Submitted:
29 January 2024
Posted:
30 January 2024
You are already at the latest version
Abstract
Keywords:
Introduction
Material and Methods
Study Protocol and Ethical Considerations
Study Aims and Objectives
Search Strategy
Inclusion and Exclusion Criteria
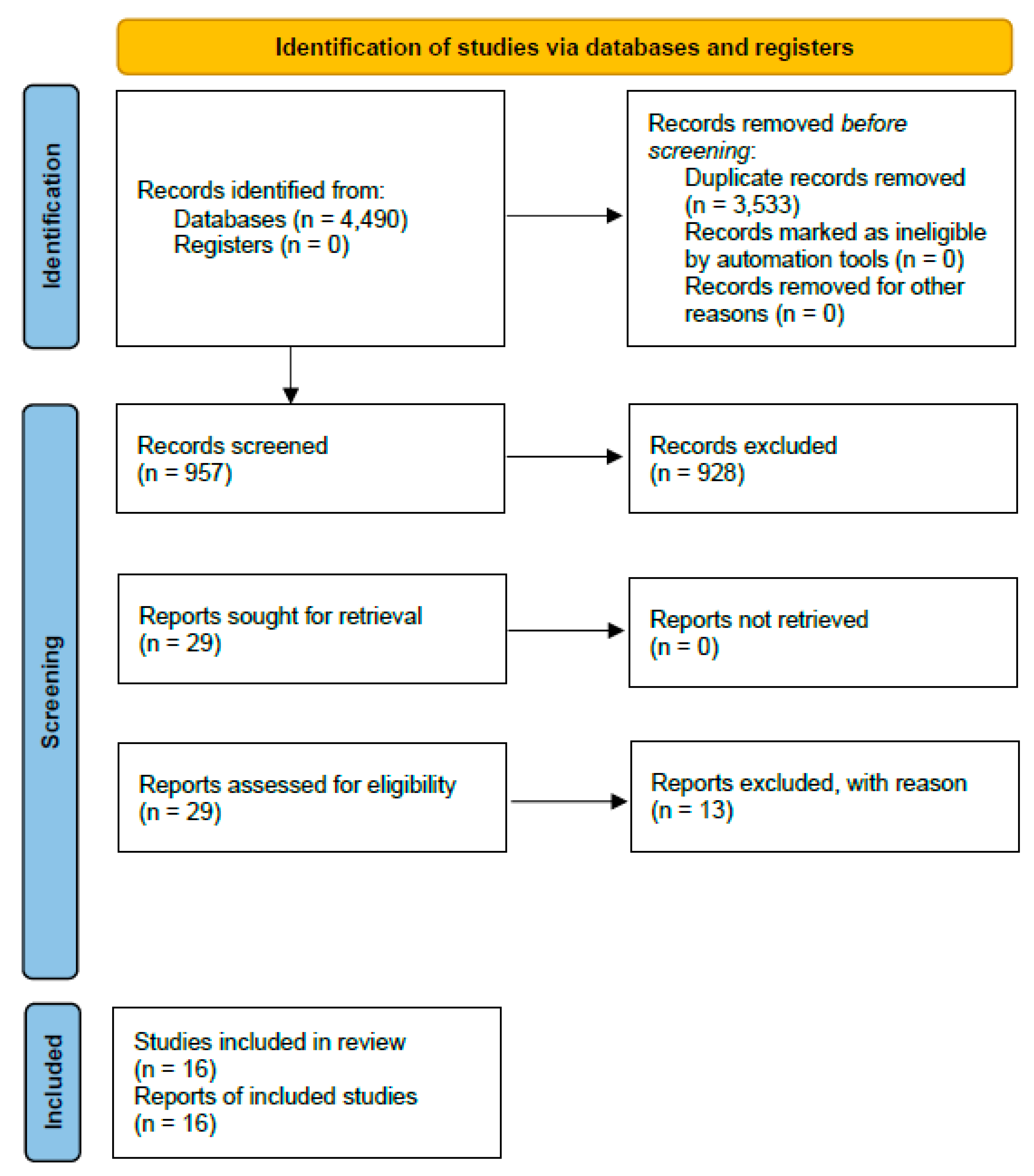
Selection and Identification Process of Eligible Studies
Data Synthesis and Finding Reporting
Gray Literature
Expected Study Outcomes
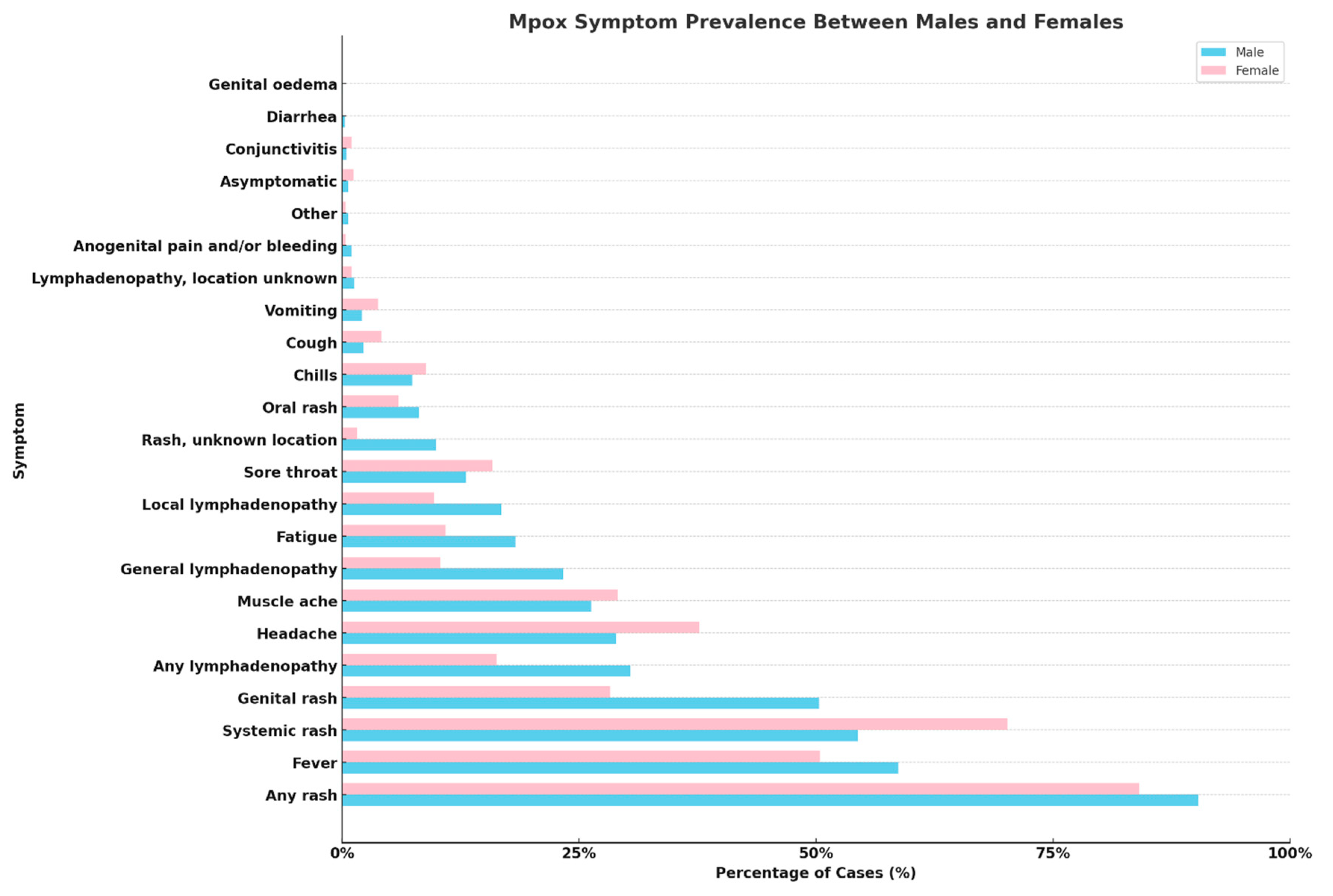
Results
Literature Search
Cohort Studies
Case Reports and Case Series
Case Series Review
Discussion
Future Directions
Conclusions
Acknowledgements
References
- Bunge EM, Hoet B, Chen L, Lienert F, Weidenthaler H, Baer LR, Steffen R. The changing epidemiology of human monkeypox-A potential threat? A systematic review. PLoS Negl Trop Dis. 2022 Feb 11;16(2):e0010141. [CrossRef]
- Muyembe-Tamfum JJ, Mulembakani P, Lekie RB, Szczeniowski M, Ježek Z, Doshi R, Hoff N, Rimoin AW. Smallpox and its eradication in the Democratic Republic of Congo: lessons learned. Vaccine. 2011 Dec 30;29 Suppl 4:D13-8. [CrossRef]
- Rimoin AW, Mulembakani PM, Johnston SC, Lloyd Smith JO, Kisalu NK, Kinkela TL, Blumberg S, Thomassen HA, Pike BL, Fair JN, Wolfe ND, Shongo RL, Graham BS, Formenty P, Okitolonda E, Hensley LE, Meyer H, Wright LL, Muyembe JJ. Major increase in human monkeypox incidence 30 years after smallpox vaccination campaigns cease in the Democratic Republic of Congo. Proc Natl Acad Sci U S A. 2010 Sep 14;107(37):16262-7. [CrossRef]
- Thornhill JP, Gandhi M, Orkin C. Mpox: The Reemergence of an Old Disease and Inequities. Annu Rev Med. 2023 Oct 3. [CrossRef] [PubMed]
- Ahmed SK, Mohamed MG, Dabou EA, Abuijlan I, Chandran D, El-Shall NA, Chopra H, Dhama K. Monkeypox (Mpox) in immunosuppressed patients. F1000Res. 2023 Feb 2;12:127. [CrossRef]
- Ogoina D, Damon I, Nakoune E. Clinical review of human Mpox. Clin Microbiol Infect. 2023 Dec;29(12):1493-1501. [CrossRef] [PubMed]
- Islam MM, Dutta P, Rashid R, Jaffery SS, Islam A, Farag E, Zughaier SM, Bansal D, Hassan MM. Pathogenicity and virulence of monkeypox at the human-animal-ecology interface. Virulence. 2023 Dec;14(1):2186357. [CrossRef]
- Zebardast A, Latifi T, Shafiei-Jandaghi NZ, Gholami Barzoki M, Shatizadeh Malekshahi S. Plausible reasons for the resurgence of Mpox (formerly Monkeypox): an overview. Trop Dis Travel Med Vaccines. 2023 Dec 25;9(1):23. [CrossRef]
- World Health Organization (WHO). WHO Director-General declares the ongoing monkeypox outbreak a Public Health Emergency of International Concern. 23 July 2022. Accessible at: https://www.who.int/europe/news/item/23-07-2022-who-director-general-declares-the-ongoing-monkeypox-outbreak-a-public-health-event-of-international-concern.
