1. Introduction
Dental implants for the treatment of missing teeth are a routine option today. There are many factors that affect the success of dental implant treatment [
1]. One of the most important factors for successful implant osseointegration is ensuring primary stability during implant placement [
2]. Primary stability is the biometric stability achieved immediately after implant placement, when the implant is inserted into its designed-open socket, and consists of the mechanical attachment of the implant to the bone [
3].
Osseointegration occurs without the need for movement in the bone socket after implant placement, inducing osteoblast proliferation and differentiation and inhibiting fibrous tissue ingrowth and encapsulation. Factors affecting primary stability include implant size, implant surface morphology and design, bone quality/quantity, surgical technique and surgeon experience [
1,
3].
Assessment of primary stability at implantation is a valid prognostic factor for successful osseointegration. A non-invasive clinical method, the IT (IT) test, is commonly used to quantify the primary stability of implants [
4]. It is a parameter that measures the frictional resistance encountered by the fixture as it rotates about its axis while advancing apically. The maximum IT is expressed in Newton centimetres (Ncm) and is predictive of the primary and secondary stability of the implant [
5]. There is no consensus on the minimum IT required to achieve osseointegration. However, to achieve "ideal" primary stability at implant placement, oral surgeons generally recommend an IT of less than 55 Ncm [
6,
7]. It has been shown that IT values in this range prevent detrimental micromovement under implant loading, and therefore promote osseointegration [
8]. There is evidence from clinical experience that there is a linear relationship between primary stability and implant IT [
9,
10]. High IT's are associated with the possible occurrence of bone overcompression and therefore bone necrosis, which could lead to failure of osseointegration. In addition, changes and deformations may occur in the various structures of the implants due to overload or irregular distribution of forces caused by the high IT [
11,
12].
Local differences in bone anatomy and morphology may explain differences in implant osseointegration results. The ratio of cortical to trabecular bone is higher in the mandible than in the maxilla. Research suggests that implant survival is longer in the mandible than in the maxilla because primary stability of the implant has been shown to be lower in low-density bone than in high-density bone [
13,
14]. Crestal cortical thickness and medial cancellous bone density and their relative distribution at the implant site determine the quantity and quality of host bone. Inadequate bone quantity and density is the major risk factor for implant failure because it is associated with excessive bone resorption and impaired healing [
15]. Several studies show an association between increased failure rates and implant placement in D4 bones. In contrast, implants placed in D1-D3 bone are associated with good osseointegration. It is important to consider bone quality when planning implant placement, surgical procedure, healing time and implant loading [
16,
17,
18].
Even if careful pre-operative planning is carried out prior to dental implant treatment and all conditions for dental implant placement are considered optimal, problems that may arise during surgery due to local factors and preparation of the surgical site may affect the treatment [
19]. If adequate stability is not provided during implant placement, micromovement may occur, a fibrous tissue capsule may form, and the healing process may be disrupted, resulting in implant mobility and subsequent implant failure [
2]. Routinely, the primary stability lost during implant placement is regained by replacing the implant with a wider implant; however, there is no established protocol in the literature for the management of this complication [
20]. There are no studies in the literature investigating the achievement of implant stability in implants where primary stability is not achieved at implant placement. The aim of this study was to evaluate the use of a flexible synthetic bone graft to provide implant stability in the absence of implant stability during implant placement in a dense cortical bone model.
