INTRODUCTION
Bronchiolitis is an acute viral infection of the lower respiratory tract that affects infants and young children. It represents the most common cause of acute respiratory failure in infants (age <12 months) and the leading cause of infant hospitalization in developed countries [
1]. Bronchiolitis accounts for up to 15–17% of all hospitalizations in children younger than 2 years, and 15% of emergency department presentations in infants [
2]. Respiratory syncytial virus (RSV) is the most common causative agent, accounting for 60–80% of all cases. Rhinovirus (RV), Parainfluenza virus, Influenza virus, Metapneumovirus (MPV), and Adenovirus have also been reported [
3,
4,
5,
6].
Seasonal variations in RSV infectivity, that is the highest during winter months in temperate zones, have been well described [
7,
8,
9].
Bronchiolitis is generally a self-limiting condition, but can lead to severe respiratory distress and potentially culminate in acute respiratory failure, especially in infants aged less than 12 months, preterm infants (born at gestational age less than 37 weeks), or with underlying comorbidities, such as chronic lung or heart diseases, neurological conditions, immunodeficiency, exposure to cigarette smoke and disadvantaged socioeconomic status [
10,
11,
12]. On the contrary, breastfeeding is associated with lower incidence and severity of lower respiratory tract disease and several studies have confirmed how longer duration of breastfeeding is associated with better clinical outcome of bronchiolitis [
13].
Diagnosis of bronchiolitis is based on clinical history and physical examination [
10]. Since there is no effective treatment for bronchiolitis, cornerstones of management are mostly supportive, consisting of fluid management and respiratory support [
10,
11,
12,
14]. Pharmacological interventions, such as nebulized bronchodilators, local or systemic steroids and antibiotics, have limited or no evidence of efficacy and generally are not recommended. As treatments are limited, preventive measures are needed to reduce morbidity and mortality, especially from RSV infections. Environmental measures are crucial in preventing and limiting bronchiolitis spreading. Moreover, pharmacological immunoprophylaxis with palivizumab has been proven beneficial to populations at increased risk for RSV infection–related complications, such as preterm babies and those affected by chronic lung or heart diseases, and it is currently available only for these specific infants [
15].
Standard oxygen supplementation in bronchiolitis is provided by nasal cannula (NC) and is upgraded to continuous positive airway pressure (CPAP) or invasive ventilation, if needed. In recent years, High-Flow Nasal Cannula oxygen therapy (HFNC), a non-invasive respiratory support supply, has emerged as a promising method to provide oxygen to children with bronchiolitis. Initially restricted to neonatal and pediatric intensive care units (NICUs and PICUs), over the last decade HFNC has migrated to emergency departments, inpatient pediatric wards, and patient transfers [
16,
17,
18].
Evidence suggests that the use of HFNC in bronchiolitis is limited to rescue therapy after failure of standard NC only in infants who are hypoxic. Different from previously, recent available data show no significant benefits for children treated with HFNC compared with NC or CPAP and suggest that HFNC produces no relevant differences in duration of hospitalization, days with oxygen supplementation and rate of admissions to Pediatric Intensive Care Unit () compared to NC [
16,
18,
20,
21]. Furthermore, some observational studies suggest that HFNC reduces respiratory work and may decrease need of intubation, but does not reduce intensive care rate of admissions [
22,
23].
However more studies are needed to evaluate the role of HFNC out of the PICU setting, as there is still a lack of guidelines to standardize the use of HFNC in children with respiratory failure.
Our local health authority (ASL TO4), in Piedmont, north-west of Italy, includes 174 municipalities, extending over a wide area of around 3165 square kilometers characterized by a great geographical variability, from high Alpine mountains to urban areas. Total population of this area is 504,467 people and the healthcare system is organized into five districts, with a great heterogeneity in demography, population density, geography and infrastructures. General Emergency Department and Pediatric Unit are present in three Spoke hospitals of Ciriè, Chivasso and Ivrea. To provide uniformity of care with an evidence-based approach, in 2013 the first “Diagnostic Therapeutic Assistance Pathway for bronchiolitis in pediatric age” was drawn up. Afterwards, it has been updated in 2016 and 2020.
Every year a palivizumab administration program is carried out in our three Pediatric Units, according to the Italian Society of Neonatology recommendations.
All three Pediatric Units of ASL TO4 are equipped with high-flow oxygen supply systems.
The aims of the present study were: 1) to describe the percentage of therapeutic success in bronchiolitis treated in Spoke hospitals of ASL TO4 over two consecutive bronchiolitis seasons, from 2021 to 2023, and 2) to evaluate clinical and biological differences between RSV positive (RSV+) and RSV negative (RSV-) patients, represented from patient-related factors (i.e. patient’s age, prematurity, weight for gestational age) and infection-related factors (i.e. presence of fever, duration of supplemental oxygen therapy, both low-flow oxygen and HFNC, use of antibiotic or steroid therapy, intravenous hydration and need to be transferred to a Hub hospital with a PICU, or a NICU).
