1. Introduction
The advent of coronavirus disease 2019 (COVID-19) in late 2019 marked a pivotal moment with far-reaching and devastating consequences, giving rise to an unprecedented surge in morbidity and mortality rates globally. This highly infectious and contagious virus, classified within the Coronaviridae family, swiftly traversed geographical boundaries, casting its shadow on every corner of the world and precipitating profound challenges for economies and healthcare systems alike (1,2). In March 2020, the Kingdom of Saudi Arabia bore witness to its initial case of COVID-19, a significant milestone that prompted swift and decisive actions by the Saudi Ministry of Health. Faced with the emergent threat, the ministry escalated preparations and implemented robust precautions to effectively control the outbreak and cater to the medical needs of the affected population. The strategic response included the allocation of resources across a network of more than 25 hospitals, boasting a collective capacity of 8,800 beds. This infrastructure encompassed not only 8,000 intensive care unit (ICU) beds but also 2,200 isolation beds dedicated to suspected and quarantined cases, illustrating a comprehensive and systematic approach to patient care during the pandemic (3,4,5). The magnitude of this concerted effort was paramount in successfully managing the expected influx of infected individuals. By proactively expanding healthcare resources and adhering to meticulous treatment guidelines, Saudi Arabia positioned itself to navigate the complexities of the pandemic and provide optimal care to those affected by COVID-19. This multifaceted response not only exemplifies the nation's commitment to public health but also serves as a noteworthy model for countries grappling with the challenges posed by the relentless spread of the virus.
The manifestation of coronavirus disease 2019 (COVID-19) is characterized by a spectrum of flu-like symptoms, encompassing fever, cough, myalgia, and gastrointestinal issues, as documented in various studies (6). While a substantial proportion of cases present with mild symptoms, it is noteworthy that approximately one-quarter of affected individuals undergo a more severe clinical trajectory, potentially progressing to the challenging stage of acute respiratory distress syndrome (ARDS). Alarmingly, about 5% of cases escalate to a critical condition, requiring specialized and intensive medical intervention (7). Critically ill COVID-19 patients confront a constellation of unique challenges that significantly compound the complexity of their medical condition. These challenges include but are not limited to acute respiratory failure characterized by resistance hypoxemia, coagulopathy, multi-system failure, and discernible alterations in both immunity and inflammatory responses (8). The intricate nature of these complications underscores the importance of a meticulous and attentive approach to patient management. As healthcare providers navigate the multifaceted landscape of critical COVID-19 cases, they are compelled to address the intricate interplay of diverse physiological systems, necessitating a comprehensive and nuanced care strategy to optimize patient outcomes. The heightened complexity of the clinical presentation underscores the critical need for a tailored and multidisciplinary approach to meet the distinctive challenges posed by severe manifestations of COVID-19.
The critical care management of patients grappling with severe manifestations of COVID-19 in the intensive care unit (ICU) necessitates the application of a multifaceted approach, incorporating not only generic measures but also drawing upon evidence-based medicine guidelines. One pivotal facet of this management involves the implementation of invasive mechanical ventilation (MV) as an integral therapeutic intervention, a strategy underscored by the evolving understanding of the disease dynamics and clinical outcomes (9). In the context of acute respiratory distress syndrome (ARDS), a condition encompassing diverse etiologies, mortality rates are influenced by an intricate interplay of various factors. Patient-specific variables, including co-morbidities, advanced age, the severity of hypoxemia, and the presence of co-existing organ failures, collectively contribute to shaping the trajectory and ultimate outcomes in ARDS cases (10). The recognition of these nuanced determinants underscores the imperative for a personalized and comprehensive approach to critical care management. As clinicians navigate the complexities inherent in severe COVID-19 cases, the integration of evidence-based guidelines and a nuanced understanding of individual patient profiles becomes paramount. The incorporation of invasive mechanical ventilation aligns with the evolving landscape of critical care interventions, emphasizing a patient-centered paradigm to enhance the prospects of favorable clinical outcomes.
Despite the growing body of research on the clinical characteristics of intensive care unit (ICU) patients in Saudi Arabia, a notable research gap persists, particularly in the realm of those necessitating mechanical ventilation. This study endeavors to address this lacuna by delving specifically into the attributes and treatment modalities deployed for critically ill COVID-19 patients admitted to ICUs, with a meticulous focus on individuals requiring mechanical ventilation. The overarching goal is to contribute nuanced insights that not only augment the existing literature on severe COVID-19 cases but also shed light on the distinctive challenges and intricacies associated with the management of this specific subgroup.
