Introduction
Community-based efforts are crucial in the continuing worldwide fight against HIV/AIDS since they have a major role in increasing awareness and avoiding the transmission of the infection. These efforts enable people and communities to assume control over their health, promoting a feeling of shared accountability. This article delves into the significance of community-based HIV awareness and prevention, emphasising essential tactics and instances of success. Community-based initiatives play a crucial role in diminishing the social stigma surrounding HIV and encouraging preventive measures via their emphasis on education, testing, and support services.
Phase 1: Social Diagnosis
These networks provide a medium for people to exchange experiences, get information, and seek emotional assistance. The creation of support networks greatly benefits communities impacted by HIV. By facilitating the connection of individuals living with HIV to support groups, communities enhance their ability to withstand and recover from adversity, while also promoting a feeling of inclusion and acceptance (Shamu et al. 2020). By engaging community members in decision-making processes and leadership positions, people develop a feeling of ownership in the battle against HIV/AIDS. Community-based projects provide empowerment as a fundamental result. This empowerment not only enhances the long-term viability of preventive initiatives but also serves to confront the underlying systemic factors that lead to the transmission of the virus.
Cooperation with community leaders, healthcare professionals, and non-governmental organisations (NGOs) is one strategy. Interviews, questionnaires, and focus groups will be used to get a better understanding of community dynamics to carry out a social diagnostic for HIV prevention.
I will use local languages and community venues to collect data in a culturally appropriate manner. A specialised education programme will help low-income women overcome linguistic obstacles and learn new concepts in a way that is easy for them to understand.
