Introduction
Ureteropelvic junction obstruction (UPJO) is a prevalent urinary tract blockage in children, constituting 30% to 40% of antenatal hydronephrosis cases[
1]. Untreated UPJO can lead to severe complications like hypertension and chronic kidney disease[
2]. The standard treatment for pediatric UPJO is pyeloplasty, a procedure involving ureteropelvic junction reconstruction[
3].
Renal function deterioration indicates the need for surgical intervention and serves as a crucial measure for postoperative prognosis[
4]. However, long-term follow-up with radionuclide renal scintigraphy, due to its expense and radiation exposure, is challenging[
5,
6]. Ultrasound, a radiation-free and cost-effective method, is commonly used for clinical follow-ups.
Ultrasound reveals kidney morphology, reflecting renal function improvements and predicting long-term outcomes, particularly through morphological recovery such as cortical restoration[
7,
8]. Previous research examined factors influencing UPJO prognosis, such as age, hydronephrosis degree, diagnosis time, and infections[
4,
9,
10]. Typically, these studies compared postoperative renal function in different groups, evaluating single factors without accounting for interactions or quantifying associations influencing UPJO surgical outcomes. Therefore, we propose a new perspective, focusing on morphology and using multifactorial logistic regression to analyze factors affecting children's UPJO prognosis, approaching real-world postoperative situations.
Our study applies logistic regression, with improved renal morphology as the outcome, to identify factors influencing UPJO surgical outcomes in children. We retrospectively studied 150 pediatric UPJO patients with APD grades 4-5, who underwent pyeloplasty between July 2012 and July 2022. Data included demographics, symptoms, preoperative findings, and postoperative renal ultrasounds.
Identifying significant prognosis predictors and creating a regression model and nomogram can aid clinicians in assessing postoperative UPJO prognosis in children.
Methods
1.Study Design and Population:
This retrospective analysis examines the clinical data of pediatric patients who underwent laparoscopic dismembered pyeloplasty for the diagnosis of ureteropelvic junction obstruction (UPJO) between July 2012 and July 2022. The study primarily focuses on analyzing factors related to the patients and their medical conditions, without incorporating surgical technique-related variables. The inclusion criteria were as follows: 1. Unilateral renal hydronephrosis; 2. APD grading system classified as grade 4-5; 3. Complete clinical data availability. Exclusion criteria comprised: 1. Refusal to participate in the study; 2. Loss to follow-up; 3. Pediatric patients with significant comorbidities affecting other organ systems, including the cardiovascular, respiratory, and neurological systems; 4. Pediatric patients with duplicated kidney, renal dysplasia, ureterovesical junction obstruction (UVJO), posterior urethral valves (PUV), vesicoureteral reflux (VUR), renal calculi, ureteral calculi, neurogenic bladder, or other conditions causing renal hydronephrosis. To optimize cost-effectiveness and time efficiency, we employed a random selection process to assign children into five age groups based on their surgical age, with each group comprising 30 participants. Consequently, a total of 150 individuals were included in the study. The age groups were defined as follows: Age < 1 year, age 1 to < 3 years, age 3 to < 6 years, age 6 to < 11 years, and age ≥ 11 years. The study was conducted at the Children's Hospital Affiliated with Chongqing Medical University and received approval from the local Institutional Review Board.
2.Data Collection:
All data were obtained from the medical records of the pediatric patients, including age at the time of surgery, sex, duration of hydronephrosis, weight, blood pressure, gestational age at birth, mode of delivery, abnormal prenatal examination results, presence of other concomitant anomalies, presence of urinary stones or tract infections, laterality of onset, degree of preoperative calyceal dilation, preoperative renal cortical thickness, blood creatinine, cystatin c, blood phosphorus, estimated glomerular filtration rate (eGFR), urine protein, postoperative calyceal dilation, and postoperative renal cortical thickness.
3.Statistical Analysis:
Logistic regression analysis was employed to analyze the data. We compared the changes in calyceal dilation and renal cortical thickness preoperatively and postoperatively, while considering potential measurement errors caused by different ultrasound technicians. A reduction in calyceal dilation >0.1 cm was considered indicative of decreased calyceal dilation, while an increase in renal cortical thickness >0.1 cm was considered indicative of restored renal cortical thickness. Postoperative outcomes were classified as good if both criteria were met, while all other cases were categorized as having a poor recovery. All variables underwent initial univariate logistic regression analysis, and statistically significant variables were subsequently included in a multivariate logistic regression analysis to identify significant predictors of postoperative outcome. Ultimately, regression models were constructed using the variables that exhibited statistical significance in the multivariate analysis, and a nomogram was generated for clinical application.
Data were processed using R 4.2.1, and statistical significance was set at P<0.05.
Results
1.Baseline Characteristics Analysis in Pediatric with Hydronephrosis Resulting from UPJO
The 150 children were stratified into two groups based on their postoperative recovery outcomes: the good recovery group and the poor recovery group.
Table 1 displays the association between baseline data and the two groups. The results show that 78 out of 150 children (52% of the total) had a good postoperative recovery.