2. Materials and Methods
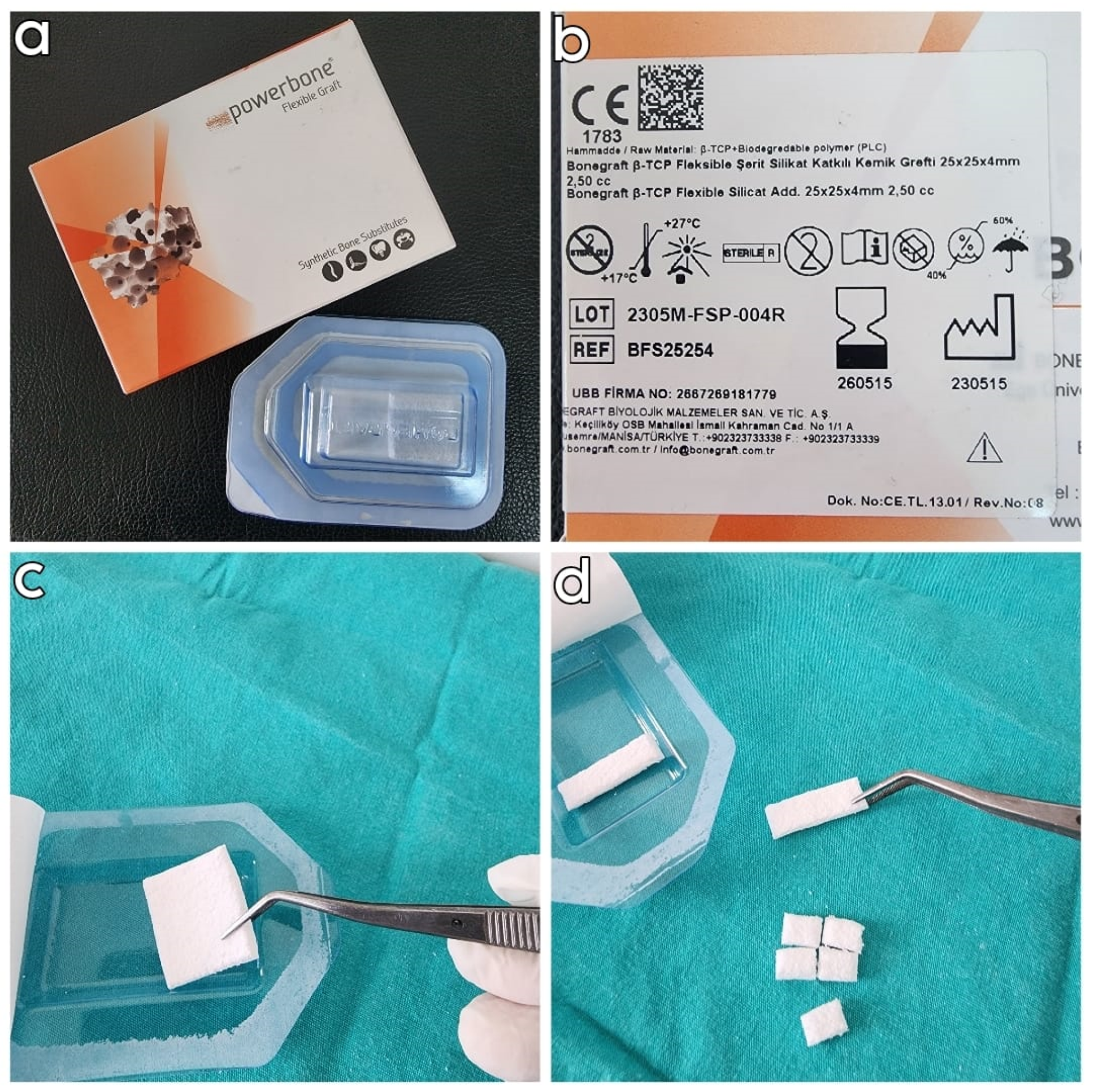
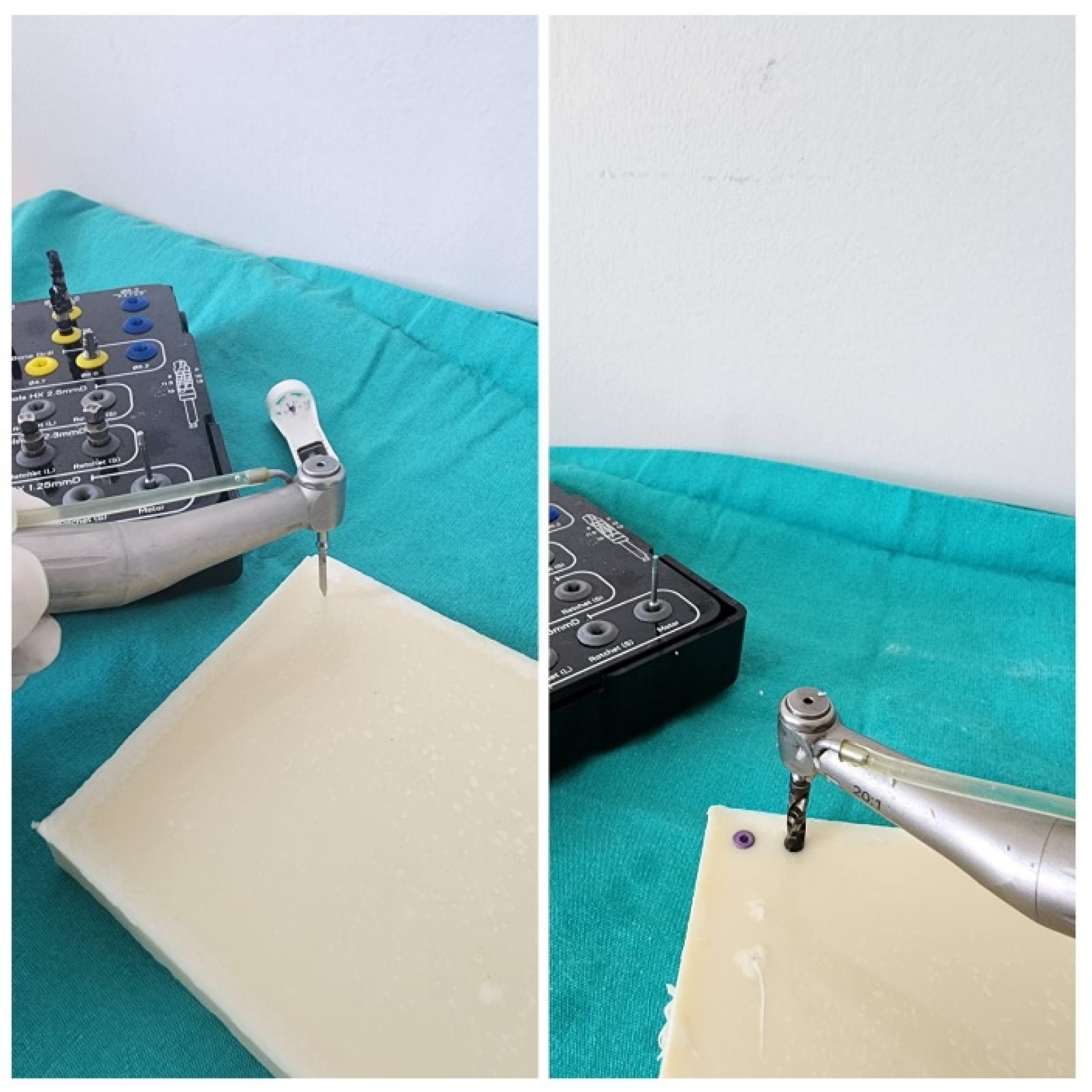
This single-blind in vitro study was conducted at the Department of Oral and Maxillofacial Surgery, Faculty of Dentistry, Van Yüzüncü Yıl University in January 2024. Polyurethane blocks measuring 25x10x2.5 cm with a density of 0.96 g/cm3 (60 pcf) (PURYAP Construction Chemicals and Machinery Industry Trade.Co.Ltd., İstanbul, Turkey) were used to simulate the dense D1 bone model. Flexible synthetic polymer bone graft (FSPBG) (Bonegraft β-TCP Flexible Strip Silicate Added Bone Graft, 25x25x4 mm, Izmir, Turkey) was used in the study groups (
Figure 1). FSPBG is composed of silicate additive β-TCP and PLA based synthetic polymer. The 8 x 5 x 4 mm and 4 x 5 x 4 mm FSPBGs were prepared from manufactured synthetic blocks with dimensions of 25 x 25 x 4 mm. It was controlled that the FSPBGs obtained had the same dimensions. The study used 4.3 x 8 mm tapered platform-switch dental implants (Medisolaris Venuscon Implant, Izmir, Turkey) with an RBM surface. According to the sample size calculation made according to the reference article, it was determined that the minimum number of n in the study groups should be 24 (power= 99%; d=1.494; α=0.01) [
21]. The study was originally designed with 4 groups and a total of 100 implant sites. In each group, implant sites were created according to a specific standard protocol. In all implant sites in the groups, 4.3 x 8 mm implants were placed at bone level. To ensure blinding of the investigators in the study, all sockets were created by a surgeon outside the study according to the protocol specified for the groups and only the assistants knew which sockets belonged to which group.