2. Materials and Methods
Our comprehensive investigation delved deeply into the landscape of COVID-19 ICU admissions at Aseer Central Hospital (ACH), strategically situated in the southern region of Saudi Arabia. Adopting a rigorous retrospective, noninterventional methodology, we meticulously scrutinized the medical charts and data of all patients who found themselves in the challenging realm of ICU admission due to COVID-19, with a particular emphasis on those necessitating crucial ventilation support. The ambit of our study extended to encompass hospitalized individuals aged 18 years and above, unequivocally diagnosed with COVID-19 through positive real-time polymerase chain reaction tests for SARS-CoV-2. Our data collection phase, spanning from August 2020 to April 2021, aimed to encapsulate a comprehensive snapshot of the evolving landscape of COVID-19 in the ICU setting. Following an assiduous process of data cleaning and the exclusion of cases not meeting our stringent inclusion criteria, our final study cohort manifested as a robust sample size, comprising 594 patients who intricately fit the specified criteria.
The granularity of our study extended beyond mere demographic details, as we meticulously gathered and organized data encompassing various facets of patients' profiles. This included in-depth information on age, gender, nationality, and the intricate tapestry of comorbidities that can significantly shape the clinical trajectory of COVID-19 cases. A specific lens was directed towards unraveling the ICU profile, probing into the diverse interventions undertaken within this critical care milieu. The overarching goal was to unearth insights into patient mortality, a pivotal outcome of interest, and to explore potential associations with blood group types. Such a nuanced exploration demanded meticulous attention to detail and a robust ethical framework, as underscored by the approval granted by the Institutional Review Board at Aseer Central Hospital and our dedicated research committee. This ethical imprimatur ensures the integrity and compliance of our study with the highest standards of research governance, thereby bolstering the credibility and reliability of our findings.
2.1. Data analysis
Following the extraction of data, a meticulous and iterative process unfolded, involving thorough revision and coding procedures. Subsequently, the data seamlessly transitioned into the statistical software IBM SPSS version 26 (SPSS, Inc. Chicago, IL), marking a pivotal phase in our analytical journey. In adherence to robust statistical principles, two-tailed tests were employed for the spectrum of statistical analyses, with a predefined threshold of a p-value less than 0.05 deemed as statistically significant. The utilization of descriptive statistics emerged as a linchpin in our analytical framework, particularly for scale and continuous variables such as laboratory findings. Mean values accompanied by standard deviations provided a comprehensive overview of the central tendencies within this domain. In parallel, frequency distributions and percentages assumed prominence in delineating the landscape of categorical variables, encompassing personal data and blood group information.