Among those with good postoperative recovery, the highest number of children (24 children, or 30.77%) were under 1 year old at the time of surgery. In contrast, among children with poor postoperative recovery, the highest number of children (23 children, or 31.94%) were over 11 years old at the time of surgery. Additionally, the highest number of children with hydronephrosis over 2 years old was observed among children with poor postoperative recovery (31 children, or 43.06%).
Regarding clinical symptoms and weight, the largest number of children with good postoperative recovery had no clinical symptoms and were of normal weight (56 children, accounting for 71.79% and 72 children, accounting for 92.31%, respectively). Furthermore, a higher proportion of children with good postoperative recovery had normal blood creatinine (84.62%). In contrast, among children with poor postoperative recovery, the majority of children (81.94%) had no obvious abnormalities in prenatal examination.
The differences in various variables between the good prognosis and poor prognosis groups were statistically significant (P < 0.05). These results suggest that factors such as age at surgery, duration of hydronephrosis, clinical symptoms, weight, antenatal examination, and serum creatinine may be closely associated with the postoperative recovery of children.
2. Univariate Logistic Regression Analysis of Pediatric Hydronephrosis Resulting from UPJO
To further explore the factors influencing postoperative recovery in pediatric patients, an univariate logistic regression analysis was conducted to identify the independent factors affecting postoperative recovery. The results are shown in
Table 2. It was found that compared with pediatric patients who underwent surgery at the age of less than 1 year, those aged between 6 and 11 years (OR: 13.14 CI: 3.84-45.02) and those aged 11 years or older (OR: 9.33 CI: 2.85-30.6) had a significantly increased risk of poorer postoperative recovery. Compared with patients with a renal pelvis dilation time of more than 2 years, patients with a dilation time of less than 6 months (OR: 0.03 CI: 0.01-0.16), a dilation time of 6 months to 1 year (OR: 0.04 CI: 0.01-0.18), and a dilation time of 1 to 2 years (OR: 0.03 CI: 0.01-0.15) had a significantly reduced risk of poorer postoperative recovery. Patients with clinical symptoms had a significantly increased risk of poorer postoperative recovery (OR: 3.56 CI: 1.8-7.04). Interestingly, patients with normal prenatal examination results had a significantly increased risk of poorer postoperative recovery (OR: 3.89 CI: 1.84-8.22). This may be due to the fact that when prenatal examination results are normal, the family members of the patient may not pay enough attention, and when the patient is born with renal pelvis dilation without clinical symptoms, early ultrasound examination of the urinary system is often not performed, resulting in a longer interval between the onset of dilation and its detection, and a more severe degree of dilation. In addition, patients with normal serum creatinine levels (OR: 0.3 CI: 0.14-0.66) and normal weight (OR: 0.32 CI: 0.12-0.87) had a significantly reduced risk of poorer postoperative recovery, while patients with clinical symptoms had a significantly increased risk of poorer postoperative recovery (OR: 3.56 CI: 1.8-7.04). These data analysis results suggest that factors such as age at surgery, duration of hydronephrosis, clinical symptoms, weight, antenatal examination, and serum creatinine may be closely related to postoperative recovery in pediatric patients.
3.Multivariate Logistic Regression Analysis of Pediatric Hydronephrosis Resulting from UPJO
The significant factors identified from the univariate logistic regression analysis were included in the Logical Multiple Regression Analysis. As shown in
Table 3, the results indicated that age at surgery, duration of hydronephrosis, body weight, and serum creatinine were significant factors (P < 0.05) that influenced the recovery of patients after surgery. Compared to patients with age at surgery less than 1 year, the risk of slightly worse postoperative recovery was significantly higher for patients aged between 3 and 6 years (OR: 12.76, CI: 1.44-147.2553) and for those aged between 6 and 11 years (OR: 64.95, CI: 5.05-2006.61). Patients with a duration of hydronephrosis less than 6 months (OR: 0.003, CI: 0.000008-0.005), between 6 months and 1 year (OR: 0.02, CI: 0.0013-0.1152), and between 1 year and 2 years (OR: 0.03, CI: 0.002-0.197) had a significantly lower risk of slightly worse postoperative recovery compared to those with a duration of hydronephrosis greater than 2 years. The risk of slightly worse postoperative recovery was significantly reduced for patients with normal body weight (OR: 0.01, CI: 0.0005-0.1049) and normal serum creatinine levels (OR: 0.16, CI: 0.04-0.53).