PATIENTS AND METHODS
We retrospectively reviewed the clinical features of infants aged less than 12 months referred to our Pediatric Units of Chivasso, Cirié and Ivrea for acute bronchiolitis requiring hospitalization over two consecutive bronchiolitis seasons (from September 1, 2021 to March 31, 2022 and from September 1, 2022 and March 31, 2023).
We collected data about clinical and epidemiological characteristics (age at onset, gender, gestational age, birth weight, comorbidities, weight at admission, diet, previous respiratory infections, fever), laboratory, microbiology and radiograph results, and short-term outcomes (length of hospital stay, complications, Hub hospital transfer).
For etiological diagnosis, nasal swabs for RSV and nasopharyngeal swabs for SARS-CoV2 were performed in all patients. When available, nasopharyngeal swabs for Influenza virus, Adenovirus and Rhinovirus were performed.
Blood cells count, C-reactive protein and chest X-ray were performed according to clinical choice.
Treatment during hospitalization (low- or high-flow oxygen supplementation, nebulized therapy, steroids, antibiotics, and intravenous hydration) and discharge therapy data were recorded in all patients. All parents gave their consent for treatment and data registration in an anonymous dataset by signing a specific consent form.
Statistical analysis
Statistical analysis included only patients at the first episode of bronchiolitis; for patients hospitalized for a second episode of bronchiolitis an extra summary table had been added.
Univariate analysis was performed with the Chi-square or Fisher’s test for dichotomous variables, for continuous variables the ANOVA test for nonparametric measures was used. To define probability of success, the Kaplan-Meier statistics was used24. The difference between groups was calculated by log-rank test25. To identify independent factors (if any), we adopted logistic regression26.
The univariate analysis was conducted by VassarStats (Statistical Computation Web Site) while the Kaplan-Meier statistics together with the logistic regression by the NCSS software for Windows (
https://www.ncss.com/). P value below 0.05 was defined as statistically significant.
RESULTS
Overall, 1331 patients were admitted to the three ASL TO4 Pediatric wards from September 1, 2021 to March 31, 2022 and from September 1, 2022 to March 31, 2023. Among these, 192 infants aged 0-12 months were admitted due to the first episode of acute bronchiolitis (14.4% of all hospitalizations, 43.6% of all hospitalizations in infants <12 months). General characteristics of our study population are resumed in
Table 1. A specific table describing the characteristics of infants with a second episode of bronchiolitis in the same timeframe was added (
Table 4).
The median age of our patients was 2 months (range 0 to 11 months) and males were more represented than females (60% vs 40%). Gestational age was known in 90% of hospitalized children. Among these, preterm infants accounted for about 13%. Seventeen preterm patients (68%) had a gestational age between 35+0 and 36+6 weeks, while 7 (28%) had a gestational age between 30+0 and 34+6 weeks and one (4%) was born at a gestational age less than 29 weeks. Bronchopulmonary dysplasia was detected in one patient (0.5% of all patients), while no chronic heart nor neurological conditions or immunodeficiency were recorded. 136 infants (71% of all) were born appropriate for gestational age (AGA), 16 infants (8%) small for gestational age (SGA) and 14 patients (7%) large for gestational age (LGA). Breastfeeding was recorded in 123 infants (64%), while formula feeding in 43 patients (22%) and 17 infants (9%) had already been weaned when admitted to hospital (data not available in 5%). No data about other risk factors for bronchiolitis (presence of siblings, smoking exposure, family's socioeconomic status…) were available in medical records.
Twelve patients (6% of all) had comorbidities (congenital kidney anomalies) or personal medical history of neonatal disorders (i.g. anemia, hypotonia, cerebral ventricular dilation, cephalocele, neonatal sepsis, neonatal invasive or non-invasive respiratory support).
A pathogen was detected in 129 of the 192 patients (67%). The most commonly detected agent was RSV (66% of all infants), without differences between the two study periods (65% in 2021-22, 67% in 2022-23). Other observed pathogens were Influenza virus in one patient, Streptococcus pneumoniae in one patient, Adenovirus, Rhinovirus and Haemophilus Influenzae simultaneously detected in another patient. One patient aged < 1 month resulted positive for both Coronavirus SARS-CoV2 and RSV; one patient was positive for both RSV and Epstein-Barr virus.
One fourth of all children presented with fever, with no differences between RSV positive and negative patients (24% vs 25%, respectively). Nebulised hypertonic saline 3% was used in 77% of patients and corticosteroids (oral or iv) in 13% of infants; no differences were observed between RSV positive and negative patients.