Assessing vulnerabilities, such women contracting HIV from male relationships, is an important aspect of identifying gaps. Through peer-led initiatives, community seminars, and targeted outreach, these women will get vital knowledge about HIV prevention and its consequences (Girum T. et all, in 2018).
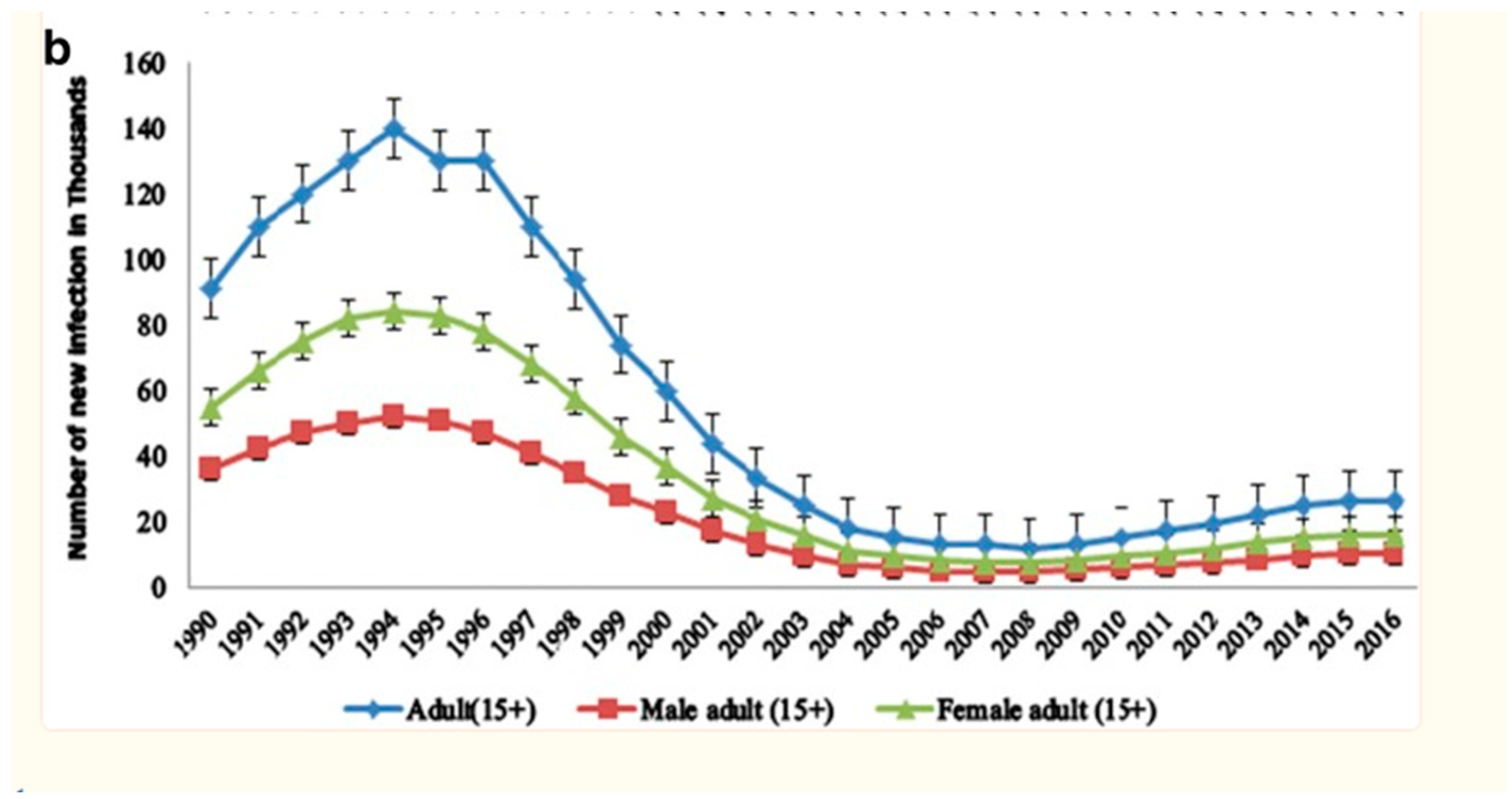
Figure 1.
Gender disparities. Souces; Girum T. et all in (2018).
Figure 1.
Gender disparities. Souces; Girum T. et all in (2018).
Phase 2: Epidemiological Diagnosis
Community-based HIV testing and counselling services are essential elements of preventative initiatives. Providing anonymous and non-judgmental testing promotes greater awareness of individuals’ HIV status, facilitating prompt intervention and treatment. These services, often offered in nearby health centres or via mobile units, bring testing closer to patients who may have obstacles in accessing conventional healthcare facilities (Ayon et al. 2019).
General population HIV prevalence was 710,000 (570,000-880,000) in 2016. In 91.5% (650,000) instances, people over 15 were affected. 400,000 (61.5%) of 650,000 adult HIV cases were female. HIV/AIDS is 1.1% (0.8-1.3%) among persons aged 15-49, with 0.8% (0.6-1%) among males and 1.3% (1-1.7%) among women. Teenage girls (10-19) and young women (15-24) made up 52.3% and 57.5% of the 67,000 and 87,000 cases, respectively.
South Africa has a large HIV population and one of the world’s highest HIV prevalence rates, according to my most recent report. Nearly 38 million individuals throughout the world were HIV positive in 2019, as reported by UNAIDS. It is crucial to consult the most recent statistics as the situation may have changed. The HIV/AIDS epidemic was particularly severe in a number of sub-Saharan African nations, including Mozambique, Lesotho, and Eswatini. Socioeconomically disadvantaged people and other vulnerable communities may be at a greater risk. A large portion of the spread of HIV is attributable to socioeconomic variables, such as low income and inadequate access to healthcare and education. It is more common for women than males in several nations, particularly those in sub-Saharan Africa. Different locations and genders may have different HIV prevalence rates.