Drilling protocol
All implant sockets in the groups were created by a single oral and maxillofacial surgeon who was independent of the study, specialised in his field, and actively performing implants. The sockets were created using a physiodispenser (Straumann Surgical Motor Pro, NSK Nakanishi Inc., Japan) and a 20:1 reduction implant handpiece (NSK S-Max SG20, Japan) at 700 rpm and 35 torque using a standardised protocol. Again, as a standard protocol during implant placement, the implant placement process was completed by starting with 5 torques at 30 rpm and increasing the torque by 5 torques at the last and highest torque value when the implant was placed in the socket at bone level. The highest torque value obtained at this point was recorded as the IT.
Study Groups
Group 1 (control group): Implant sockets were prepared using the standard 4.3 x 8 mm implant drilling protocol (The socket width was 3.8 mm in the neck region, 3.4 mm apically, and the socket length was 8 mm). Implants were placed at bone level (
Figure 2).
Group 2: Implant sockets were prepared using the standard drilling protocol for a 5.0 x 8 mm implant. The final drill of a 4.3 mm implant was then used to reach a depth of 10 mm (The socket width was 4.4 mm in the neck region, 3.8 mm apically, and the socket length was 10 mm). An 8x5x4 mm FSPBG was placed in the sockets. The implants were placed at bone level (
Figure 3).
Group 3: Implant sockets were prepared according to the standard drilling protocol of a 5.0 x 8 mm implant (The socket width was 4.4 mm in the neck region, 3.8 mm apically, and the socket length was 8 mm). An 4x5x4 mm FSPBGs were placed in the sockets. Implants were placed at bone level (
Figure 3).
Group 4: Implant sockets were prepared using the standard drilling protocol of a 5.0 x 8 mm implant (The socket width was 4.4 mm in the neck region, 3.8 mm apically, and the socket length was 8 mm). FSPBGs measuring 8x5x4 mm were placed in the sockets.
After implant placement, it was determined that none of the implants in group 4 had been placed at bone level, so group 4 was excluded from the study and not included in the statistical analysis. The study data were analysed and interpreted for 3 groups.
Statistical analysis
In evaluating the results obtained in the study, SPSS 26 was used for statistical analyses. In evaluating the study data, quantitative variables were presented using mean, standard deviation, median, minimum and maximum values and qualitative variables were presented using descriptive statistical methods such as frequency and percentage. The Shapiro-Wilks test and box plots were used to assess the suitability of the data for normal distribution. Student's t-test was used to evaluate two groups with normal distribution, one-way ANOVA test was used to compare three or more groups and Bonferroni test was used to determine the group causing the difference. The results were evaluated with 95% confidence interval and significance at p<0.05 level.
3. Results
When the socket groups used in the study were examined; 33.3% (n=25) were control, 33.3% (n=25) were oversized and deepened and 33.3% (n=25) were oversized only. IT values ranged between 10 and 65 Nm, with an average of 39.53±13.46 Nm (
Table 1).
A statistically significant difference was found between the IT values according to the groups (p=0.001; p<0.01). As a result of the pairwise comparisons made to determine the source of the difference; the IT values of the sockets in the control group are significantly higher than the oversized and deepened sockets (p=0,048; p<0,05). The IT values of the sockets in the control group are significantly higher than the oversized only sockets (p=0,001; p<0,01). The torque values of the oversized and deepened sockets were significantly higher than the oversized only sockets (p=0.001; p<0.01), (
Table 2).
