Submitted:
16 March 2024
Posted:
18 March 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
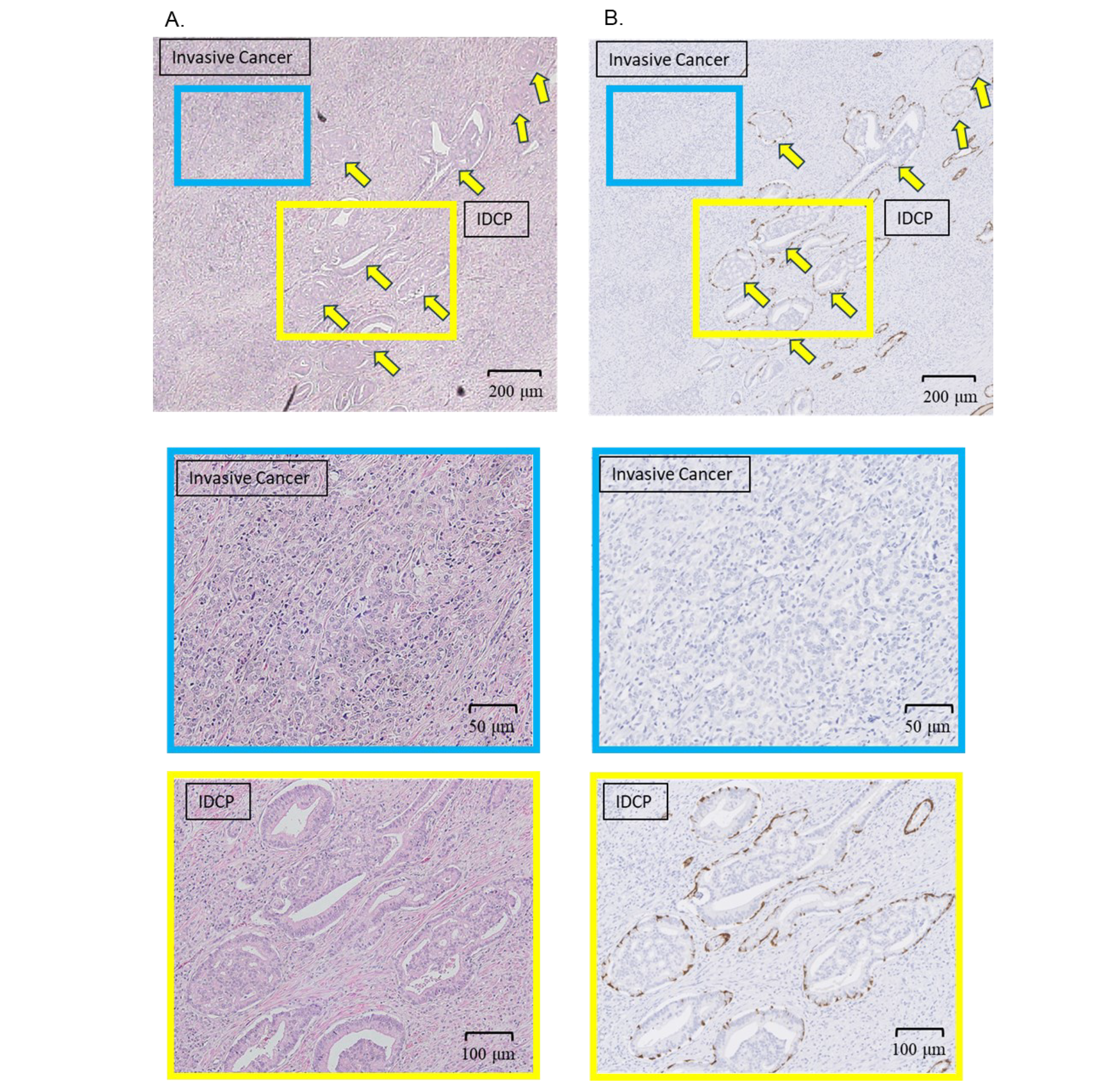
2.1. IDCP Diagnosis
2.2. Spatial Transcriptomics (CytAssist Visium)
3. Results
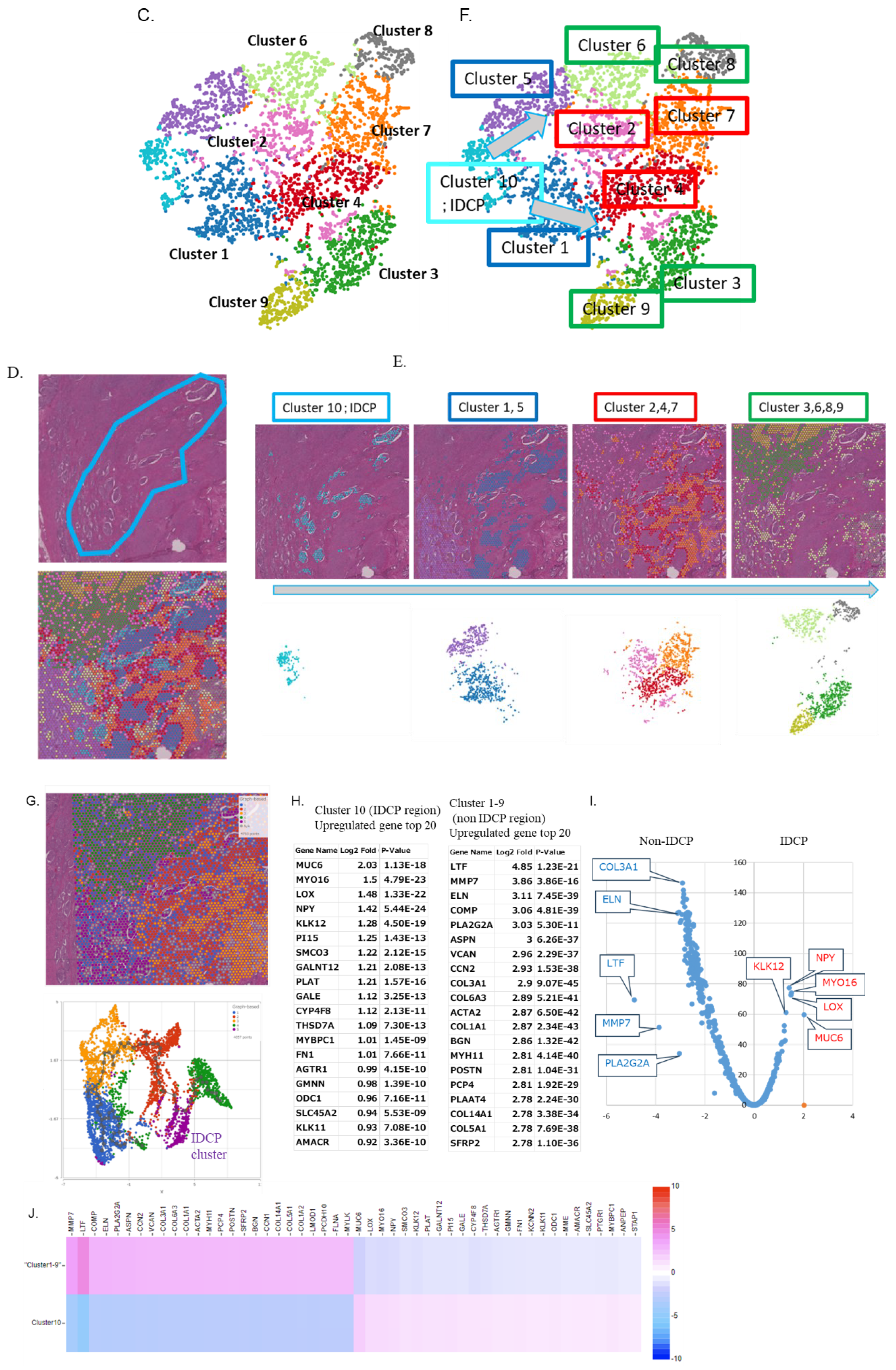
3.1. Diagnosis of IDCP and Clustering by Spatial Gene Expression Analysis
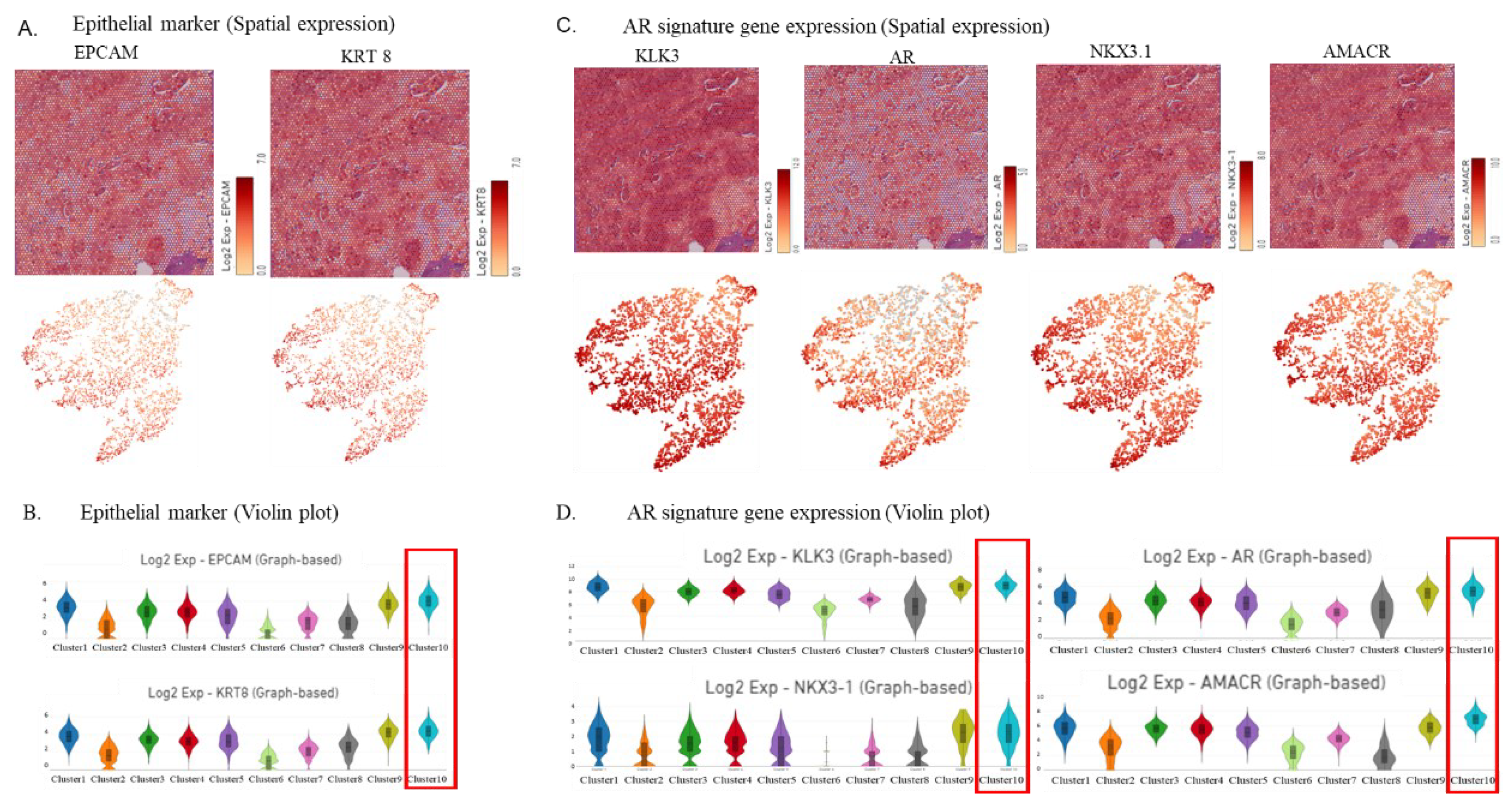
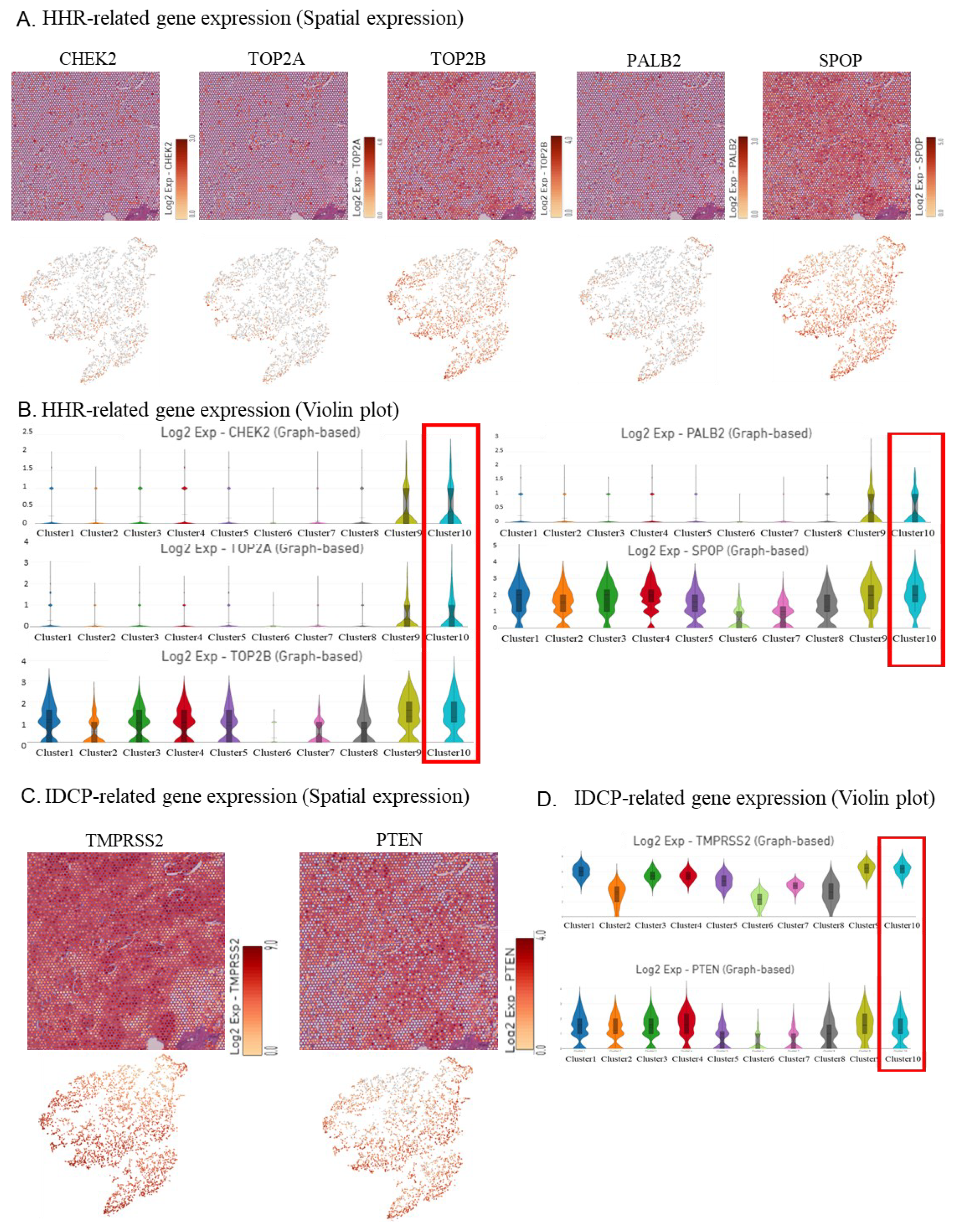
3.2. Visualization of Epithelial Cell, Androgen Receptor (AR) Signature Gene,and Other Upregulated Gene Marker Expression in the IDCP Region
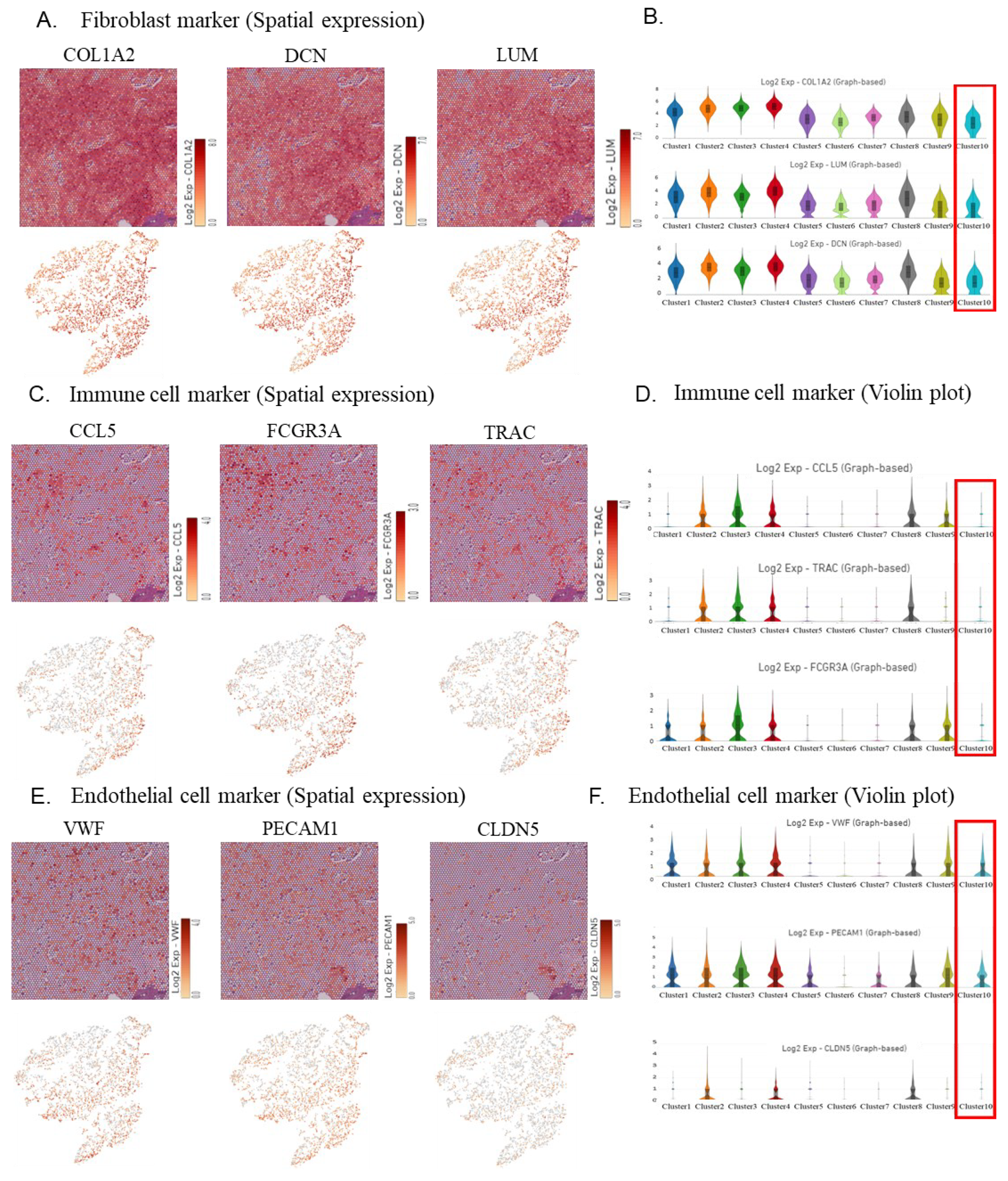
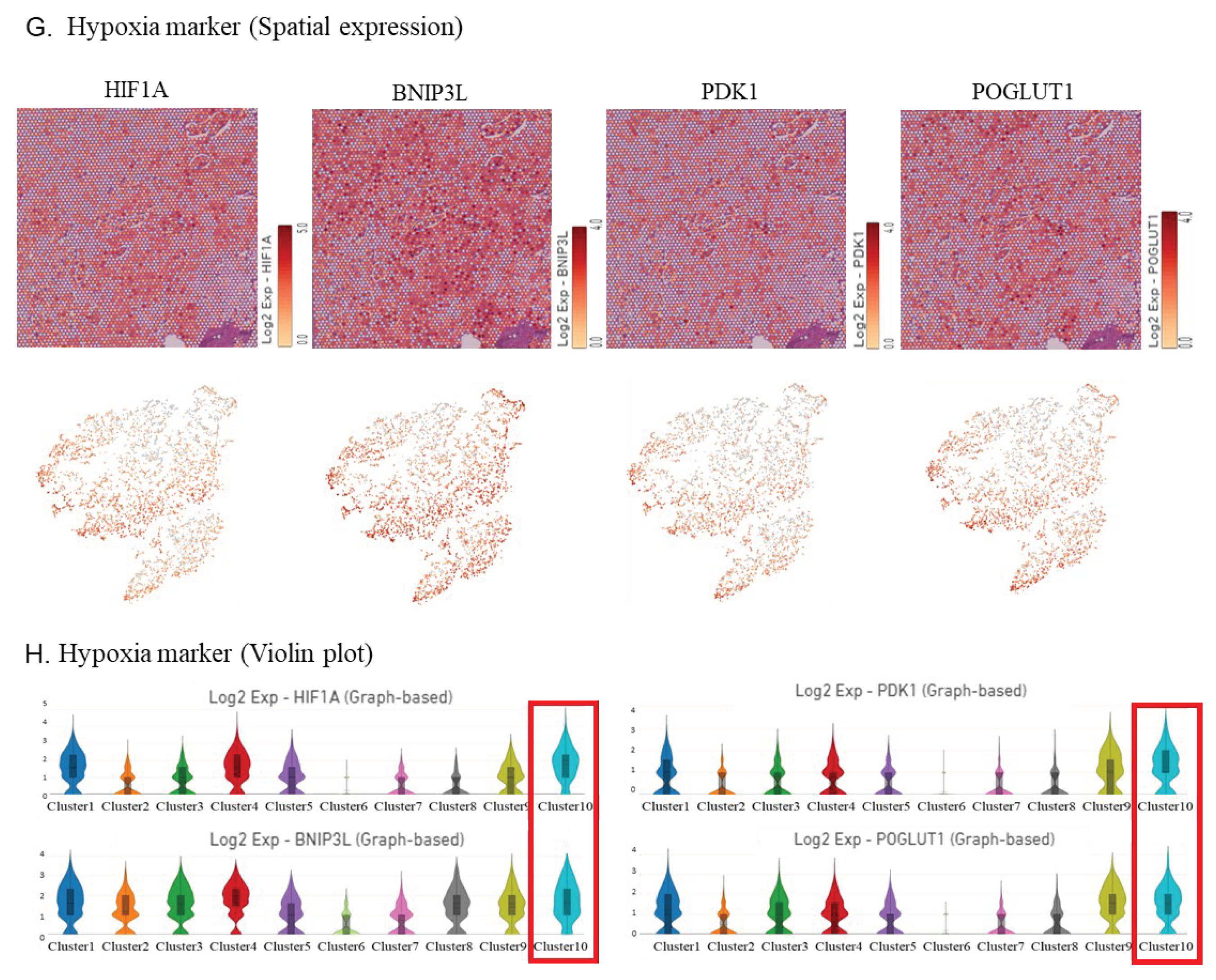