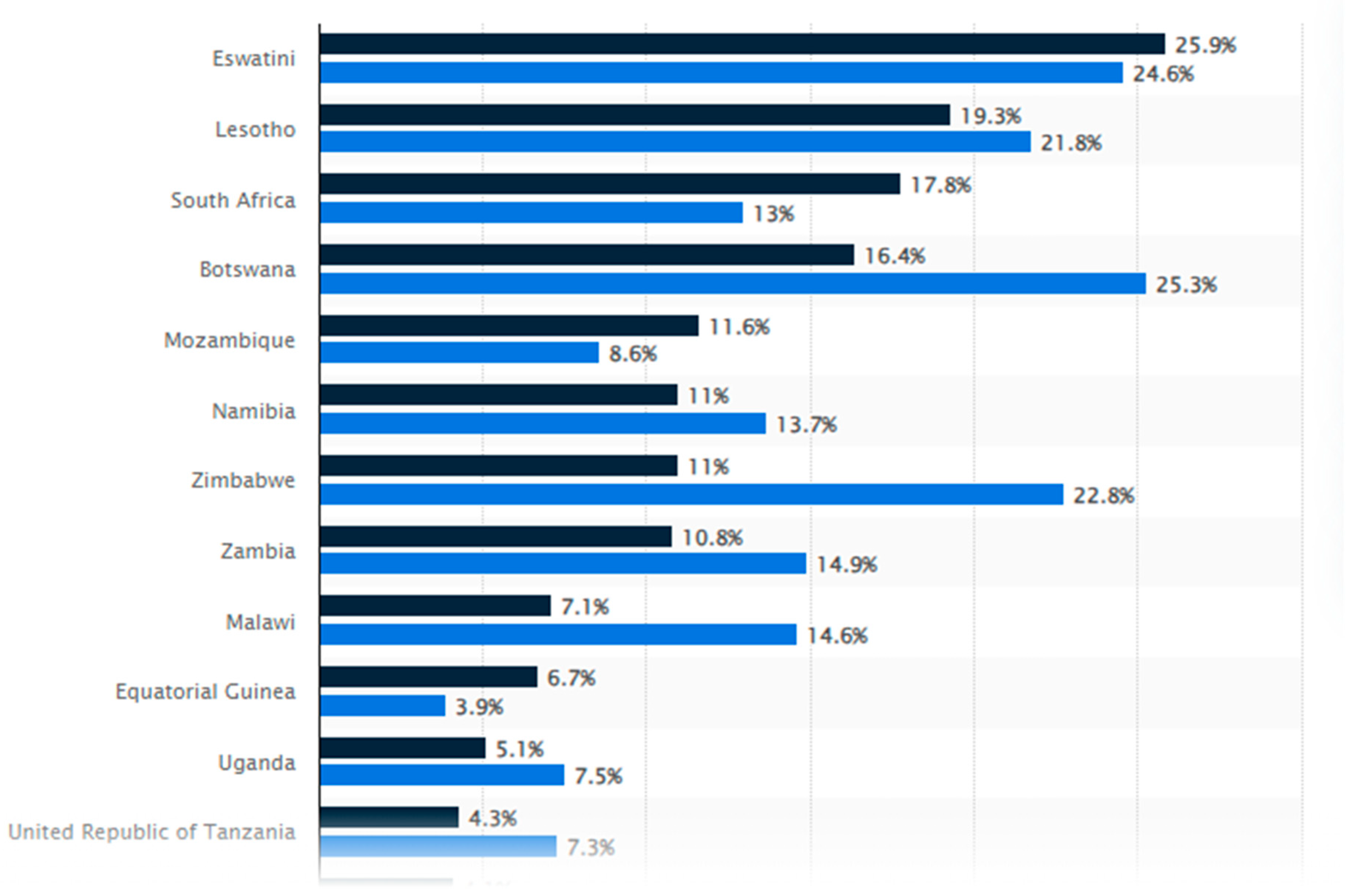
Figure 2.
Ranking of countries with the highest prevalence of HIV. Sources; Daniil F.in (2021).
Figure 2.
Ranking of countries with the highest prevalence of HIV. Sources; Daniil F.in (2021).
Eswatini had the highest HIV prevalence in 2022 at about 26%. HIV prevalence has dropped in Zimbabwe and other nations. HIV is most prevalent in sub-Saharan Africa. The highest HIV rates are in Eswatini, Lesotho, and South Africa. Community-based HIV programmes are crucial to prevention and treatment (Daniil F.in 2021).
Phase 3: Behavioural and Environmental Diagnosis
Community members who have received training serve as environmental counsellors, demonstrating cultural competency and a deep awareness of local circumstances, which in turn promotes trust among community members. Giving emotional assistance to persons living with HIV and delivering preventative recommendations to those who are at risk.
