INTRODUCTION
Introducing Patient Blood Management (PBM) principles in a small hospital, despite the absence of a specific budget allocation, poses challenges. However, various strategic steps can be pursued to integrate PBM practices without relying on additional funding.
A 350-bed urban community teaching hospital serves an acute care trauma center in a sub-served area of New York City. Using an organized, evidence-based multidisciplinary approach to transform blood transfusion practices to optimize patient care for the patients who might need blood transfusion, a patient blood management (PBM) program was initiated in 2013 and fully implemented in 2014 at the hospital.
The PBM program was designed to promote better blood management practices, reduce transfusion rates, and improve patient outcomes. To achieve these goals, the implementation of the program required the cooperation of all healthcare professionals involved in the transfusion process, including physicians, nurses, laboratory technicians, and administrators. One of the key strategies employed was the use of broad-based educational modules for licensed practitioners. These modules were updated and provided annual education, especially for new attending physicians, residents, fellows, physician assistants, and nurse practitioners. The education was designed to improve practitioners’ understanding of blood management principles and to promote best practices for the use of blood products. Transfusion guidelines and clinical transfusion protocols were adjusted to focus on symptomatic anemia rather than on hemoglobin trigger. This approach reduced the use of blood products in cases where transfusions were not clinically indicated.
Another critical aspect of the PBM program was the conversion of laboratory samples to low- volume testing. By using smaller samples, the laboratory was able to perform more efficient and cost-effective testing, reducing the need for unnecessary blood draws and minimizing the risk of iatrogenic anemia.
Furthermore, the program included a reduction in the critical-level reporting of hemoglobin (Hgb) from 7 g/dL to 6g/dL. This change helped to ensure that transfusions were only given when necessary, based on the patient’s symptoms and clinical condition. Finally, the initial orderable number of red blood cell (RBC) units in the electronic medical health record system was set to 1 unit instead of 2 units. This change helped to reduce the number of unnecessary RBC transfusions and decreased the overall cost of the transfusion process.
Overall, the PBM program was effectively implemented without any specifically allocated budgetary support. The program’s success was due in large part to the collaboration and dedication of all healthcare professionals involved in the transfusion process, as well as the commitment to evidence-based best practices for blood management.
METHODS
We conducted a retrospective analysis of all RBC transfusions from 2013 through 2019 to examine the impact of this PBM program on RBC utilization in the hospital.
This retrospective study was given an exempt status by the institutional review boards of St. Barnabas Health.
Hypothesis
Implementation of an evidence-based PBM program would effectively reduce unnecessary RBC transfusions in the hospital.
Aim
The goal of this study is to analyze the impact of this PBM program.
Data Selection Criteria
We retrospectively analyzed our health system’s blood transfusion database from January 1, 2013 - December 31, 2019. RBC transfusion events without exclusion for all patients admitted during this seven-year period were identified, regardless of age, gender, race or disease condition. Outpatient transfusion events were excluded. Transfusion events with plasma products, platelet products or cryoprecipitate were also excluded since this PBM study focused only on inpatient RBC transfusions.
Study Endpoints
To examine the impact of this restrictive PBM program, the following endpoints from 2014 - 2019 were analyzed and compared with baseline data from 2013.
Average (and median) of pre-transfusion Hgb levels which triggered the RBC transfusion orders
Volume of RBC transfusion units
Annual volume of RBC transfusion units when the pre-transfusion Hgb level was ≥7g/dL (thereafter referred to as [# Hb le7]).
Annual percentage of RBC transfusion units when the pre-transfusion Hgb level was ≥7g/dL (thereafter referred to as [% Hb le7]).
This comparison was used to show the reduction, if any, of unnecessary RBC transfusions since in the context of the PBM program, orders for RBC transfusions in nonbleeding patients with Hgb ≥7g/dL without symptomatic anemia or known cardiac disease are unnecessary. Thus, the impact on # Hb le7 and % Hb le7 reflect the effect on reduction of unnecessary RBC transfusions.
- 5.
The number of two-unit RBC transfusion orders
- 6.
When Hgb ≥7g/dL, the number and percentage of two-unit orders of RBC transfusion
- 7.
Overall Rate of RBC Transfusions
To remove the variations caused by the patient length of stay (LOS) and the number of admissions/discharges for the comparison, annual overall rate of RBC transfusion is calculated and compared to the one in 2013.
Overall Rate of RBC Transfusions is calculated as follows:
Overall Rate of RBC transfusion = RBC transfusions without exclusions per 1,000 patient-days.
Patient-days = Total number of discharges X Average LOS (days)
- 8.
Length of Stay (LOS)
Since the goal of PBM is to optimize care for patients who might need a blood transfusion, the impact estimation was not limited in transfused patients only. The yearly LOS for all of the inpatients in 2014 - 2019 was analyzed and compared with the LOS for year 2013.
- 9.
Potential cost saving from reduction of unnecessary RBC transfusion
This estimation is based on reduction of % Hb le7.