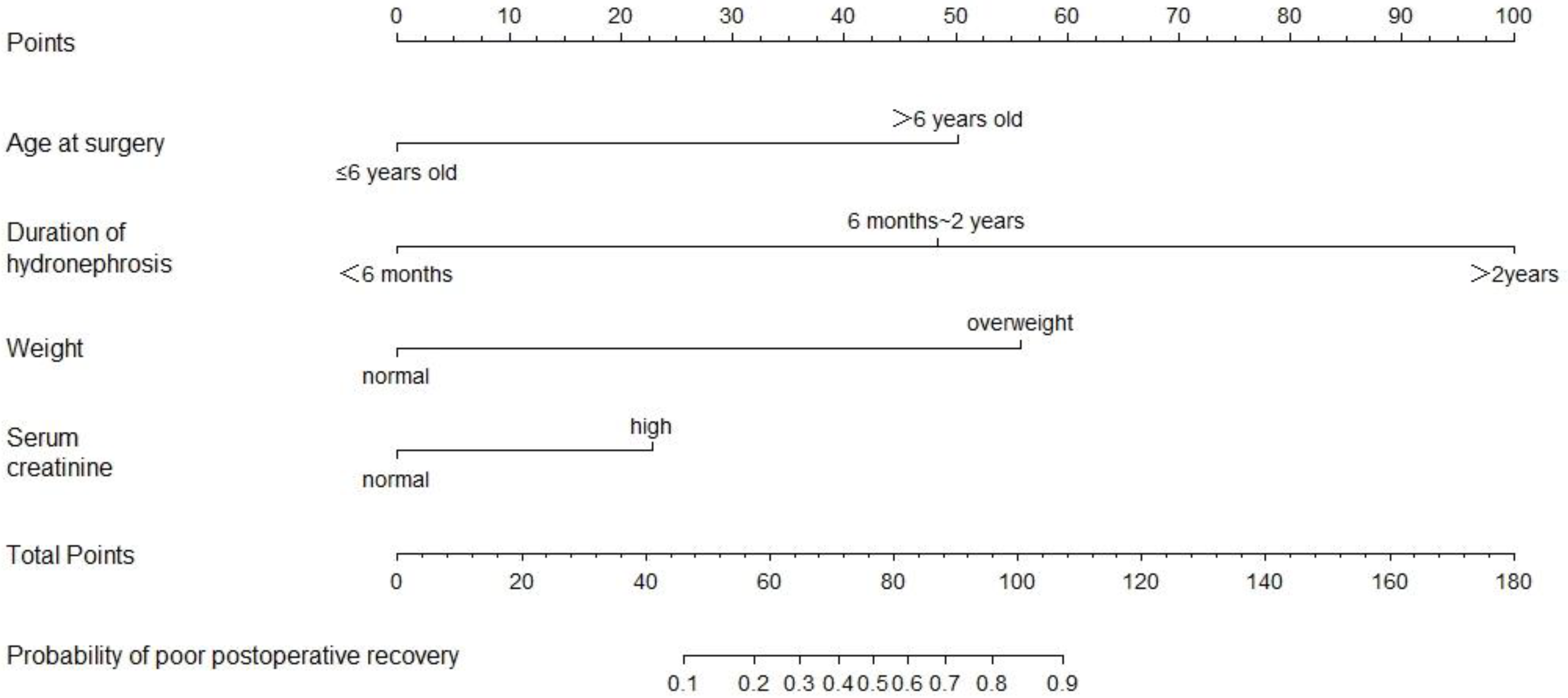
4.Developing and Validating Predictive Models
The final model incorporates four key factors, namely age at surgery, duration of hydronephrosis, weight, and serum creatinine, which have been identified as influential in the postoperative recovery of patients. Based on these factors, a nomogram was developed as a predictive tool. To enhance the model's predictive accuracy, age at surgery was categorized into two groups: ≤6 years and >6 years, while the four subgroups of hydronephrosis duration were merged into three categories: <6 months, 6 months to 2 years, and >2 years. The resulting nomogram is presented in
Figure 1.
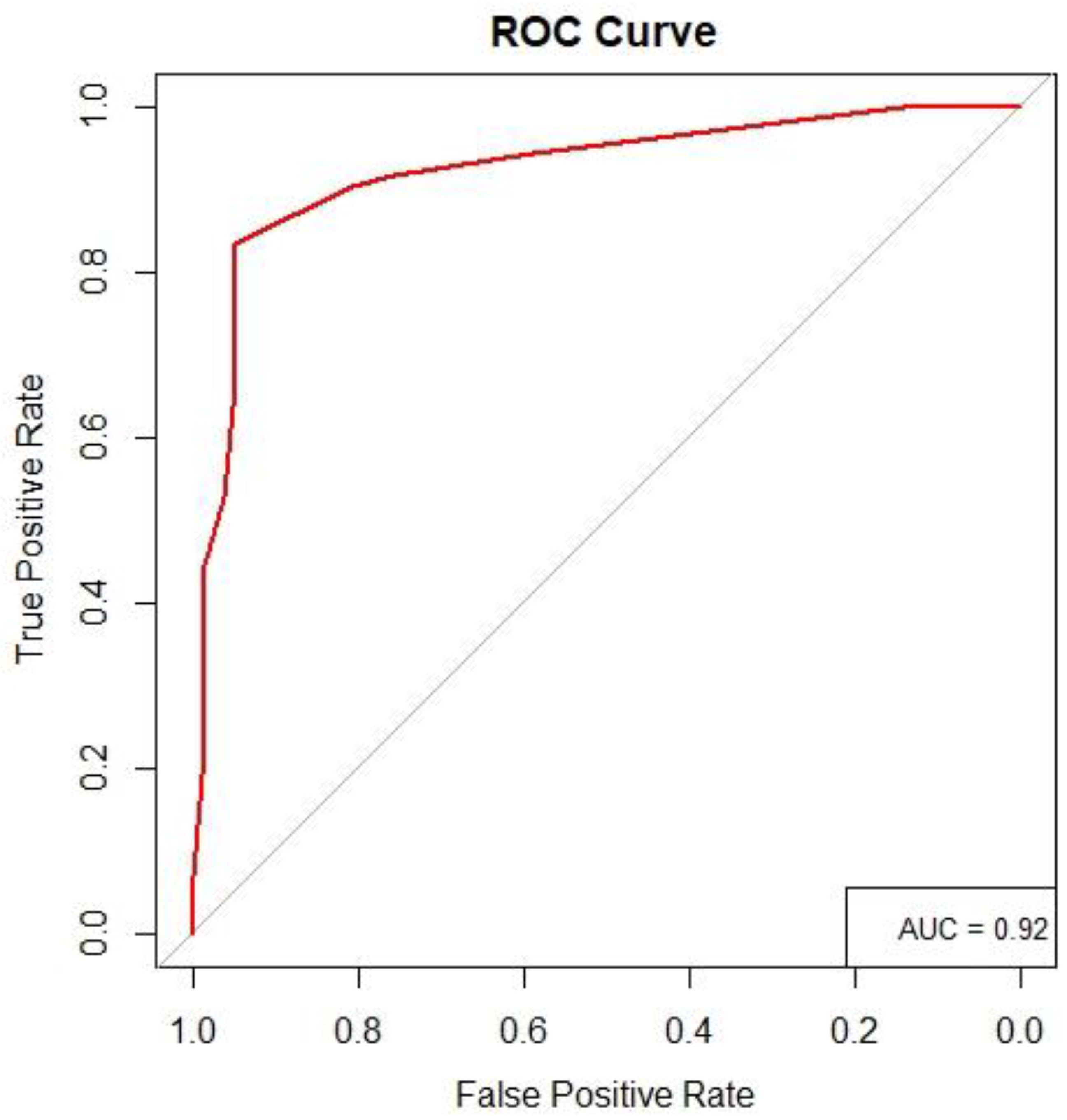
