Submitted:
01 December 2023
Posted:
04 December 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
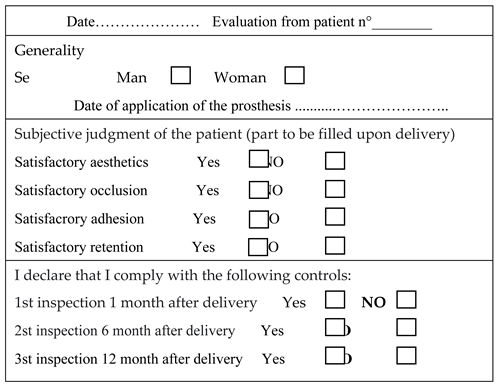
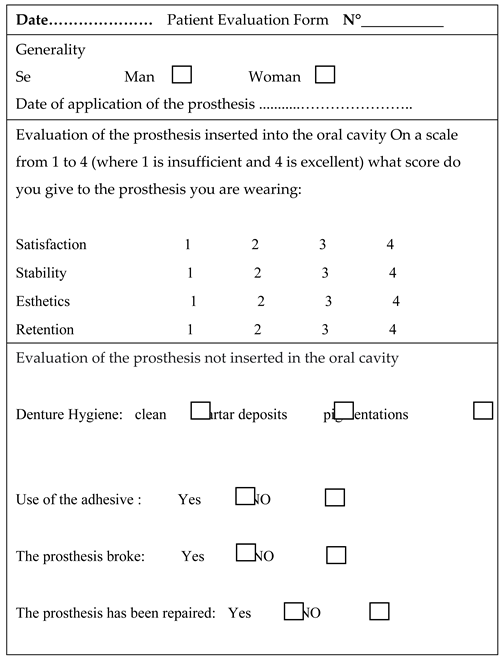
2. Materials and Methods
- presence of partial edentulism classifiable as Kennedy class II;
- absence of tori that could affect the adaptability of the prosthesis;
- non-inclined residual elements (excessive undercut);
- absence of para-functions;
- presence of stable soft tissues not affected by periodontal disease or mucogingival lesions;
- adequate depth of the roots of the abutment teeth;
- informed consent of the patient and acceptance of the therapeutic rehabilitation plan with partial removable prosthesis and compliance with the dentist's instructions.
- age between 65 and 85 years.
- poor oral hygiene and lack of patient compliance;
- smoking habits (>10 cigarettes/day);
- subjects suffering from oral pathologies;
- active periodontal disease;
- anomalies in the anatomy of the labial frenulum (which can interfere with the insertion and adaptability of the removable prosthesis);
- drug addictions;
- psychiatric pathologies;
- subjects disbarred less than 5 years ago;
- subjects on bisphosphonate therapy;
- deep bite;
- failure to consent to prosthetic rehabilitation and to comply with the dentist's instructions.