Certain Groups Fail to Recognise the Problem
There may be less open dialogue and more quiet on HIV/AIDS as a result of the stigmatisation of the illness. Inadequate education, cultural taboos, or a lack of knowledge may cause certain communities to be unaware.
Factors Affecting the Frequency of Infections
Individual behaviours and infection susceptibility are significantly influenced by environmental variables, such as healthcare accessibility, education level, and socioeconomic status. Risk factors for HIV transmission include not using condoms, abusing substances, and having several sexual partners.
Restrictions on the Use of Protection
Social norms and a lack of knowledge regarding the efficacy of preventative measures may lead to insufficient protection use. People may not always use protection due to sociocultural issues, limited access to contraception, or financial limitations.
Phase 4: Educational and Organizational Diagnosis
Community leaders, educators, and healthcare experts work together to provide precise information on the virus, mechanisms of transmission, and measures for prevention. Education is the fundamental basis for community-based HIV awareness and prevention. This educational effort has the purpose of debunking misconceptions and equipping people with the necessary information to safeguard themselves and their communities (Larson et al. 2019). Education not only focuses on vulnerable populations, but also seeks to eradicate the widespread social disapproval associated with HIV/AIDS, promoting candid discussions and diminishing prejudice. These activities provide secure environments for open conversation, cultivating a setting where people feel at ease in their pursuit of knowledge and assistance. Community-driven workshops, awareness campaigns, and peer-led conversations are efficacious means of spreading knowledge.
There are things that make people more likely to engage in certain health behaviours; these are called predisposing factors. For the purpose of raising HIV/AIDS awareness
It is possible to influence behaviour for the better by stressing that preventative steps are relevant to everyone, irrespective of their perceived risk. An individual's self-perception of their susceptibility to HIV infection may have a role in their susceptibility.
Addressing knowledge gaps and increasing the tendency towards preventive actions may be achieved via targeted education. A person's propensity to engage in healthful practises is inversely proportional to their degree of knowledge on HIV, its transmission, and preventative strategies.
More people will participate and accept the awareness programme if it is tailored to their cultural beliefs. Norms and attitudes on sexual health in a culture might impact a person's propensity.
- 2.
Reinforcement Factors
Factors that provide positive reinforcement: These are the things that make people more likely to engage in healthful behaviour.
First-hand Experiences: People are more likely to take action after hearing personal stories and testimonies. First-hand accounts, particularly those of people who have successfully adopted healthy habits, serve as potent reinforcement.
The value of preventative actions may be reinforced via the recognition and reward of healthy behaviours. Offering incentives, like free check-ups or community recognition, is a great way to encourage people to become healthy.
Support from the Community: Establishing a nurturing atmosphere encourages ongoing participation. People are more likely to engage in protective behaviours when they get positive reinforcement from their community, which includes family, friends, and leaders in the area.
- 3.
Enabling Factors
Resources and capacities that make it easier to adopt health behaviours are called enabling factors:
Enabling elements include educational programmes and skill-building endeavours. The best way to encourage people to take preventative actions is to provide them with the education and training they need to accomplish so.
It is critical to make sure people can get their hands on the materials they need. Condoms and other preventative instruments should be easily accessible and affordable in order to eliminate financial and other obstacles to their widespread use. Services that are established in the community and mobile clinics make them more accessible. Making medical treatment and diagnostic testing more accessible encourages people to take an active role in their own healthcare.
- 4.
Predisposing, Reinforcing, and Enabling (PRE) Analysis
A thorough evaluation of these aspects is involved in conducting a PRE analysis. The effectiveness of the awareness programme may be enhanced by carefully analysing each aspect to determine its strengths and areas that need development. It provides a strategic perspective on the community's ability and readiness to embrace the targeted health behaviours. In order to increase the program's efficacy in promoting good health behaviours and avoiding HIV, the analysis is used to generate focused interventions that address particular predispositions, leverage reinforcing variables, and boost enabling factors.
Phase 5: Administrative and Policy Diagnosis
Multiple instances of success exemplify the beneficial influence of community-based HIV awareness and prevention campaigns. The effectiveness of this endeavour was derived from the engagement of the community, since those involved in the sex industry had an active role in formulating and executing the programme. In Thailand, the implementation of the "100% Condom Programme" in brothels resulted in a substantial decrease in the transmission of HIV.