- (1)
Number of transfused RBC units
- (2)
# of RBC units transfused when Hgb trigger ≥7g/dL
- (3)
% of RBC units transfused when Hgb trigger ≥7g/dL
- (4)
Potential reduction of RBC units = ((3) of year 2013 - (3) of year of interest (yi)) X (1) of yi
- (5)
Potential cost saving of yi = (4) potential reduced RBC units of yi X $1000/unit.
Per estimation1, 2, it costs about ~ $1000/ per unit of RBC transfusion.
The total potential cost saving of years 2014 - 2019 = the summary of potential cost saving from years 2014 - 2019.
Statistics
Quantitative data were expressed as arithmetic mean ± standard deviation. Median of each group data was also displayed sometimes as desired. Statistical analysis was conducted with unpaired t-test using Excel 2019 (Microsoft Corp., Redmond, WA) to evaluate the difference between each endpoint value mentioned above to the counterpart value for year 2013. Values of p < 0.05 were considered statistically significant.
RESULTS
Our results show that significant improvement in RBC transfusion practices and usage occurred since implementation of the PBM program in 2014 as follows:
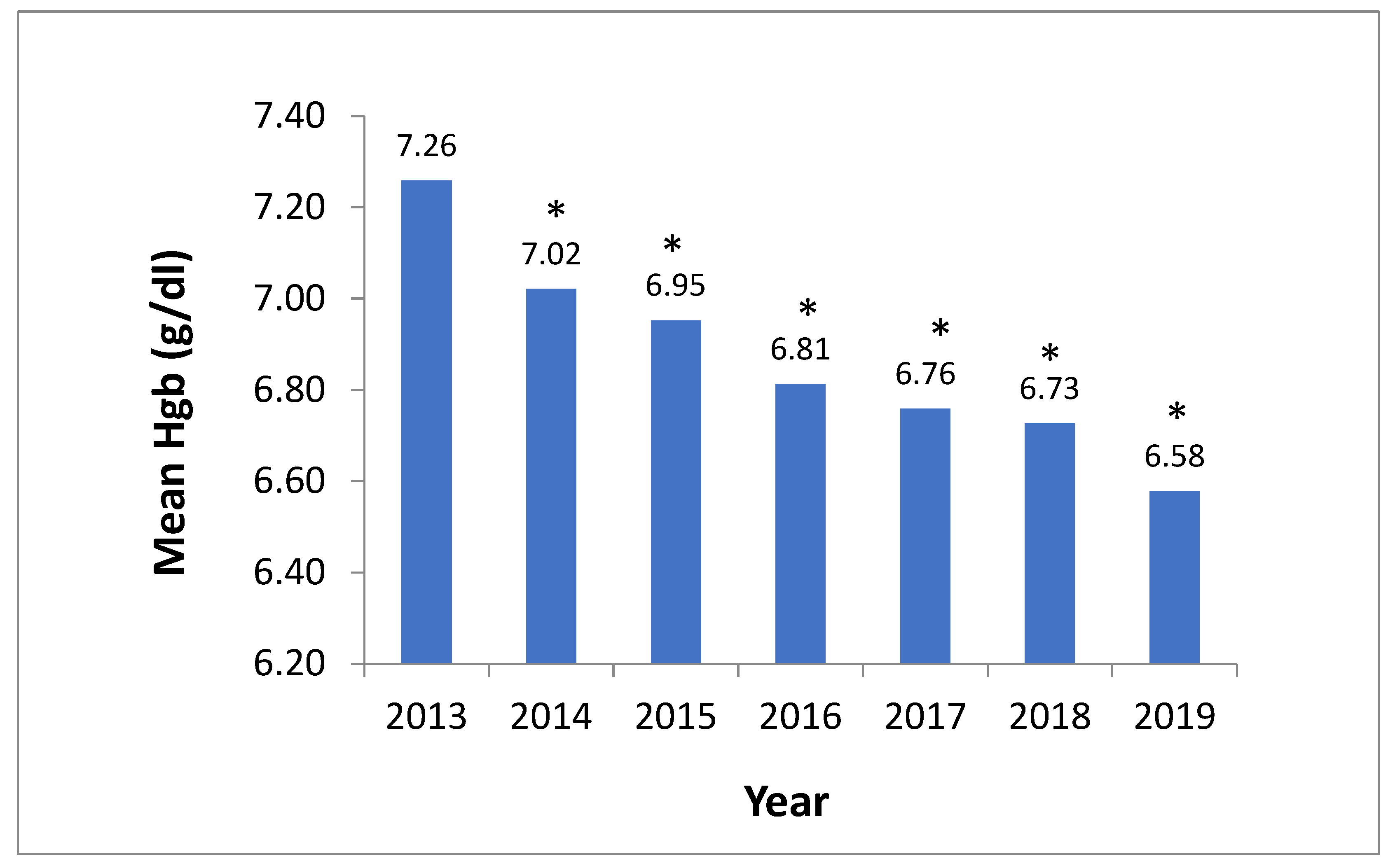
Mean pre-transfusion Hgb for RBC transfusion orders consistently decreased year-over-year after PBM program implementation comparing a nadir 6.58 g/dL in 2019 vs 7.26 g/dL in 2013 (p < 0.0001) (
Figure 1).