3. Results
4. Discussion
5. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Elfadil S, Kahatab A, Cronin E, O'Mahony A. Chairside technique for addition of teeth to an acrylic partial denture. A clinical report. Heliyon. 2023 Jul 7;9(7):e18040. PMID: 37483718; PMCID: PMC10362310. [CrossRef]
- Goswami M, Chauhan N. Prosthetic Management with Removable Partial Dentures in Pediatric Dental Care: Case Series. Int J Clin Pediatr Dent. 2023 May-Jun;16(3):534-540. PMID: 37496936; PMCID: PMC10367292. [CrossRef]
- Goguta L, Frandes M, Candea A, Ille C, Jivanescu A. Impact of unilateral removable partial dentures versus removable partial dentures with major connector on oral health-related quality of life of elder patients: a clinical study. BMC Oral Health. 2023 Mar 29;23(1):182. PMID: 36991435; PMCID: PMC10061744. [CrossRef]
- Wang WR, Xie R, Niu LN, Feng ZH, Zhao YM. Novel Digital Mouth Preparation Technique for Fabricating Implant-Retained Removable Partial Dentures with Distal Extension: a Case Report. Chin J Dent Res. 2023 Jun 23;26(2):113-117. PMID: 37395523. [CrossRef]
- Jayaraman S, Singh BP, Ramanathan B, Pazhaniappan Pillai M, MacDonald L, Kirubakaran R. Final-impression techniques and materials for making complete and removable partial dentures. Cochrane Database Syst Rev. 2018 Apr 4;4(4):CD012256. PMID: 29617037; PMCID: PMC6494560. [CrossRef]
- Kumari KS, K S A. An Esthetic Approach for Rehabilitation of Long-Span Edentulous Arch Using Artificial Intelligence. Cureus. 2023 May 7;15(5):e38683. PMID: 37292565; PMCID: PMC10244077. [CrossRef]
- Rues S, Tasaka A, Fleckenstein I, Yamashita S, Rammelsberg P, Boehm S, Schwindling FS. Fit and Retention of Cobalt-Chromium Removable Partial Denture Frameworks Fabricated with Selective Laser Melting. J Funct Biomater. 2023 Aug 8;14(8):416. PMID: 37623661; PMCID: PMC10456016. [CrossRef]
- Akinyamoju CA, Ogunrinde TJ, Taiwo JO, Dosumu OO. Comparison of patient satisfaction with acrylic and flexible partial dentures. Niger Postgrad Med J. 2017 Jul-Sep;24(3):143-149. PMID: 29082902. [CrossRef]
- Campbell SD, Cooper L, Craddock H, Hyde TP, Nattress B, Pavitt SH, Seymour DW. Removable partial dentures: The clinical need for innovation. J Prosthet Dent. 2017 Sep;118(3):273-280. Epub 2017 Mar 23. PMID: 28343666. [CrossRef]
- Bruna Benso, Ana C. Kovalik, Janaina H. Jorge & Nara H. Campanha (2013) Failures in the rehabilitation treatment with removable partial dentures, Acta Odontologica Scandinavica, 71:6, 1351-1355. [CrossRef]
- Hatayama T, Chiba A, Kainose K, Nakajima M, Hosaka K, Wakabayashi N, Foxton RM, Tagami J. Stress distribution in tooth resin core build-ups with different post-end positions in alveolar bone level under two kinds of load directions. Dent Mater J. 2018 Jun 8;37(3):474-483. Epub 2018 Feb 8. PMID: 29415970. [CrossRef]
- S. Ceraulo. Ritenzione a lamella su modifica della placca prossimale. Una nuova progettazione ideata dall’autore della ricerca in riabilitazioni Protesiche parziali rimovibili scheletrate di III classe. Protech, Anno 2, n°5, pag. 21-24, Ottobre 2001.
- S. Ceraulo. Follow-up a due anni della PPS con ritezioni a lamelle. Supplemento Doctor OS, Anno XV, n° 4, aprile 2004.
- Straulino E, Scarpazza C, Spoto A, Betti S, Chozas Barrientos B, Sartori L. The Spatiotemporal Dynamics of Facial Movements Reveals the Left Side of a Posed Smile. Biology (Basel). 2023 Aug 23;12(9):1160. PMID: 37759560; PMCID: PMC10525663. [CrossRef]
- Al-Kaisy N. Measurement of vertical anterior teeth display and lip position at smiling in Kurdish population. Age and gender-based evaluation. Heliyon. 2023 Aug 28;9(9):e19465. PMID: 37809926; PMCID: PMC10558590. [CrossRef]
- Cheng JH, Hsu YC, Lee TY, Li RW. Factors affecting perception of laypeople and dental professionals toward different smile esthetics. J Dent Sci. 2023 Apr;18(2):739-746. Epub 2022 Dec 13. PMID: 37021227; PMCID: PMC10068377. [CrossRef]
- Saffarpour A, Ghavam M, Saffarpour A, Dayani R, Fard MJ. Perception of Laypeople and Dental Professionals of Smile Esthetics. J Dent (Tehran). 2016 Mar;13(2):85-91. PMID: 27928236; PMCID: PMC5139935.
