Introduction
Xanthogranulomatous orchitis is a rare, non-neoplastic disease caused by nonspecific inflammation of the testis. Patients typically experience testicular pain and swelling. Anti-infection treatments are generally ineffective, and surgical resection is a common method of treatment. This paper presents a unique case of yellow granulomatous orchitis combined with contralateral acute pyogenic orchitis, which has not been previously reported in the literature.
Case Report
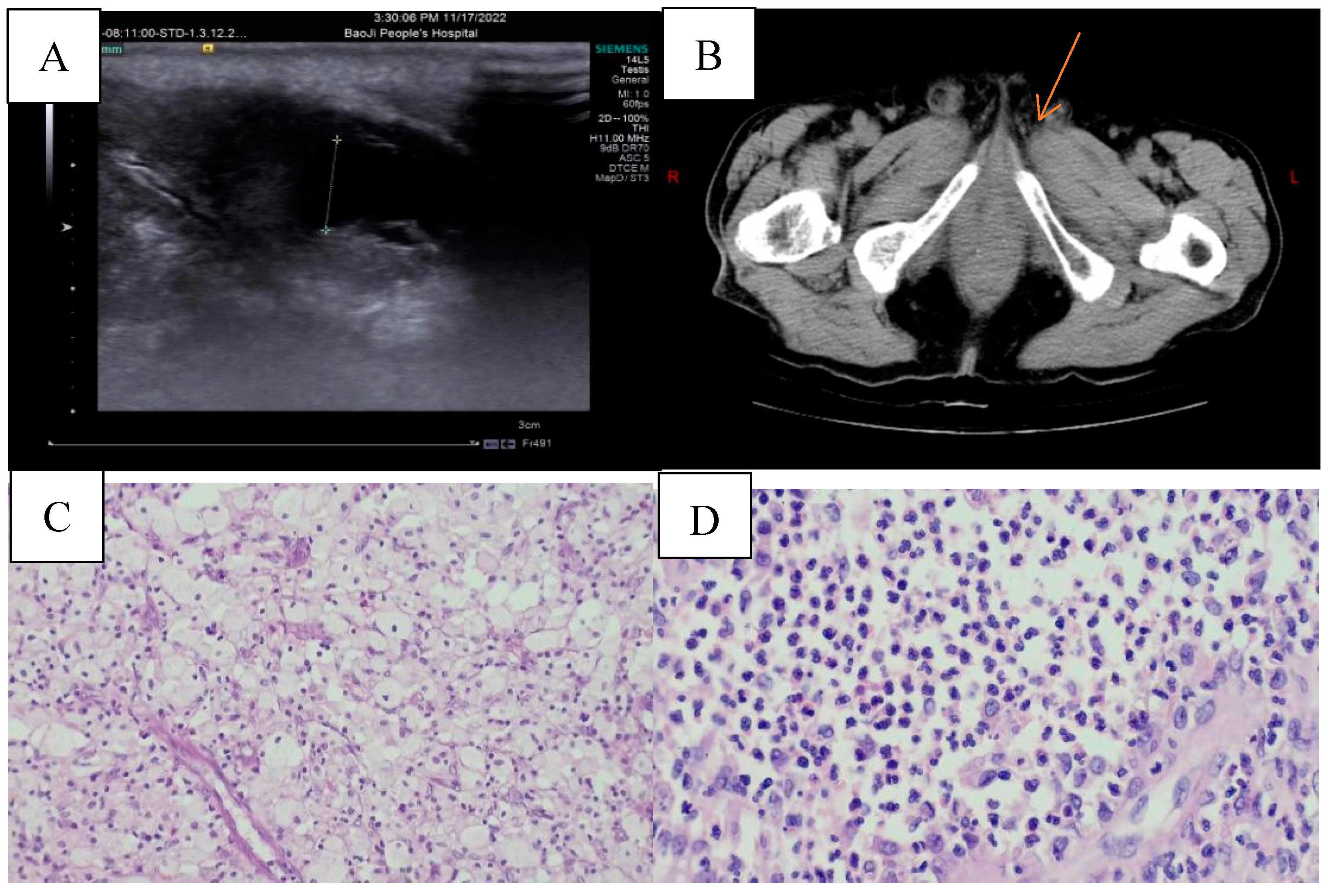
Two weeks ago, a 79-year-old male presented with bilateral scrotal edema and pain accompanied by dysuria. The patient had a medical history of chronic bronchitis and emphysema, and had undergone transurethral resection of the prostate two years prior. During the physical examination, bilateral scrotal enlargement with tenderness was noted, and a digital rectal examination indicated an enlarged prostate degree III, qualitative toughness, and no significant induration. The laboratory examination results show TPSA at 7.30 ng/ml, FPSA at 0.639 ng/ml, carcinoembryonic antigen at 4.35 ng/ml, alpha-fetoprotein at 5.26 ng/ml, testosterone at 12.22 nmol/L, and lactate dehydrogenase at 106 U/L. The urine routine indicates WBC at 2299/ul and RBC at 639.10/ul. No HCG was collected after admission. The scrotal B ultrasound reveals a mixed mass in the left testicle, which could be an inflammatory mass with a small amount of pus. The right testicle is swollen, but no abnormality in color flow was detected. The image in
Figure 1A shows a flufluid surround around the right testis. An MRI conducted at a different hospital revealed prostate enlargement that extended upward into the bladder, with a size of approximately 72.2mm x 68.2mm x 76.8mm. A urinary CT scan indicated that the left testis had reduced in volume and had uneven density, while the right testis was enlarged. Inflammatory changes were also observed, as shown in
Figure 1B.
