Introduction
Thyroglossal Duct Cyst (TGDC) is a remnant of the thyroglossal duct. The thyroid gland descends caudally from its origin at the foramen caecum in the primary pharynx to its final position under the thyroid cartilage in the antero-inferior visceral compartment of the neck during embryogenesis.[
1] The thyroglossal duct is a tubular structure that connects the thyroid gland in the neck to the foramen caecum at the junction of the anterior two-thirds and posterior one-third of the tongue.[
2] Normally the thyroglossal duct closes by the tenth week of gestation, however, if it fails to involute, it can lead to the development of cystic swellings along any part of its track from the tongue to the thyroid gland. Thyroglossal duct cyst is the most common neck swelling with a prevalence of about 7% in the world's population.[
3] However, carcinoma of the TGDC is rare and reported in 1%-3% of the cases, most commonly in older adults.[
4,
5] In this case report, we discuss the presentation, diagnosis and management of a 19-year female patient with papillary carcinoma of the thyroglossal duct cyst.
Case Report
A 19-year-old female patient presented to the hospital with chief complaints of a painless left-sided neck swelling of insidious onset for the past 6 months. On examination, an approximately 2 x 2 cm-sized submandibular swelling with a doughy consistency was noted. It was a non-tender, non-warm, non-fluctuant, fixed swelling, with uncharacteristic overlying skin without any warmth, dilated vein, scar or sinus over it. The mass did not move with deglutition or protrusion of the tongue.
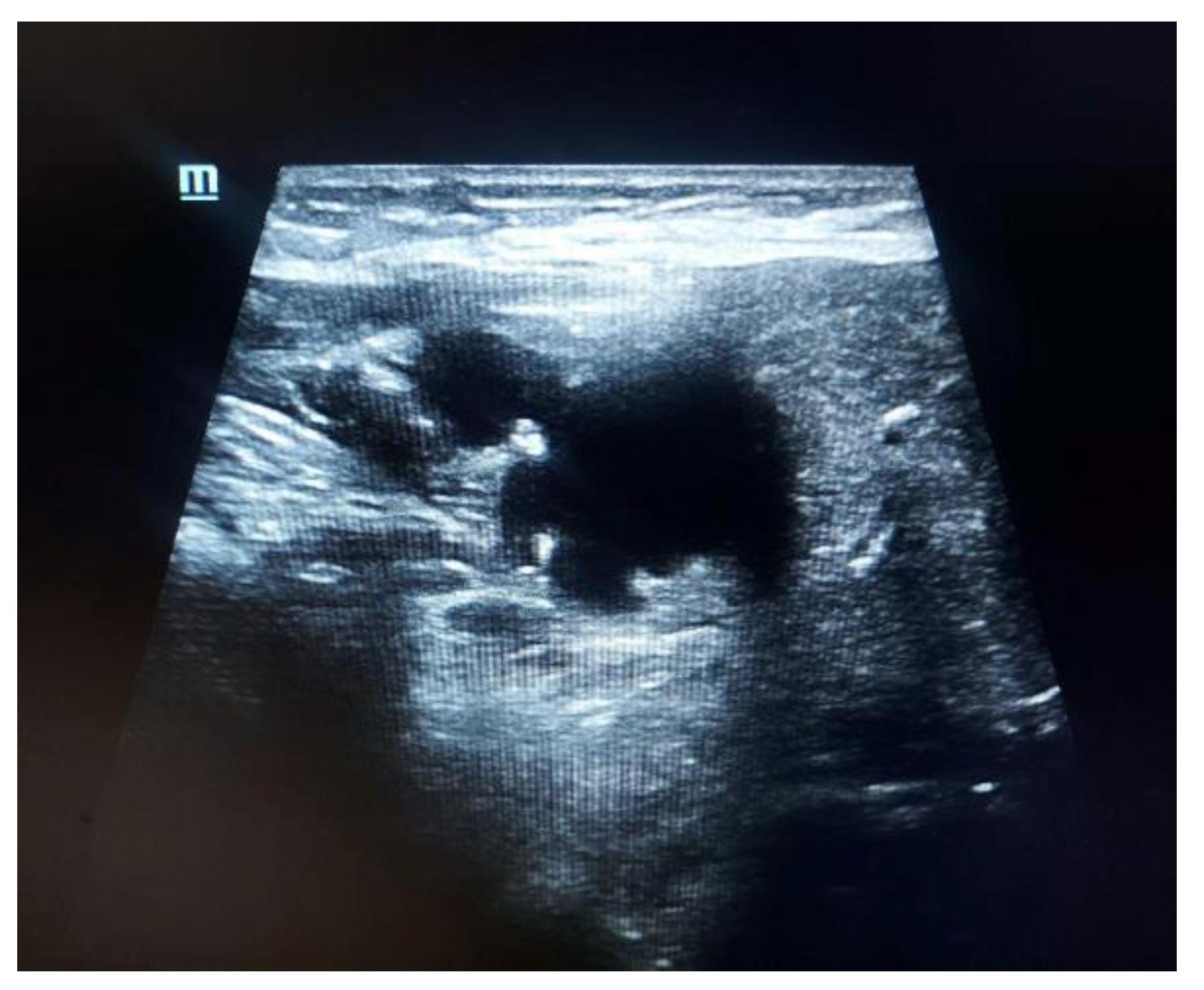
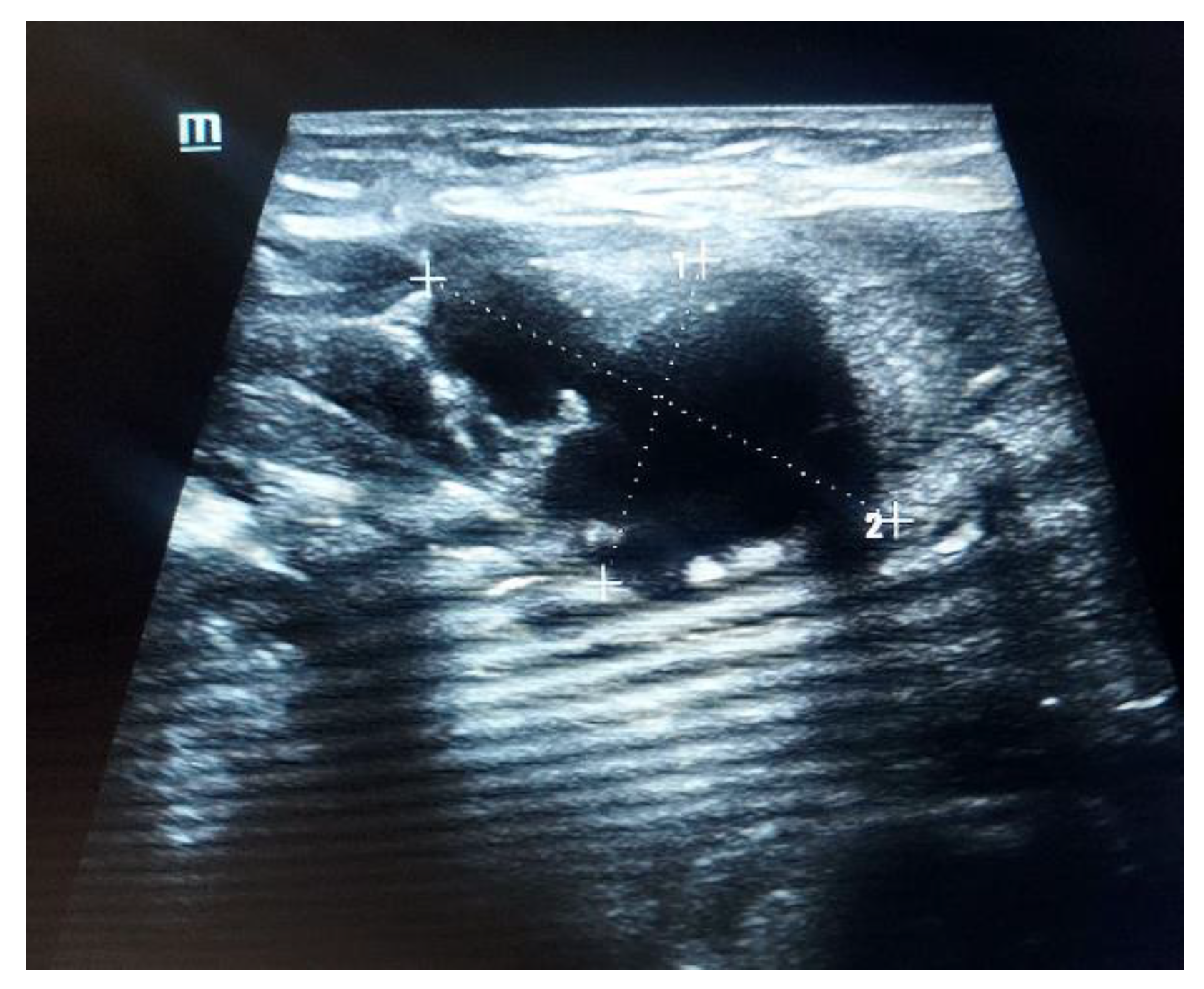
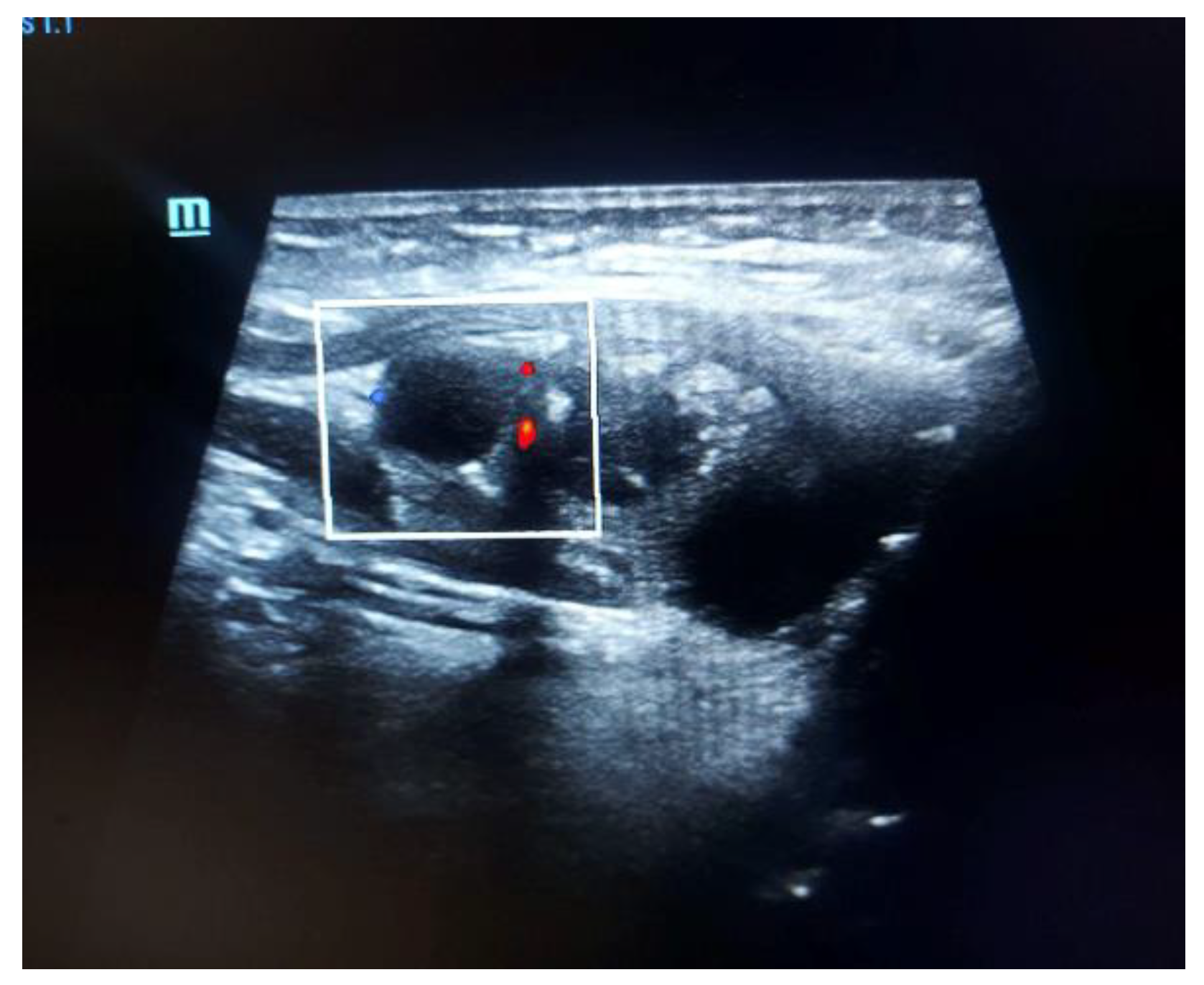
Upon ultrasound, a 28 x 17 mm sized predominantly cystic lesion with few internal echoes and hyper-echoic foci with faint peripheral vascularity was noted in the intramuscular plane medial to the left submandibular gland in the left paramedian submandibular region. It appeared to infiltrate the muscles of the floor of the mouth.
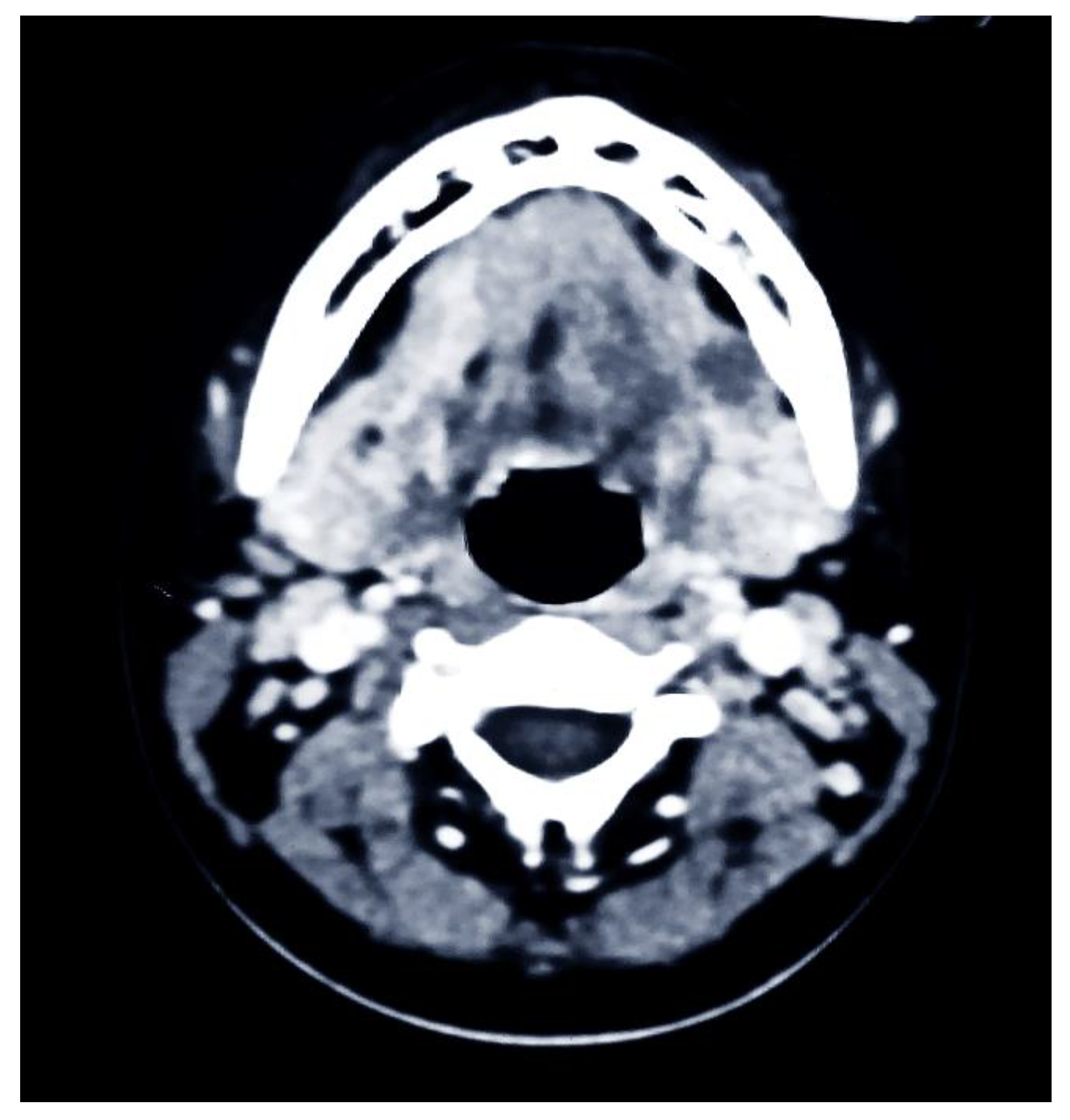