- Al-Rafee MA. The epidemiology of edentulism and the associated factors: A literature Review. J Family Med Prim Care. 2020 Apr 30;9(4):1841-1843. PMID: 32670928; PMCID: PMC7346915 . [CrossRef]
- Gabiec K, Bagińska J, Łaguna W, Rodakowska E, Kamińska I, Stachurska Z, Dubatówka M, Kondraciuk M, Kamiński KA. Factors Associated with Tooth Loss in General Population of Bialystok, Poland. Int J Environ Res Public Health. 2022 Feb 18;19(4):2369. PMID: 35206557; PMCID: PMC8872086. [CrossRef]
- Shah PD, Badner VM. Association between asthma and severe tooth loss in the adult population of the United States. J Asthma. 2022 Mar;59(3):462-468. Epub 2020 Dec 24. PMID: 33356681. [CrossRef]
- Hasegawa K, Sakurai A, Mizuki M, Kurita H, Tsukahara T, Nomiyama T. Association between the number of teeth and incident pre-diabetes among middle-aged adults with periodontal disease: a retrospective cohort analysis of Japanese claims data. BMJ Open. 2023 Nov 19;13(11):e075527. PMID: 37984959; PMCID: PMC10660919. [CrossRef]
- D'Souza NL, Hajhamid B, Somogyi-Ganss E. Postinsertion adjustment appointments and their association with cast removable partial denture survival. J Prosthet Dent. 2023 Aug;130(2):238.e1-238.e7. Epub 2023 Jul 6. PMID: 37419711. [CrossRef]
- Cumbo, E.; Messina, P.; Gallina, G.; Scardina, G.A. An Experimental Method to Add New Prosthetic Teeth in the Removable Partial Denture Framework: TIG Cold Welding and Preformed Pins. Prosthesis 2023, 5, 1120-1128. [CrossRef]
- Al-Dwairi ZN, Taani DS, Naseeb AZ, Al-Haj Husain N, Özcan M, Lynch E. Evaluation of Clinical Periodontal Parameters of Abutment Teeth Supporting Distal-Extension Base Removable Partial Dentures: A Cross-sectional Study. Eur J Prosthodont Restor Dent. 2023 Jun 15. Epub ahead of print. PMID: 37318323. [CrossRef]
- Tregerman I, Renne W, Kelly A, Wilson D. Evaluation of removable partial denture frameworks fabricated using 3 different techniques. J Prosthet Dent. 2019 Oct;122(4):390-395. Epub 2019 Apr 1. PMID: 30948301. [CrossRef]