The exploration of factors intricately linked to mortality among COVID-19 patients hinged on a multifaceted approach. Cross-tabulation, Chi-square tests, and exact tests, tailored to accommodate small sample sizes, collectively formed the methodological arsenal deployed for this nuanced investigation. Logistic regression analysis, a robust statistical tool, was judiciously applied to quantify the magnitude of the relationship between blood group, Rh factor, and the rate of patients' mortality. In the pursuit of a comprehensive understanding, the findings were not merely confined to statistical metrics but were thoughtfully presented graphically. Mortality rates, co-morbidities, medication usage patterns, culture findings, and other pertinent variables were graphically depicted, providing a visual narrative that enhances interpretability and fosters a nuanced appreciation of the multifaceted interplay within our dataset. This meticulous analytical journey, characterized by methodological rigor and a commitment to comprehensive reporting, underscores the reliability and depth of our research endeavor
3. Results
This study included 594 COVID patients admitted to Aseer Central Hospital (ACH) ICU. The patients' ages ranged from 18 to 103 years, with a mean age of 60.5 ± 17.3 years. Among them, 398 (67%) were males, and only 5 (0.8%) were smokers (
Table 1).
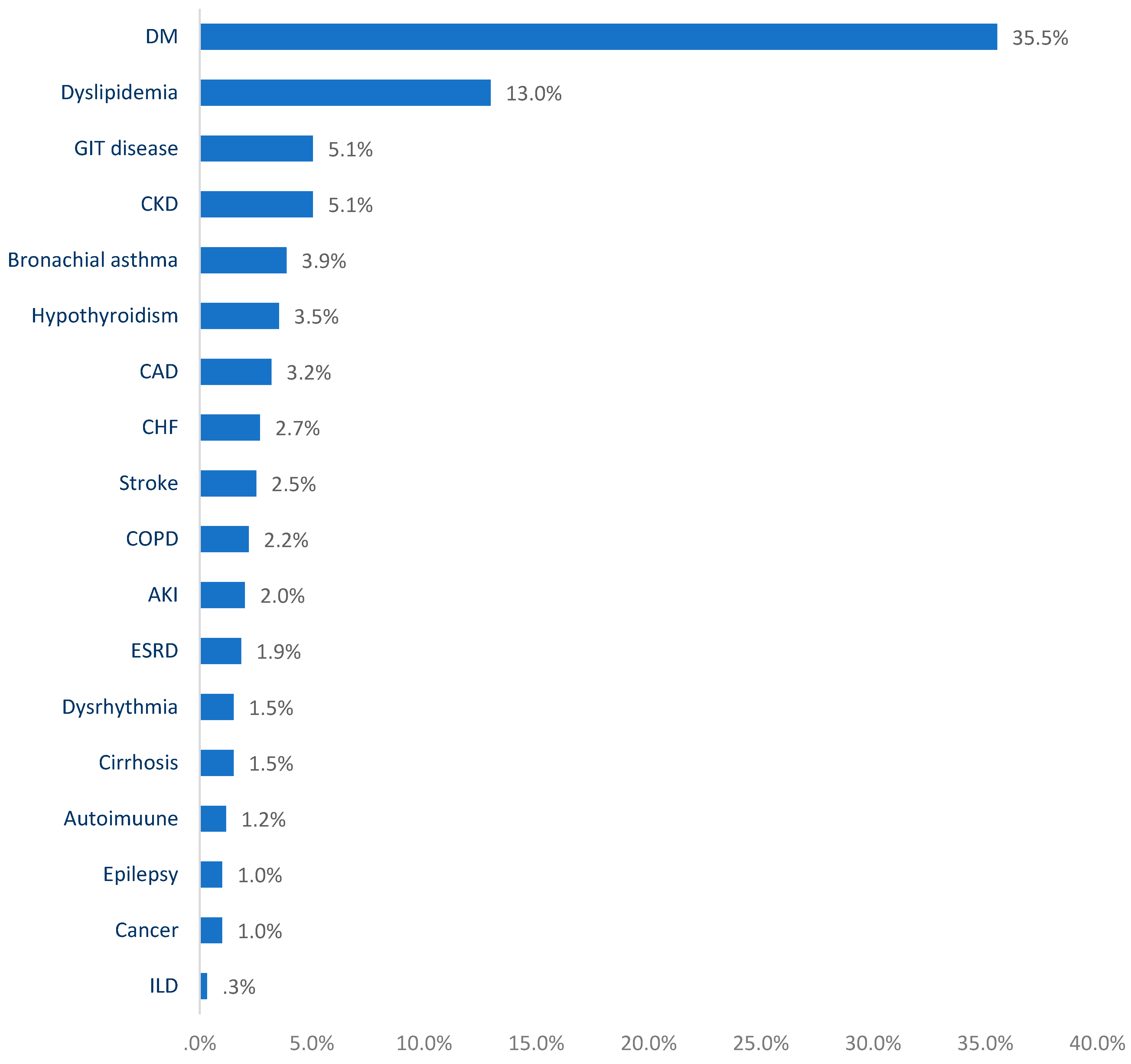
Figure 1 displays the prevalence of chronic diseases among COVID patients admitted to the ICU at Aseer Central Hospital (ACH), Saudi Arabia. The most commonly reported chronic health issues in this study included diabetes mellitus (35.5%), dyslipidemia (13%), gastrointestinal diseases (5.1%), chronic kidney disease (5.1%), bronchial asthma (3.9%), and hypothyroidism (3.5%).
Figure 2 illustrates the medications administered to COVID patients admitted to the ICU. Upon admission, 95.3% received antibiotics, 87.4% were prescribed anticoagulants, 78.3% received steroids, 75.3% were given antiviral drugs, and 55.4% received analgesics. Monoclonal antibodies (MABS) were administered to 20.4% of patients, and 14.5% received antiplatelet medication. The average laboratory findings of COVID patients admitted to Aseer Central Hospital (ACH) ICU are displayed. The blood glucose level (BGL) was recorded as 276.7 ± 12.1 mg/dl, creatinine as 2.6 ± 1.9 g/dl, erythrocyte sedimentation rate (ESR) as 62.8 ± 35.6, and C-reactive protein (CRP) as 60.4 ± 62.9 (
Table 2). Regarding chest X-ray findings, tracheostomy tubes were observed in 235 (98.7%) patients, while only 6 (2.5%) displayed signs of consolidation (
Table 2).