3.3. Visualization of the Expression of IDCP Fibroblast Markers, Immune Cell Markers, and Hypoxia Markers
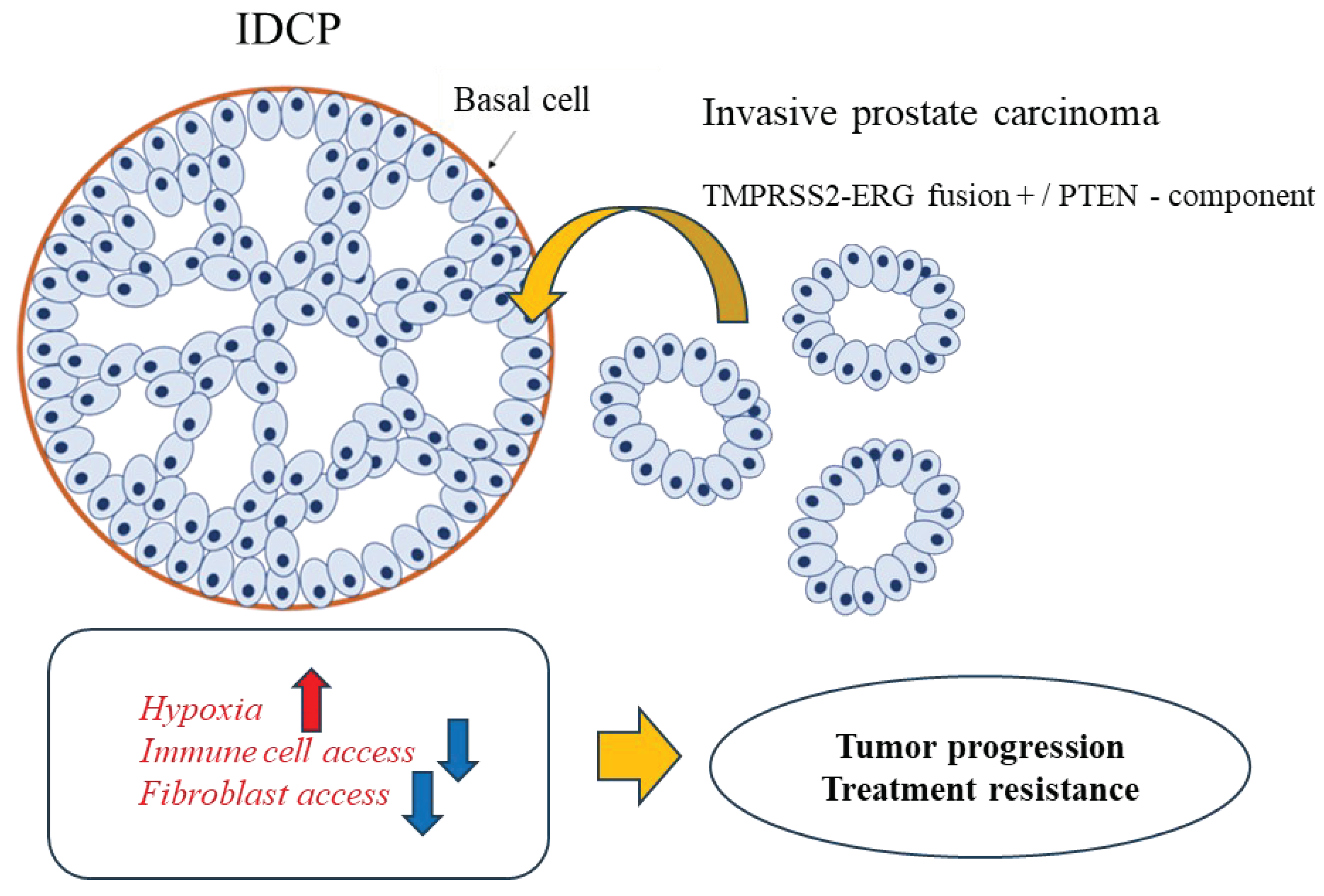
4. Discussion
5. Conclusion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- McNeal, J.E.; Yemoto, C.E.M. Spread of Adenocarcinoma Within Prostatic Ducts and Acini. Morphologic and clinical correlations. Am. J. Surg. Pathol. 1996, 20, 802–814. [Google Scholar] [CrossRef] [PubMed]
- Haffner, M.C.; Weier, C.; Xu, M.M.; Vaghasia, A.; Gürel, B.; Gümüşkaya, B.; Esopi, D.M.; Fedor, H.; Tan, H.; Kulac, I.; et al. Molecular evidence that invasive adenocarcinoma can mimic prostatic intraepithelial neoplasia (PIN) and intraductal carcinoma through retrograde glandular colonization. J. Pathol. 