Median Hgb for RBC transfusion orders revealed the same trend (Supplemental Data
Figure 1).
During the same six-year period (2014-2019), the number of annual transfused RBC units showed a significant decrease of 34% comparing to the one in year 2013 (
Table 1). (2061-1350) ÷ 2061= 34%.
Similarly, the absolute number and percentage of transfused RBC units with Hgb trigger ≥7g/dL significantly decreased year-over-year reaching a nadir in 2019 compared to 2013 (310 units vs 1210 units, p <0.0001, and 23.0% vs 58.7%) (
Table 1). This reflects a significant reduction (by 35.7%) of unnecessary RBC transfusions consistently year after year. 58.7% - 23.0% = 35.7%.
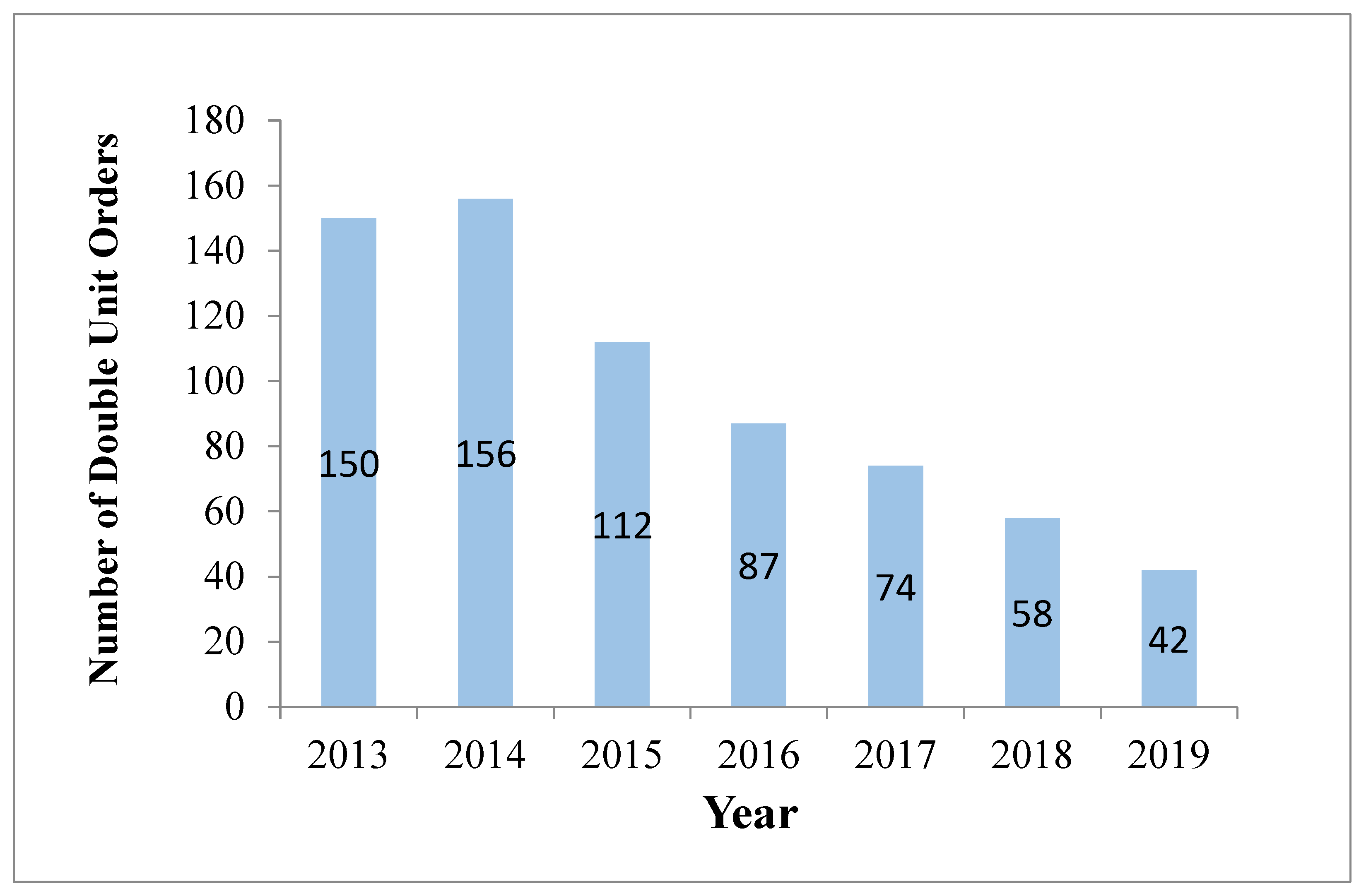
The number of two-unit RBC transfusion orders decreased from 150 to 42 post-intervention (
Figure 2).