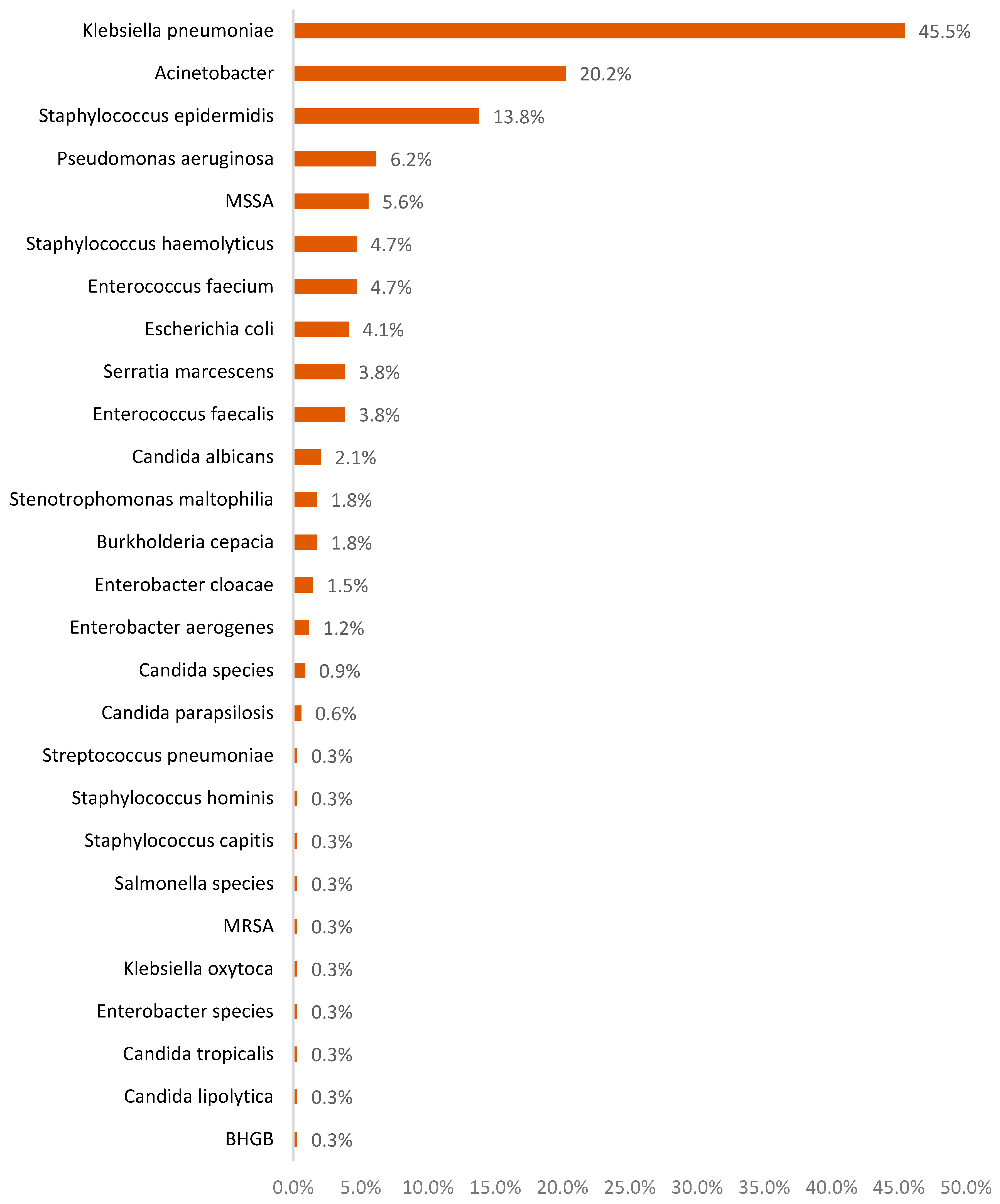
Almost 340 (57.2%) had positive culture findings. The most commonly isolated microorganisms included Klebsiella pneumoniae (45.5%), Acinetobacter (20.2%), Staphylococcus epidermidis (13.8%), Pseudomonas aeruginosa (6.2%), MSSA (5.6%), Staphylococcus haemolyticus (4.7%), and Enterococcus faecium (4.7%) (
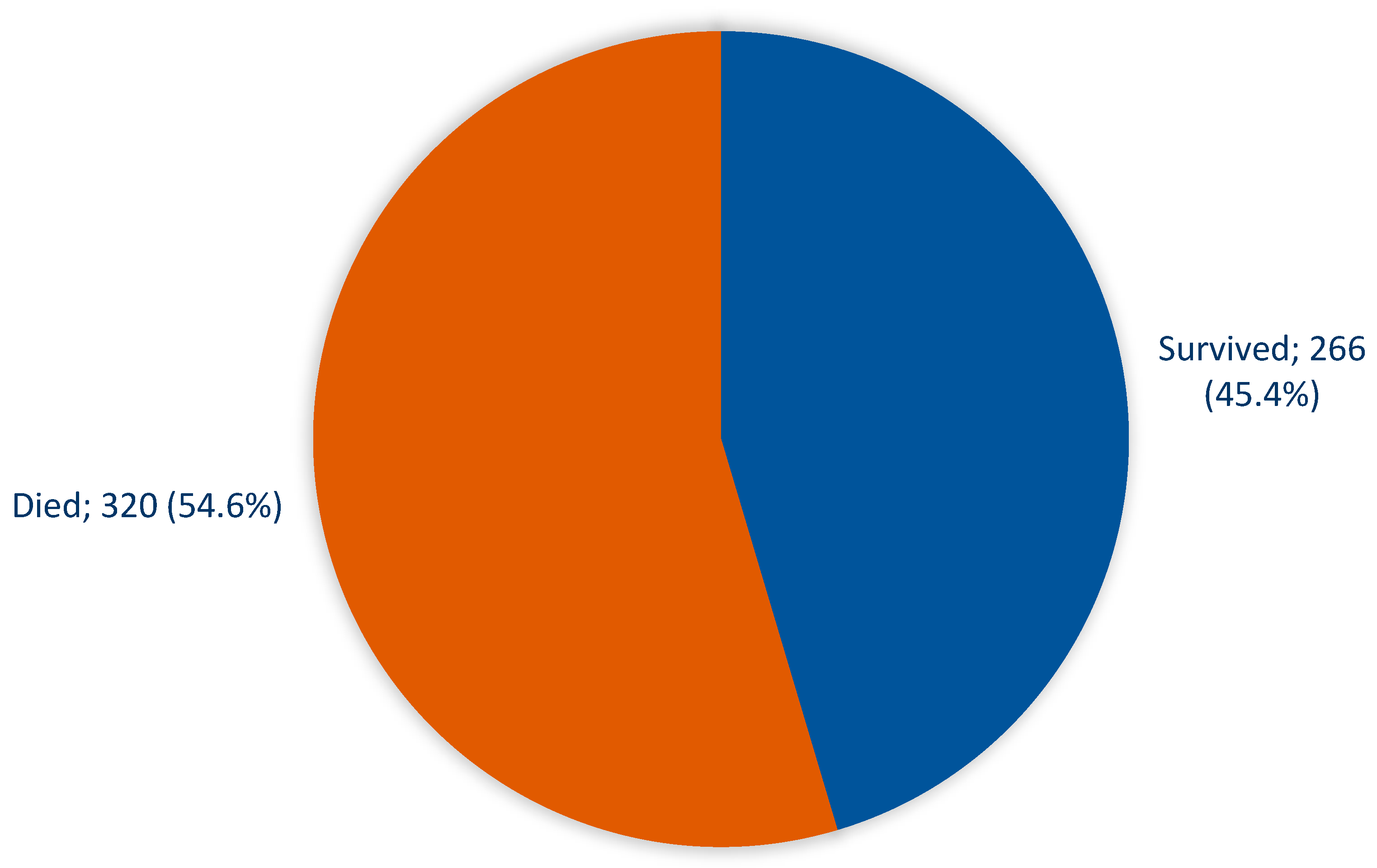
Figure 3). Among the patients, 320 (54.6%) died, while 266 (45.4%) survived (
Figure 4).
In this study, a significant correlation was found between age and mortality, with 75% of patients aged 70 years or more succumbing to the disease compared to 22.5% of those under 40 years (P=.001). Patients with positive culture results also had a higher mortality rate of 67.4% compared to 37.7% for those with negative culture findings (P=.001), Other factors examined did not show significant relations with COVID patients' mortality (
Table 3).
4. Discussion
The imperative for intensive care unit (ICU) admission arises for a substantial proportion, approximately 25%, of hospitalized individuals grappling with the complexities of COVID-19. Recognizing and delineating the characteristics of high-risk individuals within this cohort assume paramount significance, as this discernment holds the key to mitigating mortality rates and elevating overall clinical outcomes in cases where the severity of the disease necessitates such intensive care interventions (11,12,13). Against this backdrop, the primary objective of this paper is to delve into the multifaceted realm of critically ill COVID-19 patients admitted to the ICU. More specifically, our focus extends to those within this critical subset who necessitate mechanical ventilation, a pivotal aspect of the intensive care landscape. Beyond a mere exploration of their characteristics and management nuances, our study embarks on a meticulous investigation into the factors intricately associated with patient