- Karagoz A, Tombuloglu H, Alsaeed M, Tombuloglu G, AlRubaish AA, Mahmoud A, Smajlović S, Ćordić S, Rabaan AA, Alsuhaimi E. Monkeypox (Mpox) virus: Classification, origin, transmission, genome organization, antiviral drugs, and molecular diagnosis. J Infect Public Health. 2023 Apr;16(4):531-541. [CrossRef]
- Borges V, Duque MP, Martins JV, Vasconcelos P, Ferreira R, Sobral D, Pelerito A, de Carvalho IL, Núncio MS, Borrego MJ, Roemer C, Neher RA, O'Driscoll M, Rocha R, Lopo S, Neves R, Palminha P, Coelho L, Nunes A, Isidro J, Pinto M, Santos JD, Mixão V, Santos D, Duarte S, Vieira L, Martins F, Machado J, Veríssimo VC, Grau B, Peralta-Santos A, Neves J, Caldeira M, Pestana M, Fernandes C, Caria J, Pinto R, Póvoas D, Maltez F, Sá AI, Salvador MB, Teófilo E, Rocha M, Moneti V, Duque LM, E Silva FF, Baptista T, Vasconcelos J, Casanova S, Mansinho K, Alves JV, Alves J, Silva A, Alpalhão M, Brazão C, Sousa D, Filipe P, Pacheco P, Peruzzu F, de Jesus RP, Ferreira L, Mendez J, Jordão S, Duarte F, Gonçalves MJ, Pena E, Silva CN, Guimarães AR, Tavares M, Freitas G, Cordeiro R, Gomes JP. Viral genetic clustering and transmission dynamics of the 2022 Mpox outbreak in Portugal. Nat Med. 2023 Oct;29(10):2509-2517. [CrossRef]
- Bragazzi NL, Kong JD, Wu J. Integrated epidemiological, clinical, and molecular evidence points to an earlier origin of the current monkeypox outbreak and a complex route of exposure. J Med Virol. 2023 Jan;95(1):e28244. [CrossRef] [PubMed]
- Limonta S, Lapadula G, Mezzadri L, Corsico L, Rovida F, Ranzani A, Baldanti F, Bonfanti P. Mpox Virus in the Pharynx of Men Having Sex with Men: A Case Series. Pathogens. 2024 Jan 20;13(1):92. [CrossRef] [PubMed]
- Thornhill JP, Barkati S, Walmsley S, Rockstroh J, Antinori A, Harrison LB, Palich R, Nori A, Reeves I, Habibi MS, Apea V, Boesecke C, Vandekerckhove L, Yakubovsky M, Sendagorta E, Blanco JL, Florence E, Moschese D, Maltez FM, Goorhuis A, Pourcher V, Migaud P, Noe S, Pintado C, Maggi F, Hansen AE, Hoffmann C, Lezama JI, Mussini C, Cattelan A, Makofane K, Tan D, Nozza S, Nemeth J, Klein MB, Orkin CM; SHARE-net Clinical Group. Monkeypox Virus Infection in Humans across 16 Countries - April-June 2022. N Engl J Med. 2022 Aug 25;387(8):679-691. 20 June. [CrossRef] [PubMed]
- Bragazzi NL, Kong JD, Mahroum N, Tsigalou C, Khamisy-Farah R, Converti M, Wu J. Epidemiological trends and clinical features of the ongoing monkeypox epidemic: A preliminary pooled data analysis and literature review. J Med Virol. 2023 Jan;95(1):e27931. [CrossRef] [PubMed]
- World Health Organization (WHO). 2022 Mpox (Monkeypox) outbreak: global trends. December 2023. Accessible at: https://worldhealthorg.shinyapps.io/mpx_global. Accessed on 28 January 2024.
- Lawry LL, Lugo-Robles R, McIver V. Overlooked sex and gender aspects of emerging infectious disease outbreaks: Lessons learned from COVID-19 to move towards health equity in pandemic response. Front Glob Womens Health. 2023 Feb 20;4:1141064. [CrossRef]
