Introduction
The mechanical integrity of the pelvic ring is attributable to the pelvis’ highly stable structure 1. However, due to the aging population, fragility fractures are becoming more common. These fractures can be the result of low energy impact, or high-velocity injuries such as motor vehicle accidents, falls from large heights, and crush injuries 2. Pelvic ring injuries can prove to be fatal and disrupt the associated vascular and neurologic structures, especially in geriatric patients as mortality rates range between 10% and 16% 3. Classification of fractures involve many groups, including the Rommen classification for fragility fractures of the pelvic ring. In the Rommen classification, the type IIC fracture is a variant which is a non-displaced sacral, iliosacral, or ilium fracture with anterior disruption 2. The complete disruption of the posterior and anterior pelvic complex in these fractures posit a highly demanding injury and unilateral pelvic instability 3 4. The type IIC pelvic fractures are challenging in that they often require immediate stabilization which is typically performed through internal fixation to maintain circulatory balance and to achieve anatomic restoration of the pelvis 5 6 7.
Several pelvic ring fracture fixation techniques currently exist with varying levels of invasiveness. Transiliac plate fixation, which connects the left and right ilium with plates, is highly invasive to posterior soft tissues of the pelvis. To mitigate this, recent literature has investigated several minimally invasive treatment approaches that have been found to be equally stable 5, 8. These treatments include the trans-iliac trans-sacral screw (TITS) 9, the ilio-sacral (IS) screw 10, 11, the transiliac rod and screw fixation (TIF) procedure and lumbopelvic fixation (LP) 8 12, 13 14. However, controversy remains on the advantages and disadvantages of these minimally invasive treatment options for unstable pelvic fractures. Therefore, it is necessary to understand the biomechanics of the spine-pelvis complex for various pelvic ring fracture fixation techniques. By utilizing a three-dimensional finite element (FE) model, this biomechanical study compares different combinations of five minimally invasive treatments for unstable type IIC pelvic fractures.
Material and methods
Finite element model of lumbar spine pelvis
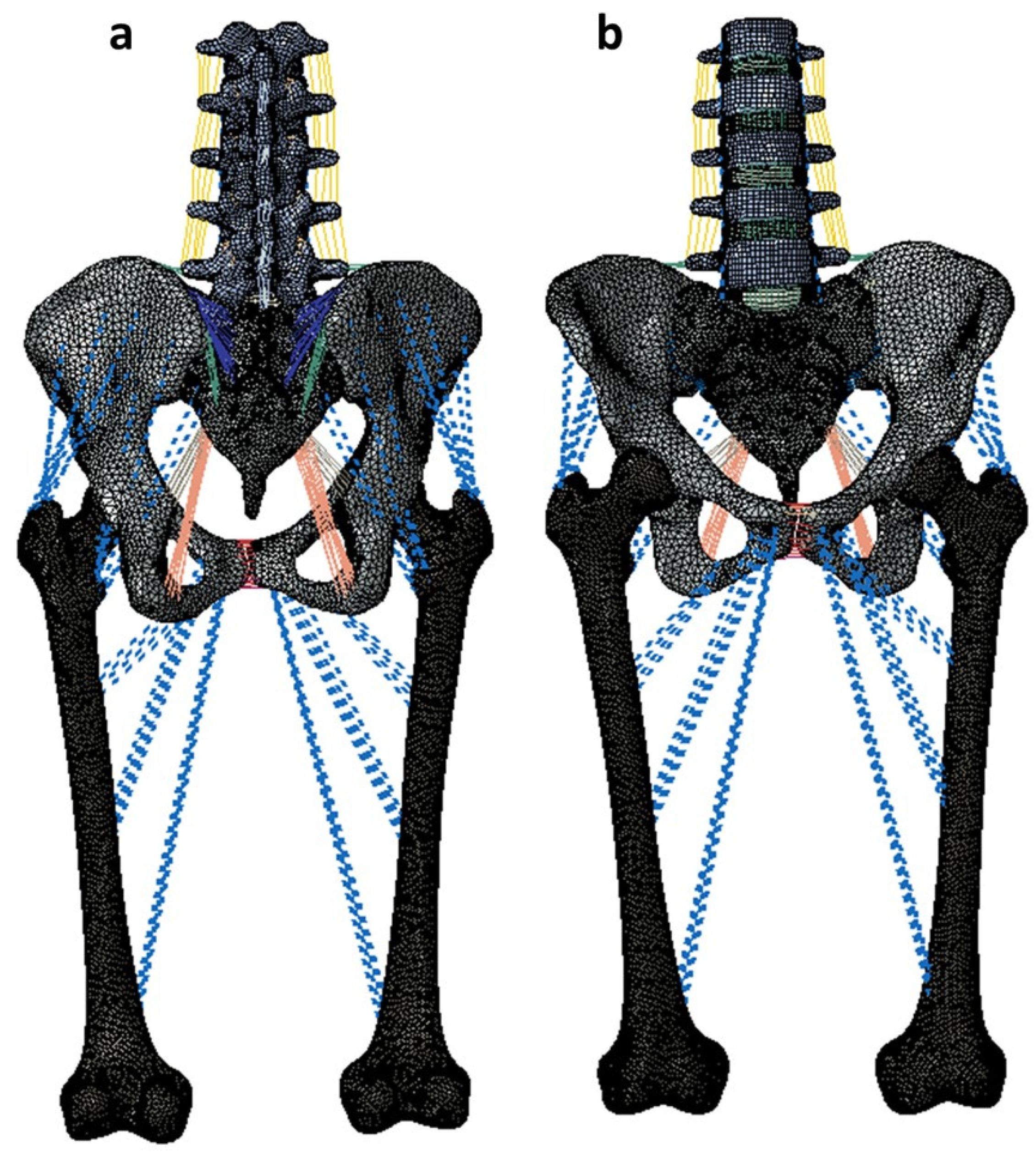
A non-linear ligamentous FE model including the lumbar spine, sacrum, pelvis and femurs was used for analyses using Abaqus 2019 software (Dassault Systèmes, Simulia Inc., Providence, RI, USA) (
Figure 1). The FE model was developed from the CT scan images of a female cadaveric spine without any abnormalities, deformities, or severe degenerative changes. The CT images were imported to Mimics (Materialize Inc, Leuven Belgium) for model reconstruction.
The FE model included the intervertebral discs, ligamentous structures, vertebral bodies, and facet joints. The initial lumbar lordosis (LL) for the adult female model was 42° representing normal spinal alignment as per Schwab classification 15. The other spinopelvic parameters of this model were SS=26°, PI=37°, and PT=11° 16, 17.
The reconstructed model was meshed using IAFE-MESH software (University of Iowa, Iowa) and Hypermesh software (Altair, Michigan, USA). Linear hexahedral elements were used for modeling the cortical bone of the vertebrae and spinal discs. Linear tetrahedral elements were used for the cancellous bone of the vertebrae and the cortical and cancellous bones of the sacrum, pelvis, and femur. The ligamentous soft tissues were modeled using truss elements. The intervertebral disc included both the annulus and nucleus. The annulus and nucleus were simulated as a composite solid using hexahedral elements. The facet and sacroiliac joints were modeled using a surface-to-surface soft contact with exponential behavior.
The material properties were assigned based on previously published literature (
Table 1)
18-22.
The model was previously validated by comparing the range of motion data against data obtained from studies on in-vitro cadaveric specimens. A mesh convergence study was also performed on the model, as reported in the previous study 23.
Simulation of pelvic ring fracture
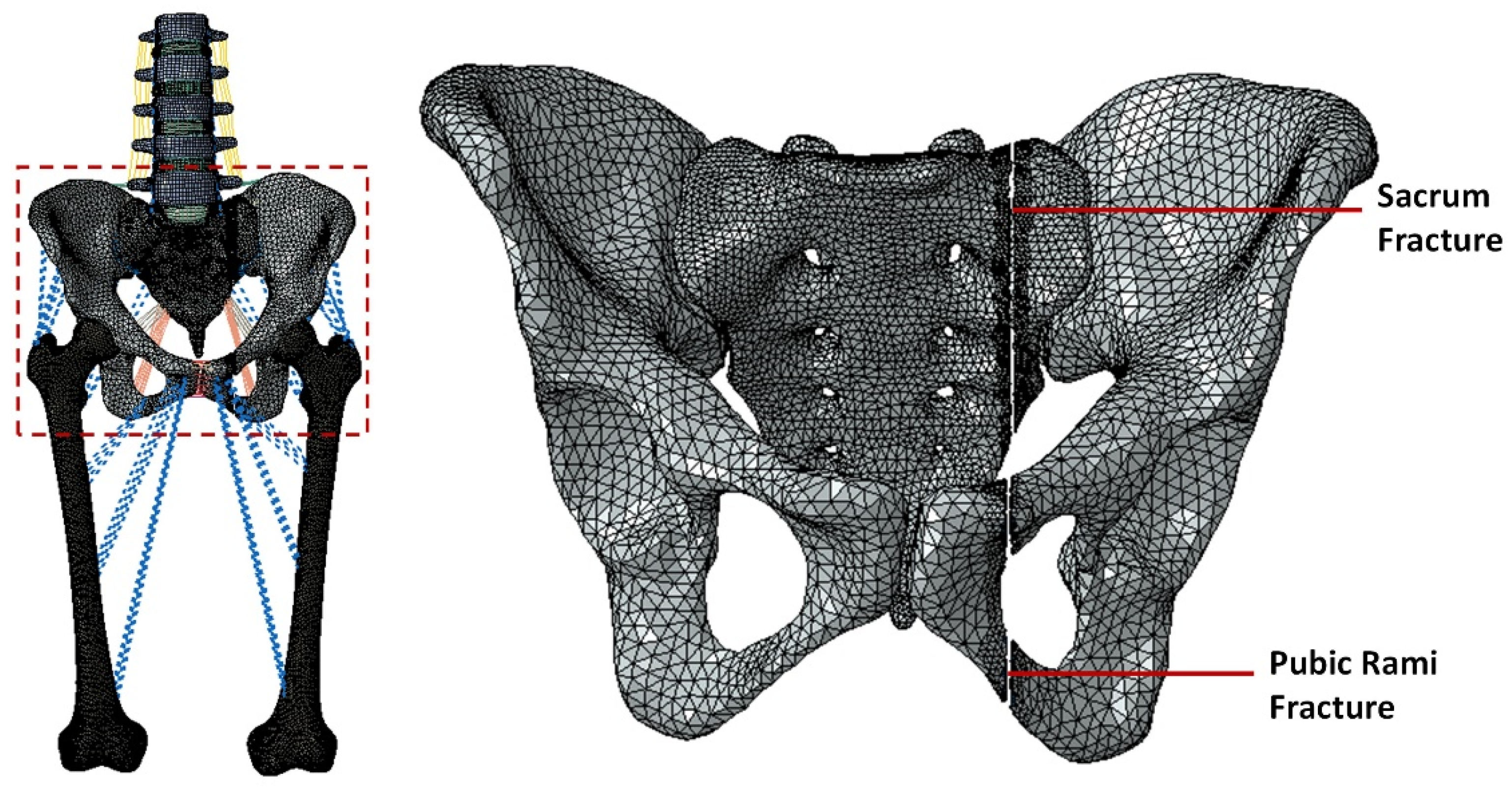
A unilateral pelvic ring fracture was simulated on the adult female spine FE model by resecting the left side of the sacrum and pelvis (
Figure 2)
24. A type IIC fracture was simulated as per Rommens classification
2 with a gap of approximately 1.7mm. A surface-to-surface interaction with hard contact was used to model the interaction between the fractured surfaces of the sacrum and the pelvis
24.