To assess the model's predictive performance, a receiver operating characteristic (ROC) curve was generated (
Figure 2). The area under the curve (AUC) was calculated to be 0.92. The AUC is a critical metric for evaluating a model's predictive ability, ranging from 0 to 1. A higher AUC value approaching 1 indicates excellent predictive capability in accurately distinguishing between positive and negative outcomes. In our study, an AUC of 0.92 demonstrates a high level of accuracy in predicting outcomes for the regression model.
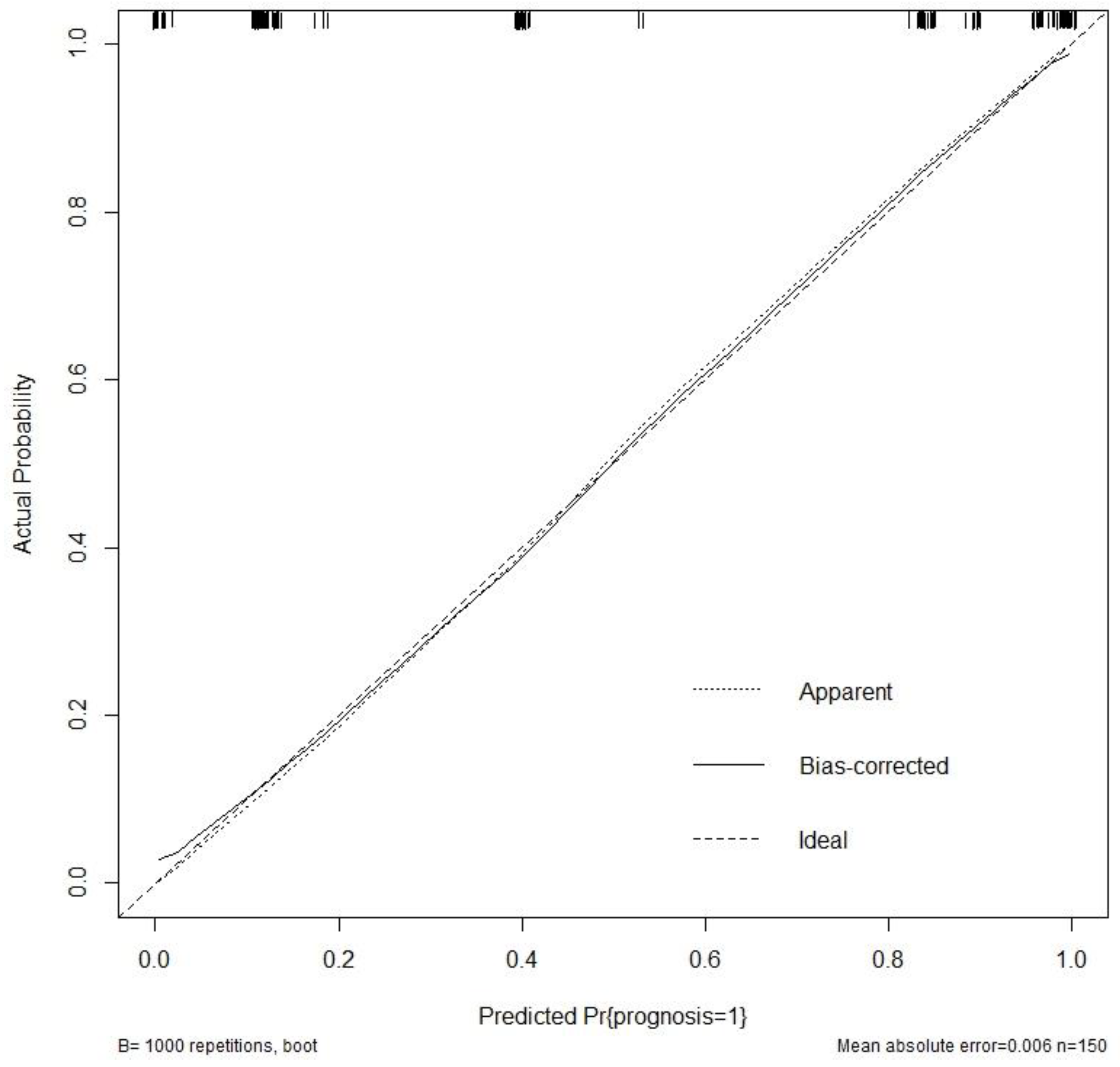
Additionally, a calibration curve (
Figure 3) was constructed to evaluate the accuracy of the model's predictions. The calibration curve provides further support for the precision of the model in predicting the outcome.