The IT values of the sockets in the control group were statistically significantly higher than the oversized sockets (p=0.001; p<0.01), (
Table 3).
4. Discussion
The increased use of dental implants in recent years has naturally led to an increase in the number of implant-related problems. Dental implant complications include infection, fracture of the jaw bone, damage to surrounding anatomical structures, bleeding, loss of hard or soft tissue in the peri-implant area, devitalisation of the adjacent tooth, aspiration of the implant, fracture of the implant, loosening/fracture of the abutment screw and loss of osseointegration of the implant. Although the cause of loss of osseointegration of the implant cannot be accurately predicted, it is generally believed to be due to micromovement of the implant during the healing process. Primary stability of the implant is assessed using various methods such as maximum IT, implant stability quotient and removal torque. To restore primary stability to an implant that has lost stability during implantation, it is replaced with a larger implant if there is sufficient surrounding tissue, or the defect area is grafted and the implant reimplanted [
22,
23,
24].
Today, scientific advances and government guidelines have led to a reduction in the use of all animal models in dental implant research. New development strategies are gradually replacing some in vivo experiments with in vitro or biomaterial approaches [
25]. In this context, polyurethane models can be used as an alternative to human bone. The homogeneity and regularity of this model makes it an ideal material for comparative testing of bone screws and other medical instruments [
26]. Looking at dental implant-related studies using polyurethane models, Di Stefano et al. compared methods for measuring primary implant stability on spongy bone-like polyurethane blocks of different densities and found that the IT-depth curve integral is a reliable method for measuring primary stability [
24]. Comuzzi et al. compared polyurethane blocks of different densities and reported that implant insertion and removal torques increased with increasing density [
27]. Similarly, Stoilov et al. found that polyurethane blocks used in different densities affected the ITs of the implant, with higher ITs being achieved with higher densities [
28]. The use of polyurethane blocks for comparison between the ITs obtained from different sockets is considered appropriate according to the studies. For this reason, a dense D1 bone-like polyurethane block (60 pcf) was used in this study, and as a result of the trials it was observed that both the surgeon had a bone-like feeling when opening the socket and that consistent results were achieved after implant placement.
When analysing the relationship between implant stability and the design of the implant socket, in the study by Haw-Ming Huang et al. in rabbits, the implant socket was prepared in 3 different ways, standard, narrower and wider, and they found that the highest stability was found in undersized sockets. Histological examinations showed similar results in bone implant contact at the end of the 2nd month [
29]. In their study of sheep proximal tibia, Yurttan et al. used 4 mm diameter implants, one group had a 3.5 mm diameter socket and the other group had an enlarged socket with a 4.2 mm diameter socket. Primary stability could only be measured in the control group, resonance frequency analysis could not be performed in the enlarged socket. At the end of 3 months, similar removal torque values were found between the groups with and without primary stability [
30]. In their study on rabbits, Cohen et al. placed 3.75 mm diameter implants in one group and 3.55 mm diameter implants in the other group in sockets drilled to a diameter of 3.65 mm. On histological examination, they found similar bone-to-implant contact between the small and large diameter socket groups [
31]. In contrast to these studies, in a study in the posterior maxilla, Seleem et al made a socket to fit the implant in one group as recommended by the implant manufacturer, and in the other group they made a socket 0.2 mm wider than the implant. At the end of the third month, the implant stability score was higher in the widened socket group than in the control group [
