Introduction:
Chronic lymphocytic inflammation with pontine perivascular enhancement responsive to steroids (CLIPPERS) is an atypical and only recently described disorder characterized by infiltration of the brain tissue by inflammatory cells (lymphocytic).[
1] The main lesions are in the pons, but CLIPPERS can also involve other parts of the brainstem, corpus callosum, white matter of the cerebellar and basal ganglia areas, and spinal cord[
2] with fairly characteristic regions of enhancement best seen on MRI scan[
3]. Patients typically present with a wide variety of signs and symptoms which include Cranial nerve dysfunction leading to altered facial sensation, diplopia and dysarthria, cerebellar signs like ataxia, imbalance walking gait, altered sensation, muscle spasticity etc[
4]. The disorder usually readily responds to steroids like glucocorticosteroids and immunosuppressant drugs[
5].
Case Presentation
A 40-year-old Indian female left-handed patient, who has studied up to 5th standard in school was admitted to SVP Hospital with complaints of Double vision for 2.5 months, Difficulty in speech and Imbalance while walking for 10 days. The patient was alright before 2.5 months then she had low-grade fever without chills and rigor with a headache of holo-cranial type for 1-2 days associated with tingling and numbness over the left half of the face since then. She had complained of deviation of mouth to the right side with drooping of saliva from the left angle of the mouth and not being able to close her left eye associated with difficulty in swallowing with occasional nasal regurgitation of food. She also complains of doubling of vision in the form of seeing 2objects in place of 1 in a horizontal plane for 3 days of fascial deviation. All that progressed over 2-3 days then became static for the next 7-10 days. During this period, she consulted a private doctor. and was given some medications in tapering doses (Data or Documentation Not available) after which she had an 80% improvement in tingling numbness and partial improvement in fascial deviation and swallowing.
But her diplopia has not improved. For that, she consulted many hospitals and finally reached our institute. For the last 10 days, she has complained of imbalance while walking in the form of sways to either side irrespective of even/uneven surfaces, dark/well-lit areas or narrow or wide areas. That progressed in a manner that she required 1–2-person support for walking for the last 5 days. She had difficulty getting up from bed and had backward falls multiple times for 3days.
Relatives also noticed a change in voice and speech in such that there was undue separation of syllables with monotonous speech for the last 10 days but her relatives were able to understand her speech.
At Present she is independent in her ADL (Activities of Daily Living), Not Associated with weakness of any limbs.
There is no History of any seizure or sleep alteration, loss of consciousness, or any involuntary movements.
Negative History of Alteration in smell, vision, eye movement, ptosis or any sensory abnormality on the face, any difficulty in hearing, tinnitus, vertigo, or diuresis, Regurgitation of food or fluid & no nasal twang of voice.
Past History
No history of seizure, sleep alteration or loss of consciousness.
No history of involuntary movements.
No history of Alteration in smell, vision, eye movement, ptosis or any sensory abnormality on the face.
No difficulty in hearing, tinnitus, vertigo, or diuresis.
No history of regurgitation of food or fluid & no nasal twang of voice.
No history of shoulder dropping or tongue deviation.
No history of difficulty in combing hair or other overhead activities.
No history of Thinning or wasting of limbs or any fasciculation.
No history of difficulty in climbing stairs or slippage of chappals.
No history of bowel and bladder involvement.
No history of palpitation, Blackening of vision, Recurrent sweating, constipation or diarrhoea.
No history of joint pain, Rash, Significant weight loss, oral or genital ulcer or dry mouth.
No history of palpitation, Syncope difficulty in breathing with or without exertion or chest pain.
No history of DM, HTN, Hypothyroidism, cold intolerance weight gain.
No history of unprotected sexual exposure or blood transfusion.
Physical Examination
On examination, the patient's general condition was good. She was conscious and well oriented to time place and person. A nervous system examination revealed that the Glass Glow Coma Scale (GCS) score was E4 M6 V5. Her pupils were Bilaterally equal in size and diameter and Reactive to Light with no ptosis. Extraocular Moments (EOM) show mild Left Rectus left palsy. Muscle Tone was normal and strength of the limbs was level 5 and muscle tension of the limbs was normal. Deep Tendon reflexes were present in the limbs with +2/+2. On Sensory examination Joint Point Sense Test (JSP) and Vibration test were normal. On Cerebellum examination primary gaze, gaze-evoked and upbeat nystagmus were present with a fast component to the left side. Both Finger Nose Finger (FNF) and Finger Nose Test showed Bilateral dysmetria. Heel Shin test showed bilateral dyssynergia. Diadochokinetic rate (DDK) showed left>right. The patient had normal sensation, no stiff neck, and no other biological pathological signs.
Laboratory Examination:
Table 1.
Blood Examination:
Table 1.
Blood Examination:
| Test |
Observed Value |
Reference Range |
| Haemoglobin |
12.6 g/dl |
(12-18) |
| WBC |
10.05 kU/L |
(5.2-12.4) |
| RBC |
4.19 * 106/ul |
(4.5-5.5) |
| Haematocrit |
38.3% |
(40-50) |
| Platelet counts |
374 kU/L |
(130-400) |
| Neutrophile |
83 % |
(49-74) |
| Lymphocyte |
11% |
(26-46) |
| Monocyte |
05% |
(2-12) |
| Eosinophil |
01% |
(0-5) |
| Basophil |
00% |
(0-2) |
Table 2.
CSF examination:
Table 2.
CSF examination:
| Test |
Observed Value |
| Quantity |
0.5ml |
| Colour |
Colourless |
| Appearance |
Clear |
| Blood |
Absent |
| Cobweb |
Absent |
| Total count |
00 |
| Polymorphs |
- |
| Lymphocytes |
- |
| RBC |
Occasional |
| CSF sugar |
57 mg/dl |
| CSF protein |
52 mg/dl |
Table 3.
Liver Function Test:
Table 3.
Liver Function Test:
| Test |
Observed Value |
Reference Range |
| SGPT serum |
27 U/L |
(10-49) |
| SGOT serum |
40 U/L |
(0-34) |
| Alkaline Phosphatase Serum |
32 U/L |
(45-129) |
| Total Bilirubin |
0.46 mg/dl |
(0.3-1.2) |
| Direct Bilirubin |
0.10 mg/dl |
(0-0.3) |
| Indirect Bilirubin |
0.36 mg/dl |
- |
Table 4.
Renal Function Test:
Table 4.
Renal Function Test:
| Test |
Observed Value |
Reference Range |
| Blood Urea |
19.0 mg/dl |
(15-45) |
| Creatinine serum |
0.77 mg/dl |
(0.5-1.1) |
| Sodium serum |
137 mmol/L |
(132-146) |
| Potassium serum |
4.22 mmol/L |
(3.5-5.5) |
| Chlorine serum |
107 mmol/L |
(99-109) |
Table 5.
