, 1271–1275. [Google Scholar] [CrossRef] [PubMed]
- Lott, R.; Zonna, X.; Jose, A.N.; Shin, J.; Roemer, M.; Nasir, A.; Iii, R.L. Artery of Percheron Infarct: A Rare Case Presentation and Recovery. Cureus 2023, 15, e44033. [Google Scholar] [CrossRef]
- Hashtjin, S.R.; Ikramuddin, S.; Streib, C. Artery of Percheron Infarction: Clinical Presentation and Outcomes (P6-5.032). Neurology 2023, 100. [Google Scholar] [CrossRef]
- Powers, W.J.; Rabinstein, A.A.; Ackerson, T.; Adeoye, O.M.; Bambakidis, N.C.; Becker, K.; Biller, J.; Brown, M.; Demaerschalk, B.M.; Hoh, B.; et al. 2018 Guidelines for the Early Management of Patients With Acute Ischemic Stroke: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke 2018, 49, e46–e99. [Google Scholar] [CrossRef] [PubMed]
- Shimizu, Y.; Tsuchiya, K.; Fujisawa, H. Deep Venous Thrombosis with Decreased Cerebral Blood Flow to the Thalamus was Completely Restored by Factor Xa Inhibitor. J. Stroke Cerebrovasc. Dis. 2019, 28, e39–e43. [Google Scholar] [CrossRef] [PubMed]
- Khanni, J.L.; A Casale, J.; Koek, A.Y.; del Pozo, P.H.E.; Espinosa, P.S. Artery of Percheron Infarct: An Acute Diagnostic Challenge with a Spectrum of Clinical Presentations. Cureus 2018, 10, e3276. [Google Scholar] [CrossRef]
- Cassourret, G.; Prunet, B.; Sbardella, F.; Bordes, J.; Maurin, O.; Boret, H. Ischemic Stroke of the Artery of Percheron with Normal Initial MRI: A Case Report. Case Rep. Med. 2010, 2010, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Lamot, U.; Ribaric, I.; Popovic, K.S. Artery of Percheron infarction: A review of the literature with a case report. Radiol. Oncol. 2015, 49, 141–146. [Google Scholar] [CrossRef] [PubMed]
- Nolte, C.; Endres, M.; Jungehulsing, G. Vaskuläre Syndrome des Thalamus. Der Nervenarzt 2011, 82, 231–241. [Google Scholar] [CrossRef] [PubMed]
- Phate, N.; Pawar, T.; Andhale, A.; Singh, R.K.; Talwar, D.; Acharya, S.; Shukla, S.; Kumar, S. Artery of Percheron Stroke: A Case Report With a Diagnostic Challenge. Cureus 2022, 14, e21939. [Google Scholar] [CrossRef] [PubMed]
- Smith, A.B.; Smirniotopoulos, J.G.; Rushing, E.J.; Goldstein, S.J. Bilateral Thalamic Lesions. Am. J. Roentgenol. 2009, 192, W53–W62. [Google Scholar] [CrossRef] [PubMed]
- Lazzaro, N.; Wright, B.; Castillo, M.; Fischbein, N.; Glastonbury, C.; Hildenbrand, P.; Wiggins, R.; Quigley, E.; Osborn, A. Artery of Percheron Infarction: Imaging Patterns and Clinical Spectrum. Am. J. Neuroradiol. 2010, 31, 1283–1289. [Google Scholar] [CrossRef] [PubMed]
- Musa, J.; Rahman, M.; Guy, A.; Kola, E.; Guy, A.; Hyseni, F.; Cobo, A.; Saliaj, K.; Bushati, F.; Ahmetgjekaj, I. Artery of Percheron infarction: A case report and literature review. Radiol. Case Rep. 2021, 16, 1271–1275. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).