survival within this highly specific and clinically intricate subgroup. By shedding light on the unique challenges and dynamics of this subset, we aspire not only to contribute to the enriched understanding of severe COVID-19 cases but also to offer nuanced insights that can inform tailored clinical strategies and ultimately enhance the outcomes for patients navigating the complexities of mechanical ventilation in the ICU setting.
In consonance with the trends delineated in various published studies, a substantial two-thirds majority within our study cohort comprises male individuals, a consistent observation mirrored in both national and international reports (14,15,16). An intriguing demographic nuance emerges as we delve into the age distribution of our intensive care unit (ICU)-admitted COVID-19 patients, where a noteworthy over 50% fall into the age bracket of 60 years or older. This demographic alignment resonates harmoniously with insights gleaned from an amalgamation of local and international studies, underscoring the predilection of older individuals toward more severe disease manifestations and complications. The predisposition of older patients to experience heightened disease severity and complications stems from a complex interplay of factors, including the presence of multiple comorbidities, compromised immunity, and an elevated susceptibility to various complications. This intricate web of vulnerabilities necessitates a nuanced understanding to facilitate targeted care strategies, ultimately culminating in improved outcomes for this particularly vulnerable population (14,17,18,19). Recognizing and comprehensively addressing these multifaceted risk factors not only enriches our understanding of the demographic dynamics within our study but also reinforces the imperative of tailored interventions to enhance the care trajectory and clinical outcomes for older COVID-19 patients admitted to the ICU.