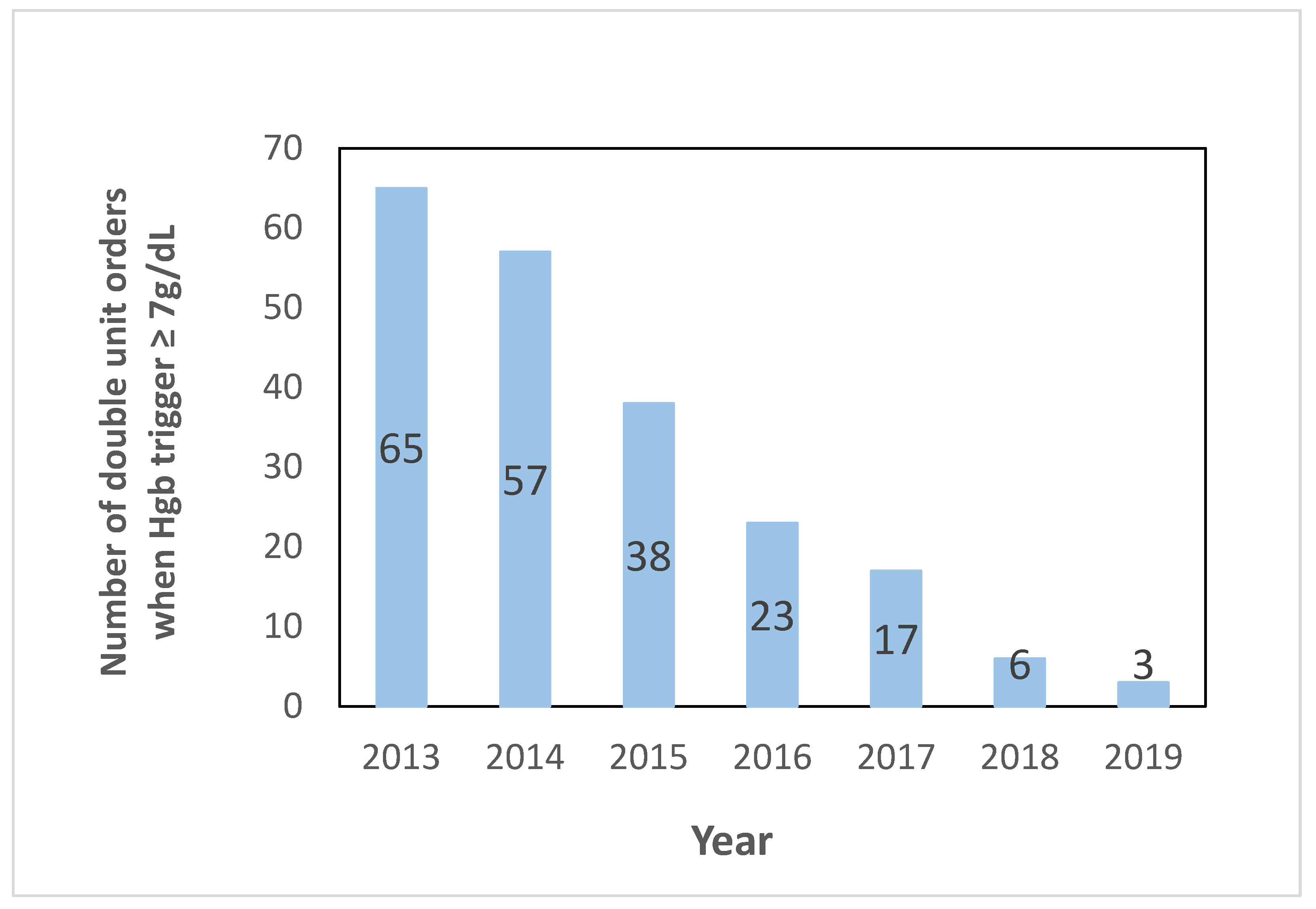
When Hgb trigger ≥ 7g/dL, the number and percentage of two-unit orders for RBC transfusions decreased from 65 (3.4 % of RBC transfusions) to 3 (0.2 %) post-intervention (p < 0.0001) as shown in
Figure 3.
