1. Introduction
Full-arch implant-supported rehabilitation is a wide-spread and predictable rehabilitation for edentulous patients or patients with hopeless dentition. This treatment modality is often associated with immediate implant loading which showed optimal clinical outcomes and high patients’ satisfaction [
1,
2,
3,
4,
5,
6,
7].
The majority of the protocols (including the All-on-4 and the Columbus Bridge Protocol) require the insertion of a reduced implant number (4-6 implants) that are considered sufficient as long as two key factors are respected: primary stability and occlusal load control in order to avoid the risk of implant micromotion [
3].
Overloading might represent a risk factor for implant survival especially in immediate loading protocols, where implants are loaded before the achievement of osseointegration. However, even once osseointegration is achieved, overloading might increase the risk of peri-implant bone resorption and technical complications [
8,
9,
10].
One of the factors that helps the control of occlusal loads is considered the rigid splinting of the implants with a passive fitting prosthodontic substructure which prevents micro-movements and optimizes the distribution of loads between the implants, reducing the risk of overload [
11]. Hasan et al. conducted a 3D-FEA simulation to compare splinted and non-splinted implants. The results suggested a positive effect on load transmission by splinting the implants, with a reduction of stress levels both on the implant system (up to 64%) and on peri-implant bone (up to 36%).
With isotropic material the elastic modulus of the material which the framework is made of can influence the stress levels transmitted to the implant system and peri-implant bone. The materials traditionally most used for implant-supported substructures are metal alloys that offer sufficient rigidity even in situations where the prosthetic space is reduced. In fact, the advantages include the ability to make implant-supported full-arch prostheses with more natural aesthetics, avoiding reconstruction of gingival tissues in pink acrylic resin or other materials in case of low prosthodontic volume.
Titanium and its alloys and zirconia are also commonly used materials for the fabrication of frameworks with CAD-CAM techniques [
12,
13,
14].
The in vitro study by Ogawa et al. [
8] compared implant-supported fixed prostheses made of three different materials: acrylic resin, glass fiber-reinforced acrylic resin, and titanium. Under stating loading, maximum bending moments were significantly lower for the titanium framework compared to the full-acrylic and the glass fiber reinforced prosthesis. The higher stiffness of titanium led to a smaller deformation of the prosthesis, thereby resulting in a better distribution of occlusal forces among the supporting implants. This might also reduce the risk of fatigue and possible failures due to overloading of the implant prosthodontic components.
A sufficient stiffness of the prosthesis might be particularly important when a reduced number of implants is used in full-arch rehabilitations since long span prosthesis should be expected and subjected to flexure.
Indeed with anisotropic composite materials such as carbon fiber reinforced composites (CFRCs), the final stiffness of the device is due not only by the fiber modulus but also by the fiber/tow orientation and by the geometry of the artifact. This is a direct consequence of adopting anisotropic materials like CFRC instead of isotropic and usually homogeneous materials like metals. The direction of the fibers as well as the applied patterns are therefore fundamental to determine the final mechanical properties of the device when dealing with FRC composite materials.
The 3D-finite element analysis by Tribst et al. [
15] simulated the all-on-4 rehabilitation with different framework materials: cobalt chromium, zirconia and polyetheretherketone (PEEK). In contrast with the PEEK framework, zirconia and cobalt chromium concentrated stresses in the framework structure, reducing the stress transmitted to the prosthetic screws and dental implants.
The production of metal frameworks for fixed implant-supported prostheses involves high costs and long processing times. In addition, the poor adhesive affinity between acrylic resin and metal is often the cause of detachment of the tooth veneer from the underlying frameworks (chipping). This disadvantage is easily solved but represents an inconvenience for the patient.
In order to reduce costs without sacrificing clinical advantages, the search for alternative materials is always growing.
Zirconia is commonly used, but, besides the high costs, several authors consider its rigidity excessive and possible cause of increased technical and biological complications in implant-supported rehabilitations, especially in case of full-arch immediate loading rehabilitations [
16,
17,
18,
19,
20].
Fiber-reinforced composites (FRCs) are anistropic composite materials that could conveniently be bio-applied dynamic strength and fracture resistance are desired especially in relation to weight [
21]. The advantages of FRCs compared to traditional metal alloys and zirconia include: reduced costs, easy of repair, possibility of both analogic or CAD-CAM fabrication technique, light weight, adhesion to composite resin veneering material, shock absorption capacity [
22]. The main disadvantages are related in prosthodontic applications to possible interaction of the polymer matrix with body fluids and abrasion in the oral cavity.
A three dimensional finite element analysis (3D-FEA) by Menini et al. [
23] compared loading stresses in an implant-supported full-arch fixed prosthesis without framework (full-acrylic) and with metallic and CFRC frameworks. The highest stresses at implant level were found in the full-acrylic prosthesis, the lowest in the prosthesis with a metallic framework, and intermediate values were found in the prosthesis with a CFRC framework.
The possibility of optimal adhesion to polymeric veneering materials, such as resin veneering, is considered a further advantage of FRC frameworks [
24].
In fact, in implant-supported rehabilitations the shock absorption capacity (and proprioceptive capacity) of the periodontal ligament is missing and the dampening effect of an elastic veneering material (such as the polymer matrix of a composite material) is considered advantageous by several authors coupled with the splinting effect of a more rigid framework [
17,
25].
FRCs consist of fibers embedded in a polymer matrix. The polymer matrix represents the weak phase but allows a firm adhesive bond between the fibers and protection from the possible damaging effects of chemical agents or mechanical trauma, forming a barrier against environmental conditions. It also allows for optimal finishing of the prosthesis surface.
Fibers are the strongest phase and can be continuous or discontinuous.
The mechanical properties of the final FRC devices can vary greatly depending on the arrangement of the fibers, type of fiber, the quantity of fibers [
26], the type of matrix, the quality of their bonding to the matrix, the fabrication technique used, and the skill of the fabricator, therefore appropriate and specific training is strongly recommended[
27,
28].
The tensile strength and elastic modulus of a unidirectionally oriented fiber-reinforced polymer will be lowest when these properties are measured at 90° to the longitudinal direction of the fibers, while they will be highest when measured in the longitudinal direction of the fibers [
29].
A multi-directional arrangement of the fibers allows the distribution of properties over multiple dimensions. Most likely, when the “woven” configuration is adopted, mechanical properties are decreased compared to the longitudinal properties of unidirectionally oriented composites, and in any case it must be considered that it works on the 2d configuration.