Please make sure that all materials and communication are available in many languages. It is important to incorporate cultural subtleties so that everyone can access the information.
Partnerships in the Community work together with neighbourhood groups, churches, and other non-governmental organisations (NGOs) to reach out to underserved communities and diverse populations.
- 2.
Stressing the Need of HIV Testing
Offer discounts at local businesses or free admission to community activities as incentives for people to be checked.
Mobile Testing Units: Send out mobile testing units to different venues, such homes, businesses, and fundraisers.
Give people the chance to take the exam anonymously to lower the barrier to entry and boost participation.
- 3.
Approaches to Conducting Research
Conduct qualitative research by holding focus group conversations to learn more about the opinions and preferences of the community.
To better understand the community’s unique HIV awareness-related needs, attitudes, and concerns, it is recommended to conduct surveys.
HIV Day
On December 1st, the world comes together to celebrate World AIDS Day, a time to remember those lost to the disease and to rally behind those fighting to end the epidemic. In honour of World AIDS Day, let us recommit ourselves to ending the global epidemic of HIV/AIDS. World AIDS Day has been observed annually since 1988 and serves as a platform to bring attention to the devastating effects of HIV/AIDS, honour the lives of those who have died as a result of this disease, and rally support for those who are currently living with it.
In doing so, it urges people on all levels of society to join forces in the fight against HIV/AIDS stigma and to support efforts that help bring an end to the worldwide epidemic. Educational programmes, candlelight vigils, community talks, and HIV testing drives are just a few of the many activities that are planned. Treatment, care, and support services should be easily accessible to anyone afflicted by the HIV/AIDS epidemic, as highlighted on World AIDS Day. Displayed prominently is the distinctive red ribbon, which represents support for those living with HIV/AIDS and serves as a visible reminder of the continuous fight against the infection. On this day, people all throughout the globe come together to raise awareness, combat stigma, and inspire others to take preventative actions. The focus of the day varies from year to year, but always revolves on the need to rally around the goal of eradicating the HIV pandemic.
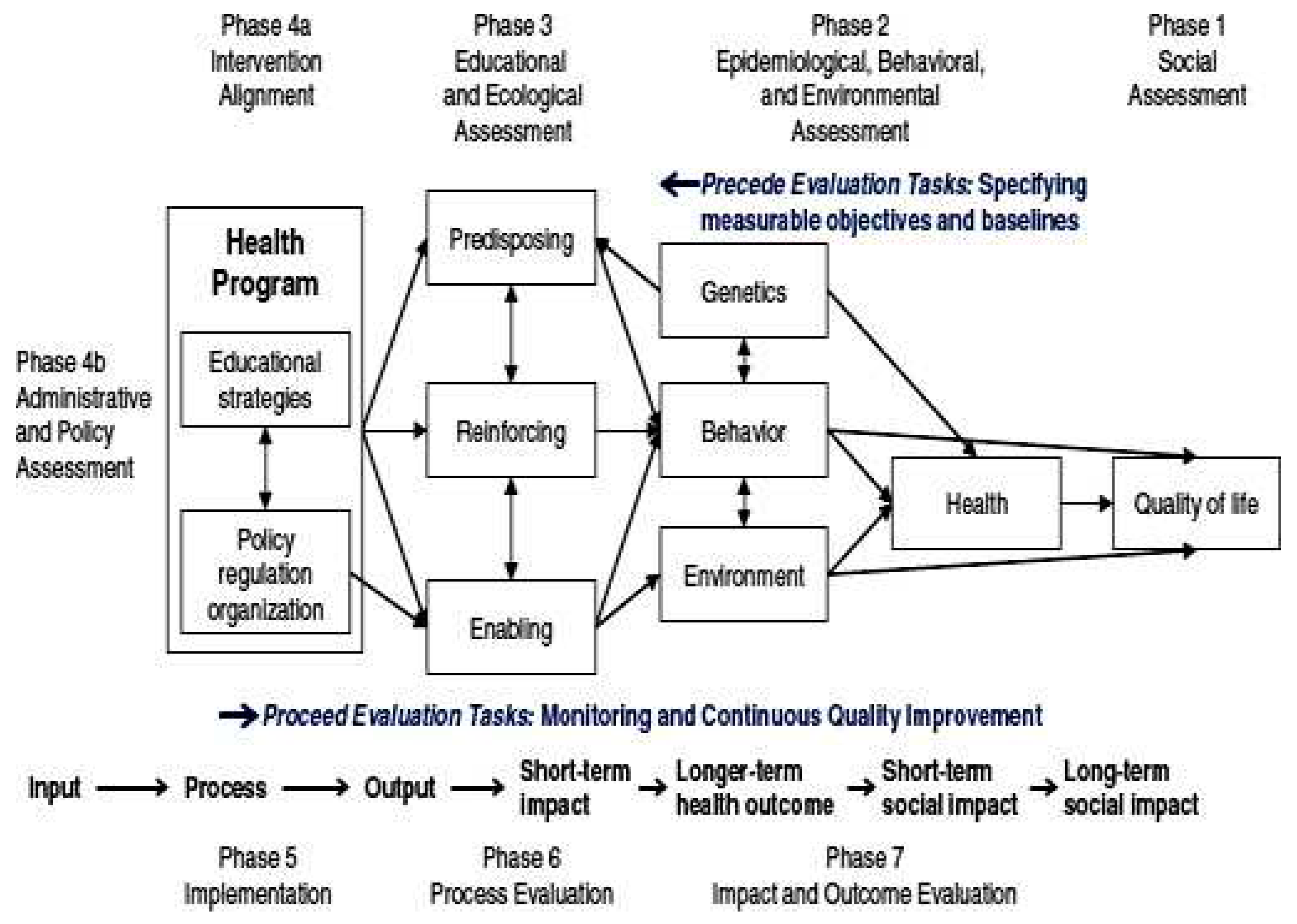
FIGURE PRECED-PROCEED MODEL(Sources; Green and Kreuter, 2005)
FIGURE PRECED-PROCEED MODEL(Sources; Green and Kreuter, 2005)
PROCEED Model