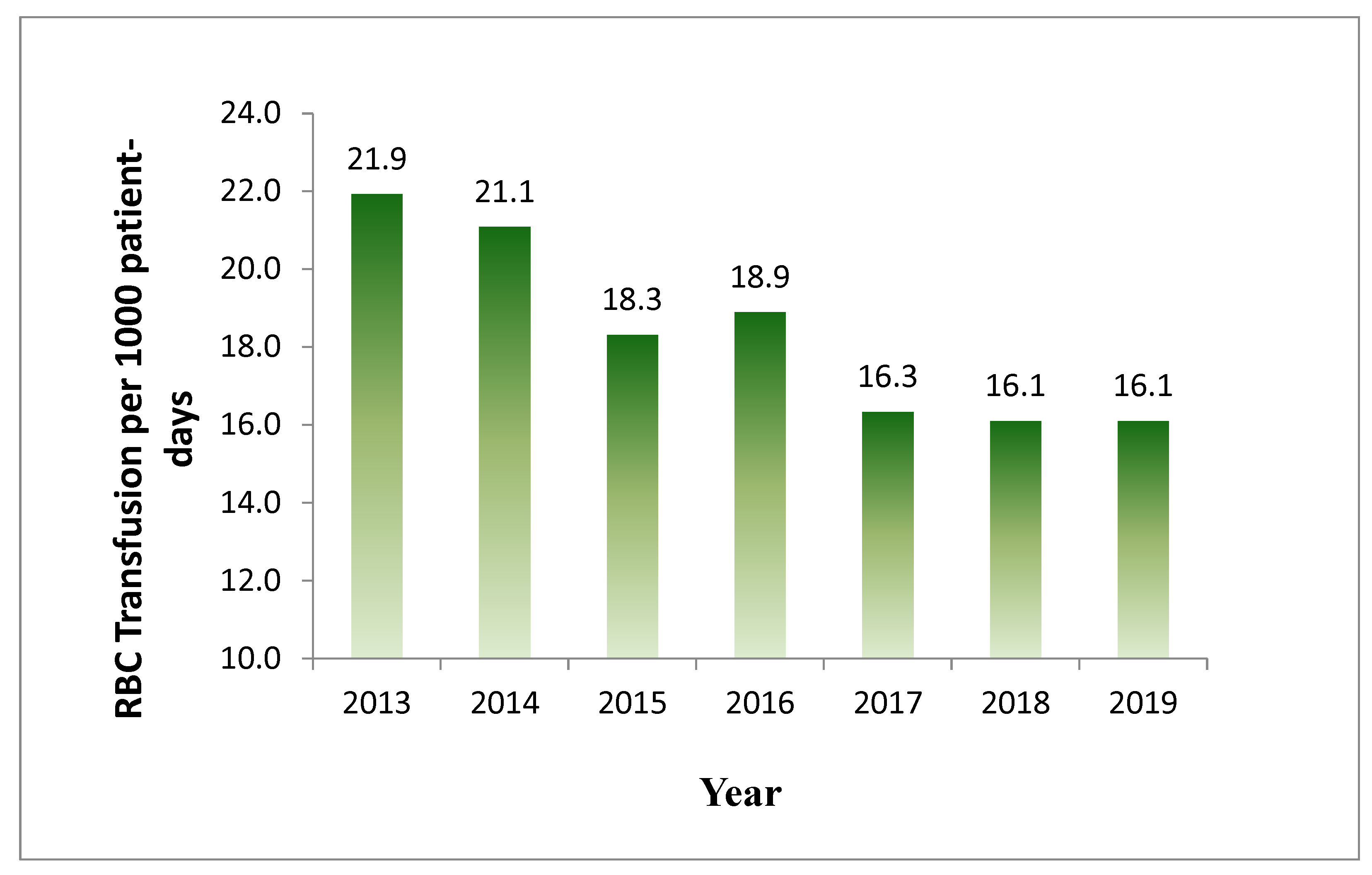
The annual overall rate of RBC transfusion without exclusion per 1,000 patient-days decreased from 21.9 in 2013 to 16.1 in 2019 (
Figure 4), demonstrating a 26% reduction.
Overall Rate of RBC Transfusions = Units of inpatient RBC Transfusion without exclusions per 1,000 inpatient-days
Little change of mean and median inpatient LOS over seven years suggested no hospital patient harm caused from the restrictive PBM program (
Table 2).
This RBC usage reduction translates into approximately 2115 units of RBC during the six-year post-launch period (2014-2019) saved. Based on a cost of ~
$1000 per unit
1, the potential cost-savings peaked at ~
$482,000 in 2019 with total savings of ~
$2.1 million during the six years of PBM implementation (
Table 1).
Remarkably, the advancement of this PBM program was achieved without any additional budget allocated to the PBM program.
DISCUSSION
The scope of overtransfusion and the problems associated with it are significant in healthcare. Overtransfusion refers to the unnecessary or excessive administration of blood or blood products to patients. Some key issues associated with overtransfusion [
1,
2] as follows:
First, Transfusion reactions and complications: Receiving unnecessary blood transfusions increases the risk of adverse reactions, which can range from mild to severe transfusion-associated circulatory overload (TACO), transfusion-related acute lung injury (TRALI), allergic reactions, hemolytic reactions, and transfusion -transmitted infections, among others. Second, Potential for adverse outcomes: Overtransfusion may not improve patient outcomes and can potentially lead to increased morbidity and mortality in certain cases [
2]. Third, Increased healthcare costs: Blood transfusions are costly and can substantially contribute to healthcare expenses. Unnecessary transfusions lead to increased healthcare spending without providing commensurate benefits to the patient. Fourth, Resource utilization: Inappropriate blood use leads to a strain on blood bank resources, potentially resulting in shortages for patients who genuinely require transfusions.