Simulating the instrumentation of pelvic ring fracture
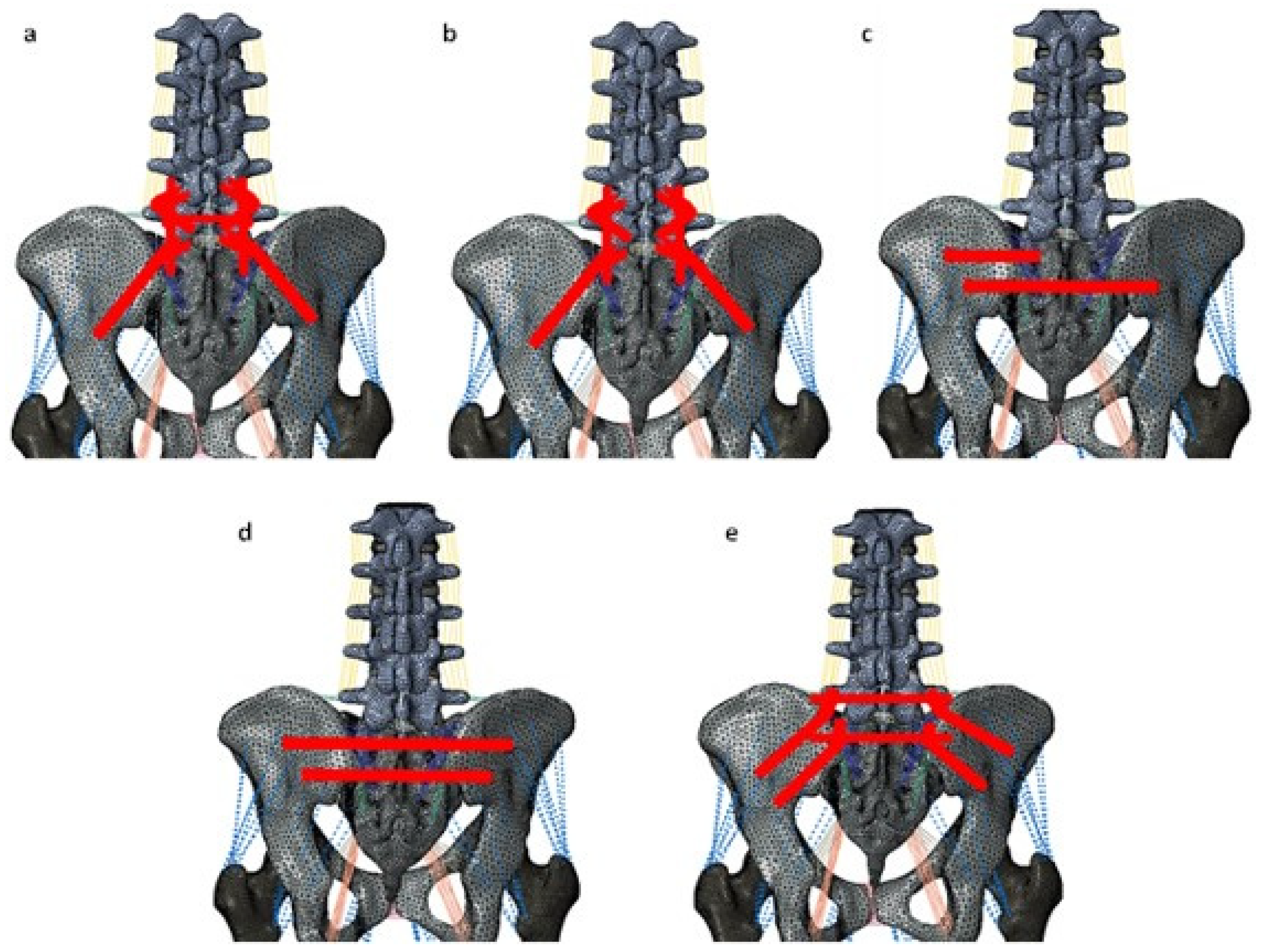
This study simulated and evaluated five posterior instrumented stabilization strategies for pelvic ring fractures (
Figure 3):
L5-Ilium posterior screw fixation without cross connectors (L5_PF_WO_CC): Bilateral posterior screw fixation was performed from L5-Ilium. The pedicle screws were connected to spinal rods.
L5-Ilium posterior screw fixation with cross connectors (L5_PF_W_CC): Bilateral posterior screw fixation was performed from L5-Ilium. The pedicle screws were connected to spinal rods. A cross connector was placed at the S1 level to connect the two rods.
TITS fixation at S1 and S2 level (S1_TITS_S2_TITS): TITS fixation was simulated at the S1 and S2 levels.
IS fixation at S1 and TITS fixation at S2 level (S1_IS_S2_TITS): A TITS fixation was simulated at the S2 level, and an ilio-sacral screw (IS) fixation was performed at the S1 level.
Double transiliac rod and screw fixation (DTSF): Two traditional iliac screws were placed bilaterally. A horizontal rod was used to connect the iliac screws.
TiAl4V alloy material properties were applied to the screws, rods, and cross-connectors. A tie interaction was used to simulate the rigid fixation between the screws, the rods/screws, and the cross-connectors. A screw-bush and bush-bone interface was utilized to simulate the screw fixation. For the screw-bush interface, a tie interaction was defined between the outer surface of the screw and the inner surface of the bush. The bush-bone interface was simulated using the “coupling” constraint 25, 26.
Loading and boundary conditions
For all models, a 400N compressive follower load was applied to simulate the weight of the upper trunk and the effect of muscle forces. A 7.5 Nm bending moment was applied to the superior surface of the L1 vertebra to simulate flexion/extension, lateral bending, and axial rotation 24. The distal portion of the femur was fixed in all degrees of freedom to simulate a two-leg stance posture.
Data analyses