After the patient received anti-infection treatment in our department, the desired effect was not achieved. Despite the treatment, the patient's scrotal pain did not show significant relief, and he continued to experience dysuria. After thorough communication with the patient and his family members, we decided to perform a transurethral prostate resection along with bilateral testicular exploration. During the operation, we discovered bilateral partial testicular tissue necrosis with a pungent odor and pus. After careful consideration, we determined that performing a bilateral orchiectomy was the best course of action. Postoperative examination revealed that the left testis had xanthogranulomatous orchitis and local hydrocele changes (
Figure 1C), while the right testis had acute suppurative inflammation with bleeding (
Figure 1D). Immunohistochemical results showed that CD68 was positive, while PSA and CK7 were negative, and Ki-67 had scattered positivity. Following a 3-month follow-up after surgery, the patient had satisfactory postoperative results and experienced no adverse events.
Discussion
Xanthogranulomatous inflammation (XGI), initially described in 1987 by Wiener LB et al., is a rare non-neoplastic condition characterized by non-specific inflammation. This condition primarily affects men aged 50 to 70 years old, with an incidence of 0.6% to 1.4% [1-4]. It is most commonly found in the kidneys and gallbladder, but it can also infect the liver, appendix, ovaries, vagina, bones, and bladder. It is known as testicular anthogranuloma when it invades the testis. (XGO). A case of yellowish granulomatous orchitis with contralateral acute suppurative orchitis is described here. This is a rare benign testicular disease characterized by necrosis of testicular tissue followed by lipid-filled macrophage infiltration [5-7]. he XGO microscopic analysis indicated an accumulation of foamy tissue cells with mixed heterogeneous inflammatory cells, resulting in significant damage and loss of the testicular parenchyma. (
Figure 1 C). widespread mixed inflammatory cell infiltration of the testicular parenchymal, testicular web, and epididymal tissue, with full destruction of seminiferous tubules, fluid necrosis, suppuration, widespread fibrosis, and foamy histiocyte aggregation with multinucleated giant cells [
8,
9].
Immunodeficiency, persistent infection, and abnormal phagocytosis of necrotic tissue are all possible causes of xanthogranulomatous lesions [
10,
11]. The pathophysiology of xanthogranulomatous orchitis is still unknown. Nistal M et al [
12] It is believed that XGO is linked to testicular chronic inflammatory infection and the ischemia process of the genital tract. Another cause of xanthogranulomatous testicular epididymitis is urine reflux via the vas deferens [
10]. Salako AA et al [
13] consider Adult testicular xanthogranuloma is thought to be caused by epididymis or spermatic cord obstruction, which causes sperm extravasation and stasis. Given that the urinary B ultrasonography and MRI show aberrant prostate volume expansion (72.2mm68.2mm76.8mm), we suspect that lower urinary tract obstruction is the root cause of this patient's xanthogranulomatous orchitis.
The differential diagnosis of xanthogranulomatous orchitis is most commonly acute orchitis and testicular tumors. Their common clinical manifestations were all those of scrotal enlargement. Common acute orchitis often has a history of acute infection, accompanied by scrotal redness and heat pain; testicular tumors generally have no obvious pain, often accompanied by obvious scrotal swelling, some patients can help serum tumor markers. Our case had atypical clinical features, only bilateral scrotal pain, negative testicular tumor markers, and an onset of 2 weeks, which could not be easily distinguished from common orchitis.
Currently,XGO has been reported to coexist with testicular tumors. Val-Bernal JF et al[
11] once reported a 52-year-old man who underwent orchiectomy for unilateral testicular enlargement and scrotal skin sinus formation, and the postoperative pathology suggested yellow granulomatous testicular epididymitis with seminoma. Given this possibility, histopathology became the most reliable evidence for the diagnosis of XGO and the exclusion of occult malignancy. Some studies have reported that B-ultrasound-guided fine needle biopsy (FNA) has diagnostic significance for yellow granulomatous pyelonephritis and cholecystitis, and FNA is expected to become a useful tool for preoperative diagnosis of XGO [
16], which may prevent orchiectomy due to unexpected diagnosis.The general management of xanthogranulomatous orchitis includes anti-inflammatory, analgesic, detumescent, and symptomatic treatment, but the effect is not ideal. Orchiectomy for [
17] was ultimately chosen in many cases. In adolescents with testicular swelling and pain, anti-infective treatment is generally preferred.