This PROCEED Model is utilized for community-based programmes that acknowledge the distinct dynamics, cultural subtleties, and trust networks that are inherent in local communities. Communities are fundamental in driving social change, and their active participation is crucial in tackling public health issues such as HIV/AIDS. By customising awareness and preventive programmes to cater to the particular requirements of a community, these efforts may dismantle obstacles and efficiently target people who may otherwise be neglected (Bhattacharjee et al. 2019). Their existence has led to a substantial rise in HIV testing rates and an enhanced comprehension of preventive measures among the local populace. Community health workers in sub-Saharan Africa have been instrumental in distributing condoms, imparting knowledge, and advocating for testing.
Phase 6: Implementation
Assess the degree to which the programme met its established deadlines and benchmarks. The success of every endeavour depends heavily on its timely implementation.
Assess the degree to which the programme was carried out in accordance with its original design. Evaluation of programme implementation includes checking in on things like intervention delivery, population reach, and budget allocation.
Use of Resources: Examine how money, people, and stuff are being put to work. This ensures the programme is running as smoothly as possible.
Participant Engagement: Track the amount of interaction from the intended audience. This requires keeping tabs on who shows up, how many people participate, and how engaged they are.
HIV screening program
Safe practises, preventative techniques, and combating HIV/AIDS stigma are all part of this effort. Policies may stress the need of giving pupils access to information that is both factual and suitable for their age. The sex education programmes in Sweden and the Netherlands, for instance, are quite effective because they teach people how to avoid contracting HIV. Comprehensive Sex Education: School curriculum in a number of nations provide comprehensive sex education.
In order to identify and intervene early, it is crucial to highlight the HIV screening programme. By providing the opportunity to take the exam anonymously, we can prevent shame while protecting people’s privacy. The program’s dedication to comprehensive healthcare is further emphasised by its post-screening assistance, which includes counselling and care connection. Strategically placed mobile testing units in high-risk locations and incentive programmes that include promotional benefits and community recognition promote extensive participation. The significance of knowing one’s HIV status is highlighted by the incorporation of screening into community activities and ongoing educational initiatives. By working together, we can make a difference in people’s lives by increasing their knowledge of health issues and encouraging them to take an active role in their own care.