The stabilization offered by the five models was quantified by analyzing the horizontal; and vertical displacement across the pelvic and sacral fractures. The standard protocol for sacral fracture fixation is typically the S1_IS_S2_TITS, therefore it was used to compare sacral fracture displacement across each case. The contralateral side (right) SIJ ROM, the L5-S1 ROM, L1-S1 ROM, and the L5-S1 nucleus stress were recorded and compared across the five instrumented models and to the intact model.
Results
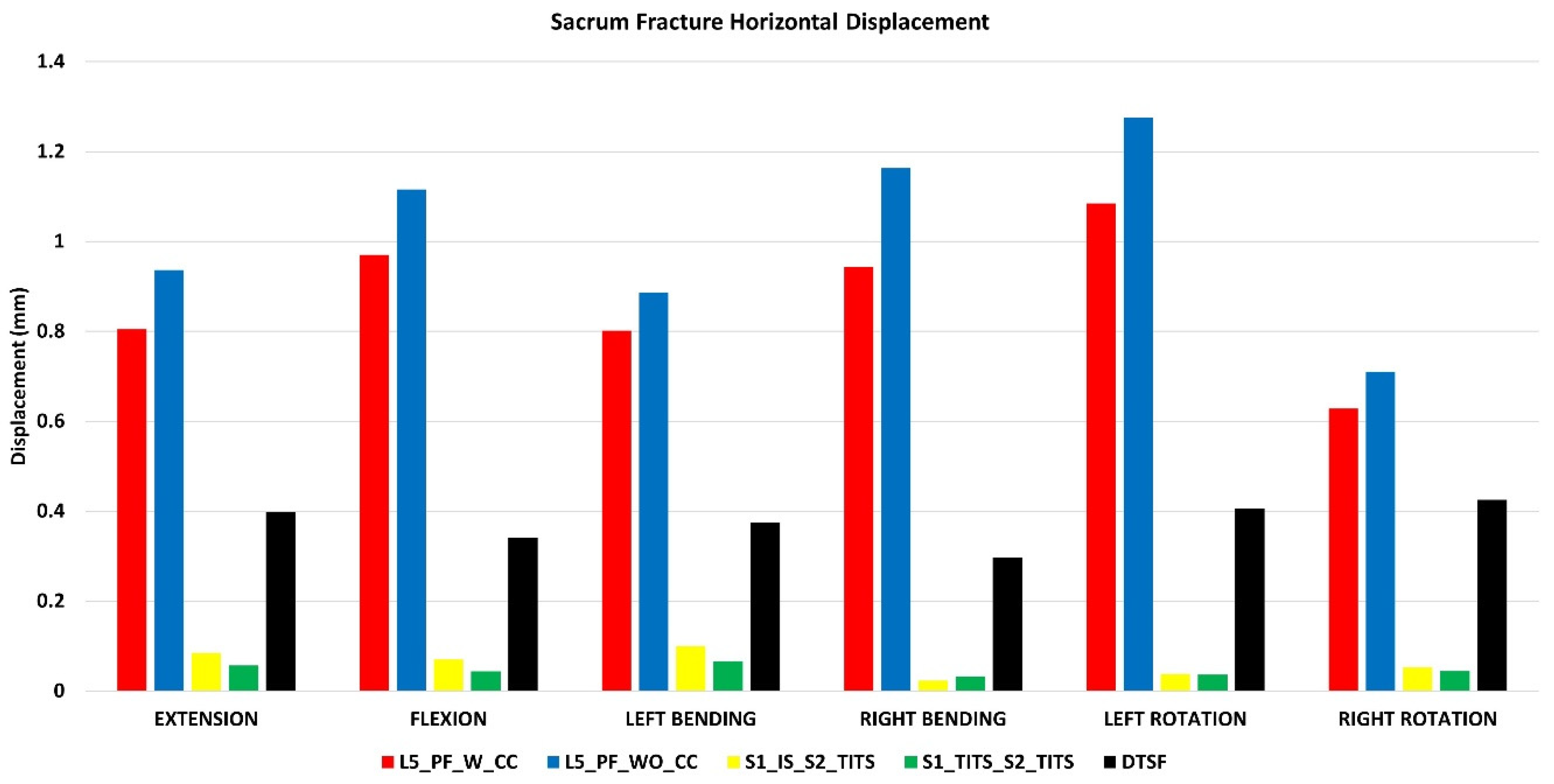
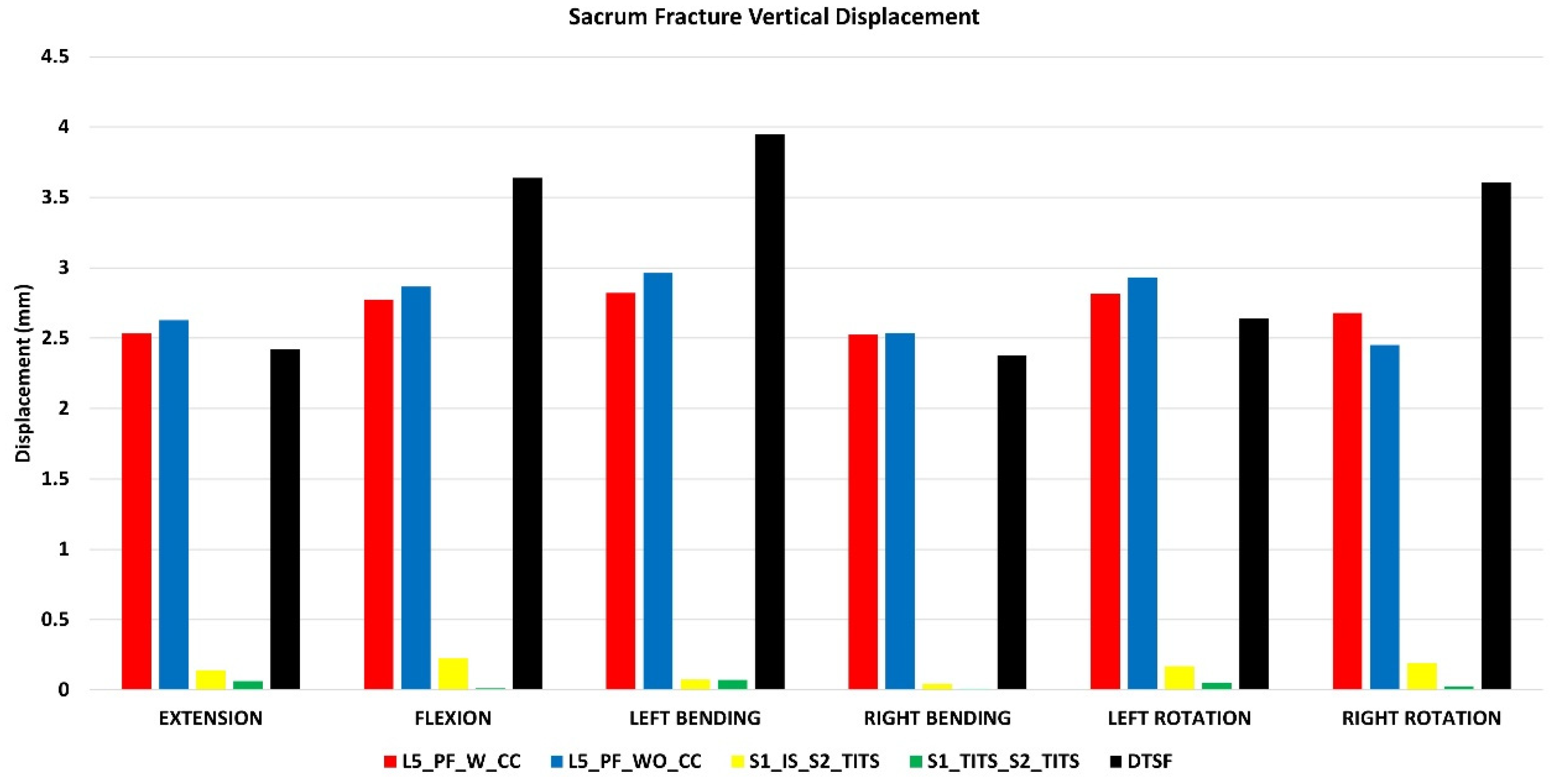
Stabilization at the Sacral fracture region (Figure 4 and Figure 5)
At the fracture site, both horizontal and vertical displacement for S1_TITS_S2_TITS fixation showed the highest stabilization. At the same time, the L5_PF_WO_CC was noted to be the most unstable for horizontal displacement, however the DTSF was most unstable due to the large vertical displacement.
Regarding the horizontal fracture site displacement, the L5_PF_W_CC configuration compared to S1_IS_S2_TITS showed more than 100% increases in extension, left bending, right bending, left rotation, and right rotation ROM, respectively. Similar trends were observed in L5_PF_WO_CC, and DTSF models, while S1_TITS_S2_TITS showed reduction in horizontal displacement at the fracture site compared to S1_IS_S2_TITS model. The reduction was approximately 32%, 34%, and 15% in extension/flexion, lateral bending, and axial rotation motions, respectively (
Figure 4).
Regrading vertical fracture site displacement, L5_PF_W_CC, L5_PF_WO_CC and DTSF models compared to S1_IS_S2_TITS showed more than 100% increases for all motions. While S1_TITS_S2_TITS showed reduction in vertical displacement at the fracture site by approximately 55%, 94%,78%, and 86% in extension, flexion, right bending, and right rotation, respectively (
Figure 5).
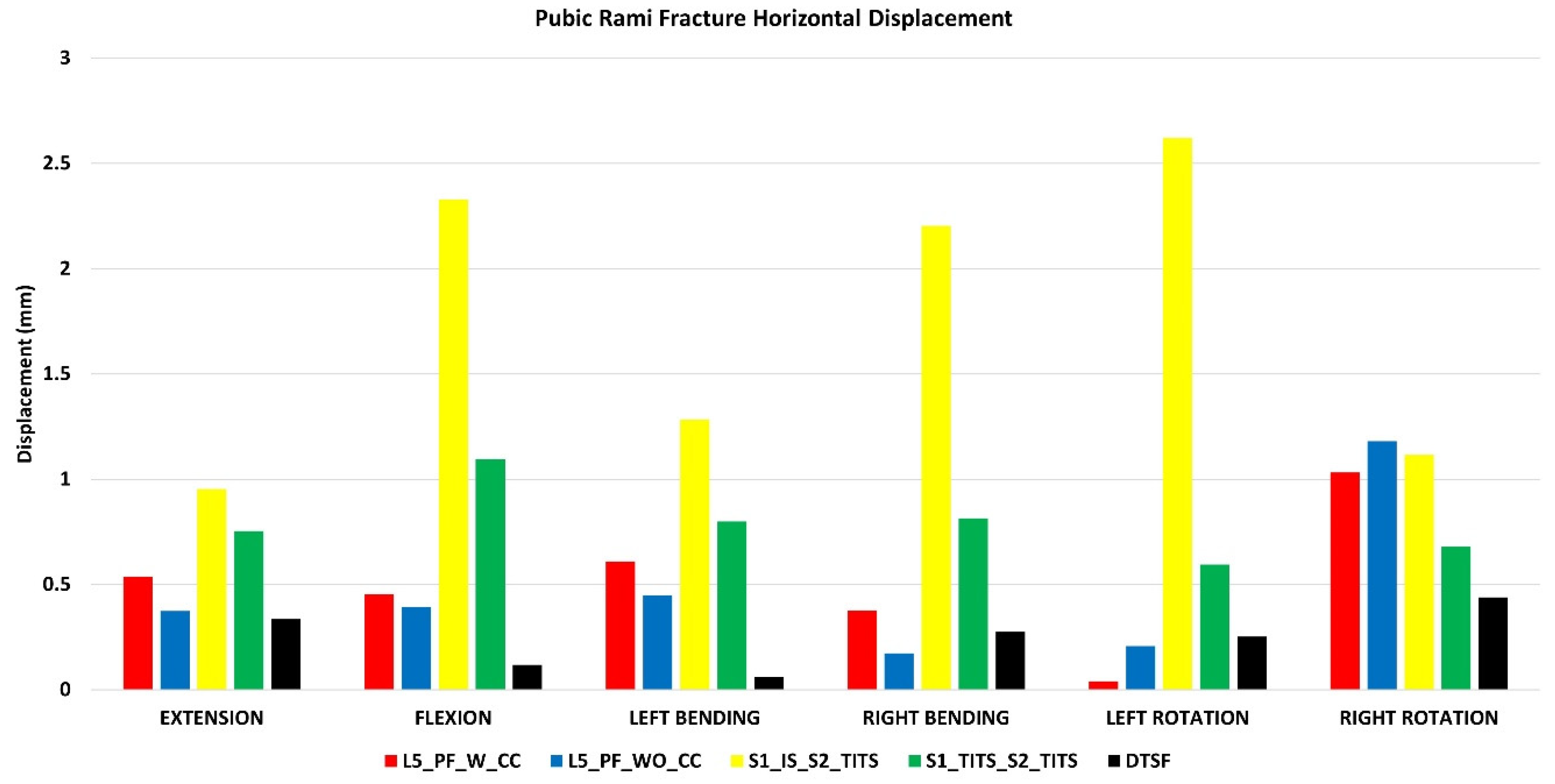
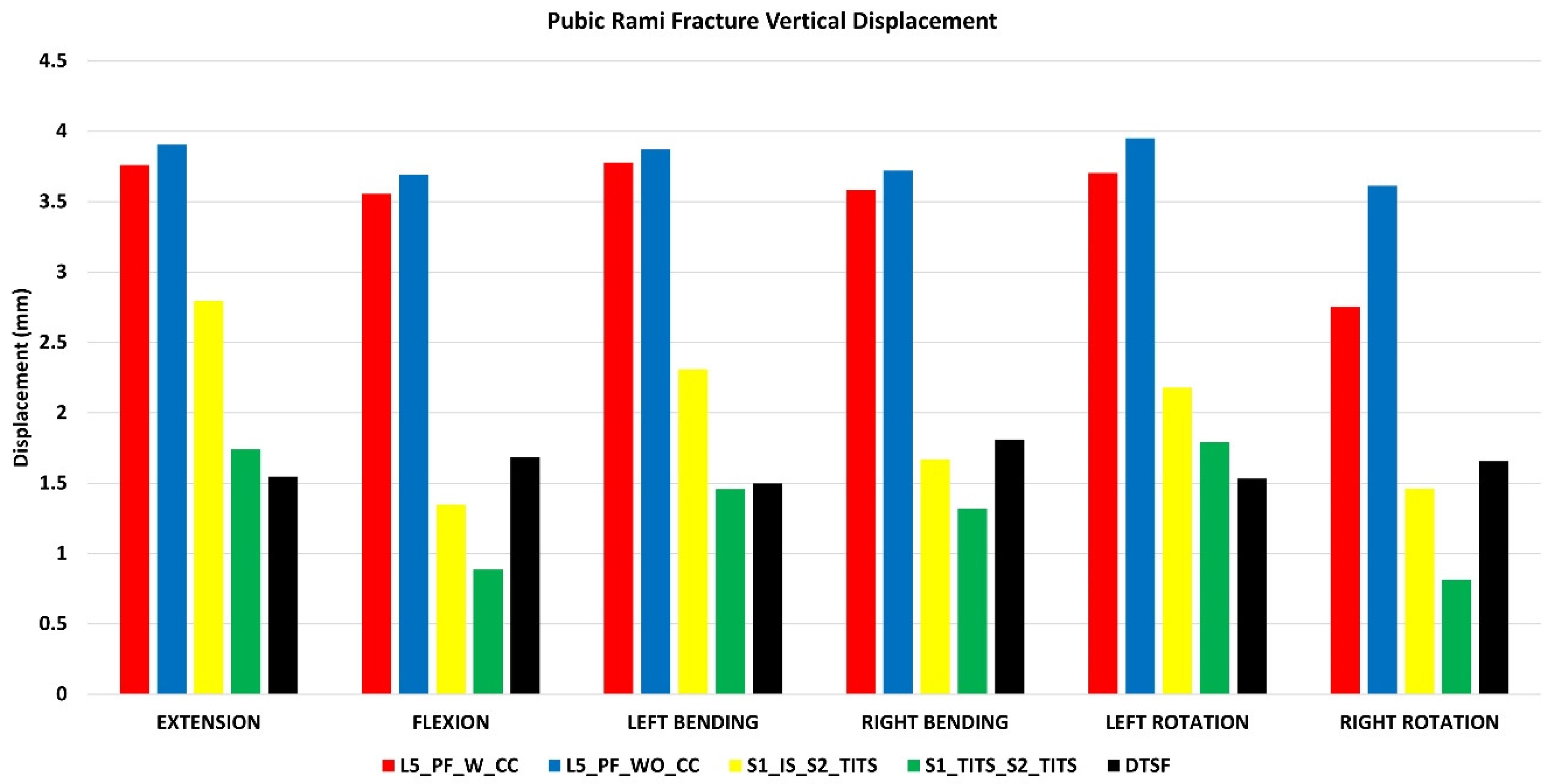
Stabilization at the Pubic Rami fracture region (Figure 6 and Figure 7)
The DTSF fixation showed the highest stabilization for horizontal and vertical displacement at the pubic rami fracture site. S1_IS_S2_TITS fixation resulted in largest horizontal displacement at the pubic rami fracture. The L5_PF_WO_CC fixation indicated the largest vertical displacement.