Antinuclear Antibody (ANA) test by Indirect Immunofluorescence:
Table 5.
Antinuclear Antibody (ANA) test by Indirect Immunofluorescence:
| Titre |
1:80 |
| Results |
Negative |
Table 6.
Other Tests:
| CRP |
0.15 mg/dl |
| ESR |
3 mm/hr |
| HIV |
Non-Reactive |
| HBsAg |
Non-Reactive |
| HCV |
Non-Reactive |
| Rapid Plasma Reagin test (RPR) for SYPHILIS |
Non-Reactive |
Table 7.
TSH- Thyroid Stimulating Hormone :.
Table 7.
TSH- Thyroid Stimulating Hormone :.
| Test |
Observed Value |
Reference Range |
| TSH |
1.15 uIU/ml |
(0.35-5.5) |
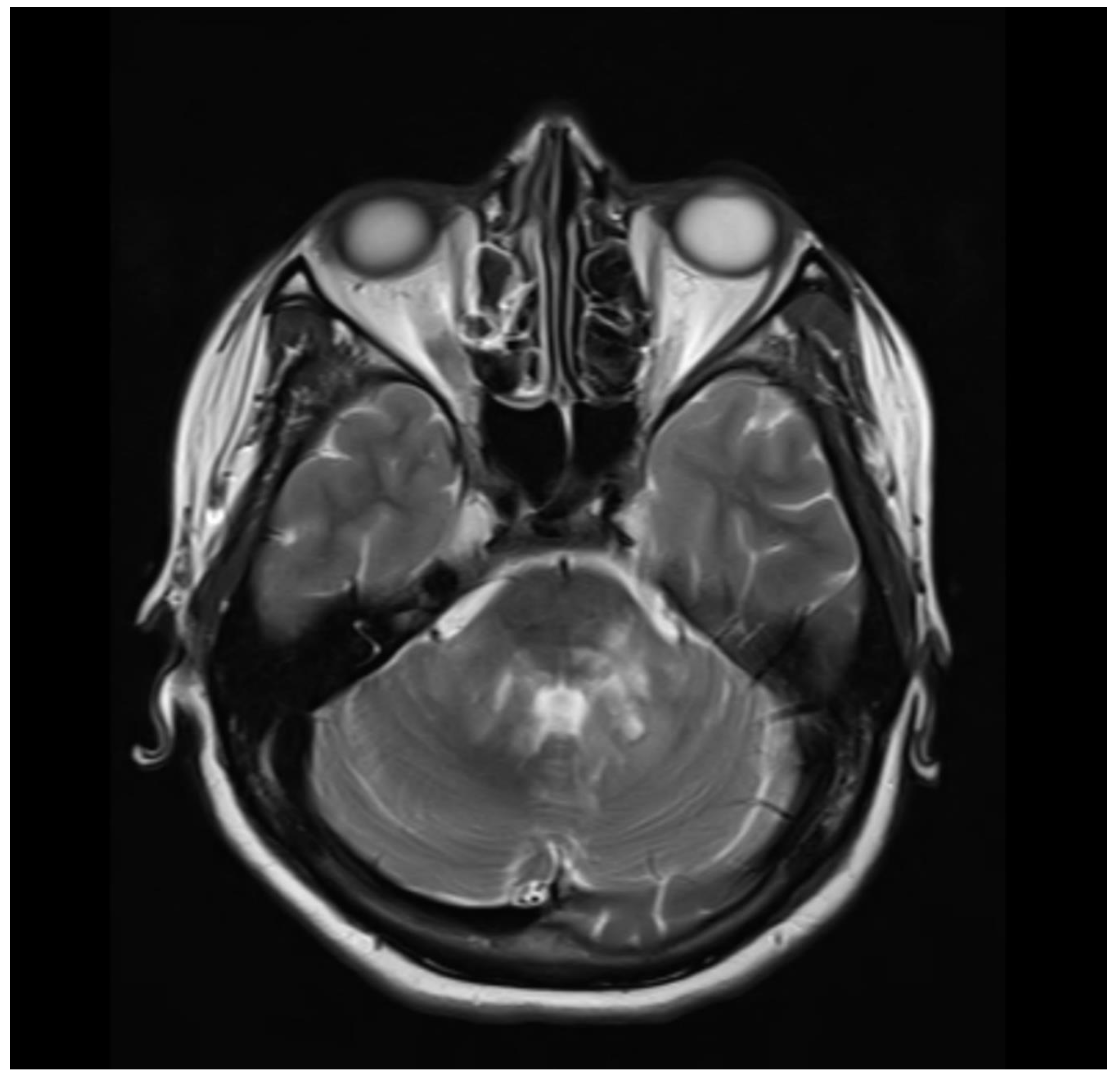
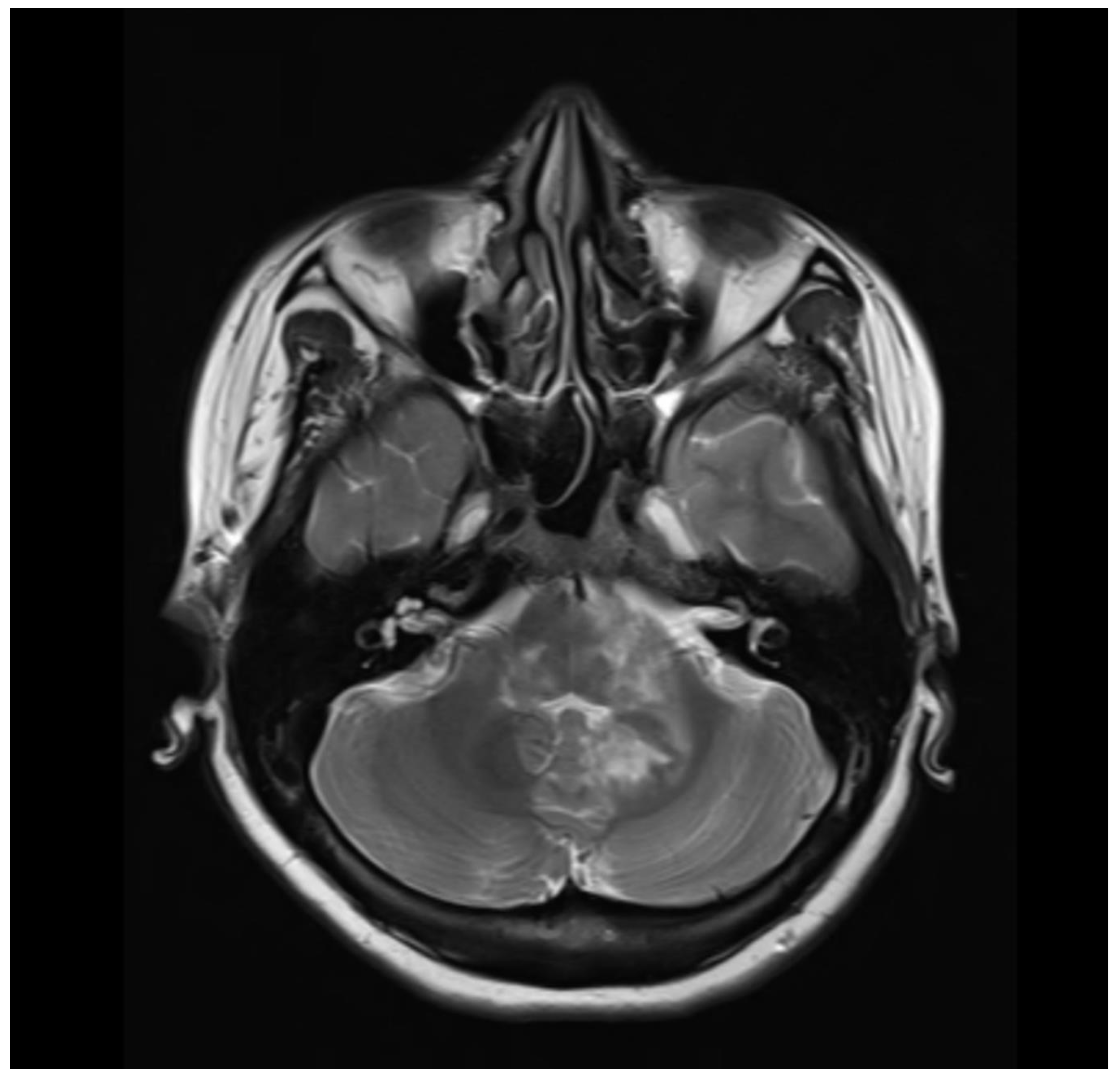
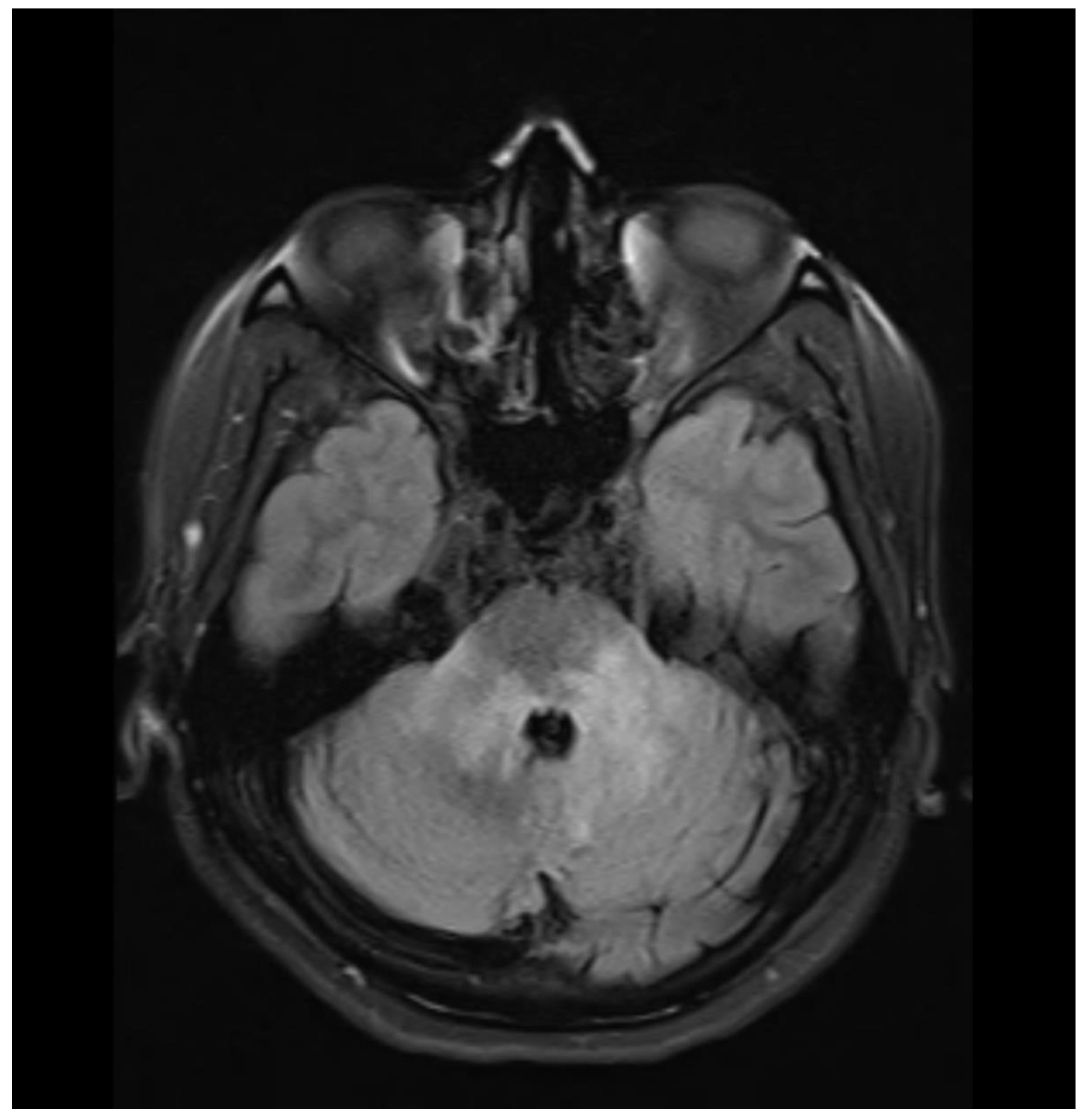
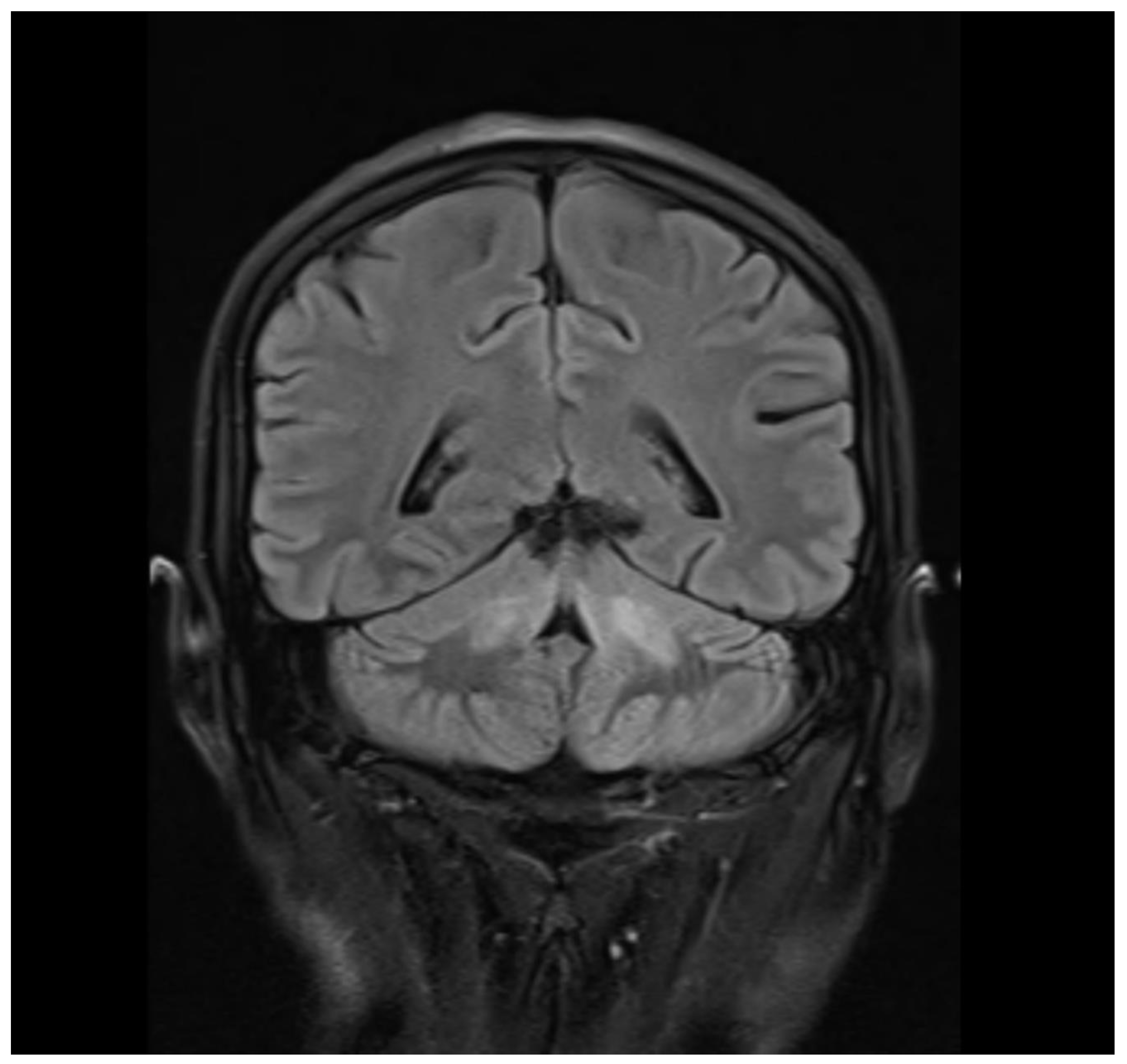
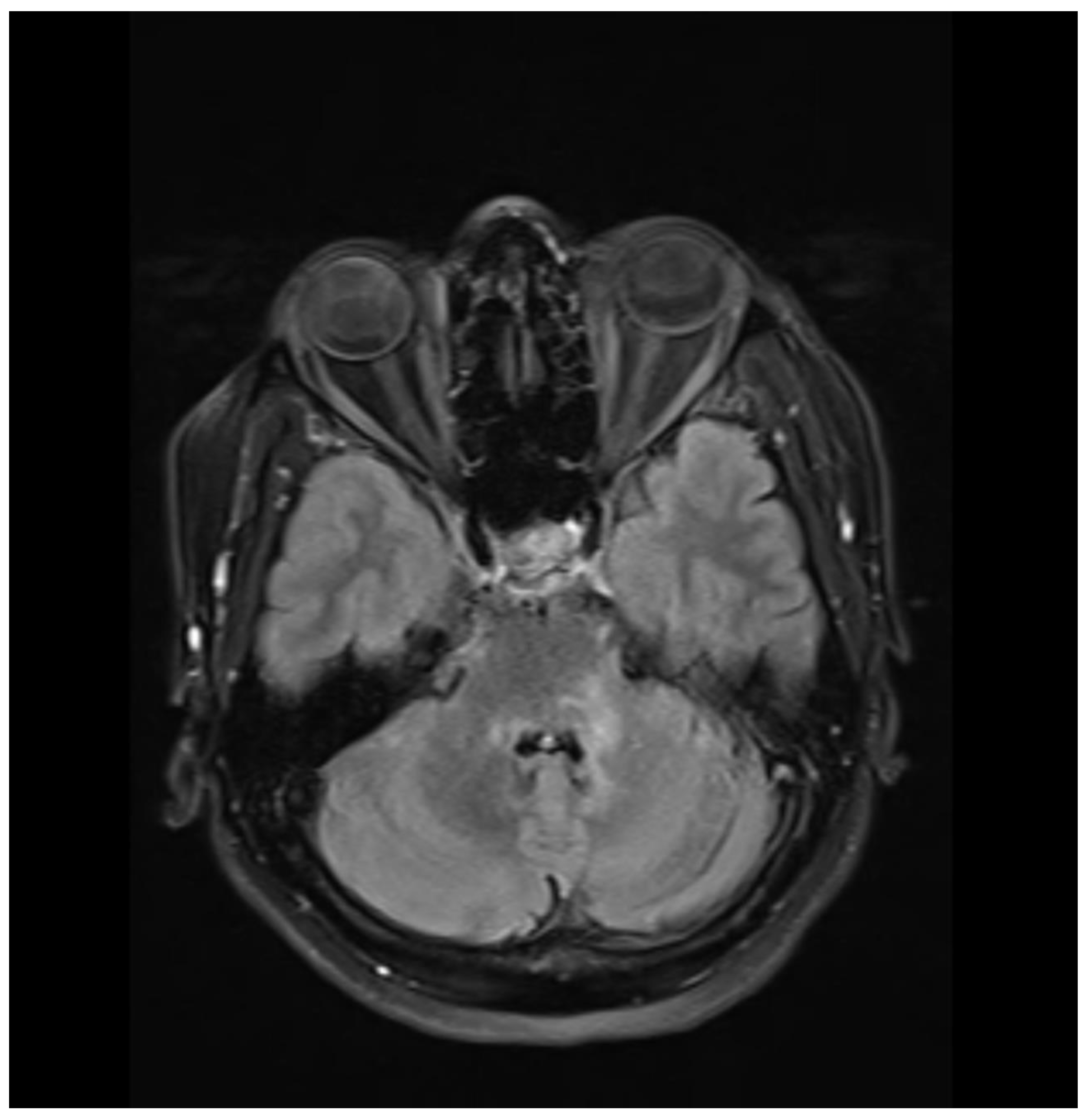
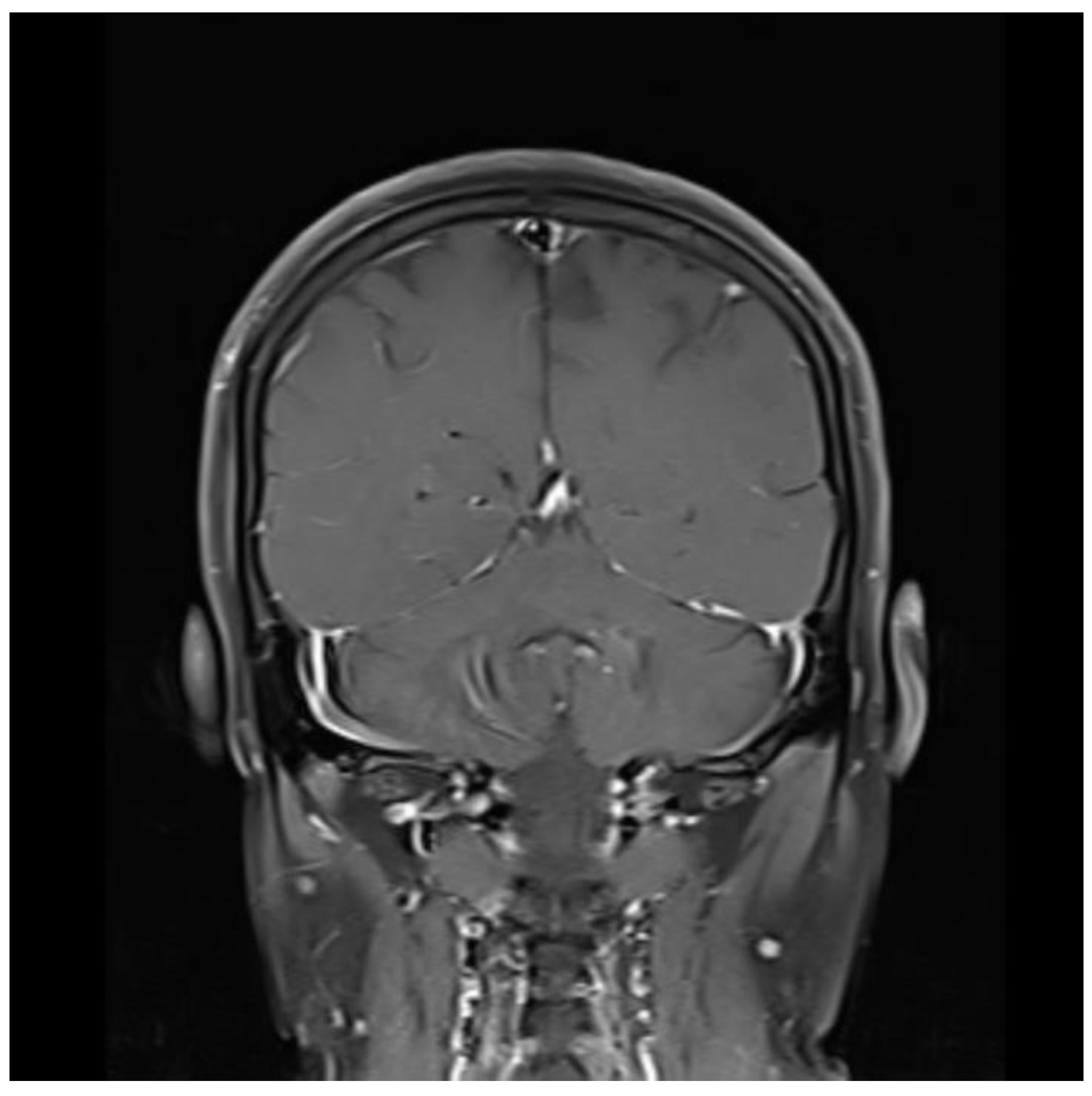