- Alvarez-Gómez AM, Vélez-Cuervo SM, Cardona-Maya WD. Monkey pox: importance in female sexual health. Rev Colomb Obstet Ginecol. 2023 Mar 30;74(1):87-89. English, Spanish. [CrossRef]
- Ghebreyesus TA, Allotey P, Narasimhan M. Advancing the "sexual" in sexual and reproductive health and rights: a global health, gender equality and human rights imperative. Bull World Health Organ. 2024 Jan 1;102(1):77-78. [CrossRef]
- Hoenig, LJ. Hoenig LJ. The Monkeypox Outbreak 2022: Women and Children Patients. Skinmed. 2022 Oct 31;20(5):334-335. [PubMed]
- Khalil A, Samara A, Ladhani S, O'Brien P. Monkeypox and pregnancy: time for global surveillance and prevention strategies. Lancet. 2022 Oct 8;400(10359):1193. [CrossRef]
- Pomar L, Favre G, Baud D. Monkeypox infection during pregnancy: European registry to quantify maternal and fetal risks. Ultrasound Obstet Gynecol. 2022 Sep;60(3):431. [CrossRef] [PubMed]
- Rodriguez-Morales AJ, Amer FA. Monkeypox virus infection in women and non-binary people: uncommon or neglected? Lancet. 2022 Dec 3;400(10367):1903-1905. [CrossRef]
- Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, Shekelle P, Stewart LA; PRISMA-P Group. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015 Jan 1;4(1):1. [CrossRef]
- Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, McGuinness LA, Stewart LA, Thomas J, Tricco AC, Welch VA, Whiting P, Moher D. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021 Mar 29;372:n71. [CrossRef]
- Oakley LP, Hufstetler K, O'Shea J, Sharpe JD, McArdle C, Neelam V, Roth NM, Olsen EO, Wolf M, Pao LZ, Gold JAW, Davis KM, Perella D, Epstein S, Lash MK, Samson O, Pavlick J, Feldpausch A, Wallace J, Nambiar A, Ngo V, Halai UA, Richardson CW, Fowler T, Taylor BP, Chou J, Brandon L, Devasia R, Ricketts EK, Stockdale C, Roskosky M, Ostadkar R, Vang Y, Galang RR, Perkins K, Taylor M, Choi MJ, Weidle PJ, Dawson P, Ellington S; CDC Mpox Analytics Team. Mpox Cases Among Cisgender Women and Pregnant Persons - United States, May 11-November 7, 2022. MMWR Morb Mortal Wkly Rep. 2023 Jan 6;72(1):9-14. [CrossRef]
- Sánchez Doncell J, Lemos M, Francos J JL, González Montaner P. Viruela símica: características en población femenina, Buenos Aires, Argentina [Monkeypox: characteristics in female population, Buenos Aires, Argentina]. Medicina (B Aires). 2024;84(1):143-147. Spanish. [PubMed]
- Coutinho C, Secco Torres Silva M, Torres TS, Peixoto E, Avelar Magalhães M, Wagner Cardoso S, Nazário G, Mendonça M, Menezes M, Almeida PM, Dias de Brito de Carvalho PR, Bia Bedin S, Almeida AM, Carvalho S, Gonçalves Veloso V, Grinsztejn B, Velasque L; INI-Fiocruz Mpox Study Group. Characteristics of women diagnosed with Mpox infection compared to men: A case series from Brazil. Travel Med Infect Dis. 2023 Nov-Dec;56:102663. [CrossRef] [PubMed]