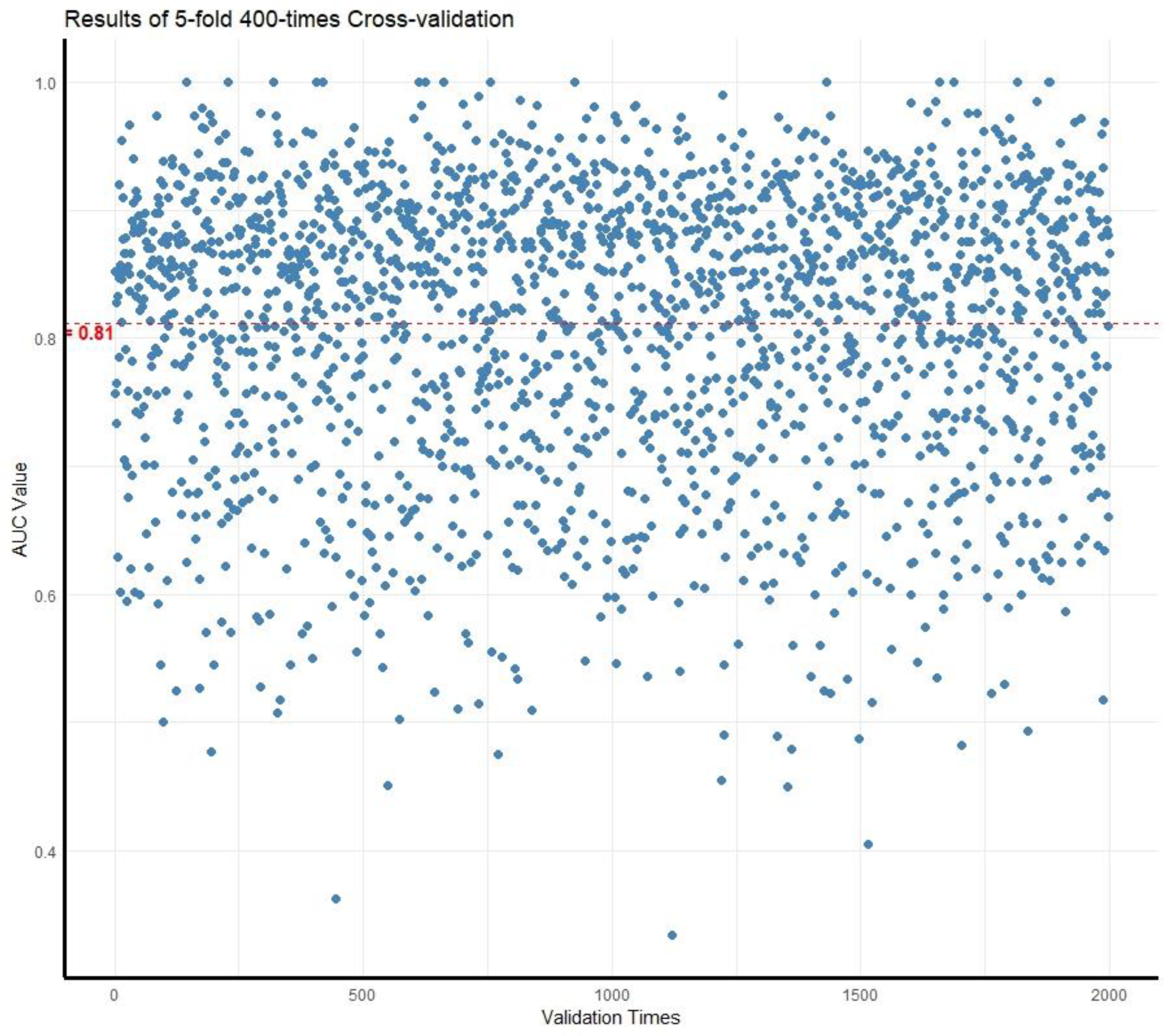
Furthermore, internal data cross-validation was performed using a 5-fold cross-validation technique, which was repeated 400 times. In each iteration, the cohort of 150 children was partitioned into 5 groups, with 4 groups utilized for training the model and 1 group for validation purposes. The entire cross-validation process was carried out using R version 4.2.1. Subsequently, the average Area Under the Curve (AUC) value was calculated to assess the accuracy of the model. The results are presented in
Figure 4. The resulting average AUC value of 0.81 demonstrated a slight reduction when compared to the initial value of 0.92. Nevertheless, it still indicates a satisfactory predictive performance.