Regarding horizontal displacement, all other configurations showed approximately a 50% reduction in all motions compared to S1_IS_S2_TITS (
Figure 6).
For vertical displacement, the L5_PF_W_CC and L5_PF_WO_CC compared to S1_IS_S2_TITS showed increased displacement at pubic rami fracture site by 35%, 30%, 35%, 20%, 21%, and 40% for extension, flexion, left bending, right bending, left and right rotations, respectively. In contrast, the S1_TITS_S2_TITS and DTSF models showed decreased displacement at pubic rami fracture site compared to S1_IS_S2_TITS by approximately 35%, 165%, 65%, 120%, 75%, and 80% for extension, flexion, left bending, right bending, left and right rotations, respectively (
Figure 7).
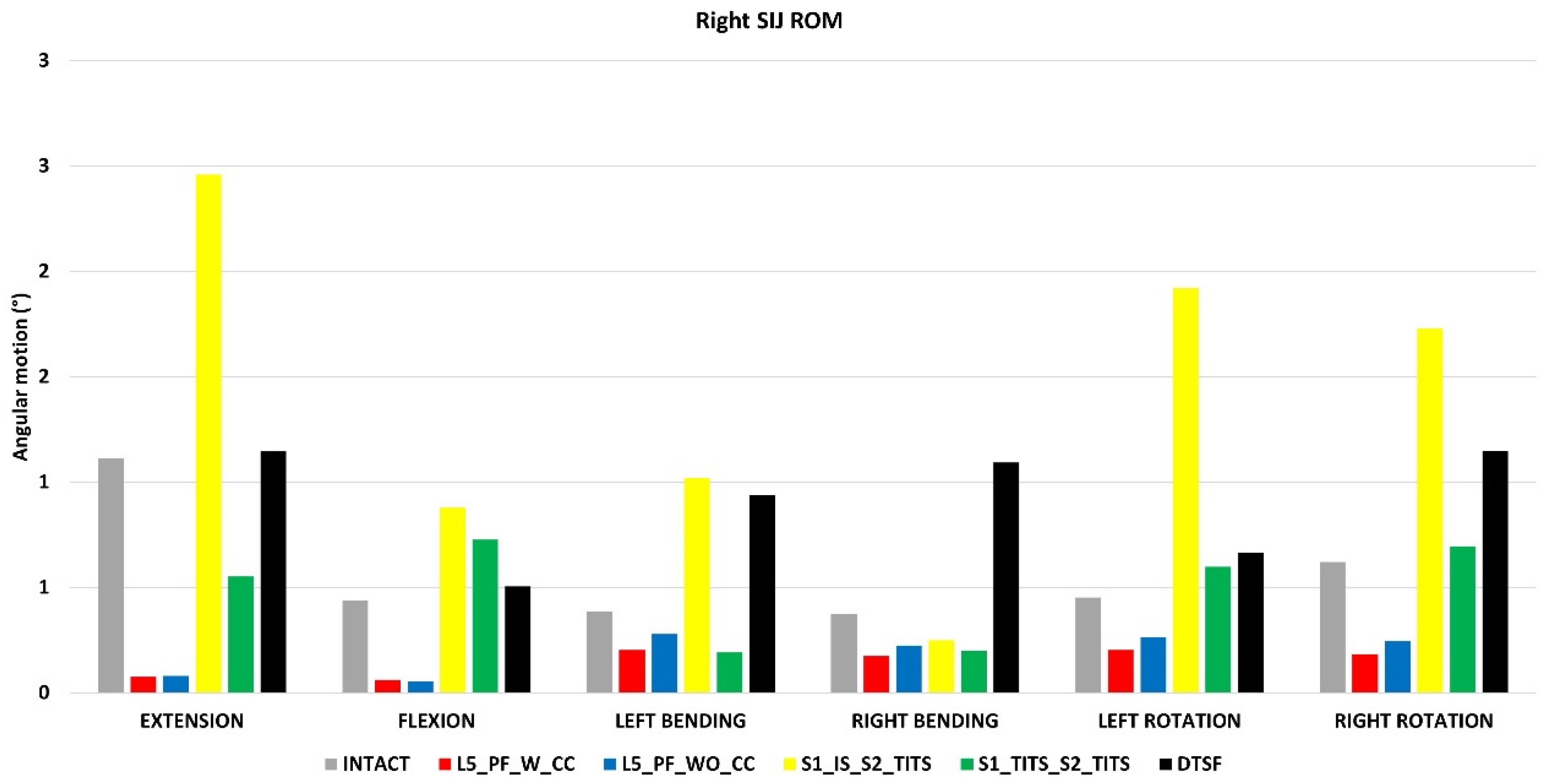
Sacroiliac joint (SIJ) range of motion (ROM) (Figure 8)
The SIJ ROM ipsilateral to the fracture site (left SIJ) indicated little motion in all fracture fixation cases and therefore was not recorded. All SIJ ROM was compared to the intact model with no instrumentation. A reduction of SIJ ROM at the contralateral side (right side) was recorded with L5_PF_W_CC, L5_PF_WO_CC, and S1_TITS_S2_TITS configurations compared with the intact model. At the same time, S1_IS_S2_TITS showed increased ROM at the right SIJ compared with the intact model.
The S1_IS_S2_TITS fixation demonstrated the highest increase in the SIJ ROM at the contralateral side (right side) in flexion, extension, left bending, left axial rotation, and right axial rotation when compared to the intact model (121% 100% 164% 325% and 178%, respectively). Similar trends were observed with L5_PF_WO_CC compared to the intact model.
The L5_PF_W_CC fixation demonstrated the highest decrease in SIJ ROM at the contralateral side (right side) in flexion, extension, left bending, right bending, left axial rotation, and right axial rotation compared to the intact model (93%, 86%, 47%, 53%, 55% and 71%, respectively). Similar results were observed in the L5_PF_WO_CC model compared with the intact model (
Figure 8).
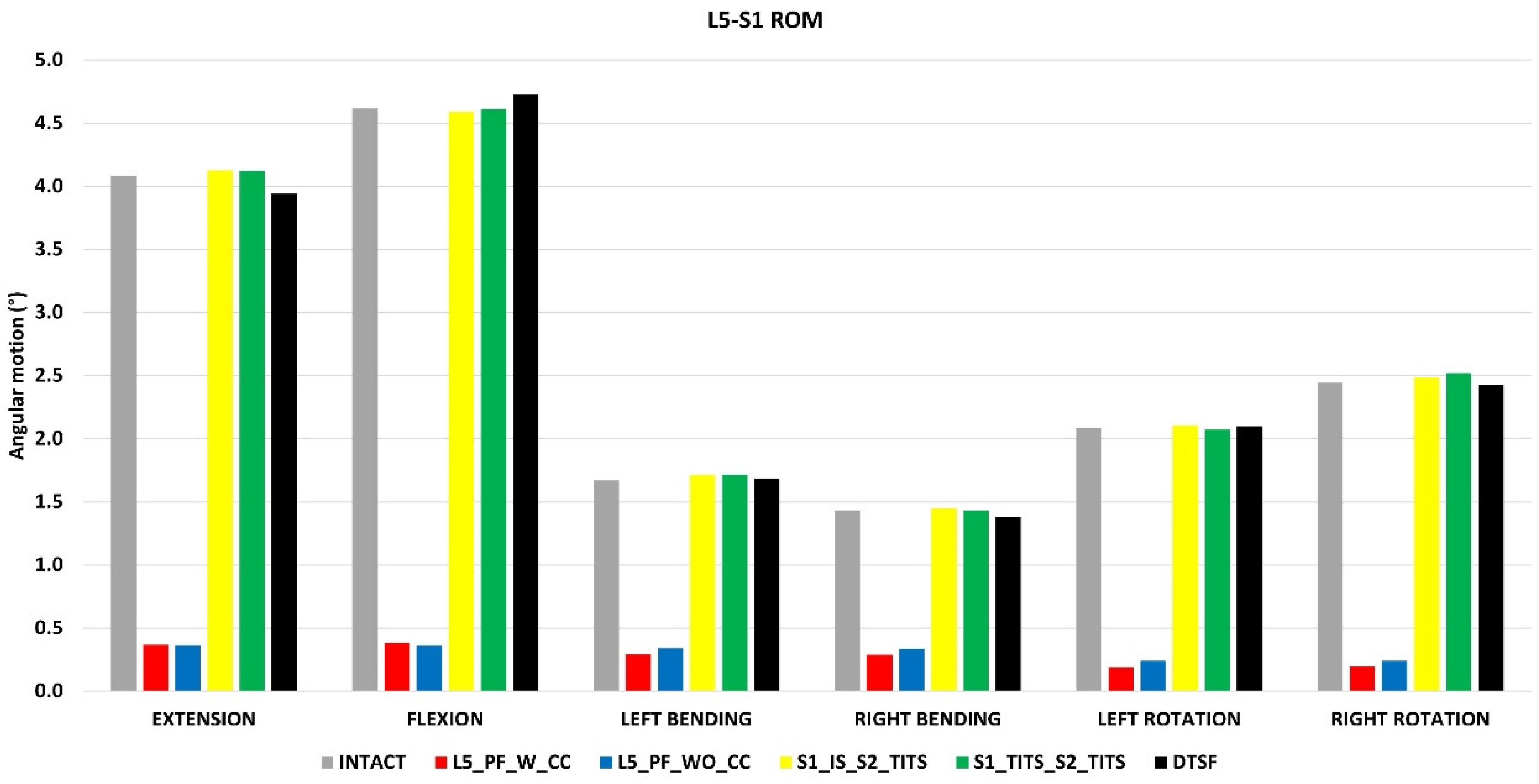
ROM at the L5-S1 level (Figure 9)
All cases for L5-S1 ROM were compared to the intact model with no instrumentation. The L5_PF_W_CC fixation showed the highest reduction in ROM at the L5-S1 level in flexion, extension, left lateral bending, right lateral bending, left axial rotation, and right axial rotation compared to the intact model (91%, 92%, 82%, 80%, 91%, and 92%, respectively). The L5_PF_WO_CC fixation also showed a substantial decrease in the ROM at the L5-S1 level. The ROM of the L5-S1 level showed negligible in the other stabilization models compared to the intact model (
Figure 9)
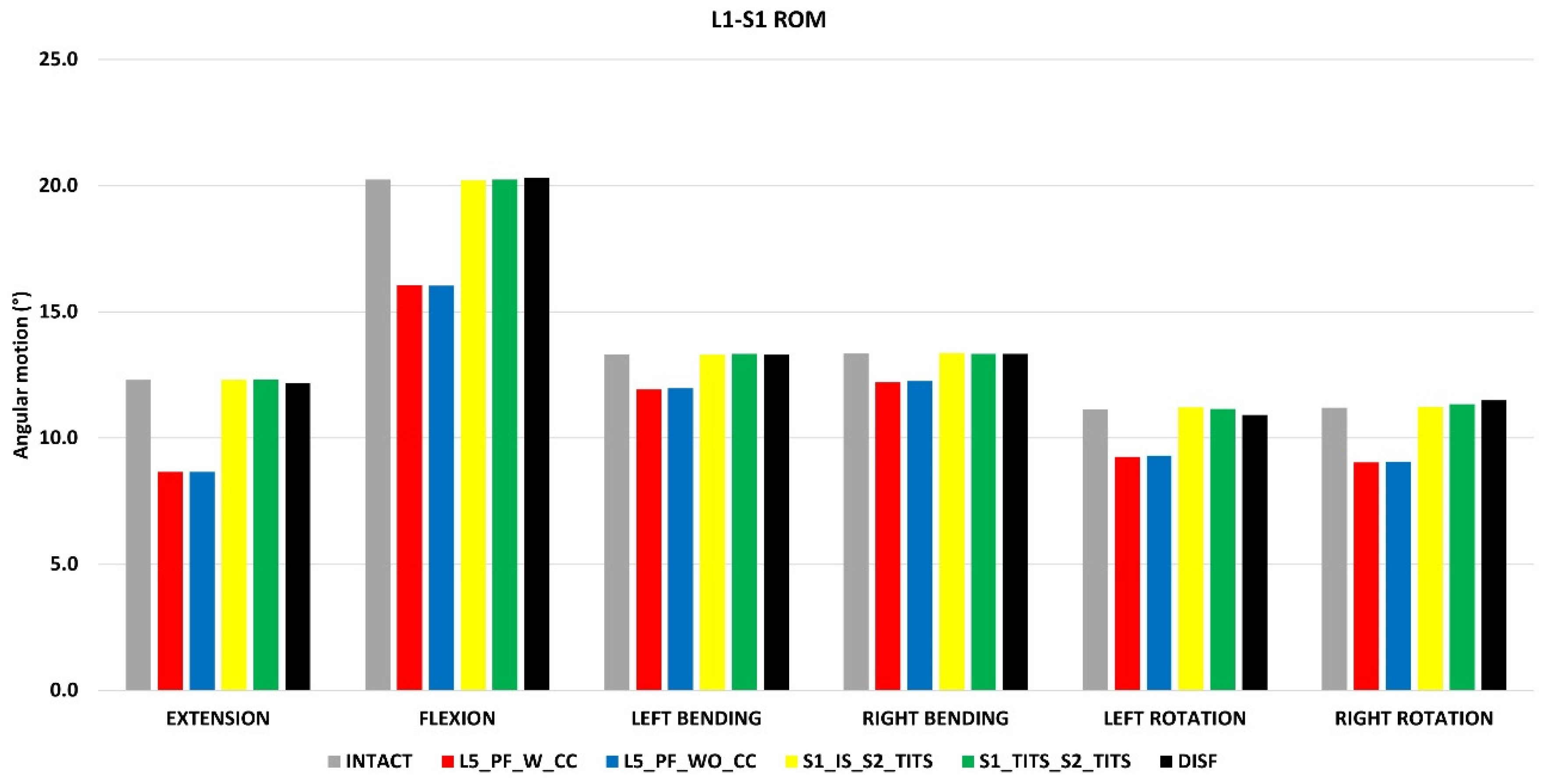
Overall ROM for L1-S1 (Figure 10)
Compared to the intact model, L5_PF_W_CC and L5_PF_WO_CC indicated a reduction in ROM for L1-S1. The ROM was reduced by 29%, 20%, 10%, 8%, 16%, and 19% for extension, flexion, left bending, right bending, left rotation, and right rotation, respectively, in both configurations. There was no change in motion for other configurations at the L1-S1 level (