- Grothe JH, Cornely OA, Salmanton-García J; VACCELERATE consortium. Monkeypox in children and adult women in Europe: Results from a flash VACCELERATE pilot survey. Enferm Infecc Microbiol Clin (Engl Ed). 2023 May;41(5):309-311. [CrossRef]
- Vallejo-Plaza A, Rodríguez-Cabrera F, Hernando Sebastián V, Guzmán Herrador BR, Santágueda Balader P, García San Miguel Rodríguez-Alarcón L, Díaz Franco A, Garzón Sánchez A, Sierra Moros MJ; Spanish Monkeypox Response Network; Simón Soria F, Suárez Rodríguez B. Mpox (formerly monkeypox) in women: epidemiological features and clinical characteristics of Mpox cases in Spain, April to November 2022. Euro Surveill. 2022 Dec;27(48):2200867. [CrossRef]
- Thornhill JP, Palich R, Ghosn J, Walmsley S, Moschese D, Cortes CP, Galliez RM, Garlin AB, Nozza S, Mitja O, Radix AE, Blanco JL, Crabtree-Ramirez B, Thompson M, Wiese L, Schulbin H, Levcovich A, Falcone M, Lucchini A, Sendagorta E, Treutiger CJ, Byrne R, Coyne K, Meyerowitz EA, Grahn AM, Hansen AE, Pourcher V, DellaPiazza M, Lee R, Stoeckle M, Hazra A, Apea V, Rubenstein E, Jones J, Wilkin A, Ganesan A, Henao-Martínez AF, Chow EJ, Titanji BK, Zucker JE, Ogoina D, Orkin CM; Share-Net writing group. Human monkeypox virus infection in women and non-binary individuals during the 2022 outbreaks: a global case series. Lancet. 2022 Dec 3;400(10367):1953-1965. [CrossRef]
- Mancha D, Brazão C, Filipe P. Oro-mammary inoculation pathway of monkeypox in a female patient. J Eur Acad Dermatol Venereol. 2023 May;37(5):e636-e637. [CrossRef] [PubMed]
- Cole J, Choudry S, Kular S, Payne T, Akili S, Callaby H, Gordon NC, Ankcorn M, Martin A, Hobson E, Tunbridge AJ. Monkeypox encephalitis with transverse myelitis in a female patient. Lancet Infect Dis. 2023 Mar;23(3):e115-e120. [CrossRef]
- Ezzat D, Barcellini B, Meier J, Duc-Ha E, Mathis J. Ulcerating vulvar lesions revealing a rare female case of monkeypox in Switzerland. AJOG Glob Rep. 2023 Feb;3(1):100155. [CrossRef]
- van Hennik MM, Petrignani MWF. Klinische presentatie van monkeypox bij de vrouw [Clinical presentation of monkeypox in women]. Ned Tijdschr Geneeskd. 2022 Nov 15;166:D7082. Dutch. [PubMed]
- Napoli E, Frizzell M, Gravell C, Vallejo S, Theodore S, Chen K, Siddiqui H, Dunn J, Marrufo D, Cadena J, Danaher PJ. Eczema Monkeypoxicum in a Female Patient With Atopic Dermatitis. Open Forum Infect Dis. 2023 Feb 10;10(3):ofad072. [CrossRef]
- Ogoina D, James IH. Mpox in a female sex worker in Nigeria: A case report. IJID Reg. 2022 Dec 14;7:143-145. [CrossRef]
- Sampson MM, Magee G, Schrader EA, Dantuluri KL, Bukhari A, Passaretti C, Temming L, Leonard M, Philips JB, Weinrib D. Mpox (Monkeypox) Infection During Pregnancy. Obstet Gynecol. 2023 May 1;141(5):1007-1010. [CrossRef] [PubMed]