Certainly, the intricate interplay between comorbidities and the trajectory of COVID infections is an undeniable facet of the evolving narrative surrounding this global health crisis (11,20). The surge in the prevalence of diabetes mellitus (DM) emerges as a formidable public health challenge, wielding a profound impact on long-term morbidity and mortality rates. Within the Gulf region, Saudi Arabia takes center stage, marked by a record of the highest diabetes-related deaths, as underscored by a pivotal study (21). The present investigation casts a revealing light on this landscape, uncovering that more than one-third of the patients under scrutiny bore the burden of a DM diagnosis. This prevalence aligns seamlessly with broader epidemiological evidence indicating that nearly half of individuals aged over 55 in Saudi Arabia grapple with type 2 diabetes mellitus (DM2). Importantly, this pattern resonates within the demographic contours of our patient age group (22). Significantly, our study's documentation of DM prevalence surpassed that reported in a study conducted in Alahsa (14), where approximately 20% of COVID patients exhibited DM, albeit with a focus outside the intensive care unit (ICU) context. Furthermore, our findings align with another influential cohort study on COVID patients, shedding light on the pervasive nature of DM in this cohort, with almost half of the patients grappling with this metabolic condition (17). This nuanced exploration not only enriches our understanding of the intricate relationship between DM and COVID-19 but also situates our findings within the broader landscape of regional and global studies, thereby contributing to a more comprehensive comprehension of the multifaceted challenges posed by the intersection of diabetes and severe COVID-19 manifestations.
Numerous studies have delved into the intricate correlations between various laboratory parameters and the nuanced landscape of COVID-19. This expansive spectrum of parameters spans procalcitonin (PCT), lactic acid, the percentage of lymphocytes, D-dimer levels, C-reactive protein (CRP), erythrocyte sedimentation rate (ESR), and serum lactate dehydrogenase (LDH), each serving as a sentinel marker in the intricate interplay of the disease's pathophysiology (23,24). In the comprehensive laboratory assessments conducted on our patient cohort, conspicuous elevations were observed in the renal profile, hepatic enzymes, and inflammatory markers, with particular emphasis on heightened ESR and CRP levels. These findings not only echo the established literature but also fortify the strong association documented in prior studies between these inflammatory markers and COVID-19 mortality.
The elevated prominence of inflammation within the pathophysiological milieu of critically ill COVID-19 patients is further accentuated by our results, hinting at a substantial role played by these inflammatory markers in shaping the clinical trajectory of severe cases. Intriguingly, our findings also posit CRP as a potential independent player in influencing ICU admission, adding a nuanced layer to our understanding of the prognostic significance of this marker (25, 26, 19, 14). As standard practice aligns with the administration of dexamethasone to moderate to severely hypoxic COVID-19 patients, a strategy linked to improved outcomes, our study dovetails into this broader treatment paradigm. Furthermore, the amalgamation of antibiotics with hydroxychloroquine, as highlighted in a multicenter study, demonstrated reduced mortality in COVID-19 cases. Notably, adherence to health protocols and local guidelines was underscored by the remarkable statistic that over two-thirds of our studied patients received antibiotics and steroids, further contributing to the contextual richness of our findings (27,28,29).
This investigation has brought to the forefront a stark reality — a substantial mortality rate among severely ill COVID-19 patients admitted to the intensive care unit (ICU) and reliant on mechanical ventilation. Within this critical cohort, a discernible correlation between age and mortality has emerged, unveiling the nuanced impact of age on the trajectory of severe cases. Intriguingly, patients with positive culture outcomes, indicative of concomitant bacterial infections, displayed a notably elevated mortality rate, further accentuating the intricate web of factors influencing outcomes in critically ill patients. Notably, our findings harmonize with a spectrum of local studies conducted in Saudi Arabia and find resonance in a sweeping analysis encapsulating 178,568 COVID-19 deaths across 16 countries. This expansive investigation illuminates a striking reality — an approximately 8-fold higher mortality rate among individuals aged 55 to 64 and an astonishing over 62-fold higher incidence rate among those aged 65 or older, compared to their counterparts aged 54 or younger (16,18,19,24,25,30). This age-dependent vulnerability can be attributed to immunosenescence, a phenomenon where the performance of innate immune cells in older individuals undergoes compromise. This leads to a diminished efficacy in viral clearance and sets the stage for an imbalanced immune response (31). The profound implications of age on the mortality dynamics uncovered in our study find resonance in the broader global context, emphasizing the need for targeted interventions and heightened vigilance in managing severe cases, particularly in the elderly population grappling with the intricate challenges of immunosenescence.
5. Conclusions
In conclusion, this study provides critical insights into the clinical and epidemiological aspects of COVID-19 patients admitted to the ICU in a Saudi Arabian hospital. The research underscores the impact of age, comorbidities, laboratory markers, and treatment interventions on patient outcomes, emphasizing the significance of tailored management strategies in this context.