Laboratory, X-ray findings and treatment during hospitalization are resumed in
Table 2. Short-term hospitalization outcomes are shown in
Table 3.
In our series we could not find statistically significant differences between RSV-positive and RSV-negative groups, except for the greater use of antibiotics in the RSV-negative group (P=0.004) and the higher probability of complications in the RSV-negative group (P=0.03).
We recorded a trend for higher need of HFNC in the RSV-positive patients (P=0.06). In our cohort we observed that 68% of RSV-positive patients (86/127) were breastfed.
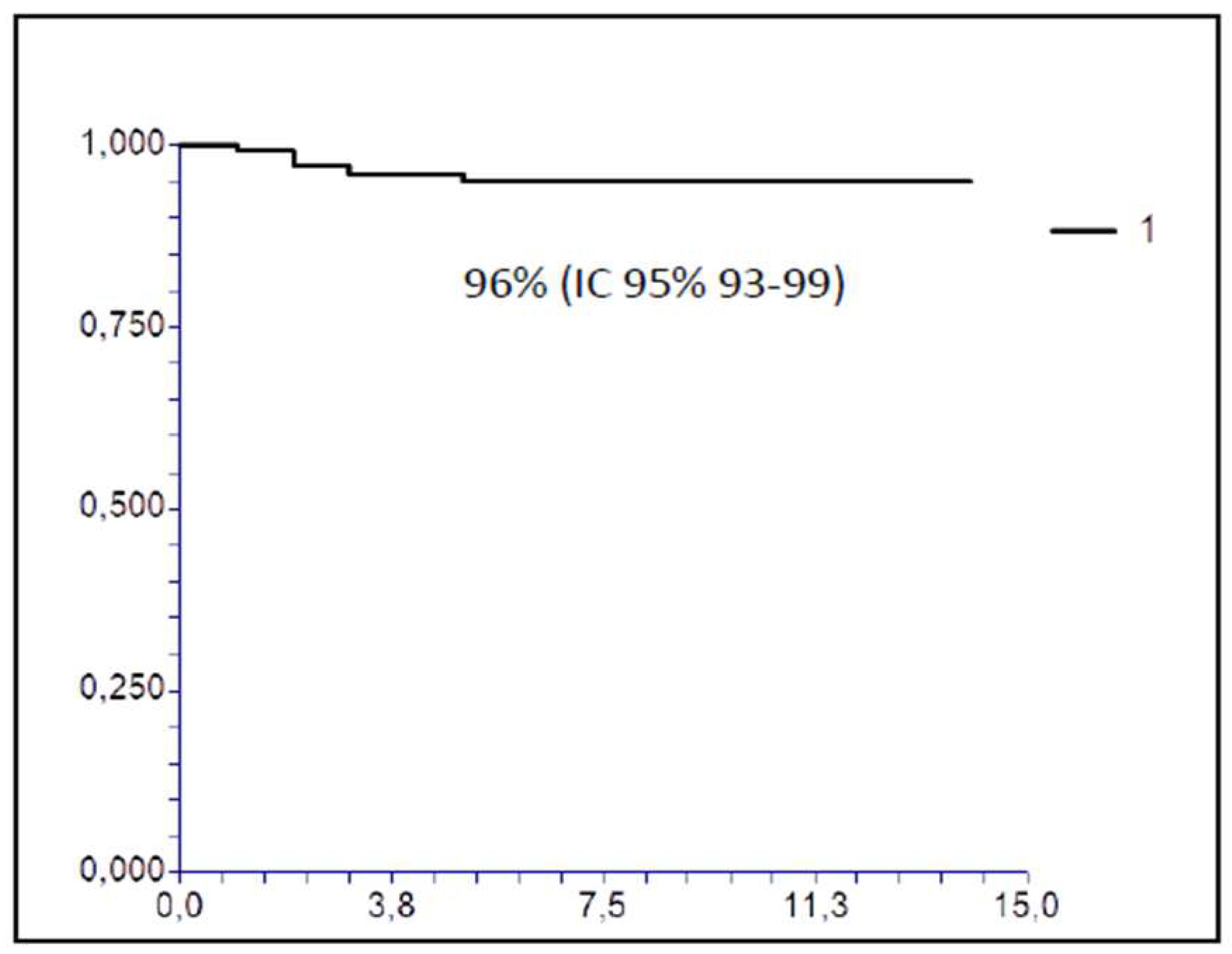
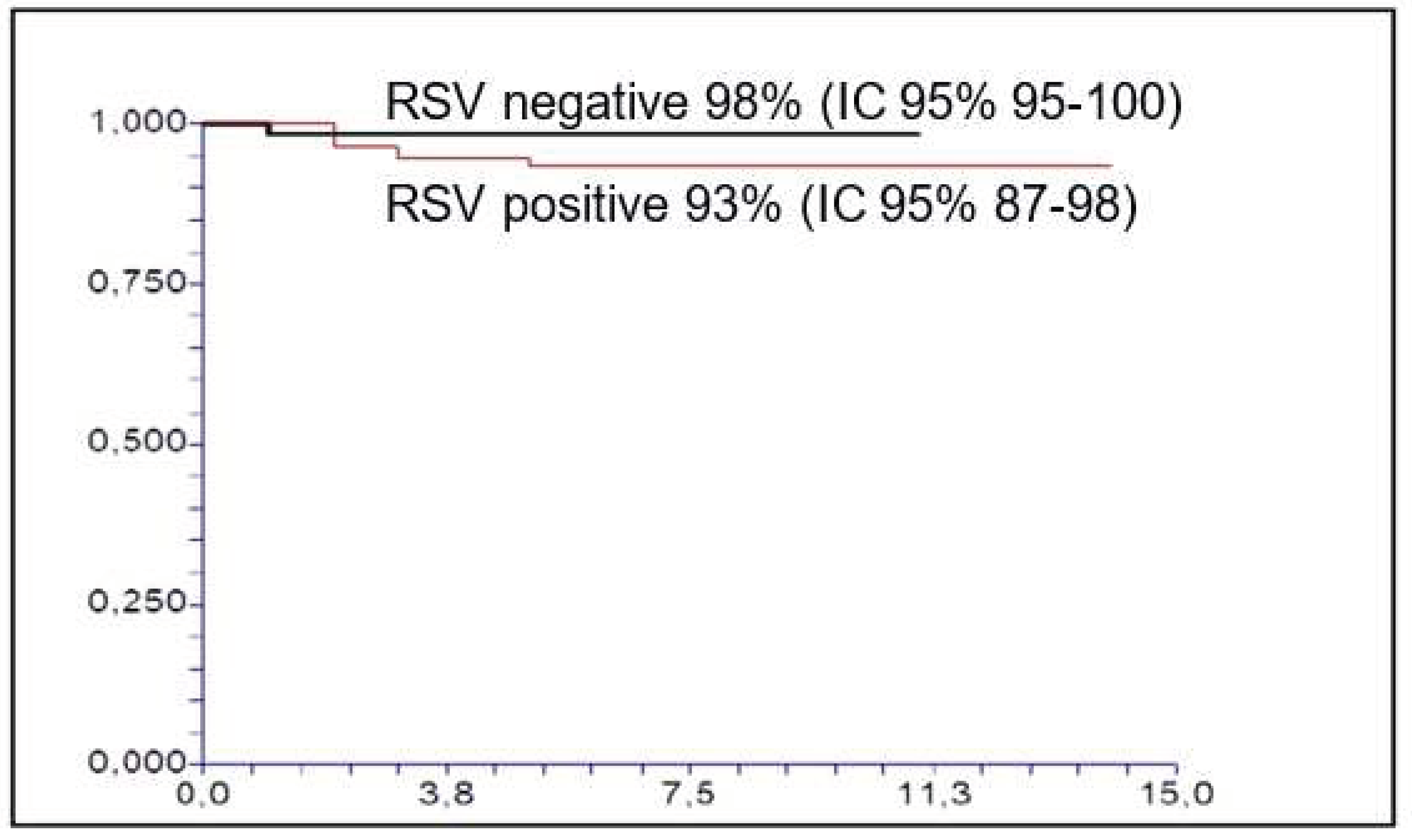
Figure 1 and
Figure 2 report the probability of treatment success (discharge to home without transfer to a Hub hospital with PICU or NICU): 96% for all patients (95% CI 93-99), 94% (95% CI 87-98) for RSV-positive and 98% (95% CI 95-100, P=NS) for RSV-negative patients when we stratify according to RSV infection.
As reported in
Table 4, nine infants had a second episode characterized by respiratory distress with crackles and wheezing over the observed period. Most of them were born at term, aged 1-3 months, breastfed and resulted RSV-negative. For these patients, the first bronchiolitis episode was RSV-positive in 4 patients (45%), while Rhinovirus was identified in one (11%).
Two patients had a personal medical history of neonatal disorders (cerebral ventricular dilation, neonatal sepsis). Three infants were febrile and two underwent chest radiography. Nebulised hypertonic saline 3% was used in 67% of patients.
As the small number of patients, we did not observe statistically significant differences between RSV-positive and RSV-negative infants, except for HFNC that was utilized more in RSV-positive patients than in RSV-negative ones.
Table 4.
Demographic and epidemiological characteristics of infants with a second episode of bronchiolitis.
Table 4.