This case suggests that in patients with acute and chronic orchitis, if lower urinary tract obstruction is present, the possibility of yellow granulomatous orchitis should be considered if antibiotic treatment is ineffective. This case has a certain guiding significance for subsequent peers to make a timely and decisive treatment plan.
Author Contributions
Conception and design:Yu Dai,Yan-hu Meng. Administrative support:Yingyi Li. Provision of study materials or patients:Shuangning Liu. Collection and assembly of data:Yu Dai. Data analysis and interpretation:Yan-hu Meng. Manuscript writing: All authors. Final approval of manuscript: All authors.
Statement of Ethics
According to our ethics review board, an ethics approval is not necessary for a case report; so ethical approval is not required for this study in accordance with local guidelines. All procedures performed in this case report were in accordance with the ethical standards of the institutional and/or national research committee and with the 1,964 Helsinki Declaration and its later amendments or comparable ethical standards. Written informed consent was obtained from the patient for publication of this case report and any accompanying images. This retrospective review of patient data did not require ethical approval in accordance with local guidelines.
Data Availability Statement
All data generated or analyzed during this study are included in this article. Further inquiries can be directed to the corresponding author.
Conflicts of Interest
The authors have no conflflicts of interest to declare.
References
- Chung MK, Seol MY, Cho WY, et al.: Xanthogranulomatous cystitis associated with suture material The Journal of urology 1998, 159(3):981-982.
- Repetto P, Bianchini MA, Ceccarelli PL, et al.: Bilateral xanthogranulomatous funiculitis and orchiepididymitis in a 13-year-old adolescent boy Journal of pediatric surgery 2012, 47(10):e33-35. [CrossRef]
- Liang L, Jiajia W, Shoubin L, et al.: Granulomatous orchitis: case report and review of the literature The Journal of international medical research 2021, 49(5):3000605211003773. [CrossRef]
- Wiener LB, Riehl PA, Baum N: Xanthogranulomatous epididymitis: a case report The Journal of urology 1987, 138(3):621-622. [CrossRef]
- Bapir R, Ali RM, Hussien DA, et al.: Xanthogranulomatous epididymo-orchitis: A case report with review of the literature International journal of surgery case reports 2022, 92:106832. [CrossRef]
- Gongora ESRF, Pinto IC, Constantino ECN, et al.: Xanthogranulomatous orchitis: case report of a rare condition AME case reports 2019, 3:4. [CrossRef]
- Sharma P, Ramteke P, Satapathy A, et al.: Xanthogranulomatous Orchitis Presenting as a Scrotal Mass in an Elderly Male: Malignancy or Mimicker?Clinical medicine insights Case reports 2019, 12:1179547619890295. [CrossRef]
- Val-Bernal JF, Argueta L, Fernández-Flórez A, et al.: Bilateral xanthogranulomatous orchitis in a tetraplegic patient Pathology, research and practice 2012, 208(1):62-64. [CrossRef]
- Ezer SS, Oguzkurt P, Temiz A, et al.: Xanthogranulomatous orchiepididymitis: a very uncommon cause of scrotal mass in childhood Urology 2013, 82(1):228-230. [CrossRef]
- Vaidyanathan S, Mansour P, Parsons KF, et al.: Xanthogranulomatous funiculitis and epididymo-orchitis in a tetraplegic patient Spinal cord 2000, 38(12):769-772. [CrossRef]
- Val-Bernal JF, González-Márquez P, Ramos-Barseló E, et al.: Concurrent xanthogranulomatous orchiepididymitis and seminoma in the same testis Pathology international 2010, 60(1):55-58. [CrossRef]
- Nistal M, Gonzalez-Peramato P, Serrano A, et al.: Xanthogranulomatous funiculitis and orchiepididymitis: report of 2 cases with immunohistochemical study and literature review Archives of pathology & laboratory medicine 2004, 128(8):911-914. [CrossRef]
- Salako AA, Olasode BJ, Eziyi AK, et al.: Xanthogranulomatous orchitis in an adult Nigerian International journal of urology : official journal of the Japanese Urological Association 2006, 13(2):186-188. [CrossRef]
- Yamashita S, Umemoto H, Kohjimoto Y, et al.: Xanthogranulomatous orchitis after blunt testicular trauma mimicking a testicular tumor: A case report and comparison with published cases Urology journal 2017, 14(3):3094-3096.
- Hama Amin Said S, Abdalla RY, Aghaways I, et al.: Xanthogranulomatous orchitis: Review of the published work, and report of one case Urology case reports 2019, 27:100908. [CrossRef]
- Vijayvergiya G, Gulwani HV, Ul Hasan S: Xanthogranulomatous epididymo-orchitis: A single-institutional case series and systematic review Indian journal of urology : IJU : journal of the Urological Society of India 2023, 39(1):58-66.
- Matsumura M, Taketani T, Horie A, et al.: Pediatric granulomatous orchitis: Case report and review of the literature Pediatrics international : official journal of the Japan Pediatric Society 2016, 58(2):155-158. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).