Author Contributions
Conceptualization, Ali, Mushary, Najla and Khalid; methodology, Ali, Mushary, Osama, Abdullah and Ahmed; software, Ali, Mushary and Najla; validation, Ali, Mushary, Khalid and Osama; formal analysis, Ali, Mushary, Osama, Abdullah and Ahmad; investigation, Ali and Mushary; resources, Ali, Ahmed, Najla, Osama and Abdullah; data curation, Ali, Khalid, Mushary and Ahmed; writing—original draft preparation, Ali, Mushary, Khalid, Najl, Abdullah and Osama; writing—review and editing, Ali, Mushary, Najla, Khalid, Abdullah, Osama and Ahmed; visualization, Ali, Mushary, Abdullah, Najla and Osama; supervision, Ali and Mushary; project administration,Ali and Mushary;. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Ethical approval was secured from the Institutional Review Board at Aseer Central Hospital, IRB Log No.:REC-11-03-2022.
Informed Consent Statement
All subjects gave their informed consent for inclusion before they participated in the study. The study was conducted in accordance with the Declaration of Helsinki, and the protocol was approved by the Ethics Committee of Board at Aseer Central Hospital, IRB Log No.:REC-11-03-2022.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Benvenuto D, Giovanetti M, Ciccozzi A, Spoto S, Angeletti S, Ciccozzi M: The 2019-new coronavirus epidemic: evidence for virus evolution. J Med Virol. 2020, 92:455-459. [CrossRef]
- Lai C, Shih T, Ko W, Tang H, Hsueh P: Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019 (COVID- 19): the epidemic and the challenges. Int J Antimicrob Agents. 2020, 55:105924. [CrossRef]
- Saudi Ministry of Health. MOH reports first case of Coronavirus infection 2021 [cited 2 January 2021]. https:// www. moh. gov. sa/ en/ Minis try/ Media Center/ News/ Pages/ News-2020-03-02-002. aspx.
- Barry M, Ghonem L, Alsharidi A, Alanazi A, Alotaibi NH, Al-Shahrani FS, et al.: Coronavirus disease-2019 pandemic in the Kingdom of Saudi Arabia: mitigation measures and hospital preparedness. J Nat Sci Med. 2020, 3:155. [CrossRef]
- Saudi Ministry of Health. ICU Triage, Admission, and Discharge Criteria during the COVID 19 pandemic V2 2020 [cited 30 April 2021]. https:// www. moh. gov. sa/ Minis try/ Media Center/ Publi catio ns/ Docum ents/ ICUCrite ria-during. pdf.
- Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, et al.: Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020, 395:507-13.
- Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al.: Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020, 395:1054-62.
- Lillicrap D: Disseminated intravascular coagulation in patients with 2019-nCoV pneumonia. J Thromb Haemost. 2020, 18:786-7.
- Claesson J, Freundlich M, Gunnarsson I, et al.: Scandinavian clinical practice guideline on mechanical ventilation in adults with the acute respiratory distress syndrome. Acta Anaesthesiol Scand. 2015, 59:286-297. [CrossRef]
- Murthy S, Gomersall CD, Fowler RA. Care for critically Ill patients with COVID-19. JAMA. 2020;323:1499-1500. [CrossRef]
- Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, Wang B, Xiang H, Cheng Z, Xiong Y. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus infected pneumonia in Wuhan, China. JAMA.2020;323(11):1061–9. [CrossRef]
- Vahidy FS, Drews AL, Masud FN, Schwartz RL, Boom ML, Phillips RA. Characteristics and outcomes of COVID-19 patients during initial peak and resurgence in the Houston metropolitan area. JAMA.2020;324(10):998–1000. [CrossRef]
- Guan W-J, Ni Z-Y, Hu Y, Liang W-H, Ou C-Q, He J-X, Liu L, Shan H, Lei C-L, Hui DS. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708–20. [CrossRef]
- Saad Alhumaid, Abbas Al Mutair, Zainab Al Alawi, Khulud Al Salman, Nourah Al Dossary, Ahmed Omar, Clinical features and prognostic factors of intensive and non-intensive 1014 COVID-19 patients: an experience cohort from Alahsa, Saudi Arabia, European Journal of Medical Research, (2021) 26:47. [CrossRef]
- Shruti Gupta, MD, MPH; Salim S. Hayek, MD;WeiWang, PhD; Lili Chan, MD, MSCR; Kusum S. Mathews, MD, MPH, MSCR; Michal L. Melamed, MD, MHS; Samantha K. Brenner,MD, MPH; Factors Associated With Death in Critically Ill Patients With Coronavirus Disease 2019 in the US, JAMA Intern Med. doi:10.1001/jamainternmed.2020.3596, Published online July 15, 2020.