The study by Pesce et al. [
30] investigated the mechanical properties of carbon fiber-reinforced composite frameworks by comparing unidirectional and multidirectional fibers. Following destructive and nondestructive mechanical tests to evaluate static and dynamic elastic modulus, it was revealed that composites with unidirectional carbon fibers are suitable for the fabrication of frameworks for full-arch implant-supported rehabilitations, with a higher dynamic elastic modulus than that of composites with multidirectional carbon fibers, which instead presented higher static elastic modulus. This is a consequence of the specific features of the dynamic vs static tests [
30] .
Most FRCs used in dental applications are fabricated with glass fibers for aesthetic reasons (in contrast with black carbon fibers) and for their surface chemistry, which improves their adhesion to the polymer matrix [
31]. The application of glass fiber-reinforced composites ranges from the fabrication of endodontic posts to implant prosthodontics using both analogic or CAD/CAM techniques [
32]. Great attention has to be payed to the fact that meanwhile CFRC are anisotropic in their mechanical/thermal response, the most commonly adopted GFRC in dental applications are constituted of short fibers randomly dispersed into the supporting polymer matrix and this changes dramatically the overall attended mechanical performances.
Nakamura et al. [
33] examined flexural strength and elastic modulus of three glass fiber-reinforced composites for framework fabrication compared to three veneer composites. The values recorded for framework composites were three times higher than those of veneer composites.
FRC bridges with glass fibers can become an alternative to restorations with metal frameworks. Some studies demonstrate high fracture toughness with reliable marginal fit after thermal cycling and mechanical loading [
34].
However, the application of FRCs in the implant-prosthodontic field has not yet been sufficiently investigated by the Literature and needs further studies.
The purpose of the present in vitro study was to compare the mechanical characteristics of seven implant-supported full-arch prostheses made with framework and veneer of different materials through flexural tests. In particular, the flexion of the different prostheses was measured when a vertical load was applied.
2. Materials and Methods
The samples of this study consist of 12-unit screw-retained upper full-arch fixed prostheses supported by 4 implants at the two lateral incisors and the two first molars.
All the prostheses have the same shape and size and were fabricated from one single extra-hard plaster model of the upper maxilla (
Figure 1), that included the analogs of 4 angled abutments (Biomet 3i, PalmBeach Gardens, FL) with a 4 mm diameter and a 17° inclination at the level of the lateral incisors and a 30° inclination at the level of the first molars, to form an optimal polygonal support. The distance between the implants at the lateral incisor sites was 19.4 mm. The distance between the lateral incisor and the first premolar was 27.6 mm on the left side and 26.0 mm on the right side.
The materials used to fabricate the seven samples examined in this study were (framework material + veneering material):
Gold alloy framework + resin veneering (Au+R)
Titanium framework + resin veneering (Ti+R)
CFRC with braided fibers framework + resin veneering (ICFRC+AR)
CFRC with unidirectional fibers framework + composite resin veneering (UCFRC+C)
FRC with glass fibers framework + resin veneering (GFRC+AR)
FRC with glass fibers framework +composite resin veneering (GFRC+C)
Acrylic resin (full-acrylic prosthesis) (R)
Due to an overlapping between composite material science and dental terminology, it must be specified that here as “resin” it has not to be intended the polymer matrix that embedds the fibers of the composite material, but the aesthetic material that is supported by the supporting core (framework); similarly “composite” intends common dental composite resin with inorganic filler, usually applied for the realization of fixed prostheses.
Table 1 reports the dental materials examined (Tab 1). It must be noted that the value given for CFRCs is the elastic modulus of the fibers, while for FRCs with glass fibers it is of the final composite.
The guidelines of the respective materials manufacturers were followed for the fabrication of the frameworks and prostheses. Muffle molding or scanning and milling (depending on the materials used) ensured identical shape of all the prostheses to be tested.
The gold alloy (Ney-Oro CB, Dentsply Int, York, PA) framework was the first to be fabricated. It was made by lost-wax casting technique, followed by passivation technique luting the titanium prosthetic cylinders (Biomet 3i) using an anaerobic composite luting agent BeautiCem SA (SHOFU) [
27,
28]. Sandblasting with aluminum oxide (250 µm), and subsequent application of opaquer (SR Ivocron Opaquer Liquid) with firing at 100 °C at 6 atm pressure for 10 minutes was implemented.
The veneer was made of acrylic resin (SR Ivocron, Ivoclar Vivadent, Schaan, Liechtenstein) by clear muffle molding and firing at 120 °C at 6 atm for 15 minutes and finishing.
For the titanium framework (F.A.B.O.), laser welding of the preformed titanium bars to the titanium cylinders and microcharacterization of the framework was performed [
25]. The same surface treatment and the same veneering described above for the gold alloy framework was performed.
The composite materials devices were fabricated following the standard procedures recommended by the manufacturers for dental labs. This strategy was set up in order not to go for highly specialized engineering supported labs, certainly able to provide the state-of-the-art performances by the viewpoint of the Composite Theory but indeed far from the experience of the dental community.
To fabricate the CFRC framework made of multidirectional carbon fibers, in the fashion of sheets layers of woven carbon fibers, not pre-impregnated laminae (Dream frame, DEI Italia s.r.l.) were cut out in a horseshoe shape and soaked with Dream Frame Bio Resin plant-derived epoxy resin (DEI Italia s.r.l.). Fifteen Carbon fiber sheets were superimposed and arranged parallel to the occlusal plane to form the framework in a muffle furnace. The countermold was applied to the model, passing the cylinders between the sheet meshes.
Mold firing was performed under vacuum and under pressure, at 6 atm, at 120 °C for 90 minutes.
Then a primer (visio.link PMMA & Composite Primer) was applied followed by opaquing with SR Ivocron Opaquer Liquid, and firing at 100 °C at 6 atm pressure for 10 minutes.
The veneer was made of resin (SR Ivocron, Ivoclar Vivadent AG) by clear muffle molding and firing at 120 °C at 6 atm for 15 minutes and finishing.
Unidirectional carbon fibers (Bio Carbon Bridge Wires, Micro.Medica s.r.l.) were uniformly impregnated with Bio Carbon Bridge resin (Micro.Medica s.r.l.) and arranged along the entire length of the framework. The countermold was applied to the model, passing the cylinders between the fibers. Mold firing, under vacuum and under pressure, 6 atm, at 120 °C for 90 minutes. This was followed by application of primer (visio.link PMMA & Composite Primer) and opaquer (SR Ivocron Opaquer Liquid) fired at 100 °C at 6 atm pressure for 10 minutes.
The veneer was made of composite (SR Nexco Paste, Ivoclar Vivadent AG): a layer of primer was placed first, followed by light-curing in a transparent muffle furnace, with Xenon Lamp Cure System (TOESCO) for 20 minutes and finishing.