- Renfro ZT, Contag CA, Lu J, Solis D, Huang C, Sahoo MK, Yamamoto F, Mah J, Jones MS, Lin J, Levy V, Pinsky BA. Two cases of MPXV infection during pregnancy in heterosexual cisgender women without classic cutaneous lesions, Northern California, 2022. IDCases. 2023 Aug 21;33:e01881. [CrossRef]
- Dung NT, Hung LM, Hoa HTT, Nga LH, Hong NTT, Thuong TC, Ngoc NM, Ny NTH, Quy VT, Thoa VTK, Thanh NT, Tho PV, Toan LM, Quang VM, Man DNH, Phat NT, Phuong TTL, Tam TTT, Thoa PTN, Tam NH, Lan TTT, Thanh TT, Maurer-Stroh S, Khanh LTT, Yen LM, Hung NH, Thwaites G, Tung NLN, Thwaites L, Chau NVV, Anh NT, Van Tan L. Monkeypox Virus Infection in 2 Female Travelers Returning to Vietnam from Dubai, United Arab Emirates, 2022. Emerg Infect Dis. 2023 Apr;29(4):778-781. [CrossRef]
- Schwartz DA, Pittman PR. Mpox (Monkeypox) in Pregnancy: Viral Clade Differences and Their Associations with Varying Obstetrical and Fetal Outcomes. Viruses. 2023 Jul 28;15(8):1649. [CrossRef]
- Bragazzi NL, Khamisy-Farah R, Tsigalou C, Mahroum N, Converti M. Attaching a stigma to the LGBTQI+ community should be avoided during the monkeypox epidemic. J Med Virol. 2023 Jan;95(1):e27913. [CrossRef] [PubMed]
- Tascini C, Geminiani M, Sbrana F, Pagotto A, Martini L. Possible tattoo-transmitted monkeypox viral infection. Intern Emerg Med. 2022 Nov;17(8):2421-2422. [CrossRef]
- Del Río García V, Palacios JG, Morcillo AM, Duran-Pla E, Rodríguez BS, Lorusso N. Monkeypox outbreak in a piercing and tattoo establishment in Spain. Lancet Infect Dis. 2022 Nov;22(11):1526-1528. [CrossRef]
- Viedma-Martinez M, Dominguez-Tosso FR, Jimenez-Gallo D, Garcia-Palacios J, Riera-Tur L, Montiel-Quezel N, Linares-Barrios M. MPXV Transmission at a Tattoo Parlor. N Engl J Med. 2023 Jan 5;388(1):92-94. [CrossRef] [PubMed]
- Beaumont AL, Raphaël E, Bertin C, Lariven S, Peiffer-Smadja N. Mpox lesions on a tattoo. Lancet Infect Dis. 2023 Jun;23(6):762. [CrossRef] [PubMed]
- Tascini C, Sbrana F, Giuliano S, Geminiani M, Pagotto A. Monkeypox virus transmission in tattoo parlor. New Microbiol. 2023 Sep;46(3):315-316. [PubMed]
- Mbala PK, Huggins JW, Riu-Rovira T, Ahuka SM, Mulembakani P, Rimoin AW, Martin JW, Muyembe JT. Maternal and Fetal Outcomes Among Pregnant Women With Human Monkeypox Infection in the Democratic Republic of Congo. J Infect Dis. 2017 Oct 17;216(7):824-82. [CrossRef] [PubMed]
- Schwartz DA, Mbala-Kingebeni P, Patterson K, Huggins JW, Pittman PR. Congenital Mpox Syndrome (Clade I) in Stillborn Fetus after Placental Infection and Intrauterine Transmission, Democratic Republic of the Congo, 2008. Emerg Infect Dis. 2023 Nov;29(11):2198-2022. [CrossRef]
- Cono J, Cragan JD, Jamieson DJ, Rasmussen SA. Prophylaxis and treatment of pregnant women for emerging infections and bioterrorism emergencies. Emerg Infect Dis. 2006 Nov;12(11):1631-7. [CrossRef]