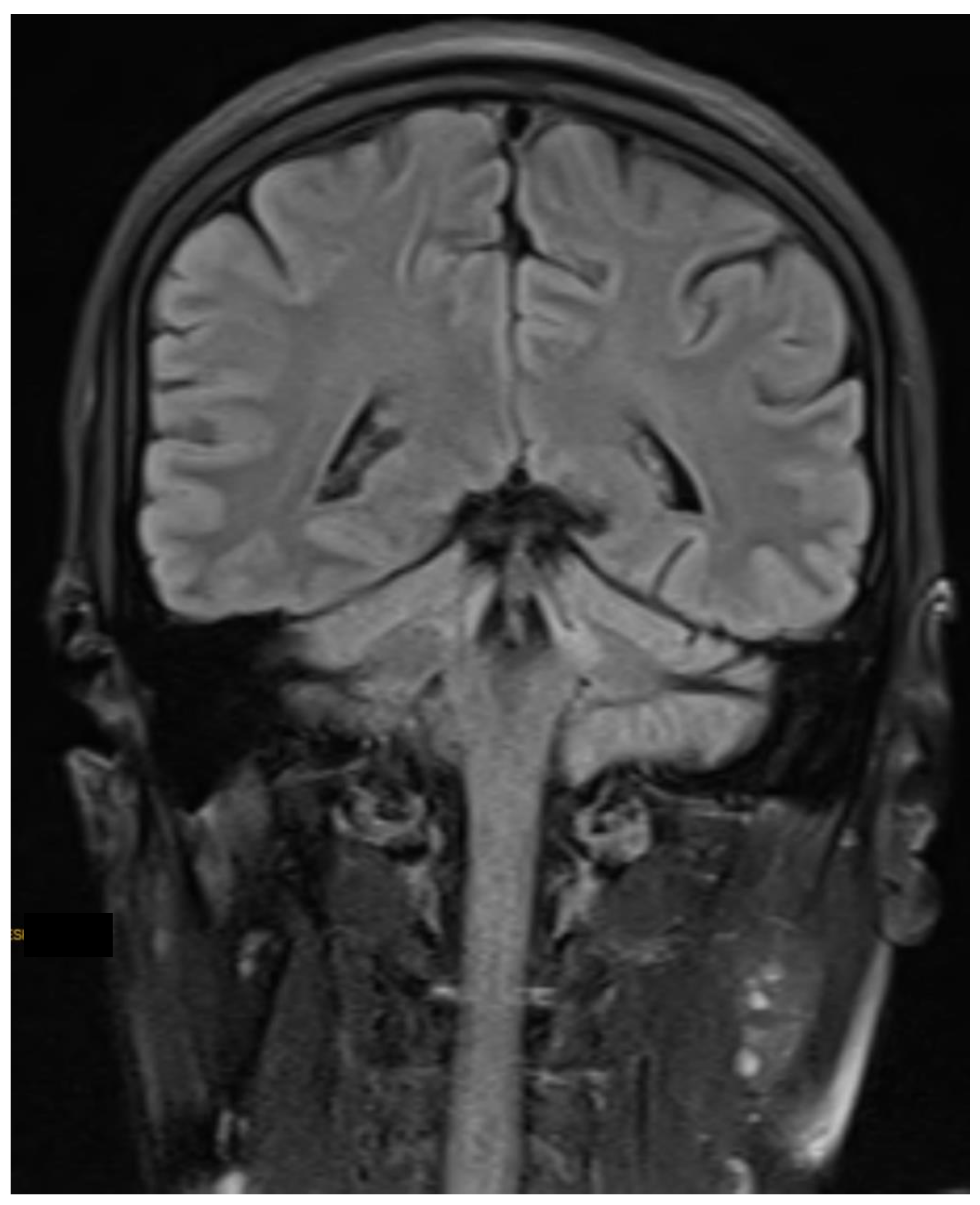
Radiological Imaging (MRI Brain Plain and Contrast):
Observation:
Before Steroid Therapy:
Ill-defined abnormal T2/Flair Hyperintensities noted involving the posterolateral aspect of pons, bilateral middle cerebral peduncle and periventricular region of bilateral cerebellar hemisphere (Left>Right) and upper 1/3rd of the medulla. It shows few areas of diffusion restriction. No evidence of any GRE Blooming. In post-contrast study, there is evidence of patchy, punctate and linear enhancement of the lesion. Abnormal T2/FLAIR hyperintensities were noted involving root entry zones and cisternal segments of bilateral Vth and root entry zones of VIIth & VIIIth. No evidence of any abnormal enhancement or nerve thickening.