For the glass fibers-reinforced composite (GFRC) framework, preformed Trilor arches (Bioloren S.r.l.), constituted of woven glass fibers in an epossidic resin, were milled by CAD/CAM technique. As reported by the manufacturer, Trilor arches present the following mechanical characteristics: density: 1.8 g/cm³; flexural strength: 540 MPa; tensile strength: 380 MPa. Two milled frameworks were realized and luted to the titanium cylinders (Biomet 3i).
Being whitish in color, no opaque is necessary and only priming is required to promote adhesion of the veneer.
One GFRC framework was veneered with composite resin (SR Nexco Paste, Ivoclar Vivadent AG), light-cured in transparent muffle molding with Xenon Lamp Cure System TOESCO for 20 minutes and finished.
The other was veneered with acrylic resin (SR Ivocron, Ivoclar Vivadent AG), clear muffle molded and fired at 120 °C, at 6 atm for 15 minutes and then finished.
All the mechanical tests were performed at the Department of Civil, Chemical and Environmental Engineering (DICCA) of the University of Genoa.
Fiber composites are not isotropic materials. As a consequence, the mechanical properties of these materials are extremely variable when measured in different directions. This characteristic can be observed either on the microscale, that is at the fiber level, and on the macroscale, that is the final product. Thus the final characteristics of the composite will be influenced by the total fiber percentage, their orientation and by the geometrical arrangement of the layers adopted to create the samples. Due to the experimental nature of these preliminary tests and the specific shapes of implant-supported prostheses, no specific testing protocols or regulatory indications were applied at this stage of the investigation herein described, in order to test prostheses realized as in ordinary clinical practice.
All the samples were measured with a caliper to verify that their dimension could be considered identical and weighed with Exacta Optech precision scales (1000 g full scale, 0.001 g resolution) before compression testing began.
The prostheses were subjected to compression tests using the Zwick/Roell Z 0.5 single-column electromechanical machine with a maximum load of 500 N and 0.1% accuracy.
Before starting the tests, the prostheses were mechanically screwed onto the plaster model using GoldTite retention screws (Biomet 3i) at a torque of 10 N as recommended by the manufacturer with a torque instrument (Contra-Angle Torque Driver, Biomet 3i).
Each prosthesis was loaded in 3 different areas at successive times:
at the first right premolar (that is equidistant between the retention screw at the lateral incisor level and the one at the first molar level)
at the first left premolar (that is equidistant between the retention screw at the lateral incisor level and the one at the first molar level)
between the two central incisors (at the interincisal line)
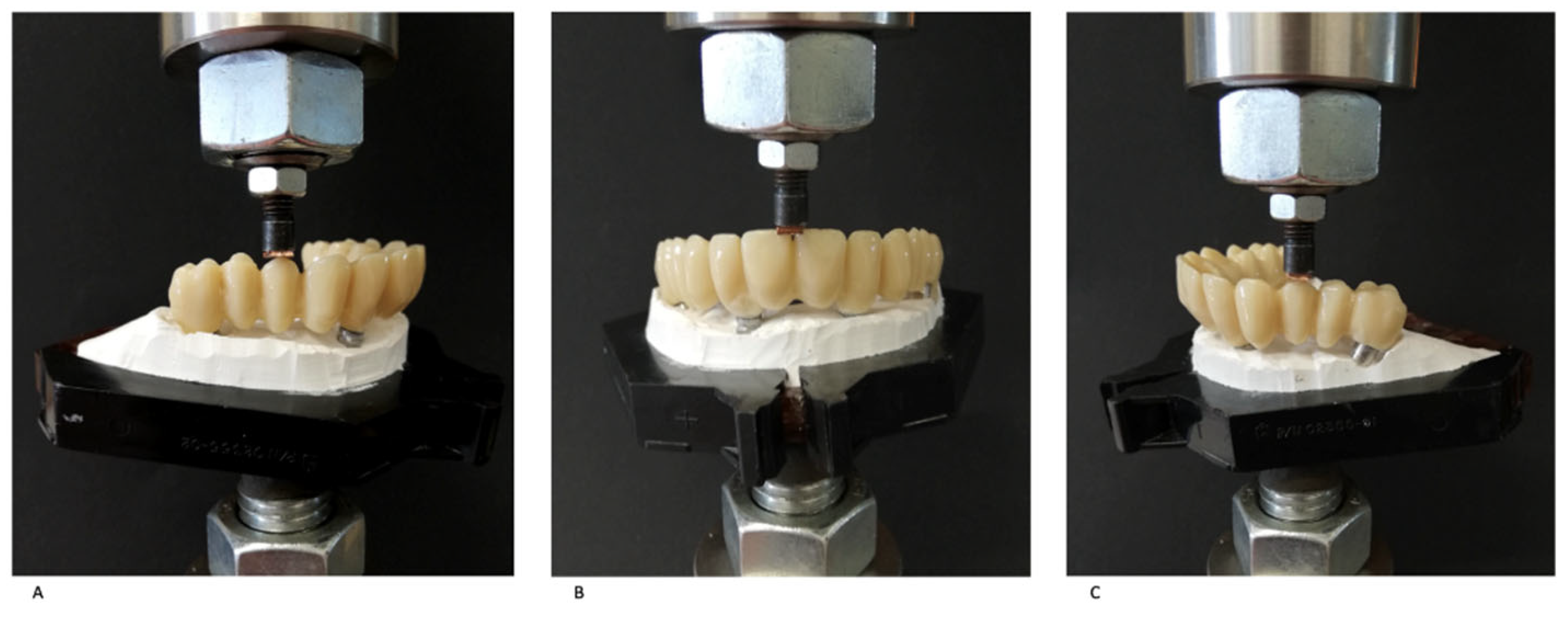
The purpose of the study was to evaluate the deflexion of the prostheses, measured by using a flexural extensometer applyied to the lower surface of the sample, following the application of a vertical load (
Figure 2). The overall experimental set-up was created in order to test the specific samples herein described (as per clinical-use prostheses).
A 6-mm-diameter cylindrical punch was screwed to the upper load cell to transmit the vertical load (perpendicular to the occlusal plane) by descending onto the prosthesis.
At the sites described above, the three following loading conditions were sequentially applied (
Figure 2):
increasing load up to 100 N at a speed of 8 mm/min
increasing load up to 200 N at a speed of 16 mm/min
increasing load up to 300 N (for premolar sites) or up to 260 N (for the interincisive site) at 16 mm/min
The values of 100 N and 200 N were chosen to simulate a typical masticatory load generated during the routine mastication of softer and stiffer food. The forces of 300 N and 260 N corresponded instead at an extimate of the bite force of the posterior region (pre-molar) and of the anterior segment (intercanine) respectively [
35].