Demographic and epidemiological characteristics of infants with a second episode of bronchiolitis.
| |
|
All patients
N (%)
9 (100) |
VRS+
N (%)
3 (100) |
VRS –
N (%)
6 (100) |
P value |
| Gender |
Male |
6 (67) |
1 (33) |
5 (83) |
0.46 |
| |
Female |
3 (33) |
2 (67) |
1 (17) |
|
| Prematurity |
Yes |
1 (11) |
1 (33) |
0 |
0.33 |
| |
No |
7 (78) |
2 (67) |
5 (83) |
|
| |
Unknown |
1 (11) |
0 (0) |
1 (17) |
|
| Months at diagnosis |
<1 |
0 |
0 |
0 |
0.31 |
| |
1-3 |
8 (89) |
3 (100) |
5 (83) |
|
| |
4-6 |
1 (11) |
0 (0) |
1 (17) |
|
| |
7-12 |
0 (0) |
0 (0) |
0 (0) |
|
| CRP higher level (mg/dl) |
|
3.3 (0.06-67.6) |
1.9 (0.6-30) |
12.3 (0.34-67.6) |
0.33 |
| pCO2 higher level (mmHg) |
|
48.6 (41.1-61) |
48.9 (41.1-59.9) |
48 (42.2-61) |
0.80 |
| Hospitalization day |
|
5 (2-11) |
9 (2-11) |
5 (3-6) |
0.32 |
| Low-Flow Oxygen |
Yes |
5 (55) |
2 (67) |
3 (50) |
1 |
| |
No |
4 (44) |
1 (33) |
3 (50) |
|
| High-Flow Oxygen |
Yes |
3 (33) |
3 (33) |
0 (0) |
0.011 |
| |
No |
6 (67) |
0 (0) |
6 (100) |
|
| High-Flow Oxygen days |
|
5 (1-8) |
5 (1-8) |
NA |
NA |
| Fraction of inspired Oxygen % |
|
40 (25-50) |
40 (25-50) |
NA |
NA |
| Need to transfer to a Hub hospital |
Yes |
1 (11) |
1 (33) |
0 (0) |
0.33 |
| |
No |
8 (89) |
2 (67) |
6 (100) |
|
Table 5 reports the univariate (Kaplan-Meier) analysis with the probability of treatment success of bronchiolitis (discharge to home without transfer to a Hub hospital with a PICU or a NICU) as endpoint.
All infants who did not receive oxygen therapy or required only low-flow oxygen support were discharged to home. Among patients treated with HFNC oxygen support, 19% needed to be transferred to a Hub hospital (P=0.005).
Patient’s age was the second statistically significant variable related to the outcome: patients aged less than 1 month had a lower probability of treatment success (83%) than older infants (97% in children aged 1-3 months, 100% in children aged 4-6 months and 94% in children older than 6 months, P=0.045).
We observed a trend for a better outcome with the use of antibiotics (P=0.06), that was more frequent in RSV-negative patients. The outcome was not related to causative agent, gender, children’s growth, presence of fever, pCO2 value, use of steroids or intravenous hydration (data not shown).
On multivariate analysis, the patient's age (P=0.022) and the need of HFNC support (P<0.0000001) have been confirmed to be independent factors. (
Table 6)
DISCUSSION
Our study described the characteristics of infants aged less than 12 months hospitalized for bronchiolitis in the three ASL TO4 Pediatric Units over two consecutive seasons (September-March 2021-2023).
Most infants with bronchiolitis were previously healthy. Among risk factors, bronchodysplasia was detected in 0.5% and prematurity in 13% of infants. This rate was lower than those reported in recent Italian and USA studies (24.5% and 33%, respectively) [
7,
29] and could be influenced by the short distance between our Pediatrics Units and the Hub Hospital: infants might have directly access to Hub center were they undergo follow-up for prematurity or other risk conditions.
In our area all infants at increased risk for RSV infection–related complications received palivizumab according to the Italian Society of Neonatology recommendations [
11].
In this retrospective study, from available data in medical records, we were not able to collect information about other risk factors for bronchiolitis (siblings, smoking exposure, family’s socioeconomic status…) that can influence the disease course.
We confirm the prevalent role of RSV as causative agent of bronchiolitis requiring hospitalization (detected in 66% of hospitalized infants).
In our study, RSV-positive patients underwent less frequently to administration of antibiotic therapy than RSV-negative ones: even if no differences were observed in patients with fever between the two groups, the different use of antibiotics was due to a more frequent finding of complications in RSV-negative population such as pneumonia, bacterial superinfection, postinfectious neutropenia and apnea. Among protective factors for infections, we observed that about half of RSV-negative patients were breastfed.