2015, 238, 31–41. [Google Scholar] [CrossRef] [PubMed]
- Tsuzuki, T. Intraductal carcinoma of the prostate: A comprehensive and updated review. Int. J. Urol. 2014, 22, 140–145. [Google Scholar] [CrossRef] [PubMed]
- Zhou, M. Intraductal carcinoma of the prostate: the whole story. Pathology 2013, 45, 533–539. [Google Scholar] [CrossRef] [PubMed]
- Varma, M.; Delahunt, B.; Egevad, L.; Samaratunga, H.; Kristiansen, G. Intraductal carcinoma of the prostate: a critical re-appraisal. Virchows Arch. 2019, 474, 525–534. [Google Scholar] [CrossRef] [PubMed]
- Miura, N.; Mori, K.; Mostafaei, H.; Quhal, F.; Motlagh, R.S.; Pradere, B.; Laukhtina, E.; D’andrea, D.; Saika, T.; Shariat, S.F. The Prognostic Impact of Intraductal Carcinoma of the Prostate: A Systematic Review and Meta-Analysis. J. Urol. 2020, 204, 909–917. [Google Scholar] [CrossRef]
- Kimura, K.; Tsuzuki, T.; Kato, M.; Saito, A.M.; Sassa, N.; Ishida, R.; Hirabayashi, H.; Yoshino, Y.; Hattori, R.; Gotoh, M. Prognostic value of intraductal carcinoma of the prostate in radical prostatectomy specimens. Prostate 2014, 74, 680–687. [Google Scholar] [CrossRef]