Figure 10).
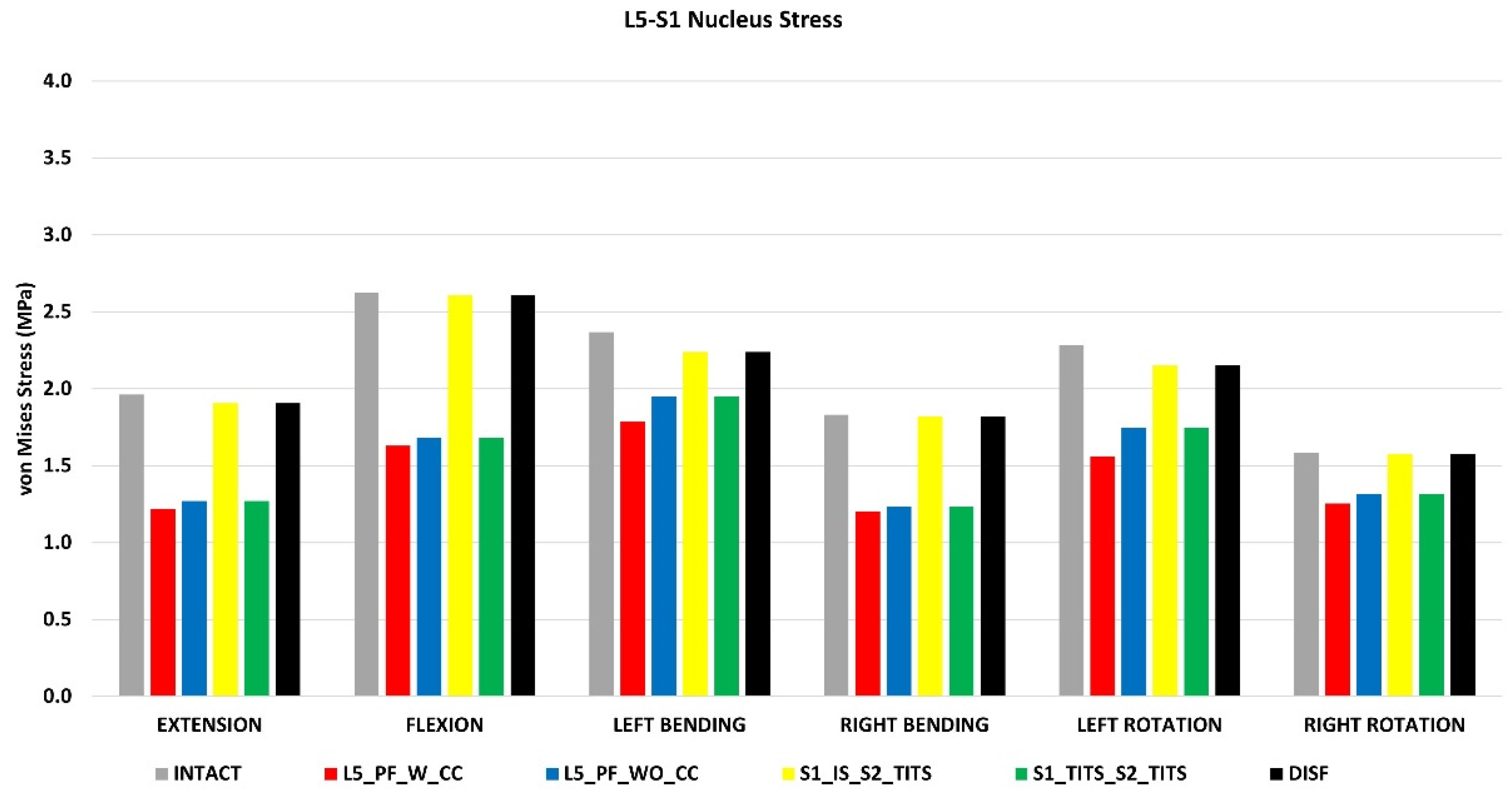
Peak von Mises stresses at the L5-S1 intervertebral disc (Figure 11)
All surgical cases were compared to the intact model with no instrumentation. The L5_PF_W_CC showed the highest reduction in peak von Mises stresses in the L5-S1 nucleus (38%, 38%, 24%, 34%, 32%, and 20% decrease in flexion, extension, left and right lateral bending, and left and right axial rotation, respectively) compared to the intact model.
The L5_PF_WO_CC and S1_TITS_S2_TITS fixations also showed a substantial decrease in the von Mises stresses in the L5-S1 nucleus.
The von Mises stresses in the L5-S1 nucleus negligible changes for the other stabilization models compared to the intact model (
Figure 11).
Stress on the implants (Table 2)
Peak stresses on the rods and screws are shown in
Table 2 for all the configurations for different loading conditions. Rods of L5_PF_WO_CC showed the largest stresses followed by L5_PF_W_CC and DTSF configuration. The screws of S1_TITS_S2_TITS indicated the higher stresses compared to the S1_IS_S2_TITS configuration.
Discussion
To the author’s knowledge, this analysis is the first to evaluate the biomechanical effects of five different minimally invasive procedures for unstable pelvic fractures on the devices described, the fracture site and the lumbar spine.
During treatment of pelvic ring fractures, posterior stability is of paramount importance to ensure proper fracture union. Minimally invasive procedures have been proposed to avoid many of the complications associated with the traditional locking plate fixation used for sacral fractures; however, surgical treatment plans are highly dependent on the type of fracture pattern leading to debate on the optimal technique 27. Due to this, we examined the biomechanical effects of various procedures including TITS, IS, DTSF and LP fixators on a Rommens Type IIC pelvic fracture.
In the present study, the cases that included the trans-sacral trans-iliac screws (S1_IS_S2_TITS and S1_TITS_S2_TITS) resulted in superior stabilization of the sacral fracture compared to the other fixations. In an FE analysis for posterior internal fixation for unstable pelvic fracture, Zhang created fixation models with a single S1 screw (S1-1), single S2 screw (S2-1), two S1 screws (S1-2) and a combination of a single S1 and a single S2 screw (S1–S2). They concluded that for type C fractures, a two screw construct (S1–S2) allowed for biomechanical stability 28. Our results in the present study display a similar outcome with the S1_IS_S2_TITS and S1_TITS_S2_TITS resulting in superior reduction of sacral fracture displacement compared to the other studied fixations, as indicated by the sustained sacral fracture stability in vertical displacement.