Recent data about breastfeeding in ASL TO4, collected during pediatric health check in 2021, show that 68% of infants are exclusively breastfed in the first month of life, 60% at 2-3 months and 54% at 4-5 months. In our cohort 64% of patients were breastfed; even if 67% of RSV-positive were exclusively breastfed, the absolute protective role of breastfeeding should be evaluated by analyzing the type of feeding among infants with bronchiolitis treated at home.
Despite the low prevalence of risk factors, more than 70% of children required oxygen supplementation, mostly low-flow oxygen. This is due to the fact that mild bronchiolitis are usually treated by Pediatricians at home or, eventually, in hospital in Brief Intensive Observation areas before being discharged at home.
A trend towards a higher use of HFNC was observed more frequently in RSV-positive infants, presumably because they had a more severe clinical picture. An increased use of HFNC for bronchiolitis after the SARS-CoV-2 pandemic was observed in a recent Italian study [
27]. In the pandemic period these authors noticed an increase of RSV bronchiolitis (from 61% in 2018-19 to 80% in 2021-22), without a more severe clinical course (intubation rate and length of stay did not change), concluding that the increasing use of HFNC was mostly caused by a more aggressive therapeutic approach of pediatricians.
A recent Italian study of Istituto Superiore di Sanità demonstrated a change in RSV subtype circulation in the post-pandemic period [
31]. In 2021-2022 the intense RSV peak was driven by RSV-A and was not associated with increased clinical severity of bronchiolitis in children younger than one year with respect to previous seasons. RSV-B predominance was instead reported in 2022-23 causing a more severe disease, due in part to RSV-B specific immune debt, in part to new RSV-B genetic strains that might have enhanced RSV-B pathogenicity.
However, in our series, we did not observe an increase in RSV bronchiolitis in the period 2022-23 in comparison with the previous one (2021-22). In our region it was not possible to obtain the RSV subtype.
All transferred infants were refractory to HFNC and the majority of them were RSV-positive (88% of cases). In our study, patients with a more severe clinical picture, who required the use of HNFC, had similar duration of oxygen supply and hospitalization to that of patients with a milder clinical picture, confirming the usefulness of this therapeutic approach21.
Despite a trend towards a higher incidence of RSV+ bronchiolitis in the total breastfed population, most RSV-positive infants less than <1 month who were transferred to Hub hospital were fed with infant formula. This is consistent with other studies in which human milk showed a protective role in RSV-positive infants. Jang
et al demonstrated a lower severity of RSV infection requiring oxygen therapy in breastfed hospitalized infants than in formula fed ones [
13]. We did not demonstrate a significant correlation between HFNC treatment and breastfeeding (P=0.19).
Multivariate analysis confirmed that age <1 month and the need of HFNC support were independently associated with a worse clinical outcome and a more frequent need for transfer to Hub hospital with a PICU or a NICU, according to literature [
28,
30].
In our setting, after the failure of low-flow oxygen administration, HFNC treatment represented a rescue therapy in bronchiolitis permitting to treat moderate to severe bronchiolitis also in Pediatric Units in Spoke hospitals.
RSV bronchiolitis was a more severe illness, mostly in infants younger than 1 month of age. In our cohort of hospitalized infants with acute bronchiolitis, disease outcome was influenced by infant’s age and type of treatment, being HFNC treatment an indicator of illness severity. Infant’s age >1 month and no need of HFNC predicted a better outcome, avoiding infant transfer to hub hospital with a PICU or a NICU.
CONCLUSIONS
In our study, age less than 1 month and the need of treatment with HFNC were prognostic factors associated with a worse outcome.
Recent wide and increasing use of HFNC in pediatric inpatients improved management of bronchiolitis in Spoke hospitals, reducing transfer to a Hub hospital provided with Intensive Care Units.
In our series, the majority of patients hospitalized for RSV bronchiolitis were patients not at risk. A different prophylactic strategy is necessary to reduce the social costs of this disease.
References
- Meissner, H.C. Viral Bronchiolitis in Children. N Engl J Med. 2016, 374, 62–72. [Google Scholar] [CrossRef]
- Hasegawa, K.; Tsugawa, Y.; Brown, D.F.; Mansbach, J.M.; Camargo, C.A., Jr. Trends in bronchiolitis hospitalizations in the United States, 2000–2009. Pediatrics 2013, 132, 28–36. [Google Scholar] [CrossRef] [PubMed]
- Ricci, V.; Delgado Nunes, V.; Murphy, M.S.; Cunningham, S. Guideline Development Group and Technical Team. Bronchiolitis in children: summary of NICE guidance. BMJ 2015, 350, h2305. [Google Scholar] [CrossRef] [PubMed]
- Wolf, D.G.; Greenberg, D.; Kalkstein, D.; Shemer-Avni, Y.; Givon-Lavi, N.; Saleh, N.; Goldberg, M.D.; Dagan, R. Comparison of human metapneumovirus, respiratory syncytial virus and influenza A virus lower respiratory tract infections in hospitalized young children. Pediatr Infect Dis J 2006, 25, 320–324. [Google Scholar] [CrossRef]
- Mansbach, J.M.; McAdam, A.J.; Clark, S.; Hain, P.D.; Flood, R.G.; Acholonu, U.; Camargo, C.A., Jr. Prospective multicenter study of the viral etiology of bronchiolitis in the emergency department. Acad Emerg Med 2008, 15, 111–118. [Google Scholar] [CrossRef] [PubMed]
- Boivin, G.; De Serres, G.; Cộté, S.; Gilca, R.; Abed, Y.; Rochette, L.; Bergeron M.G.; Déry, P.