Patient Blood Management (PBM) aims to mitigate these problems by optimizing blood use, minimizing unnecessary transfusions, and improving patient outcomes through evidence-based practices tailored to individual patient needs. It emphasizes a personalized approach to care that prioritizes patient safety and well-being while conserving precious blood resources [
3,
4,
5].
The primary pillars of PBM typically include:
- (1)
Optimizing red blood cell mass: Ensuring patients have adequate red blood cell levels before surgery or invasive procedures through treatments like iron supplementation, erythropoietin therapy, or other medications. (2) Minimizing blood loss: Employing surgical techniques, such as minimally invasive surgery, to reduce blood loss during procedures. Additionally, using specific medications or interventions to control bleeding. (3) Enhancing patient's tolerance to anemia: Some patients may tolerate lower blood levels without experiencing adverse effects. PBM involves identifying patients who can safely function with lower hemoglobin levels without the need for transfusion. (4) Appropriate blood transfusion: Making evidence-based decisions on when to transfuse blood, ensuring that transfusions are only administered when necessary and beneficial.
Implementing PBM in a small hospital without a dedicated budget can be challenging, but there are several steps that can be taken to introduce PBM principles [
4,
5] without requiring significant additional funding.
- (1)
Education and training: Start by educating staff, including physicians, nurses, and other healthcare professionals, about the principles and benefits of PBM. Utilize internal expertise that may offer free or low-cost educational materials and training sessions.
- (2)
Clinical guidelines and pathways: Develop and implement evidence-based clinical guidelines and pathways that emphasize conservative blood management strategies. These guidelines can include practices such as minimizing unnecessary blood tests, optimizing hemoglobin levels preoperatively, and employing blood conservation techniques during surgery.
- (3)
Utilize existing resources: Assess and optimize the use of existing resources within the hospital. Work with the laboratory and clinical staff to reduce unnecessary blood tests, adopt restrictive transfusion thresholds, and explore alternatives to transfusions, such as iron supplementation or medications that reduce bleeding.
- (4)
Quality improvement initiatives: Implement quality improvement initiatives aimed at reducing blood product waste, improving blood utilization practices, and ensuring that transfusions are given based on established clinical criteria rather than routine practice.
- (5)
Collaboration and partnerships: Collaborate with blood banks, regional blood centers, or other healthcare facilities in the area to explore cost-sharing opportunities, joint training programs, or information sharing related to best practices in blood management.
- (6)
Utilize data and analytics: Leverage data analytics to monitor blood utilization patterns, transfusion rates, and associated costs. This information can help identify areas for improvement and guide decision-making to optimize blood utilization without requiring additional funds.
- (7)
Engage stakeholders: Involve stakeholders across different departments and specialties in discussions about PBM. Encourage collaborative efforts to implement changes and promote a culture of responsible blood use throughout the hospital.
- (8)
Adopt technology solutions: Implement electronic health record (EHR) systems or clinical decision support tools that can help clinicians adhere to evidence-based transfusion guidelines, thereby reducing unnecessary blood transfusions.
- (9)
Evaluate and Adjust: Continuously monitor the impact of PBM initiatives on patient outcomes, transfusion rates, and associated costs. Use this data to refine strategies and make necessary adjustments to improve the effectiveness of PBM practices.
- (10)
Seek Grants or Collaborative Opportunities: Look for grants or collaborative opportunities within the healthcare community that support PBM initiatives or projects aimed at improving blood management. Participating in such programs can provide additional resources and support without requiring a separate budget allocation.
By focusing on education, utilizing existing resources efficiently, implementing evidence-based guidelines, and fostering a culture of responsible blood utilization, a hospital can implement PBM practices without a dedicated budget.
Our study validates the principle that successful implementation of practical PBM strategies is achievable without budgetary support and no funds allocated toward the PBM program in a small urban community teaching hospital. Main outcome measures across the seven-year study period showed that statistically-significant (i.e., p <0.05) improvements in RBC utilization occurred marked by reductions in the overall number of transfused RBC units, transfusion rate per 1,000 patient days, two vs. single unit transfusions, transfusions with a Hgb trigger greater than 7g/dL, and blood product wastage. In addition, PBM implementation led to significant cost savings. These beneficial study outcomes were realized despite inclusion of all inpatient populations, including trauma and neonatal patients; larger reductions in blood utilization and cost savings may have resulted had these patient populations been excluded from the study. The observational nature of this study is a noted limitation, though.