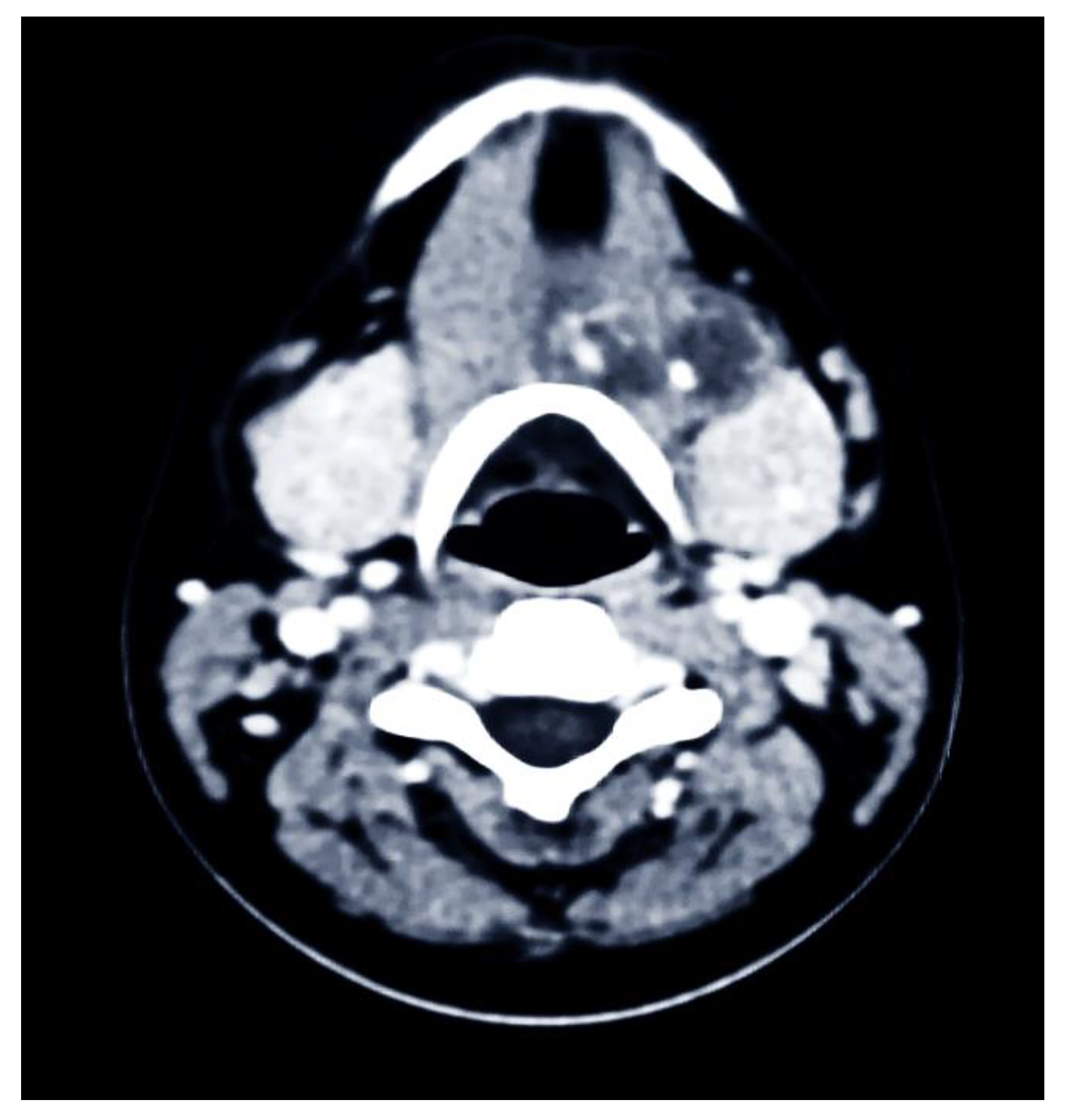
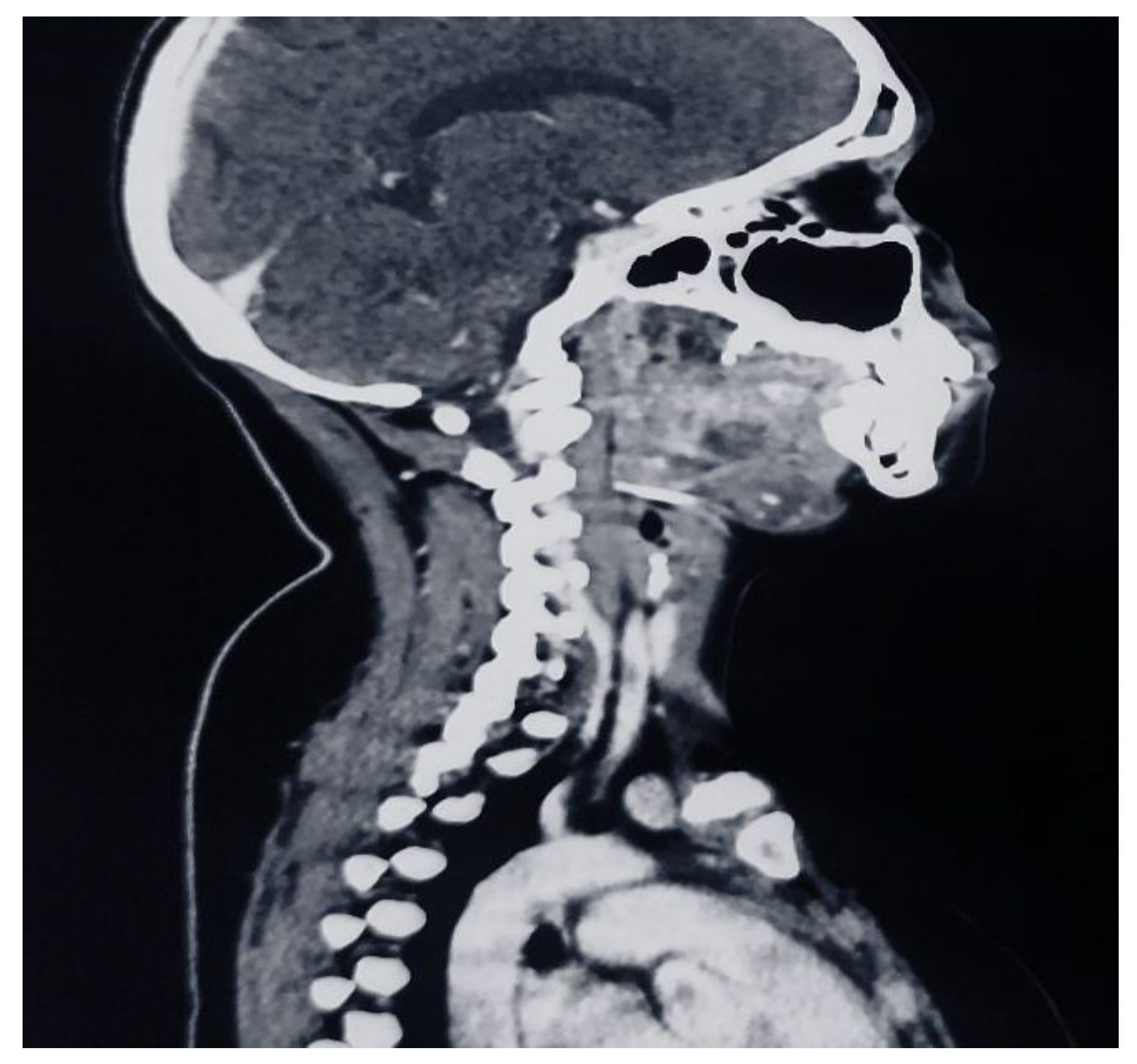
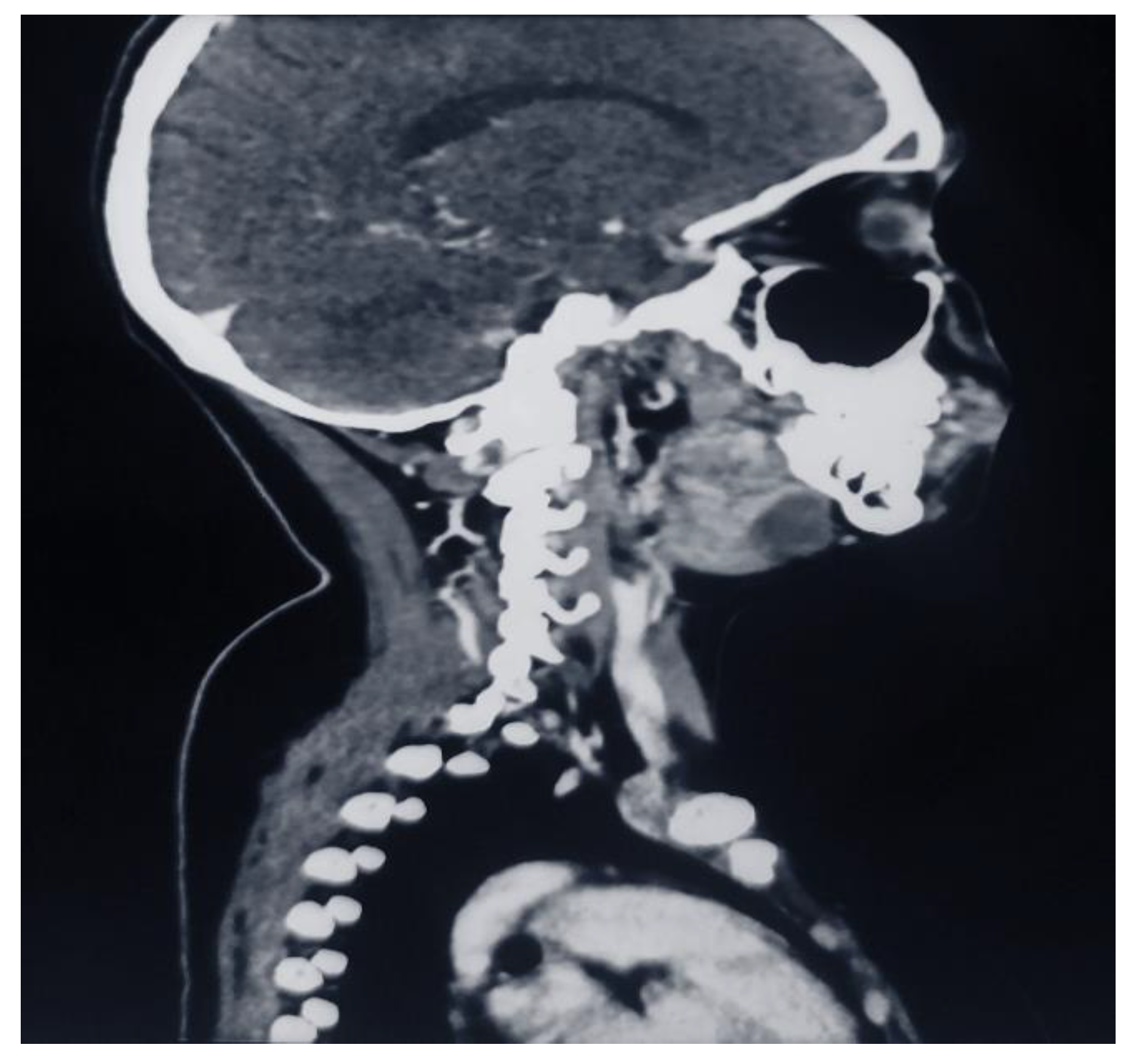
To differentiate between a ranula and a TGDC a CECT Neck was done. A 23 x 29 x 26 mm sized ill-defined, peripherally enhancing, multiloculated cystic lesion with few calcific foci within was noted. It was situated on the floor of the mouth on the left side involving the mylohyoid muscle and anterior belly of the digastric muscle. The left submandibular gland was observed to be separate from the lesion. Postero-laterally it appeared to abut the medial surface of the left submandibular gland. Posteriorly it appeared to abut the left side of the hyoid bone.
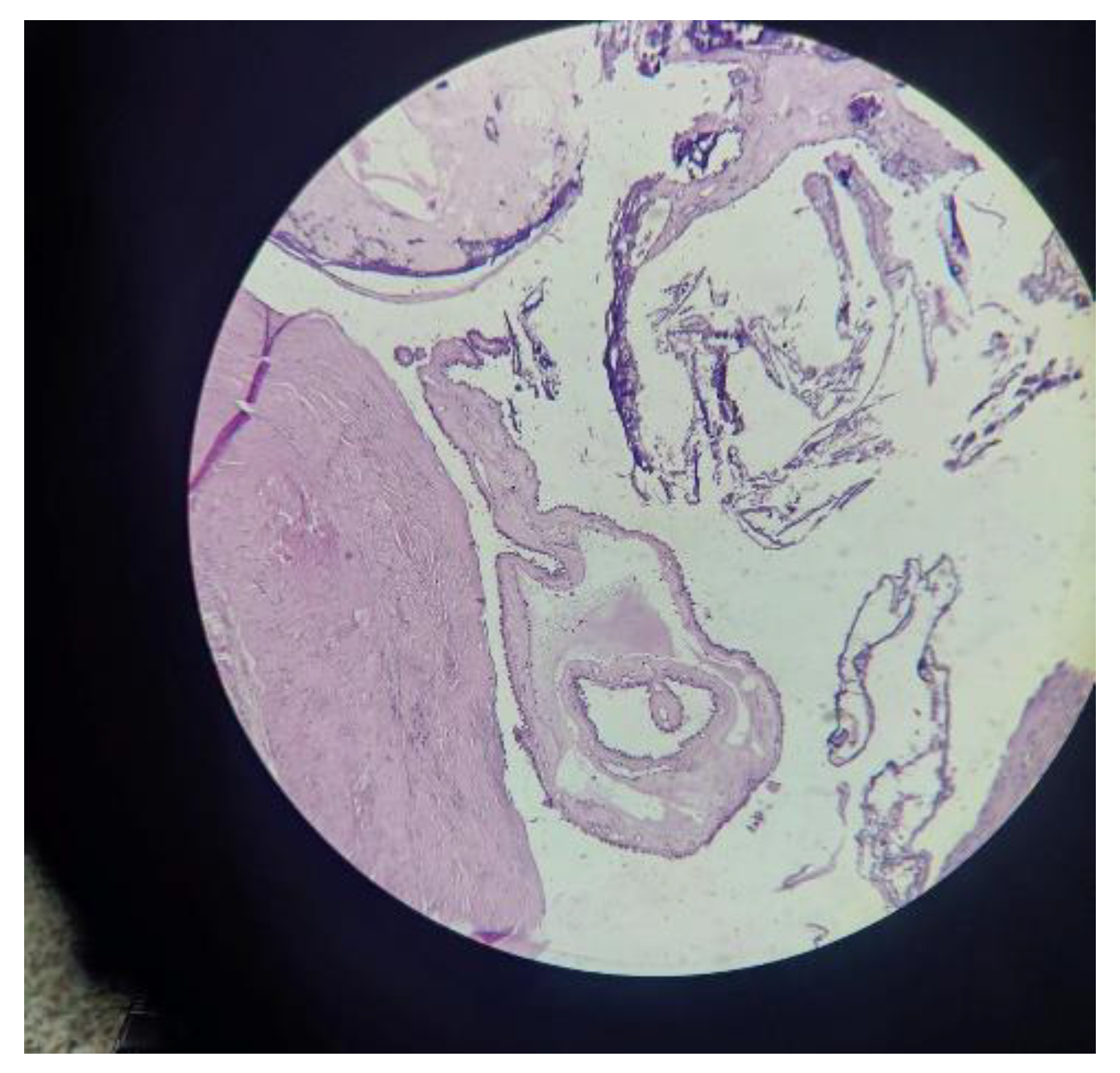
Surgical excision of the cystic swelling was done and the sample was sent for histopathological examination (HPE). HPE showed that the cyst wall was composed of fibromuscular tissues, lymphocytic infiltrate and lined by squamous to low cuboidal cells. Cyst lumen comprised papillae with a fibrovascular core, while some of the