- Al-Omari A, Alhuqbani WN, Zaidi ARZ, Al-Subaie MF, AlHindi AM, Abogosh AK, Alrasheed AK, Alsharafi AA, Alhuqbani MN, Salih S. Clinical characteristics of non-intensive care unit COVID-19 patients in Saudi Arabia: a descriptive cross-sectional study. J Infect Public Health. 2020;13(11):1639–44. [CrossRef]
- Aljuaid M, Alotair H, Alnajjar F, Alonazi W,Sharaf H, Sheshah E, et al. (2022) Risk factors associated with in-hospital mortality patients with COVID-19 in Saudi Arabia. PLoS ONE 17(6): e0270062. [CrossRef]
- Al-Otaiby M, Almutairi KM, Vinluan JM, Al Seraihi A, Alonazi WB, Qahtani MH, Aljeri T, Alhumud MA, Alobaidi N and Alhurishi SA (2022) Demographic Characteristics, Comorbidities, and Length of Stay of COVID-19 Patients Admitted Into Intensive Care Units in Saudi Arabia: A Nationwide Retrospective Study. Front. Med. 9:893954. [CrossRef]
- Saleh Alghamdi, Clinical characteristics and treatment outcomes of severe (ICU) COVID-19 patients in Saudi Arabia: A single centre study, Saudi Pharmaceutical Journal 29 (2021) 1096–1101. [CrossRef]
- Alenazi AM, Alqahtani BA. National and regional prevalence rates of hypertension in Saudi Arabia: A descriptive analysis using the national survey data. Front Public Health. 2023 Apr 4;11:1092905. PMID: 37081959; PMCID: PMC10110943. [CrossRef]
- Aljulifi MZ. Prevalence and reasons of increased type 2 diabetes in Gulf cooperation council countries. Saudi Med J. 2021;42:481–90. [CrossRef]
- Jarrar M, Abusalah MAH, Albaker W, Al-Bsheish M, Alsyouf A, Al-Mugheed K, Issa MR, Alumran A. Prevalence of Type 2 Diabetes Mellitus in the General Population of Saudi Arabia, 2000-2020: A Systematic Review and Meta-Analysis of Observational Studies. Saudi J Med Med Sci. 2023 Jan-Mar;11(1):1-10. Epub 2023 Jan 14. PMID: 36909010; PMCID: PMC9997860. [CrossRef]
- Tan L, Kang X, Ji X, et al. Validation of predictors of disease severity and outcomes in COVID-19 patients: a descriptive and retrospective study. Med. 2020;1(1):128–138.e3. [CrossRef]
- Alharthy A, Aletreby W, Faqihi F, et al. Clinical characteristics and predictors of 28-day mortality in 352 critically ill patients with COVID-19: a retrospective study. J Epidemiol Glob Health. 2021;11(11):98. [CrossRef]
- Ansari KA, Alwazzeh MJ, Alkuwaiti FA, Farooqi FA, Al Khathlan N, Almutawah H, Alahmed M, Alfaraj H, Aljarrash A, Almadhary J, Alwarthan S, Alsahlawi AM, Almashouf AB, Alqasim M, Alkuwaiti E. Early Determinants of Mortality in Hospitalized COVID-19 Patients in the Eastern Province of Saudi Arabia. Int J Gen Med. 2022 Feb 16;15:1689-1701. PMID: 35210838; PMCID: PMC8858956. [CrossRef]
- Sadeghi A, Eslami P, Dooghaie Moghadam A, Pirsalehi A, Shojaee S, Vahidi M, Soheili A, Ghanimat F, Keshmiri Y, Abdi S, Zali MR. COVID-19 and ICU admission associated predictive factors in Iranian patients. Caspian J Intern Med. 2020 Fall;11(Suppl 1):512-519. PMID: 33425268; PMCID: PMC7780877. [CrossRef]
- Rosenberg ES, Dufort EM, Udo T, Wilberschied LA, Kumar J, Tesoriero J, et al., Association of treatment with hydroxychloroquine or azithromycin with in-hospital mortality in patients with COVID-19 in New York State. Jama. 2020 Jun 23; 323(24):2493–502. PMID: 32392282. [CrossRef] [PubMed]
- Arshad S, Kilgore P, Chaudhry ZS, Jacobsen G, Wang DD, Huitsing K, et al., Treatment with hydroxychloroquine, azithromycin, and combination in patients hospitalized with COVID-19. International journal of infectious diseases. 2020 Aug 1; 97:396–403. PMID:32623082. [CrossRef]
- Wootton D. Dexamethasone in hospitalized patients with COVID-19. New England Journal of Medicine.2021 Feb 25; 384(8):693–704. PMID: 32678530. [CrossRef]
- Yanez ND, Weiss NS, Romand J-A, Treggiari MM. COVID-19 mortality risk for older men and women. BMC Public Health. 2020; 20(1):1–7. [CrossRef]
- Kang SJ, Jung SI. Age-related morbidity and mortality among patients with COVID-19. Infection & chemotherapy. 2020 Jun; 52(2):154. PMID: 32537961. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).