Phase 7: Process Evaluation
Assess the efficiency of interventions, the skill of staff, and the reliability of the programme by evaluating the quality of implementation. Analyse the program’s logic model to see whether its actions, inputs, outputs, and results are in line with its stated objectives. This phase establishes a solid foundation for knowing what to anticipate from the programme.
Collecting participant feedback is important for learning about the participants’ perspectives, struggles, and experiences. This qualitative information is very helpful for understanding the program’s successes and failures. Analyse the external and contextual components that may affect the success of the programme. This process is useful for identifying potential external factors that might affect the outcome of the programme.
Goal: Use targeted outreach and content to modify programme components for certain groups.
To prevent new infections, it is important to keep an eye on epidemiological statistics and identify patterns. Then, may work to improve public education and discourage harmful habits.
Plan the program’s rollout and use an iterative method that takes into account user input in real time.
Services for assistance: Work together with healthcare providers and non-governmental organisations to provide all-encompassing assistance, including mental health, physical health, and community participation programmes.
Engage people in adopting healthy behaviours via the use of evidence-based interventions, culturally appropriate messages, and peer education.
Compliance and Reporting: Set up reliable systems for gathering data and reporting it so monitor programs can performance and make informed decisions about how to improve it.
Phase 8: Impact Evaluation
To determine whether or whether improvements seen may be ascribed to the programme rather than external influences, it is necessary to establish a comparison group and conduct a comparison group analysis. This method is useful for separating the effects of the programme.
Determine what kinds of immediate shifts or impacts the programme is having by measuring intermediate outcomes. The intended audience may undergo a shift in their level of understanding, perspective, or practise.
Quantitative approaches should be used to analyse the data gathered over the course of the programme. The relevance and size of the program’s influence may be measured using statistical analysis.
Determine whether there is a connection between the programme and the results that were measured. Find out how much of an effect the programme had on the outcomes.
Although the awareness programme aims to encourage healthy behaviours, it is difficult to put a precise estimate on how many people will really stop engaging in unsafe sexual practises as a result. With proper implementation, the programme may reach a large enough percentage of the target population to reduce the prevalence of STIs and their associated health problems.
On the other hand, if the programme is successful, it will have raised HIV testing rates, decreased hazardous behaviours, and enhanced awareness. A better understanding of the program’s efficacy and public health effects may be gained by tracking changes in behaviour and STI prevalence over time.
The programme aims to significantly expand primary HIV screenings. This method removes testing hurdles and promotes proactive health management. Our goal is to screen 70% of the population in six months using mobile clinics, community-based testing, and incentive marketing.
This requires working with schools, creating age-appropriate materials, and training teachers to offer effective health education. The programme plans to incorporate HIV awareness into all school and university curriculum next year. By including HIV awareness into the curriculum, the programme hopes to raise a generation that understands prevention, stigma reduction, and healthy living.
Within six months, an objective is established to stimulate behavioural change. Customised outreach techniques like peer-led campaigns and local influencer alliances can help achieve this aim. The programme uses educational advertising, community workshops, and internet channels to get 20% of people to avoid unprotected sex. Progress may be tracked and tactics adjusted with continuous input.
Phase 9: Outcome Evaluation
Summarise the most important results, the lessons learned, and suggestions for moving forward with the project. This phase provides valuable feedback for improving the programme or creating future initiatives along similar lines.
Evaluation of Long-Term Results: Find out how effective the programme has been over time. Testing how long the effect of the programme last is part of this evaluation.
Analyse how long the programme might potentially go for. Find out whether this programme has potential for future replication. Analyse the program’s cost-effectiveness and value to determine whether it’s worth continuing. The results of the programme, both monetary and otherwise, are evaluated at this stage.
Objective: Encourage general wellness to cultivate a healthy populace.
Prevention of Diseases; Make people more aware of the need to take preventative measures to lower the incidence of potentially fatal illnesses, especially STDs.