These findings are suggestive of autoimmune aetiology Chronic Lymphocytic inflammation with pontine perivascular enhancement responsive to steroids (CIPPERS) more 'likely over demyelinating disease.
MRI scans were done at the time. T2 imaging showed perivascular infiltration in the pons area in Axial cuts
(Figure 1 and
Figure 2) and Dark Fluid T2 was also used showing a similar feature (
Figure 3). Sagittal Section Cut was also evident of the same (
Figure 4).
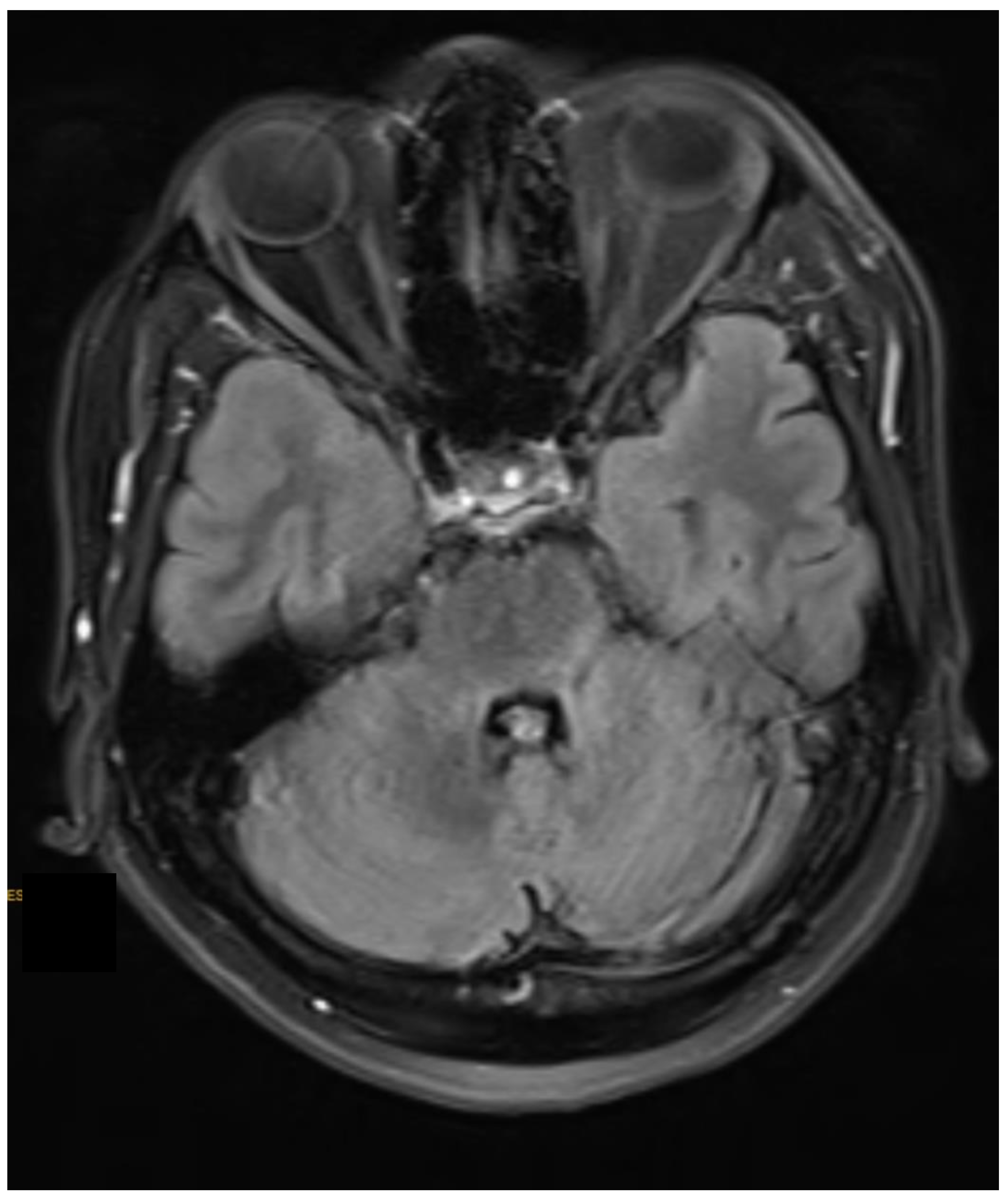
Following Steroid treatment for about 3 months:
As compared to the previous scan dated 3 months back, there is a significant reduction in abnormal T2W1/FLAIR hyperintensity and no evidence of post-contrast enhancement.