papillae showed a hyalinized and edematous core. Papillae were lined by low to cuboidal epithelium with marked calcification. No evidence of salivary gland tissue was seen in the peripheral rim. Papillary carcinoma of the thyroglossal duct cyst was suspected.
On a post-op CECT Scan of the neck, a 15x16 mm sized non-enhancing residual cystic lesion was noted in the left paramedic region at the floor or the mouth, deep in the mylohyoid muscle. Minimal peripheral hyperdensity was noted which was adjudged to be due to the vasculature. Serum thyroglobulin and Immunohistochemistry reports were ordered and a re-excision and total thyroidectomy procedure was planned.
Discussion
Thyroglossal Duct Cysts typically present as a mass at or around the hyoid with only about 20% of the cases reporting a suprahyoid mass. Typically, the TGDC is a midline swelling that elevates with deglutition and protrusion of the tongue unlike the TGDC in this patient was suprahyoid and fixed with no movement on deglutition or protrusion of the tongue.
Thyroglossal duct cyst carcinomas are found in less than 1% of the patients with TGDC and display a female predominance.[
6] Histopathological examination reveals that Papillary carcinoma is the most common malignancy (91.2%) found, followed by Squamous Cell Carcinoma (4.3%).[
1] TGDC carcinoma is diagnosed as an incidental finding on pathological examination is about 71.3% and most commonly presents asymptomatically.[
1] Their cause is unclear and there are no predisposing factors, i.e. neither clinical history nor physical examination findings can lead to a preoperative diagnosis.
While the origin of TGDC carcinomas is widely debated, two main schools of thought exist. ‘De Novo theory’ argues the origin of thyroid carcinomas in the TGDC. Supported by the fact that approximately 62% of the TDGCs are reported to have ectopic thyroid tissue in the cyst walls. his is further substantiated as medullary carcinoma of the thyroid (originates from parafollicular cells) has never been reported in a TGDC.[