- Human metapneumovirus infections in hospitalized children. Emerg Infect Dis 2003, 9, 634–640. [CrossRef] [PubMed]
- Barbati, F.; Moriondo, M.; Pisano, L.; Calistri, E.; Lodi, L.; Ricci, S.; Giovannini, M.; Canessa, C.; Indolfi, G.; Azzari, C. Epidemiology of respiratory syncytial virus-related hospitalization over a 5 year period in Italy: evaluation of seasonality and age distribution before vaccine introduction. Vaccines (Basel) 2020, 8, 15: 1–15: 9. [Google Scholar] [CrossRef]
- Price, R.H.M.; Graham, C.; Ramalingam, S. Association between viral seasonality and meteorological factors. Sci Rep 2019, 11, 929: 1–929: 11. [Google Scholar] [CrossRef]
- Walsh, E.E. Respiratory syncytial virus infection: an illness for all ages. Clin Chest Med 2017, 38, 29–36. [Google Scholar] [CrossRef]
- Ralston, S.L.; Lieberthal, A.S.; Meissner, H.C.; Alverson, B.K.; Baley, J.E.; Gadomski, A.M.; Johnson, D.W.; Light, M.J.; Maraga, N.F.; Mendonca, E.A.; et al. Clinical Practice Guideline: The Diagnosis, Management, and Prevention of Bronchiolitis. Pediatrics 2014, 134, 1474–1502. [Google Scholar] [CrossRef]
- Manti, S.; Staiano, A.; Orfeo, L.; Midulla, F.; Marseglia, G.L.; Ghizzi, C.; Zampogna, S.; Carnielli, V.P.; Favilli, S.; Ruggieri, M.; et al. UPDATE-2022 Italian guidelines on the management of bronchiolitis in infants. Ital J Pediatr 2023, 49, 19: 1–19: 18. [Google Scholar] [CrossRef]
- National Institute for Health and Care Excellence. Bronchiolitis: diagnosis and management of bronchiolitis in children, 2017. https://www.nice.org.uk/guidance/ng9/evidence/full-guideline-pdf-64023661.
- Jang, M.J.; Kim, Y.J.; Hong, S.; Na, J.; Hwang, J.H.; Shin, S.M.; Ahn, Y.M.; et al. Positive association of breastfeeding on respiratory syncytial virus infection in hospitalized infants: a multicenter retrospective study. Clin Exp Pediatr 2020, 63, 135–140. [Google Scholar] [CrossRef]
- Baraldi, E.; Lanari, M.; Manzoni, P.; Rossi, G.A.; Vandini, S.; Rimini, A.; Romagnoli, C.; Colonna, P.; Biondi, A.; Biban, P.; et al. Intersociety consensus document on treatment and prevention of bronchiolitis in newborns and infants. Ital J Pediatr 2014, 24, 65: 1–65: 13. [Google Scholar] [CrossRef]
- Azzari, C.; Baraldi, E.; Bonanni, P.; Bozzola, E.; Coscia, A.; Lanari, M.; Manzoni, P.; Mazzone, T.; Sandri, F.; Checcucci Lisi, G.; et al. Epidemiology and prevention of respiratory syncytial virus infections in children in Italy. Ital J Pediatr 2021, 47, 198: 1–198: 12. [Google Scholar] [CrossRef]
- Lin, J.; Zhang, Y.; Xiong, L.; Liu, S.; Gong, C.; Dai, J. High-flow nasal cannula therapy for children with bronchiolitis: a systematic review and meta-analysis. Arch Dis Child 2019, 104, 564–576. [Google Scholar] [CrossRef]
- O’Brien, S.; Craig, S.; Babl, F.E.; Borland, M.L.; Oakley, E.; Dalziel, S.R. Paediatric Research in Emergency Departments International Collaborative (PREDICT) Network, Australasia. Rational use of high-flow therapy in infants with bronchiolitis. What do the latest trials tell us? A paediatric research in emergency departments international collaborative perspective. J Paediatr Child Health 2019, 55, 746–752. [Google Scholar] [CrossRef] [PubMed]
- Franklin, D.; Babl, F.E.; Schlapbach, L.J.; Oakley, E.; Craig, S.; Neutze, J.; Furyk, J.; Fraser, J.F.; Jones, M.; Whitty, J.A.; et al. A randomized trial of high-flow oxygen therapy in infants with bronchiolitis. N Engl J Med 2018, 378, 1121–1131. [Google Scholar] [CrossRef] [PubMed]