To ensure uniform load distribution on the surface where the load was applied by the cylindrical punch, due to the irregularity of the aesthetic surface, a thin copper foil with a surface area of 4 mm², thickness 1 mm, was interposed between the punch and the prosthesis while applying an increasing load up to 100 N and up to 200 N. On the other hand, when a maximum load of 300 N was applied, a lead foil of the same size was used to avoid damaging the aesthetic coating.
During increasing loading application, the deflexion of the intaglio surface of the prostheses was measured.
The tests were repeated 3 times on all the sites examined at all the loading conditions and before carrying out the final tests, which are reported in this study, several load cycles were made, at the value of the final load, to allow the metal plate of copper or lead, to deform plastically adapting to the profile of the aesthetic part.
3. Results
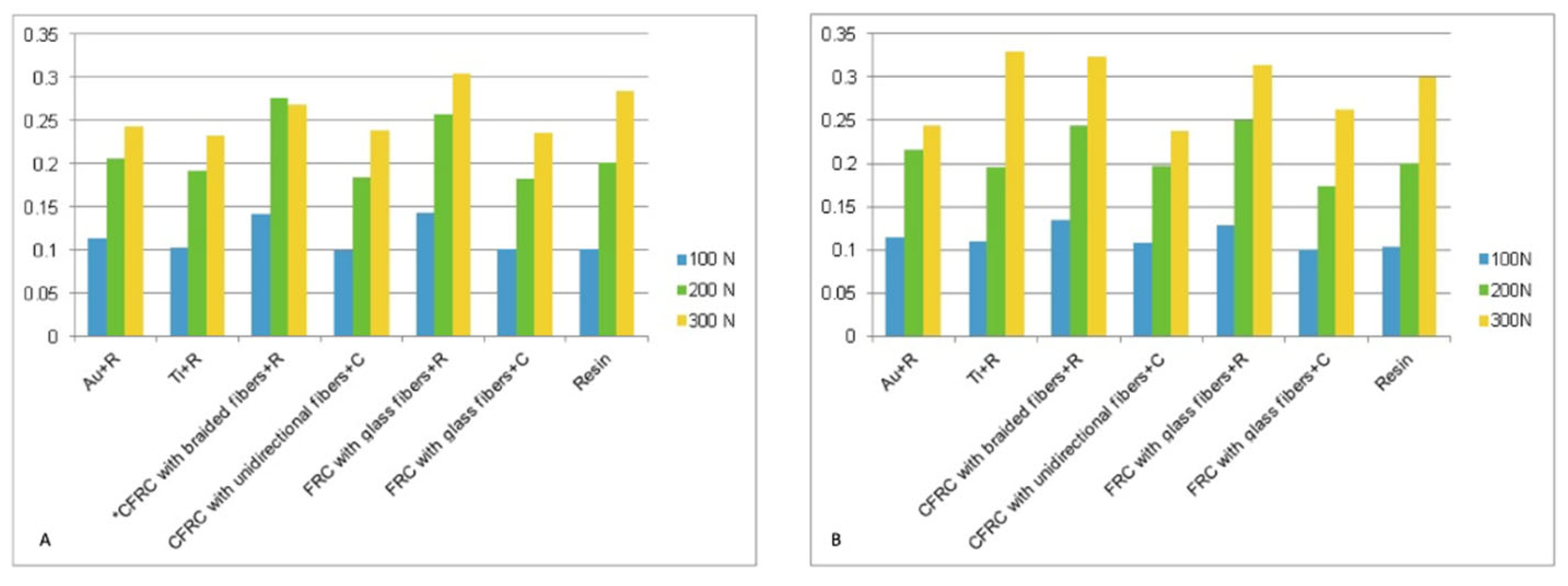
Table 2 reports the weight of the samples and deflection values of the prostheses (mm) during different load application on the first left premolar, right premolar and interincisal line.
No chipping nor fractures of the prostheses occurred during the test.
Compression tests at the level of the right and left first premolars yielded comparable data regarding the mechanical behavior of the prosthesis tested.
Table 2 and
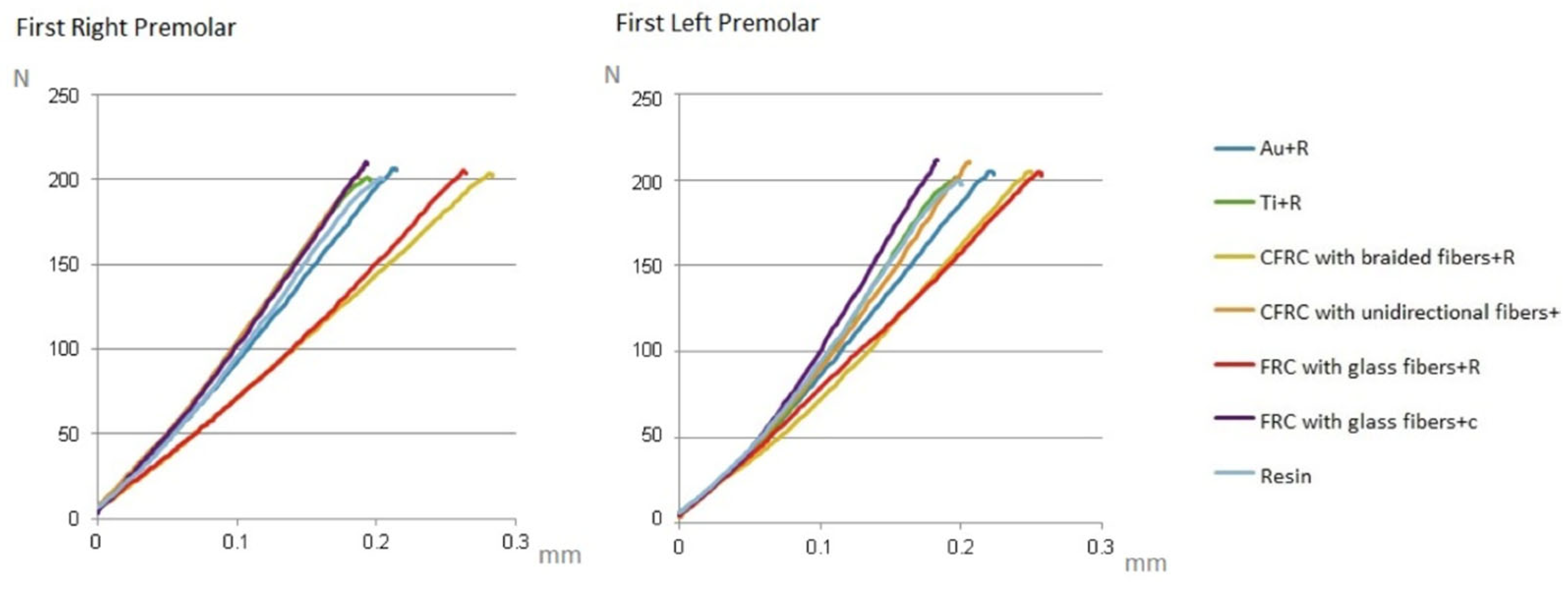
Figure 3 report the deflaction values (mm) of the prostheses collected in the 3 successive tests (with maximum load at 100, 200 and 300 N) at the level of the right first premolar and at the level of the left first premolar. On the base of the data collected the load/deflection graphs were obtained (
Figure 4).