- Carneiro Pereira AL, Bezerra de Medeiros AK, de Sousa Santos K, Oliveira de Almeida É, Seabra Barbosa GA, da Fonte Porto Carreiro A. Accuracy of CAD-CAM systems for removable partial denture framework fabrication: A systematic review. J Prosthet Dent. 2021 Feb;125(2):241-248. Epub 2020 Mar 5. PMID: 32147252. [CrossRef]
- Ahmed N, Abbasi MS, Haider S, Ahmed N, Habib SR, Altamash S, Zafar MS, Alam MK. Fit Accuracy of Removable Partial Denture Frameworks Fabricated with CAD/CAM, Rapid Prototyping, and Conventional Techniques: A Systematic Review. Biomed Res Int. 2021 Sep 6;2021:3194433. PMID: 34532499; PMCID: PMC8440078. [CrossRef]
- Takaichi A, Fueki K, Murakami N, Ueno T, Inamochi Y, Wada J, Arai Y, Wakabayashi N. A systematic review of digital removable partial dentures. Part II: CAD/CAM framework, artificial teeth, and denture base. J Prosthodont Res. 2022 Jan 11;66(1):53-67. Epub 2021 Jan 26. PMID: 33504722. [CrossRef]
- Jafarpour D, Feine JS, Morris M, Souza RF. Patient-reported outcomes and clinical performance of CAD/CAM removable dentures: A scoping review. Int J Prosthodont. 2023 Oct 12;0(0). Epub ahead of print. PMID: 37824115. [CrossRef]
- Ali IE, Tanikawa C, Chikai M, Ino S, Sumita Y, Wakabayashi N. Applications and performance of artificial intelligence models in removable prosthodontics: A literature review. J Prosthodont Res. 2023 Oct 5. Epub ahead of print. PMID: 37793819. [CrossRef]
- Iannello, G.; Fiorillo, L.; D’Amico, C.; Minervini, G.; Terranova, A.; Cervino, G. Presenting a Protocol for Dental Implant Restorations. Prosthesis 2023, 5, 1153-1170. [CrossRef]
- Shen X, Zhang C, Jia X, Li D, Liu T, Tian S, Wei W, Sun Y, Liao W. TranSDFNet: Transformer-Based Truncated Signed Distance Fields for the Shape Design of Removable Partial Denture Clasps. IEEE J Biomed Health Inform. 2023 Oct;27(10):4950-4960. Epub 2023 Oct 5. PMID: 37471183. [CrossRef]
- Pordeus MD, Gasparetto GD, Machado LMR, Noritomi PY, Costa RMBD, Chappuis-Chocano AP, Venante HS, Junior JFS, Porto VC. A New Proposal for Calibrated Gauges for Removable Partial Dentures: A Finite Element Analysis. J Contemp Dent Pract. 2022 Dec 1;23(12):1230-1236. PMID: 37125521. [CrossRef]