7] On the contrary, the ‘Metastatic Theory’ argues that the papillary carcinoma of the TGDC represents the cystic metastases of the thyroid neoplasm as papillary carcinoma is the most common thyroid neoplasm and is known to spread to regional lymph nodes.[
8] The logical line of reasoning reinforces that although TDGC is lined by pseudostratified squamous epithelium or squamous epithelium, Squamous Cell Carcinomas only make up about 4.1% of TGDC malignancies.[
9]
The origin of TGDC Carcinoma is important from an academic point of view and imperative to developing standard treatment guidelines. While there is a debate as to the best management practices of a TGDC and/or TGDC Carcinoma, it is universally agreed that a Sistrunk procedure must be performed to excise the cyst, central part of the hyoid bone and the remainder of the tract and the tissue around it, from the foramen caecum to the thyroid gland.[
10,
11] As per Patel et al [
12], the only significant predictor of outcomes is the extent of the original procedure with thyroidectomy adding no significant benefit. This is further substantiated by the popular De Novo theory of the origin of the papillary carcinoma of the TGDC. Thyroid gland involvement in TGDC Carcinoma ranges from 33%-45%[
10], but this is misleading as the rate of incidental thyroid carcinoma being diagnosed on autopsy is also 30-35%.[
13,
14] However, total thyroidectomy can be performed to facilitate Radioactive Iodine Ablation (RIA), and hence various authors have recommended total thyroidectomy in addition to the Sistrunk procedure for TGDC carcinoma.[
15,
16,
17]
Conclusion
Thyroglossal duct cyst is one of the most common neck swellings, however, TGDC Carcinoma is very rare. There are no etiological factors and/or signs and symptoms that can aid in the pre-surgical diagnosis of TGDC Carcinoma. Papillary Carcinoma is the most common subtype identified followed by Squamous Cell Carcinoma. While the exact origin of the malignancy is unclear, the Sistrunk procedure remains the procedure of choice, which may be followed up by a total /near total thyroidectomy and RAI ablation, depending on the subtype of carcinoma.