These results are consistent with Turbucz et al who conducted a biomechanical study on a Denis Type II sacral fracture. They evaluated and compared the biomechanical efficacy of six iliosacral screw fixation techniques with different lengths on literature based and patient specific bone material properties. Their results indicated that the S1_TITS_S2_TITS had the highest vertical stabilization in the sacral fracture for all cases, including in osteoporotic bone 29. It should be noted, however, that despite providing the highest stabilization in the sacral fracture region, the pubic rami fracture site showed the least stabilization in horizontal displacement in both fixation techniques. Furthermore, our study illustrated the sacral and pubic rami fractures were subject to less vertical displacement in the S1_TITS_S2_TITS compared to the S1_IS_S2_TITS, suggesting that inserting two longer trans-iliac trans-sacral screws was more effective for fracture stabilization, agreeing with previous studies 30.
Moreover, S1_TITS_S2_TITS decreased contralateral SIJ ROM during extension and bending, compared to the intact model due to the longer screws fusing the joints.
S1_IS_S2_TITS produced increased contralateral SIJ ROM compared to the intact model due to the shorter IS screw not fusing the contralateral SIJ.
In both surgical cases that included SIJ fusion, negligible changes were seen in L1-S1 and L5-S1 ROM. Interestingly, there was a decrease in L5-S1 nucleus stress in the S1_TITS_S2_TITS, despite retaining L5-S1 ROM. This finding may be attributed to the higher sacral stability resulting from the fusion of both joints when using two trans-iliac-trans-sacral screws. These results agree with previous studies examining how SIJ fusion limits adjacent segment changes in the lumbar spine 21.
Regarding screw stresses, the fixation devices that assumed the greatest loading achieved the most fracture stabilization on the sacral region. When comparing the sacral fixation devices (S1_IS_S2_TITS and S1_TITS_S2_TITS), the S1_TITS_S2_TITS case indicated the highest implant stress and most stabilization on the sacral fracture compared to the S1_IS_S2_TITS case. Previous clinical results have noted high rates of screw loosening in IS and TITS fixations 31-33. Our results numerically support these clinical findings as higher stresses on the screws may contribute to the risk of screw failure, especially when using two trans-iliac trans-sacral screws. The higher screw stresses can be attributed to the TITS screws extending across and fusing both SIJs compared to the IS screw, which only fused the left SIJ. Bastian et al further correlated screw breakaway within the sacrum and noted the superior portion of the sacrum provided optimal bone quality compared to the inferior portion for screw placement 31. Moreover, the S2 segment is attributed by decreased bone density compared to the S1 segment 34 and has been clinically associated with S2 screw failures 35, 36. However, Eastman et al revealed the region of the posterior ilium and SIJ to have the higher bone density compared to the sacral segments. This may indicate a decreased risk of screw failure for TITS placement due to crossing the posterior iliac region 37. Interestingly, our results for the DTSF, placed in the posterior ilium, was also subject to the lowest stresses while reducing the pubic rami fracture more than the trans-iliac trans-sacral fixations (S1_IS_S2_TITS and S1_TITS_S2_TITS). Clinical reports have noted transilliac screws have excellent results and lower complication rates compared to LCP and IS 8, 13, 38 which is further supported by the decrease implant stress noted by our study. Additionally, DTSF retained SIJ motion since the screws did not fuse the joint. L1-S1 and L5-S1 ROM are minimally changed compared to the intact which retains similar L5-S1 nucleus stress as the intact case. These outcomes warrant further investigation for DTSF as a favorable option for patients with poor sacral bone quality density. However, our results indicated that DTSF provided the least stabilization in the sacral fracture which may contribute to post-operative instability. Therefore, a delay in weight bearing conditions for patients treated with DTSF may be required to mitigate non-union at the cost of potentially unfavorable clinical outcomes 39.
Spinal instruments were originally applied with the Galveston technique for treatment of lumbosacral junction fractures. LP fixation with transpedicular screws are placed in the lower lumbar spine and additional screws in the posterior ilium 40. Fixation in this regard is strong, however the mobility of the lumbopelvic region is restricted 41. In this study, the LP fixations (L5_PF_WO_CC and L5_PF_W_CC) contributed to the greatest stability based on small horizontal displacement at the pubic rami fracture compared to the other studied fixations. The addition of a connector further increased the horizontal and vertical stability of the sacral fracture compared to the LP fixation without a cross connector. These results indicate certain fracture characteristics may benefit from cross connector due to increased facture site stability despite increased surgical time 42. Thus, addition of a connector should be carefully considered depending on the instability of the fracture and other patient specific factors 43, 44. The fracture stability resulting from LP fixations allow for immediate weight bearing which poses an increased benefit for younger or certain at-risk patients44. However, based on our results, the stability of this construct comes into question as loosening of screws and instrument failure is possible as a result of the highest instrument stresses compared to the other fixation devices in this study. Additionally, L5_PF_WO_CC and L5_PF_W_CC led to the largest reduction of ROM and nucleus stress in the L5-S1 joint due to the fusion of the intervertebral levels. These fixations also produced the greatest decrease in the contralateral SIJ ROM, overall L1-S1 ROM and reduced the fused level’s nucleus stress. Previous clinical and biomechanical reports have suggested an increase in adjacent segment degeneration due to spinal fusions 45, 46. Our results may suggest a similar trend as stresses in other segments may increase due to the increased ROM at these regions Based on the highlighted limitations of LP fixations noted in our study, we suggest that these constructs should only be considered in patients with lumbosacral junction instability or patients with sacral instability not amenable to sacroiliac screw fixation 47. However, further clinical studies are needed to support this theory.
Limitations
This biomechanical study has some inherent limitations that need to be addressed. Firstly, absence of complex muscle forces, particularly to paraspinal muscles, was addressed by substituting them with follower load on the spine, while simplified elastic properties were employed for the lower extremity muscles. Secondly, the assumption was made that the implants and bones exhibit bonding. This research did not examine multiple screw diameters and lengths. However, previous biomechanical studies have confirmed that increasing the length or diameter of the iliac screws can significantly enhance the iliac fixation strength 48, 49. Different body weight and more osteoporosis were not simulated, and it will be interesting to explore these factors in future studies. This research relies on a limited number of finite element models, with only one model representing each configuration. This insufficient dataset poses a challenge for conducting statistical analysis, highlighting the need for additional patient models encompassing diverse races and ages. Nonetheless, it is believed that this limitation is unlikely to significantly impact the study’s findings.
Conclusions
The present study is the first to examine the mechanics of multiple fixation techniques for pelvic fractures and may assist clinicians in understanding their characteristics, advantages, and disadvantages.
Author Contributions
Sudharshan Tripathi: Writing – Original draft, Conceptualization, Investigation. Norihiro Nishida: Editing, Formal analysis, Validation, Investigation. Sophia Soehnlen: Writing, Formal Analysis. Amey Kelkar: Reviewing, Modelling. Yogesh Kumaran: Editing, Formal Analysis. Toshihiro Seki: Reviewing, Editing. Takashi Sakai: Editing, Formal Analysis. Vijay K. Goel: Conceptualization, Writing – reviewing and editing, Supervision.
Acknowledgments
The work was supported in part by NSF Industry/University Cooperative Research Center at The University of California at San Francisco, CA, The Ohio State University, Columbus, Ohio, The University of Toledo, Toledo, OH (
www.nsfcdmi.org) and AO Foundation.
Abbreviations
FE: Finite Element; SIJ: Sacroiliac Joint; TITS: Transiliac-trans sacral screw: IS Iliac screw; L5_PF_W_CC: L5-ilium posterior screw fixation with cross connector; L5_PF_WO_CC: L5-ilium posterior screw fixation without cross connector; S1_TITS_S2_TITS: TITS fixation at S1 and S2 level; S1_IS_S2_TITS: IS fixation at S1 and TITS at S2 level; DTSF: Double transiliac rod and screw fixation; ROM: Range of Motion; LL: Lumbar Lordosis; SS: Sacral Slope; PT: Pelvic Tilt; PI: Pelvic Incidence
References
- Davis, D.D.; Foris, L.A.; Kane, S.M.; Waseem, M. Pelvic Fracture. StatPearls, S: Island (FL), 2021. [Google Scholar]
- Rommens, P.M.; Hofmann, A. Comprehensive classification of fragility fractures of the pelvic ring: Recommendations for surgical treatment. Injury 2013, 44, 1733–1744. [Google Scholar] [CrossRef]
- Grotz, M.R.; Allami, M.K.; Harwood, P.; Pape, H.C.; Krettek, C.; Giannoudis, P.V. Open pelvic fractures: epidemiology, current concepts of management and outcome. Injury 2005, 36, 1–13. [Google Scholar] [CrossRef]
- Isler, B.; Ganz, R. Classification of pelvic ring injuries. Injury 1996, 27 (Suppl. 1), S-a3–12. [Google Scholar] [CrossRef]
- Simonian, P.T.; Routt, M.L.; Jr Harrington, R.M.; Tencer, A.F. Internal fixation of the unstable anterior pelvic ring: a biomechanical comparison of standard plating techniques and the retrograde medullary superior pubic ramus screw. J. Orthop. Trauma. 1994, 8, 476–482. [Google Scholar] [CrossRef]
- Elzohairy, M.M.; Salama, A.M. Open reduction internal fixation versus percutaneous iliosacral screw fixation for unstable posterior pelvic ring disruptions. Orthop. Traumatol. Surg. Res. 2017, 103, 223–227. [Google Scholar] [CrossRef]
- Yinger, K.; Scalise, J.; Olson, S.A.; Bay, B.K.; Finkemeier, C.G. Biomechanical comparison of posterior pelvic ring fixation. J. Orthop. Trauma. 2003, 17, 481–487. [Google Scholar] [CrossRef]