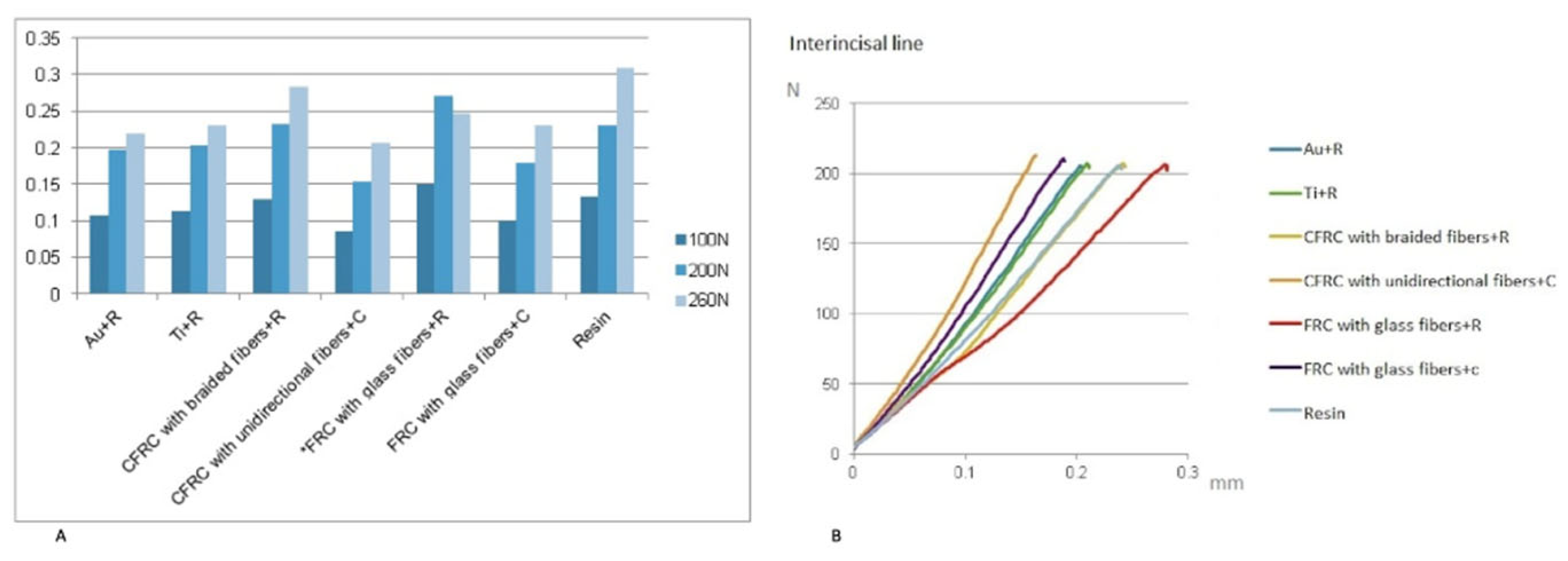
Table 2 and
Figure 5 reports the deflection values of the prostheses (mm) during load application at the interincisal line.
4. Discussion
Fiber-reinforced composites (FRCs), differently fashioned in long as well as short fibers and in woven or not-woven configurations, have been proposed as an alternative to traditional metal alloys for the realization of frameworks in full-arch implant supported prostheses. The overall performances of these composites materials are definitely different but both are applied in dentistry and this pushed us to evaluate their performances.
Gold alloy is the metal that is traditionally used for dentures and bridges, and its properties are proven by long years of use. It is extremely compatible for this type of application, and its mechanical behavior is taken as a reference for evaluating the behavior of other alternative materials [
36,
37].
The traditional gold alloy+resin prosthesis was considered the gold standard in full-arch implant-supported prosthesis since the metal framework provides strength and rigidly splint implants, while the resinous veneering materials provides shock absorption of occlusal loads for optimal loads control [
17,
25].
In the present investigation, the gold alloy+resin prosthesis showed a gradual increase of the deflection as the load increased up to 200 N, while at the maximum load of 300 N it showed a progressive reduction of the deflection gradient as a consequence of an increase in the stiffness. No plastic behavior was observed.
Disadvantages of this material include its high cost and relatively time-consuming and complex fabrication technique (need for casting and passivation technique by luting the titanium cylinders). The latter feature in particular is disadvantageous when immediate loading of implants is desired and it is necessary to realize the prosthesis in a short span of time. For these reasons CAD-CAM techniques are preferred nowadays.
In addition, the prosthesis with the gold alloy framework showed the highest weight among those analyzed, and this represents a further disadvantage in terms of patient comfort.
Frameworks made of CFRC have been presented as a cheaper alternative to metal alloy frameworks [
31,
38,
39]. In addition to being less expensive, they are easier to manufacture (they do not require casting and special passivation techniques), are lighter, allow better adhesion of the veneering material (reducing chipping), and do not require special machinery and tools for their fabrication using analogic techniques. As an alternative, disks are available to be milled applying CAD-CAM technology.
In a clinical investigation, full-arch prostheses on immediately loaded implants with CFRC frameworks demonstrated less implant failure and significantly less peri-implant bone resorption than full-arch prostheses with metal alloy frameworks [
40].
On the other hand, the mechanical properties of this material are operator-dependent and vary considerably depending on the fabrication protocol, material nature, laminate pattern set up, optimum wetting performances between fiber and polymer matrix, lab pollution, trapped air bubbles, and the skill of the technician in implementing it; therefore, it is desirable to determine a strict fabrication protocol accompanied by adequate and specific training of the dental technician [
28].