Jenkins
et al. implemented a restrictive transfusion strategy with a typical quality improvement framework and based on education and computer-physician order entry (CPOE) enhancements significantly reduced off-protocol and total blood transfusions [
3]. Our keys to successful implementation included ongoing PBM education via online learning modules targeted for licensed practitioners along with the use of PBM tools such as restrictive transfusion guidelines, computer-physician-order entry alerts with clinical decision choices in the hospital EMR system to guide physicians in transfusion decisions, use of low-volume test sample tubes to reduce hospital-acquired anemia, and the reduction of the critical Hgb alert value from 7g/dL to 6g/dL. The calculation method of overall RBC transfusion rate by Jenkins
et al was utilized in this study.
In comparison, Warner
et al. published observational data from an eight-year study to support successful implementation of PBM in a large U.S. academic medical center without evidence of patient harm. Their data, which included 400,998 admissions, showed a 33% reduction of allogenic transfusions per 1000 admissions, an absolute risk reduction for transfusion of 6%, and a 22% decrease in the rate of transfusions over projected [
4].
Hofmann
et al. examined PBM implementation across 12 nations using semi-structured interviews. These investigators found that although there was consensus that PBM would benefit patients because of improved outcomes and patient safety, as well as cost savings, the lack of experience with PBM was one of the most important barriers for implementation along with the need to change work practice and for collaboration and communication. They identified six intervention levels for PBM implementation, including government, healthcare providers, education, funders, research, and patients [
5]. Education of the healthcare providers for better patient care was our focus of the PBM project. The providers were encouraged to dual role as front-line care providers and quality improvement leaders to implement and practice PBM.
Utilizing the strategy of Podlasek
et al. [
6], we launched a “Why give 2 when 1 will do?” Choosing Wisely campaign. And we have been sustaining it using education and computer-physician-order entry alerts with clinical decision support (CPOE-CDS). We witnessed an overall decrease of 2-unit orders for Hgb ≥7g/ dL progressively from 65 orders per year (3.4% of total orders) to 3 orders (0.2%) from 2013-2019.
Fischer
et al. studied the effect of PBM implementation on physicians’ risk perception, clinical knowledge, and perioperative practice across four German university hospitals. Key implementation strategies targeted knowledge (i.e., development and distribution of PBM educational materials and local guidelines; standardization of performance metrics and data collection to allow valid benchmarking within organizations, etc.), attitude (i.e., fostering team spirit and corporate identity; aggressive marketing, etc.), and behavior (i.e., changing the infrastructure and preoperative flow of patients; preoperative anemia assessment, measurement of individual physician transfusion practice, etc.). Utilizing pre- and post-implementation questionnaires, they found significant increases in favorable attitudes toward preoperative anemia treatment and patient assessment after each single unit RBC transfusion. Furthermore, there was a reduction in the percent of physician respondents who stated that they routinely use Hgb <6g/dL as an indicator for transfusion with a corresponding increase in those who stated that they use physiological transfusion triggers (e.g., electrocardiogram changes or lactic acidosis) [
7]. Our strategies of education and CPOE local guidance successfully improved clinicians’ knowledge, attitude and behavior for RBC transfusion orders, with evidence of progressively substantial decrease of RBC transfusions.
Finally, in its policy brief calling for the urgent implementation of PBM, the World Health Organization [
8] highlighted data from the largest study on PBM outcomes to date published by the Western Australia PBM Program. This study included over 600,000 patients admitted to Western Australia’s four major adult hospitals during a six-year study period and showed significant reductions in mortality, infection, acute myocardial infarction and stroke, and hospital length of stay. Improved key indicators showed reductions in preoperative anemia, pre-transfusion Hgb, and transfused blood products. Meanwhile, single unit RBC transfusions increased. The program resulted in an estimated product cost savings of
$18.5 million and activity cost savings of
$80-
$100 million [
9]. Our study demonstrated that our PBM was successful in reducing unnecessary blood products with a total cost saving of 2.1 million US dollars over 6 years (2014-2019). Our experience also showed that the PBM can be achieved in a community hospital without budgetary support. Lowering the hemoglobin trigger for blood transfusion may reduce the amount of blood transfused to patients, which could result in lower risks of transfusion reactions, infections, and other adverse events associated with blood transfusions. On the other hand, a lower hemoglobin trigger may increase the risk of patient harm, especially in patients with cardiac disease or other medical conditions where a higher hemoglobin level may be required to maintain adequate oxygen delivery. The decision to lower the hemoglobin trigger from 7g/dL to 6g/dL for non-cardiac patient was made in conjunction with an interdisciplinary team of healthcare providers, taking into account the patient's individual needs, the clinical context, and the best available evidence.
The little change in the mean and median of the inpatient length of stay over a 7-year period indicates that the restrictive PBM program did not result in harm to hospital patients.