- Kerschbaum, M.; Hausmann, N.; Worlicek, M.; Pfeifer, C.; Nerlich, M.; Schmitz, P. Patient-related outcome of unstable pelvic ring fractures stabilized with a minimal invasive screw-rod system. Health Qual. Life Outcomes 2017, 15, 248. [Google Scholar] [CrossRef]
- Yuan, B.M.; Huang, G.; Zheng, S.; Yu, T.; Zhao, J.W. A screw view model of navigation guided minimal invasive percutaneous pelvic screws insertion for lateral compression pelvic ring injuries: A case report. Medicine (Baltimore) 2020, 99, e21755. [Google Scholar] [CrossRef]
- Routt, M.L.; Jr Kregor, P.J.; Simonian, P.T.; Mayo, K.A. Early results of percutaneous iliosacral screws placed with the patient in the supine position. J. Orthop. Trauma. 1995, 9, 207–214. [Google Scholar] [CrossRef]
- Schweitzer, D.; Zylberberg, A.; Córdova, M.; Gonzalez, J. Closed reduction and iliosacral percutaneous fixation of unstable pelvic ring fractures. Injury 2008, 39, 869–874. [Google Scholar] [CrossRef]
- Wu, T.; Ren, X.; Cui, Y.; et al. Biomechanical study of three kinds of internal fixation for the treatment of sacroiliac joint disruption using biomechanical test and finite element analysis. J. Orthop. Surg. Res. 2018, 13, 152. [Google Scholar] [CrossRef] [PubMed]
- Toda, K.; Yagata, Y.; Kikuchi, T.; Takigawa, T.; Ito, Y. Minimally Invasive Surgery for Unstable Pelvic Ring Fractures: Transiliac Rod and Screw Fixation. Acta Med. Okayama 2020, 74, 27–32. [Google Scholar] [CrossRef] [PubMed]
- Allen, B.L.; Jr Ferguson, R.L. The Galveston technique for L rod instrumentation of the scoliotic spine. Spine (Phila. Pa. 1976) 1982, 7, 276–284. [Google Scholar] [CrossRef] [PubMed]
- Schwab, F.; Ungar, B.; Blondel, B.; et al. Scoliosis Research Society-Schwab adult spinal deformity classification: a validation study. Spine (Phila. Pa. 1976) 2012, 37, 1077–1082. [Google Scholar] [CrossRef] [PubMed]
- Kumaran, Y.; Nishida, N.; Tripathi, S.; et al. Effects of Sacral Slope Changes on the Intervertebral Disc and Hip Joint: A Finite Element Analysis. World Neurosurgery 2023. [Google Scholar] [CrossRef] [PubMed]
- Nishida, N.; Mumtaz, M.; Tripathi, S.; et al. The Effect of Posterior Lumbar Interbody Fusion in Lumbar Spine Stenosis with Diffuse Idiopathic Skeletal Hyperostosis: A Finite Element Analysis. World Neurosurgery 2023, 176, e371–e379. [Google Scholar] [CrossRef] [PubMed]
- Goel, V.K.; Grauer, J.N.; Patel, T.; et al. Effects of charité artificial disc on the implanted and adjacent spinal segments mechanics using a hybrid testing protocol. Spine (Phila. Pa. 1976) 2005, 30, 2755–2764. [Google Scholar] [CrossRef]
- Dalstra, M.; Huiskes, R.; van Erning, L. Development and validation of a three-dimensional finite element model of the pelvic bone. J. Biomech. Eng. 1995, 117, 272–278. [Google Scholar] [CrossRef]
- Momeni Shahraki, N.; Fatemi, A.; Goel, V.K.; Agarwal, A. On the Use of Biaxial Properties in Modeling Annulus as a Holzapfel-Gasser-Ogden Material. Front. Bioeng. Biotechnol. 2015, 3, 69. [Google Scholar] [CrossRef]
- Lindsey, D.P.; Kiapour, A.; Yerby, S.A.; Goel, V.K. Sacroiliac Joint Fusion Minimally Affects Adjacent Lumbar Segment Motion: A Finite Element Study. Int. J. Spine Surg. 2015, 9, 64. [Google Scholar] [CrossRef]
- Ivanov, A.A.; Kiapour, A.; Ebraheim, N.A.; Goel, V. Lumbar fusion leads to increases in angular motion and stress across sacroiliac joint: a finite element study. Spine (Phila. Pa. 1976) 2009, 34, E162–E169. [Google Scholar] [CrossRef]
- Joukar, A.; Shah, A.; Kiapour, A.; et al. Sex Specific Sacroiliac Joint Biomechanics During Standing Upright: A Finite Element Study. Spine (Phila. Pa. 1976) 2018, 43, E1053–e1060. [Google Scholar] [CrossRef]
- Tripathi, S. Finite element analyses of stabilization of sacral fractures (zone I Denis fracture) under one leg standing stance. University of Toledo;
- Nishida, N.; Mumtaz, M.; Tripathi, S.; et al. Biomechanical analysis of laminectomy, laminoplasty, posterior decompression with instrumented fusion, and anterior decompression with fusion for the kyphotic cervical spine. International Journal of Computer Assisted Radiology and Surgery 2022, 17, 1531–1541. [Google Scholar] [CrossRef]
- Nishida, N.; Tripathi, S.; Mumtaz, M.; et al. Soft Tissue Injury in Cervical Spine Is a Risk Factor for Intersegmental Instability: A Finite Element Analysis. World Neurosurgery 2022, 164, e358–e366. [Google Scholar] [CrossRef]
- Guerado, E.; Cervan, A.M.; Cano, J.R.; Giannoudis, P.V. Spinopelvic injuries. Facts and controversies. Injury 2018, 49, 449–456. [Google Scholar] [CrossRef]
- Zhang, L.; Peng, Y.; Du, C.; Tang, P. Biomechanical study of four kinds of percutaneous screw fixation in two types of unilateral sacroiliac joint dislocation: a finite element analysis. Injury 2014, 45, 2055–2059. [Google Scholar] [CrossRef]
- Turbucz, M.; Pokorni, A.J.; Bigdon, S.F.; et al. Patient-specific bone material modelling can improve the predicted biomechanical outcomes of sacral fracture fixation techniques: A comparative finite element study. Injury 2023, 54, 111162. [Google Scholar] [CrossRef]
- Engelmann, C. [Reconstructive surgery of the bronchi in inflammatory lesions]. Zentralbl Chir. 1989, 114, 286–296. [Google Scholar] [PubMed]
- Bastian, J.D.; Bergmann, M.; Schwyn, R.; Keel, M.J.; Benneker, L.M. Assessment of the Breakaway Torque at the Posterior Pelvic Ring in Human Cadavers. J. Invest. Surg. 2015, 28, 328–333. [Google Scholar] [CrossRef] [PubMed]
- Kim, C.H.; Kim, J.W. Plate versus sacroiliac screw fixation for treating posterior pelvic ring fracture: a Systematic review and meta-analysis. Injury 2020, 51, 2259–2266. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.W.; Oh, C.W.; Oh, J.K.; et al. The incidence of and factors affecting iliosacral screw loosening in pelvic ring injury. Arch. Orthop. Trauma. Surg. 2016, 136, 921–927. [Google Scholar] [CrossRef]
- Salazar, D.; Lannon, S.; Pasternak, O.; et al. Investigation of bone quality of the first and second sacral segments amongst trauma patients: concerns about iliosacral screw fixation. J. Orthop. Traumatol. 2015, 16, 301–308. [Google Scholar] [CrossRef]
- Moed, B.R.; Geer, B.L. S2 iliosacral screw fixation for disruptions of the posterior pelvic ring: a report of 49 cases. J. Orthop. Trauma. 2006, 20, 378–383. [Google Scholar] [CrossRef]
- Griffin, D.R.; Starr, A.J.; Reinert, C.M.; Jones, A.L.; Whitlock, S. Vertically unstable pelvic fractures fixed with percutaneous iliosacral screws: does posterior injury pattern predict fixation failure? J. Orthop. Trauma. 2006, 20 (Suppl. 1), S30–S36; [Google Scholar] [CrossRef]
- Eastman, J.G.; Shelton, T.J.; Routt, M.L.C.; Jr Adams, M.R. Posterior pelvic ring bone density with implications for percutaneous screw fixation. Eur. J. Orthop. Surg. Traumatol. 2021, 31, 383–389. [Google Scholar] [CrossRef]
- Wu, C.C.; Jin, H.M.; Yan, Y.Z.; et al. Biomechanical Role of the Thoracolumbar Ligaments of the Posterior Ligamentous Complex: A Finite Element Study. World Neurosurg. 2018, 112, e125–e133. [Google Scholar] [CrossRef]
- Rommens, P.M.; Arand, C.; Hofmann, A.; Wagner, D. When and How to Operate Fragility Fractures of the Pelvis? Indian. J. Orthop. 2019, 53, 128–137. [Google Scholar] [CrossRef] [PubMed]
- König, M.A.; Jehan, S.; Boszczyk, A.A.; Boszczyk, B.M. Surgical management of U-shaped sacral fractures: a systematic review of current treatment strategies. Eur. Spine J. 2012, 21, 829–836. [Google Scholar] [CrossRef]
- Chon, C.S.; Jeong, J.H.; Kang, B.; Kim, H.S.; Jung, G.H. Computational simulation study on ilio-sacral screw fixations for pelvic ring injuries and implications in Asian sacrum. Eur. J. Orthop. Surg. Traumatol. 2018, 28, 439–444. [Google Scholar] [CrossRef] [PubMed]
- Wakely, P.E.; Jr Giacomantonio, M. Fine needle aspiration cytology of metastatic malignant rhabdoid tumor. Acta Cytol. 1986, 30, 533–537. [Google Scholar] [PubMed]
- Jazini, E.; Klocke, N.; Tannous, O.; et al. Does Lumbopelvic Fixation Add Stability? A Cadaveric Biomechanical Analysis of an Unstable Pelvic Fracture Model. J. Orthop. Trauma. 2017, 31, 37–46. [Google Scholar] [CrossRef]
- Wenning, K.E.; Yilmaz, E.; Schildhauer, T.A.; Hoffmann, M.F. Comparison of lumbopelvic fixation and iliosacral screw fixation for the treatment of bilateral sacral fractures. J. Orthop. Surg. Res. 2021, 16, 604. [Google Scholar] [CrossRef]
- Virk, S.S.; Niedermeier, S.; Yu, E.; Khan, S.N. Adjacent segment disease. Orthopedics 2014, 37, 547–555. [Google Scholar] [CrossRef]
- Kumaran, Y.; Shah, A.; Katragadda, A.; et al. Iatrogenic muscle damage in transforaminal lumbar interbody fusion and adjacent segment degeneration: a comparative finite element analysis of open and minimally invasive surgeries. Eur. Spine J. 2021, 30, 2622–2630. [Google Scholar] [CrossRef] [PubMed]
- Halawi, M.J. Pelvic ring injuries: Surgical management and long-term outcomes. J. Clin. Orthop. Trauma. 2016, 7, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Zheng, Z.M.; Yu, B.S.; Chen, H.; et al. Effect of iliac screw insertion depth on the stability and strength of lumbo-iliac fixation constructs: an anatomical and biomechanical study. Spine (Phila. Pa. 1976) 2009, 34, E565–E572. [Google Scholar] [CrossRef] [PubMed]
- Akesen, B.; Wu, C.; Mehbod, A.A.; Sokolowski, M.; Transfeldt, E.E. Revision of loosened iliac screws: a biomechanical study of longer and bigger screws. Spine (Phila. Pa. 1976) 2008, 33, 1423–1428. [Google Scholar] [CrossRef] [PubMed]
Figure 1.
Intact female model developed from CT images of a female with no abnormalities or degenerative changes. 1a indicates the posterior view while 1b indicates the anterior view.
Figure 1.
Intact female model developed from CT images of a female with no abnormalities or degenerative changes. 1a indicates the posterior view while 1b indicates the anterior view.
Figure 2.
Simulation of the Rommens Type IIC pelvic ring fracture on the left side. The fracture was simulated by deleting the elements in the sacrum and ilium.
Figure 2.
Simulation of the Rommens Type IIC pelvic ring fracture on the left side. The fracture was simulated by deleting the elements in the sacrum and ilium.
Figure 3.
Stabilization of the pelvic ring fracture with various fracture fixation techniques. 3a indicates the L5-ilium fixation with cross connector (L5_PF_W_CC). 3b indicates the L5-ilium fixation without cross connector (L5_PF_WO_CC). 3c indicates the iliosacral screws at S1 and the trans-iliac-trans-sacral screw at S2 (S1_IS_S2_TITS). 3d indicates the trans-iliac-trans-sacral screw at both S1 and S2 (S1_TITS_S2_TITS). 3e indicates the double transiliac rod and screw fixation (DTSF).
Figure 3.