By considering the findings from the nomogram, ROC curve, calibration curve, and the cross-validation results, it is evident that our model holds promise for accurately evaluating postoperative prognosis in patients. These results provide valuable insights for clinicians and researchers in the field, ensuring a comprehensive understanding of the model's predictive performance.
Discussion
This study aimed to identify predictors of postoperative outcomes in pediatric UPJO patients and create a nomogram for prediction. The results highlighted significant factors: age at surgery, duration of hydronephrosis, weight, and serum creatinine. These align with prior research emphasizing their importance in UPJO surgery[
7,
11,
12,
13]. Unlike most studies focusing on single-factor analysis, we used comprehensive multivariate logistic regression for a more realistic understanding of UPJO surgical outcomes.
Age at surgery was identified as a significant prognostic factor for postoperative outcomes in this study, which is consistent with previous research demonstrating that a younger age at the time of surgery is associated with more favorable outcomes[
7,
10]. Despite the relatively limited regenerative potential of the kidneys, they do exhibit certain reparative capabilities following partial tissue injury[
14]. Notably, studies have revealed the existence of a specific cell population termed progenitor cells within the kidney, endowed with critical attributes such as proliferation, self-renewal, and epithelial differentiation capacities. Although these cells account for only an estimated 0.5%-4% of the entire kidney cell population, they play a pivotal role in the process of kidney injury repair[
15,
16,
17]. As age advances, there is a gradual decline in the number of these progenitor cells, consequently resulting in a reduction of the kidneys' regenerative capacity[
18]. This may elucidate the improved recovery observed in the younger age group after alleviating the effects of renal hydronephrosis.
The duration of hydronephrosis emerged as a significant prognostic factor for postoperative outcomes in this study, with longer durations being associated with poorer outcomes. This finding aligns with previous research indicating that delayed surgery is linked to worse outcomes[
19,
20,
21]. Hydronephrosis induces distension of the renal pelvis and calyces, resulting in elevated intrarenal pressure. This pressure effect leads to cortical thinning, deformation of renal medulla blood vessels, activation of relevant inflammatory factors, and progressive renal parenchymal shrinkage, culminating in fibrosis[
22,
23]. Moreover, a prolonged duration of kidney exposure to hydronephrosis intensifies the degree of compression, resulting in worsened kidney morphology and function, ultimately leading to a poorer postoperative recovery outcome[
23,
24]. Supporting evidence from animal experiments underscores this pathological transformation, affirming that the recovery after the resolution of urinary tract obstruction in mice depends on both the duration and severity of the obstruction[
25]. Consequently, early surgical intervention is recommended to prevent further damage to the renal tissue and improve postoperative outcomes.
With the improvement of living standards, there is an increasing proportion of overweight children. In this study, we observed that 14% of the children presented weight problems. Surgeons widely acknowledge that operating on overweight patients can be potentially challenging[
26]. In the context of renal laparoscopic surgery, a significant correlation between the BMI index and intraoperative complications has been established. Obesity can exacerbate the complexity of surgical procedures, leading to prolonged operation times and impeding postoperative recovery[
27]. This concern is also evident in our present study. While we did not conduct a detailed analysis regarding whether overweight children experience elevated surgical complications and extended operation durations, the results of our COX regression analysis reveal that body weight does indeed impact the postoperative recovery outcomes of UPJO children. Therefore, it is imperative to place greater emphasis on addressing weight-related issues in children diagnosed with UPJO.
Serum creatinine was found to be a significant prognostic factor for postoperative outcomes, with elevated serum creatinine levels associated with worse outcomes. This is consistent with previous studies that have shown that higher serum creatinine levels are associated with an increased risk of postoperative complications[
28]. Serum creatinine serves as a reliable indicator for assessing renal function, with higher levels often indicating more severe impairment of renal function[
29]. Studies have highlighted that children with severely impaired renal function exhibit a significantly increased proportion of collagen in the renal pelvis, which, in turn, negatively affects renal pelvis compliance[
30]. The reduced compliance of the renal pelvis may lead to suboptimal improvement in renal morphology following relief of obstruction. Nevertheless, since most children in our study cohort did not undergo more comprehensive examinations such as ECT that provide a more accurate reflection of renal function, a deeper exploration of the impact of renal function beyond serum creatinine on postoperative recovery remains unattainable. Thus, relevant experiments can be designed for further research.