Ill-defined abnormal T2 /FLAIR hyperintensities noted involving posterolateral aspects of pons predominantly on the left side, bilateral middle cerebellar peduncle and periventricular region of left cerebellar hemisphere suggestive of inflammatory/demyelinating disease. Chronic lymphocytic inflammation with pontine perivascular enhancement responsive to steroids (CLIPPERS) is likely. In T2 MRI, this decrease can be appreciated in the Axial cut (
Figure 5) and Sagittal section
(Figure 6).
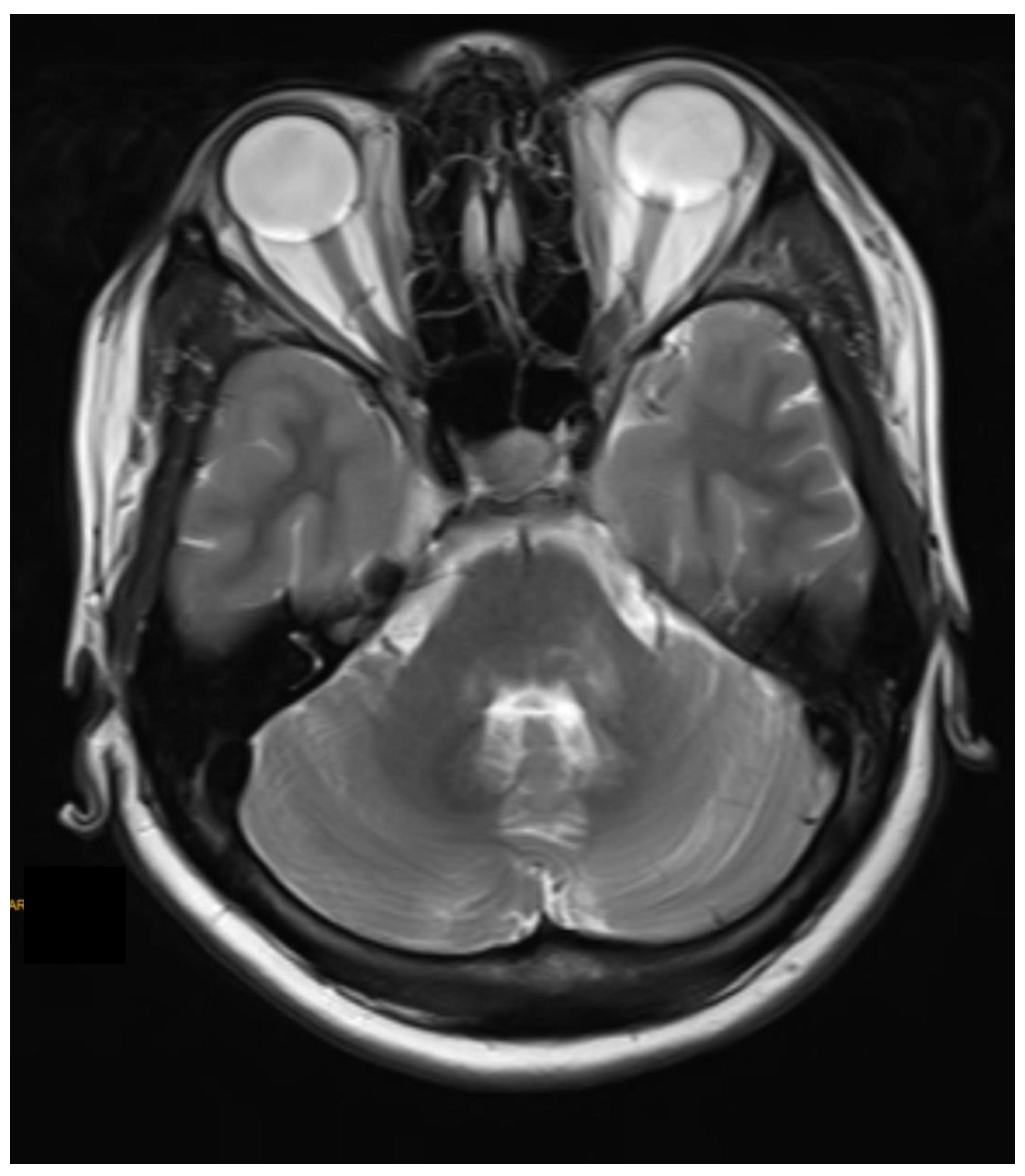
Follow-up Scan after about 8 months:
As compared to the previous scan dated 8 months back, there is a mild reduction in abnormal T2W1/FLAIR hyperintensity and no evidence of post-contrast enhancement.
Ill-defined abnormal T2 /FLAIR hyperintensities noted involving posterolateral aspects of pons predominantly on the left side, bilateral middle cerebellar peduncle and periventricular region of left cerebellar hemisphere suggestive of inflammatory/demyelinating disease. Chronic lymphocytic inflammation with pontine perivascular enhancement responsive to steroids (CLIPPERS) is likely. It can be seen in T2 MRI Axial cuts
(Figure 7 and
Figure 8) and sagittal section (
Figure 9).
Treatment:
The patient was started on oral steroid therapy that includes Prednisolone 30mg once a day and immunosuppressant Azathioprine 50mg twice a day along with supportive therapy like Pantoprazole 40mg, Folic acid and Vitamin B complex, Vitamin D3 and Calcium tablets once a day, all for 20 days. The patient was discharged after her condition stabilized and her symptoms improved.
Three months after treatment, the patient came in for a re-examination, and her clinical symptoms of imbalance in walking and voice changes had disappeared, without discomfort. MRI was performed again which showed there is a significant reduction in abnormal T2W1/FLAIR hyperintensity and no evidence of post-contrast enhancement.
Follow Up Care:
This patient was followed up for around 1 year, and there has been no recurrence or aggravation.
Diagnosis:
The patient received steroid therapy for approximately three months, resulting in a significant reduction in abnormal hyperintensity on MRI imaging and symptom improvement. Based on the clinical presentation, imaging findings, and response to steroid therapy, the patient was diagnosed with Chronic Lymphocytic Inflammation with Pontine Perivascular Enhancement Responsive to Steroids (CLIPPERS) is known for its response to steroids and immunosuppressive therapy.
Discussion and Literature:
Chronic Lymphocytic Inflammation with Pontine Perivascular Enhancement Responsive to Steroids (CLIPPERS) is a relatively rare neurological disorder that was first reported in 2010 by Pittock et al[
6]. After that, there have been several case reports and studies published contributing others to understanding of this neurological disorder better. The exact cause remains unclear, but it is thought CLIPPERS to be an autoimmune disorder involving inflammatory changes in small blood vessels of the brainstem and cerebellum.