While the elastic modulus of isotropic materials from which the framework is made can influences the stress levels transmitted to the implant system and peri-implant bone, in case of multilayer composites, either unidirectional, multidirectional and even woven materials, the overall distribution pattern is indeed the most important parameter to determine the mechanical behavior under load. This is clinically relevant since in multiunit prostheses, a deflection of the prosthesis might lead to noxious loads at the abutments, and overloading of the implants supporting the prosthesis.
In the present investigation, the multidirection-fiber-CFRC+resin prosthesis showed a stiff behavior but with greater deflection gradient up to the 200 N load, while at the 300 N load (on dental element 24) an increase in stiffness was observed, presumably due to possible "settling" of the braided fibers, but with still greater deformations than the ones observed in the gold alloy prosthesis.
These results are compatible with previous studies: the study by Menini et al. [
41] tested prostheses with gold alloy frameworks and prostheses with CFRC frameworks with woven fibers by applying a vertical load identical to that reproduced in this research. The final values demonstrated that the two prostheses had similar behavior and that the least deformation was with the gold alloy framework. However, while the prosthesis with CFRC framework had an elastic behavior, recovering its original shape upon removal of the load, the gold+resin prosthesis showed a slight plastic deformation at the end of the load test (maximum load applied: 300 N). In contrast, this phenomenon was not found in the series of tests performed in the present study, where both specimens showed an elastic behavior with full recovery of the sample original shape once the load was removed. All these results are indeed due to the specific number and orientation set of the muldirectional layers that have been adopted in the present study. Any change in the laminae total number and orientation parameter may drive to sensible different conclusions.
The prosthesis with unidirectional fiber CFRC+composite showed lower deformation than the metal alloy and woven CFRC up to the load of 200 N, with further decrease at 300 N.
This result confirms the observation described in the study by Pesce et al. [
30] that supports the mechanical advantage of the unidirectional fiber CFRC, due to the possibility of realizing frameworks with longer whole fibers. In fact, common protocols for making an artifact of a complex shape, such as a full-arch framework, involve cutting out fabrics of pre-interwoven fibers that will then be overlaid. As a result, the fibers in the framework will be shorter.
Instead, the unidirectional fibers can be directly arranged to fit the shape of the framework, which is then traversed along its entire length by whole fibers.
The unidirectional-fiber CFRC prosthesis weighs slightly more than the multidirectional-fiber CFRC prosthesis, and together they are the lightest prostheses after the full-acrylic prosthesis.
In contrast, the titanium prosthesis is slightly heavier than the unidirectional-fiber CFRC prosthesis.
Resin-only and titanium+resin prosthesis presented intermediate behavior between unidirectional fiber CFRC and gold alloy: they exhibit less deflection than the latter up to the 200 N load. When loading at 300 N an increase in stiffness was observed for titanium (on dental element 14) while, differently to the other materials, this phenomenon did not occur in the resin, that presented an increase in strain gradient.
Some materials, such as resin, at low load (100 N) exhibited less ductility than others, such as metal alloy, while at higher values of load (200-300 N) the situation was reversed. This can be attributed to the nonlinearity of elastic deformation that occurs especially for polymeric materials (such as resin) in some specific loading procedures highly dependant upon temperature and testing speed: as the load increases, they progressively reduce the resistance to deformation while remaining in the elastic range.
In addition, the presence of acrylic resin coating instead of composite resin veneering material may have slightly influenced the deformation values of the prosthesis with titanium framework.
The FRC prosthesis with glass fibers+resin veneering showed a behavior close to that of woven-fiber CFRC up to the load of 200 N. At the load of 300 N there was an increase in stiffness. This is due to the less anisotropic behaviour of woven based CFRC.
In contrast, the FRC prosthesis with glass fiber+composite recorded higher stiffness up to the load of 200 N, with a curve load vs. deflection that remained close to that of unidirectional fiber CFRCs and of titanium. At 300 N (at site 14) there was an increase in stiffness.
The results in the incisal region were slightly different because the framework was thinner in this area and there was a different ratio of framework to veneering material, which was more represented than in the premolar region.
The prostheses with the least deflection at the 200 N load were those made of CFRC with unidirectional fibers+composite and FRC with glass fibers+composite, followed by gold alloy+resin and titanium+resin.
The greatest deformations occurred for resin alone, CFRC with woven fibers+resin and FRC with glass fibers+resin.
At the load of 300 N there was an increase in stiffness and thus less deformation only by the gold+resin alloy and titanium+resin.
The results of the present research confirm the usefulness of using a rigid substructure in full-arch prostheses. The resin-only prosthesis, in fact, showed high deformation values that might be detrimental, especially in immediate loading rehabilitations, since bending moments would be increased at the implants. Sufficient rigidity of a full-acrylic prosthesis would require greater thicknesses than those simulated in this research. Sufficient prosthetic volume may be present in case of severe bone atrophy, or it is achieved by invasive osteoplastic surgery, such as in the All-on-4 technique where the immediately loaded prosthesis is resin-only [
42].
The full-acrylic prosthesis also has aesthetic disadvantages. In fact, having greater thickness it will necessarily include a pink resin part to reproduce the soft tissues (Toronto bridge type or “hybrid” prosthesis) [
43], moving away from the "Natural bridge" type prosthesis simulated in the present research that best reproduces the patient's natural smile. In our study we assessed prosthesis under clinical use conditions, prioritizing analysis on real devices rather than simplified samples, aiming for more accurate and meaningful evaluations.
It must be remembered that many factors must be taken into consideration when choosing the prosthetic material in a specific clinical case. Besides the mechanical aspects investigated in the present research, also esthetic needs, extent of occlusal load (e.g., possible parafunctions), type of antagonist, prosthetic space, prosthesis design, biocompatibility, cost, time required for processing, and durability are among the aspects to be considered.
5. Conclusions
In conclusion, the present mechanical investigation demonstrated that fiber-reinforced composites can be a viable alternative to metal alloys for the fabrication of frameworks for full-arch implant-supported prostheses, presenting additional advantages such as lower cost, easy of repair and lower weight.
Frameworks made of unidirectional fibers CFRC demonstrated lower deflexion under load compared to woven CFRC.
As for glass fiber reinforced composite, further studies are needed in order to investigate their mechanical properties in implant-supported prostheses, in relation to the prosthesis thickness.
Resin alone, in the thicknesses simulated in the present research, does not provide a sufficiently rigid structure to ensure sufficient strength and rigidity for full-arch implant-supported rehabilitations.