- Milési, C.; Boubal, M.; Jacquot, A.; Baleine, J.; Durand, S.; Odena, M.P.; Cambonie, G. High-flow nasal cannula: recommendations for daily practice in pediatrics. Ann Intensive Care 2014, 4, 29: 1–29: 7. [Google Scholar] [CrossRef]
- Kepreotes, E.; Whitehead, B.; Attia, J.; Oldmeadow, C.; Collison, A.; Searles, A.; Goddard, B.; Hilton, J.; Lee, M.; Mattes, J. High-flow warm humidified oxygen versus standard low-flow nasal cannula oxygen for moderate bronchiolitis (HFWHO RCT): an open, phase 4, randomised controlled trial. Lancet 2017, 389, 930–939. [Google Scholar] [CrossRef] [PubMed]
- Moreel, L.; Proesmans, M. High flow nasal cannula as respiratory support in treating infant bronchiolitis: a systematic review. Eur J Pediatr 2020, 179, 711–718. [Google Scholar] [CrossRef]
- Schibler, A.; Pham, T.M.T.; Dunster, K.R.; Foster, K.; Barlow, A.; Gibbons, K.; Hough, J.L. Reduced intubation rates for infants after introduction of high-flow nasal prong oxygen delivery. Intensive Care Med 2011, 37, 847–852. [Google Scholar] [CrossRef]
- Goh, C.T.; Kirby, L.J.; Schell, D.N.; Egan, J.R. Humidified high-flow nasal cannula oxygen in bronchiolitis reduces need for invasive ventilation but not intensive care admission: High-flow nasal.
- cannula in bronchiolitis. J Paediatr Child Health 2017, 53, 897–902. [CrossRef]
- Kaplan, E.L.; Meier, P. Nonparametric estimation from incomplete observation. J Am Stat Assoc 1958, 53, 457–481. [Google Scholar] [CrossRef]
- Gooley, T.A.; Leisenring, W.; Crowley, J.; Storer, B.E. Estimation of failure probabilities in the presence of competing risk: new representation of old estimators. Stat Med 1999, 18, 695–706. [Google Scholar] [CrossRef]
- Schober, P.; Vetter, T.R. Logistic regression in Medical Research. Anesth Analg 2021, 132, 365–366. [Google Scholar] [CrossRef] [PubMed]
- Ghirardo, S.; Cozzi, G.; Tonin, G.; Risso, F.M.; Dotta, L.; Zago, A.; Lupia, D.; Cogo1, P.; Ullmann, N.; Coretti, A.; et al. Increased use of high-flow nasal cannulas after the pandemic in bronchiolitis: a more severe disease or a changed physician’s attitude? Eur J Pediatr 2022, 181, 3931–3936. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez-Fernandez R, González-Sánchez MI, Perez-Moreno J, González-Martínez F, de la Mata Navazo S, Mejias A, Ramilo O. Age and respiratory syncytial virus etiology in bronchiolitis clinical outcomes. J Allergy Clin Immunol Global 2022, 1, 91–98. [CrossRef]
- Ramilo, O.; Mejias, A. Measuring the burden of RSV in children to precisely assess the impact of preventive strategies. Pediatrics 2020, 146, e20201727. [Google Scholar] [CrossRef] [PubMed]
- Baldassarre, M.E.; Loconsole, D.; Centrone, F.; Caselli, D.; Baldassarre, M.; Quartulli, L.; Acquafredda, A.; D’Amato, G.; Maffei, G.; Latorre, G.; et al. Hospitalization for bronchiolitis in children aged ≤ 1year, Southern Italy, year 2021: need for new preventive strategies? Ital J Pediatr 2023, 49, 66: 1–66: 7. [Google Scholar] [CrossRef]
- Pierangeli, A.; Nenna, R.; Fracella, M.; Scagnolari, C.; Oliveto, G.; Sorrentino, L.; Frasca, F.; Conti, M.G.; Petrarca, L.; Papoff, P.; et al. Genetic diversity and its impact on disease severity in respiratory syncytial virus subtype-A and -B bronchiolitis before and after pandemic restrictions in Rome. J Infect 2023, 87, 305–314. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).