- Kopanou Taliaka P, Tsantes AG, Konstantinidi A, Liakou P, Tavoulari EF, Piovani D, Bonovas S, Iacovidou N, Tsantes AE, Sokou R. Monkeypox disease and pregnancy. Where are we today? A review of literature. J Perinatol. 2023 Apr;43(4):417-423. [CrossRef] [PubMed]
- Mattar R, Neto ARB, Luz AG, Hatanaka A, Zaconeta A, Guazzelli CAF, Traina E, Baptista FS, Osanan G, Duarte G, Ramos JGL, Oppermann ML, Francisco RPV, Cardoso SMLQ, Quintana SM, Sun SY, Borges VTM. Expert Recommendations on Monkeypox (MPX) in Pregnancy, Postpartum and Lactating Women. Rev Bras Ginecol Obstet. 2022 Dec;44(12):1122-1125. [CrossRef]
- Dashraath P, Nielsen-Saines K, Mattar C, Musso D, Tambyah P, Baud D. Guidelines for pregnant individuals with monkeypox virus exposure. Lancet. 2022 Jul 2;400(10345):21-22. [CrossRef]
- Dashraath P, Nielsen-Saines K, Rimoin A, Mattar CNZ, Panchaud A, Baud D. Monkeypox in pregnancy: virology, clinical presentation, and obstetric management. Am J Obstet Gynecol. 2022 Dec;227(6):849-861.e7. [CrossRef]
| Search criteria | Brief description |
|---|---|
| Population | Women affected by Mpox, including cisgender and transgender women, and non-binary individuals assigned female at birth |
| Exposure | Infection with Mpox virus |
| Comparator | Men (either cisgender or transgender, and non-binary individuals assigned male at birth) |
| Outcome | Clinical manifestations of Mpox, epidemiological features, transmission routes, treatment responses |
| Study Design | Cohort studies, case reports, cross-sectional studies, online surveys focusing on Mpox in the specified population |
| Keywords | (Monkeypox OR Mpox) AND (women OR woman OR female* OR male-to-female OR transwoman OR transwomen OR pregnant OR pregnancy OR lactation OR breastfeeding OR postpartum) |
| Databases Searched | MEDLINE/PubMed, Scopus, Web of Science, EMBASE |
| Hand-searched target journals | AJOG Glob Rep: Emerg Infect Dis; Enferm Infecc Microbiol Clin; Euro Surveill; IDCases; IJID Reg; J Eur Acad Dermatol Venereol; Lancet; Lancet Infect Dis; MMWR Morb Mortal Wkly Rep; Medicina (B Aires); Ned Tijdschr Geneeskd; Obstet Gynecol; Open Forum Infect Dis; Travel Med Infect Dis; Viruses |
| Gray literature | WHO, PHAC, CDC, ECDC, UKHSA |
| Study | Study location | Study type | Participant details | Main findings | Specific observations |
|---|---|---|---|---|---|
| Oakley et al. [26] | USA | Cohort Study | 769 cisgender women, including 23 pregnant individuals (21 cases of Mpox during pregnancy and 2 within 3 weeks of pregnancy) | Predominant impact on specific ethnic groups; sexual or intimate contact as primary transmission route | Cases among pregnant women; some required hospitalization |
| Sánchez Doncell et al. [27] | Argentina | Retrospective Analysis | 3 women, including 2 cisgender women, and 1 transgender woman | Low incidence among women; focus on sexual health impacts | No complications reported; symptoms included headache, myalgias, fever |