Author Contributions
Conceptualization, M.M. and L.D.G; methodology, F.B.; software, A.L.; formal analysis, F.B.; investigation, P.P.; resources, F.P.; data curation, L.D.G.; writing—original draft preparation, L.D.G. and P.P.; writing—review and editing, L.C.; All authors have read and agreed to the published version of the manuscript.” Please turn to the CRediT taxonomy for the term explanation. Authorship must be limited to those who have contributed substantially to the work reported.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data available on request.
Acknowledgments
The authors wish to thank the technician Paolo Cirillo and dental technician Alessandro Manca for their support for the present research. The fiber reinforced materials used in the present research were provided for free by the respective manufacturers (Bioloren, Micromedica, DEIItalia).
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Tealdo, T.; Menini, M.; Bevilacqua, M.; Pera, F.; Pesce, P.; Signori, A.; Pera, P. Immediate versus delayed loading of dental implants in edentulous patients' maxillae: a 6-year prospective study. Int J Prosthodont 2014, 27, 207-214. [CrossRef]
- Pera, P.; Menini, M.; Bevilacqua, M.; Pesce, P.; Pera, F.; Signori, A.; Tealdo, T. Factors affecting the outcome in the immediate loading rehabilitation of the maxilla: a 6-year prospective study. Int J Periodontics Restorative Dent 2014, 34, 657-665. [CrossRef]
- Pera, P.; Menini, M.; Pesce, P.; Bevilacqua, M.; Pera, F.; Tealdo, T. Immediate Versus Delayed Loading of Dental Implants Supporting Fixed Full-Arch Maxillary Prostheses: A 10-year Follow-up Report. Int J Prosthodont 2019, 32, 27-31. [CrossRef]
- Tsigarida, A.; Chochlidakis, K. A Comparison Between Fixed and Removable Mandibular Implant-Supported Full-Arch Prostheses: An Overview of Systematic Reviews. Int J Prosthodont 2021, 34, s85-s92. [CrossRef]
- Del Fabbro, M.; Pozzi, A.; Romeo, D.; de Araujo Nobre, M.; Agliardi, E. Outcomes of Fixed Full-Arch Rehabilitations Supported by Tilted and Axially Placed Implants: A Systematic Review and Meta-Analysis. Int J Oral Maxillofac Implants 2022, 37, 1003-1025. [CrossRef]
- Dellepiane, E.; Pera, F.; Zunino, P.; Mugno, M.G.; Pesce, P.; Menini, M. Oral Health-Related Quality of Life and Full-Arch Immediate Loading Rehabilitation: An Evaluation of Preoperative, Intermediate, and Posttreatment Assessments of Patients Using a Modification of the OHIP Questionnaire. J Oral Implantol 2020, 46, 540-549. [CrossRef]
- Goncalves, G.S.Y.; de Magalhaes, K.M.F.; Rocha, E.P.; Dos Santos, P.H.; Assuncao, W.G. Oral health-related quality of life and satisfaction in edentulous patients rehabilitated with implant-supported full dentures all-on-four concept: a systematic review. Clin Oral Investig 2022, 26, 83-94. [CrossRef]
- Ogawa, T.; Dhaliwal, S.; Naert, I.; Mine, A.; Kronstrom, M.; Sasaki, K.; Duyck, J. Impact of implant number, distribution and prosthesis material on loading on implants supporting fixed prostheses. J Oral Rehabil 2010, 37, 525-531. [CrossRef]
- Pjetursson, B.E.; Sailer, I.; Zwahlen, M.; Hammerle, C.H. A systematic review of the survival and complication rates of all-ceramic and metal-ceramic reconstructions after an observation period of at least 3 years. Part I: Single crowns. Clin Oral Implants Res 2007, 18 Suppl 3, 73-85. [CrossRef]
- Sailer, I.; Pjetursson, B.E.; Zwahlen, M.; Hammerle, C.H. A systematic review of the survival and complication rates of all-ceramic and metal-ceramic reconstructions after an observation period of at least 3 years. Part II: Fixed dental prostheses. Clin Oral Implants Res 2007, 18 Suppl 3, 86-96. [CrossRef]
- Hasan, I.; Bourauel, C.; Keilig, L.; Stark, H.; Luckerath, W. The effect of implant splinting on the load distribution in bone bed around implant-supported fixed prosthesis with different framework materials: A finite element study. Ann Anat 2015, 199, 43-51. [CrossRef]
- Barootchi, S.; Askar, H.; Ravida, A.; Gargallo-Albiol, J.; Travan, S.; Wang, H.L. Long-term Clinical Outcomes and Cost-Effectiveness of Full-Arch Implant-Supported Zirconia-Based and Metal-Acrylic Fixed Dental Prostheses: A Retrospective Analysis. Int J Oral Maxillofac Implants 2020, 35, 395-405. [CrossRef]
- Ortorp, A.; Jemt, T. CNC-milled titanium frameworks supported by implants in the edentulous jaw: a 10-year comparative clinical study. Clin Implant Dent Relat Res 2012, 14, 88-99. [CrossRef]
- Tartaglia, G.M.; Maiorana, C.; Gallo, M.; Codari, M.; Sforza, C. Implant-Supported Immediately Loaded Full-Arch Rehabilitations: Comparison of Resin and Zirconia Clinical Outcomes in a 5-Year Retrospective Follow-Up Study. Implant Dent 2016, 25, 74-82. [CrossRef]
- Tribst, J.P.M.; Campanelli de Morais, D.; Melo de Matos, J.D.; Lopes, G.; Dal Piva, A.M.O.; Souto Borges, A.L.; Bottino, M.A.; Lanzotti, A.; Martorelli, M.; Ausiello, P. Influence of Framework Material and Posterior Implant Angulation in Full-Arch All-on-4 Implant-Supported Prosthesis Stress Concentration. Dent J (Basel) 2022, 10. [CrossRef]
- Delucchi, F.; De Giovanni, E.; Pesce, P.; Bagnasco, F.; Pera, F.; Baldi, D.; Menini, M. Framework Materials for Full-Arch Implant-Supported Rehabilitations: A Systematic Review of Clinical Studies. Materials (Basel) 2021, 14. [CrossRef]
- Menini, M.; Conserva, E.; Tealdo, T.; Bevilacqua, M.; Pera, F.; Signori, A.; Pera, P. Shock absorption capacity of restorative materials for dental implant prostheses: an in vitro study. Int J Prosthodont 2013, 26, 549-556. [CrossRef]
- Tiossi, R.; Gomes, E.A.; Faria, A.C.L.; Rodrigues, R.C.S.; Ribeiro, R.F. Biomechanical behavior of titanium and zirconia frameworks for implant-supported full-arch fixed dental prosthesis. Clin Implant Dent Relat Res 2017, 19, 860-866. [CrossRef]
- Katsoulis, J.; Takeichi, T.; Sol Gaviria, A.; Peter, L.; Katsoulis, K. Misfit of implant prostheses and its impact on clinical outcomes. Definition, assessment and a systematic review of the literature. Eur J Oral Implantol 2017, 10 Suppl 1, 121-138.