32]. In their study on rat tibiae, Dündar et al. placed implants with primary stability in one group and implants without primary stability in the other. They reported that better osseointegration was achieved in the primary stabilised group compared to the implants without primary stability [
33]. The above studies have shown that osteointegration can be achieved in the long term in the absence of implant stability, but the rate of reintegration is higher for implants with initial stability. In addition, studies showing no difference in long-term osteointegration have shown that implants should have low initial stability. In this study, the application of FSPBG to the sockets during implant placement was shown to be effective in providing initial implant stability in implants without initial primary stability. The highest ITs were achieved in the control group with the sockets prepared according to the manufacturer's instructions. When the two groups of oversized sockets were compared, it was found that the oversized and deepened sockets achieved higher torque values. This suggests that in the event of loss of primary stability during implant placement, re-implantation by deepening the implant socket and applying FSPBG to the socket will provide a more successful result if the surrounding anatomy allows. Again, in cases where socket deepening is not possible and implant stability is lost due to socket widening, we have shown that implant stability can be achieved by placing FSPBG in the socket. No study was found in the literature that ensured stability of implants without IT during implantation, and this study was the first in the literature to do so. The limitations of this study were as follows. It was observed that the FSPBG placed in the sockets in the study groups were placed apically during implant placement and very few of them were present laterally to the implant. Therefore, despite the primary stability of the implants, it is possible that the resistance to lateral forces is low in the initial phase. When determining the size of the grafts applied to the sockets, they were prepared to be close to the size of the socket. No other parameters were used. Although we have shown that FSPBG is effective in mechanically compressing the implant in vitro, it is not known whether it will provide the same result in the clinical setting. It has not been evaluated whether the primary stability achieved with the use of FSPBG in the oversized and deepened group can be achieved by simply placing the implant without the use of graft for the same socket model. The study was designed to measure the removal torque of the implants in addition to the insertion torque. However, it was found that the lateral forces generated during removal due to the wide implant sockets negatively affected the measurements, and the evaluation of removal torque was cancelled due to the lack of standardisation of this factor.
5. Conclusions
In conclusion, this study was the first to evaluate the use of FSPBG to achieve primary stability in cases of loss of implant stability. The application of FSPBG to oversized implant sockets was found to be successful in increasing implant stability and, in addition, deepening the socket was found to further increase primary stability. Further clinical studies are required to confirm the results of this in vitro study.
Author Contributions
Conceptualization, L.C. and Z.D.O.; methodology, Z.D.O.; software, Z.D.O.; validation, L.C.; formal analysis, L.C.; investigation, L.C.; resources, L.C.; data curation, Z.D.O.; writing—original draft preparation, L.C.; writing—review and editing, Z.D.O.; visualization, Z.D.O; supervision, Z.D.O.; project administration, Z.D.O. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors on request.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Ustaoğlu, G.; Paksoy, T.; Gümüş, K. Evaluating the Effect of Design and Length of Implants on Primary Stability Using Resonance Frequency Analysis: An in Vitro Study. Selcuk Dental Journal 2020, 7, 265–272. [Google Scholar] [CrossRef]
- Sachdeva, A.; Dhawan, P.; Sindwani, S. Assessment of Implant Stability: Methods and Recent Advances. British Journal of Medicine and Medical Research 2016, 12, 1. [Google Scholar] [CrossRef]
- Javed, F.; Almas, K.; Crespi, R.; Romanos, G.E. Implant Surface Morphology and Primary Stability: Is There a Connection? Implant dentistry 2011, 20, 40–46. [Google Scholar] [CrossRef]