- Zhao, T.; Liao, B.; Yao, J.; Liu, J.; Huang, R.; Shen, P.; Peng, Z.; Gui, H.; Chen, X.; Zhang, P.; et al. Is there any prognostic impact of intraductal carcinoma of prostate in initial diagnosed aggressively metastatic prostate cancer? Prostate 2015, 75, 225–232. [Google Scholar] [CrossRef]
- Kato, M.; Tsuzuki, T.; Kimura, K.; Hirakawa, A.; Kinoshita, F.; Sassa, N.; Ishida, R.; Fukatsu, A.; Kimura, T.; Funahashi, Y.; et al. The presence of intraductal carcinoma of the prostate in needle biopsy is a significant prognostic factor for prostate cancer patients with distant metastasis at initial presentation. Mod. Pathol. 2016, 29, 166–173. [Google Scholar] [CrossRef]
- Epstein, J.I.; Egevad, L.; Amin, M.B.; Delahunt, B.; Srigley, J.R.; Humphrey, P.A. The 2014 International Society of Urological Pathology (ISUP) Consensus Conference on Gleason Grading of Prostatic Carcinoma: Definition of Grading Patterns and Proposal for a New Grading System. Am. J. Surg. Pathol. 2016, 40, 244–252. [Google Scholar] [CrossRef]
- Humphrey, P.A.; Moch, H.; Cubilla, A.L.; Ulbright, T.M.; Reuter, V.E. The 2016 WHO Classification of Tumours of the Urinary System and Male Genital Organs—Part B: Prostate and Bladder Tumours. Eur. Urol. 2016, 70, 106–119. [Google Scholar] [CrossRef] [PubMed]
- Network NCC NCCN clinical practice guidelines in oncology: prostate cancer, version 1. 2023.