Stabilization of the pelvic ring fracture with various fracture fixation techniques. 3a indicates the L5-ilium fixation with cross connector (L5_PF_W_CC). 3b indicates the L5-ilium fixation without cross connector (L5_PF_WO_CC). 3c indicates the iliosacral screws at S1 and the trans-iliac-trans-sacral screw at S2 (S1_IS_S2_TITS). 3d indicates the trans-iliac-trans-sacral screw at both S1 and S2 (S1_TITS_S2_TITS). 3e indicates the double transiliac rod and screw fixation (DTSF).
Figure 4.
Comparison of sacrum fracture horizontal displacement at 7.5Nm moment with 400N follower load under two leg stance condition for five different pelvic ring fracture stabilization configurations. The vertical axis is the displacement in mm and the horizontal axis indicates the motions simulated.
Figure 4.
Comparison of sacrum fracture horizontal displacement at 7.5Nm moment with 400N follower load under two leg stance condition for five different pelvic ring fracture stabilization configurations. The vertical axis is the displacement in mm and the horizontal axis indicates the motions simulated.
Figure 5.
Comparison of sacrum fracture vertical displacement at 7.5Nm moment with 400N follower load under two leg stance condition for five different pelvic ring fracture stabilization configurations. The vertical axis is the displacement in mm and the horizontal axis indicates the motions simulated.
Figure 5.
Comparison of sacrum fracture vertical displacement at 7.5Nm moment with 400N follower load under two leg stance condition for five different pelvic ring fracture stabilization configurations. The vertical axis is the displacement in mm and the horizontal axis indicates the motions simulated.
Figure 6.
Comparison of Pubic Rami fracture horizontal displacement at 7.5Nm moment with 400N follower load under two leg stance condition for five different pelvic ring fracture stabilization configurations. The vertical axis is the displacement in mm and the horizontal axis indicates the motions simulated.
Figure 6.
Comparison of Pubic Rami fracture horizontal displacement at 7.5Nm moment with 400N follower load under two leg stance condition for five different pelvic ring fracture stabilization configurations. The vertical axis is the displacement in mm and the horizontal axis indicates the motions simulated.
Figure 7.
Comparison of Pubic Rami fracture vertical displacement at 7.5Nm moment with 400N follower load under two leg stance condition for five different pelvic ring fracture stabilization configurations. The vertical axis is the displacement in mm and the horizontal axis indicates the motions simulated.
Figure 7.
Comparison of Pubic Rami fracture vertical displacement at 7.5Nm moment with 400N follower load under two leg stance condition for five different pelvic ring fracture stabilization configurations. The vertical axis is the displacement in mm and the horizontal axis indicates the motions simulated.
Figure 8.
Comparison of right (contralateral to fracture site) SIJ ROM at 7.5Nm moment with 400N follower load under two leg stance condition for five different pelvic ring fracture stabilization configurations. The vertical axis is the angle in degrees and the horizontal axis indicates the motions simulated.
Figure 8.
Comparison of right (contralateral to fracture site) SIJ ROM at 7.5Nm moment with 400N follower load under two leg stance condition for five different pelvic ring fracture stabilization configurations. The vertical axis is the angle in degrees and the horizontal axis indicates the motions simulated.
Figure 9.
Comparison of L5-S1 ROM at 7.5Nm moment with 400N follower load under two leg stance condition for five different pelvic ring fracture stabilization configurations. The vertical axis is the angle in degrees and the horizontal axis indicates the motions simulated.
Figure 9.
Comparison of L5-S1 ROM at 7.5Nm moment with 400N follower load under two leg stance condition for five different pelvic ring fracture stabilization configurations. The vertical axis is the angle in degrees and the horizontal axis indicates the motions simulated.
Figure 10.
Comparison of L1-S1 ROM at 7.5Nm moment with 400N follower load under two leg stance condition for five different pelvic ring fracture stabilization configurations. The vertical axis is the angle in degrees and the horizontal axis indicates the motions simulated.
Figure 10.
Comparison of L1-S1 ROM at 7.5Nm moment with 400N follower load under two leg stance condition for five different pelvic ring fracture stabilization configurations. The vertical axis is the angle in degrees and the horizontal axis indicates the motions simulated.
Figure 11.
Comparison of L5-S1 Nucleus Stress at 7.5Nm moment with 400N follower load under two leg stance condition for five different pelvic ring fracture stabilization configurations. The vertical axis is the stress in MPa, and the horizontal axis indicates the motions simulated.
Figure 11.
Comparison of L5-S1 Nucleus Stress at 7.5Nm moment with 400N follower load under two leg stance condition for five different pelvic ring fracture stabilization configurations. The vertical axis is the stress in MPa, and the horizontal axis indicates the motions simulated.
Table 1.
Material properties assigned to the finite element model [14-17]. E represents.
Table 1.
Material properties assigned to the finite element model [14-17]. E represents.
| Component |
Material Properties |
Constitute Relation |
Element Type |
| Vertebral Cortical Bone |
E= 12000MPa |
Isotropic, Elastic |
8 Node Brick Element (C3D8) |
| v= 0.3 |
|
|
| Vertebral Cancellous Bone |
E= 100MPa |
Isotropic, Elastic |
4 Node Tetrahedral Element (C3D4) |
| v= 0.2 |
|
|
| Pelvis Cortical Bone (Sacrum, Ilium) |
E= 17000MPa |
Isotropic, Elastic |
4 Node Tetrahedral Element (C3D4) |
| v= 0.3 |
|
|
| Sacrum Cancellous Bone |
Heterogenous |
Isotropic, Elastic |
4 Node Tetrahedral Element (C3D4) |
| Ilium Cancellous Bone |
E= 70 MPa |
Isotropic, Elastic |
|
| |
v= 0.2 |
|
4 Node Tetrahedral Element (C3D4) |
| Femur Cortical Bone |
E= 17000MPa |
Isotropic, Elastic |
4 Node Tetrahedral Element (C3D4) |
| v= 0.29 |
|
|
| Femur Cancellous Bone |
E= 100 MPa |
Isotropic, Elastic |
4 Node Tetrahedral Element (C3D4) |
| v= 0.2 |
|
|
| Ground Substance of Annulus Fibrosis |
c10= 0.035 |
|
|
| k1= 0.296 |
Hyper elastic anisotropic (HGO) |
8 Node Brick Element (C3D8) |
| k2= 65 |
|
|
| Nucleus Pulposus |
E= 1 MPa |
Isotropic, Elastic |
8 Node Brick Element (C3D8) |
| |
v= 0.499 |
|
|
| Anterior Longitudinal |
7.8 MPa (<12%),
20 MPa (>12%) |
Non-linear Hypo elastic |
Truss Element (T3D2) |
| Posterior Longitudinal |
10 MPa (<11%),
20 MPa (>11%) |
Non-linear Hypo elastic |
Truss Element (T3D2) |
| Ligamentum Flavum |
15 MPa (<6.2%),
19.5 MPa (>6.2%) |
Non-linear Hypo elastic |
Truss Element (T3D2) |
| Intertransverse |
10 MPa (<18%),
58.7 MPa (>18%) |
Non-linear Hypo elastic |
Truss Element (T3D2) |
| Interspinous |
10 MPa (<14%),
11.6 MPa (>14%) |
Non-linear Hypo elastic |
Truss Element (T3D2) |
| Supraspinous |
8 MPa (<20%), 15
MPa (>20%) |
Non-linear Hypo elastic |
Truss Element (T3D2) |
| Capsular |
7.5 MPa (<25%),
32.9 MPa (>25%) |
Non-linear Hypo elastic |
Truss Element (T3D2) |
| Anterior SIJ |
125 MPa (5%), 325
MPa (>10%), 316
MPa (>15%) |
Non-linear Hypo elastic |
Truss Element (T3D2) |
| Short Posterior SI |
43 MPa (5%), 113
MPa (>10%), 110
MPa (>15%) |
Non-linear Hypo elastic |
Truss Element (T3D2) |
| Long Posterior SI |
150 MPa (5%), 391
MPa (>10%), 381
MPa (>15%) |
Non-linear Hypo elastic |
Truss Element (T3D2) |
| Interosseous |
40 MPa (5%), 105
MPa (>10%), 102
MPa (>15%) |
Non-linear Hypo elastic |
Truss Element (T3D2) |
| Sacrospinous |
304 MPa (5%), 792
MPa (>10%), 771
MPa (>15%) |
Non-linear Hypo elastic |
Truss Element (T3D2) |
| Sacrotuberous Ligament |
326 MPa (5%), 848
MPa (>10%), 826
MPa (>15%) |
Non-linear Hypo elastic |
Truss Element (T3D2) |
| Gluteus Maximus |
k = 344 N/mm |
|
Connector Element |
| Gluteus Medius |
k = 779 N/mm |
|
Connector Element |
| Gluteus Minimus |
k = 660 N/mm |
|
Connector Element |
| Psoas Major |
k = 100 N/mm |
|
Connector Element |
| Adductor Magnus |
k = 257 N/mm |
|
Connector Element |
| Adductor Longus |
k = 134 N/mm |
|
Connector Element |
| Adductor Brevis |
k = 499 N/mm |
|
Connector Element |
| Rods (Titanium) |
E= 120000 MPa |
Isotropic, Elastic |
Hexahedral Element |
| v=0.3 |
|
|
| Pedicle Screws (Titanium) |
E= 120000 MPa |
Isotropic, Elastic |
Hexahedral Element |
| v=0.3 |
|
|
Table 2.
Maximum von Mises Stress (MPa) on the implants for each motion simulated.
Table 2.
Maximum von Mises Stress (MPa) on the implants for each motion simulated.
| von Mises Stress (MPa) |
| |
Extension |
Flexion |
Left Bending |
Right Bending |
Left Rotation |
Right Rotation |
| L5_PF_W_CC |
310.2 |
251.7 |
368.8 |
209 |
279.3 |
266.8 |
| Left Rod |
Left Rod |
Left Rod |
Left Rod |
Left Rod |
Left Rod |
| Between L5 & ilium Tulip |
Between L5 & ilium Tulip |
Between L5 & ilium Tulip |
Between L5 & ilium Tulip |
Between L5 & ilium Tulip |
Between L5 & ilium Tulip |
L5_PF_WO_CC
|
308.2 |
287.9 |
403 |
212.4 |
307.6 |
307.3 |
| Left Rod |
Left Rod |
Left Rod |
Left Rod |
Left Rod |
Left Rod |
| Between L5 & ilium Tulip |
Between L5 & ilium Tulip |
Between L5 & ilium Tulip |
Between L5 & ilium Tulip |
Between L5 & ilium Tulip |
Between L5 & ilium Tulip |
| |
| S1_IS_S2_TITS |
114.2 |
132.1 |
155.3 |
86.17 |
154.8 |
168.2 |
| |
TITS |
TITS |
TITS |
TITS |
TITS |
TITS |
| S1_TITS_S2_TITS |
194 |
188.9 |
243.6 |
200.3 |
188.1 |
218.2 |
| |
Top TITS |
Top TITS |
Top TITS |
Top TITS |
Top TITS |
Top TITS |
| DTSF |
75.76 |
81.97 |
71.3 |
114.4 |
94.15 |
99.15 |
| Top Rod |
Top Rod |
Top Rod |
Top Rod |
Top Rod |
Top Rod |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).