| Coutinho et al. [28] | Brazil | Surveillance Data | 108 women (cisgender and transgender), 10 non-binary persons | Older women, more non-sexual contact, fewer genital lesions, lower HIV prevalence compared to men | Hospitalizations but no deaths among women |
| Grothe et al. [29] | Europe | Online Survey | Women across Spain and Belgium, among others | Higher likelihood of infection in Spain and Portugal | Disparities in diagnosis delays and clinical manifestations between genders |
| Vallejo-Plaza et al. [30] | Spain | Surveillance data analysis | Both men and women with Mpox cases reported in Spain | Women constituted 2.1% of total Mpox cases, showing a younger median age compared to men The primary route of transmission was close contact during sexual relations for both genders, but women also had significant other transmission routes |
Women experienced longer diagnosis delays Women showed different symptom patterns and risk profiles |
| Thornhill et al., [31] | Global (15 countries) | Data Collection | 136 cisgender and transgender women, non-binary individuals | High HIV prevalence among trans women; many contracted virus through sexual contact | Misdiagnosis in a significant portion; majority presented with anogenital rash |
| Mancha et al. [32]; Cole et al. [33]; Ezzat et al. [34]; van Hennik and Petrignani [35]; Napoli et al. [36]; Ogoina and James [37]; Sampson et al. [38]; Renfro et al. [39]; Dung et al. [40] | Globally (various case Reports) | Case Reports | Individual women cases | Unusual transmission routes; severe complications in some cases | Diversity in clinical manifestations and transmission routes highlighted |
| Schwartz and Pittman [41] | Globally (various case reports) | Review of 58 cases | Cases of pregnant women positive for Mpox infection during the 2022–2023 outbreak | No documented cases of negative outcomes Absence of complications linked to Mpox Clade IIb |
Mpox clade could influence the severity of the infection and its impact on pregnancy and fetal health |
| Study | Patient Profile | Transmission Route | Clinical Presentation | Treatment and Outcome |
|---|---|---|---|---|
| Mancha et al. [29] | 30-year-old female, Fitzpatrick phototype III | Oro-mammary sex | Erythematous papule on left nipple evolving into flat ulceration with hemorrhagic crust and umbilicated pustules; fever, lymphadenopathy | Symptomatic care, topical fusidic acid; recovered |
| Cole et al. [30] | 35-year-old White, apparently healthy woman from the UK | Unprotected sex | Severe genital lesions, systemic symptoms, encephalitis, longitudinally extensive transverse myelitis | Antivirals (tecovirimat, cidofovir), analgesia, antibiotics, steroids, plasma exchange; remarkable neurological recovery |