Systemic Effects on Healthcare; Make healthcare systems more efficient by reducing the strain on infection prevention and management.
Enhancement of Immunity; Improve people’s ability to withstand and recover from infections, particularly coronaviruses, by boosting their immunity and resistance.
All-Inclusive Medical Procedures: In order to build a strong community that can make a lasting difference in public health, it is important to encourage holistic health practises.
Summary
In our ongoing battle against HIV/AIDS, it is crucial to enhance the effectiveness of community-based initiatives and give priority to the participation of communities in creating the future of HIV prevention and awareness. These efforts enable people to take control of their health by acknowledging the distinct characteristics of each community, customising educational programmes, offering convenient diagnostic services, and cultivating support networks. Community-driven HIV awareness and prevention efforts play a crucial role in establishing a long-lasting and efficient approach to combat the worldwide HIV/AIDS pandemic.
References
- Ayon, S., Jeneby, F., Hamid, F., Badhrus, A., Abdulrahman, T., & Mburu, G. (2019). Developing integrated community-based HIV prevention, harm reduction, and sexual and reproductive health services for women who inject drugs. Reproductive Health, 16, 1-11. https://link.springer.com/article/10.1186/s12978-019-0711-z.
- Bhattacharjee, P., Rego, D., Musyoki, H., Becker, M., Pickles, M., Isac, S., Lorway, R., Musimbi, J., Walimbwa, J., Olango, K., & Kuria, S. (2019). Evaluation of community-based HIV self-testing delivery strategies on reducing undiagnosed HIV infection, and improving linkage to prevention and treatment services, among men who have sex with men in Kenya: a programme science study protocol. BMC Public Health, 19(1), 1-13. https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-019-7291-2.
- Centers for Disease Control and Prevention (CDC) - HIV Testing. (2020). https://www.cdc.gov/hiv/testing/index.html.
- Crosboy R., Seth M., N. (2011). What is a planning model? An introduction to PRECEDE – PROCEED. Public Health Dentistry. https://onlinelibrary.wiley.com/doi/10.1111/j.1752-7325.2011.00235.x.
- Daniil Filipenco (2023). HIV statistics around the world in 2021: TOP-10 countries with the highest infection rates. Development aid. https://www.developmentaid.org/news-stream/post/161014/hiv-aids-statistics-by-country.
- Gender disparity in HIV for every year. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6139900/.
- Green, L. W., and M. W. Kreuter. (2005). Health program planning: An educational and ecological approach, 4th ed. New York: McGraw-Hill.
- Girum T., Wasie A., Lentiro K., Muktar E., Shumbej T, Difer M., Shegaze M., and Worku A. (2018). Gender disparity in epidemiological trend of HIV/AIDS infection and treatment in Ethiopia. Arch Public Health. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6139900/.
- Larson, B., Cele, R., Girdwood, S., Long, L., & Miot, J. (2020). Understanding the costs and the cost structure of a community-based HIV and gender-based violence (GBV) prevention program: the Woza Asibonisane Community Responses Program in South Africa. BMC health services research, 20(1), 1-10. https://bmchealthservres.biomedcentral.com/articles/10.1186/s12913-020-05385-1.
- PEPFAR. https://www.pepfar.gov/.
- Ranking of countries with the highest prevalence of HIV. https://www.statista.com/statistics/270209/countries-with-the-highest-global-hiv-prevalence/.
- Shamu, S., Khupakonke, S., Farirai, T., Slabbert, J., Chidarikire, T., Guloba, G., & Nkhwashu, N. (2020). Knowledge, attitudes and practices of young adults towards HIV prevention: an analysis of baseline data from a community-based HIV prevention intervention study in two high HIV burden districts, South Africa. BMC Public Health, 20, 1-10. https://link.springer.com/article/10.1186/s12889-020-09356-3.
- UNAIDS. https://www.unaids.org/.
- U.S. National HIV/AIDS Strategy. https://www.hiv.gov/federal-response/national-hiv-aids-strategy/nhas-update.
- World Health Organization - World AIDS Day (2022). https://www.who.int/campaigns/world-aids-day-2022.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).