CLIPPERS is considered a rare disorder, and its exact prevalence is not well established. The disease can occur in all age groups, and both men and women can be affected. Patients with CLIPPERS typically present with a range of neurological symptoms that can vary in severity and progression. The main lesions are in the pons, but CLIPPERS pathology can also involve other parts of the brainstem, corpus callosum, white matter of the cerebellar and basal ganglia areas, and spinal cord[
7]. Common clinical manifestations include double vision (diplopia), imbalance, ataxia, dysarthria (speech difficulties), and facial weakness. Neurological symptoms in CLIPPERS can mimic those seen in other central nervous system disorders, making diagnosis challenging. CLIPPERS can also be accompanied by some non-specific symptoms, like dizziness, nausea, vomiting, dysphagia, choking on water, and cognitive impairment. The signs and symptoms vary according to the location of the lesion.
The diagnosis of CLIPPERS is primarily based on clinical features, neuroimaging findings, cerebrospinal fluid (CSF) analysis, and response to corticosteroid therapy[
8]. Key diagnostic criteria include characteristic MRI brain findings of punctate or curvilinear gadolinium enhancement in the pons, periventricular regions, or other brainstem and cerebellar structures. CSF analysis may show lymphocytic pleocytosis and elevated protein levels. Histopathologically, CLIPPERS is an inflammatory lesion with the infiltration of lymphocytes around small blood vessels, involving both white and grey matter.
The Radiological imaging diagnosis of CLIPPERS syndrome is mainly performed using enhanced MRI head scans. On MRI imaging, CLIPPERS typically reveal T2/FLAIR hyperintense lesions in the brainstem (especially the pons), cerebellum, and periventricular regions. These lesions often exhibit patchy, punctate, or linear gadolinium enhancement[
9].
CLIPPERS can be challenging to diagnose because its clinical presentation and MRI features overlap with other conditions such as multiple sclerosis, primary central nervous system vasculitis, and tumorous lesions. Therefore, a thorough evaluation is essential to differentiate CLIPPERS from other disorders. Differentials to be considered include Inflammatory lesions like CLIPPERS syndrome/sarcoidosis/vasculitis, autoimmune encephalitis or a very remote possibility of Demyelination.
Treatment includes medium to high-dose corticosteroids, often followed by a gradual taper, which is the primary treatment for CLIPPERS. Patients typically respond well to steroids, with clinical improvement and resolution of MRI abnormalities. In cases of steroid dependence or relapse, immunosuppressive therapies like Azathioprine, Mycophenolate Mofetil, or Rituximab can be considered to maintain remission. However, no clinical studies have shown that this disease can be cured, as a result, long-term hormone maintenance is needed to prevent disease recurrence. Many trials of immunoglobulin have been reported in some literature[
10] but this treatment regime may not be effective and remains to be topic for further exploration. In addition, some scholars have also reported that the use of hydroxychloroquine for the treatment of CLIPPERS syndrome, not only leads to rapid remission but also effectively prevents recurrence with less adverse reactions.[
11]With appropriate treatment, CLIPPERS generally has a good prognosis. Most patients experience significant symptom relief and show improvement in neuroimaging findings. However, long-term immunosuppressive therapy may be necessary to prevent relapses. There is ongoing research to understand the immunological mechanisms involved in the disease, and it is believed that the immune system's response to an unknown trigger plays a role in the occurrence of CLIPPERS.
Conclusion:
CLIPPERS disease is a rare neurological disorder that has gained attention and increased interest from the medical community since its first case was reported. As researchers dive deeper into understanding its pathophysiology and exploring different treatment options, there is hope that the mysteries regarding this disease will be revealed and prompt management of patients can be done.
For patients diagnosed with CLIPPERS, timely recognition and the early initiation of appropriate treatment can significantly improve the patient’s quality of life.
Ethical Statement
Being a case report study, there were no ethical issues and the IRB was notified about the topic and the case. Still, no formal permission was required as this was a record-based case report. Permission from the patient for the article has been acquired and it has been made sure that their information or identity is not disclosed.
Conflicts of interest
The authors declare no conflict of interest.
References
- Dudesek et al., “CLIPPERS: chronic lymphocytic inflammation with pontine perivascular enhancement responsive to steroids. Review of an increasingly recognized entity within the spectrum of inflammatory central nervous system disorders,” Clin Exp Immunol, vol. 175, no. 3, pp. 385–396, Feb. 2014. [CrossRef]
- N. M. Shrestha, N. Acharya, and R. Desar, “Chronic Lymphocytic Inflammation with Pontine Perivascular Enhancement Responsive to Steroids (CLIPPERS Syndrome): A Case Report and Literature Review,” Case Rep Neurol Med, vol. 2023, pp. 1–5, Jul. 2023. [CrossRef]
- A. M. Korostyshevskaya et al., “CLIPPERS: Multiparametric and quantitative MRI features,” Radiol Case Rep, vol. 18, no. 1, pp. 368–376, Jan. 2023. [CrossRef]
- D. P. Breen, S. Rawal, E. J. Slow, and A. E. Lang, “CLIPPERS: A Treatable Cause of Spastic Ataxia,” Mov Disord Clin Pract, vol. 5, no. 2, pp. 212–214, Mar. 2018. [CrossRef]
- G. Taieb, T. Allou, and P. Labauge, “Therapeutic Approaches in CLIPPERS,” Curr Treat Options Neurol, vol. 19, no. 5, p. 17, May 2017. [CrossRef]
- S. J. Pittock et al., “Chronic lymphocytic inflammation with pontine perivascular enhancement responsive to steroids (CLIPPERS),” Brain, vol. 133, no. 9, pp. 2626–2634, Sep. 2010. [CrossRef]
- L. Cao, M. Liu, L. Guo, M. Li, M. Xu, and R. Wang, “The pathogenesis hypothesis and research progress of CLIPPERS: A literature review,” Medicine, vol. 102, no. 11, p. e33211, Mar. 2023. [CrossRef]
- A. Axelerad et al., “CLIPPERS, chronic lymphocytic inflammation with pontine perivascular enhancement responsive to steroids: A challenge in neurological practice, clinical landmarks (Review),” Exp Ther Med, vol. 22, no. 4, p. 1191, Aug. 2021. [CrossRef]
- M. Filippi et al., “Assessment of lesions on magnetic resonance imaging in multiple sclerosis: practical guidelines,” Brain, vol. 142, no. 7, pp. 1858–1875, Jul. 2019. [CrossRef]
- Gabilondo, A. Saiz, F. Graus, and P. Villoslada, “Response to immunotherapy in CLIPPERS syndrome,” J Neurol, vol. 258, no. 11, pp. 2090–2092, Nov. 2011. [CrossRef]
- L. Tan, M. Agzarian, and D. W. Schultz, “CLIPPERS: Induction and maintenance of remission using hydroxychloroquine,” Neurology - Neuroimmunology Neuroinflammation, vol. 2, no. 1, p. e56, Feb. 2015. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).