| Ezzat et al. [31] | 31-year-old female in Switzerland | Not specified | Painful vulvar lesions, generalized Mpox lesions | Initial misdiagnosis; confirmed Mpox through PCR; treatment details not specified |
| van Hennik and Petrignani [32] | 57-year-old female, partner of a bisexual man | Close contact | Lesions at vaginal opening | Symptom duration and treatment not detailed |
| Napoli et al. [33] | 28-year-old woman with gastroesophageal reflux, untreated atopic dermatitis | Not specified, recent tattoo | Intense ear pain, multiple vesiculopustular lesions | Oral tecovirimat; complications included pain, GI distress, bacterial superinfection, AKI, anemia |
| Ogoina and James [34] | 24-year-old Nigerian female sex worker | Sexual contact | Fever, vesiculopustular lesions on groin and genital area | Not specified |
| Sampson et al. [35] | 20-year-old pregnant woman at 31 weeks of gestation | Sexual contact | Vaginal discharge, bleeding, painful urination, labial ulcer, herpes-like rash | Tecovirimat and acyclovir; stable condition, discharged, lesions resolved |
| Renfro et al. [36] | Two pregnant, heterosexual cisgender women | Not specified | Vaginal itching, chorioamnionitis during childbirth | Induced labor, antibiotics for chorioamnionitis; details of Mpox treatment not specified |
| Dung et al. [37] | Two women, 35 and 38 years old, traveled from UAE to Vietnam | Sexual contact | Fever, maculopapular rash | Isolation, oral acyclovir for co-infection in Patient 1; treatment for Patient 2 not specified |
| Research area | Recommendations | Suggestions |
|---|---|---|
| Transmission Dynamics.. | Conduct studies focusing on non-sexual transmission routes and environmental factors | Collaborate with community organizations to reach diverse populations |
| Clinical Manifestations. | Investigate unique clinical manifestations in women, especially those with underlying health conditions | Develop specialized training for healthcare providers on recognizing and managing Mpox in women |
| Mpox in Pregnancy | Systematically document Mpox outcomes in pregnant women to inform management guidelines | Engage obstetric and gynecological associations to develop and disseminate guidelines |
| Impact on Transgender Women and Non-Binary Individuals | Address the lack of data for transgender women and non-binary individuals, focusing on their specific health needs | Include transgender and non-binary individuals in research and public health campaigns |
| Genomic Monitoring | Implement genomic analysis to track virus evolution and its implications for treatment and vaccine efficacy | Coordinate with international health organizations for data sharing and joint research initiatives |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