- Kolgeci, L.; Mericske, E.; Worni, A.; Walker, P.; Katsoulis, J.; Mericske-Stern, R. Technical complications and failures of zirconia-based prostheses supported by implants followed up to 7 years: a case series. Int J Prosthodont 2014, 27, 544-552. [CrossRef]
- Vallittu, P.K. High-aspect ratio fillers: fiber-reinforced composites and their anisotropic properties. Dent Mater 2015, 31, 1-7. [CrossRef]
- Vallittu, P.K. An overview of development and status of fiber-reinforced composites as dental and medical biomaterials. Acta Biomater Odontol Scand 2018, 4, 44-55. [CrossRef]
- Menini, M.; Pesce, P.; Bevilacqua, M.; Pera, F.; Tealdo, T.; Barberis, F.; Pera, P. Effect of Framework in an Implant-Supported Full-Arch Fixed Prosthesis: 3D Finite Element Analysis. Int J Prosthodont 2015, 28, 627-630. [CrossRef]
- Menini, M.; Pera, F.; Barberis, F.; Rosenberg, G.; Bagnasco, F.; Pesce, P. Evaluation of Adhesion Between Carbon Fiber Frameworks and Esthetic Veneering Materials. Int J Prosthodont 2018, 31, 453-455. [CrossRef]
- Skalak, R. Biomechanical considerations in osseointegrated prostheses. J Prosthet Dent 1983, 49, 843-848. [CrossRef]
- Zhang, M.; Matinlinna, J.P. E-Glass Fiber Reinforced Composites in Dental Applications. Silicon 2011, 4, 73-78. [CrossRef]
- Menini, M.; Dellepiane, E.; Pera, P.; Bevilacqua, M.; Pesce, P.; Pera, F.; Tealdo, T. A Luting Technique for Passive Fit of Implant-Supported Fixed Dentures. J Prosthodont 2016, 25, 77-82. [CrossRef]
- Menini, M.; Pera, F.; Migliorati, M.; Pesce, P.; Pera, P. Adhesive strength of the luting technique for passively fitting screw-retained implant-supported prostheses: an in vitro evaluation. Int J Prosthodont 2015, 28, 37-39. [CrossRef]
- Wolff, D.; Wohlrab, T.; Saure, D.; Krisam, J.; Frese, C. Fiber-reinforced composite fixed dental prostheses: A 4-year prospective clinical trial evaluating survival, quality, and effects on surrounding periodontal tissues. J Prosthet Dent 2018, 119, 47-52. [CrossRef]
- Pesce, P.; Lagazzo, A.; Barberis, F.; Repetto, L.; Pera, F.; Baldi, D.; Menini, M. Mechanical characterisation of multi vs. uni-directional carbon fiber frameworks for dental implant applications. Mater Sci Eng C Mater Biol Appl 2019, 102, 186-191. [CrossRef]
- Freilich, M.A.; Karmaker, A.C.; Burstone, C.J.; Goldberg, A.J. Development and clinical applications of a light-polymerized fiber-reinforced composite. J Prosthet Dent 1998, 80, 311-318. [CrossRef]
- Collaert, B.; De Bruyn, H. Immediate functional loading of TiOblast dental implants in full-arch edentulous maxillae: a 3-year prospective study. Clin Oral Implants Res 2008, 19, 1254-1260. [CrossRef]
- Nakamura, T.; Waki, T.; Kinuta, S.; Tanaka, H. Strength and elastic modulus of fiber-reinforced composites used for fabricating FPDs. Int J Prosthodont 2003, 16, 549-553.
- Behr, M.; Rosentritt, M.; Lang, R.; Chazot, C.; Handel, G. Glass-fibre-reinforced-composite fixed partial dentures on dental implants. J Oral Rehabil 2001, 28, 895-902. [CrossRef]
- Karataban, P.; Demirel, O.; Ortug, G. An investigation into the total mandibular length and its potential correlation with the intraoral forces. Translational Research in Anatomy 2022, 27. [CrossRef]
- Pjetursson, B.E.; Fehmer, V.; Sailer, I. EAO Position Paper: Material Selection for Implant-Supported Restorations. Int J Prosthodont 2022, 35, 7-16. [CrossRef]
- Poggio, C.E.; Ercoli, C.; Rispoli, L.; Maiorana, C.; Esposito, M. Metal-free materials for fixed prosthodontic restorations. Cochrane Database Syst Rev 2017, 12, CD009606. [CrossRef]
- Bjork, N.; Ekstrand, K.; Ruyter, I.E. Implant-fixed, dental bridges from carbon/graphite fibre reinforced poly(methyl methacrylate). Biomaterials 1986, 7, 73-75. [CrossRef]
- Ruyter, I.E.; Ekstrand, K.; Bjork, N. Development of carbon/graphite fiber reinforced poly (methyl methacrylate) suitable for implant-fixed dental bridges. Dent Mater 1986, 2, 6-9. [CrossRef]
- Pera, F.; Pesce, P.; Solimano, F.; Tealdo, T.; Pera, P.; Menini, M. Carbon fibre versus metal framework in full-arch immediate loading rehabilitations of the maxilla - a cohort clinical study. J Oral Rehabil 2017, 44, 392-397. [CrossRef]
- Menini, M.; Pesce, P.; Pera, F.; Barberis, F.; Lagazzo, A.; Bertola, L.; Pera, P. Biological and mechanical characterization of carbon fiber frameworks for dental implant applications. Mater Sci Eng C Mater Biol Appl 2017, 70, 646-655. [CrossRef]
- Malo, P.S.; de Araujo Nobre, M.A.; Ferro, A.S.; Parreira, G.G. Five-year outcome of a retrospective cohort study comparing smokers vs. nonsmokers with full-arch mandibular implant-supported rehabilitation using the All-on-4 concept. J Oral Sci 2018, 60, 177-186. [CrossRef]
- Malo, P.; de Araujo Nobre, M.; Moura Guedes, C.; Almeida, R.; Silva, A.; Sereno, N.; Legatheaux, J. Short-term report of an ongoing prospective cohort study evaluating the outcome of full-arch implant-supported fixed hybrid polyetheretherketone-acrylic resin prostheses and the All-on-Four concept. Clin Implant Dent Relat Res 2018, 20, 692-702. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).