- Han, B.; Suleman, K.; Wang, L.; Siddiqui, J.; Sercia, L.; Magi-Galluzzi, C.; Palanisamy, N.; Chinnaiyan, A.M.; Zhou, M.; Shah, R.B. ETS gene aberrations in atypical cribriform lesions of the prostate: implications for the distinction between intraductal carcinoma of the prostate and cribriform high-grade prostatic intraepithelial neoplasia. Am. J. Surg. Pathol. 2010, 34, 478–485. [Google Scholar] [CrossRef] [PubMed]
- Bettendorf, O.; Schmidt, H.; Staebler, A.; Grobholz, R.; Heinecke, A.; Boecker, W.; Hertle, L.; Semjonow, A. Chromosomal imbalances, loss of heterozygosity, and immunohistochemical expression of TP53, RB1, and PTEN in intraductal cancer, intraepithelial neoplasia, and invasive adenocarcinoma of the prostate. Genes, Chromosom. Cancer 2008, 47, 565–572. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Wang, Y.; Zhang, J.; Hu, Q.; Zhi, F.; Zhang, S.; Mao, D.; Zhang, Y.; Liang, H. Significance of the TMPRSS2:ERG gene fusion in prostate cancer. Mol. Med. Rep. 2017, 16, 5450–5458. [Google Scholar] [CrossRef]
- Shah, R.B.; Shore, K.T.; Yoon, J.; Mendrinos, S.; McKenney, J.K.; Tian, W. PTEN loss in prostatic adenocarcinoma correlates with specific adverse histologic features (intraductal carcinoma, cribriform Gleason pattern 4 and stromogenic carcinoma). Prostate 2019, 79, 1267–1273. [Google Scholar] [CrossRef]
- Risbridger, G.P.; Taylor, R.A.; Clouston, D.; Sliwinski, A.; Thorne, H.; Hunter, S.; Li, J.; Mitchell, G.; Murphy, D.; Frydenberg, M.; et al. Patient-derived Xenografts Reveal that Intraductal Carcinoma of the Prostate Is a Prominent Pathology in BRCA2 Mutation Carriers with Prostate Cancer and Correlates with Poor Prognosis. Eur. Urol. 2015, 67, 496–503. [Google Scholar] [CrossRef]
- Taylor, R.A.; Fraser, M.; Rebello, R.J.; Boutros, P.C.; Murphy, D.G.; Bristow, R.G.; Risbridger, G.P. The influence of BRCA2 mutation on localized prostate cancer. Nat. Rev. Urol. 2019, 16, 281–290. [Google Scholar] [CrossRef]
- Watanabe, R.; Miura, N.; Kurata, M.; Kitazawa, R.; Kikugawa, T.; Saika, T. Spatial Gene Expression Analysis Reveals Characteristic Gene Expression Patterns of De Novo Neuroendocrine Prostate Cancer Coexisting with Androgen Receptor Pathway Prostate Cancer. Int. J. Mol. Sci. 2023, 24, 8955. [Google Scholar] [CrossRef]
- Wong, H.Y.; Sheng, Q.; Hesterberg, A.B.; Croessmann, S.; Rios, B.L.; Giri, K.; Jackson, J.; Miranda, A.X.; Watkins, E.; Schaffer, K.R.; et al. Single cell analysis of cribriform prostate cancer reveals cell intrinsic and tumor microenvironmental pathways of aggressive disease. Nat. Commun. 2022, 13, 1–21. [Google Scholar] [CrossRef]
- Miyai, K.; Divatia, M.K.; Shen, S.S.; Miles, B.J.; Ayala, A.G.; Ro, J.Y. Heterogeneous clinicopathological features of intraductal carcinoma of the prostate: a comparison between "precursor-like" and "regular type" lesions. . 2014, 7, 2518–26. [Google Scholar]
- Guo, C.C.; I Epstein, J. Intraductal carcinoma of the prostate on needle biopsy: histologic features and clinical significance. Mod. Pathol. 2006, 19, 1528–1535. [Google Scholar] [CrossRef]
- Robinson, B.D.; Epstein, J.I.; J, Z.; J, L.; G, S.; M, Z.; J, C.; P, S.; Z, L.; B, L.; et al. Intraductal Carcinoma of the Prostate Without Invasive Carcinoma on Needle Biopsy: Emphasis on Radical Prostatectomy Findings. J. Urol. 2010, 184, 1328–1333. [Google Scholar] [CrossRef]
- Varma, M.; I Epstein, J. Head to head: should the intraductal component of invasive prostate cancer be graded? Histopathology 2020, 78, 231–239. [Google Scholar] [CrossRef]
- Zong, Y.; Montironi, R.; Massari, F.; Jiang, Z.; Lopez-Beltran, A.; Wheeler, T.M.; Scarpelli, M.; Santoni, M.; Cimadamore, A.; Cheng, L. Intraductal Carcinoma of the Prostate: Pathogenesis and Molecular Perspectives. Eur. Urol. Focus 2020, 7, 955–963. [Google Scholar] [CrossRef]
- Fulgione, C.; Raffone, A.; Travaglino, A.; Arciuolo, D.; Santoro, A.; Cianfrini, F.; Russo, D.; Varricchio, S.; Raimondo, I.; Inzani, F.; et al. Diagnostic accuracy of HIK1083 and MUC6 as immunohistochemical markers of endocervical gastric-type adenocarcinoma: A systematic review and meta-analysis. Pathol. - Res. Pr. 2023, 241, 154261. [Google Scholar] [CrossRef] [PubMed]