- Di Stefano, D.A.; Arosio, P.; Capparè, P.; Barbon, S.; Gherlone, E.F. Stability of Dental Implants and Thickness of Cortical Bone: Clinical Research and Future Perspectives. A Systematic Review. Materials 2021, 14, 7183. [Google Scholar] [CrossRef] [PubMed]
- Di Stefano, D.A.; Arosio, P.; Perrotti, V.; Iezzi, G.; Scarano, A.; Piattelli, A. Correlation between Implant Geometry, Bone Density, and the Insertion Torque/Depth Integral: A Study on Bovine Ribs. Dentistry journal 2019, 7, 25. [Google Scholar] [CrossRef]
- Aldahlawi, S.; Demeter, A.; Irinakis, T. The Effect of Implant Placement Torque on Crestal Bone Remodeling after 1 Year of Loading. Clinical, cosmetic and investigational dentistry 2018, 203–209. [Google Scholar] [CrossRef] [PubMed]
- Ebenezer, S.; Kumar, V.V.; Thor, A. Basics of Dental Implantology for the Oral Surgeon. Oral and Maxillofacial Surgery for the Clinician 2021, 385–405. [Google Scholar]
- Ziebart, J.; Fan, S.; Schulze, C.; Kämmerer, P.; Bader, R.; Jonitz-Heincke, A. Effects of Interfacial Micromotions on Vitality and Differentiation of Human Osteoblasts. Bone & Joint Research 2018, 7, 187–195. [Google Scholar]
- Baldi, D.; Lombardi, T.; Colombo, J.; Cervino, G.; Perinetti, G.; Di Lenarda, R.; Stacchi, C. Correlation between Insertion Torque and Implant Stability Quotient in Tapered Implants with Knife-Edge Thread Design. BioMed research international 2018, 2018. [Google Scholar] [CrossRef]
- Barone, A.; Alfonsi, F.; Derchi, G.; Tonelli, P.; Toti, P.; Marchionni, S.; Covani, U. The Effect of Insertion Torque on the Clinical Outcome of Single Implants: A Randomized Clinical Trial. Clinical implant dentistry and related research 2016, 18, 588–600. [Google Scholar] [CrossRef]
- Bashutski, J.D.; D’Silva, N.J.; Wang, H. Implant Compression Necrosis: Current Understanding and Case Report. Journal of periodontology 2009, 80, 700–704. [Google Scholar] [CrossRef]
- Trisi, P.; Todisco, M.; Consolo, U.; Travaglini, D. High versus Low Implant Insertion Torque: A Histologic, Histomorphometric, and Biomechanical Study in the Sheep Mandible. International Journal of Oral & Maxillofacial Implants 2011, 26. [Google Scholar]
- Farré-Pagès, N.; Augé-Castro, M.L.; Alaejos-Algarra, F.; Mareque-Bueno, J.; Ferrés-Padró, E.; Hernández-Alfaro, F. Relation between Bone Density and Primary Implant Stability. Med Oral Patol Oral Cir Bucal 2011, 16, e62–7. [Google Scholar] [CrossRef]
- Tabassum, A.; Meijer, G.J.; Wolke, J.G.; Jansen, J.A. Influence of the Surgical Technique and Surface Roughness on the Primary Stability of an Implant in Artificial Bone with a Density Equivalent to Maxillary Bone: A Laboratory Study. Clinical oral implants research 2009, 20, 327–332. [Google Scholar] [CrossRef]
- Javed, F.; Ahmed, H.B.; Crespi, R.; Romanos, G.E. Role of Primary Stability for Successful Osseointegration of Dental Implants: Factors of Influence and Evaluation. Interventional Medicine and Applied Science 2013, 5, 162–167. [Google Scholar] [CrossRef]
- Alsaadi, G.; Quirynen, M.; Michiels, K.; Jacobs, R.; Van Steenberghe, D. A Biomechanical Assessment of the Relation between the Oral Implant Stability at Insertion and Subjective Bone Quality Assessment. Journal of clinical periodontology 2007, 34, 359–366. [Google Scholar] [CrossRef] [PubMed]
- Molly, L. Bone Density and Primary Stability in Implant Therapy. Clinical oral implants research 2006, 17, 124–135. [Google Scholar] [CrossRef] [PubMed]
- Linetskiy, I.; Demenko, V.; Linetska, L.; Yefremov, O. Impact of Annual Bone Loss and Different Bone Quality on Dental Implant Success–A Finite Element Study. Computers in biology and medicine 2017, 91, 318–325. [Google Scholar] [CrossRef]
- Peker, E.; Karaca, İ. İmplant Tedavisinin Prognozunu Etkileyen Lokal Risk Faktörleri. Atatürk Üniversitesi Diş Hekimliği Fakültesi Dergisi 2015, 25, 105–111. [Google Scholar]
- Lee, C.; Chen, Y.; Starr, J.R.; Chuang, S. Survival Analysis of Wide Dental Implant: Systematic Review and Meta-analysis. Clinical oral implants research 2016, 27, 1251–1264. [Google Scholar] [CrossRef] [PubMed]
- Ciğerim, L.; Orhan, Z.D.; Kahraman, N.H.; Alsmadı, M.; Bsaileh, M. İmplant Stabilitesi Değerlendirmesinde Model Materyali Olarak Kalsiyum Fosfat Kullanılabilir Mi? Van Diş Hekimliği Dergisi 2023, 4, 1–8. [Google Scholar]
- Liaw, K.; Delfini, R.H.; Abrahams, J.J. Dental Implant Complications.; Elsevier, 2015; Vol. 36, pp. 427–433.