Based on the factors influencing postoperative recovery, we have developed a relevant predictive model that demonstrated excellent prognostic capability upon validation. The utilization of a nomogram generated by this model can assist clinicians in identifying high-risk patients for adverse postoperative outcomes, thereby facilitating proactive clinical intervention. Nevertheless, it is crucial to acknowledge the inherent limitations stemming from the retrospective design and single-center setting of this model, which may constrain the generalizability of the research findings. Consequently, further validation in more extensive, multicenter cohorts is imperative to corroborate the results of this study.
Our comprehensive analysis of these influencing factors has revealed that a younger age at the time of surgery, a shorter duration of the disease, and milder impairment of renal function serve as indicators of better recovery outcomes. Hence, we emphasize the importance of considering the relationship between age and renal recovery capacity, as well as the impact of hydronephrosis duration on the renal pelvis, in the context of children with UPJO. Selecting a more opportune time for proactive intervention may lead to improved recovery outcomes for pediatric patients.
Conclusions
In this study, we investigated the significant prognostic factors influencing postoperative outcomes in pediatric patients diagnosed with UPJO and more severe hydronephrosis. Age at the time of surgery, duration of hydronephrosis, weight, and preoperative creatinine levels were identified as important predictors for postoperative outcomes. Based on the obtained results, we have developed a nomogram to effectively predict postoperative outcomes in these patients. Our findings suggest, when dealing with children affected by UPJO leading to hydronephrosis, those who are younger, have a shorter duration of illness, normal serum creatinine levels, and a healthy body weight tend to experience better postoperative recovery.
Author Contributions
Conceptualization, Deying Zhang; Data curation, Qingtao Zhong and Xuan Wang; Formal analysis, Li Zhang, Peng Li and Xianhai YU; Investigation, Qingtao Zhong, Xuan Wang and Jiali He; Methodology, Deying Zhang; Project administration, Shengde Wu, Yi Hua, Feng Liu, Xing Liu, Dawei He, Tao Lin and Guanghui Wei; Resources, Li Zhang, Shengde Wu, Yi Hua, Feng Liu, Xing Liu, Dawei He, Tao Lin and Guanghui Wei; Software, Li Zhang; Supervision, Deying Zhang; Validation, Li Zhang; Visualization, Jiali He and Peng Li; Writing – original draft, Li Zhang.
Funding
The authors did not receive any financial support for the research, authorship, and publication of this article.
Data Availability Statement
Raw data were generated at the Department of Urology, Children's Hospital of Chongqing Medical University. Derived data supporting the findings of this study are available on request.
Conflicts of Interest
All authors certify that they have no financial and/or personal relationship with any person or organization that could have inappropriately influenced their work. The authors declare no conflicts of interest.
Ethics approval and consent: Ethical approval was waived by the local Ethics Committee of Chongqing Medical University in view of the retrospective nature of the study and all the procedures being performed were part of the routine care
Consent for publication: The final manuscript is approved for publication by all authors.
References
- Nguyen, H.T., C.A. Herndon, C. Cooper, et al. (2010) The Society for Fetal Urology consensus statement on the evaluation and management of antenatal hydronephrosis. J Pediatr Urol 6: 212-231. [CrossRef]
- Begou, O., A. Pavlaki, O. Deda, et al. (2021) Diminished systemic amino acids metabolome and lipid peroxidation in ureteropelvic junction obstruction (UPJO) infants requiring surgery. J Clin Med 10: 1467. [CrossRef]
- Knudson, M.J., J.C. Austin, Z.M. McMillan, et al. (2007) Predictive factors of early spontaneous resolution in children with primary vesicoureteral reflux. J Urol 178: 1684-1688. [CrossRef]
- A‘t Hoen, L., G. Bogaert, C. Radmayr, et al. (2021) Update of the EAU/ESPU guidelines on urinary tract infections in children. J Pediatr Urol 17: 200-207. [CrossRef]
- Gharpure, K.V., B. Jindal, B.K. Naredi, et al. (2021) Calyx to Parenchymal Ratio (CPR): An unexplored tool and its utility in the follow-up of pyeloplasty. J Pediatr Urol 17: 234. e1-234. e7. [CrossRef]
- Rodigas, J., H. Kirsch, U. John, et al. (2018) Static and functional MR urography to assess congenital anomalies of the kidney and urinary tract in infants and children: comparison with MAG3 renal scintigraphy and sonography. AJR Am J Roentgenol 211: 193-203. [CrossRef]