Another limitation in our PBM implementation is that although the initial orderable RBC units was set to one unit per order in our EMR, the full impact of computer-physician order entry with clinical decision support (CPOE-CDS) may not have been realized to its maximum potential. Goodnough and Hollenhorst [
10] demonstrated a 42% reduction in RBC transfusions using a targeted CPOE-CDS to promote restrictive blood transfusion practices in their institution through smart best practice alerts (SBPA’s) that are triggered for RBC orders above 7g/dL, or 8g/dL for patients with acute coronary syndrome or post-cardiothoracic procedure. Inclusion of CPOE-CDS with SBPA’s could potentially have impacted further reductions in RBC transfusions in our institution.
The study authors believe that this report demonstrates that successful PBM can be achieved without allocation of significant additional resources or budgetary support through implementation of a few common-sense strategies. It should serve as a source of inspiration for other healthcare facilities that have yet to embark upon their journey toward successful PBM implementation.
CONCLUSION
The retrospective seven-year study demonstrated that this multidiscipline PBM program in an urban community teaching hospital using education and restrictive tools effectively reduced total RBC usage without specific budgetary support. In particular the PBM program markedly reduced the unnecessary RBC transfusion for Hgb ≥7g/dL (by 35.7%) and total RBC transfusion (by 28%), and reduced unnecessary 2-unit RBC orders for Hgb ≥7g/dL (from 3.4% to 0.2%). Potential cost saving is estimated 2.1 million US dollars. The research underscores how effective PBM implementation can occur without the need for substantial extra resources or increased budgetary support by adopting a handful of practical strategies.
Supplementary Materials
The following supporting information can be downloaded at the website of this paper posted on Preprints.org.
Author Contributions
Conceptualization, R.K., D.W.W., and M.F.; Study methodology, D.W.W.; Validation, D.W.W.; Study analysis, D.W.W.; Data curation, R. K., D.L., R.H., J. S., V.C.; Writing – Original Draft Preparation, D.W.W., M.F. and Y.L; Writing – Review & Editing, M.F., D.W.W., and M.N.
Funding
This research received no external funding and internal budget allocation.
Institutional Review Board Statement
This retrospective study was given an exempt status by the institutional review boards of St. Barnabas Health.
Informed Consent Statement
Patient consent was waived due to the nature of a retrospective study, which was initially designed to monitor the impact of the PBM program for quality improvement initiative.
Data Availability Statement
Data are unavailable due to privacy and ethical restrictions.
Acknowledgment
The authors express their gratitude to Mr. Zane Last, IT Director, for timely providing the essential data files required for our study's analysis.
Conflicts of Interest
All authors have no relevant conflicts of interest.
References
- Shander, A.; Hofmann, A.; Ozawa, S.; Theusinger, O.M.; Gombotz, H.; Spahn, D.R. Activity-based costs of blood transfusions in surgical patients at four hospitals. Transfusion. 2010, 50, 753–765. [Google Scholar] [CrossRef] [PubMed]
- Shander, A. Transfusion Overuse exposing an international problem and patient safety issue. https://www.sabm.org/wp-content/uploads/SABM-Transfusion-Overuse-2019.
- Jenkins, I.; Doucet, J.J.; Clay, B.; Kopko, P.; et al. Transfusing Wisely: Clinical Decision Support Improves Blood Transfusion Practices. The Joint Commission Journal on Quality and Patient Safety 2017, 43, 389–395. [Google Scholar] [CrossRef] [PubMed]
- Warner, M.A.; Schulte, P.J.; Hanson, A.C.; et al. Implementation of a Comprehensive Patient Blood Management Program for Hospitalized Patients at a Large United States Medical Center. Mayo Clinic Proceedings 2021, 96, 2980–2990. [Google Scholar] [CrossRef] [PubMed]
- Hofmann, A.; Spahn, D.R.; Holtorf, A.P.; et al. Making patient blood management the new norm(al) as experienced by implementors in diverse countries. BMC Health Serv Res 2021, 21, 634. [Google Scholar] [CrossRef] [PubMed]
- Podlasek, S.J.; Thakkar, R.N.; Rotello, L.C.; Fleury, T.A.; et al. Implementing a "Why give 2 when 1 will do? " Choosing Wisely campaign. Transfusion. 2016, 56, 2164. [Google Scholar] [PubMed]
- Fischer, D.P.; Zacharowski, K.D.; Müller, M.M.; et al. Patient blood management implementation strategies and their effect on physicians' risk perception, clinical knowledge and perioperative practice - the frankfurt experience. Transfus Med Hemother. 2015, 42, 91–97. [Google Scholar] [CrossRef]
- WHO. The urgent need to implement patient blood management. Oct 19, 2021.
- Leahy, M.F.; Hofmann, A.; Towler, S.; et al. Improved outcomes and reduced costs associated with a health-system-wide patient blood management program: a retrospective observational study in four major adult tertiary-care hospitals. Transfusion. 2017, 57, 1347–1358. [Google Scholar] [CrossRef] [PubMed]
- Goodnough, L.T.; Hollenhorst, M.A. Clinical decision support and improved blood use in patient blood management. Hematology Am Soc Hematol Educ Program 2019, 577–582. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).