- Ergüven, S.S.; Yıldızer, E.; Ozkan, A.; Şahin, Z.S.; Sarı, S.K.; Peker, F. Correlation between Preoperative Bone Quality and Primer Stability for Mandibular Posterior Implants. ADO Klinik Bilimler Dergisi 13, 2–9.
- Di Stefano, D.A.; Arosio, P.; Gastaldi, G.; Gherlone, E. The Insertion Torque-Depth Curve Integral as a Measure of Implant Primary Stability: An in Vitro Study on Polyurethane Foam Blocks. The Journal of Prosthetic Dentistry 2018, 120, 706–714. [Google Scholar] [CrossRef]
- Blanc-Sylvestre, N.; Bouchard, P.; Chaussain, C.; Bardet, C. Pre-Clinical Models in Implant Dentistry: Past, Present, Future. Biomedicines 2021, 9, 1538. [Google Scholar] [CrossRef] [PubMed]
- Okazaki, Y.; Hayakawa, E.; Tanahashi, K.; Mori, J. Mechanical Performance of Metallic Bone Screws Evaluated Using Bone Models. Materials 2020, 13, 4836. [Google Scholar] [CrossRef]
- Comuzzi, L.; Tumedei, M.; Covani, U.; Romasco, T.; Petrini, M.; Montesani, L.; Piattelli, A.; Di Pietro, N. Primary Stability Assessment of Conical Implants in Under-Prepared Sites: An in Vitro Study in Low-Density Polyurethane Foams. Applied Sciences 2023, 13, 6041. [Google Scholar] [CrossRef]
- Stoilov, M.; Shafaghi, R.; Stark, H.; Marder, M.; Kraus, D.; Enkling, N. Influence of Implant Macro-Design,-Length, and-Diameter on Primary Implant Stability Depending on Different Bone Qualities Using Standard Drilling Protocols—An In Vitro Analysis. Journal of Functional Biomaterials 2023, 14, 469. [Google Scholar] [CrossRef] [PubMed]
- Huang, H.-M.; Chee, T.-J.; Lew, W.-Z.; Feng, S.-W. Modified Surgical Drilling Protocols Influence Osseointegration Performance and Predict Value of Implant Stability Parameters during Implant Healing Process. Clinical Oral Investigations 2020, 24, 3445–3455. [Google Scholar] [CrossRef]
- Yurttutan, M.E.; Kestane, R.; Keskin, A.; Dereci, O. Biomechanical Evaluation of Oversized Drilling on Implant Stability-an Experimental Study in Sheep. JPMA. The Journal of the Pakistan Medical Association 2016, 66, 147–150. [Google Scholar]
- Cohen, O.; Ormianer, Z.; Tal, H.; Rothamel, D.; Weinreb, M.; Moses, O. Differences in Crestal Bone-to-Implant Contact Following an under-Drilling Compared to an over-Drilling Protocol. A Study in the Rabbit Tibia. Clinical oral investigations 2016, 20, 2475–2480. [Google Scholar] [CrossRef]
- Seleem, A.; Tawfik, O.K.; El-Nahass, H. Evaluation of Oversized Drilling on Implant Survival and Stability Versus Traditional Drilling Technique: A Randomized Clinical Trial. International Journal of Oral & Maxillofacial Implants 2021, 36. [Google Scholar]
- Dündar, S.; Çakmak, Ö.; Solmaz, M.Y. Primer Stabilizasyon Olan ve Olmayan Implantlarda Kemik Implant Kaynaşmasının Biyomekanik Incelenmesi: In Vivo Bir Çalışma. Atatürk Üniversitesi Diş Hekimliği Fakültesi Dergisi 2018, 28, 188–193. [Google Scholar]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).