- Li, Y., Y. He, W. Zhang, et al. (2022) Factors predicting improvement of differential renal function after pyeloplasty in children of ureteropelvic junction obstruction. J Pediatr Urol 18: 504. e1-504. e6. [CrossRef]
- Wickramasekara, N., J. IgnatiusA.J.P.S.I. Lamahewage (2023) Sonographic follow-up after pyeloplasty: a large, retrospective cohort analysis. Pediatr Surg Int 39: 132. [CrossRef]
- Nordenström, J., G. Koutozi, G. Holmdahl, et al. (2020) Changes in differential renal function after pyeloplasty in infants and children. J Pediatr Urol 16: 329. e1-329. e8. [CrossRef]
- Muradi, T., Z. Turkyilmaz, R. Karabulut, et al. (2021) Our experience of operated pediatric ureteropelvic junction obstruction patients. Urologia 03915603211046161. [CrossRef]
- Wang, H., C. Hao, D.J.C. Bai, et al. (2022) Risk Factors of Urinary Tract Infection in Pediatric Patients with Ureteropelvic Junction Obstruction after Primary Unilateral Pyeloplasty. Comput Math Methods Med 2022. [CrossRef]
- Kafka, I.Z., S. Kocherov, J. Jaber, et al. (2019) Pediatric robotic-assisted laparoscopic pyeloplasty (RALP): does weight matter? Pediatr Surg Int 35: 391-396. [CrossRef]
- Vemulakonda, V.M., D.T. Wilcox, T.M. Crombleholme, et al. (2015) Factors associated with age at pyeloplasty in children with ureteropelvic junction obstruction. Pediatr Surg Int 31: 871-877. [CrossRef]
- Little, M.H.P.J.J.o.t.A.S.o.N.J. Kairath (2017) Does renal repair recapitulate kidney development? J Am Soc Nephrol 28: 34. [CrossRef]
- Bussolati, B., S. Bruno, C. Grange, et al. (2005) Isolation of renal progenitor cells from adult human kidney. Am J Pathol 166: 545-555. [CrossRef]
- Angelotti, M.L., E. Ronconi, L. Ballerini, et al. (2012) Characterization of renal progenitors committed toward tubular lineage and their regenerative potential in renal tubular injury. Stem Cells 30: 1714-1725. [CrossRef]
- Andrianova, N.V., M.I. Buyan, L.D. Zorova, et al. (2019) Kidney cells regeneration: dedifferentiation of tubular epithelium, resident stem cells and possible niches for renal progenitors. Int J Mol Sci 20: 6326. [CrossRef]
- Buyan, M.I., N.V. Andrianova, V.A. Popkov, et al. (2022) Age-Associated Loss in Renal Nestin-Positive Progenitor Cells. Int J Mol Sci 23: 11015. [CrossRef]
- Onen, A.J.J.o.P.U. (2007) An alternative grading system to refine the criteria for severity of hydronephrosis and optimal treatment guidelines in neonates with primary UPJ-type hydronephrosis. J Pediatr Urol 3: 200-205. [CrossRef]
- Babu, R., V.R. RathishV.J.J.o.p.u. Sai (2015) Functional outcomes of early versus delayed pyeloplasty in prenatally diagnosed pelvi-ureteric junction obstruction. J Pediatr Urol 11: 63. e1-63. e5. [CrossRef]
- Tokas, T., T.R. Herrmann, A. Skolarikos, et al. (2019) Pressure matters: intrarenal pressures during normal and pathological conditions, and impact of increased values to renal physiology. World J Urol 37: 125-131. [CrossRef]
- Chevalier, R.L., B.A. Thornhill, M.S. Forbes, et al. (2010) Mechanisms of renal injury and progression of renal disease in congenital obstructive nephropathy. Pediatr Nephrol 25: 687-697. [CrossRef]
- Deng, Q.-F., H. Chu, B. Peng, et al. (2021) Outcome analysis of early surgery and conservative treatment in neonates and infants with severe hydronephrosis. J Int Med Res 49: 03000605211057866. [CrossRef]
- Thornhill, B.A., L.E. Burt, C. Chen, et al. (2005) Variable chronic partial ureteral obstruction in the neonatal rat: A new model of ureteropelvic junction obstruction1. Kidney Int 67: 42-52. [CrossRef]
- Lindgren, B.W., B.T. Frainey, E.Y. Cheng, et al. (2014) Robot assisted laparoscopic pyeloplasty in obese and non-obese patients. J Pediatr Urol 10: 1206-1211. [CrossRef]
- Gong, E.M., M.A. Orvieto, M.B. Lyon, et al. (2007) Analysis of impact of body mass index on outcomes of laparoscopic renal surgery. Urology 69: 38-43. [CrossRef]
- Ceyhan, E., F. Ileri, T. Ceylan, et al. (2019) Predictors of recurrence and complications in pediatric pyeloplasty. Urology 126: 187-191. [CrossRef]
- El-Nahas, A.R., A.M. Shoma, I. Eraky, et al. (2006) Percutaneous endopyelotomy for secondary ureteropelvic junction obstruction: prognostic factors affecting late recurrence. Scand J Urol Nephrol 40: 385-390. [CrossRef]
- Levey, A.S., R.D. PerroneN.E.J.A.r.o.m. Madias (1988) Serum creatinine and renal function. Annu Rev Med 39: 465-490. [CrossRef]
- Ulusoy, O., E. Aydın, O. Ateş, et al. (2023) Clues for the early loss of renal function in congenital hydronephrosis: analysis of renal pelvis collagen ratio, diuresis renography and upper urinary tract morphology. J Pediatr Urol 19: 197. e1-197. e7. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).