Funding
None of the authors are financially interested in any of the products, devices or drugs mentioned in this manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
Ethical Statement
Being a case report study, there were no ethical issues and the IRB was notified about the topic and the case. Still, no formal permission was required as this was a record-based case report. Permission from the patient for the article has been acquired and ensured that their information or identity is not disclosed.
References
- Amos J, Shermetaro C. Thyroglossal Duct Cyst [Internet]. PubMed. Treasure Island (FL): StatPearls Publishing; 2020. Available from: https://www.ncbi.nlm.nih.gov/books/NBK519057/.
- Chou J, Walters A, Hage R, Zurada A, Michalak M, Tubbs RS, Loukas M. Thyroglossal duct cysts: anatomy, embryology and treatment. Surg Radiol Anat. 2013;35(10):875–81. [CrossRef]
- Peretz A, Leiberman E, Kapelushnik J, Hershkovitz E. Thyroglossal duct carcinoma in children: case presentation and literature review. Thyroid: Official Journal of the American Thyroid Association [Internet]. 2004 Sep 1 [cited 2023 Dec 25];14(9):777–85. Available from: https://pubmed.ncbi.nlm.nih.gov/15361266/.
- Lester D.R. Thompson, Herrera HB, Lau SK. Thyroglossal Duct Cyst Carcinomas: A Clinicopathologic Series of 22 Cases with Staging Recommendations. Head and Neck Pathology. 2016 Oct 4;11(2):175–85. [CrossRef]
- Falconieri G, Duilio Della Libera, Zanella M. Papillary Thyroid Carcinoma of the Thyroglossal Duct Cyst. International Journal of Surgical Pathology. 2001 Jan 1;9(1):65–71. [CrossRef]
- Hilger AW, Thompson S, Smallman LA, Watkinson J. Papillary carcinoma arising in a thyroglossal duct cyst: a case report and literature review. Journal of Laryngology and Otology. 1995 Nov 1;109(11):1124–7. [CrossRef]
- Balalaa N, Megahed M, Al Ashari M, Branicki F. Thyroglossal Duct Cyst Papillary Carcinoma. Case Reports in Oncology. 2011 Jan 29;4(1):39–43. [CrossRef]
- Seow Wan Tew, Reeve TS, Poole AG, Delbridge L. PAPILLARY THYROID CARCINOMA ARISING IN THYROGLOSSAL DUCT CYSTS: INCIDENCE AND MANAGEMENT. Anz Journal of Surgery. 1995 Oct 1;65(10):717–8. [CrossRef]
- Judd, ES. Thyroglossal-Duct Cysts and Sinuses. Surgical Clinics of North America [Internet]. 1963 Aug 1 [cited 2023 Dec 26];43(4):1023–32. Available from: https://www.sciencedirect.com/science/article/abs/pii/S0039610916370384?via=ihub.
- Rayess HM, Monk I, Svider PF, Gupta A, Raza SN, Lin HS. Thyroglossal Duct Cyst Carcinoma: A Systematic Review of Clinical Features and Outcomes. Otolaryngology–Head and Neck Surgery. 2017 Mar 21;156(5):794–802. [CrossRef]
- Sistrunk, WE. THE SURGICAL TREATMENT OF CYSTS OF THE THYROGLOSSAL TRACT. Annals of Surgery [Internet]. 1920 Feb 1 [cited 2023 Dec 26];71(2):121-122.2. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1410396/.
- Patel SG, Escrig M, Shaha AR, Singh B, Shah JP. Management of well-differentiated thyroid carcinoma presenting within a thyroglossal duct cyst. Journal of Surgical Oncology. 2002 Feb 21;79(3):134–9. [CrossRef]
- Martinez-Tello FJ, R. Martinez-Cabruja, Fernandez-Martin J, Lasso-Oria C, Ballestin-Carcavilla C. Occult carcinoma of the thyroid. A systematic autopsy study from Spain of two series was performed with two different methods. Cancer. 1993 Jun 15;71(12):4022–9. [CrossRef]
- Harach HR, Franssila KO, Wasenius VM. Occult papillary carcinoma of the thyroid. A “normal” finding in Finland. A systematic autopsy study. Cancer. 1985 Aug 1;56(3):531–8. [CrossRef]
- Miccoli P, Minuto MN, Galleri D, Puccini M, Berti P. Extent of Surgery in Thyroglossal Duct Carcinoma: Reflections on a Series of Eighteen Cases. Thyroid. 2004 Feb;14(2):121–3. [CrossRef]
- Kennedy TL, Whitaker M, Wadih G. Thyroglossal duct carcinoma: A rational approach to management. Laryngoscope. 1998 Aug 1;108(8):1154–8. [CrossRef]
- Heshmati HM, Vahab Fatourechi, Jon, Hay ID, Goellner JR. Thyroglossal Duct Carcinoma: Report of 12 Cases. 1997 Apr 1;72(4):315–9. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).