- Zhang N, Mao B, Dai Y, Chen S, You Z, Zhang J, Chen X, Dong H, Yue L, Yu H. Audit to assess the quality of 916 prosthetic prescriptions of removable partial dentures. Hua Xi Kou Qiang Yi Xue Za Zhi. 2023 Jun 1;41(3):315-322. English, Chinese. PMID: 37277798; PMCID: PMC10317851. [CrossRef]
- Jayaraman S, Singh BP, Ramanathan B, Pazhaniappan Pillai M, MacDonald L, Kirubakaran R. Final-impression techniques and materials for making complete and removable partial dentures. Cochrane Database Syst Rev. 2018 Apr 4;4(4):CD012256. PMID: 29617037; PMCID: PMC6494560. [CrossRef]
- Radford PJ, Walton J, McManus R. Should dental technicians play a greater role in the education of foundation dentists? Br Dent J. 2020 Nov;229(10):653-654. Epub 2020 Nov 27. PMID: 33247254. [CrossRef]
- Juszczyk AS, Clark RK, Radford DR. UK dental laboratory technicians' views on the efficacy and teaching of clinical-laboratory communication. Br Dent J. 2009 May 23;206(10):E21; discussion 532-3. PMID: 19444251. [CrossRef]


| Dentist 1 | Age | Sex | Abutment teeth |
| 1 | 66 | M | 14, 11, 21, 22, 23, 27 |
| 2 | 68 | M | 17, 16, 13, 12, 11, 21, 22, 23, 24 |
| 3 | 67 | W | 15, 14, 13, 11, 21, 22, 23, 27 |
| 4 | 76 | W | 14, 13, 11, 21, 22, 23, 26, 27 |
| Dentist 2 | |||
| 5 | 69 | W | 17, 14, 13, 11, 21, 22, 24 |
| 6 | 72 | W | 15, 13, 12, 11, 21, 23, 27 |
| 7 | 74 | M | 14, 11, 21, 22, 23, 27 |
| 8 | 72 | M | 17, 14, 13, 11, 21, 22, 23, 24 |
| Dentist 3 | |||
| 9 | 71 | W | 15, 14, 23, 24, 27 |
| 10 | 76 | W | 15, 14, 11, 21, 23, 24, 27 |
| 11 | 68 | M | 15, 13, 12, 11, 21, 23, 27 |
| 12 | 67 | M | 13, 12, 11, 21, 22, 23, 27 |
| Dentist 4 | |||
| 13 | 70 | W | 14, 13, 11, 21, 23, 27 |
| 14 | 73 | W | 17, 13, 12, 11, 21, 22, 23, 24, 25 |
| 15 | 76 | M | 14, 13, 12, 22, 23, 26, 27 |
| 16 | 82 | M | 14, 13, 12, 11, 22, 23, 24, 27 |
 |
 |
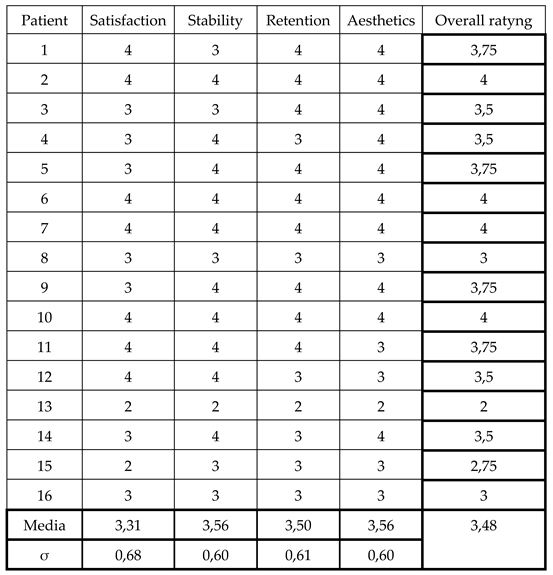 |
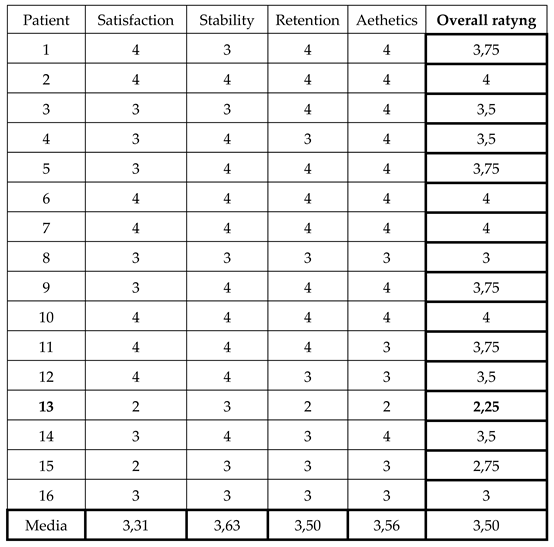
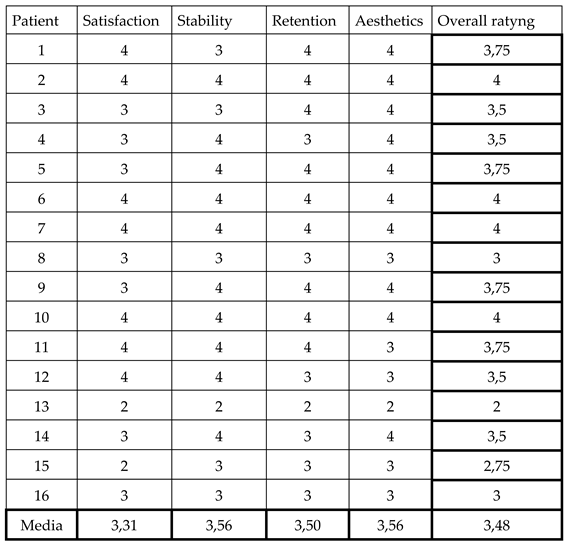
| Reference values | Satisfaction | Stability | Retention | Aesthetics |
| 1- 2,99 | Not satisfied | Not stable | He wasn't retentive | Not aesthetic |
| 3- 3,99 | Satisfied | Stable | Retentve | Aesthetics |
| 4 | Very satisfied | Stable | Very retentive | Very aesthetic |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).