- Yamanoi, K.; Fujii, C.; Yuzuriha, H.; Kumazawa, M.; Shimoda, M.; Emoto, K.; Asamura, H.; Nakayama, J. MUC6 expression is a preferable prognostic marker for invasive mucinous adenocarcinoma of the lung. Histochem. 2022, 157, 671–684. [Google Scholar] [CrossRef] [PubMed]
- Lose, F.; Batra, J.; O'Mara, T.; Fahey, P.; Marquart, L.; Eeles, R.A.; Easton, D.F.; Al Olama, A.A.; Kote-Jarai, Z.; Guy, M.; et al. Common variation in Kallikrein genes KLK5, KLK6, KLK12, and KLK13 and risk of prostate cancer and tumor aggressiveness. Urol. Oncol. Semin. Orig. Investig. 2011, 31, 635–643. [Google Scholar] [CrossRef] [PubMed]
- Korbakis, D.; Soosaipillai, A.; Diamandis, E.P. Study of kallikrein-related peptidase 6 (KLK6) and its complex with α1-antitrypsin in biological fluids. cclm 2017, 55, 1385–1396. [Google Scholar] [CrossRef] [PubMed]
- Yamanoi, K.; Fujii, C.; Yuzuriha, H.; Kumazawa, M.; Shimoda, M.; Emoto, K.; Asamura, H.; Nakayama, J. MUC6 expression is a preferable prognostic marker for invasive mucinous adenocarcinoma of the lung. Histochem. 2022, 157, 671–684. [Google Scholar] [CrossRef]
- Ruscica, M.; Dozio, E.; Boghossian, S.; Bovo, G.; Riaño, V.M.; Motta, M.; Magni, P. Activation of the Y1 Receptor by Neuropeptide Y Regulates the Growth of Prostate Cancer Cells. Endocrinology 2006, 147, 1466–1473. [Google Scholar] [CrossRef]
- Sigorski, D.; Wesołowski, W.; Gruszecka, A.; Gulczyński, J.; Zieliński, P.; Misiukiewicz, S.; Kitlińska, J.; Iżycka-Świeszewska, E. Neuropeptide Y and its receptors in prostate cancer: associations with cancer invasiveness and perineural spread. J. Cancer Res. Clin. Oncol. 2022, 149, 5803–5822. [Google Scholar] [CrossRef]
- Ikeda, J.; Ohe, C.; Ohsugi, H.; Matsuda, T.; Tsuta, K.; Kinoshita, H. Association of intraductal carcinoma of the prostate detected by initial histological specimen and neuroendocrine prostate cancer: A report of three cases. Pathol. Int. 2021, 71, 621–626. [Google Scholar] [CrossRef] [PubMed]
- Naito, Y.; Kato, M.; Nagayama, J.; Sano, Y.; Matsuo, K.; Inoue, S.; Sano, T.; Ishida, S.; Matsukawa, Y.; Tsuzuki, T.; et al. Recent insights on the clinical, pathological, and molecular features of intraductal carcinoma of the prostate. Int. J. Urol. 2023. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, R.; Maekawa, M.; Hieda, M.; Taguchi, T.; Miura, N.; Kikugawa, T.; Saika, T.; Higashiyama, S. SPOP is essential for DNA–protein cross-link repair in prostate cancer cells: SPOP-dependent removal of topoisomerase 2A from the topoisomerase 2A-DNA cleavage complex. Mol. Biol. Cell 2020, 31, 478–490. [Google Scholar] [CrossRef]
- Hoang, K.N.L.; Anstee, J.E.; Arnold, J.N. The Diverse Roles of Heme Oxygenase-1 in Tumor Progression. Front. Immunol. 2021, 12, 658315. [Google Scholar] [CrossRef] [PubMed]
- Liu, T.; Zhou, L.; Li, D.; Andl, T.; Zhang, Y. Cancer-Associated Fibroblasts Build and Secure the Tumor Microenvironment. Front. Cell Dev. Biol. 2019, 7, 60. [Google Scholar] [CrossRef] [PubMed]
- Ren, J.; Smid, M.; Iaria, J.; Salvatori, D.C.F.; van Dam, H.; Zhu, H.J.; Martens, J.W.M.; Dijke, P.T. Cancer-associated fibroblast-derived Gremlin 1 promotes breast cancer progression. Breast Cancer Res. 2019, 21, 1–19. [Google Scholar] [CrossRef] [PubMed]
- de Hosson, L.D.; Takkenkamp, T.J.; Kats-Ugurlu, G.; Bouma, G.; Bulthuis, M.; de Vries, E.G.E.; van Faassen, M.; Kema, I.P.; Walenkamp, A.M.E. Neuroendocrine tumours and their microenvironment. Cancer Immunol. Immunother. 2020, 69, 1449–1459. [Google Scholar] [CrossRef]
- Kobayashi, H.; Enomoto, A.; Woods, S.L.; Burt, A.D.; Takahashi, M.; Worthley, D.L. Cancer-associated fibroblasts in gastrointestinal cancer. Nat. Rev. Gastroenterol. Hepatol. 2019, 16, 282–295. [Google Scholar] [CrossRef]
- Séguier, D.; Adams, E.S.; Kotamarti, S.; D’anniballe, V.; Michael, Z.D.; Deivasigamani, S.; Olivier, J.; Villers, A.; Hoimes, C.; Polascik, T.J. Intratumoural immunotherapy plus focal thermal ablation for localized prostate cancer. Nat. Rev. Urol. 2023. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).




